Promising Antioxidant and Antimicrobial Potencies of Chemically-Profiled Extract from Withania aristata (Aiton) Pauquy against Clinically-Pathogenic Microbial Strains
Abstract
:1. Introduction
2. Results and Discussion
2.1. Chemical Composition of RWA
| Plant Name | Plant Part Used | Extract Type | Major Compounds | Pharmacological Activities | References |
|---|---|---|---|---|---|
| Withania aristata | Leaves | Crude extract | 2-(4-hydroxy-3,5 dimethoxyphenyl)-3-oxetanamine and N-4-(3-furoylamine)-1-butanol | Anti-plasmodial activity | [44] |
| Leaves | Isolation | Withanolides | cytotoxic activity | [45] | |
| Leaves | Isolation | Apocarotenoids, carotenoid, tetra-acetylated apocarotenoid, glucosides | Phytotoxic activity | [46] | |
| Leaves | Isolation | hydroxywithanolide F, withanolide A, withacoagulin | inhibitors of SARS-CoV-2 main protease (Mpro) | [47] | |
| Withania frutescens | Leaves | Essential oil | camphor, thujone, carvacrol, and thymol | Antioxidant and antimicrobial activities | [20] |
| Leaves | Essential oil | camphor, carvacrol, and thymol | Insecticidal and antifungal activities | [48] | |
| Leaves | Crude extract | Epicatechin, apigenin, caffeic acid, ferulic acid, and p-coumaric acid | Analgesic, anti-inflammatory, and healing activities | [26] | |
| Leaves | Crude extract | 4β,17α,27-trihydroxy-1-oxo-22-R-witha-2,5,24-trienolide (1), 5β,6β-epoxy-4β,17α,27-trihydroxy-1-oxowitha-2,24-dienolide (2), and 2,3-dihydroxywithaferin A-3β-O-sulfate (3) | cytotoxic activity against cancer cell lines (HepG2 and HT29) | [49] | |
| Leaves | Total polyphenols | - | Antifungal and antioxidant activity | [50] | |
| Withania somnifera | Roots | Crude extract | withanoside IV, physagulin D, 27-hydroxywithanone, withanoside V, withaferin A, withastramonolide, withanolide A, withanone, and withanolide B | Cytotoxic and pro-inflammatory enzyme inhibitory properties | [30] |
| Aerial parts | Crude extract | isopelletierine, anaferine, withanolides, withaferins | Immunomodulatory activity, anti-inflammatory activities, anticancer and chemoprotective activities, hepatoprotective activity | [51] | |
| Leaves and roots | Crude extract | withaferin A and withanolide D | Antibacterial synergistic activities | [52] |
2.2. Antioxidant Activity
2.3. Antibacterial Activity
2.4. Antifungal Activity
3. Conclusions
4. Material and Methods
4.1. Growth Media and Chemical Material
4.2. Plant Material
4.3. Preparation of Plant Extract
4.4. HPLC/MS Analysis
4.5. Antioxidant Activity
4.5.1. DPPH Test
4.5.2. FRAP Test
4.5.3. Total Antioxidant Capacity
4.5.4. β-Carotene Bleaching Assay
4.6. Antimicrobial Activities
4.6.1. Microbial Inoculum Preparation
4.6.2. Disc Diffusion Method
4.6.3. Determination of Minimum Inhibitory Concentration (MIC)
4.7. Statistical Analysis
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Egamberdieva, D.; Mamedov, N.; Ovidi, E.; Tiezzi, A.; Craker, L. Phytochemical and Pharmacological Properties of Medicinal Plants from Uzbekistan: A Review. J. Med. Act. Plants 2017, 5, 59–75. [Google Scholar]
- Bourhia, M.; Messaoudi, M.; Bakrim, H.; Mothana, R.A.; Sddiqui, N.A.; Almarfadi, O.M.; El Mzibri, M.; Gmouh, S.; Laglaoui, A.; Benbacer, L. Citrullus colocynthis (L.) Schrad: Chemical Characterization, Scavenging and Cytotoxic Activities. Open Chem. 2020, 18, 986–994. [Google Scholar] [CrossRef]
- Maroyi, A. Traditional Use of Medicinal Plants in South-Central Zimbabwe: Review and Perspectives. J. Ethnobiol. Ethnomed. 2013, 9, 31. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodríguez-Yoldi, M.J. Anti-Inflammatory and Antioxidant Properties of Plant Extracts. Antioxidants 2021, 10, 921. [Google Scholar] [CrossRef] [PubMed]
- Stohs, S.J.; Bagchi, D. Antioxidant, Anti-Inflammatory, and Chemoprotective Properties of Acacia Catechu Heartwood Extracts. Phytother. Res. 2015, 29, 818–824. [Google Scholar] [CrossRef]
- Tan, M.L.; Hamid, S.B.S. Beetroot as a Potential Functional Food for Cancer Chemoprevention, a Narrative Review. J. Cancer Prev. 2021, 26, 1–17. [Google Scholar] [CrossRef]
- Herrmann, F.; Romero, M.R.; Blazquez, A.G.; Kaufmann, D.; Ashour, M.L.; Kahl, S.; Marin, J.J.; Efferth, T.; Wink, M. Diversity of Pharmacological Properties in Chinese and European Medicinal Plants: Cytotoxicity, Antiviral and Antitrypanosomal Screening of 82 Herbal Drugs. Diversity 2011, 3, 547–580. [Google Scholar] [CrossRef] [Green Version]
- Heinrich, M.; Leonti, M.; Nebel, S.; Peschel, W. “Local Food-Nutraceuticals”: An Example of a Multidisciplinary Research Project on Local Knowledge. J. Physiol. Pharmacol. Suppl. 2005, 56, 5–22. [Google Scholar]
- Krishnaiah, D.; Sarbatly, R.; Nithyanandam, R. A Review of the Antioxidant Potential of Medicinal Plant Species. Food Bioprod. Process. 2011, 89, 217–233. [Google Scholar] [CrossRef]
- Aruoma, O.I. Free Radicals, Oxidative Stress, and Antioxidants in Human Health and Disease. J. Am. Oil Chem. Soc. 1998, 75, 199–212. [Google Scholar] [CrossRef]
- Knekt, P.; Jarvinen, R.; Reunanen, A.; Maatela, J. Flavonoid Intake and Coronary Mortality in Finland: A Cohort Study. BMJ 1996, 312, 478–481. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Founou, R.C.; Founou, L.L.; Essack, S.Y. Clinical and Economic Impact of Antibiotic Resistance in Developing Countries: A Systematic Review and Meta-Analysis. PLoS ONE 2017, 12, e0189621. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centers for Disease Control and Prevention. Antibiotic Resistance Threats in the United States. 2013. Available online: https://www.cdc.gov/drugresistance/pdf/ar-threats-2013-508.pdf (accessed on 10 January 2017).
- Bourhia, M.; Ullah, R.; Alqahtani, A.S.; Ibenmoussa, S. Evidence of Drug-Induced Hepatotoxicity in the Maghrebian Population. Drug Chem. Toxicol. 2020, 45, 985–989. [Google Scholar] [CrossRef]
- Dadgostar, P. Antimicrobial Resistance: Implications and Costs. Infect. Drug Resist. 2019, 12, 3903. [Google Scholar] [CrossRef] [Green Version]
- Annavajhala, M.K.; Gomez-Simmonds, A.; Uhlemann, A.-C. Multidrug-Resistant Enterobacter Cloacae Complex Emerging as a Global, Diversifying Threat. Front. Microbiol. 2019, 10, 44. [Google Scholar] [CrossRef] [Green Version]
- Mohammad Salamatullah, A.; Hayat, K.; Mabood Husain, F.; Asif Ahmed, M.; Arzoo, S.; Musaad Althbiti, M.; Alzahrani, A.; Al-Zaied, B.A.M.; Kahlil Alyahya, H.; Albader, N. Effects of Different Solvents Extractions on Total Polyphenol Content, HPLC Analysis, Antioxidant Capacity, and Antimicrobial Properties of Peppers (Red, Yellow, and Green (Capsicum annum L.)). Evid.-Based Complement. Altern. Med. 2022, 2022, 7372101. [Google Scholar] [CrossRef] [PubMed]
- Llor, C.; Bjerrum, L. Antimicrobial Resistance: Risk Associated with Antibiotic Overuse and Initiatives to Reduce the Problem. Ther. Adv. Drug Saf. 2014, 5, 229–241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rabhi, C.; Arcile, G.; Le Goff, G.; Da Costa Noble, C.; Ouazzani, J. Neuroprotective Effect of CR-777, a Glutathione Derivative of Withaferin A, Obtained through the Bioconversion of Withania somnifera (L.) Dunal Extract by the Fungus Beauveria bassiana. Molecules 2019, 24, 4599. [Google Scholar] [CrossRef] [Green Version]
- EL Moussaoui, A.; Bourhia, M.; Jawhari, F.Z.; Salamatullah, A.M.; Ullah, R.; Bari, A.; Majid Mahmood, H.; Sohaib, M.; Serhii, B.; Rozhenko, A. Chemical Profiling, Antioxidant, and Antimicrobial Activity against Drug-Resistant Microbes of Essential Oil from Withania frutescens L. Appl. Sci. 2021, 11, 5168. [Google Scholar] [CrossRef]
- Mesaik, M.A.; Zaheer-Ul-Haq; Murad, S.; Ismail, Z.; Abdullah, N.R.; Gill, H.K.; Atta-Ur-Rahman; Yousaf, M.; Siddiqui, R.A.; Ahmad, A.; et al. Biological and Molecular Docking Studies on Coagulin-H: Human IL-2 Novel Natural Inhibitor. Mol. Immunol. 2006, 43, 1855–1863. [Google Scholar] [CrossRef]
- Jayaprakasam, B.; Nair, M.G. Cyclooxygenase-2 Enzyme Inhibitory Withanolides from Withania somnifera Leaves. Tetrahedron 2003, 59, 841–849. [Google Scholar] [CrossRef]
- Bhattacharya, A.; Ghosal, S.; Bhattacharya, S.K. Anti-Oxidant Effect of Withania somnifera Glycowithanolides in Chronic Footshock Stress-Induced Perturbations of Oxidative Free Radical Scavenging Enzymes and Lipid Peroxidation in Rat Frontal Cortex and Striatum. J. Ethnopharmacol. 2001, 74, 1–6. [Google Scholar] [CrossRef]
- Cordero, C.P.; Morantes, S.J.; Páez, A.; Rincón, J.; Aristizábal, F.A. Cytotoxicity of Withanolides Isolated from Acnistus arborescens. Fitoterapia 2009, 80, 364–368. [Google Scholar] [CrossRef] [PubMed]
- El Bouzidi, L.; Larhsini, M.; Markouk, M.; Abbad, A.; Bekkouche, K. Antioxidant and Antimicrobial Activities of Withania frutescens. Nat. Prod. Commun. 2011, 6, 1447–1450. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- El Moussaoui, A.; Jawhari, F.Z.; Bourhia, M.; Maliki, I.; Sounni, F.; Mothana, R.A.; Bousta, D.; Bari, A. Withania frutescens: Chemical Characterization, Analgesic, Anti-Inflammatory, and Healing Activities. Open Chem. 2020, 18, 927–935. [Google Scholar] [CrossRef]
- El Moussaoui, A.; Mechchate, H.; Bourhia, M.; Es-Safi, I.; Salamatullah, A.M.; Alkaltham, M.S.; Alyahya, H.K.; Bousta, D.; Bari, A. Glycemic Control Potential of Chemically Characterized Extract from Withania frutescens L. Roots in Severe Diabetes-Induced Mice. Appl. Sci. 2021, 11, 3998. [Google Scholar] [CrossRef]
- EL Moussaoui, A.; Zahra, J.F.; EL Ouahdani, K.; Es-safi, I.; Bousta, D.; Bari, A. Valorization of the Pharmacological Potential of Phytochemical Compounds Contained in the Crude Extract of the Root of a Plant of Withania frutescens L. Phytotherapie 2019, 19, 77–82. [Google Scholar] [CrossRef]
- Tripathi, N.; Kumar, S.; Singh, R.; Singh, C.J.; Singh, P.; Varshney, V.K. Isolation and Identification of γ-Sitosterol by GC-MS from the Leaves of Girardinia heterophylla (Decne). Open Bioact. Compd. J. 2013, 4, 25–27. [Google Scholar] [CrossRef] [Green Version]
- Nile, S.H.; Liang, Y.; Wang, Z.; Zheng, J.; Sun, C.; Nile, A.; Patel, G.; Kai, G. Chemical Composition, Cytotoxic and pro-Inflammatory Enzyme Inhibitory Properties of Withania somnifera (L.) Dunal Root Extracts. S. Afr. J. Bot. 2021. [Google Scholar] [CrossRef]
- Zhao, H.; Shi, X.; Shen, C.; Chen, C.; Qu, C.; Patel, G.; Zhou, W.; Kai, G. Comparative Analysis of miRNA Expression Profiles Provides Insight into Regulation of Biosynthesis of Flavonoids and Terpenoids between Two Varieties of Toona sinensis Sprouts. J. Plant Biol. 2021, 1–20. [Google Scholar] [CrossRef]
- Li, J.H.; Nesumi, A.; Shimizu, K.; Sakata, Y.; Liang, M.Z.; He, Q.Y.; Zhou, H.J.; Hashimoto, F. Chemosystematics of Tea Trees Based on Tea Leaf Polyphenols as Phenetic Markers. Phytochemistry 2010, 71, 1342–1349. [Google Scholar] [CrossRef]
- Trabelsi, N.; Oueslati, S.; Falleh, H.; Waffo-Téguo, P.; Papastamoulis, Y.; Mérillon, J.M.; Abdelly, C.; Ksouri, R. Isolation of Powerful Antioxidants from the Medicinal Halophyte Limoniastrum guyonianum. Food Chem. 2012, 135, 1419–1424. [Google Scholar] [CrossRef] [PubMed]
- Trabelsi, N.; Oueslati, S.; Henry-Vitrac, C.; Waffo-Téguo, P.; Medini, F.; Mérillon, J.M.; Abdelly, C.; Ksouri, R. Phenolic Contents and Biological Activities of Limoniastrum guyonianum Fractions Obtained by Centrifugal Partition Chromatography. Ind. Crops Prod. 2013, 49, 740–746. [Google Scholar] [CrossRef]
- EL Moussaoui, A.; Bourhia, M.; Jawhari, F.Z.; Es-safi, I.; Ali, S.S.; Bari, A.; Mahmood, H.M.; Bousta, D.; Bari, A. Withania frutescens L. Extract: Phytochemical Characterization and Acute and Repeated Dose 28-Day Oral Toxicity Studies in Mice. BioMed. Res. Int. 2020, 2020, 1976298. [Google Scholar] [CrossRef] [PubMed]
- Moussaoui, A.E.L.; Bourhia, M.; Jawhari, F.Z.; Mechchate, H.; Slighoua, M.; Bari, A.; Ullah, R.; Mahmood, H.M.; Ali, S.S.; Ibenmoussa, S.; et al. Phytochemical Identification, Acute, and Sub-Acute Oral Toxicity Studies of the Foliar Extract of Withania frutescens. Molecules 2020, 25, 4528. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.-X.; He, H.; Qiu, F. Natural Withanolides: An Overview. Natural product reports 2011, 28, 705–740. [Google Scholar] [CrossRef]
- Zhang, H.; Samadi, A.K.; Cohen, M.S.; Timmermann, B.N. Antiproliferative Withanolides from the Solanaceae: A Structure-Activity Study. Pure Appl. Chem. 2012, 84, 1353–1367. [Google Scholar] [CrossRef] [Green Version]
- Eich, E. Solanaceae and Convolvulaceae: Secondary Metabolites; Springer Nature: Cham, Switzerland, 2008. [Google Scholar] [CrossRef]
- Khan, P.M.; Ahmad, S.; Rubnawaz, H.; Malik, A. The First Report of a Withanolide from the Family Labiatae. Phytochemistry 1999, 51, 669–671. [Google Scholar] [CrossRef]
- Ksebati, M.B.; Schmitz, F.J. Minabeolides: A Group of Withanolides from a Soft Coral, Minabea Sp. J. Org. Chem. 2002, 53, 3926–3929. [Google Scholar] [CrossRef]
- Vankar, P.S.; Srivastava, J.; Molčanov, K.; Kojic-Prodić, B. Withanolide A Series Steroidal Lactones from Eucalyptus globulus Bark. Phytochem. Lett. 2009, 2, 67–71. [Google Scholar] [CrossRef]
- Yokosuka, A.; Mimaki, Y.; Sashida, Y. Chantriolides A and B, Two New Withanolide Glucosides from the Rhizomes of Tacca chantrieri. J. Nat. Prod. 2003, 66, 876–878. [Google Scholar] [CrossRef] [PubMed]
- Llanos, G.; Callies, O.; Gutiérrez, D.; Flores, N.; Jiménez, I.; Giménez, A.; Bazzocchi, I. Antiplasmodial Activity of Amides and Amines from Withania aristata, an Endemic Species of the Canary Islands. Planta Med. 2010, 76, P423. [Google Scholar] [CrossRef]
- LLanos, G.G.; Araujo, L.M.; Jiménez, I.A.; Moujir, L.M.; Vázquez, J.T.; Bazzocchi, I.L. Withanolides from Withania aristata and Their Cytotoxic Activity. Steroids 2010, 75, 974–981. [Google Scholar] [CrossRef] [PubMed]
- Llanos, G.G.; Varela, R.M.; Jiménez, I.A.; Molinillo, J.M.; Macías, F.A.; Bazzocchi, I.L. Metabolites from Withania aristata with Potential Phytotoxic Activity. Nat. Prod. Commun. 2010, 5, 1934578X1000500712. [Google Scholar] [CrossRef] [Green Version]
- Verma, S.; Patel, C.N.; Chandra, M. Identification of Novel Inhibitors of SARS-CoV-2 Main Protease (Mpro) from Withania Sp. by Molecular Docking and Molecular Dynamics Simulation. J. Comput. Chem. 2021, 42, 1861–1872. [Google Scholar] [CrossRef]
- Abdelfattah, E.M.; Aimad, A.; Bourhia, M.; Chebbac, K.; Salamatullah, A.M.; Soufan, W.; Nafidi, H.-A.; Aboul-Soud, M.A.; Ouahmane, L.; Bari, A. Insecticidal and Antifungal Activities of Chemically-Characterized Essential Oils from the Leaves of Withania frutescens L. Life 2022, 12, 88. [Google Scholar] [CrossRef]
- El Bouzidi, L.; Mahiou-Leddet, V.; Bun, S.-S.; Larhsini, M.; Abbad, A.; Markouk, M.; Fathi, M.; Boudon, M.; Ollivier, E.; Bekkouche, K. Cytotoxic Withanolides from the Leaves of Moroccan Withania frutescens. Pharm. Biol. 2013, 51, 1040–1046. [Google Scholar] [CrossRef] [Green Version]
- El Moussaoui, A.; Jawhari, F.Z.; Almehdi, A.M.; Elmsellem, H.; Benbrahim, K.F.; Bousta, D.; Bari, A. Antibacterial, Antifungal and Antioxidant Activity of Total Polyphenols of Withania frutescens L. Bioorg. Chem. 2019, 93, 103337. [Google Scholar]
- Tebeka Simur, T. Phytochemical Investigation and Antioxidant Activity of Leaf Extract of Withania somnifera from Konso, South Ethiopia. Orient. J. Chem. 2018, 34, 1824–1831. [Google Scholar] [CrossRef]
- Ozsoy, N.; Can, A.; Yanardag, R.; Akev, N. Antioxidant Activity of Smilax excelsa L. Leaf Extracts. Food Chem. 2008, 110, 571–583. [Google Scholar] [CrossRef]
- Bourhia, M.; Elmoussaoui, A.; Kadiri, M.; Chedadi, M.; Agour, A.; Sfaira, M.; Bari, A. Promising Antioxidant and Anticorrosion Activities of Mild Steel in 1.0 M Hydrochloric Acid Solution by Withania frutescens L. Essential Oil. Front. Chem. 2021, 760, 739273. [Google Scholar]
- Bourhia, M.; Moussaoui, A.E.; Jawhari, F.Z.; Khalis, H.; Chedadi, M.; Agour, A.; Bousta, D.; Bari, A. Responses of Withania frutescens L. Growing in the Mediterranean Area to Changes in the Environmental Conditions: An Approach of Adaptation. Front. Ecol. Evol. 2021, 9, 470. [Google Scholar]
- Der Duh, P.; Yen, G.C. Antioxidative Activity of Three Herbal Water Extracts. Food Chem. 1997, 60, 639–645. [Google Scholar] [CrossRef]
- Armoskaite, V.; Ramanauskiene, K.; Maruska, A.; Razukas, A.; Dagilyte, A.; Baranauskas, A.; Briedis, V. The Analysis of Quality and Antioxidant Activity of Green Tea Extracts. J. Med. Plants Res. 2011, 5, 811–816. [Google Scholar]
- Akter, R.; Hasan, S.M.R.; Hossain, M.M.; Jamila, M.; Chowdhury, S.S.; Mazumder, M.E.H.; Rahman, S. Antidiarrhoeal and Antioxidant Properties of Curcuma alismatifolia Leaves. Aust. J. Basic Appl. Sci. 2010, 4, 450–456. [Google Scholar]
- Akinwumi, K.A.; Eleyowo, O.O.; Oladipo, O.O. A Review on the Ethnobotanical Uses, Phytochemistry and Pharmacology Effect of Luffa cylindrica. In Natural Drugs from Plants; IntechOpen: London, UK, 2021. [Google Scholar]
- Ardohain, E.N.G. Avaliação Da Composição Química e Bioativa de Cultivares de Petroselinum crispum (Mill.) Nym. Ph.D. Thesis, Federal Technological University of Paraná, Curitiba, Brazil, 2022. [Google Scholar]
- Campos, F.M.; Couto, J.A.; Hogg, T.A. Influence of Phenolic Acids on Growth and Inactivation of Oenococcus oeni and Lactobacillus hilgardii. J. Appl. Microbiol. 2003, 94, 167–174. [Google Scholar] [CrossRef] [Green Version]
- Yadav, S.A.; Hakkim, L.; Ramalingam, S. Antioxidant Activity of Withania somnifera (L.) Dunal by Different Solvent Extraction Methods. J. Pharm. Res. 2011, 4, 1428–1430. [Google Scholar]
- Paul, R.K.; Kabir, H.; Chowdhury, U.K.; Rahaman, M.S.; Ahmad, M.F.; Bhattacharjya, D.K. In Vitro Antioxidant Activity of Withania somnifera Root. Int. J. Adv. Res. Chem. Sci. 2016, 3, 45–56. [Google Scholar]
- Jawhari, F.Z.; Moussaoui, A.E.L.; Bourhia, M.; Imtara, H.; Saghrouchni, H.; Ammor, K.; Ouassou, H.; Elamine, Y.; Ullah, R.; Ezzeldin, E.; et al. Anacyclus pyrethrum var. pyrethrum (L.) and Anacyclus pyrethrum var. depressus (Ball) Maire: Correlation between Total Phenolic and Flavonoid Contents with Antioxidant and Antimicrobial Activities of Chemically Characterized Extracts. Plants 2021, 10, 149. [Google Scholar] [CrossRef]
- Jeyanthi, T.; Subramanian, P.; Kumaravel, P. A Comparative Analysis of Antibacterial Activity of Withania somnifera Root Extract with Commercial Antibiotics. Asian J. Pharm. Res. 2013, 3, 98–102. [Google Scholar]
- Guzman, J.D. Natural Cinnamic Acids, Synthetic Derivatives and Hybrids with Antimicrobial Activity. Molecules 2014, 19, 19292–19349. [Google Scholar] [CrossRef] [PubMed]
- Masadeh, M.M.; Alkofahi, A.S.; Alzoubi, K.H.; Tumah, H.N.; Bani-Hani, K. Anti-Helicobactor Pylori Activity of Some Jordanian Medicinal Plants. Pharm. Biol. 2014, 52, 566–569. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liberal, Â.; Fernandes, Â.; Polyzos, N.; Petropoulos, S.A.; Dias, M.I.; Pinela, J.; Petrović, J.; Soković, M.; Ferreira, I.C.; Barros, L. Bioactive Properties and Phenolic Compound Profiles of Turnip-Rooted, Plain-Leafed and Curly-Leafed Parsley Cultivars. Molecules 2020, 25, 5606. [Google Scholar] [CrossRef] [PubMed]
- Almajano, M.P.; Carbó, R.; Delgado, M.E.; Gordon, M.H. Effect of PH on the Antimicrobial Activity and Oxidative Stability of Oil-in-Water Emulsions Containing Caffeic Acid. Food Chem. Toxicol. 2007, 72, 258–263. [Google Scholar] [CrossRef]
- Nayaka, H.B.; Londonkar, R.L.; Umesh, M.K.; Tukappa, A. Antibacterial Attributes of Apigenin, Isolated from Portulaca oleracea L. Int. J. Bacteriol. 2014, 2014, 175851. [Google Scholar] [CrossRef] [Green Version]
- Chebbac, K.; Moussaoui, A.E.; Bourhia, M.; Salamatullah, A.M.; Alzahrani, A.; Guemmouh, R. Chemical Analysis and Antioxidant and Antimicrobial Activity of Essential Oils from Artemisia negrei L. against Drug-Resistant Microbes. Evid.-Based Complement. Altern. Med. 2021, 2021, 5902851. [Google Scholar] [CrossRef]
- Askarne, L.; Talibi, I.; Boubaker, H.; Boudyach, E.H.; Msanda, F.; Saadi, B.; Serghini, M.A.; Ait Ben Aoumar, A. In Vitro and in Vivo Antifungal Activity of Several Moroccan Plants against Penicillium italicum, the Causal Agent of Citrus Blue Mold. Crop Prot. 2012, 40, 53–58. [Google Scholar] [CrossRef]
- Sadeghi, M.; Zolfaghari, B.; Senatore, M.; Lanzotti, V. Phytochemistry Letters Antifungal Cinnamic Acid Derivatives from Persian Leek (Allium ampeloprasum Subsp. Persicum). Phytochem. Lett. 2013, 6, 360–363. [Google Scholar] [CrossRef]
- Zhang, Z.; Qin, G.; Li, B.; Tian, S. Effect of Cinnamic Acid for Controlling Gray Mold on Table Grape and Its Possible Mechanisms of Action. Curr. Microbiol. 2015, 71, 396–402. [Google Scholar] [CrossRef]
- Chebbac, K.; Ghneim, H.K.; El Moussaoui, A.; Bourhia, M.; El Barnossi, A.; Benziane Ouaritini, Z.; Salamatullah, A.M.; Alzahrani, A.; Aboul-Soud, M.A.; Giesy, J.P. Antioxidant and Antimicrobial Activities of Chemically-Characterized Essential Oil from Artemisia aragonensis Lam. against Drug-Resistant Microbes. Molecules 2022, 27, 1136. [Google Scholar] [CrossRef]
- Mašković, P.Z.; Manojlović, N.T.; Mandić, A.I.; Mišan, A.Č.; Milovanović, I.L.; Radojković, M.M.; Cvijović, M.S.; Solujić, S.R. Phytochemical Screening and Biological Activity of Extracts of Plant Species Halacsya sendtneri (Boiss.) Dörfl. Hem. Ind. 2012, 66, 43–51. [Google Scholar] [CrossRef] [Green Version]
- Bourhia, M.; Laasri, F.E.; Aghmih, K.; Ullah, R.; Alqahtani, A.S.; Mahmood, H.M.; El Mzibri, M.; Said, G.; Khlil, N.; Benbacer, L. Phytochemical Composition, Antioxidant Activity, Antiproliferative Effect and Acute Toxicity Study of Bryonia Dioica Roots Used in North African Alternative Medicine. Int. J. Agric. Biol. 2020, 23, 597–602. [Google Scholar]
- Bourhia, M.; Bouothmany, K.; Bakrim, H.; Hadrach, S.; Salamatullah, A.M.; Alzahrani, A.; Khalil Alyahya, H.; Albadr, N.A.; Gmouh, S.; Laglaoui, A. Chemical Profiling, Antioxidant, Antiproliferative, and Antibacterial Potentials of Chemically Characterized Extract of Citrullus colocynthis L. Seeds. Separations 2021, 8, 114. [Google Scholar] [CrossRef]
- Aoussar, N.; Laasri, F.E.; Bourhia, M.; Manoljovic, N.; Mhand, R.A.; Rhallabi, N.; Ullah, R.; Shahat, A.A.; Noman, O.M.; Nasr, F.A. Phytochemical Analysis, Cytotoxic, Antioxidant, and Antibacterial Activities of Lichens. Evid.-Based Complement. Altern. Med. 2020, 2020, 8104538. [Google Scholar] [CrossRef]
- Agour, A.; Mssillou, I.; Saghrouchni, H.; Bari, A.; Lyoussi, B.; Derwich, E. Chemical Composition, Antioxidant Potential and Antimicrobial Properties of the Essential Oils of Haplophyllum tuberculatum (Forsskal) A. Juss from Morocco. Trop. J. Nat. Prod. Res. 2020, 4, 1108–1115. [Google Scholar] [CrossRef]
- Saghrouchni, H.; El Barnossi, A.; Salamatullah, A.M.; Bourhia, M.; Alzahrani, A.; Alkaltham, M.S.; Alyahya, H.K.; Tahiri, N.E.H.; Imtara, H.; Var, I. Carvacrol: A Promising Environmentally Friendly Agent to Fight Seeds Damping-Off Diseases Induced by Fungal Species. Agronomy 2021, 11, 985. [Google Scholar] [CrossRef]
- Amrati, F.E.-Z.; Bourhia, M.; Saghrouchni, H.; Slighoua, M.; Grafov, A.; Ullah, R.; Ezzeldin, E.; Mostafa, G.A.; Bari, A.; Ibenmoussa, S.; et al. Caralluma europaea (Guss.) N.E.Br.: Anti-Inflammatory, Antifungal, and Antibacterial Activities against Nosocomial Antibiotic-Resistant Microbes of Chemically Characterized Fractions. Molecules 2021, 26, 636. [Google Scholar] [CrossRef]
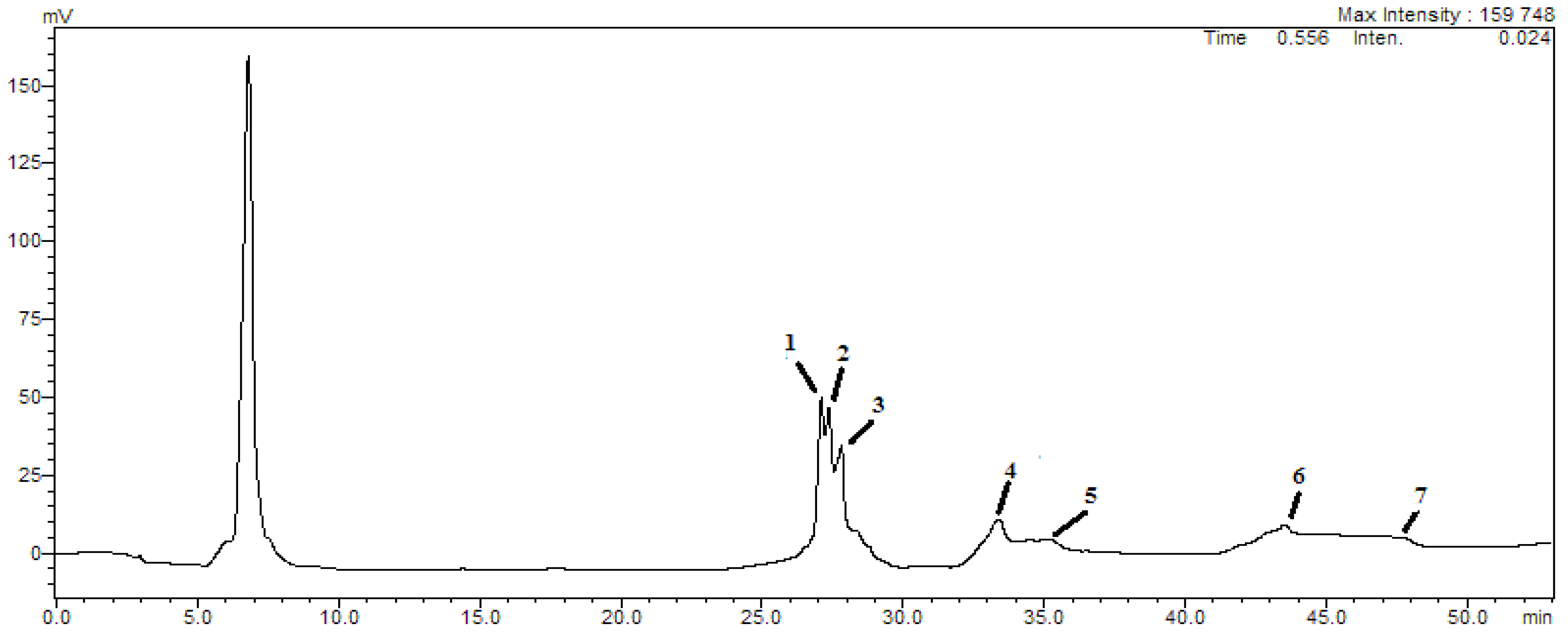

| Peaks | Retention Time | Compound | [M-H]− | mg/kg |
|---|---|---|---|---|
| 1 | 26.12 | Cichoric acid | 473 | 259.47 ± 2.57 |
| 2 | 26.81 | Caffeic acid | 179 | 189.42 ± 1.08 |
| 3 | 27.70 | Apigenin | 593 | 215.18 ± 1.87 |
| 4 | 33.34 | Luteolin | 593 | 186.74 ± 2.51 |
| 5 | 34.90 | Quercetin | 477 | 173.68 ± 3.05 |
| 6 | 43.58 | Catechin | 289 | 189.71 ± 1.93 |
| 7 | 47.69 | P-coumaric acid | 325 | 173.28 ± 2.49 |
| Diameter of the Inhibition Zone (mm) | |||||
|---|---|---|---|---|---|
| Strain | RWA | Kanamycin | Oxacillin | Streptomycin | Ceftizoxime |
| E. coli | 19.51 ± 0.74 | 0 | 11.71 ± 0.54 | 0 | 0 |
| K. pneumoniae | 18.36 ± 1.73 | 0 | 0 | 0 | 0 |
| A. baumanii | 16.21 ± 1.45 | 0 | 0 | 0 | 0 |
| S. pneumoniae | 17.5 ± 1.08 | 0 | 0 | 0 | 0 |
| S. aureus | 15.24 ± 1.31 | 0 | 9.89 ± 0.94 | 0 | 0 |
| Minimum Inhibitory Concentration (mg/mL) | |||||
|---|---|---|---|---|---|
| Strain | RWA | Oxacillin | Streptomycin | Kanamycin | Ceftizoxime |
| E. coli | 2.13 ± 0.82 | 0.041 ± 0.001 | 0.052 ± 0.003 | 0.031 ± 0.003 | 0.064 ± 0.009 |
| K. pneumoniae | 2.45 ± 0.32 | 0.041 ± 0.005 | 0.026 ± 0.007 | 0.023 ± 0.006 | 0.023 ± 0.001 |
| A. baumanii | 3.08 ± 0.27 | 0.039 ± 0.004 | 0.024 ± 0.007 | 0.014 ± 0.007 | 0.016 ± 0.004 |
| S. pneumoniae | 2.35 ± 0.64 | 0.045 ± 0.003 | 0.032 ± 0.005 | 0.022 ± 0.003 | 0.027 ± 0.003 |
| S. aureus | 4.83 ± 0.76 | 0.036 ± 0.002 | 0.029 ± 0.001 | 0.012 ± 0.004 | 0.017 ± 0.001 |
| Inhibition Diameter Zone (mm) | Minimum Inhibitory Concentration (mg/mL) | |||
|---|---|---|---|---|
| Strains | RWA | Fluconazole | RWA | Fluconazole |
| C. albicans | 29.00 ± 1.51 | 32.08 ± 1.36 | 2.04 ± 0.61 | 3.21 ± 0.04 |
| A. niger | 28.41 ± 1.08 | 35.45 ± 1.28 | 2.84 ± 0.61 | 2.44 ± 0.08 |
| A. flavus | 25.65 ± 1.14 | 31.69 ± 1.92 | 5.71 ± 0.54 | 2.52 ± 0.03 |
| F. oxysporum | 26.71 ± 1.45 | 37.74 ± 1.34 | 3.24 ± 0.38 | 3.68 ± 0.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alzahrani, A.J. Promising Antioxidant and Antimicrobial Potencies of Chemically-Profiled Extract from Withania aristata (Aiton) Pauquy against Clinically-Pathogenic Microbial Strains. Molecules 2022, 27, 3614. https://doi.org/10.3390/molecules27113614
Alzahrani AJ. Promising Antioxidant and Antimicrobial Potencies of Chemically-Profiled Extract from Withania aristata (Aiton) Pauquy against Clinically-Pathogenic Microbial Strains. Molecules. 2022; 27(11):3614. https://doi.org/10.3390/molecules27113614
Chicago/Turabian StyleAlzahrani, Alhusain J. 2022. "Promising Antioxidant and Antimicrobial Potencies of Chemically-Profiled Extract from Withania aristata (Aiton) Pauquy against Clinically-Pathogenic Microbial Strains" Molecules 27, no. 11: 3614. https://doi.org/10.3390/molecules27113614
APA StyleAlzahrani, A. J. (2022). Promising Antioxidant and Antimicrobial Potencies of Chemically-Profiled Extract from Withania aristata (Aiton) Pauquy against Clinically-Pathogenic Microbial Strains. Molecules, 27(11), 3614. https://doi.org/10.3390/molecules27113614





