Direct Identification of Urinary Tract Pathogens by MALDI-TOF/TOF Analysis and De Novo Peptide Sequencing
Abstract
1. Introduction
2. Results
2.1. Results of Standard Urine Culture Test and Identification of Urine Bacterial Isolates Grown on Blood Agar Plates
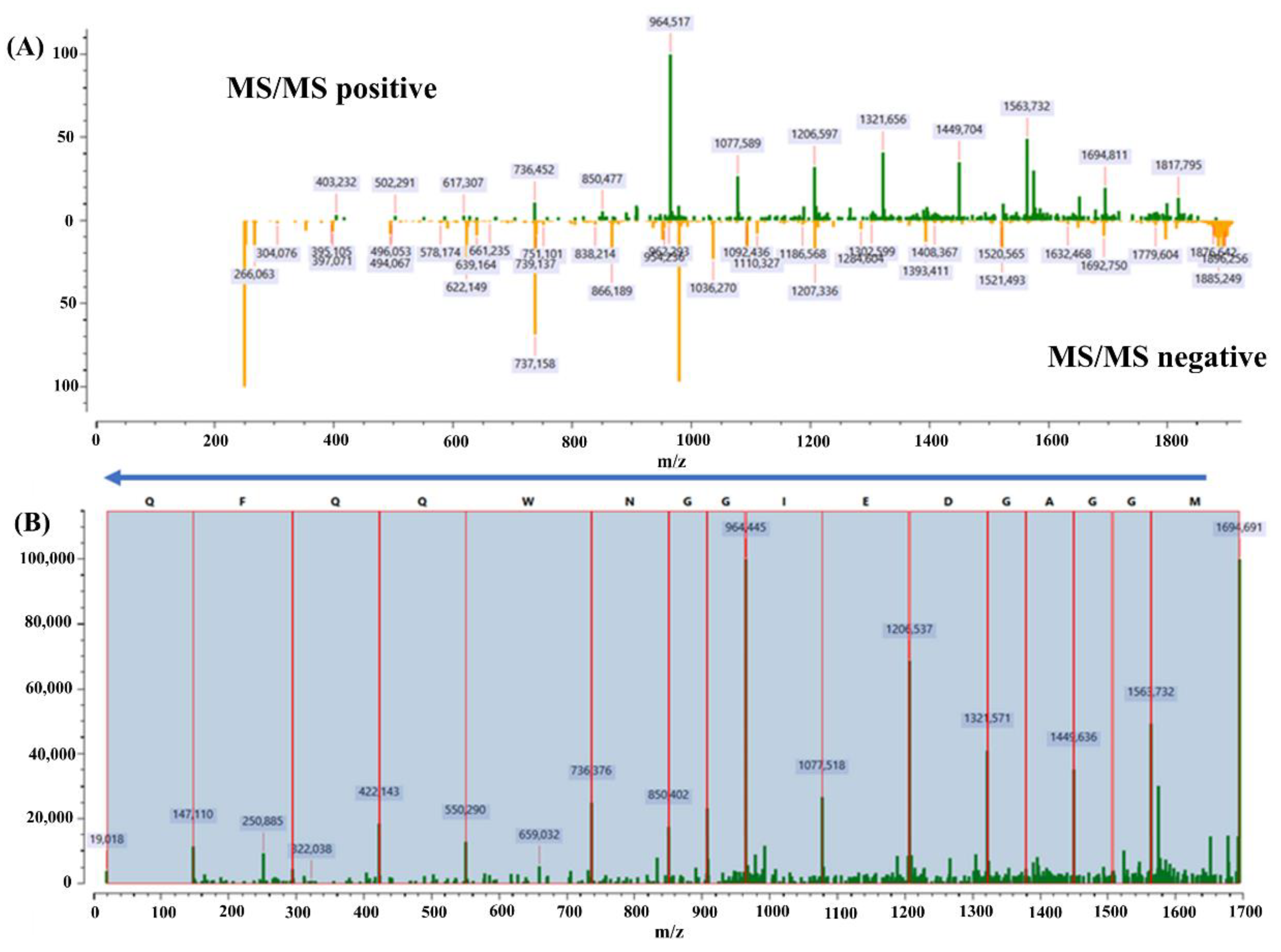
2.2. Protein Acrobat De Novo Sequencing Algorithm
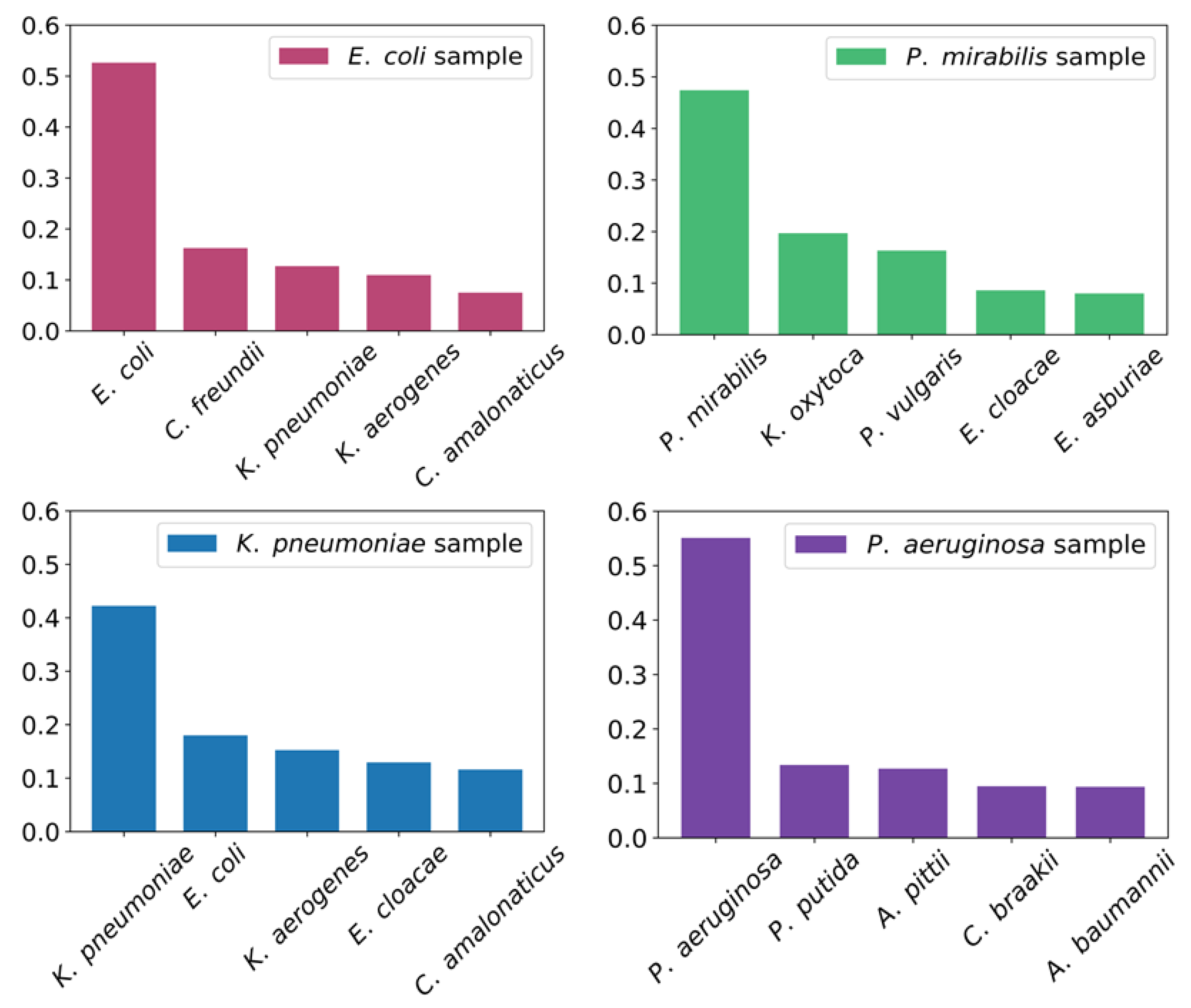
2.3. Direct Identification of Uropathogenic Bacteria from Urine Samples
3. Discussion
4. Materials and Methods
4.1. Raw Materials
4.2. Urine Sample Collection Ethics
4.3. Protein Extraction
4.4. Protein Purification and Digestion
4.5. Derivatization Procedure
4.6. Two Dimensional Fractionation of Peptide Mixture
4.7. Mass Spectrometry
4.8. BLASTp Parameters
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Cheng, K.; Chui, H.; Domish, L.; Hernandez, D.; Wang, G. Recent Development of Mass Spectrometry and Proteomics Applications in Identification and Typing of Bacteria. Prot. Clin. Appl. 2016, 10, 346–357. [Google Scholar] [CrossRef] [PubMed]
- Janda, J.M.; Abbott, S.L. 16S RRNA Gene Sequencing for Bacterial Identification in the Diagnostic Laboratory: Pluses, Perils, and Pitfalls. J. Clin. Microbiol. 2007, 45, 2761–2764. [Google Scholar] [CrossRef]
- Zauli, D.A.G. PCR and Infectious Diseases. Synth. Biol.-New Interdiscip. Sci. 2019, 137–147. [Google Scholar] [CrossRef]
- Church, D.L.; Cerutti, L.; Gürtler, A.; Griener, T.; Zelazny, A.; Emler, S. Performance and Application of 16S RRNA Gene Cycle Sequencing for Routine Identification of Bacteria in the Clinical Microbiology Laboratory. Clin. Microbiol. Rev. 2020, 33, e00053-19. [Google Scholar] [CrossRef] [PubMed]
- Ni, P.-X.; Ding, X.; Zhang, Y.-X.; Yao, X.; Sun, R.-X.; Wang, P.; Gong, Y.-P.; Zhou, J.-L.; Li, D.-F.; Wu, H.-L.; et al. Rapid Detection and Identification of Infectious Pathogens Based on High-Throughput Sequencing. Chin. Med. J. (Engl.) 2015, 128, 877–883. [Google Scholar] [CrossRef]
- Rodriguez-Saona, L.E.; Khambaty, F.M.; Fry, F.S.; Calvey, E.M. Rapid Detection and Identification of Bacterial Strains by Fourier Transform Near-Infrared Spectroscopy. J. Agric. Food Chem. 2001, 49, 574–579. [Google Scholar] [CrossRef]
- Ho, C.-S.; Jean, N.; Hogan, C.A.; Blackmon, L.; Jeffrey, S.S.; Holodniy, M.; Banaei, N.; Saleh, A.A.E.; Ermon, S.; Dionne, J. Rapid Identification of Pathogenic Bacteria Using Raman Spectroscopy and Deep Learning. Nat. Commun. 2019, 10, 4927. [Google Scholar] [CrossRef]
- Locke, A.; Fitzgerald, S.; Mahadevan-Jansen, A. Advances in Optical Detection of Human-Associated Pathogenic Bacteria. Molecules 2020, 25, 5256. [Google Scholar] [CrossRef]
- Flores-Mireles, A.L.; Walker, J.N.; Caparon, M.; Hultgren, S.J. Urinary Tract Infections: Epidemiology, Mechanisms of Infection and Treatment Options. Nat. Rev. Microbiol. 2015, 13, 269–284. [Google Scholar] [CrossRef]
- DeMarco, M.L.; Burnham, C.-A.D. Diafiltration MALDI-TOF Mass Spectrometry Method for Culture-Independent Detection and Identification of Pathogens Directly from Urine Specimens. Am. J. Clin. Pathol. 2014, 141, 204–212. [Google Scholar] [CrossRef]
- Tracz, D.M.; McCorrister, S.J.; Chong, P.M.; Lee, D.M.; Corbett, C.R.; Westmacott, G.R. A Simple Shotgun Proteomics Method for Rapid Bacterial Identification. J. Microbiol. Methods 2013, 94, 54–57. [Google Scholar] [CrossRef]
- Boulund, F.; Karlsson, R.; Gonzales-Siles, L.; Johnning, A.; Karami, N.; AL-Bayati, O.; Åhrén, C.; Moore, E.R.B.; Kristiansson, E. Typing and Characterization of Bacteria Using Bottom-up Tandem Mass Spectrometry Proteomics. Mol. Cell. Proteom. 2017, 16, 1052–1063. [Google Scholar] [CrossRef] [PubMed]
- Alves, G.; Wang, G.; Ogurtsov, A.Y.; Drake, S.K.; Gucek, M.; Sacks, D.B.; Yu, Y.-K. Rapid Classification and Identification of Multiple Microorganisms with Accurate Statistical Significance via High-Resolution Tandem Mass Spectrometry. J. Am. Soc. Mass Spectrom. 2018, 29, 1721–1737. [Google Scholar] [CrossRef]
- Alves, G.; Wang, G.; Ogurtsov, A.Y.; Drake, S.K.; Gucek, M.; Suffredini, A.F.; Sacks, D.B.; Yu, Y.-K. Identification of Microorganisms by High Resolution Tandem Mass Spectrometry with Accurate Statistical Significance. J. Am. Soc. Mass Spectrom. 2016, 27, 194–210. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, R.; Thorsell, A.; Gomila, M.; Salvà-Serra, F.; Jakobsson, H.E.; Gonzales-Siles, L.; Jaén-Luchoro, D.; Skovbjerg, S.; Fuchs, J.; Karlsson, A.; et al. Discovery of Species-Unique Peptide Biomarkers of Bacterial Pathogens by Tandem Mass Spectrometry-Based Proteotyping *. Mol. Cell. Proteom. 2020, 19, 518–528. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, L.; Sanchez-Juanes, F.; Gonzalez-Avila, M.; Cembrero-Fucinos, D.; Herrero-Hernandez, A.; Gonzalez-Buitrago, J.M.; Munoz-Bellido, J.L. Direct Identification of Urinary Tract Pathogens from Urine Samples by Matrix-Assisted Laser Desorption Ionization-Time of Flight Mass Spectrometry. J. Clin. Microbiol. 2010, 48, 2110–2115. [Google Scholar] [CrossRef]
- Pinault, L.; Chabrière, E.; Raoult, D.; Fenollar, F. Direct Identification of Pathogens in Urine by Use of a Specific Matrix-Assisted Laser Desorption Ionization–Time of Flight Spectrum Database. J. Clin. Microbiol. 2019, 57, e01678-18. [Google Scholar] [CrossRef]
- Li, W.; Sun, E.; Wang, Y.; Pan, H.; Zhang, Y.; Li, Y.; Zhang, X.; Li, C.; Du, L.; Wang, C. Rapid Identification and Antimicrobial Susceptibility Testing for Urinary Tract Pathogens by Direct Analysis of Urine Samples Using a MALDI-TOF MS-Based Combined Protocol. Front. Microbiol. 2019, 10, 1182. [Google Scholar] [CrossRef]
- Huang, B.; Zhang, L.; Zhang, W.; Liao, K.; Zhang, S.; Zhang, Z.; Ma, X.; Chen, J.; Zhang, X.; Qu, P.; et al. Direct Detection and Identification of Bacterial Pathogens from Urine with Optimized Specimen Processing and Enhanced Testing Algorithm. J. Clin. Microbiol. 2017, 55, 8. [Google Scholar] [CrossRef]
- Köhling, H.L.; Bittner, A.; Müller, K.-D.; Buer, J.; Becker, M.; Rübben, H.; Rettenmeier, A.W.; Mosel, F. Direct Identification of Bacteria in Urine Samples by Matrix-Assisted Laser Desorption/Ionization Time-of-Flight Mass Spectrometry and Relevance of Defensins as Interfering Factors. J. Med. Microbiol. 2012, 61, 339–344. [Google Scholar] [CrossRef]
- Spanu, T.; Posteraro, B.; Fiori, B.; D’Inzeo, T.; Campoli, S.; Ruggeri, A.; Tumbarello, M.; Canu, G.; Trecarichi, E.M.; Parisi, G.; et al. Direct MALDI-TOF Mass Spectrometry Assay of Blood Culture Broths for Rapid Identification of Candida Species Causing Bloodstream Infections: An Observational Study in Two Large Microbiology Laboratories. J. Clin. Microbiol. 2012, 50, 176–179. [Google Scholar] [CrossRef] [PubMed]
- Leli, C.; Cenci, E.; Cardaccia, A.; Moretti, A.; D’Alò, F.; Pagliochini, R.; Barcaccia, M.; Farinelli, S.; Vento, S.; Bistoni, F.; et al. Rapid Identification of Bacterial and Fungal Pathogens from Positive Blood Cultures by MALDI-TOF MS. Int. J. Med. Microbiol. 2013, 303, 205–209. [Google Scholar] [CrossRef] [PubMed]
- Idelevich, E.A.; Schüle, I.; Grünastel, B.; Wüllenweber, J.; Peters, G.; Becker, K. Rapid Identification of Microorganisms from Positive Blood Cultures by MALDI-TOF Mass Spectrometry Subsequent to Very Short-Term Incubation on Solid Medium. Clin. Microbiol. Infect. 2014, 20, 1001–1006. [Google Scholar] [CrossRef] [PubMed]
- Roux-Dalvai, F.; Gotti, C.; Leclercq, M.; Hélie, M.-C.; Boissinot, M.; Arrey, T.N.; Dauly, C.; Fournier, F.; Kelly, I.; Marcoux, J.; et al. Fast and Accurate Bacterial Species Identification in Urine Specimens Using LC-MS/MS Mass Spectrometry and Machine Learning. Mol. Cell. Proteom. 2019, 18, 2492–2505. [Google Scholar] [CrossRef]
- Yu, Y.; Sikorski, P.; Bowman-Gholston, C.; Cacciabeve, N.; Nelson, K.E.; Pieper, R. Diagnosing Inflammation and Infection in the Urinary System via Proteomics. J. Transl. Med. 2015, 13, 111. [Google Scholar] [CrossRef]
- Wilson, S.R.; Vehus, T.; Berg, H.S.; Lundanes, E. Nano-LC in Proteomics: Recent Advances and Approaches. Bioanalysis 2015, 7, 1799–1815. Available online: https://www.future-science.com/doi/abs/10.4155/bio.15.92 (accessed on 6 June 2022). [CrossRef]
- Maus, A.; Mignon, R.; Basile, F. Enhanced Protein Identification Using Graphite-Modified MALDI Plates for Offline LC-MALDI-MS/MS Bottom-up Proteomics. Anal. Biochem. 2018, 545, 31. [Google Scholar] [CrossRef]
- Cindric, M.; Pavelic, K.; Dodig, I. Mass Spectrometry-Based Protein Identification Method with Selectiven-Terminus Dervatization. U.S. Patent 8,647,880, 11 February 2014. [Google Scholar]
- Butorac, A.; Dodig, I.; Bačun-Družina, V.; Tishbee, A.; Mrvčić, J.; Hock, K.; Diminić, J.; Cindrić, M. The Effect of Starvation Stress on Lactobacillus Brevis L62 Protein Profile Determined by de Novo Sequencing in Positive and Negative Mass Spectrometry Ion Mode: CAF−/CAF+ Peptide de novo Sequencing. Rapid Commun. Mass Spectrom. 2013, 27, 1045–1054. [Google Scholar] [CrossRef]
- Hassell, K.M.; Stutzman, J.R.; McLuckey, S.A. Gas-Phase Bioconjugation of Peptides via Ion/Ion Charge Inversion: Schiff Base Formation on the Conversion of Cations to Anions. Anal. Chem. 2010, 82, 1594–1597. [Google Scholar] [CrossRef][Green Version]
- Altschul, S.F.; Gish, W.; Miller, W.; Myers, E.W.; Lipman, D.J. Basic Local Alignment Search Tool. J. Mol. Biol. 1990, 215, 403–410. [Google Scholar] [CrossRef]
- Chen, C.; Li, Z.; Huang, H.; Suzek, B.E.; Wu, C.H. A Fast Peptide Match Service for UniProt Knowledgebase. Bioinformatics 2013, 29, 2808–2809. [Google Scholar] [CrossRef] [PubMed]
- Aspevall, O.; Hallander, H.; Gant, V.; Kouri, T. European Guidelines for Urinalysis: A Collaborative Document Produced by European Clinical Microbiologists and Clinical Chemists under ECLM in Collaboration with ESCMID. Clin. Microbiol. Infect. 2001, 7, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Cisse, M.; Dauphin, Y.N.; Lopez-Paz, D. Mixup: Beyond Empirical Risk Minimization. arXiv 2018, arXiv:1710.09412. [Google Scholar]
- Karlsson, R.; Davidson, M.; Svensson-Stadler, L.; Karlsson, A.; Olesen, K.; Carlsohn, E.; Moore, E.R.B. Strain-Level Typing and Identification of Bacteria Using Mass Spectrometry-Based Proteomics. J. Proteome Res. 2012, 11, 2710–2720. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, R.; Gonzales-Siles, L.; Gomila, M.; Busquets, A.; Salvà-Serra, F.; Jaén-Luchoro, D.; Jakobsson, H.E.; Karlsson, A.; Boulund, F.; Kristiansson, E.; et al. Proteotyping Bacteria: Characterization, Differentiation and Identification of Pneumococcus and Other Species within the Mitis Group of the Genus Streptococcus by Tandem Mass Spectrometry Proteomics. PLoS ONE 2018, 13, e0208804. [Google Scholar] [CrossRef]
- Manadas, B.; Mendes, V.M.; English, J.; Dunn, M.J. Peptide Fractionation in Proteomics Approaches. Expert Rev. Proteom. 2010, 7, 655–663. [Google Scholar] [CrossRef]
- Cheng, G.; Zheng, S.-Y. Construction of a High-Performance Magnetic Enzyme Nanosystem for Rapid Tryptic Digestion. Sci. Rep. 2014, 4, 6947. [Google Scholar] [CrossRef]
- Dycka, F.; Bobal, P.; Mazanec, K.; Bobalova, J. Rapid and Efficient Protein Enzymatic Digestion: An Experimental Comparison. Electrophoresis 2012, 33, 288–295. [Google Scholar] [CrossRef]
- Brisse, S.; Verhoef, J. Phylogenetic Diversity of Klebsiella Pneumoniae and Klebsiella Oxytoca Clinical Isolates Revealed by Randomly Amplified Polymorphic DNA, GyrA and ParC Genes Sequencing and Automated Ribotyping. Int. J. Syst. Evol. Microbiol. 2001, 51, 915–924. [Google Scholar] [CrossRef]
- Kumar, V.; Sun, P.; Vamathevan, J.; Li, Y.; Ingraham, K.; Palmer, L.; Huang, J.; Brown, J.R. Comparative Genomics of Klebsiella Pneumoniae Strains with Different Antibiotic Resistance Profiles. Antimicrob. Agents Chemother. 2011, 55, 4267–4276. [Google Scholar] [CrossRef]
- Tran, N.H.; Zhang, X.; Xin, L.; Shan, B.; Li, M. De Novo Peptide Sequencing by Deep Learning. Proc. Natl. Acad. Sci. USA 2017, 114, 8247–8252. [Google Scholar] [CrossRef] [PubMed]
- Allmer, J. Algorithms for the de Novo Sequencing of Peptides from Tandem Mass Spectra. Expert Rev. Proteom. 2011, 8, 645–657. [Google Scholar] [CrossRef]
- Devabhaktuni, A.; Elias, J.E. Application of de Novo Sequencing to Large-Scale Complex Proteomics Data Sets. J. Proteome Res. 2016, 15, 732–742. [Google Scholar] [CrossRef] [PubMed]
- Cindric, M.; Hamersak, Z.; Dodig, I. Method of Detection of Amino Acid Sequence and/or Identification of Peptides and Proteins, by Use of a New Derivatization Reagent and Synthesis of 5-Formyl-Benzene-1,3-Disulphonic Acid as Derivatization Reagent. U.S. Patent 9,581,601, 28 February 2017. [Google Scholar]
- Yu, Y.; Pieper, R. Urinary Pellet Sample Preparation for Shotgun Proteomic Analysis of Microbial Infection and Host-Pathogen Interactions. Methods Mol. Biol. 2015, 1295, 65–74. [Google Scholar] [CrossRef] [PubMed]

| Standard Urine Culture | Proteomic Method | Conf. 1 | Standard Urine Culture | Proteomic Method | Conf. 1 |
|---|---|---|---|---|---|
| Klebsiella pneumoniae | Escherichia coli | 1 | Escherichia coli | Escherichia coli | 3 |
| Klebsiella aerogenes | /2 | 1 | Escherichia coli | Escherichia coli | 3 |
| Klebsiella pneumoniae | Escherichia coli | 1 | Escherichia coli | Escherichia coli | 3 |
| Escherichia coli | Escherichia coli | 1 | Escherichia coli | Escherichia coli | 3 |
| Candida albicans | Candida albicans | 2 | Escherichia coli | Escherichia coli | 3 |
| Escherichia coli | Escherichia coli | 2 | Escherichia coli | Escherichia coli | 3 |
| Escherichia coli | Escherichia coli | 2 | Escherichia coli | Escherichia coli | 3 |
| Klebsiella pneumoniae | Klebsiella pneumoniae | 2 | Escherichia coli | Escherichia coli | 3 |
| Enterococcus faecalis | Enterococcus faecalis | 2 | Enterococcus faecalis | Enterococcus faecalis | 3 |
| Proteus mirabilis | Proteus mirabilis | 2 | Enterococcus faecalis | Enterococcus faecalis | 3 |
| Stenotrophomonas maltophilia | Stenotrophomonas maltophilia | 2 | Pseudomonas aeruginosa | Pseudomonas aeruginosa | 3 |
| Citrobacter freundii | Klebsiella pneumoniae | 3 | Pseudomonas aeruginosa | Pseudomonas aeruginosa | 3 |
| Escherichia coli | Escherichia coli | 3 | Pseudomonas aeruginosa | Pseudomonas aeruginosa | 3 |
| Escherichia coli | Escherichia coli | 3 | Pseudomonas aeruginosa | Pseudomonas aeruginosa | 3 |
| Escherichia coli | Escherichia coli | 3 | Proteus mirabilis | Proteus mirabilis | 3 |
| Escherichia coli | Escherichia coli | 3 | Proteus mirabilis | Proteus mirabilis | 3 |
| Escherichia coli | Escherichia coli | 3 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Svetličić, E.; Dončević, L.; Ozdanovac, L.; Janeš, A.; Tustonić, T.; Štajduhar, A.; Brkić, A.L.; Čeprnja, M.; Cindrić, M. Direct Identification of Urinary Tract Pathogens by MALDI-TOF/TOF Analysis and De Novo Peptide Sequencing. Molecules 2022, 27, 5461. https://doi.org/10.3390/molecules27175461
Svetličić E, Dončević L, Ozdanovac L, Janeš A, Tustonić T, Štajduhar A, Brkić AL, Čeprnja M, Cindrić M. Direct Identification of Urinary Tract Pathogens by MALDI-TOF/TOF Analysis and De Novo Peptide Sequencing. Molecules. 2022; 27(17):5461. https://doi.org/10.3390/molecules27175461
Chicago/Turabian StyleSvetličić, Ema, Lucija Dončević, Luka Ozdanovac, Andrea Janeš, Tomislav Tustonić, Andrija Štajduhar, Antun Lovro Brkić, Marina Čeprnja, and Mario Cindrić. 2022. "Direct Identification of Urinary Tract Pathogens by MALDI-TOF/TOF Analysis and De Novo Peptide Sequencing" Molecules 27, no. 17: 5461. https://doi.org/10.3390/molecules27175461
APA StyleSvetličić, E., Dončević, L., Ozdanovac, L., Janeš, A., Tustonić, T., Štajduhar, A., Brkić, A. L., Čeprnja, M., & Cindrić, M. (2022). Direct Identification of Urinary Tract Pathogens by MALDI-TOF/TOF Analysis and De Novo Peptide Sequencing. Molecules, 27(17), 5461. https://doi.org/10.3390/molecules27175461






