Duguetia pycnastera Sandwith (Annonaceae) Leaf Essential Oil Inhibits HepG2 Cell Growth In Vitro and In Vivo
Abstract
:1. Introduction
2. Results and Discussion
2.1. Chemical Composition of D. pycnastera Leaf EO
2.2. D. pycnastera Leaf EO Has In Vitro Cytotoxic Activity
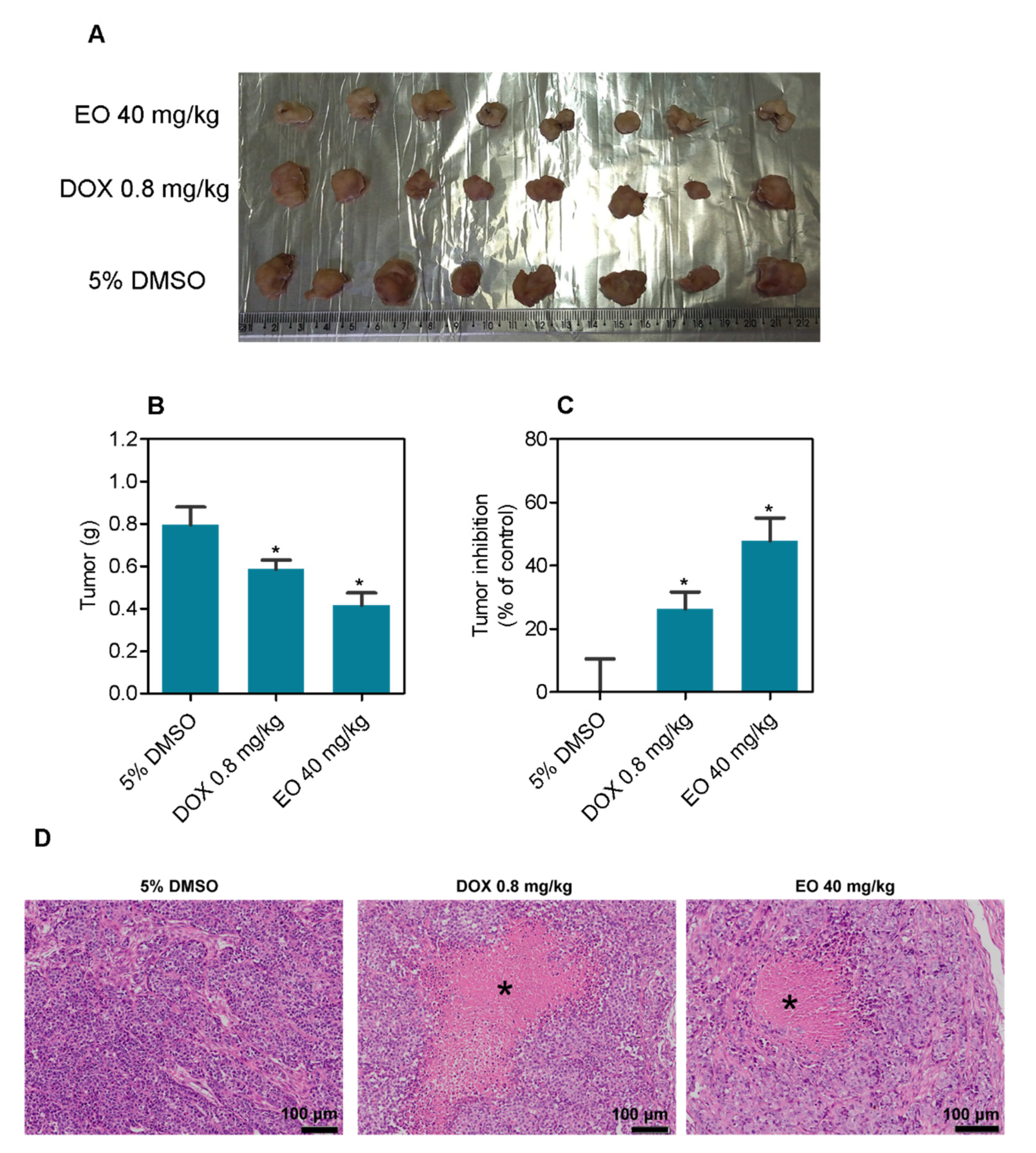
2.3. D. pycnastera Leaf EO Has an Antitumor Effect In Vivo
3. Materials and Methods
3.1. Botanical Material
3.2. Chemical Evaluation
3.2.1. Essential Oil Extraction
3.2.2. GC–FID and GC–MS Analyses
3.3. Pharmacological Evaluation
3.3.1. In Vitro
Cells
Alamar Blue Assay
Internucleosomal DNA Fragmentation and Cell Cycle Distribution
3.4. In Vivo
3.4.1. Animals
3.4.2. Human Liver Cancer Xenograft Model
3.4.3. Systemic Toxicity Assessment
3.5. Statistical Analysis
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Muhammad, I.; Dunbar, D.C.; Takamatsu, S.; Walker, L.A.; Clark, A.M. Antimalarial, cytotoxic, and antifungal alkaloids from Duguetia hadrantha. J. Nat. Prod. 2001, 64, 559–562. [Google Scholar] [CrossRef]
- Brastianos, H.C.; Sturgeon, C.M.; Roberge, M.; Andersen, R.J. Inhibition of the G2 DNA damage checkpoint by oliveroline isolated from Duguetia odorata. J. Nat. Prod. 2007, 70, 287–288. [Google Scholar] [CrossRef]
- Matos, M.F.C.; Leite, L.I.S.P.; Brustolim, D.; De Siqueira, J.M.; Carollo, C.A.; Hellmann, A.R.; Pereira, N.F.G.; Da Silva, D.B. Antineoplastic activity of selected constituents of Duguetia glabriuscula. Fitoterapia 2006, 77, 227–229. [Google Scholar] [CrossRef]
- Silva, D.B.; Tulli, E.C.; Militão, G.C.; Costa-Lotufo, L.V.; Pessoa, C.; de Moraes, M.O.; Albuquerque, S.; de Siqueira, J.M. The antitumoral, trypanocidal and antileishmanial activities of extract and alkaloids isolated from Duguetia furfuracea. Phytomedicine 2009, 16, 1059–1063. [Google Scholar] [CrossRef]
- Rodrigues, A.C.B.C.; Bomfim, L.M.; Neves, S.P.; Menezes, L.R.A.; Dias, R.B.; Soares, M.B.P.; Prata, A.P.N.; Rocha, C.A.G.; Costa, E.V.; Bezerra, D.P. Antitumor Properties of the Essential Oil from the Leaves of Duguetia gardneriana. Planta Med. 2015, 81, 798–803. [Google Scholar] [CrossRef]
- Paz, W.H.P.; de Oliveira, R.N.; Heerdt, G.; Angolini, C.F.F.; S de Medeiros, L.; Silva, V.R.; Santos, L.S.; Soares, M.B.P.; Bezerra, D.P.; Morgon, N.H.; et al. Structure-Based Molecular Networking for the Target Discovery of Oxahomoaporphine and 8-Oxohomoaporphine Alkaloids from Duguetia surinamensis. J. Nat. Prod. 2019, 82, 2220–2228. [Google Scholar] [CrossRef]
- Souza, C.A.S.; Nardellia, V.B.; Paza, W.H.P.; Pinheiro, M.L.B.; Rodrigues, A.C.B.C.; Bomfim, L.M.; Soares, M.B.P.; Bezerra, D.P.; Chaar, J.S.; Koolen, H.H.F.; et al. Asarone-derived Phenylpropanoids and isoquinoline-derived alkaloids from the bark of Duguetia pycnastera (Annonaceae) and their cytotoxicities. Quim. Nova 2020, 15, 1–7. [Google Scholar] [CrossRef]
- Maas, P.J.M.; Maas, H.; Miralha, J.M.S.; Junikka, L. Flora da Reserva Ducke, Amazonas, Brasil: Annonaceae. Rodriguesia 2007, 58, 617–662. [Google Scholar] [CrossRef]
- DeFilipps, R.A.; Maina, S.L.; Crepin, J. Medicinal Plants of the Guianas (Guyana, Surinam, French Guiana). Departament of Botany, National Museum of Natural History, Smithsonian Institution: Washington, DC, USA, 2004; pp. 20013–27012. [Google Scholar]
- Nardelli, V.B.; Souza, C.A.S.; Chaar, J.S.; Koolen, H.H.F.; Silva, F.M.A.; Costa, E.V. Isoquinoline-derived alkaloids and one terpene lactone from the leaves of Duguetia pycnastera (Annonaceae). Biochem. Syst. Ecol. 2021, 94, 23–26. [Google Scholar] [CrossRef]
- Maia, J.G.S.; Andrade, E.H.A.; Carreira, L.M.M.; Oliveira, J. Essential oil composition from Duguetia species (annonaceae). J. Essent. Oil Res. 2006, 18, 60–63. [Google Scholar] [CrossRef]
- Van Den Dool, H.; Kratz, P.D. A generalization of the retention index system including linear temperature programmed gas-liquid partition chromatography. J. Chromatogr. A 1963, 11, 463–471. [Google Scholar] [CrossRef]
- Adams, R.P. Identification of Essential Oil Components by Gas Chromatography/Mass Spectroscopy, 4th ed.; Allured Publishing Corp.: Carol Stream, IL, USA, 2007; 803p. [Google Scholar]
- Santos, A.C.d.; Nogueira, M.L.; Oliveira, F.P.d.; Costa, E.V.; Bezerra, D.P. Essential Oils of Duguetia Species A. St. Hill (Annonaceae): Chemical Diversity and Pharmacological Potential. Biomolecules 2022, 12, 615. [Google Scholar] [CrossRef]
- Sousa, O.V.; Del-Vechio-Vieira, G.; Alves, M.S.; Araújo, A.A.L.; Pinto, M.A.O.; Amaral, M.P.H.; Rodarte, M.P.; Kaplan, M.A. Chemical composition and biological activities of the essential oils from Duguetia lanceolata St. Hil. barks. Molecules 2012, 17, 11056–11066. [Google Scholar] [CrossRef]
- Silva, D.B.; Tulli, E.C.O.; Garcez, W.S.; Nascimento, E.A.; Siqueira, J.M. Chemical constituents of the underground stem bark of Duguetia furfuracea (Annonaceae). J. Braz. Chem. Soc. 2007, 18, 1560–1565. [Google Scholar] [CrossRef]
- Galvão, A.F.C.; Araújo, M.d.S.; Silva, V.R.; Santos, L.d.S.; Dias, R.B.; Rocha, C.A.G.; Soares, M.B.P.; Silva, F.M.A.d.; Koolen, H.H.F.; Zengin, G.; et al. Antitumor Effect of Guatteria olivacea R. E. Fr. (Annonaceae) Leaf Essential Oil in Liver Cancer. Molecules 2022, 27, 4407. [Google Scholar] [CrossRef]
- Ribeiro, S.S.; Jesus, A.M.; Anjos, C.S.; Silva, T.B.; Santos, A.D.; Jesus, J.R.; Andrade, M.S.; Sampaio, T.S.; Gomes, W.F.; Alves, P.B.; et al. Evaluation of the cytotoxic activity of some Brazilian medicinal plants. Planta Med. 2012, 78, 1601–1606. [Google Scholar] [CrossRef]
- Britto, A.C.; Oliveira, A.C.; Henriques, R.M.; Cardoso, G.M.; Bomfim, D.S.; Carvalho, A.A.; Moraes, M.O.; Pessoa, C.; Pinheiro, M.L.; Costa, E.V.; et al. In vitro and in vivo antitumor effects of the essential oil from the leaves of Guatteria friesiana. Planta Med. 2012, 78, 409–414. [Google Scholar] [CrossRef]
- Bay, M.; Oliveira, J.V.S.; Sales-Junior, P.A.; Murta, S.M.F.; Santos, A.R.; Bastos, I.S.; Orlandi, P.P.; Sousa-Junior, P.T. In vitro Trypanocidal and Antibacterial Activities of Essential Oils from Four Species of the Family Annonaceae. Chem. Biodivers. 2019, 16, e1900359. [Google Scholar] [CrossRef]
- Palazzo, M.C.; Wright, H.L.; Agius, B.R.; Wright, B.S.; Moriarity, D.M.; Haber, W.A.; Setzer, W.N. Chemical compositions and biological activities of leaf essential oils of six species of Annonaceae from Monteverde. Costa Rica. Rec. Nat. Prod. 2009, 3, 153–160. [Google Scholar]
- Silva, E.B.; Matsuo, A.L.; Figueiredo, C.R.; Chaves, M.H.; Sartorelli, P.; Lago, J.H. Chemical constituents and cytotoxic evaluation of essential oils from leaves of Porcelia macrocarpa (Annonaceae). Nat. Prod. Commun. 2013, 8, 277–279. [Google Scholar] [CrossRef] [Green Version]
- Bomfim, L.M.; Menezes, L.R.; Rodrigues, A.C.; Dias, R.B.; Rocha, C.A.; Soares, M.B.; Neto, A.F.; Nascimento, M.P.; Campos, A.F.; Silva, L.C.; et al. Antitumour activity of the microencapsulation of Annona vepretorum essential oil. Basic Clin. Pharmacol. Toxicol. 2016, 118, 208–213. [Google Scholar] [CrossRef]
- Chen, Y.Y.; Peng, C.X.; Hu, Y.; Bu, C.; Guo, S.C.; Li, X.; Chen, Y.; Chen, J.W. Studies on chemical constituents and anti-hepatoma effects of essential oil from Annona squamosa L. pericarps. Nat. Prod. Res. 2017, 31, 1305–1308. [Google Scholar] [CrossRef] [PubMed]
- Costa, R.G.A.; Anunciação, T.A.D.; Araujo, M.S.; Souza, C.A.; Dias, R.B.; Sales, C.B.S.; Rocha, C.A.G.; Soares, M.B.P.; Silva, F.M.A.D.; Koolen, H.H.F.; et al. In vitro and in vivo growth inhibition of human acute promyelocytic leukemia HL-60 cells by Guatteria megalophylla Diels (Annonaceae) leaf essential oil. Biomed. Pharmacother. 2020, 122, 109713. [Google Scholar] [CrossRef]
- Ferraz, R.P.; Cardoso, G.M.; da Silva, T.B.; Fontes, J.E.; Prata, A.P.; Carvalho, A.A.; Moraes, M.O.; Pessoa, C.; Costa, E.V.; Bezerra, D.P. Antitumour properties of the leaf essential oil of Xylopia frutescens Aubl. (Annonaceae). Food Chem. 2013, 141, 196–200. [Google Scholar] [CrossRef]
- Quintans, J.S.; Soares, B.M.; Ferraz, R.P.; Oliveira, A.C.; Silva, T.B.; Menezes, L.R.; Sampaio, M.F.; Prata, A.P.; Moraes, M.O.; Pessoa, C.; et al. Chemical constituents and anticancer effects of the essential oil from leaves of Xylopia laevigata. Planta Med. 2013, 79, 123–130. [Google Scholar] [CrossRef]
- do N Fontes, J.E.; Ferraz, R.P.; Britto, A.C.; Carvalho, A.A.; Moraes, M.O.; Pessoa, C.l.; Costa, E.V.; Bezerra, D.P. Antitumor effect of the essential oil from leaves of Guatteria pogonopus (Annonaceae). Chem. Biodivers. 2013, 10, 722–729. [Google Scholar] [CrossRef]
- Silva, T.B.; Menezes, L.R.A.; Sampaio, M.F.C.; Meira, C.S.; Guimarães, E.T.; Soares, M.B.P.; Prata, A.P.N.; Nogueira, P.C.L.; Costa, E.V. Chemical composition and anti-Trypanosoma cruzi activity of essential oils obtained from leaves of Xylopia frutescens and X. laevigata (Annonaceae). Nat. Prod. Commun. 2013, 8, 403–406. [Google Scholar]
- Ahmed, S.A.; Gogal, R.M., Jr.; Walsh, J.E. A new rapid and simple non-radioactive assay to monitor and determine the proliferation of lymphocytes: An alternative to [3H]-thymidine incorporation assay. J. Immunol. Methods 1994, 170, 211–224. [Google Scholar] [CrossRef]
- Santos, L.S.; Silva, V.R.; Menezes, L.R.A.; Soares, M.B.P.; Costa, E.V.; Bezerra, D.P. Xylopine induces oxidative stress and causes G2/M phase arrest, triggering caspase-mediated apoptosis by p53-independent pathway in HCT116 cells. Oxid. Med. Cell Longev. 2017, 2017, 7126872. [Google Scholar] [CrossRef]
- Silva, V.R.; Corrêa, R.S.; Santos, L.S.; Soares, M.B.P.; Batista, A.A.; Bezerra, D.P. A ruthenium-based 5-fluorouracil complex with enhanced cytotoxicity and apoptosis induction action in HCT116 cells. Sci. Rep. 2018, 8, 288. [Google Scholar] [CrossRef]
- Nicoletti, I.; Migliorati, G.; Pagliacci, M.C.; Grignani, F.; Riccardi, C. A rapid and simple method for measuring thymocyte apoptosis by propidium iodide staining and flow cytometry. J. Immunol. Methods 1991, 139, 271–279. [Google Scholar] [CrossRef]
- Lima, E.J.S.P.; Fontes, S.S.; Nogueira, M.L.; Silva, V.R.; Santos, L.S.; D’Elia, G.M.A.; Dias, R.B.; Sales, C.B.S.; Rocha, C.A.G.; Vannier-Santos, M.A.; et al. Essential oil from leaves of Conobea scoparioides (Cham. & Schltdl.) Benth. (Plantaginaceae) causes cell death in HepG2 cells and inhibits tumor development in a xenograft model. Biomed. Pharmacother. 2020, 129, 110402. [Google Scholar] [CrossRef]
- Nogueira, M.L.; Lima, E.J.S.P.; Adrião, A.A.X.; Fontes, S.S.; Silva, V.R.; Santos, L.S.; Soares, M.B.P.; Dias, R.B.; Rocha, C.A.G.; Costa, E.V.; et al. Cyperus articulatus L. (Cyperaceae) Rhizome Essential Oil Causes Cell Cycle Arrest in the G2/M Phase and Cell Death in HepG2 Cells and Inhibits the Development of Tumors in a Xenograft Model. Molecules 2020, 25, 2687. [Google Scholar] [CrossRef]
- Oliveira, F.P.; Rodrigues, A.C.B.C.; Lima, E.J.S.P.; Silva, V.R.; Santos, L.S.; Anunciação, T.A.; Nogueira, M.L.; Soares, M.B.P.; Dias, R.B.; Rocha, C.A.G.; et al. Essential Oil from Bark of Aniba parviflora (Meisn.) Mez (Lauraceae) Reduces HepG2 Cell Proliferation and Inhibits Tumor Development in a Xenograft Model. Chem. Biodivers. 2021, 18, e2000938. [Google Scholar] [CrossRef]




| Compounds | AI a | AI b | Peak Area% | |
|---|---|---|---|---|
| 1 | δ-Elemene | 1334 | 1335 | 1.54 ± 0.03 |
| 2 | α-Cubebene | 1347 | 1348 | 1.80 ± 0.02 |
| 3 | Ciclosativene | 1364 | 1369 | 0.36 ± 0.01 |
| 4 | α-Ylangene | 1373 | 1373 | 0.91 ± 0.03 |
| 5 | β-Bourbonene | 1381 | 1387 | 0.14 ± 0.01 |
| 6 | β-Cubebene | 1387 | 1387 | 0.24 ± 0.01 |
| 7 | β-Elemene | 1389 | 1389 | 0.43 ± 0.00 |
| 8 | α-Gurjunene | 1406 | 1409 | 26.83 ± 0.10 |
| 9 | (E)-Caryophyllene | 1415 | 1417 | 1.27 ± 0.01 |
| 10 | β-Copaene | 1425 | 1430 | 0.72 ± 0.01 |
| 11 | α-Guaiene | 1436 | 1437 | 0.43 ± 0.03 |
| 12 | α-Humulene | 1450 | 1452 | 0.42 ± 0.02 |
| 13 | allo-Aromadendrene | 1457 | 1458 | 2.21 ± 0.02 |
| 14 | γ-Gurjunene | 1474 | 1475 | 0.45 ± 0.06 |
| 15 | Germacrene D | 1478 | 1480 | 15.35 ± 0.01 |
| 16 | Bicyclogermacrene | 1493 | 1500 | 24.90 ± 0.03 |
| 17 | α-Muurolene | 1498 | 1500 | 1.26 ± 0.01 |
| 18 | Viridiflorene | 1503 | 1496 | 0.54 ± 0.01 |
| 19 | γ-Cadinene | 1511 | 1513 | 0.44 ± 0.01 |
| 20 | δ-Cadinene | 1520 | 1522 | 1.20 ± 0.10 |
| 21 | Palustrol | 1562 | 1567 | 1.40 ± 0.03 |
| 22 | Spathulenol | 1572 | 1577 | 12.97 ± 0.02 |
| 23 | Viridiflorol | 1596 | 1592 | 0.94 ± 0.02 |
| Sesquiterpene hydrocarbons | 81.44 | |||
| Oxygenated sesquiterpenes | 15.31 | |||
| Total not identified | 3.25 | |||
| Total identified | 96.75 | |||
| Cells | Histological Type | IC50 and 95% CI (in μg/mL) | |
|---|---|---|---|
| DOX | EO | ||
| Cancer cells | |||
| HepG2 | human hepatocellular carcinoma | 0.09 0.06–0.12 | 11.70 6.10–22.43 |
| NB4 | human acute promyelocytic leukemia | 0.05 0.03–0.07 | 9.23 8.38–10.17 |
| THP-1 | human monocytic leukemia | 0.08 0.05–0.12 | 13.05 10.73–15.87 |
| JURKAT | human acute T cell leukemia | 0.03 0.02–0.05 | 8.01 6.94–9.24 |
| K562 | human chronic myelogenous leukemia | 0.70 0.36–1.36 | 14.59 12.58–16.91 |
| HL-60 | human acute promyelocytic leukemia | 0.05 0.03–0.10 | 19.74 15.62–24.95 |
| KG-1a | human myeloid leukemia | 0.01 0.01–0.11 | 20.75 16.59–25.96 |
| MCF-7 | human breast adenocarcinoma | 1.45 1.00–2.11 | 32.85 22.47–48.03 |
| HCT116 | human colon carcinoma | 0.06 0.03–0.12 | 15.51 12.39–19.41 |
| SCC4 | human oral squamous cell carcinoma | 0.01 0.002–0.04 | 3.28 3.00–3.59 |
| CAL27 | human oral squamous cell carcinoma | 0.65 0.26–1.65 | 39.39 27.37–56.68 |
| HSC-3 | human oral squamous cell carcinoma | 0.66 0.49–0.87 | 30.95 21.01–45.60 |
| B16-F10 | mouse melanoma | 0.28 0.23–0.35 | 28.20 21.52–36.96 |
| Non-cancerous cells | |||
| MRC-5 | human lung fibroblast | 0.91 0.30–2.73 | 16.57 12.91–21.28 |
| PBMC | human peripheral blood mononuclear cells | 0.67 0.48–0.94 | 21.28 17.72–25.56 |
| BJ | human foreskin fibroblast | 0.55 0.22–1.37 | >50 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Costa, E.V.; de Souza, C.A.S.; Galvão, A.F.C.; Silva, V.R.; Santos, L.d.S.; Dias, R.B.; Rocha, C.A.G.; Soares, M.B.P.; da Silva, F.M.A.; Koolen, H.H.F.; et al. Duguetia pycnastera Sandwith (Annonaceae) Leaf Essential Oil Inhibits HepG2 Cell Growth In Vitro and In Vivo. Molecules 2022, 27, 5664. https://doi.org/10.3390/molecules27175664
Costa EV, de Souza CAS, Galvão AFC, Silva VR, Santos LdS, Dias RB, Rocha CAG, Soares MBP, da Silva FMA, Koolen HHF, et al. Duguetia pycnastera Sandwith (Annonaceae) Leaf Essential Oil Inhibits HepG2 Cell Growth In Vitro and In Vivo. Molecules. 2022; 27(17):5664. https://doi.org/10.3390/molecules27175664
Chicago/Turabian StyleCosta, Emmanoel V., César A. S. de Souza, Alexandre F. C. Galvão, Valdenizia R. Silva, Luciano de S. Santos, Rosane B. Dias, Clarissa A. Gurgel Rocha, Milena B. P. Soares, Felipe M. A. da Silva, Hector H. F. Koolen, and et al. 2022. "Duguetia pycnastera Sandwith (Annonaceae) Leaf Essential Oil Inhibits HepG2 Cell Growth In Vitro and In Vivo" Molecules 27, no. 17: 5664. https://doi.org/10.3390/molecules27175664
APA StyleCosta, E. V., de Souza, C. A. S., Galvão, A. F. C., Silva, V. R., Santos, L. d. S., Dias, R. B., Rocha, C. A. G., Soares, M. B. P., da Silva, F. M. A., Koolen, H. H. F., & Bezerra, D. P. (2022). Duguetia pycnastera Sandwith (Annonaceae) Leaf Essential Oil Inhibits HepG2 Cell Growth In Vitro and In Vivo. Molecules, 27(17), 5664. https://doi.org/10.3390/molecules27175664









