Antiviral Activities of Halogenated Emodin Derivatives against Human Coronavirus NL63
Abstract
:1. Introduction
2. Results and Discussion
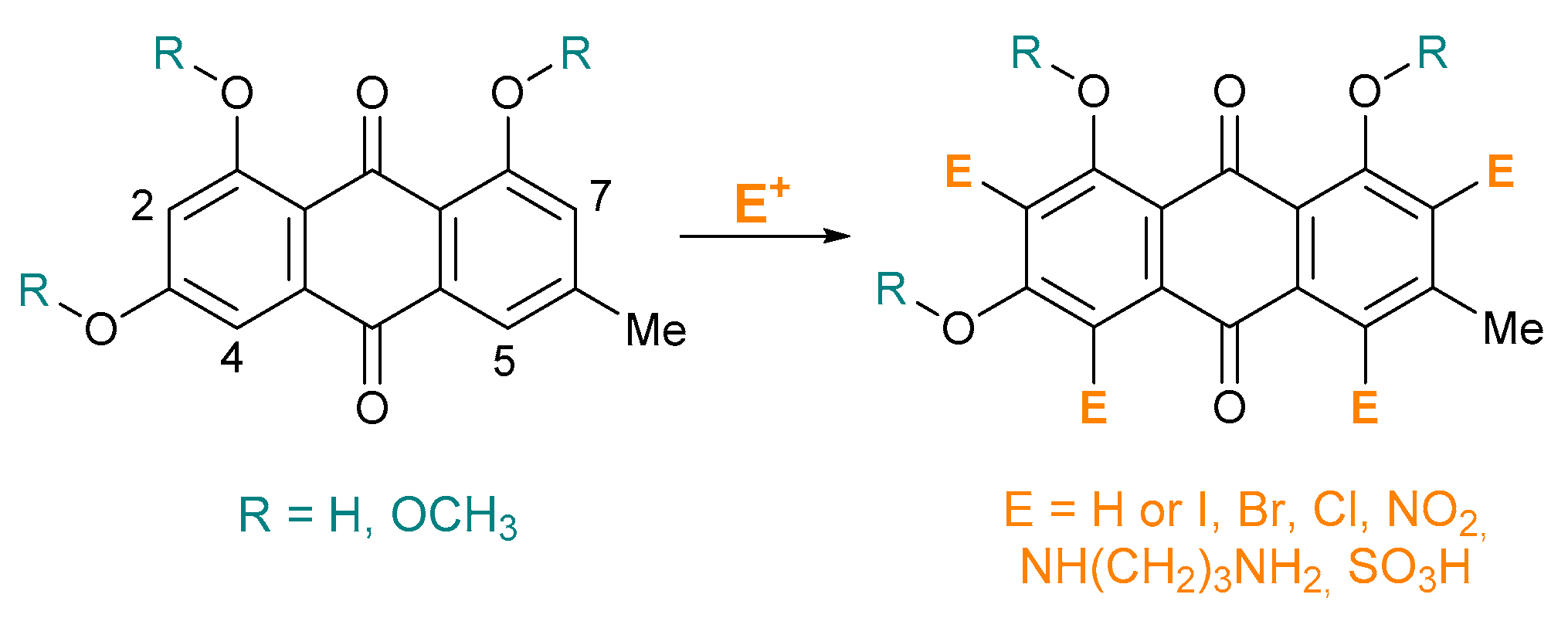
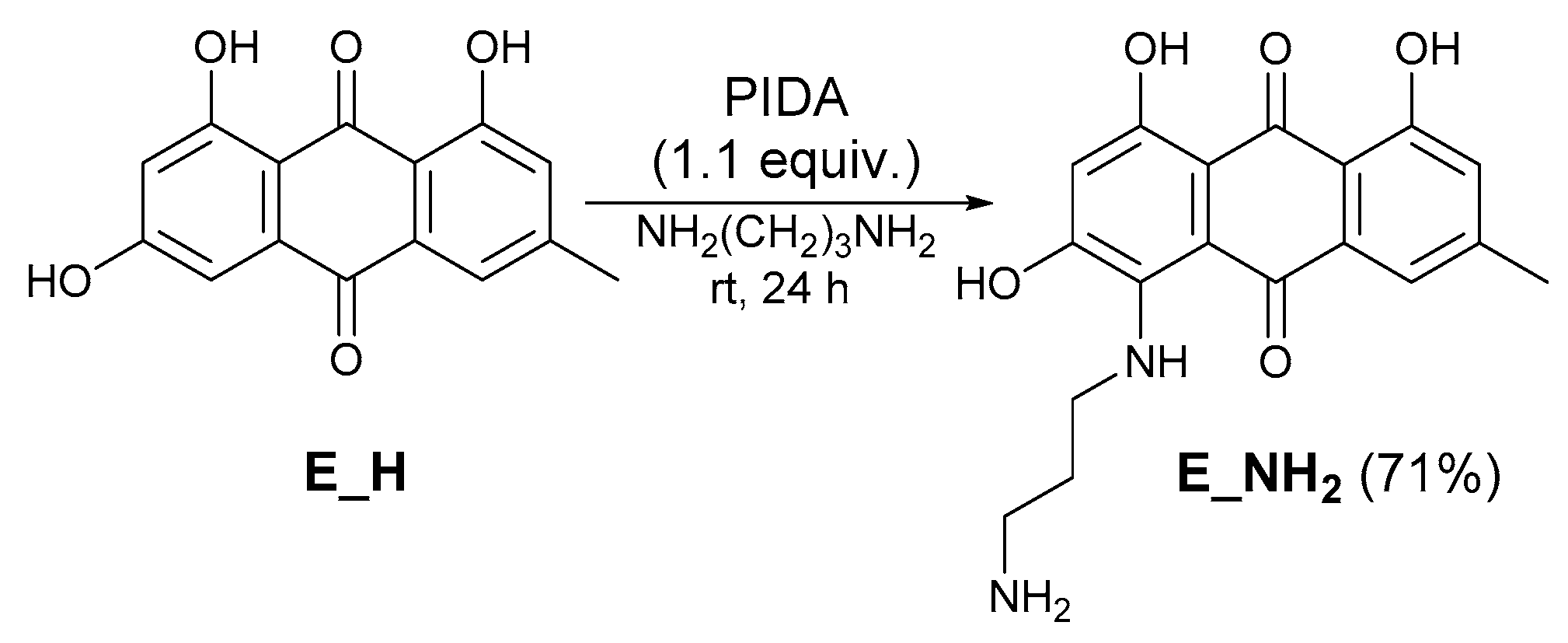
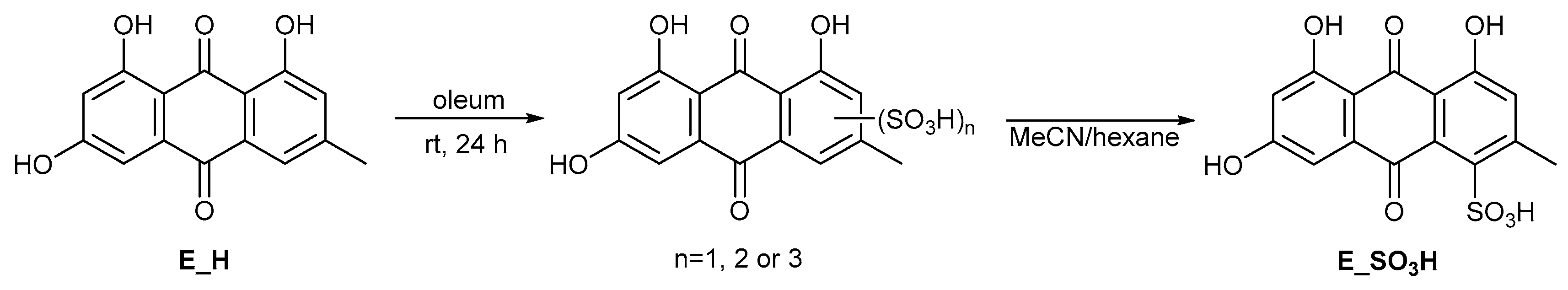
2.1. Synthesis of Emodin Derivatives
2.2. Antiviral Activity of Emodin Analogues
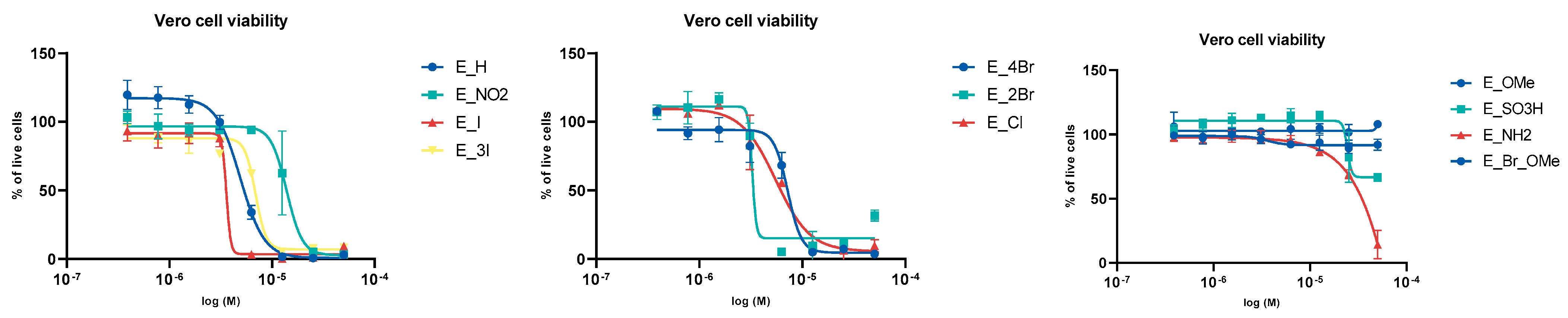
2.2.1. Evaluation of the Viability of Vero Cells in the Presence of Emodin and Emodin Analogues
2.2.2. Anti-Viral Activity of Emodin and Emodin Derivatives
3. Materials and Methods
3.1. Compound Synthesis and Structure Confirmation
3.2. Evaluation of Antiviral Activity
3.3. Evaluation of Cytotoxic and Anti-Viral Activities
4. Conclusions
5. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Xia, S.; Zhu, Y.; Liu, M.; Lan, Q.; Xu, W.; Wu, Y.; Ying, T.; Liu, S.; Shi, Z.; Jiang, S.; et al. Fusion mechanism of 2019-nCoV and fusion inhibitors targeting HR1 domain in spike protein. Cell. Mol. Immunol. 2020, 17, 765–767. [Google Scholar] [CrossRef]
- Xia, S.; Liu, M.; Wang, C.; Xu, W.; Lan, Q.; Feng, S.; Qi, F.; Bao, L.; Du, L.; Liu, S.; et al. Inhibition of SARS-CoV-2 (previously 2019-nCoV) infection by a highly potent pan-coronavirus fusion inhibitor targeting its spike protein that harbors a high capacity to mediate membrane fusion. Cell Res. 2020, 30, 343–355. [Google Scholar] [CrossRef] [Green Version]
- Attia, Y.A.; El-Saadony, M.T.; Swelum, A.A.; Qattan, S.Y.A.; Al-qurashi, A.D.; Asiry, K.A.; Shafi, M.E.; Elbestawy, A.R.; Gado, A.R.; Khafaga, A.F.; et al. COVID-19: Pathogenesis, advances in treatment and vaccine development and environmental impact-an updated review. Environ. Sci. Pollut. Res. 2021, 24, 22241–22264. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Krüger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.-H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280. [Google Scholar] [CrossRef] [PubMed]
- Walls, A.C.; Park, Y.-J.; Tortorici, M.A.; Wall, A.; McGuire, A.T.; Veesler, D. Structure, Function, and Antigenicity of the SARS-CoV-2 Spike Glycoprotein. Cell 2020, 181, 281–292. [Google Scholar] [CrossRef] [PubMed]
- Awadasseid, A.; Wu, Y.; Tanaka, Y.; Zhang, W. Effective drugs used to combat SARS-CoV-2 infection and the current status of vaccines. Biomed. Pharmacother. 2021, 137, 111330. [Google Scholar] [CrossRef] [PubMed]
- Pruijssers, A.J.; George, A.S.; Schäfer, A.; Leist, S.R.; Gralinksi, L.E.; Dinnon, K.H.; Yount, B.L.; Agostini, M.L.; Stevens, L.J.; Chappell, J.D.; et al. Remdesivir Inhibits SARS-CoV-2 in Human Lung Cells and Chimeric SARS-CoV Expressing the SARS-CoV-2 RNA Polymerase in Mice. Cell Rep. 2020, 32, 107940. [Google Scholar] [CrossRef]
- Izhaki, I. Emodin—A secondary metabolite with multiple ecological functions in higher plants. New Phytol. 2002, 155, 205–217. [Google Scholar] [CrossRef] [Green Version]
- Hsu, S.-C.; Chung, J.-G. Anticancer potential of emodin. BioMedicine 2012, 2, 108–116. [Google Scholar] [CrossRef]
- Benova, B.; Adam, M.; Pavlikova, P.; Fischer, J. Supercritical fluid extraction of piceid, resveratrol and emodin from Japanese knotweed. J. Supercrit. Fluids 2010, 51, 325–330. [Google Scholar] [CrossRef]
- Bashtanova, U.B.; Beckett, K.P.; Flowers, T.J. Review: Physiological Approaches to the Improvement of Chemical Control of Japanese Knotweed (Fallopia japonica). Weed Sci. 2009, 57, 584–592. [Google Scholar] [CrossRef]
- Chen, H.; Tuck, T.; Ji, X.; Zhou, X.; Kelly, G.; Cuerrier, A.; Zhang, J. Quality Assessment of Japanese Knotweed (Fallopia japonica) Grown on Prince Edward Island as a Source of Resveratrol. J. Agric. Food Chem. 2013, 61, 6383–6392. [Google Scholar] [CrossRef] [PubMed]
- Chang, S.-J.; Huang, S.-H.; Lin, Y.-J.; Tsou, Y.-Y.; Lin, C.-W. Antiviral activity of Rheum palmatum methanol extract and chrysophanol against Japanese encephalitis virus. Arch. Pharm. Res. 2014, 37, 1117–1123. [Google Scholar] [CrossRef]
- Dong, X.; Fu, J.; Yin, X.; Cao, S.; Li, X.; Lin, L.; Huyiligeqi; Ni, J. Emodin: A Review of Its Pharmacology, Toxicity and Pharmacokinetics. Phytother. Res. 2016, 30, 1207–1218. [Google Scholar] [CrossRef] [PubMed]
- Tuli, H.S.; Aggarwal, V.; Tuorkey, M.; Aggarwal, D.; Parashar, N.C.; Varol, M.; Savla, R.; Kaur, G.; Mittal, S.; Sak, K. Emodin: A metabolite that exhibits anti-neoplastic activities by modulating multiple oncogenic targets. Toxicol. In Vitro 2021, 73, 105142. [Google Scholar] [CrossRef] [PubMed]
- Shrimali, D.; Shanmugam, M.K.; Kumar, A.P.; Zhang, J.; Tan, B.K.H.; Ahn, K.S.; Sethi, G. Targeted abrogation of diverse signal transduction cascades by emodin for the treatment of inflammatory disorders and cancer. Cancer Lett. 2013, 341, 139–149. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, Q.; Gao, J.; Pang, X.; Chen, A.; Wang, Y. Molecular Mechanisms of Action of Emodin: As an Anti-Cardiovascular Disease Drug. Front. Pharmacol. 2020, 11, 559607. [Google Scholar] [CrossRef] [PubMed]
- Cui, Y.; Chen, L.-J.; Huang, T.; Ying, J.-Q.; Li, J. The pharmacology, toxicology and therapeutic potential of anthraquinone derivative emodin. Chin. J. Nat. Med. 2020, 18, 425–435. [Google Scholar] [CrossRef]
- Schwarz, S.; Wang, K.; Yu, W.; Sun, B.; Schwarz, W. Emodin inhibits current through SARS-associated coronavirus 3a protein. Antivir. Res. 2011, 90, 64–69. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.; Guo, M.; Wen, S.; Zhao, R.; Wang, J.; Sun, Y.; Liu, Q.; Zhou, H. Poly(ethylene glycol) dimethyl ether mediated oxidative scission of aromatic olefins to carbonyl compounds by molecular oxygen. RSC Adv. 2021, 11, 13848–13852. [Google Scholar] [CrossRef]
- Li, B.; Zhao, X.; Zhang, L.; Cheng, W. Emodin Interferes with AKT1-Mediated DNA Damage and Decreases Resistance of Breast Cancer Cells to Doxorubicin. Front. Oncol. 2021, 10, 58853. [Google Scholar] [CrossRef]
- Paudel, P.; Shrestha, S.; Park, S.E.; Seong, S.H.; Fauzi, F.M.; Jung, H.A.; Choi, J.S. Emodin Derivatives as Multi-Target-Directed Ligands Inhibiting Monoamine Oxidase and Antagonizing Vasopressin V1A Receptors. ACS Omega 2020, 5, 26720–26731. [Google Scholar] [CrossRef]
- Paudel, P.; Seong, S.H.; Fauzi, F.M.; Bender, A.; Jung, H.A.; Choi, J.S. Establishing GPCR Targets of hMAO Active Anthraquinones from Cassia obtusifolia Linn Seeds Using In Silico and In Vitro Methods. ACS Omega 2020, 5, 7705–7715. [Google Scholar] [CrossRef] [Green Version]
- Teich, L.; Daub, K.S.; Krügel, V.; Nissler, L.; Gebhardt, R.; Eger, K. Synthesis and biological evaluation of new derivatives of emodin. Bioorg. Med. Chem. 2004, 12, 5961–5971. [Google Scholar] [CrossRef]
- Wang, X.P.; Xu, W.F. Facile Synthesis of Emodin Derivatives as Potential MMPIs. Bull. Korean Chem. Soc. 2005, 26, 1923–1924. [Google Scholar] [CrossRef]
- Zhu, X.; Chen, Q.; Yang, Y.; Ai, X.; Chen, S.; Song, Y. Synthesis and anti-inflammatory effects of novel emodin derivatives bearing azole moieties. Arch. Pharm. 2020, 353, 1900264. [Google Scholar] [CrossRef] [PubMed]
- Yang, K.; Jin, M.-J.; Quan, Z.-S.; Piao, H.-R. Design and Synthesis of Novel Anti-Proliferative Emodin Derivatives and Studies on Their Cell Cycle Arrest, Apoptosis Pathway and Migration. Molecules 2019, 24, 884. [Google Scholar] [CrossRef] [Green Version]
- Duan, F.; Li, X.; Cai, S.; Xin, G.; Wang, Y.; Du, D.; He, S.; Huang, B.; Guo, X.; Zhao, H.; et al. Haloemodin as Novel Antibacterial Agent Inhibiting DNA Gyrase and Bacterial Topoisomerase I. J. Med. Chem. 2014, 57, 3707–3714. [Google Scholar] [CrossRef] [PubMed]
- Koerner, S.K.; Hanai, J.-I.; Bai, S.; Jernigan, F.E.; Oki, M.; Komaba, C.; Shuto, E.; Sukhatme, V.P.; Sun, L. Design and synthesis of emodin derivatives as novel inhibitors of ATP-citrate lyase. Eur. J. Med. Chem. 2017, 126, 920–928. [Google Scholar] [CrossRef] [PubMed]
- Chalothorn, T.; Rukachaisirikul, V.; Phongpaichit, S.; Pannara, S.; Tansakul, C. Synthesis and antibacterial activity of emodin and its derivatives against methicillin-resistant Staphylococcus aureus. Tetrahedron Lett. 2019, 60, 151004. [Google Scholar] [CrossRef]
- Duan, F.; Xin, G.; Niu, H.; Huang, W. Chlorinated emodin as a natural antibacterial agent against drug-resistant bacteria through dual influence on bacterial cell membranes and DNA. Sci. Rep. 2017, 7, 12721. [Google Scholar] [CrossRef] [Green Version]
- Xiong, H.-R.; Luo, J.; Hou, W.; Xiao, H.; Yang, Z.-Q. The effect of emodin, an anthraquinone derivative extracted from the roots of Rheum tanguticum, against herpes simplex virus in vitro and in vivo. J. Ethnopharmacol. 2011, 133, 718–723. [Google Scholar] [CrossRef] [PubMed]
- Hsiang, C.Y.; Ho, T.Y. Emodin is a novel alkaline nuclease inhibitor that suppresses herpes simplex virus type 1 yields in cell cultures. Br. J. Pharmacol. 2008, 155, 227–235. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shuangsuo, D.; Zhengguo, Z.; Yunru, C.; Xin, Z.; Baofeng, W.; Lichao, Y.; Yan’an, C. Inhibition of the replication of hepatitis B virus in vitro by emodin. Med. Sci. Monit. 2006, 12, Br302–Br306. [Google Scholar]
- Parvez, M.K.; Al-Dosari, M.S.; Alam, P.; Rehman, M.; Alajmi, M.F.; Alqahtani, A.S. The anti-hepatitis B virus therapeutic potential of anthraquinones derived from Aloe vera. Phytother. Res. 2019, 33, 2960–2970. [Google Scholar] [CrossRef] [PubMed]
- Barnard, D.L.; Huffman, J.H.; Morris, J.L.B.; Wood, S.G.; Hughes, B.G.; Sidwell, R.W. Evaluation of the antiviral activity of anthraquinones, anthrones and anthraquinone derivatives against human cytomegalovirus. Antivir. Res. 1992, 17, 63–77. [Google Scholar] [CrossRef]
- Dai, J.-P.; Wang, Q.-W.; Su, Y.; Gu, L.-M.; Zhao, Y.; Chen, X.-X.; Chen, C.; Li, W.-Z.; Wang, G.-F.; Li, K.-S. Emodin Inhibition of Influenza A Virus Replication and Influenza Viral Pneumonia via the Nrf2, TLR4, p38/JNK and NF-kappaB Pathways. Molecules 2017, 22, 1754. [Google Scholar] [CrossRef] [Green Version]
- Batista, M.N.; Braga, A.C.S.; Campos, G.R.F.; Souza, M.M.; Matos, R.P.A.; Lopes, T.Z.; Candido, N.M.; Lima, M.L.D.; Machado, F.C.; Andrade, S.T.Q.d.; et al. Natural Products Isolated from Oriental Medicinal Herbs Inactivate Zika Virus. Viruses 2019, 11, 49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, H.M.; Wang, F.; Qiu, Y.; Ye, X.; Hanson, P.; Shen, H.; Yang, D. Emodin inhibits coxsackievirus B3 replication via multiple signalling cascades leading to suppression of translation. Biochem. J. 2016, 473, 473–485. [Google Scholar] [CrossRef] [PubMed]
- Ding, Y.; Xu, J.; Cheng, L.-B.; Huang, Y.-Q.; Wang, Y.-Q.; Li, H.; Li, Y.; Ji, J.-Y.; Zhang, J.-H.; Zhao, L. Effect of Emodin on Coxsackievirus B3m-Mediated Encephalitis in Hand, Foot, and Mouth Disease by Inhibiting Toll-Like Receptor 3 Pathway In Vitro and In Vivo. J. Infect. Dis. 2020, 222, 443–455. [Google Scholar] [CrossRef] [PubMed]
- Semple, S.J.; Pyke, S.M.; Reynolds, G.D.; Flower, R.L.P. In vitro antiviral activity of the anthraquinone chrysophanic acid against poliovirus. Antiv. Res. 2001, 49, 169–178. [Google Scholar] [CrossRef]
- Wang, Z.; Zheng, N.; Liang, J.; Wang, Q.; Zu, X.; Wang, H.; Yuan, H.; Zhang, R.; Guo, S.; Liu, Y.; et al. Emodin resists to Cyprinid herpesvirus 3 replication via the pathways of Nrf2/Keap1-ARE and NF-κB in the ornamental koi carp (Cyprinus carpio haematopterus). Comp. Biochem. Physiol. Part C: Toxicol. Pharmacol. 2021, 246, 109023. [Google Scholar] [CrossRef] [PubMed]
- Adhikari, B.; Marasini, B.P.; Rayamajhee, B.; Bhattarai, B.R.; Lamichhane, G.; Khadayat, K.; Adhikari, A.; Khanal, S.; Parajuli, N. Potential roles of medicinal plants for the treatment of viral diseases focusing on COVID-19: A review. Phytother. Res. 2021, 35, 1298–1312. [Google Scholar] [CrossRef] [PubMed]
- Vougogiannopoulou, K.; Corona, A.; Tramontano, E.; Alexis, M.N.; Skaltsounis, A.-L. Natural and Nature-Derived Products Targeting Human Coronaviruses. Molecules 2021, 26, 448. [Google Scholar] [CrossRef]
- Remali, J.; Aizat, W.M. A Review on Plant Bioactive Compounds and Their Modes of Action Against Coronavirus Infection. Front. Pharmacol. 2021, 11, 589044. [Google Scholar] [CrossRef] [PubMed]
- Illian, D.N.; Siregar, E.S.; Sumaiyah, S.; Utomo, A.R.; Nuryawan, A.; Basyuni, M. Potential compounds from several Indonesian plants to prevent SARS-CoV-2 infection: A mini-review of SARS-CoV-2 therapeutic targets. Heliyon 2021, 7, e06001. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Hou, Y.; Shen, J.; Huang, Y.; Martin, W.; Cheng, F. Network-based drug repurposing for novel coronavirus 2019-nCoV/SARS-CoV-2. Cell Discov. 2020, 6, 14. [Google Scholar] [CrossRef] [Green Version]
- Islam, M.T.; Sarkar, C.; El-Kersh, D.M.; Jamaddar, S.; Uddin, S.J.; Shilpi, J.A.; Mubarak, M.S. Natural products and their derivatives against coronavirus: A review of the non-clinical and pre-clinical data. Phytother. Res. 2020, 34, 2471–2492. [Google Scholar] [CrossRef]
- Ho, T.-Y.; Wu, S.-L.; Chen, J.-C.; Li, C.-C.; Hsiang, C.-Y. Emodin blocks the SARS coronavirus spike protein and angiotensin-converting enzyme 2 interaction. Antivir. Res. 2007, 74, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Das, S.; Singha Roy, A. Naturally Occurring Anthraquinones as Potential Inhibitors of SARS-CoV-2 Main Protease: A Molecular Docking Study. In ChemRxiv; Cambridge Open Engage: Cambridge, UK, 2020. [Google Scholar] [CrossRef]
- Singh, J.; Pandit, P.; McArthur, A.G.; Banerjee, A.; Mossman, K. Evolutionary trajectory of SARS-CoV-2 and emerging variants. Virol. J. 2021, 18, 166. [Google Scholar] [CrossRef] [PubMed]
- Abdul-Rasool, S.; Fielding, B.C. Understanding Human Coronavirus HCoV-NL63. Open Virol. J. 2010, 4, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Chakraborty, A.; Diwan, A. NL63: A Better Surrogate Virus for studying SARS-CoV-2. Integr. Mol. Med. 2020, 7, 1–9. [Google Scholar] [CrossRef]
- Muzychkina, R.A.; Pribytkova, L.N. Bromination of emodin. Chem. Nat. Compd. 1990, 26, 524–527. [Google Scholar] [CrossRef]

| Entry | Reagent (equiv.) | Solvent | Conditions | Relative Distribution a | |||
|---|---|---|---|---|---|---|---|
| E_H | E_I | E_2I | E_3I | ||||
| 1 | I2 (2), NaHCO3 | THF/H2O | rt., 1 h | - | 100 (73%) | - | - |
| 2 | I2 (4), NaHCO3 | THF/H2O | rt., 1 h | - | 100 | - | - |
| 3 | I2 (10), NaHCO3 | THF/H2O | rt., 24 h | - | - | - | 100 (81%) |
| 4 | I2 (10), NaHCO3 | THF/H2O | 60 °C, 24 h | - | - | - | 100 |
| 5 | NIS (1) | THF | rt., 24 h | 3 | 97 | - | - |
| 6 | NIS (1.3) | THF | rt., 3 h | - | 100 (84%) | - | - |
| 7 | NIS (1.3) | THF | rt., 24 h | - | 93 | 7 | - |
| 8 | NIS (2) | THF | rt., 24 h | - | 86 | 14 | - |
| 9 | NIS (4) | THF | rt., 24 h | - | - | 56 | 44 |
| 10 | NIS (4) | THF | 60 °C, 24 h | - | - | - | 100 (79%) |
| 11 | I2 (1) | 2-MeTHF | rt., 24 h | 100 | - | - | - |
| 12 | I2 (0.5), H2O2 (8) | 2-MeTHF | rt., 24 h | 56 | 44 | - | - |
| 13 | I2 (1), H2O2 (8) | 2-MeTHF | rt., 24 h | 21 | 79 | - | - |
| 14 | I2 (1.5), H2O2 (2.5) | 2-MeTHF | rt., 24 h | 16 | 84 | - | - |
| 15 | I2 (1.5), H2O2 (4) | 2-MeTHF | rt., 24 h | 13 | 87 | - | - |
| 16 | I2 (2), H2O2 (2.5) | 2-MeTHF | rt., 24 h | - | 100 (93%) | - | - |
| 17 | I2 (8), H2O2 (8) | 2-MeTHF | rt., 24 h | - | 100 | - | - |
| Entry | Reagent (Equiv.) | Solvent | Conditions | Relative Distribution a | ||||
|---|---|---|---|---|---|---|---|---|
| E_H | E_Br | E_2Br | E_3Br | E_4Br | ||||
| 1 | NBS (1) | THF | 0 °C, 10 min | 34 | 40 | 26 | - | - |
| 2 | NBS (1.5) | THF | 0 °C, 15 min | 17 | 43 | 40 | - | - |
| 3 | NBS (2.2) | THF | 0 °C, 30 min | - | - | 100 (88%) | - | - |
| 4 | NBS (3) | THF | 0 °C, 24 h | - | - | 63 | 37 | - |
| 5 | NBS (3) | THF | rt., 24 h | - | - | 27 | 73 | - |
| 6 | NBS (4) | THF | rt., 24 h | - | - | - | 60 | 40 |
| 7 | NBS (5) | THF | rt., 24 h | - | - | - | - | 100 (83%) |
| 8 | HBr (1), H2O2 (2.5) | TFE | 0 °C, 2 h | 29 | 71 | - | - | - |
| 9 | HBr (1.3), H2O2 (5) | TFE | 0 °C, 2 h | 67 | 31 | 2 | - | - |
| 10 | HBr (2.5), H2O2 (5) | TFE | 0 °C, 2 h | 8 | 81 | 11 | - | - |
| 11 | HBr (1), H2O2 (5) | TFE | rt., 24 h | 9 | 79 | 12 | - | - |
| 12 | HBr (2), H2O2 (5) | TFE | rt., 24 h | - | 28 | 72 | - | - |
| 13 | HBr (2.4), H2O2 (5) | TFE | rt., 24 h | - | 14 | 86 | - | - |
| 14 | HBr (4), H2O2 (5) | TFE | rt., 24 h | - | - | 100 (91%) | - | - |
| Entry | Reagent (Equiv.) | Solvent | Conditions | Relative Distribution a | |||
|---|---|---|---|---|---|---|---|
| E_H | E_Cl | E_2Cl | E_3Cl | ||||
| 1 | NCS (1) | THF | rt., 24 h | 100 | - | - | - |
| 2 | NCS (2) | THF | rt., 24 h | 49 | 42 | 9 | - |
| 3 | NCS b (2.5) | THF | rt., 3 h | - | - | 100 (81%) | - |
| 4 | NCS b (6) | THF | 60 °C, 24 h | - | - | 100 | - |
| 5 | HCl (1), H2O2 (2) | TFE | rt., 24 h | 56 | 36 | 8 | - |
| 6 | HCl (2), H2O2 (5) | TFE | rt., 24 h | 10 | 68 | 22 | - |
| 7 | HCl (3), H2O2 (5) | TFE | rt., 24 h | - | 44 | 39 | 17 |
| 8 | HCl (4), H2O2 (5) | TFE | rt., 24 h | - | 41 | 37 | 22 |
| 9 | HCl (5), H2O2 (10) | TFE | rt., 24 h | - | 17 | 50 | 33 |
| Entry | Reagent (Equiv.) a | Conditions | Conv. b | |
|---|---|---|---|---|
| E_X | E_4NO2 | |||
| 1 | HNO3 (1), H2SO4 (4), MeCN | 0 °C, 1 h | 2% | - |
| 2 | HNO3 (2.5), H2SO4 (10) | 0 °C, 1 h | 78% | 22% |
| 3 | HNO3 (2.5), H2SO4 (20) | 0 °C, 1 h | 79% | 21% |
| 4 | HNO3 (3), H2SO4 (10) | 0 °C, 1 h | 59% | 41% |
| 5 | HNO3 (3), H2SO4 (20) | 0 °C, 1 h | 27% | 73% |
| 6 | HNO3 (4.4), H2SO4 (20) | 0 °C, 1 h | 10% | 90% |
| 7 | HNO3 (6.2), H2SO4 (5) | 0 °C, 0.25 h | 13% | 87% |
| 8 | HNO3 (6.2), H2SO4 (10) | 0 °C, 0.5 h | - | 100 (91%) |
| 9 | HNO3 (63), H2SO4 (80) | 0 °C, 1 h; rt, 4 h | - | 100 % [24] |
| IC50 (µM) | ||
|---|---|---|
| Exp. | CT | |
| E_H | 2.5 | 4.9 |
| E_4NO2 | 6.1 | 6.1 |
| E_I | 1.3 | 3.6 |
| E_3I | 0.5 | 4.9 |
| E_4Br | 1.7 | 7.2 |
| E_2Br | 1.0 | 5.4 |
| E_2Cl | 1.1 | 7.5 |
| E_OMe | >50 | 8.7 |
| E_SO3H | 22.0 | >50 |
| E_NH2 | 6.3 | 41.8 |
| E_Br_OMe | >50 | >50 |
| Remdesivir | 0.61 | |
| Chloroquine | 19.2 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Horvat, M.; Avbelj, M.; Durán-Alonso, M.B.; Banjanac, M.; Petković, H.; Iskra, J. Antiviral Activities of Halogenated Emodin Derivatives against Human Coronavirus NL63. Molecules 2021, 26, 6825. https://doi.org/10.3390/molecules26226825
Horvat M, Avbelj M, Durán-Alonso MB, Banjanac M, Petković H, Iskra J. Antiviral Activities of Halogenated Emodin Derivatives against Human Coronavirus NL63. Molecules. 2021; 26(22):6825. https://doi.org/10.3390/molecules26226825
Chicago/Turabian StyleHorvat, Monika, Martina Avbelj, María Beatriz Durán-Alonso, Mihailo Banjanac, Hrvoje Petković, and Jernej Iskra. 2021. "Antiviral Activities of Halogenated Emodin Derivatives against Human Coronavirus NL63" Molecules 26, no. 22: 6825. https://doi.org/10.3390/molecules26226825
APA StyleHorvat, M., Avbelj, M., Durán-Alonso, M. B., Banjanac, M., Petković, H., & Iskra, J. (2021). Antiviral Activities of Halogenated Emodin Derivatives against Human Coronavirus NL63. Molecules, 26(22), 6825. https://doi.org/10.3390/molecules26226825







