Abstract
Streptococcus agalactiae is a significant pathogen that can affect both human beings and animals. The extensive current use of antibiotics has resulted in antibiotic resistance. In our previous research, we found that zinc oxide quantum dots (ZnO QDs) had inhibitory effects on antibiotic-resistant microorganisms. In this study, a strain of Streptococcus agalactiae WJYT1 with a broad antibiotic-resistant spectrum was isolated and identified from Lama glama at Sichuan Agricultural University Teaching Animal Hospital. The genome for the resistance and virulence genes was analyzed. Additionally, the antibacterial effects and anti-virulence mechanism of ZnO QDs for S. agalactiae WJYT1 were investigated. The results showed that the genome of S. agalactiae WJYT1 is 1,943,955 bp, containing 22 resistance genes and 95 virulence genes. ZnO QDs have a good antibacterial effect against S. agalactiae WJYT1 by reducing bacterial growth and decreasing the expression of virulence genes, including bibA, hylB, sip, and cip, which provides a novel potential treatment for S. agalactiae.
1. Introduction
Streptococcus agalactiae, commonly known as group B Streptococcus, was first identified by Rebecca Lancefield in the 1930s [1]. This pathogen can affect both humans and animals and is associated with various conditions, including mastitis, caseous lymphadenitis, infectious skin necrosis, and purulent infections in Lama glama [2,3]. Recently, antibiotic resistance has become a growing concern [4,5]; microbiome adaptability, pathogenicity, and transmissibility [6], posing a threat to both the environment and human health. Therefore, there is an urgent to explore a novel antibacterial strategy.
In recent years, biomedical nanomaterials have attracted great attention because of their outstanding biological characteristics and wide application prospects. At present, novel nanocomposites, such as ZnO [7], CuO/ZnCdS [8], Mn2CuO4/CdO [9], and Ag/Cu2MoO4 [10] nano-materials, have made great breakthroughs in the inhibition of bacteria and the treatment of diseases. Among them, zinc oxide quantum dots (ZnO QDs) have interested researchers due to their excellent antibacterial effect [11,12]. Relevant studies have shown that the main antimicrobial toxicity mechanism of ZnO QDs is based on their ability to induce excess ROS production [13] and the cumulative release of Zn2+ [14], which can prevent the formation and spread of bacterial biofilms, leading to bacterial death [15,16]. Our previous research found that ZnO QDs had an inhibitory effect on antibiotic-resistant microorganisms [17,18].
Virulence genes and antibiotic resistance genes are crucial in understanding the pathogenic and antibiotic resistance mechanisms of pathogens. However, there is little research on ZnO QDs for S. agalactiae virulence and antibiotic resistance genes. In this study, a strain of S. agalactiae WJYT1 with muti-antibiotic-resistance from a sick llama (Lama glama) at Sichuan Agricultural University Teaching Animal Hospital was isolated and identified. The aim of this study was to identify the virulence and antibiotic resistance genes of S. agalactiae WJYT1 as well as the potential interventional effect of ZnO QDs in treating S. agalactiae infections.
2. Results
2.1. Results for the Isolation and Identification of S. agalactiae
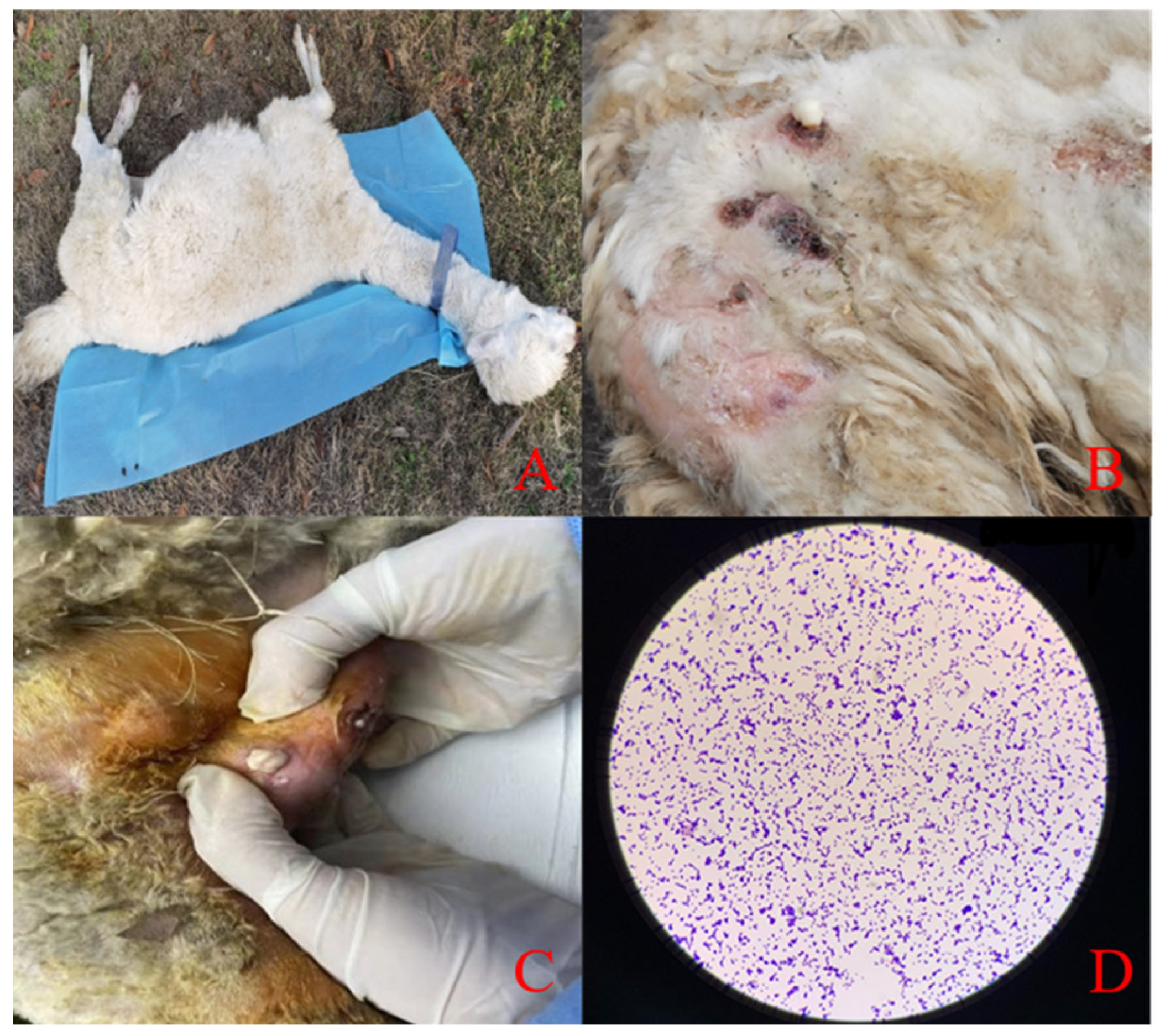
The sick Lama glama showed an increased body temperature, confusion, depression, decreased appetite, and decreased activity. A physical examination of its eyes, ears, and nasal cavity showed no obvious secretions. The palpation of its superficial lymph nodes was enlarged. The auscultation of its chest cavity had no obvious murmur while its heart rate was accelerated. The Lama glama had a disheveled coat and septic infections on all its extremities. White cheese-like nodules were observed after squeezing the abscess. The results of the microscopic examination of the isolated strain showed single or chain Gram-positive bacteria microscopically (Figure 1).
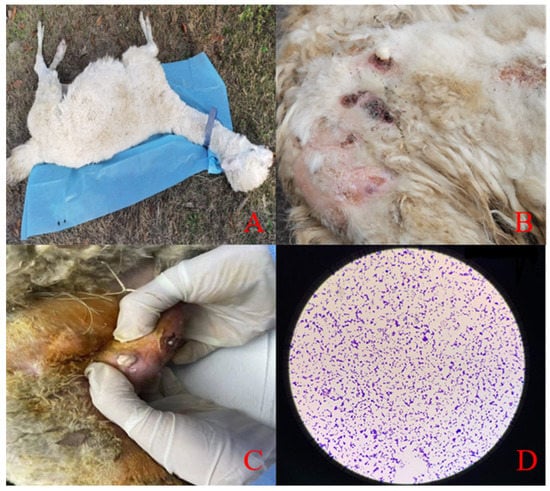
Figure 1.
(A) The general photo of the clinical case of a llama. (B) Superficial abscesses. (C) White thick juice was observed by squeezing the abscess site. (D) Isolated strain, Gram stain, 40×.
2.2. Molecular Identification Results
According to the 16S rRNA alignment, the isolated strain was distinguished as S. agalactiae, specifically S. agalactiae WJYT1. Its sequence was uploaded to the NCBI database with the accession number OQ930763.
2.3. Identification of Antibiotic Susceptibility
Our antibiotic resistance tests showed that S. agalactiae WJYT1 is resistant to all tested antibiotics, including aminoglycosides, β-lactams, sulfonamides, chloramphenicol, quinolones, glycylcyclines, tetracyclines, glycopeptides, and lincosamides (Table 1).

Table 1.
Antimicrobial resistance profile of S. agalactiae.
2.4. High-Throughput Sequencing Results
The original data were 1217 MB, and after data processing, they were filtered down to 1062 MB clean data. After genome assembly, the total genome length was 1,943,955 bp, with a GC ratio of 35.22%. According to their alignment, 6736 genes were mapped on the GO database. Specifically, 3328 genes were enriched in biological processes, many of which are related to cellular processes, metabolic processes, and localization (Figure S1). The KEGG metabolic classification showed that 63 genes were enriched in human disease, with many associated with antibiotic resistance, immune diseases, and infectious diseases (Figure S2). Similarly, through the analysis of the COG database, a total of 24 functional annotations were obtained (Figure S3). Among them, most of the gene clusters (containing 205 genes) were involved in translation, ribosomal structure, and biogenesis. The second largest category was carbohydrate transport and metabolism, with 167 genes involved.
2.5. Virulence and Pathogenic Analysis
Through their alignment in the VFDB database, a total of 95 virulence genes were identified, including the following: capsule-related genes (23 genes such as neuA, neuC, and neuD), beta-hemolysin-related genes (9 genes such as cylX, cylD, cylG), group B Streptococcus immunogenic bacterial adhesin-related genes (such as bibA), bacterial surface immunogenic protein-related genes (such as sip), hyaluronidase-related genes (such as hylB), and CAMP factor-related genes (such as cfb). The specific results are shown in Table 2.

Table 2.
Classification of virulence genes in VFDB database.
2.6. Analysis of Antibiotic Resistance Genes of S. agalactiae
The results of the resistance gene information annotated in the CARD database are shown in Table 3, of which the main mechanisms of resistance are as follows: antibiotic target alteration, antibiotic efflux, antibiotic target replacement, antibiotic inactivation. The other database of the ARDB results is listed in Supplementary Materials Table S1.

Table 3.
S. agalactiae antibiotic resistance genes and corresponding antibiotic resistance mechanisms.
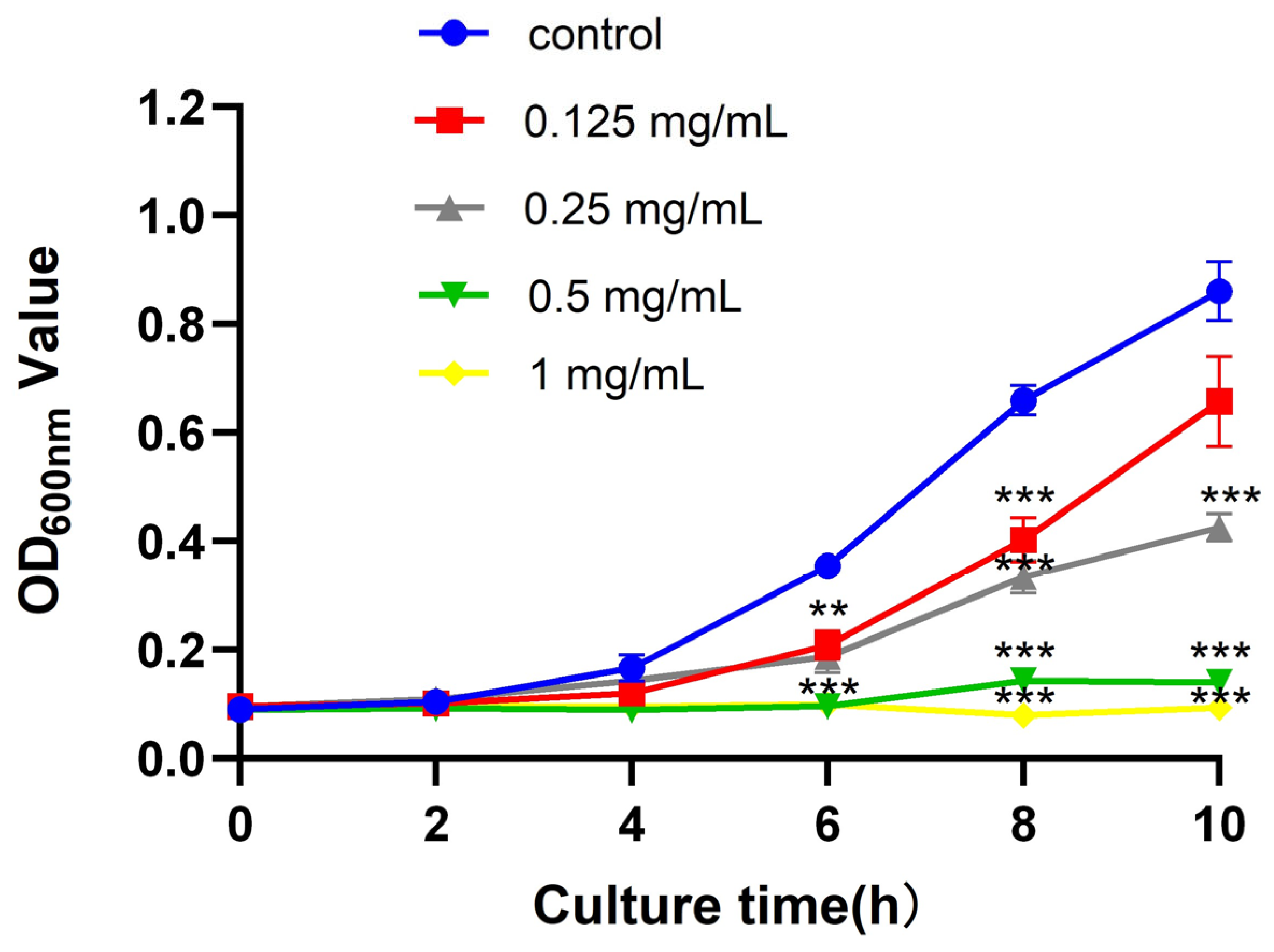
2.7. Effect of ZnO QDs on S. agalactiae
Through the plate coating experiment, the ZnO QDs were shown to have an inhibitory effect on the isolated antibiotic-resistant S. agalactiae WJYT1 with a minimum inhibitory concentration of 0.5 mg/mL (Figure S4). The growth curve experiment revealed that the antimicrobial effect of the ZnO QDs was insignificant within the first 2 h (Figure 2). After 10 h, S. agalactiae WJYT1 was significantly inhibited by the ZnO QDs with concentrations of 0.25–1 mg/mL decreasing by 49.17%, 78.3%, and 88.01% (p < 0.001), compared to those of the control group, respectively. There was no significant difference between the group with 0.125 mg/mL and the control group (p > 0.05).
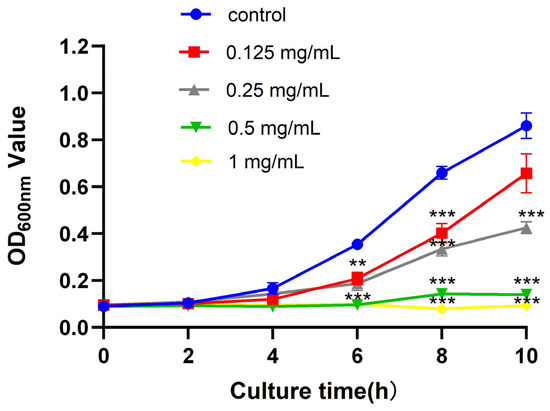
Figure 2.
Growth curves of S. agalactiae lactis under the action of different concentrations of nano-zinc oxide. Error bars refer to the SD of 3 replicates of each assay (** p < 0.01, *** p < 0.001).
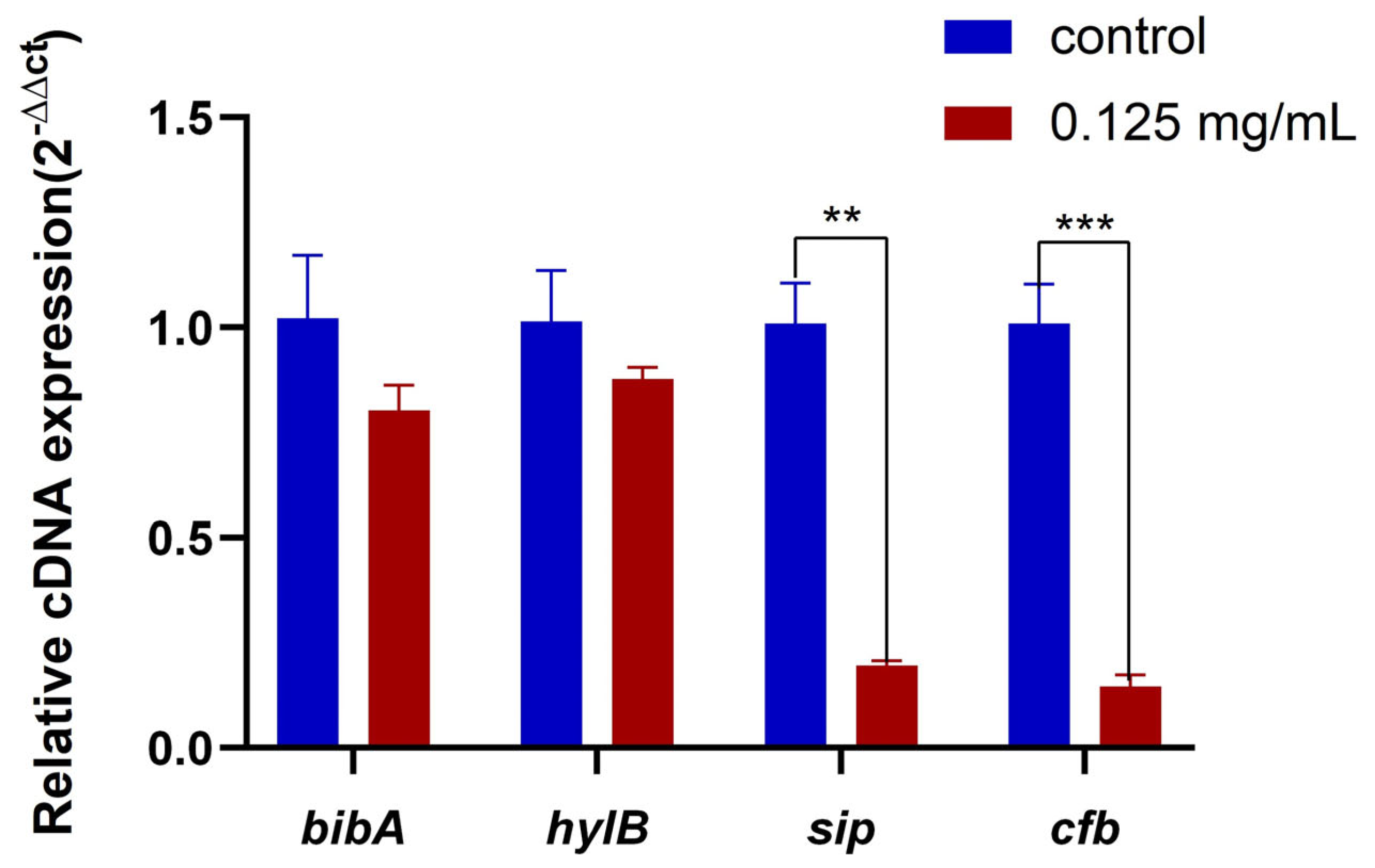
2.8. Effect of ZnO QDs on Virulence Genes of S. agalactiae
When the concentration of the ZnO QDs was 0.125 mg/mL (1/4 MIC), the expression levels of sip and cfb were significantly inhibited (Figure 3). Although there was no significant difference between the hylB and bibA genes, the transcription levels were reduced by 21.4% and 13.5%, respectively, compared to those of the control group.
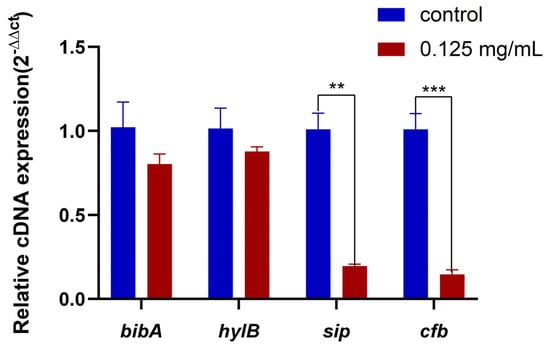
Figure 3.
Changes in the expression levels of bibA, hylB, sip, and cfb genes after different concentrations of ZnO QDs acting on S. agalactiae (** p < 0.01, *** p < 0.001). Error bars refer to the SD of 3 replicates of each assay.
3. Discussion
S. agalactiae is a pathogenic bacterium that affects both animals and humans and is a common cause of neonatal sepsis, mastitis, sepsis, and other diseases [19]. In this study, we isolated a highly antibiotic-resistant strain of S. agalactiae from a sick Lama glama in an animal hospital in Sichuan Province, China. The llama had a large abscess on the surface of its skin and had been treated with multiple ineffective antibiotics, indicating severe systemic sepsis due to S. agalactiae infection.
β-lactams, aminoglycosides, macrolides, lincosamides, fluoroquinolones, and tetracyclines are all first-line antibiotics for the treatment of S. agalactiae [20,21]. Penicillin antibiotics are the drug of choice for the treatment of S. agalactiae infections, which are typically highly sensitive to this class of antibiotics [22]. According to the treatments in the other animal hospital, the attending physicians had failed to treat the animal using the antibiotics enrofloxacin, amikacin, and meropenem. Our susceptibility results showed that the isolated S. agalactiae strain was resistant to aminoglycosides, β-lactams, sulfonamides chloramphenicol, quinolones, glycylcyclines, tetracyclines, glycopeptides, and lincosamides. Using NGS, the genes related to antibiotic resistance were found to be pbp2x, rpoB, and mexD, consistent with the resistance phenotypes. Meanwhile, related studies have shown the potential for the horizontal transfer of several of these genes [23,24,25]. Notably, we identified the pbp2x gene, a penicillin-binding protein involved in the final stages of peptidoglycan assembly and essential for bacterial growth and survival [26]. Our analysis of S. agalactiae with reduced penicillin sensitivity and insensitivity to fluoroquinolone drugs suggests possible amino acid mutations in penicillin-binding proteins such as pbp2x [27]. We also discovered the existence of rpoB, coding for the RNA polymerase β subunit, which is the target of rifampicin [28]. An essential drug in the treatment of tuberculosis and other mycobacterial infections, more than 95% of RIF-resistant mutations are associated with mutations in the rpoB gene [27]. The isolated strain’s resistance to rifamycin may be related to the expression regulation of rpoB. In addition, our analysis revealed the presence of mexD, a member of the resistance-nodulation-division (RND) antibiotic efflux pump MexCD-OprJ. Previous studies have shown that the MexCD-OprJ efflux pump is associated with multiantibiotic resistance [29]. The isolated strain’s resistance to multiple antibiotics may be related to the expression regulation of mexD. Further analyses are needed to confirm this conjecture.
S. agalactiae is a main pathogen in Lama glama mastitis, caseous lymphadenitis, infectious skin necrosis, and purulent infection [3]. To detect virulence genes, the genome of S. agalactiae WJYT1 was aligned to the VFDB database. The resulting analysis revealed the presence of several virulence genes, including hylB, cfb, sip, and bibA. Among these genes, hylB is particularly important as it plays a crucial role in invading the host and evading host immunity [30]. hylB’s primary mechanism is related to the degradation of hyaluronic acid, which enables the colonization and invasion of pathogenic bacteria at the epithelial barrier, thereby contributing to the pathogenesis of infection [31]. Cfp is a CAMP factor, which is closely related to the virulence and pathogenicity of S. agalactiae [32]. It has been shown to form discrete transmembrane pores in cell membranes, causing the lysis of components of the cell membrane, damaging host antibodies and weakening host immunity [33,34]. The pathogenicity of S. agalactiae is mainly caused by virulence factors and surface proteins. Surface immunogenic protein (Sip) is an S. agalactiae surface-exposed protein found to be present in every serotype of S. agalactiae isolates and highly conserved [35].
ZnO is a material with excellent antibacterial activity in many drug-resistant pathogens, including S. aureus, Escherichia coli (E. coli) [36], and Candida albicans [37]. Compared to traditional metal bacteriostatic materials, when the size of ZnO is reduced to the nanometer range, ZnO QDs typically exhibit additional morphologies and significant antibacterial activity against various bacterial species, e.g., E. coli, S. aureus, and Salmonella pullorum, which have been explored by numerous researchers [18,38,39,40], prompting us to explore whether they also have inhibitory effects on drug-resistant S. agalactiae in our study. Our experimental results showed that the inhibition ability of ZnO QDs for S. agalactiae WJYT1 was concentration dependent. In our study, the MIC of ZnO QDs for S. agalactiae WJYT1 was lower than that for E. coli while higher than that for S. aureus [18]. This gap may due to the strong resistance for the isolated bacterial species in our study. Although ZnO QDs at 1/4 MIC could not significantly inhibit the growth of S. agalactiae, the experimental results showed that it could significantly inhibit the expression of partial S. agalactiae virulence genes, such as sip and cfb. The pathogenic mechanism of S. agalactiae relies mainly on its ability to adhere and invade host cells, evade phagocytosis and immune clearance, and eventually produce pathogenicity [41]. The pathogenicity of S. agalactiae depends mainly on its virulence genes, of which cfp and sip can help the bacterium invade and evade host immunity [41]. Our experimental results showed that ZnO QDs can inhibit partial virulence without inhibiting growth. Therefore, it is speculated that ZnO QDs may affect the ability of S. agalactiae to invade host cells and evade host immunity by inhibiting the expression of these virulence genes. The effect mechanism of ZnO QDs on bacteria may include the following: (1) the smaller particle size of ZnO QDs makes it easier to attach to the bacterial surface, which is conducive to reactive oxygen species (ROS) and Zn2+ entering the bacterial body, thereby producing beneficial antibacterial activity; and (2) ZnO QDs can interact with the surface of bacteria, even entering the cell nucleus, interfering with bacterial biochemical reactions [42]. Interestingly, some research reports have shown that ZnO QDs are non-toxic to animal cells with good biocompatibility, while harmful to microorganisms, indicating their potential use as antibacterial agents [43]. In our study, the decrease in the invading and evading genes proved the effect of the ZnO QDs on S. agalactiae. However, the specific mechanism of action in Lama glama requires further in-depth research.
Llamas have a high economic value due to their fur, meat, skin, and milk. In recent years, llamas have become highly social animals and live in animal parks, attracting large numbers of tourists. However, close contact with llamas increases the risk of transmission of zoonotic diseases. Although currently no human infection with S. agalactiae has been reported, the potential for the transmission of S. agalactiae from animals to humans has been briefly described in cattle [44]. Therefore, there may be a possible link between Lama glama exposure and S. agalactiae in humans. Horizontal transfer is an important mechanism for strengthening antibiotic resistance and enriching resistance genes. We isolated a highly antibiotic-resistant strain in Lama glama, which indicated that it may have shared horizontal metastasis with many resistant bacteria. The llama in our study came from a local alpaca park, but it was kept alone and not in contact with other animals, so the possibility of human movement causing the transfer of resistant genes cannot be ruled out. Therefore, we should pay more attention to the prevention and control of group B Streptococcus in the future.
4. Materials and Methods
4.1. Basic Information of Animals
In November 2021, a sick llama (Lama glama) was brought to Sichuan Agricultural University for treatment. The llama had been treated with various antibiotics, including enrofloxacin, amikacin, and meropenem previously in another animal hospital. The sick llama showed symptoms of sepsis, including increased body temperature, confusion, depression, decreased appetite, and decreased activity.
4.2. Isolation and Identification of S. agalactiae
Samples were collected from lesions in the extremities and streaked in Luria-Bertani (LB) medium with 5% defibrous sheep blood, incubated at 37 °C for 48 h. Individual colonies with different morphologies were selected and purified through three continuous passages on blood agar. Purified isolates were stored at −80 °C in 50% glycerol for subsequent experiments. Gram staining was performed to identify bacterial morphology.
4.3. Molecular Identification
DNA of the bacterial isolates was extracted using a DNA Extraction Kit (Tiangen, Beijing, China) and measured by ND-1000 microUV spectrophotometer (NanoDrop Technologies, Wilmington, DE, USA). The primers 27F (5′-AGAGTTTGATCCTGGCTCAG-3′) and 1492R (5′-GGTTACCTTGTTACGACTT-3′) were used to amplify 16S rDNA gene. PCR reactions (25 μL) contained 12.5 μL PCR Master Mix, 9.5 μL nuclease-free H2O, 1 μL forward primer, 1 μL reverse primer, and 1 μL DNA sample. The PCR procedure was performed as follows: predenaturation at 94 °C for 5 min, followed by 30 cycles (30 s of denaturation at 94 °C, 30 s of annealing at 55 °C, and 1 min of extension at 72 °C), with a final extension at 72 °C for 7 min. The PCR products were stored at 4 °C for subsequent checking on 2% agarose gel and sent to Sangon Biotech Co. Ltd. (Shanghai, China) for sequencing. A homology search was performed by Blast function in the GenBank database (http://www.ncbi.nlm.nih.gov/BLAST, accessed on 22 November 2021).
4.4. Antibiotic Susceptibility Testing
The disc-diffusion test was used to assess the antibiotic susceptibility of the bacteria isolated above. Fourteen antimicrobials were tested, including amikacin, gentamicin, meropenem, cefepime, ampicillin, amoxicillin, ceftriaxone, cefoperazone, chloramphenicol, ciprofloxacin, tigecycline, doxycycline, vancomycin, and clindamycin. The diameters (mm) of the inhibition zones were measured to classify the antibiotic susceptibility as resistance (R), moderate susceptibility (MS), or susceptibility (S) based on the parameters of the Clinical and Laboratory Standards Institute [45].
4.5. High-Throughput Sequencing
The purified DNA was sent to Novogene Co. Ltd. (Beijing, China) for Hi-seq 2000 Next Generation Sequencing (NGS). After sequencing, clean data were obtained, assembled by SOAP denovo (version 2.04) [46,47], SPAdes (version 3.6.2) [48], and AbySS (version 2.0) [49], and finally integrated by CISA (version 1.3) [50]. The protein sequences of the predicted genes were compared to the GO, KEGG, and COG databases as well as the classic protein function database using Diamond (version 2.1.8) [51]. The amino acid sequences were aligned to VFDB (version 2022) and ARDB (version 1.1) [52] databases using Diamond. The amino acid sequences of target species were compared with the CARD database (version 3.2.2) using Resistance Gene Identifier (RGI) software provided by the CARD database, which obtained annotated results [53]. The raw data were uploaded to NCBI database with the accession number PRJNA970803.
4.6. Antibacterial Effect of ZnO QDs
To investigate the effect of ZnO QDs on S. agalactiae, we conducted a series of experiments. The enriched bacterial solution was firstly adjusted to a concentration of 1 × 108 CFU/mL. The microbroth dilution method was then performed to determine the minimum inhibitory concentration (MIC). The prepared ZnO QDs were added to the bacterial solution to obtain concentrations of 0, 1/4, 1/2, 1, and 2 MIC, respectively. The growth curve was measured for 10 h in each group cultured in a shaker at 37 °C.
4.7. Detection of Virulence Genes
To further investigate the effect of ZnO QDs on virulence genes, four virulence genes including bibA, hylB, sip, and cip, representing adhesion and colonization, invasion, and immune evasion, were selected. ZnO QDs with a concentration of 1/4 MIC and no significant inhibitory effect at 10 h were added to the bacterial solution and incubated at 37 °C for 24 h. Bacterial total RNA was extracted using an RNA extraction kit (Tiangen, Beijing, China). Reverse transcription was performed with a reverse transcription kit (Tsingke, Beijing, China). The mRNA expression of virulence genes was detected by qPCR using SYBR Green dye (Servicebio, Wuhan, China). IBM SPSS Statistics (version 27) was used for statistical analysis.
5. Conclusions
S. agalactiae is a kind of conditional pathogen, which can cause serious infection when the body’s immunity is decreased. Currently, antibiotic resistance is increasing the urgency of finding alternative treatment methods. Our study illustrated that a biomedical nanomaterial, ZnO QDs, could inhibit the growth of S. agalactiae with a broad antibiotic-resistant spectrum isolated from Lama glama, further reducing the expression of the virulence gene even with a low concentration. Therefore, ZnO QDs are expected to become a potential alternative for antibiotic-resistant bacteria.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/molecules28135115/s1, Figure S1: S. agalactiae WJYT1 gene function annotation GO functional classification chart; Figure S2: Functional annotation of the WJYT1 gene of S. agalactiae KEGG metabolic pathway; Figure S3: S. agalactiae WJYT1 gene function annotation COG function classification chart; Figure S4: ZnO QDs has an inhibitory effect on antibiotic-resistance S. agalactiae WJYT1; Table S1: S. agalactiae ARDB database alignment.
Author Contributions
Conceptualization: G.P. and Z.Z. (Ziyao Zhou); clinical case handling: Y.C., Y.Z. and X.Z.; formal analysis: T.Z.; software: H.L.; methodology: Z.Z. (Zhijun Zhong); resources: Y.H.; Writing—original draft: T.Z.; Writing—review and editing: Z.Z. (Ziyao Zhou), F.L., X.W. and G.P. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by Sichuan Wolong National Nature Reserve Administration (510000-02-064387), the State Forestry and Grassland Administration (2022-2222219002), and Qingzhen City Science and Technology Project Support Program (2023-25).
Institutional Review Board Statement
The animal use protocol has been reviewed and approved by the Sichuan Agricultural University Animal Ethical and Welfare Committee, with the approval number 20220012.
Data Availability Statement
The 16S rRNA sequencing data are available in the NCBI database with the accession number OQ930763. The genome raw data are available in the NCBI database with the accession number PRJNA970803.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Raabe, V.N.; Shane, A.L. Group B Streptococcus (Streptococcus agalactiae). Microbiol. Spectr. 2019, 7, 17. [Google Scholar] [CrossRef] [PubMed]
- Fischer, A.; Liljander, A.; Kaspar, H.; Muriuki, C.; Fuxelius, H.H.; Bongcam-Rudloff, E.; de Villiers, E.P.; Huber, C.A.; Frey, J.; Daubenberger, C.; et al. Camel Streptococcus agalactiae populations are associated with specific disease complexes and acquired the tetracycline resistance gene tetM via a Tn916-like element. Vet. Res. 2013, 44, 86. [Google Scholar] [CrossRef] [PubMed]
- Tavella, A.; Bettini, A.; Cocchi, M.; Idrizi, I.; Colorio, S.; Viel, L.; Zanardello, C.; Zanolari, P. Isolation of Streptococcus agalactiae in a female llama (Lama glama) in South Tyrol (Italy). BMC Vet. Res. 2018, 14, 343. [Google Scholar] [CrossRef] [PubMed]
- Lerminiaux, N.A.; Cameron, A.D.S. Horizontal transfer of antibiotic resistance genes in clinical environments. Can. J. Microbiol. 2019, 65, 34–44. [Google Scholar] [CrossRef]
- Frieri, M.; Kumar, K.; Boutin, A. Antibiotic resistance. J. Infect. Public Health 2017, 10, 369–378. [Google Scholar] [CrossRef]
- Paitan, Y. Current Trends in Antimicrobial Resistance of Escherichia coli. Curr. Top. Microbiol. Immunol. 2018, 416, 181–211. [Google Scholar] [CrossRef]
- Vijayakumar, S.; Saravanakumar, K.; Malaikozhundan, B.; Divya, M.; Vaseeharan, B.; Durán-Lara, E.F.; Wang, M.-H. Biopolymer K-carrageenan wrapped ZnO nanoparticles as drug delivery vehicles for anti MRSA therapy. Int. J. Biol. Macromol. 2020, 144, 9–18. [Google Scholar] [CrossRef]
- Lei, C.; Sun, N.; Wu, H.; Zhao, Y.; Yu, C.; Janani, B.J.; Fakhri, A. Bio-photoelectrochemical degradation, and photocatalysis process by the fabrication of copper oxide/zinc cadmium sulfide heterojunction nanocomposites: Mechanism, microbial community and antifungal analysis. Chemosphere 2022, 308, 136375. [Google Scholar] [CrossRef]
- Yao, X.; BahrAluloom, Y.J.; Jawad, S.F.; Abdtawfeeq, T.H.; Al-janabi, D.R.; Ahmad, N.; Alshehri, A.; Hadrawi, S.K.; Al-Taee, M.M.; Riadi, Y. Multipurpose properties the Z-scheme dimanganese copper oxide/cadmium sulfide nanocomposites for photo-or photoelectro-catalytic, antibacterial applications, and thiamine detection process. J. Photochem. Photobiol. A: Chem. 2023, 436, 114374. [Google Scholar] [CrossRef]
- Liu, Z.; Hadi, M.A.; Aljuboory, D.S.; Ali, F.A.; Jawad, M.A.; Ameen, A.-A.; Hadrawi, S.K.; Mundher, T.; Riadi, Y.; Amer, R.F. High efficiency of Ag0 decorated Cu2MoO4 nanoparticles for heterogeneous photocatalytic activation, bactericidal system, and detection of glucose from blood sample. J. Photochem. Photobiol. B Biol. 2022, 236, 112571. [Google Scholar] [CrossRef]
- Mishra, P.K.; Mishra, H.; Ekielski, A.; Talegaonkar, S.; Vaidya, B. Zinc oxide nanoparticles: A promising nanomaterial for biomedical applications. Drug Discov. Today 2017, 22, 1825–1834. [Google Scholar] [CrossRef]
- Ruszkiewicz, J.A.; Pinkas, A.; Ferrer, B.; Peres, T.V.; Tsatsakis, A.; Aschner, M. Neurotoxic effect of active ingredients in sunscreen products, a contemporary review. Toxicol. Rep. 2017, 4, 245–259. [Google Scholar] [CrossRef]
- Zhang, Z.-Y.; Xiong, H.M. Photoluminescent ZnO nanoparticles and their biological applications. Materials 2015, 8, 3101–3127. [Google Scholar] [CrossRef]
- Dutta, R.K.; Nenavathu, B.P.; Gangishetty, M.K.; Reddy, A.V.R. Antibacterial effect of chronic exposure of low concentration ZnO nanoparticles on E. Coli. J. Environ. Sci. Health Part A 2013, 48, 871–878. [Google Scholar] [CrossRef]
- Luo, Z.; Liu, J.; Lin, H.; Ren, X.; Tian, H.; Liang, Y.; Wang, W.; Wang, Y.; Yin, M.; Huang, Y. In situ fabrication of nano ZnO/BCM biocomposite based on MA modified bacterial cellulose membrane for antibacterial and wound healing. Int. J. Nanomed. 2020, 15, 1–15. [Google Scholar] [CrossRef]
- Chen, H.; Zhang, M.; Li, B.; Chen, D.; Dong, X.; Wang, Y.; Gu, Y. Versatile antimicrobial peptide-based ZnO quantum dots for in vivo bacteria diagnosis and treatment with high specificity. Biomaterials 2015, 53, 532–544. [Google Scholar] [CrossRef]
- Shu, G.; Xu, D.; Xie, S.; Chang, L.-J.; Liu, X.; Yang, J.; Li, Y.; Wang, X. The antioxidant, antibacterial, and infected wound healing effects of ZnO quantum dots-chitosan biocomposite. Appl. Surf. Sci. 2023, 611, 155727. [Google Scholar] [CrossRef]
- Li, Y.; Xie, S.; Xu, D.; Shu, G.; Wang, X. Antibacterial activity of ZnO quantum dots and its protective effects of chicks infected withSalmonella pullorum. Nanotechnology 2021, 32, 505104. [Google Scholar] [CrossRef]
- M100-S23; Performance Standards for Antimicrobial Susceptibility Testing: Twenty-Third Informational Supplement. Clinical and Laboratory Standards Institute: Wayne, PA, USA, 2017.
- Li, R.; Zhu, H.; Ruan, J.; Qian, W.; Fang, X.; Shi, Z.; Li, Y.; Li, S.; Shan, G.; Kristiansen, K. De novo assembly of human genomes with massively parallel short read sequencing. Genome Res. 2010, 20, 265–272. [Google Scholar] [CrossRef]
- Li, R.; Li, Y.; Kristiansen, K.; Wang, J.J.B. SOAP: Short oligonucleotide alignment program. Bioinformatics 2008, 24, 713–714. [Google Scholar] [CrossRef]
- Bankevich, A.; Nurk, S.; Antipov, D.; Gurevich, A.A.; Dvorkin, M.; Kulikov, A.S.; Lesin, V.M.; Nikolenko, S.I.; Pham, S.; Prjibelski, A. SPAdes: A new genome assembly algorithm and its applications to single-cell sequencing. J. Comput. Biol. 2012, 19, 455–477. [Google Scholar] [CrossRef] [PubMed]
- Simpson, J.T.; Wong, K.; Jackman, S.D.; Schein, J.E.; Jones, S.J.; Birol, I. ABySS: A parallel assembler for short read sequence data. Genome Res. 2009, 19, 1117–1123. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.H.; Liao, Y.C. CISA: Contig integrator for sequence assembly of bacterial genomes. PLoS ONE 2013, 8, e60843. [Google Scholar] [CrossRef] [PubMed]
- Buchfink, B.; Xie, C.; Huson, D.H. Fast and sensitive protein alignment using DIAMOND. Nat. Methods 2015, 12, 59–60. [Google Scholar] [CrossRef]
- Liu, B.; Pop, M.J.N.A.R. ARDB—antibiotic resistance genes database. Nucleic Acids Res. 2009, 37, D443–D447. [Google Scholar] [CrossRef]
- Alcock, B.P.; Raphenya, A.R.; Lau, T.T.; Tsang, K.K.; Bouchard, M.; Edalatmand, A.; Huynh, W.; Nguyen, A.-L.V.; Cheng, A.A.; Liu, S. CARD 2020: Antibiotic resistome surveillance with the comprehensive antibiotic resistance database. Nucleic Acids Res. 2020, 48, D517–D525. [Google Scholar] [CrossRef]
- Zimmermann, P.; Gwee, A.; Curtis, N. The controversial role of breast milk in GBS late-onset disease. J. Infect. 2017, 74 (Suppl. S1), S34–S40. [Google Scholar] [CrossRef]
- Haenni, M.; Lupo, A.; Madec, J.Y. Antimicrobial Resistance in Streptococcus spp. Microbiol. Spectr. 2018, 6. [Google Scholar] [CrossRef]
- Guo, H.; Fu, M.; Peng, Q.; Chen, Z.; Liu, J.; Qiu, Y.; Huang, Y. Antimicrobial resistance and molecular characterization of Streptococcus agalactiae from pregnant women in southern China. J. Infect. Dev. Ctries. 2019, 13, 802–809. [Google Scholar] [CrossRef]
- Rigvava, S.; Kharebava, S.; Giorgobiani, T.; Dvalidze, T.; Goderdzishvili, M. Identification And Antibiotic Susceptibility Patterns Of Streptococcus agalactiae. Georgian Med. News 2019, 297, 149–153. [Google Scholar]
- Gibson, P.S.; Bexkens, E.; Zuber, S.; Cowley, L.A.; Veening, J.W. The acquisition of clinically relevant amoxicillin resistance in Streptococcus pneumoniae requires ordered horizontal gene transfer of four loci. PLoS Pathog. 2022, 18, e1010727. [Google Scholar] [CrossRef]
- Suchland, R.J.; Sandoz, K.M.; Jeffrey, B.M.; Stamm, W.E.; Rockey, D.D. Horizontal transfer of tetracycline resistance among Chlamydia spp. in vitro. Antimicrob. Agents Chemother. 2009, 53, 4604–4611. [Google Scholar] [CrossRef]
- Remenant, B.; de Cambiaire, J.-C.; Cellier, G.; Jacobs, J.M.; Mangenot, S.; Barbe, V.; Lajus, A.; Vallenet, D.; Medigue, C.; Fegan, M. Ralstonia syzygii, the blood disease bacterium and some Asian R. solanacearum strains form a single genomic species despite divergent lifestyles. PLoS ONE 2011, 6, e24356. [Google Scholar] [CrossRef]
- Schweizer, I.; Peters, K.; Stahlmann, C.; Hakenbeck, R.; Denapaite, D. Penicillin-binding protein 2x of Streptococcus pneumoniae: The mutation Ala707Asp within the C-terminal PASTA2 domain leads to destabilization. Microb. Drug Resist. 2014, 20, 250–257. [Google Scholar] [CrossRef]
- Piccinelli, G.; Carlentini, G.; Gargiulo, F.; Caruso, A.; De Francesco, M.A. Analysis of Point Mutations in the pbp2x, pbp2b, and pbp1a Genes of Streptococcus agalactiae and Their Relation with a Reduced Susceptibility to Cephalosporins. Microb. Drug Resist. 2017, 23, 1019–1024. [Google Scholar] [CrossRef]
- André, E.; Goeminne, L.; Cabibbe, A.; Beckert, P.; Mukadi, B.K.; Mathys, V.; Gagneux, S.; Niemann, S.; Van Ingen, J.; Cambau, E.J.C.M.; et al. Consensus numbering system for the rifampicin resistance-associated rpoB gene mutations in pathogenic mycobacteria. Clin. Microbiol. Infect. 2017, 23, 167–172. [Google Scholar] [CrossRef]
- Terzi, H.A.; Kulah, C.; Ciftci, I.H. The effects of active efflux pumps on antibiotic resistance in Pseudomonas aeruginosa. World J. Microbiol. Biotechnol. 2014, 30, 2681–2687. [Google Scholar] [CrossRef]
- Coleman, M.; Armistead, B.; Orvis, A.; Quach, P.; Brokaw, A.; Gendrin, C.; Sharma, K.; Ogle, J.; Merillat, S.; Dacanay, M.; et al. Hyaluronidase Impairs Neutrophil Function and Promotes Group B Streptococcus Invasion and Preterm Labor in Nonhuman Primates. mBio 2021, 12, eaah4576. [Google Scholar] [CrossRef]
- Sun, X.; Wang, Z.; Bi, Y.; Wang, Y.; Liu, H. Genetic and functional characterization of the hyaluronate lyase HylB and the beta-N-acetylglucosaminidase HylZ in Streptococcus zooepidemicus. Curr. Microbiol. 2015, 70, 35–42. [Google Scholar] [CrossRef]
- Jin, T.; Brefo-Mensah, E.; Fan, W.; Zeng, W.; Li, Y.; Zhang, Y.; Palmer, M. Crystal structure of the Streptococcus agalactiae CAMP factor provides insights into its membrane-permeabilizing activity. J. Biol. Chem. 2018, 293, 11867–11877. [Google Scholar] [CrossRef]
- Hensler, M.E.; Quach, D.; Hsieh, C.J.; Doran, K.S.; Nizet, V. CAMP factor is not essential for systemic virulence of Group B Streptococcus. Microb. Pathog. 2008, 44, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Lang, S.; Palmer, M. Characterization of Streptococcus agalactiae CAMP factor as a pore-forming toxin. J. Biol. Chem. 2003, 278, 38167–38173. [Google Scholar] [CrossRef] [PubMed]
- Huang, L.Y.; Wang, K.Y.; Xiao, D.; Chen, D.F.; Geng, Y.; Wang, J.; He, Y.; Wang, E.L.; Huang, J.L.; Xiao, G.Y. Safety and immunogenicity of an oral DNA vaccine encoding Sip of Streptococcus agalactiae from Nile tilapia Oreochromis niloticus delivered by live attenuated Salmonella typhimurium. Fish Shellfish Immunol. 2014, 38, 34–41. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.M.; Tsay, L.Y. ZnO quantum dots-decorated ZnO nanowires for the enhancement of antibacterial and photocatalytic performances. Nanotechnology 2015, 26, 395704. [Google Scholar] [CrossRef]
- Liu, J.; Wang, Y.; Ma, J.; Peng, Y.; Wang, A. A review on bidirectional analogies between the photocatalysis and antibacterial properties of ZnO. J. Alloy. Compd. 2019, 783, 898–918. [Google Scholar] [CrossRef]
- Brayner, R.; Ferrari-Iliou, R.; Brivois, N.; Djediat, S.; Benedetti, M.F.; Fiévet, F. Toxicological impact studies based on Escherichia coli bacteria in ultrafine ZnO nanoparticles colloidal medium. Nano Lett. 2006, 6, 866–870. [Google Scholar] [CrossRef]
- Jalal, R.; Goharshadi, E.K.; Abareshi, M.; Moosavi, M.; Yousefi, A.; Nancarrow, P. ZnO nanofluids: Green synthesis, characterization, and antibacterial activity. Mater. Chem. Phys. 2010, 121, 198–201. [Google Scholar] [CrossRef]
- Jones, N.; Ray, B.; Ranjit, K.T.; Manna, A.C. Antibacterial activity of ZnO nanoparticle suspensions on a broad spectrum of microorganisms. FEMS Microbiol. Lett. 2008, 279, 71–76. [Google Scholar] [CrossRef]
- Yuan, X.Y.; Liu, H.Z.; Liu, J.F.; Sun, Y.; Song, Y. Pathogenic mechanism, detection methods and clinical significance of group B Streptococcus. Future Microbiol. 2021, 16, 671–685. [Google Scholar] [CrossRef]
- Seil, J.T.; Webster, T.J. Antimicrobial applications of nanotechnology: Methods and literature. Int. J. Nanomed. 2012, 7, 2767. [Google Scholar]
- Padmavathy, N.; Vijayaraghavan, R. Enhanced bioactivity of ZnO nanoparticles-an antimicrobial study. Sci. Technol. Adv. Mater 2008, 9, 035004. [Google Scholar] [CrossRef]
- Carvalho-Castro, G.A.; Silva, J.R.; Paiva, L.V.; Custódio, D.A.C.; Moreira, R.O.; Mian, G.F.; Prado, I.A.; Chalfun-Junior, A.; Costa, G.M. Molecular epidemiology of Streptococcus agalactiae isolated from mastitis in Brazilian dairy herds. Braz. J. Microbiol. Publ. Braz. Soc. Microbiol. 2017, 48, 551–559. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).