Self-Assembling Drug Formulations with Tunable Permeability and Biodegradability
Abstract
1. Introduction
2. Patient- and Eco-Friendly Amphiphilic Nanocontainers
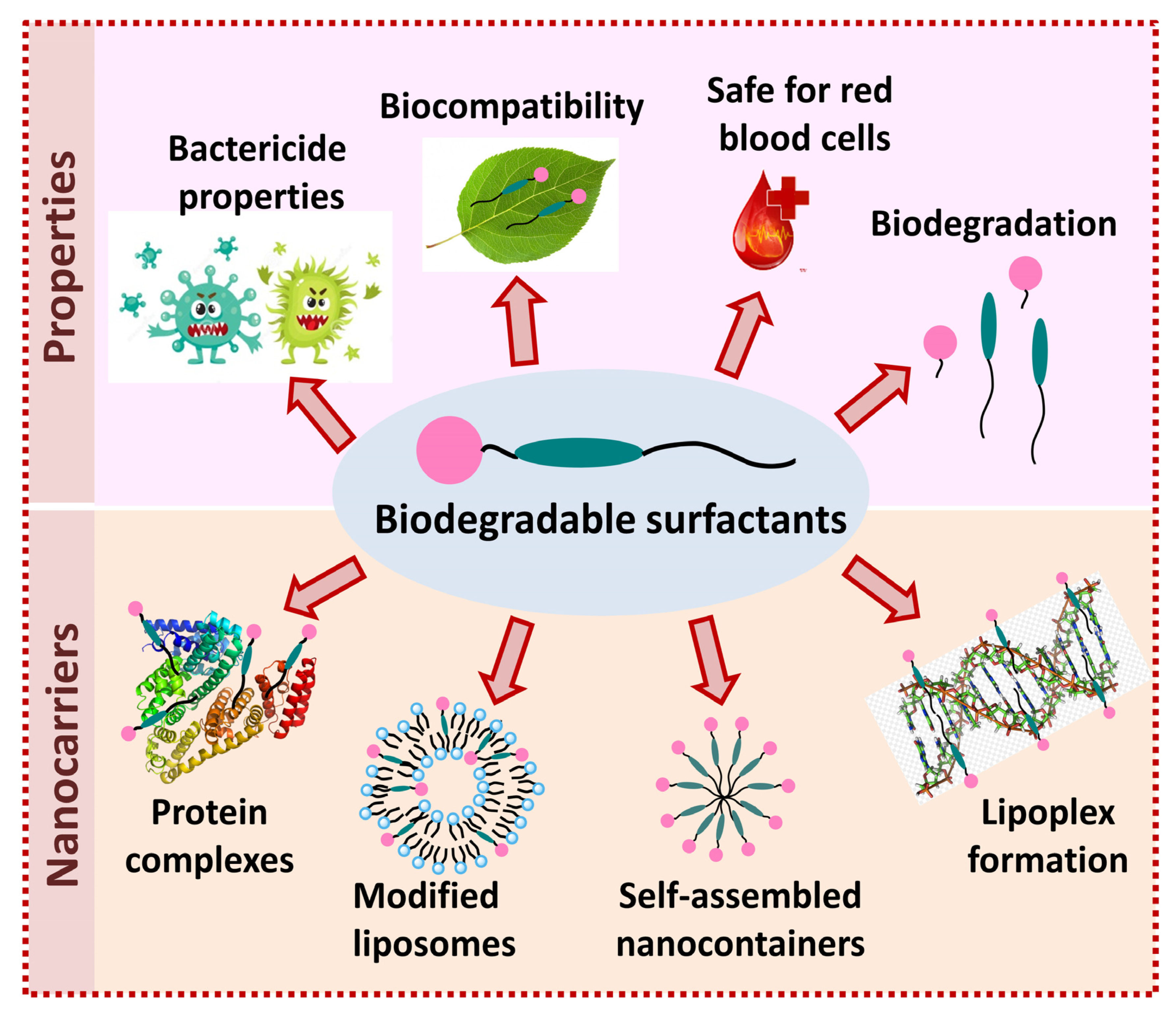
2.1. Nanocontainers Based on Biodegradable Surfactants
2.2. Biodegradable Surfactants
2.2.1. Amino Acid Surfactants
2.2.2. Surfactants with Ester and Carbamate Fragments
3. Nanoencapsulation of Drugs as Powerful and Versatile Tool to Cross the Biological Barriers
3.1. Lipid-Based Nanocarriers
3.1.1. Niosomes
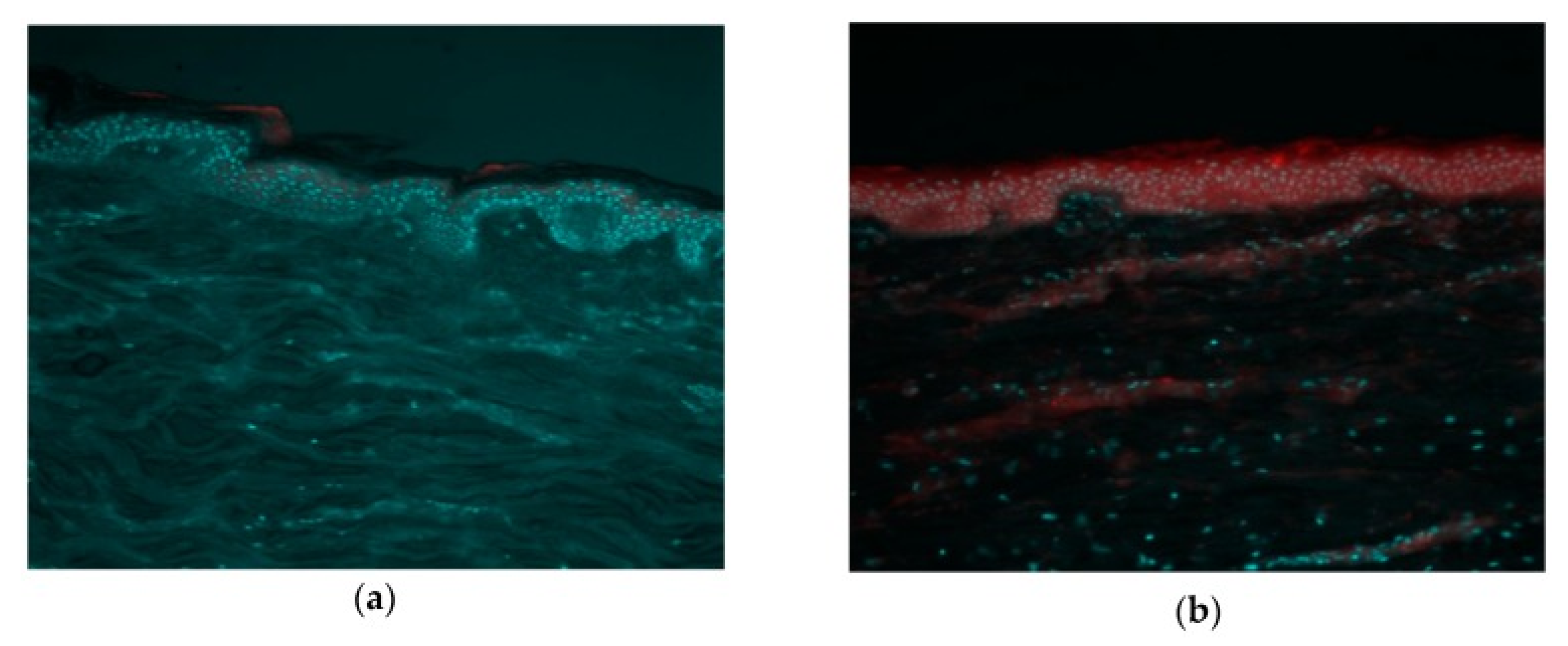
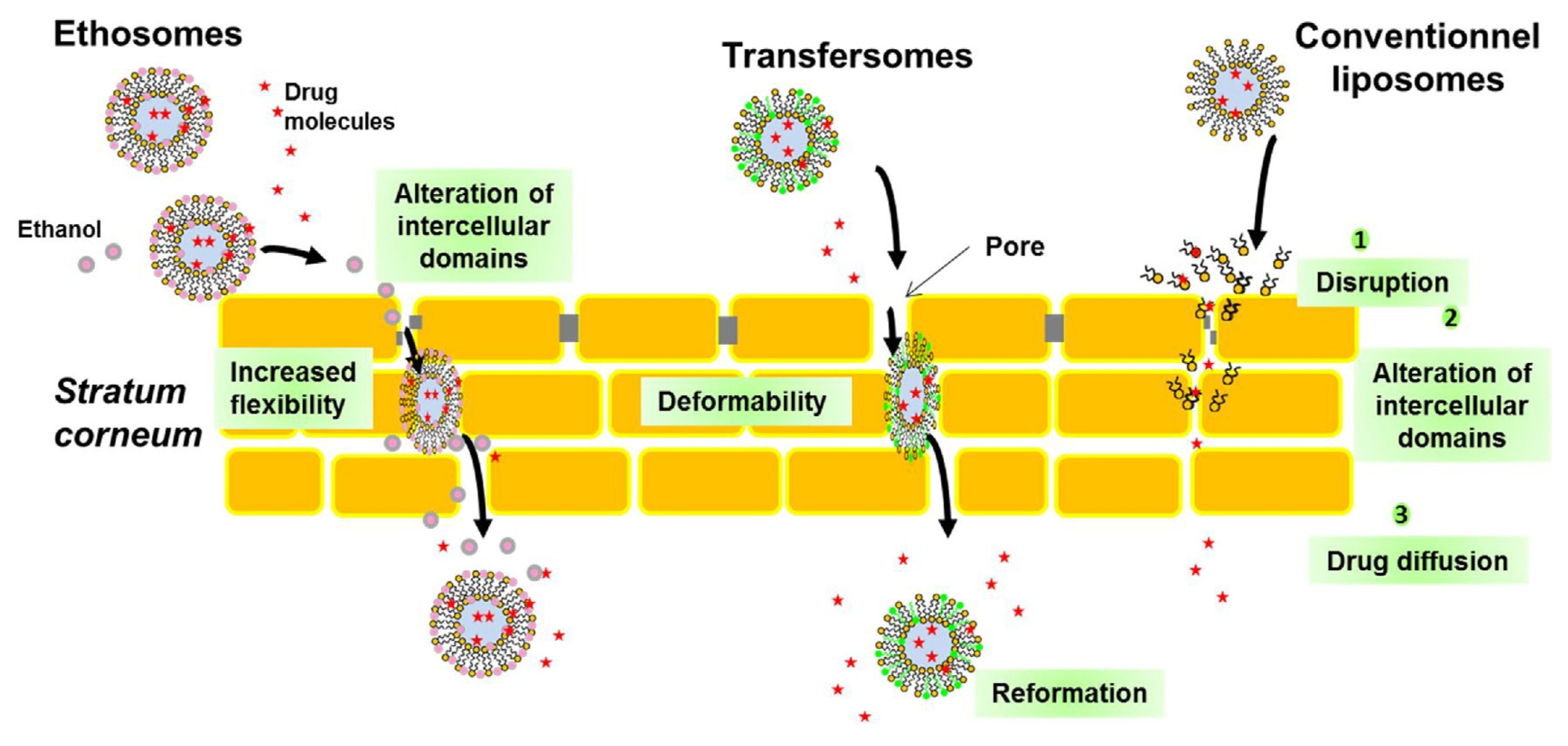
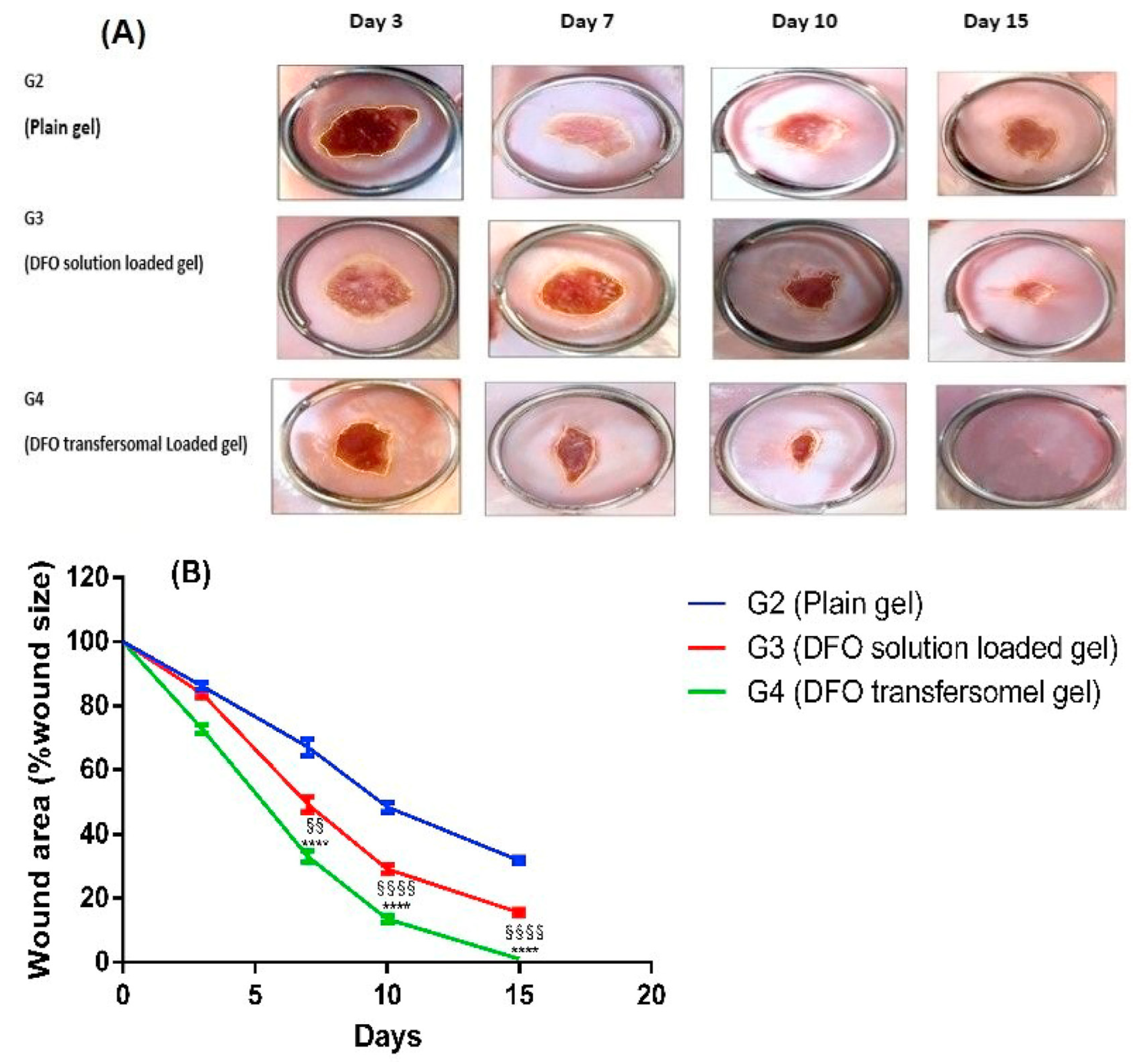
3.1.2. Transfersomes and Transethosomes
3.1.3. Chitosomes
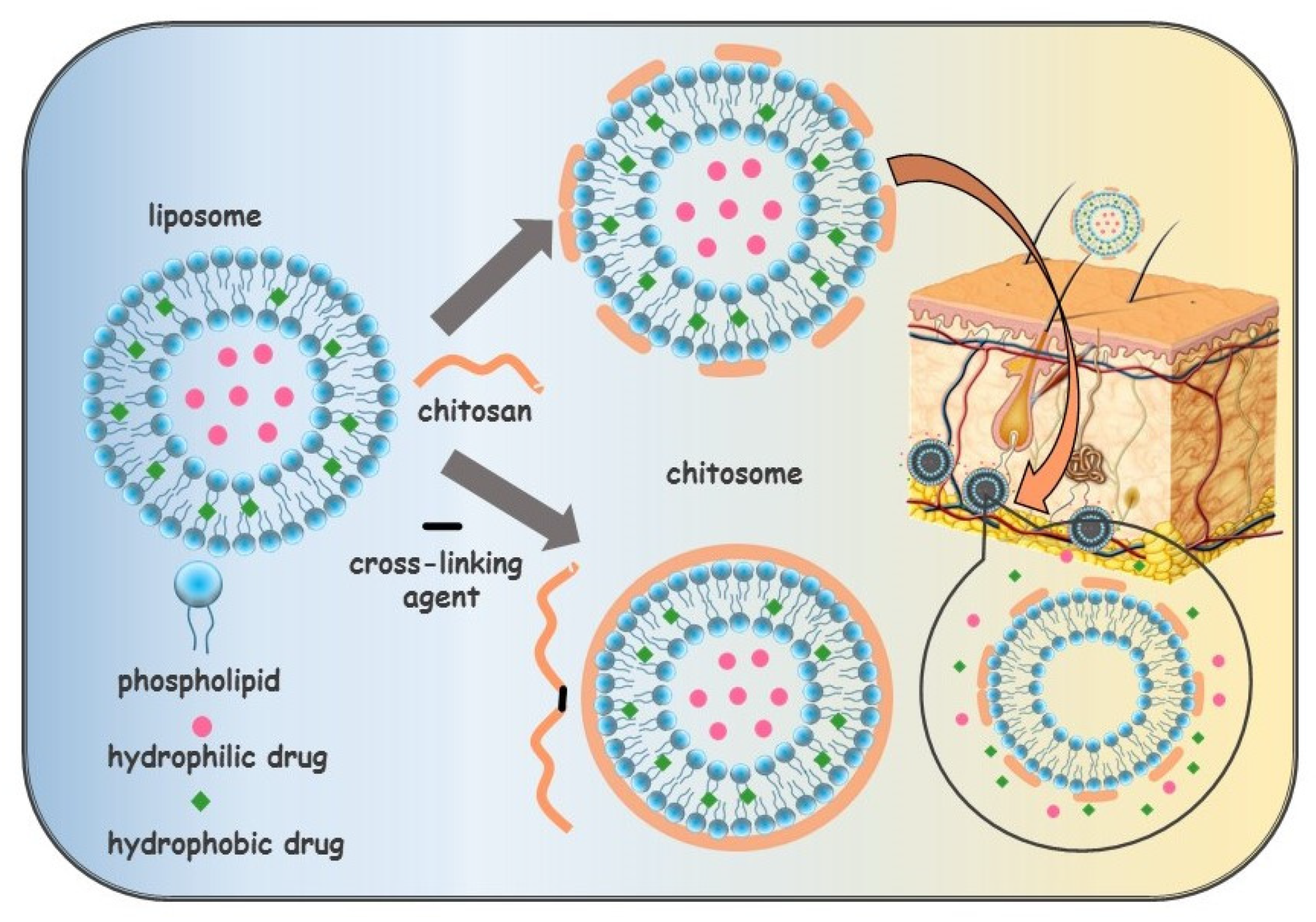
3.1.4. Invasomes
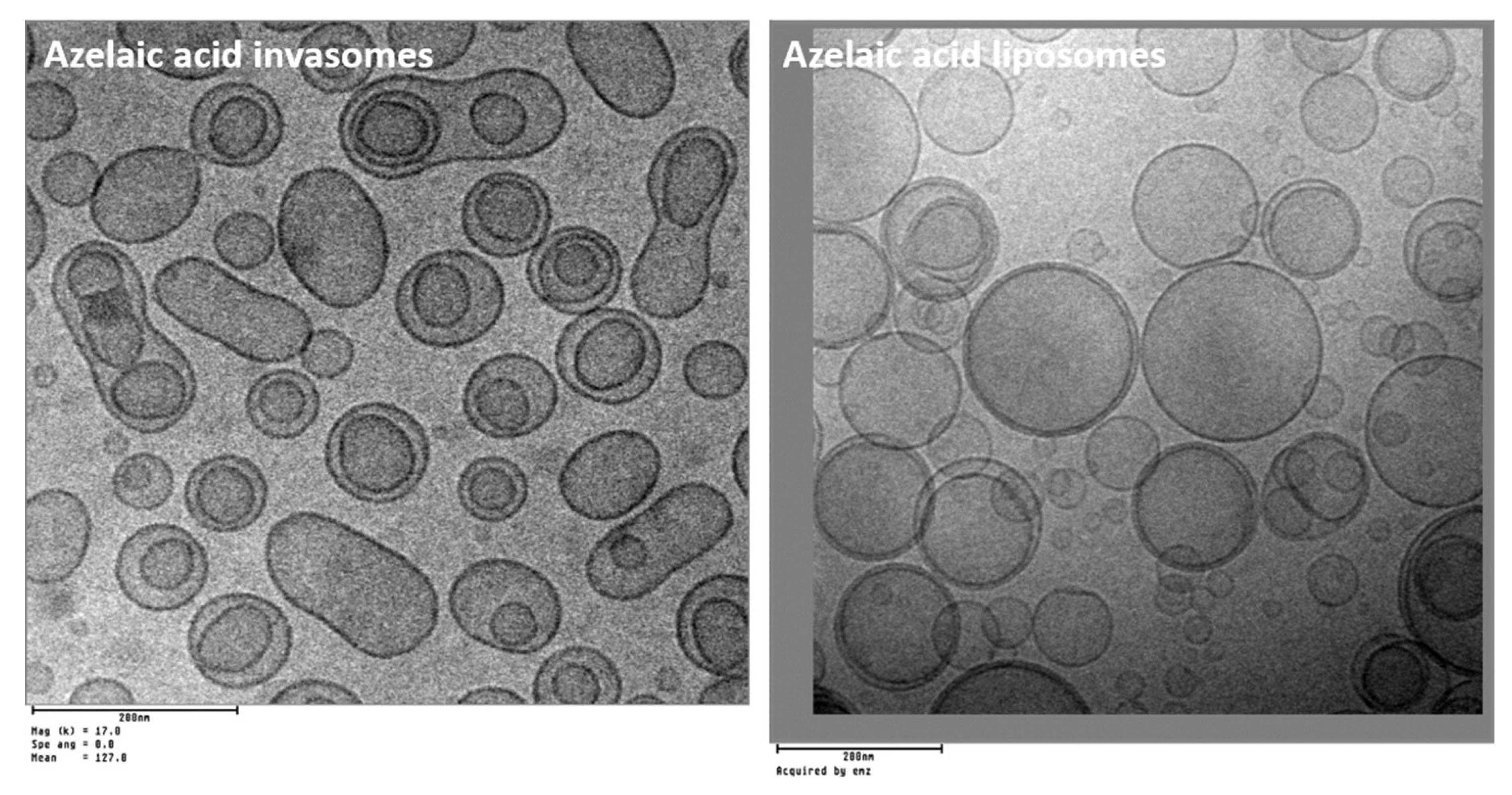
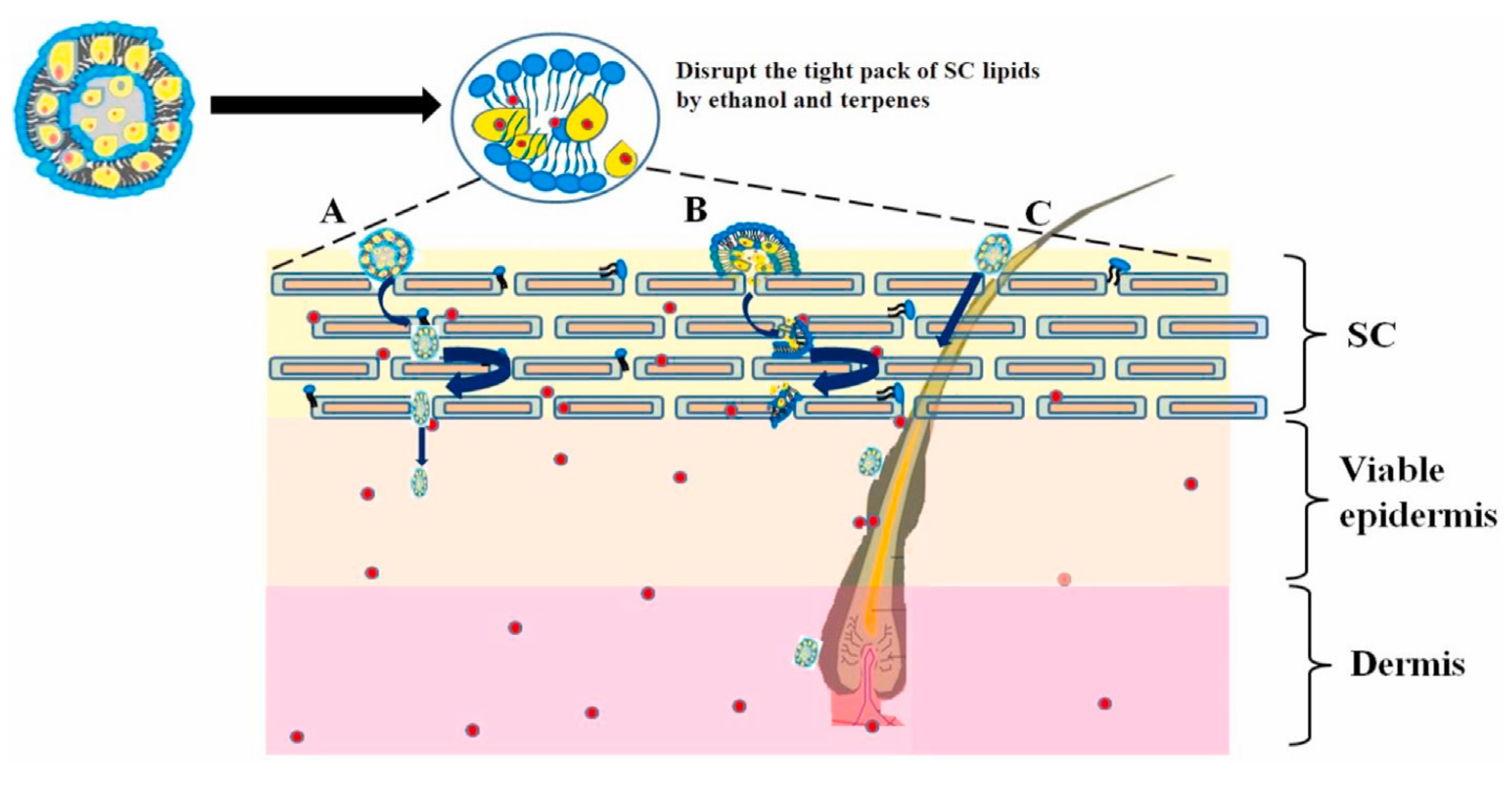
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ouma Okeyo, P.; Thoppe Rajendran, S.; Zór, K.; Boisen, A. Sensing technologies and experimental platforms for the characterization of advanced oral drug delivery systems. Adv. Drug Deliv. Rev. 2021, 176, 113850. [Google Scholar] [CrossRef] [PubMed]
- Xu, Y.; Michalowski, C.B.; Beloqui, A. Advances in lipid carriers for drug delivery to the gastrointestinal tract. Curr. Opin. Colloid Interface Sci. 2021, 52, 101414. [Google Scholar] [CrossRef]
- Emad, N.A.; Ahmed, B.; Alhalmi, A.; Alzobaidi, N.; Al-Kubati, S.S. Recent progress in nanocarriers for direct nose to brain drug delivery. J. Drug Deliv. Sci. Technol. 2021, 64, 102642. [Google Scholar] [CrossRef]
- Guimarães, D.; Cavaco-Paulo, A.; Nogueira, E. Design of liposomes as drug delivery system for therapeutic applications. Int. J. Pharm. 2021, 601, 120571. [Google Scholar] [CrossRef]
- Zhiltsova, E.P.; Ibatullina, M.R.; Mirgorodskaya, A.B.; Gainanova, G.A.; Kuznetsova, D.A.; Kashapov, R.R.; Zakharova, L.Y. Polyfunctional nanosystems on amphiphilic and hybrid platform: Self-assembly, mesogenic properties and application. Liq. Cryst. Their Appl. 2020, 20, 5–25. [Google Scholar] [CrossRef]
- Kuznetsova, D.A.; Vasileva, L.A.; Gaynanova, G.A.; Pavlov, R.V.; Sapunova, A.S.; Voloshina, A.D.; Sibgatullina, G.V.; Samigullin, D.V.; Petrov, K.A.; Zakharova, L.Y.; et al. Comparative study of cationic liposomes modified with triphenylphosphonium and imidazolium surfactants for mitochondrial delivery. J. Mol. Liq. 2021, 330, 115703. [Google Scholar] [CrossRef]
- Kuznetsova, D.A.; Gaynanova, G.A.; Vasileva, L.A.; Sibgatullina, G.V.; Samigullin, D.V.; Sapunova, A.S.; Voloshina, A.D.; Galkina, I.V.; Petrov, K.A.; Zakharova, L.Y. Mitochondria-targeted cationic liposomes modified with alkyltriphenylphosphonium bromides loaded with hydrophilic drugs: Preparation, cytotoxicity and colocalization assay. J. Mater. Chem. B 2019, 7, 7351–7362. [Google Scholar] [CrossRef]
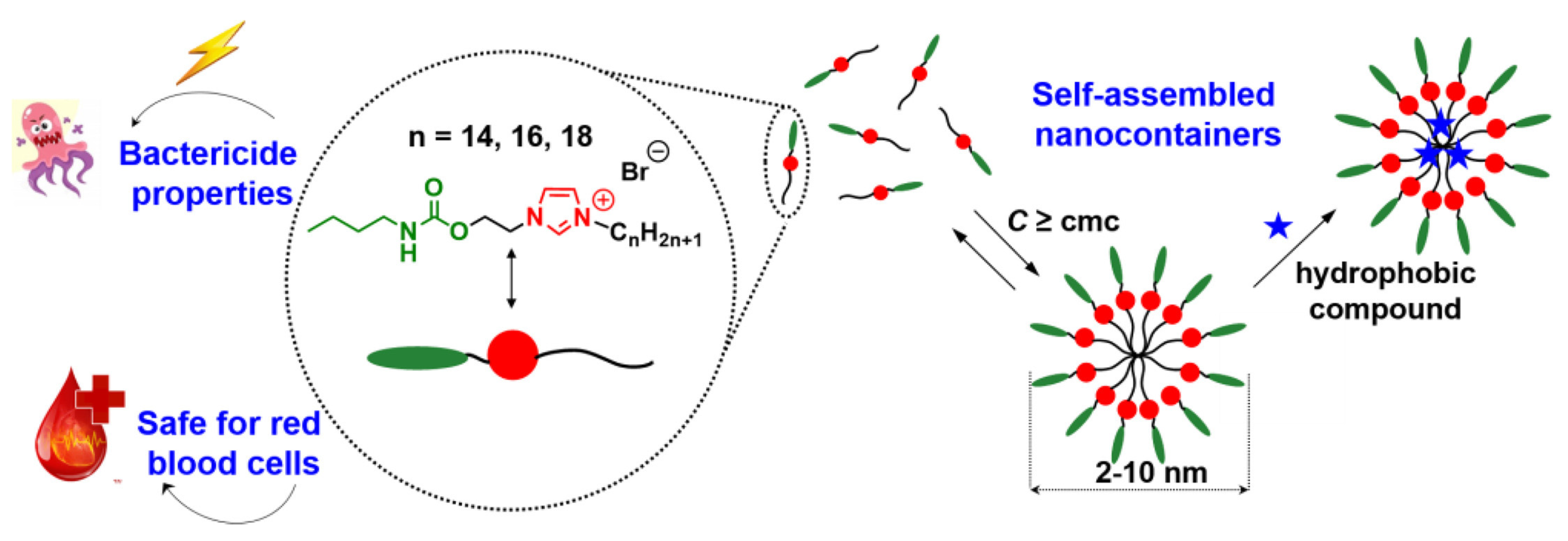
- Kuznetsova, D.A.; Gabdrakhmanov, D.R.; Kuznetsov, D.M.; Lukashenko, S.S.; Sapunova, A.S.; Voloshina, A.D.; Nizameev, I.R.; Kadirov, M.K.; Zakharova, L.Y. Biocompatible supramolecular systems based on novel cationic imidazolium- and urethane-containing amphiphiles: Self-assembly and antimicrobial properties. J. Mol. Liq. 2020, 319, 114094. [Google Scholar] [CrossRef]
- Kashapov, R.; Gaynanova, G.; Gabdrakhmanov, D.; Kuznetsov, D.; Pavlov, R.; Petrov, K.; Zakharova, L.; Sinyashin, O. Self-assembly of amphiphilic compounds as a versatile tool for construction of nanoscale drug carriers. Int. J. Mol. Sci. 2020, 21, 6961. [Google Scholar] [CrossRef]
- Zakharova, L.Y.; Pashirova, T.N.; Doktorovova, S.; Fernandes, A.R.; Sanchez-Lopez, E.; Silva, A.M.; Souto, E.B. Cationic surfactants: Self-assembly, structure-activity correlation and their biological applications. Int. J. Mol. Sci. 2019, 20, 5534. [Google Scholar] [CrossRef]
- Pashirova, T.N.; Zueva, I.V.; Petrov, K.A.; Babaev, V.M.; Lukashenko, S.S.; Rizvanov, I.K.; Souto, E.B.; Nikolsky, E.E.; Zakharova, L.Y.; Masson, P.; et al. Nanoparticle-delivered 2-PAM for rat brain protection against paraoxon central toxicity. ACS Appl. Mater. Interfaces 2017, 9, 16922–16932. [Google Scholar] [CrossRef]
- Pavlov, R.V.; Gaynanova, G.A.; Kuznetsova, D.A.; Vasileva, L.A.; Zueva, I.V.; Sapunova, A.S.; Buzyurova, D.N.; Babaev, V.M.; Voloshina, A.D.; Lukashenko, S.S.; et al. Biomedical potentialities of cationic geminis as modulating agents of liposome in drug delivery across biological barriers and cellular uptake. Int. J. Pharm. 2020, 587, 119640. [Google Scholar] [CrossRef] [PubMed]
- Le Guenic, S.; Chaveriat, L.; Lequart, V.; Joly, N.; Martin, P. Renewable surfactants for biochemical applications and nanotechnology. J. Surfactants Deterg. 2019, 22, 5–21. [Google Scholar] [CrossRef]
- Atta, D.Y.; Negash, B.M.; Yekeen, N.; Habte, A.D. A state-of-the-art review on the application of natural surfactants in enhanced oil recovery. J. Mol. Liq. 2021, 321, 114888. [Google Scholar] [CrossRef]
- Moldes, A.B.; Rodríguez-López, L.; Rincón-Fontán, M.; López-Prieto, A.; Vecino, X.; Cruz, J.M. Synthetic and bio-derived surfactants versus microbial biosurfactants in the cosmetic industry: An overview. Int. J. Mol. Sci. 2021, 22, 2371. [Google Scholar] [CrossRef]
- Antipin, I.S.; Alfimov, M.V.; Arslanov, V.V.; Burilov, V.A.; Vatsadze, S.Z.; Voloshin, Y.Z.; Volcho, K.P.; Gorbatchuk, V.V.; Gorbunova, Y.G.; Gromov, S.P.; et al. Functional supramolecular systems: Design and applications. Russ. Chem. Rev. 2021, 90, 895–1107. [Google Scholar] [CrossRef]
- Limeres, M.J.; Suñé-Pou, M.; Prieto-Sánchez, S.; Moreno-Castro, C.; Nusblat, A.D.; Hernández-Munain, C.; Castro, G.R.; Suñé, C.; Suñé-Negre, J.M.; Cuetsas, M.L. Development and characterization of an improved formulation of cholesteryl oleate-loaded cationic solid-lipid nanoparticles as an efficient non-viral gene delivery system. Colloids Surf. B 2019, 184, 110533. [Google Scholar] [CrossRef]
- Burilova, E.A.; Pashirova, T.N.; Zueva, I.V.; Gibadullina, E.M.; Lushchekina, S.V.; Sapunova, A.S.; Kayumova, R.M.; Rogov, A.M.; Evtjugin, V.G.; Sudakov, I.A.; et al. Bi-functional sterically hindered phenol lipid-based delivery systems as potential multi-target agents against alzheimer’s disease: Via an intranasal route. Nanoscale 2020, 12, 13757–13770. [Google Scholar] [CrossRef] [PubMed]
- Valeeva, F.G.; Karimova, T.R.; Pavlov, R.V.; Bakhtiyarov, D.I.; Sapunova, A.S.; Ivshin, K.A.; Kataeva, O.N.; Gaynanova, G.A.; Syakaev, V.V.; Voloshina, A.D.; et al. Introduction of isothiuronium surfactant series: Synthesis, structure-dependent aggregation overview and biological activity. J. Mol. Liq. 2021, 324, 114721. [Google Scholar] [CrossRef]
- Kuznetsova, D.A.; Gabdrakhmanov, D.R.; Gaynanova, G.A.; Vasileva, L.A.; Kuznetsov, D.M.; Lukashenko, S.S.; Voloshina, A.D.; Sapunova, A.S.; Nizameev, I.R.; Sibgatullina, G.V.; et al. Novel biocompatible liposomal formulations for encapsulation of hydrophilic drugs—Chloramphenicol and cisplatin. Colloids Surf. A 2021, 610, 125673. [Google Scholar] [CrossRef]
- Osorno, L.L.; Brandley, A.N.; Maldonado, D.E.; Yiantsos, A.; Mosley, R.J.; Byrne, M.E. Review of contemporary self-assembled systems for the controlled delivery of therapeutics in medicine. Nanomaterials 2021, 11, 278. [Google Scholar] [CrossRef] [PubMed]
- Lam, H.T.; Le-Vinh, B.; Phan, T.N.Q.; Bernkop-Schnürch, A. Self-emulsifying drug delivery systems and cationic surfactants: Do they potentiate each other in cytotoxicity? J. Pharm. Pharmacol. 2019, 71, 156–166. [Google Scholar] [CrossRef]
- Mirgorodskaya, A.B.; Kushnazarova, R.A.; Lukashenko, S.S.; Zakharova, L.Y. Self-assembly of mixed systems based on nonionic and carbamate-bearing cationic surfactants as a tool for fabrication of biocompatible nanocontainers. J. Mol. Liq. 2019, 292, 111407. [Google Scholar] [CrossRef]
- Kashapov, R.; Ibragimova, A.; Pavlov, R.; Gabdrakhmanov, D.; Kashapova, N.; Burilova, E.; Zakharova, L.; Sinyashin, O. Nanocarriers for biomedicine: From lipid formulations to inorganic and hybrid nanoparticles. Int. J. Mol. Sci. 2021, 22, 7055. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, S.; Rakshit, A.; Acharjee, A.; Saha, B. Biodegradability and biocompatibility: Advancements in synthetic surfactants. J. Mol. Liq. 2021, 324, 115105. [Google Scholar] [CrossRef]
- Blessy, M.; Patel, R.D.; Prajapati, P.N.; Agrawal, Y.K. Development of forced degradation and stability indicating studies of drugs—A review. J. Pharm. Anal. 2014, 4, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Perrigue, P.M.; Murray, R.A.; Mielcarek, A.; Henschke, A.; Moya, S.E. Degradation of drug delivery nanocarriers and payload release: A review of physical methods for tracing nanocarrier biological fate. Pharmaceutics 2021, 13, 770. [Google Scholar] [CrossRef] [PubMed]
- Larson, N.R.; Wei, Y.; Prajapati, I.; Chakraborty, A.; Peters, B.; Kalonia, C.; Hudak, S.; Choudhary, S.; Esfandiary, R.; Dhar, P.; et al. Comparison of polysorbate 80 hydrolysis and oxidation on the aggregation of a monoclonal antibody. J. Pharm. Sci. 2020, 109, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Lou, J.; Best, M.D. Strategies for altering lipid self-assembly to trigger liposome cargo release. Chem. Phys. Lipids 2020, 232, 104966. [Google Scholar] [CrossRef] [PubMed]
- Wu, W.; Luo, L.; Wang, Y.; Wu, Q.; Dai, H.B.; Li, J.S.; Durkan, C.; Wang, N.; Wang, G.X. Endogenous pH-responsive nanoparticles with programmable size changes for targeted tumor therapy and imaging applications. Theranostics 2018, 8, 3038–3058. [Google Scholar] [CrossRef] [PubMed]
- Mukherjee, S.; Mehta, D.; Dhangar, K.; Kumar, M. Environmental fate, distribution and state-of-the-art removal of antineoplastic drugs: A comprehensive insight. Chem. Eng. J. 2021, 407, 127184. [Google Scholar] [CrossRef]
- Tahri, N.; Bahafid, W.; Sayel, H.; El Ghachtouli, N. Biodegradation: Involved Microorganisms and Genetically Engineered Microorganisms. In Biodegradation—Life of Science; Chamy, R., Rosenkranz, F., Eds.; IntechOpen: London, UK, 2013; Volume 1, pp. 289–320. [Google Scholar] [CrossRef]
- Tiecco, M.; Alonso, D.A.; Ñíguez, D.R.; Ciancaleoni, G.; Guillena, G.; Ramón, D.J.; Bonillo, A.A.; Germani, R. Assessment of the organocatalytic activity of chiral L-proline-based deep eutectic solvents based on their structural features. J. Mol. Liq. 2020, 313, 113573. [Google Scholar] [CrossRef]
- Scott, M.J.; Jones, M.N. The biodegradation of surfactants in the environment. Biochim. Biophys. Acta Biomembr. 2000, 1508, 235–251. [Google Scholar] [CrossRef]
- Brown, D. Introduction to surfactant biodegradation. In Biodegradability of Surfactants; Karsa, D.R., Porter, M.R., Eds.; Springer: Cham, Switzerland, 1995; pp. 1–27. [Google Scholar] [CrossRef]
- Tehrani-Bagha, A.R.; Oskarsson, H.; van Ginkel, C.G.; Holmberg, K. Cationic ester-containing gemini surfactants: Chemical hydrolysis and biodegradation. J. Colloid Interface Sci. 2007, 312, 444–452. [Google Scholar] [CrossRef] [PubMed]
- Tehrani-Bagha, A.R.; Holmberg, K.; van Ginkel, C.G.; Kean, M. Cationic gemini surfactants with cleavable spacer: Chemical hydrolysis, biodegradation, and toxicity. J. Colloid Interface Sci. 2014, 449, 72–79. [Google Scholar] [CrossRef] [PubMed]
- Brovč, E.V.; Mravljak, J.; Šink, R.; Pajk, S. Degradation of polysorbates 20 and 80 catalysed by histidine chloride buffer. Eur. J. Pharm. Biopharm. 2020, 154, 236–245. [Google Scholar] [CrossRef]
- Stjerndahl, M.; Lundberg, D.; Chauhan, V.; Bordes, R.; Holmberg, K. Cleavable surfactants: A comparison between ester, amide, and carbonate as the weak bond. J. Surfactants Deterg. 2019, 22, 1139–1145. [Google Scholar] [CrossRef]
- Chauhan, V.; Holmberg, K.; Bordes, R. A reverse degradation vs. temperature relationship for a carbonate-containing gemini surfactant. J. Colloid Interface Sci. 2018, 531, 189–193. [Google Scholar] [CrossRef]
- Petrović, M.; Barceló, D. Determination of anionic and nonionic surfactants, their degradation products, and endocrine-disrupting compounds in sewage sludge by liquid chromatography/mass spectrometry. Anal. Chem. 2000, 72, 4560–4567. [Google Scholar] [CrossRef] [PubMed]
- Pisárčik, M.; Polakovičová, M.; Markuliak, M.; Lukáč, M.; Devínsky, F. Self-assembly properties of cationic gemini surfactants with biodegradable groups in the spacer. Molecules 2019, 24, 1481. [Google Scholar] [CrossRef] [PubMed]
- Kuznetsova, D.A.; Gabdrakhmanov, D.R.; Ahtamyanova, L.R.; Lukashenko, S.S.; Kusova, A.M.; Zuev, Y.F.; Voloshina, A.D.; Sapunova, A.S.; Kulik, N.V.; Kuznetsov, D.M.; et al. Novel self-assembling systems based on imidazolium amphiphiles with cleavable urethane fragment for construction of soft nanocontainers for biomedicine application. J. Mol. Liq. 2020, 298, 111961. [Google Scholar] [CrossRef]
- Shen, J.; Bai, Y.; Yin, Q.; Wang, W.; Ma, X.; Wang, G. Adsorption, aggregation and wetting behaviors of biodegradable surfactant: Perfluoropolyether quaternary ammonium salt. J. Ind. Eng. Chem. 2017, 56, 82–89. [Google Scholar] [CrossRef]
- Wu, Q.; Zhao, L.; Song, R.; Ma, A. Research progress of surfactant biodegradation. IOP Conf. Ser. Earth Environ. Sci. 2019, 227, 052023. [Google Scholar] [CrossRef]
- Muhammad, M.T.; Khan, M.N. Eco-friendly, biodegradable natural surfactant (Acacia Concinna): An alternative to the synthetic surfactants. J. Clean. Prod. 2018, 188, 678–685. [Google Scholar] [CrossRef]
- Gawali, I.T.; Usmani, G.A. Synthesis, surface active properties and applications of cationic gemini surfactants from triethylenetetramine. J. Dispers. Sci. Technol. 2020, 41, 450–460. [Google Scholar] [CrossRef]
- García, M.T.; Ribosa, I.; Kowalczyk, I.; Pakiet, M.; Brycki, B. Biodegradability and aquatic toxicity of new cleavable betainate cationic oligomeric surfactants. J. Hazard. Mater. 2019, 371, 108–114. [Google Scholar] [CrossRef]
- Ghosh, R.; Dey, J.; Kumar, B.V.N.P. Thermodynamically stable vesicle formation of biodegradable double mPEG-tailed amphiphiles with sulfonate head group. RSC Adv. 2020, 10, 32522–32531. [Google Scholar] [CrossRef]
- Umapathy, M.J.; Lakshimi Narayanan, V.; Magesan, P.; Chiranjeevi, P.; Jemima, S.W. Synthesis and characterization of biodegradable cationic esterquat surfactants and the evaluation of its physico-chemical properties. Tenside Surfact. Det. 2016, 53, 249–258. [Google Scholar] [CrossRef]
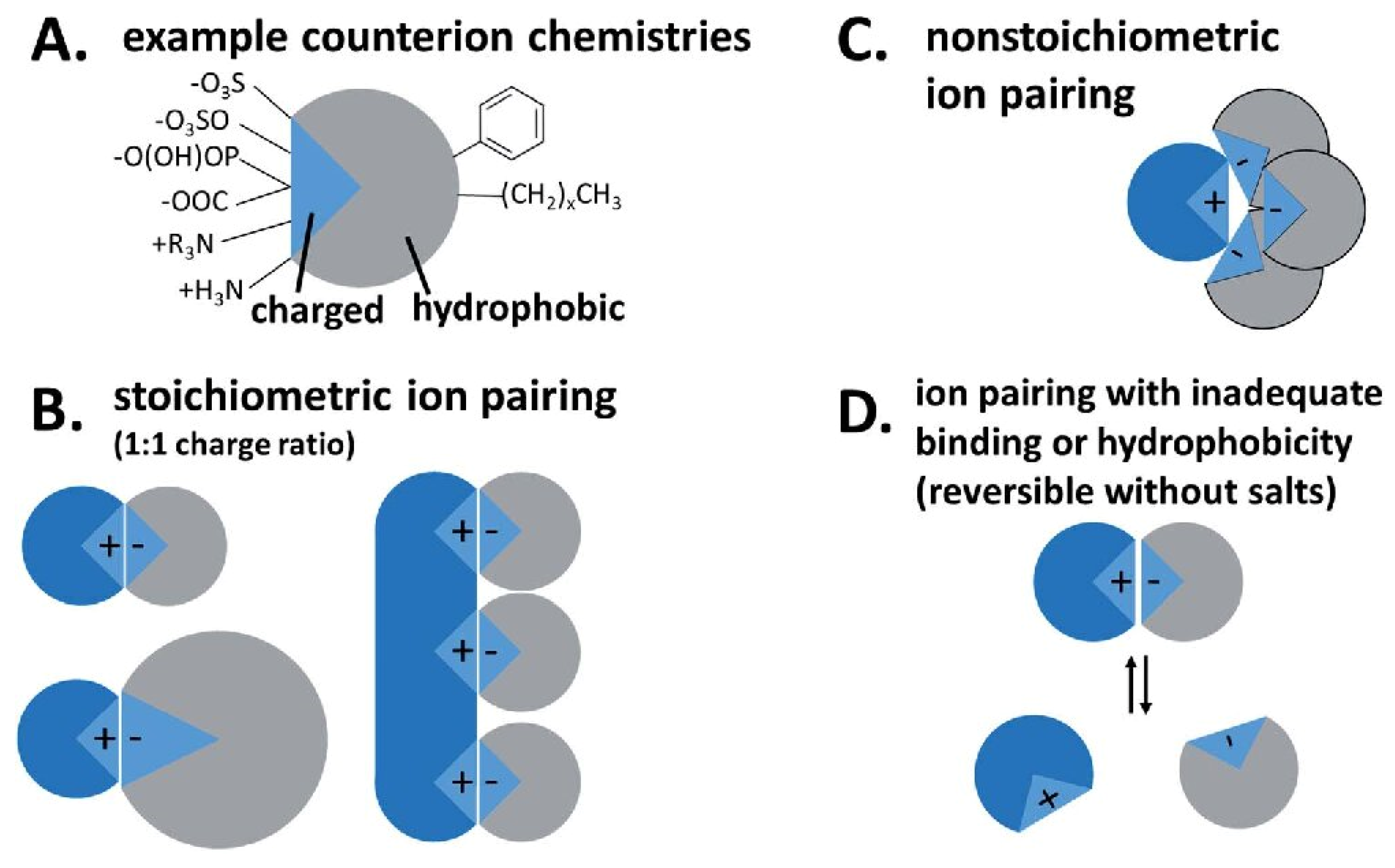
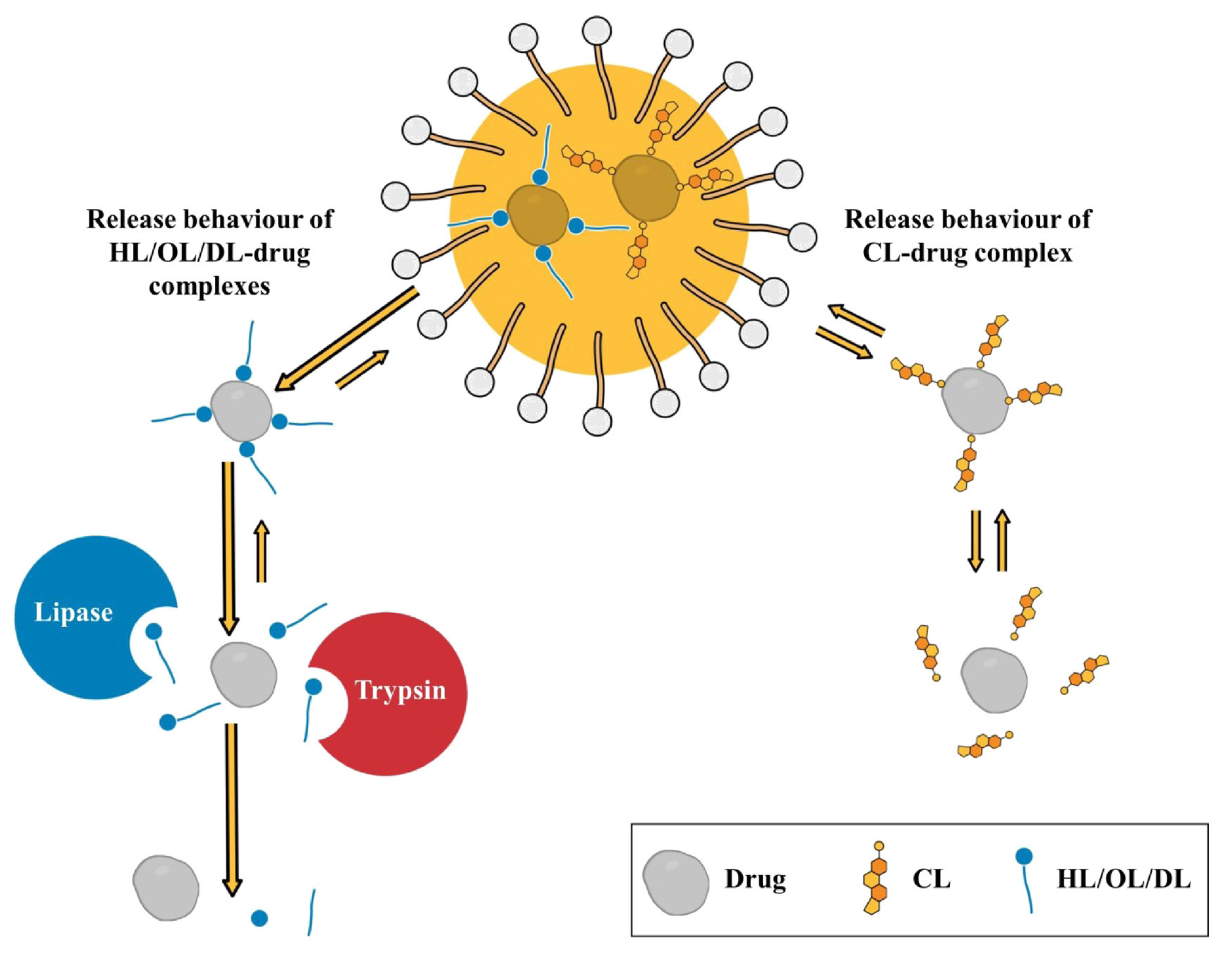
- Kurpiers, M.; Wolf, J.D.; Spleis, H.; Steinbring, C.; Jörgensen, A.M.; Matuszczak, B.; Bernkop-Schnürch, A. Lysine-based biodegradable surfactants: Increasing the lipophilicity of insulin by hydrophobic ion paring. J. Pharm. Sci. 2021, 110, 124–134. [Google Scholar] [CrossRef]
- Wolf, J.D.; Kurpiers, M.; Baus, R.A.; Götz, R.X.; Griesser, J.; Matuszczak, B.; Bernkop-Schnürch, A. Characterization of an amino acid based biodegradable surfactant facilitating the incorporation of DNA into lipophilic delivery systems. J. Colloid Interface Sci. 2020, 566, 234–241. [Google Scholar] [CrossRef]
- Shahzadi, I.; Asim, M.H.; Dizdarević, A.; Wolf, J.D.; Kurpiers, M.; Matuszczak, B.; Bernkop-Schnürch, A. Arginine-based cationic surfactants: Biodegradable auxiliary agents for the formation of hydrophobic ion pairs with hydrophilic macromolecular drugs. J. Colloid Interface Sci. 2019, 552, 287–294. [Google Scholar] [CrossRef]
- Wang, Y.; Jiang, Y.; Geng, T.; Ju, H.; Duan, S. Synthesis, surface/interfacial properties, and biological activity of amide-based Gemini cationic surfactants with hydroxyl in the spacer group. Colloids Surf. A 2019, 563, 1–10. [Google Scholar] [CrossRef]
- Singh, A.; Tyagi, V.K. Arginine based novel cationic surfactants: A. review. Tenside Surfact. Det. 2014, 51, 202–213. [Google Scholar] [CrossRef]
- Nogueira, D.R.; Mitjans, M.; Moran, M.C.; Pérez, L.; Vinardell, M.P. Membrane-destabilizing activity of pH-responsive cationic lysine-based surfactants: Role of charge position and alkyl chain length. Amino Acids 2012, 43, 1203–1215. [Google Scholar] [CrossRef]
- Nogueira, D.R.; Scheeren, L.E.; Pilar Vinardell, M.; Mitjans, M.; Rosa Infante, M.; Rolim, C.M.B. Nanoparticles incorporating pH-responsive surfactants as a viable approach to improve the intracellular drug delivery. Mater. Sci. Eng. C 2015, 57, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Zhang, N.; Qi, R.; Li, H.; Guan, B.; Liu, Y.; Han, Y.; Wang, Y. Interaction of phospholipid vesicles with gemini surfactants of different lysine spacer lengths. Soft Matter 2019, 15, 9458–9467. [Google Scholar] [CrossRef]
- Ménard, N.; Tsapis, N.; Poirier, C.; Arnauld, T.; Moine, L.; Lefoulon, F.; Péan, J.M.; Fattal, E. Drug solubilization and in vitro toxicity evaluation of lipoamino acid surfactants. Int. J. Pharm. 2012, 423, 312–320. [Google Scholar] [CrossRef]
- Bračič, M.; Pérez, L.; Martinez-Pardo, R.I.; Kogej, K.; Hribernik, S.; Šauperl, O.; Fras Zemljič, L. A novel synergistic formulation between a cationic surfactant from lysine and hyaluronic acid as an antimicrobial coating for advanced cellulose materials. Cellulose 2014, 21, 2647–2663. [Google Scholar] [CrossRef]
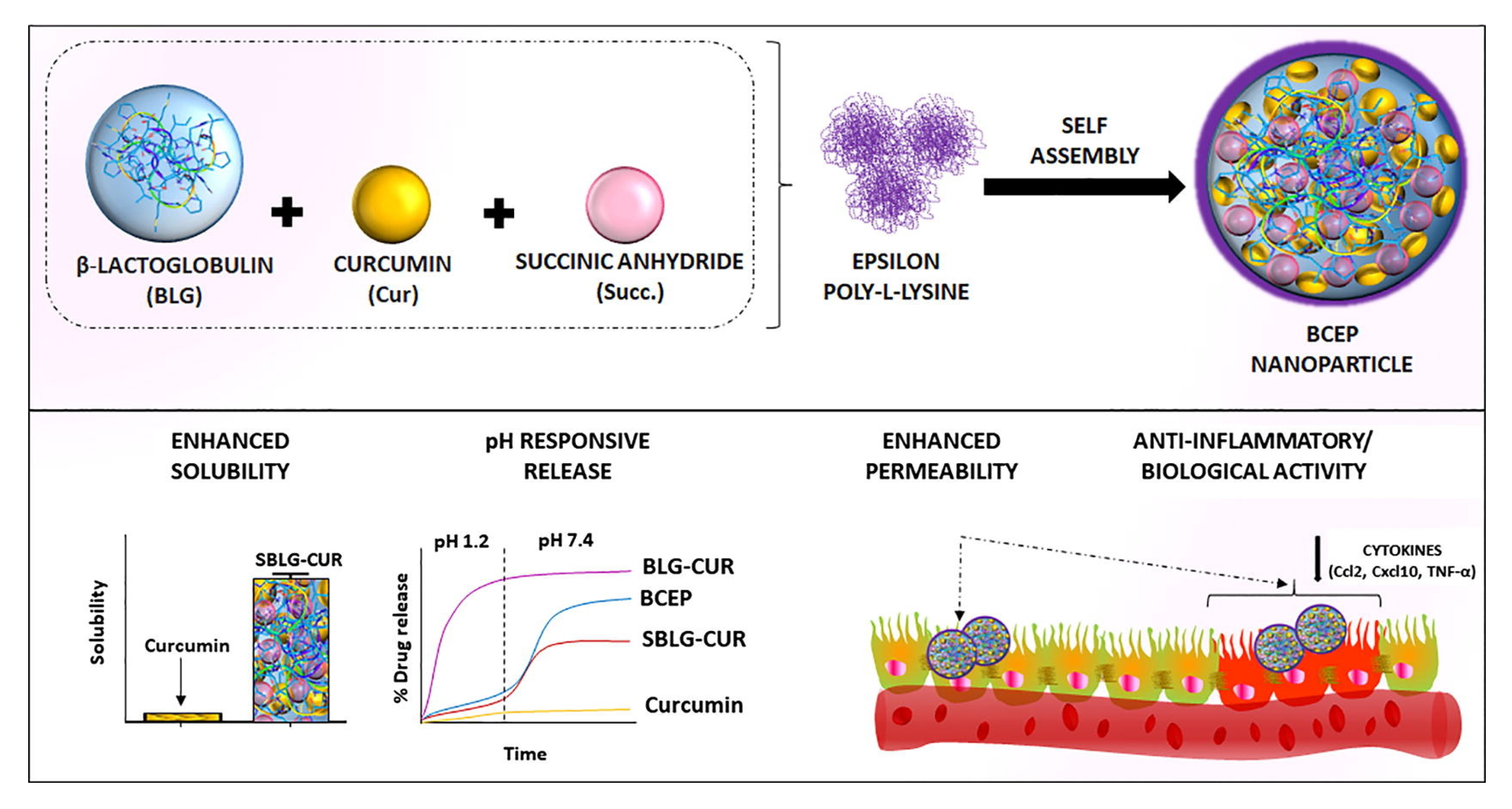
- Pujara, N.; Giri, R.; Wong, K.Y.; Qu, Z.; Rewatkar, P.; Moniruzzaman, M.; Begun, J.; Ross, B.P.; McGuckin, M.; Popat, A. pH—Responsive colloidal carriers assembled from β-lactoglobulin and Epsilon poly-L-lysine for oral drug delivery. J. Colloid Interface Sci. 2021, 589, 45–55. [Google Scholar] [CrossRef]
- Ristroph, K.D.; Prud’homme, R.K. Hydrophobic ion pairing: Encapsulating small molecules, peptides, and proteins into nanocarriers. Nanoscale Adv. 2019, 1, 4207–4237. [Google Scholar] [CrossRef]
- Griesser, J.; Hetényi, G.; Moser, M.; Demarne, F.; Jannin, V.; Bernkop-Schnürch, A. Hydrophobic ion pairing: Key to highly payloaded self-emulsifying peptide drug delivery systems. Int. J. Pharm. 2017, 520, 267–274. [Google Scholar] [CrossRef]
- Lundquist, P.; Artursson, P. Oral absorption of peptides and nanoparticles across the human intestine: Opportunities, limitations and studies in human tissues. Adv. Drug Deliv. Rev. 2016, 106, 256–276. [Google Scholar] [CrossRef]
- Tavano, L.; Pinazo, A.; Abo-Riya, M.; Infante, M.R.; Manresa, M.A.; Muzzalupo, R.; Pérez, L. Cationic vesicles based on biocompatible diacyl glycerol-arginine surfactants: Physicochemical properties, antimicrobial activity, encapsulation efficiency and drug release. Colloids Surf. B 2014, 120, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Pinazo, A.; Manresa, M.A.; Marques, A.M.; Bustelo, M.; Espuny, M.J.; Pérez, L. Amino acid-based surfactants: New antimicrobial agents. Adv. Colloid Interface 2016, 228, 17–39. [Google Scholar] [CrossRef] [PubMed]
- Pashirova, T.N.; Zhukova, N.A.; Lukashenko, S.S.; Valeeva, F.G.; Burilova, E.A.; Sapunova, A.S.; Voloshina, A.D.; Mirgorodskaya, A.B.; Zakharova, L.Y.; Sinyashin, O.G.; et al. Multi-targeted approach by 2-benzimidazolylquinoxalines-loaded cationic arginine liposomes against cervical cancer cells in vitro. Colloids Surf. B 2019, 178, 317–328. [Google Scholar] [CrossRef]
- Rosa, M.; Penacho, N.; Simões, S.; Lima, M.C.P.; Lindman, B.; Miguel, M.G. DNA pre-condensation with an amino acid-based cationic amphiphile. a viable approach for liposome-based gene delivery. Mol. Membr. Biol. 2008, 25, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Fait, M.E.; Hermet, M.; Comelles, F.; Clapés, P.; Alvarez, H.A.; Prieto, E.; Herlax, V.; Morcelle, S.R.; Bakás, L. Microvesicle release and micellar attack as the alternative mechanisms involved in the red-blood-cell-membrane solubilization induced by arginine-based surfactants. RSC Adv. 2017, 7, 37549–37558. [Google Scholar] [CrossRef]
- Branco, M.A.; Pinheiro, L.; Faustino, C. Amino acid-based cationic gemini surfactant-protein interactions. Colloids Surf. A 2015, 480, 105–112. [Google Scholar] [CrossRef]
- Faustino, C.; Serafim, C.; Ferreira, I.; Pinheiro, L.; Calado, A. Solubilization power of an amino acid-based gemini surfactant towards the hydrophobic drug amphotericin B. Colloids Surf. A 2015, 480, 426–432. [Google Scholar] [CrossRef]
- Serafim, C.; Ferreira, I.; Rijo, P.; Pinheiro, L.; Faustino, C.; Calado, A.; Garcia-Rio, L. Lipoamino acid-based micelles as promising delivery vehicles for monomeric amphotericin B. Int. J. Pharm. 2016, 497, 23–35. [Google Scholar] [CrossRef]
- Wu, J.; Gao, H.; Shi, D.; Yang, Y.; Zhang, Y.; Zhu, W. Cationic gemini surfactants containing both amide and ester groups: Synthesis, surface properties and antibacterial activity. J. Mol. Liq. 2020, 299, 112248. [Google Scholar] [CrossRef]
- Wang, Y.; Deng, M.; Tang, Y.; Han, Y.; Huang, X.; Hou, Y.; Wang, Y. Aggregation of biodegradable cationic gemini surfactants with amide or ester groups. Acta Phys. Chim. Sin. 2020, 36, 1909046. [Google Scholar] [CrossRef]
- Liu, D.; Yang, X.; Liu, P.; Mao, T.; Shang, X.; Wang, L. Synthesis and characterization of gemini ester surfactant and its application in efficient fabric softening. J. Mol. Liq. 2020, 299, 112236. [Google Scholar] [CrossRef]
- Tehrani-Bagha, A.R.; Singh, R.G.; Holmberg, K. Solubilization of two organic dyes by cationic ester-containing gemini surfactants. J. Colloid Interface Sci. 2012, 376, 112–118. [Google Scholar] [CrossRef] [PubMed]
- Lundberg, D.; Ljusberg-Wahren, H.; Norlin, A.; Holmberg, K. Studies on dodecyl betainate in combination with its degradation products or with phosphatidyl choline-phase behavior and hemolytic activity. J. Colloid Interface. Sci. 2004, 278, 478–487. [Google Scholar] [CrossRef] [PubMed]
- Banno, T.; Kawada, K.; Matsumura, S. Creation of novel green and sustainable gemini-type cationics containing carbonate linkages. J. Surfactants Deterg. 2010, 13, 387–398. [Google Scholar] [CrossRef]
- Banno, T.; Toshima, K.; Kawada, K.; Matsumura, S. Synthesis and properties of gemini-type cationic surfactants containing carbonate linkages in the linker moiety directed toward green and sustainable chemistry. J. Surfactants Deterg. 2009, 12, 249–259. [Google Scholar] [CrossRef]
- Mirgorodskaya, A.B.; Kushnazarova, R.A.; Lukashenko, S.S.; Voloshina, A.D.; Lenina, O.A.; Zakharova, L.Y.; Sinyashin, O.G. Carbamate-bearing surfactants: Micellization, solubilization, and biological activity. J. Mol. Liq. 2018, 269, 203–210. [Google Scholar] [CrossRef]
- Kushnazarova, R.A.; Mirgorodskaya, A.B.; Lukashenko, S.S.; Voloshina, A.D.; Sapunova, A.S.; Nizameev, I.R.; Kadirov, M.K.; Zakharova, L.Y. Novel cationic surfactants with cleavable carbamate fragment: Tunable morphological behavior, solubilization of hydrophobic drugs and cellular uptake study. J. Mol. Liq. 2020, 318, 113894. [Google Scholar] [CrossRef]
- Mirgorodskaya, A.B.; Kushnazarova, R.; Lukashenko, S.S.; Nikitin, E.N.; Sinyashin, K.O.; Nesterova, L.M.; Zakharova, L.Y. Carbamate-bearing surfactants as effective adjuvants promoted the penetration of the herbicide into the plant. Colloids Surf. A 2020, 586, 124252. [Google Scholar] [CrossRef]
- Kuznetsova, D.A.; Gabdrakhmanov, D.R.; Lukashenko, S.S.; Faizullin, D.A.; Zuev, Y.F.; Nizameev, I.R.; Kadirov, M.K.; Kuznetsov, D.M.; Zakharova, L.Y. Interaction of bovine serum albumin with cationic imidazolium-containing amphiphiles bearing urethane fragment: Effect of hydrophobic tail length. J. Mol. Liq. 2020, 307, 113001. [Google Scholar] [CrossRef]
- Samarkina, D.A.; Gabdrakhmanov, D.R.; Lukashenko, S.S.; Khamatgalimov, A.R.; Kovalenko, V.I.; Zakharova, L.Y. Cationic amphiphiles bearing imidazole fragment: From aggregation properties to potential in biotechnologies. Colloids Surf. A 2017, 529, 990–997. [Google Scholar] [CrossRef]
- Kuznetsova, D.A.; Gabdrakhmanov, D.R.; Lukashenko, S.S.; Voloshina, A.D.; Sapunova, A.S.; Kulik, N.V.; Nizameev, I.R.; Kadirov, M.K.; Kashapov, R.R.; Zakharova, L.Y. Supramolecular systems based on cationic imidazole-containing amphiphiles bearing hydroxyethyl fragment: Aggregation properties and functional activity. J. Mol. Liq. 2019, 289, 111058. [Google Scholar] [CrossRef]
- Kuznetsova, D.A.; Gabdrakhmanov, D.R.; Kuznetsov, D.M.; Lukashenko, S.S.; Zakharov, V.M.; Sapunova, A.S.; Amerhanova, S.K.; Lyubina, A.P.; Voloshina, A.D.; Salakhieva, D.V.; et al. Polymer–colloid complexes based on cationic imidazolium amphiphile, polyacrylic acid and DNA decamer. Molecules 2021, 26, 2363. [Google Scholar] [CrossRef] [PubMed]
- Saal, W.; Wyttenbach, N.; Alsenz, J.; Kuentz, M. The quest for exceptional drug solubilization in diluted surfactant solutions and consideration of residual solid state. Eur. J. Pharm. Sci. 2018, 111, 96–103. [Google Scholar] [CrossRef]
- Vinarov, Z.; Gancheva, G.; Burdzhiev, N.; Tcholakova, S. Solubilization of itraconazole by surfactants and phospholipid-surfactant mixtures: Interplay of amphiphile structure, pH and electrostatic interactions. J. Drug Deliv. Sci. Technol. 2020, 57, 101688. [Google Scholar] [CrossRef]
- Mirgorodskaya, A.B.; Kuznetsova, D.A.; Kushnazarova, R.A.; Gabdrakhmanov, D.R.; Zhukova, N.A.; Lukashenko, S.S.; Sapunova, A.S.; Voloshina, A.D.; Sinyashin, O.G.; Mamedov, V.A.; et al. Soft nanocarriers for new poorly soluble conjugate of pteridine and benzimidazole: Synthesis and cytotoxic activity against tumor cells. J. Mol. Liq. 2020, 317, 114007. [Google Scholar] [CrossRef]
- Moshikur, R.M.; Ali, M.K.; Moniruzzaman, M.; Goto, M. Recent advances in surface-active ionic liquid-assisted self-assembly systems for drug delivery. Curr. Opin. Colloid Interface Sci. 2021, 56, 101515. [Google Scholar] [CrossRef]
- Javadian, S.; Kakemam, J. Intermicellar interaction in surfactant solutions; a review study. J. Mol. Liq. 2017, 242, 115–128. [Google Scholar] [CrossRef]
- Torchilin, V.P. Structure and design of polymeric surfactant-based drug delivery systems. J. Control. Release 2001, 73, 137–172. [Google Scholar] [CrossRef]
- Ghezzi, M.; Pescina, S.; Padula, C.; Santi, P.; Del Favero, E.; Cantù, L.; Nicoli, S. Polymeric micelles in drug delivery: An insight of the techniques for their characterization and assessment in biorelevant conditions. J. Control. Release 2021, 332, 312–336. [Google Scholar] [CrossRef] [PubMed]
- Beltrán-Gracia, E.; López-Camacho, A.; Higuera-Ciapara, I.; Velázquez-Fernández, J.B.; Vallejo-Cardona, A.A. Nanomedicine review: Clinical developments in liposomal applications. Cancer Nanotechnol. 2019, 10, 11. [Google Scholar] [CrossRef]
- Zakharova, L.Y.; Ibragimova, A.R.; Vasilieva, E.A.; Mirgorodskaya, A.B.; Yackevich, E.I.; Nizameev, I.R.; Kadirov, M.K.; Zuev, Y.F.; Konovalov, A.I. Polyelectrolyte capsules with tunable shell behavior fabricated by the simple layer-by-layer technique for the control of the release and reactivity of small guests. J. Phys. Chem. C 2012, 116, 18865–18872. [Google Scholar] [CrossRef]
- Mirgorodskaya, A.B.; Kushnazarova, R.A.; Nikitina, A.V.; Semina, I.I.; Nizameev, I.R.; Kadirov, M.K.; Khutoryanskiy, V.V.; Zakharova, L.Y.; Sinyashin, O.G. Polyelectrolyte nanocontainers: Controlled binding and release of indomethacin. J. Mol. Liq. 2018, 272, 982–989. [Google Scholar] [CrossRef]
- Zakharova, L.Y.; Vasilieva, E.A.; Gaynanova, G.A.; Mirgorodskaya, A.B.; Ibragimova, A.R.; Salnikov, V.V.; Uchegbu, I.F.; Konovalov, A.I.; Zuev, Y.F. The polyacrylic acid/modified chitosan capsules with tunable release of small hydrophobic probe and drug. Colloids Surf. A 2015, 471, 93–100. [Google Scholar] [CrossRef]
- Vasilieva, E.A.; Ibragimova, A.R.; Mirgorodskaya, A.B.; Yackevich, E.I.; Dobrynin, A.B.; Nizameev, I.R.; Kadirov, M.K.; Zakharova, L.Y.; Zuev, Y.F.; Konovalov, A.I. Polyelectrolyte micro- and nanocapsules with varied shell permeability controlling the rate of esters hydrolysis. Russ. Chem. Bull. 2014, 63, 232–238. [Google Scholar] [CrossRef]
- Tetro, N.; Moushaev, S.; Rubinchik-Stern, M.; Eyal, S. The placental barrier: The gate and the fate in drug distribution. Pharm. Res. 2018, 35, 71. [Google Scholar] [CrossRef]
- Pradhan-Sundd, T.; Monga, S.P. Blood-bile barrier: Morphology, regulation, and pathophysiology. Gene Expr. 2019, 19, 69–87. [Google Scholar] [CrossRef] [PubMed]
- Naidu, E.C.S.; Olojede, S.O.; Lawal, S.K.; Rennie, C.O.; Azu, O.O. Nanoparticle delivery system, highly active antiretroviral therapy, and testicular morphology: The role of stereology. Pharmacol. Res. Perspect. 2021, 9, e00776. [Google Scholar] [CrossRef]
- Yan Cheng, C.; Mruk, D.D. The blood-testis barrier and its implications for male contraception. Pharmacol. Rev. 2012, 64, 16–64. [Google Scholar] [CrossRef]
- Hawkins, B.T.; Davis, T.P. The blood-brain barrier/neurovascular unit in health and disease. Pharmacol. Rev. 2005, 57, 173–185. [Google Scholar] [CrossRef]
- Johanson, C. Choroid plexus blood-CSF barrier: Major player in brain disease modeling and neuromedicine. J. Neurol. Neuromed. 2018, 3, 39–58. [Google Scholar] [CrossRef]
- Cunha-Vaz, J. The blood-ocular barriers. Surv. Ophthalmol. 1979, 23, 279–296. [Google Scholar] [CrossRef]
- Elmowafy, M. Skin penetration/permeation success determinants of nanocarriers: Pursuit of a perfect formulation. Colloids Surf. B 2021, 203, 111748. [Google Scholar] [CrossRef]
- Uchida, N.; Yanagi, M.; Hamada, H. Physical enhancement? Nanocarrier? Current progress in transdermal drug delivery. Nanomaterials 2021, 11, 335. [Google Scholar] [CrossRef]
- Patel, D.; Patel, B.; Thakkar, H. Lipid based nanocarriers: Promising drug delivery system for topical application. Eur. J. Lipid Sci. Technol. 2021, 123, 2000264. [Google Scholar] [CrossRef]
- Yang, R.; Wei, T.; Goldberg, H.; Wang, W.; Cullion, K.; Kohane, D.S. Getting drugs across biological barriers. Adv. Mater. 2017, 29, 1606596. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.Y.; Dao, H. Physiology, Integument. Available online: https://www.ncbi.nlm.nih.gov/books/NBK554386/ (accessed on 9 May 2021).
- Brown, T.M.; Krishnamurthy, K. Histology, Dermis. Available online: https://www.ncbi.nlm.nih.gov/books/NBK535346/ (accessed on 10 May 2021).
- Dąbrowska, A.K.; Spano, F.; Derler, S.; Adlhart, C.; Spencer, N.D.; Rossi, R.M. The relationship between skin function, barrier properties, and body-dependent factors. Ski. Res. Technol. 2018, 24, 165–174. [Google Scholar] [CrossRef]
- Desai, P.; Patlolla, R.R.; Singh, M. Interaction of nanoparticles and cell-penetrating peptides with skin for transdermal drug delivery. Mol. Membr. Biol. 2010, 27, 247–259. [Google Scholar] [CrossRef]
- Bos, J.D.; Meinardi, M.M.H.M. The 500 Dalton rule for the skin penetration of chemical compounds and drugs. Exp. Dermatol. 2000, 9, 165–169. [Google Scholar] [CrossRef]
- Hadgraft, J. Modulation of the barrier function of the skin. Skin Pharmacol. Appl. Skin Physiol. 2001, 14, 72–81. [Google Scholar] [CrossRef]
- Vogt, A.; Wischke, C.; Neffe, A.T.; Ma, N.; Alexiev, U.; Lendlein, A. Nanocarriers for drug delivery into and through the skin—Do existing technologies match clinical challenges? J. Control. Release 2016, 242, 3–15. [Google Scholar] [CrossRef]
- Alkilani, A.Z.; McCrudden, M.T.C.; Donnelly, R.F. Transdermal drug delivery: Innovative pharmaceutical developments based on disruption of the barrier properties of the stratum corneum. Pharmaceutics 2015, 7, 438–470. [Google Scholar] [CrossRef]
- Carter, P.; Narasimhan, B.; Wang, Q. Biocompatible nanoparticles and vesicular systems in transdermal drug delivery for various skin diseases. Int. J. Pharm. 2019, 555, 49–62. [Google Scholar] [CrossRef]
- Cevc, G.; Blume, G. Lipid vesicles penetrate into intact skin owing to the transdermal osmotic gradients and hydration force. BBA—Biomembr. 1992, 1104, 226–232. [Google Scholar] [CrossRef]
- Seweryn, A. Interactions between surfactants and the skin—Theory and practice. Adv. Colloid Interface 2018, 256, 242–255. [Google Scholar] [CrossRef]
- Kapoor, B.; Gupta, R.; Gulati, M.; Singh, S.K.; Khursheed, R.; Gupta, M. The why, where, who, how, and what of the vesicular delivery systems. Adv. Colloid Interface 2019, 271, 101985. [Google Scholar] [CrossRef]
- Chacko, I.A.; Ghate, V.M.; Dsouza, L.; Lewis, S.A. Lipid vesicles: A versatile drug delivery platform for dermal and transdermal applications. Colloids Surf. B 2020, 195, 111262. [Google Scholar] [CrossRef]
- Mbah, C.C.; Attama, A.A. Vesicular carriers as innovative nanodrug delivery formulations. In Organic Materials as Smart Nanocarriers for Drug Delivery; Elsevier: Amsterdam, The Netherlands, 2018; pp. 519–559. [Google Scholar]
- Basiri, L.; Rajabzadeh, G.; Bostan, A. Physicochemical properties and release behavior of Span 60/Tween 60 niosomes as vehicle for α-Tocopherol delivery. LWT—Food Sci. Technol. 2017, 84, 471–478. [Google Scholar] [CrossRef]
- Gharbavi, M.; Amani, J.; Kheiri-Manjili, H.; Danafar, H.; Sharafi, A. Niosome: A promising nanocarrier for natural drug delivery through blood-brain barrier. Adv. Pharmacol. Sci. 2018, 2018, 6847971. [Google Scholar] [CrossRef]
- Chen, S.; Hanning, S.; Falconer, J.; Locke, M.; Wen, J. Recent advances in non-ionic surfactant vesicles (niosomes): Fabrication, characterization, pharmaceutical and cosmetic applications. Eur. J. Pharm. Biopharm. 2019, 144, 18–39. [Google Scholar] [CrossRef]
- AlQahtani, A.D.; O’Connor, D.; Domling, A.; Goda, S.K. Strategies for the production of long-acting therapeutics and efficient drug delivery for cancer treatment. Biomed. Pharmacother. 2019, 113, 108750. [Google Scholar] [CrossRef]
- Cerqueira-Coutinho, C.; dos Santos, E.P.; Mansur, C.R.E. Niosomes as nano-delivery systems in the pharmaceutical field. Crit. Rev. Ther. Drug Carrier Syst. 2016, 33, 195–212. [Google Scholar] [CrossRef]
- Aghajani, A.; Kazemi, T.; Enayatifard, R.; Amiri, F.T.; Narenji, M. Investigating the skin penetration and wound healing properties of niosomal pentoxifylline cream. Eur. J. Pharm. Sci. 2020, 151, 105434. [Google Scholar] [CrossRef]
- Shehata, T.M.; Nair, A.B.; Al-Dhubiab, B.E.; Shah, J.; Jacob, S.; Alhaider, I.A.; Attimarad, M.; Elsewedy, H.S.; Ibrahim, M.M. Vesicular emulgel based system for transdermal delivery of insulin: Factorial design and in vivo evaluation. Appl. Sci. 2020, 10, 5341. [Google Scholar] [CrossRef]
- Salem, H.F.; Kharshoum, R.M.; Abou-Taleb, H.A.; Farouk, H.O.; Zaki, R.M. Fabrication and appraisal of simvastatin via tailored niosomal nanovesicles for transdermal delivery enhancement: In vitro and in vivo assessment. Pharmaceutics 2021, 13, 138. [Google Scholar] [CrossRef] [PubMed]
- Ramadan, A.A.; Eladawy, S.A.; El-Enin, A.S.M.A.; Hussein, Z.M. Development and investigation of timolol maleate niosomal formulations for the treatment of glaucoma. J. Pharm. Investig. 2020, 50, 59–70. [Google Scholar] [CrossRef]
- Barani, M.; Mirzaei, M.; Torkzadeh-Mahani, M.; Lohrasbi-Nejad, A.; Nematollahi, M.H. A new formulation of hydrophobin-coated niosome as a drug carrier to cancer cells. Mater. Sci. Eng. C 2020, 113, 110975. [Google Scholar] [CrossRef]
- Sita, V.G.; Jadhav, D.; Vavia, P. Niosomes for nose-to-brain delivery of bromocriptine: Formulation development, efficacy evaluation and toxicity profiling. J. Drug Deliv. Sci. Technol. 2020, 58, 101791. [Google Scholar] [CrossRef]
- Shah, H.S.; Usman, F.; Ashfaq-Khan, M.; Khalil, R.; Ul-Haq, Z.; Mushtaq, A.; Qaiser, R.; Iqbal, J. Preparation and characterization of anticancer niosomal withaferin–A formulation for improved delivery to cancer cells: In vitro, in vivo, and in silico evaluation. J. Drug Deliv. Sci. Technol. 2020, 59, 101863. [Google Scholar] [CrossRef]
- Teaima, M.H.; El Mohamady, A.M.; El-Nabarawi, M.A.; Mohamed, A.I. Formulation and evaluation of niosomal vesicles containing ondansetron HCL for trans-mucosal nasal drug delivery. Drug Dev. Ind. Pharm. 2020, 46, 751–761. [Google Scholar] [CrossRef]
- Saimi, N.I.M.; Salim, N.; Ahmad, N.; Abdulmalek, E.; Rahman, M.B.A. Aerosolized niosome formulation containing gemcitabine and cisplatin for lung cancer treatment: Optimization, characterization and in vitro evaluation. Pharmaceutics 2021, 13, 59. [Google Scholar] [CrossRef] [PubMed]
- Gugleva, V.; Titeva, S.; Ermenlieva, N.; Tsibranska, S.; Tcholakova, S.; Rangelov, S.; Momekova, D. Development and evaluation of doxycycline niosomal thermoresponsive in situ gel for ophthalmic delivery. Int. J. Pharm. 2020, 591, 120010. [Google Scholar] [CrossRef]
- Allam, A.; Elsabahy, M.; El Badry, M.; Eleraky, N.E. Betaxolol-loaded niosomes integrated within pH-sensitive in situ forming gel for management of glaucoma. Int. J. Pharm. 2021, 598, 120380. [Google Scholar] [CrossRef]
- Rinaldi, F.; Seguella, L.; Gigli, S.; Hanieh, P.N.; Del Favero, E.; Cantù, L.; Pesce, M.; Sarnelli, G.; Marianecci, C.; Esposito, G.; et al. inPentasomes: An innovative nose-to-brain pentamidine delivery blunts MPTP parkinsonism in mice. J. Control. Release 2019, 294, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Mirzaei-Parsa, M.J.; Najafabadi, M.R.H.; Haeri, A.; Zahmatkeshan, M.; Ebrahimi, S.A.; Pazoki-Toroudi, H.; Adel, M. Preparation, characterization, and evaluation of the anticancer activity of artemether-loaded nano-niosomes against breast cancer. Breast Cancer 2020, 27, 243–251. [Google Scholar] [CrossRef] [PubMed]
- El-Nabarawi, M.A.; Abd El Rehem, R.T.; Teaima, M.; Abary, M.; El-Mofty, H.M.; Khafagy, M.M.; Lotfy, N.M.; Salah, M. Natamycin niosomes as a promising ocular nanosized delivery system with ketorolac tromethamine for dual effects for treatment of candida rabbit keratitis; in vitro/in vivo and histopathological studies. Drug Dev. Ind. Pharm. 2019, 45, 922–936. [Google Scholar] [CrossRef] [PubMed]
- Lu, B.; Huang, Y.; Chen, Z.; Ye, J.; Xu, H.; Chen, W.; Long, X. Niosomal nanocarriers for enhanced skin delivery of quercetin with functions of anti-tyrosinase and antioxidant. Molecules 2019, 24, 2322. [Google Scholar] [CrossRef]
- Bhardwaj, P.; Tripathi, P.; Gupta, R.; Pandey, S. Niosomes: A review on niosomal research in the last decade. J. Drug Deliv. Sci. Technol. 2020, 56, 101581. [Google Scholar] [CrossRef]
- Münch, S.; Wohlrab, J.; Neubert, R.H.H. Dermal and transdermal delivery of pharmaceutically relevant macromolecules. Eur. J. Pharm. Biopharm. 2017, 119, 235–242. [Google Scholar] [CrossRef]
- Jacob, S.; Nair, A.B.; Al-Dhubiab, B.E. Preparation and evaluation of niosome gel containing acyclovir for enhanced dermal deposition. J. Liposome Res. 2017, 27, 283–292. [Google Scholar] [CrossRef] [PubMed]
- Kassem, A.A.; Abd El-Alim, S.H.; Asfour, M.H. Enhancement of 8-methoxypsoralen topical delivery via nanosized niosomal vesicles: Formulation development, in vitro and in vivo evaluation of skin deposition. Int. J. Pharm. 2017, 517, 256–268. [Google Scholar] [CrossRef]
- Shah, H.; Nair, A.B.; Shah, J.; Bharadia, P.; Al-Dhubiab, B.E. Proniosomal gel for transdermal delivery of lornoxicam: Optimization using factorial design and in vivo evaluation in rats. DARU 2019, 27, 59–70. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.; Parashar, P.; Kanoujia, J.; Singh, I.; Saha, S.; Saraf, S.A. Transdermal potential and anti-gout efficacy of Febuxostat from niosomal gel. J. Drug Deliv. Sci. Technol. 2017, 39, 348–361. [Google Scholar] [CrossRef]
- Muzzalupo, R.; Tavano, L.; Cassano, R.; Trombino, S.; Ferrarelli, T.; Picci, N. A new approach for the evaluation of niosomes as effective transdermal drug delivery systems. Eur. J. Pharm. Biopharm. 2011, 79, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Nigro, F.; dos Santos Cerqueira Pinto, C.; dos Santos, E.P.; Mansur, C.R.E. Niosome-based hydrogel as a potential drug delivery system for topical and transdermal applications. Int. J. Polym. Mater. Polym. Biomater. 2020, 8833. [Google Scholar] [CrossRef]
- Ghafelehbashi, R.; Akbarzadeh, I.; Tavakkoli Yaraki, M.; Lajevardi, A.; Fatemizadeh, M.; Heidarpoor Saremi, L. Preparation, physicochemical properties, in vitro evaluation and release behavior of cephalexin-loaded niosomes. Int. J. Pharm. 2019, 569, 118580. [Google Scholar] [CrossRef]
- Nene, S.; Shah, S.; Rangaraj, N.; Mehra, N.K.; Singh, P.K.; Srivastava, S. Lipid based nanocarriers: A novel paradigm for topical antifungal therapy. J. Drug Deliv. Sci. Technol. 2021, 62, 102397. [Google Scholar] [CrossRef]
- Sadeghi Ghadi, Z.; Dinarvand, R.; Asemi, N.; Talebpour Amiri, F.; Ebrahimnejad, P. Preparation, characterization and in vivo evaluation of novel hyaluronan containing niosomes tailored by Box-Behnken design to co-encapsulate curcumin and quercetin. Eur. J. Pharm. Sci. 2019, 130, 234–246. [Google Scholar] [CrossRef]
- Cheng, R.; Xu, T.; Wang, C.; Gan, C. The stabilization and antioxidant performances of coenzyme Q10-loaded niosomes coated by PEG and chitosan. J. Mol. Liq. 2021, 325, 115194. [Google Scholar] [CrossRef]
- Radmard, A.; Saeedi, M.; Morteza-Semnani, K.; Hashemi, S.M.H.; Nokhodchi, A. An eco-friendly and green formulation in lipid nanotechnology for delivery of a hydrophilic agent to the skin in the treatment and management of hyperpigmentation complaints: Arbutin niosome (Arbusome). Colloids Surf. B 2021, 201, 111616. [Google Scholar] [CrossRef]
- Qumbar, M.; Imam, S.S.; Ali, J.; Ahmad, J.; Ali, A. Formulation and optimization of lacidipine loaded niosomal gel for transdermal delivery: In-vitro characterization and in-vivo activity. Biomed. Pharmacother. 2017, 93, 255–266. [Google Scholar] [CrossRef] [PubMed]
- Grijalvo, S.; Puras, G.; Zárate, J.; Sainz-Ramos, M.; Qtaish, N.A.L.; López, T.; Mashal, M.; Attia, N.; Díaz, D.; Pons, R.; et al. Cationic niosomes as non-viral vehicles for nucleic acids: Challenges and opportunities in gene delivery. Pharmaceutics 2019, 11, 50. [Google Scholar] [CrossRef]
- Mashal, M.; Attia, N.; Martínez-Navarrete, G.; Soto-Sánchez, C.; Fernández, E.; Grijalvo, S.; Eritja, R.; Puras, G.; Pedraz, J.L. Gene delivery to the rat retina by non-viral vectors based on chloroquine-containing cationic niosomes. J. Control. Release 2019, 304, 181–190. [Google Scholar] [CrossRef]
- Roque, L.; Fernández, M.; Benito, J.M.; Escudero, I. Stability and characterization studies of Span 80 niosomes modified with CTAB in the presence of NaCl. Colloids Surf. A 2020, 601, 124999. [Google Scholar] [CrossRef]
- Chaikul, P.; Khat-udomkiri, N.; Iangthanarat, K.; Manosroi, J.; Manosroi, A. Characteristics and in vitro anti-skin aging activity of gallic acid loaded in cationic CTAB niosome. Eur. J. Pharm. Sci. 2019, 131, 39–49. [Google Scholar] [CrossRef]
- Muzzalupo, R.; Pérez, L.; Pinazo, A.; Tavano, L. Pharmaceutical versatility of cationic niosomes derived from amino acid-based surfactants: Skin penetration behavior and controlled drug release. Int. J. Pharm. 2017, 529, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Kushnazarova, R.A.; Mirgorodskaya, A.B.; Zakharova, L.Y. Niosomes modified with cationic surfactants to increase the bioavailability and stability of indomethacin. Russ. Chem. Bull. 2021, 70, 585–591. [Google Scholar] [CrossRef]
- Cevc, G.; Blume, G.; Schätzlein, A.; Gebauer, D.; Paul, A. The skin: A pathway for systemic treatment with patches and lipid-based agent carriers. Adv. Drug Deliv. Rev. 1996, 18, 349–378. [Google Scholar] [CrossRef]
- Pena-Rodríguez, E.; Moreno, M.C.; Blanco-Fernandez, B.; González, J.; Fernández-Campos, F. Epidermal delivery of retinyl palmitate loaded transfersomes: Penetration and biodistribution studies. Pharmaceutics 2020, 12, 112. [Google Scholar] [CrossRef]
- Touitou, E.; Dayan, N.; Bergelson, L.; Godin, B.; Eliaz, M. Ethosomes—Novel vesicular carriers for enhanced delivery: Characterization and skin penetration properties. J. Control. Release 2000, 65, 403–418. [Google Scholar] [CrossRef]
- Song, C.K.; Balakrishnan, P.; Shim, C.K.; Chung, S.J.; Chong, S.; Kim, D.D. A novel vesicular carrier, transethosome, for enhanced skin delivery of voriconazole: Characterization and in vitro/in vivo evaluation. Colloids Surf. B 2012, 92, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Sala, M.; Diab, R.; Elaissari, A.; Fessi, H. Lipid nanocarriers as skin drug delivery systems: Properties, mechanisms of skin interactions and medical applications. Int. J. Pharm. 2018, 535, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Garg, V.; Singh, H.; Bimbrawh, S.; Singh, S.K.; Gulati, M.; Vaidya, Y.; Kaur, P. Ethosomes and transfersomes: Principles, perspectives and practices. Curr. Drug Deliv. 2016, 14, 613–633. [Google Scholar] [CrossRef] [PubMed]
- Goyal, N.; Thatai, P.; Sapra, B. Skin cancer: Symptoms, mechanistic pathways and treatment rationale for therapeutic delivery. Ther. Deliv. 2017, 8, 265–287. [Google Scholar] [CrossRef] [PubMed]
- Sardana, V.; Burzynski, J.; Zalzal, P. Safety and efficacy of topical ketoprofen in transfersome gel in knee osteoarthritis: A systematic review. Musculoskeletal Care 2017, 15, 114–121. [Google Scholar] [CrossRef]
- Verma, S.; Utreja, P. Vesicular nanocarrier based treatment of skin fungal infections: Potential and emerging trends in nanoscale pharmacotherapy. Asian J. Pharm. Sci. 2019, 14, 117–129. [Google Scholar] [CrossRef]
- Fernández-García, R.; Lalatsa, A.; Statts, L.; Bolás-Fernández, F.; Ballesteros, M.P.; Serrano, D.R. Transferosomes as nanocarriers for drugs across the skin: Quality by design from lab to industrial scale. Int. J. Pharm. 2020, 573, 118817. [Google Scholar] [CrossRef]
- Natsheh, H.; Touitou, E. Phospholipid vesicles for dermal/transdermal and nasal administration of active molecules: The effect of surfactants and alcohols on the fluidity of their lipid bilayers and penetration enhancement properties. Molecules 2020, 25, 2959. [Google Scholar] [CrossRef]
- Opatha, S.A.T.; Titapiwatanakun, V.; Chutoprapat, R. Transfersomes: A promising nanoencapsulation technique for transdermal drug delivery. Pharmaceutics 2020, 12, 855. [Google Scholar] [CrossRef]
- Nangare, S.; Bhatane, D.; Mali, R.; Shitole, M. Development of a novel freeze-dried mulberry leaf extract-based transfersome gel. Turk. J. Pharm. Sci. 2021, 18, 44–55. [Google Scholar] [CrossRef]
- Gupta, N.; Jain, S. Designing and optimization of naproxen sodium deformable vesicular systems through factorial design: Box behenken model. Int. J. Appl. Pharm. 2021, 13, 190–197. [Google Scholar] [CrossRef]
- González-Rodríguez, M.L.; Arroyo, C.M.; Cózar-Bernal, M.J.; González-R, P.L.; León, J.M.; Calle, M.; Canca, D.; Rabasco, A.M. Deformability properties of timolol-loaded transfersomes based on the extrusion mechanism. Statistical optimization of the process. Drug Dev. Ind. Pharm. 2016, 42, 1683–1694. [Google Scholar] [CrossRef]
- El-Gizawy, S.A.; Nouh, A.; Saber, S.; Kira, A.Y. Deferoxamine-loaded transfersomes accelerates healing of pressure ulcers in streptozotocin-induced diabetic rats. J. Drug Deliv. Sci. Technol. 2020, 58, 101732. [Google Scholar] [CrossRef]
- Balata, G.F.; Faisal, M.M.; Elghamry, H.A.; Sabry, S.A. Preparation and characterization of ivabradine HCl transfersomes for enhanced transdermal delivery. J. Drug Deliv. Sci. Technol. 2020, 60, 101921. [Google Scholar] [CrossRef]
- Iskandarsyah; Masrijal, C.D.P.; Harmita. Formulation, characterization, evaluation and in vitro study of transfersomal gel medroxyprogesterone acetate for transdermal drug delivery. Int. J. Res. Pharm. Sci. 2020, 11, 5373–5381. [Google Scholar] [CrossRef]
- Luiz, M.T.; Viegas, J.S.R.; Abriata, J.P.; Tofani, L.B.; de Menezes Vaidergorn, M.; da Silva Emery, F.; Chorilli, M.; Marchetti, J.M. Docetaxel-loaded folate-modified TPGS-transfersomes for glioblastoma multiforme treatment. Mater. Sci. Eng. C 2021, 124, 112033. [Google Scholar] [CrossRef]
- Verma, N.; Saraf, S. Development and optimization of mannosylated naringenin loaded transfersomes using response surface methodology for skin carcinoma. Int. J. Appl. Pharm. 2021, 13, 235–241. [Google Scholar] [CrossRef]
- Dudhipala, N.; Phasha Mohammed, R.; Adel Ali Youssef, A.; Banala, N. Effect of lipid and edge activator concentration on development of aceclofenac-loaded transfersomes gel for transdermal application: In vitro and ex vivo skin permeation. Drug Dev. Ind. Pharm. 2020, 46, 1334–1344. [Google Scholar] [CrossRef] [PubMed]
- Nurfitriyana, N.; Harmita, H.; Iskandarsyah, I. In vitro study of a transfersomal gel preparation containing lynestrenol as a transdermal drug delivery system. Int. J. Appl. Pharm. 2020, 12, 242–244. [Google Scholar] [CrossRef]
- Nnamani, P.O.; Ugwu, A.A.; Nnadi, O.H.; Kenechukwu, F.C.; Ofokansi, K.C.; Attama, A.A.; Lehr, C.-M. Formulation and evaluation of transdermal nanogel for delivery of artemether. Drug Deliv. Transl. Res. 2021, 11, 1655–1674. [Google Scholar] [CrossRef]
- Kawar, D.; Abdelkader, H. Hyaluronic acid gel-core liposomes (hyaluosomes) enhance skin permeation of ketoprofen. Pharm. Dev. Technol. 2019, 24, 947–953. [Google Scholar] [CrossRef] [PubMed]
- Das, B.; Sen, S.O.; Maji, R.; Nayak, A.K.; Sen, K.K. Transferosomal gel for transdermal delivery of risperidone: Formulation optimization and ex vivo permeation. J. Drug Deliv. Sci. Technol. 2017, 38, 59–71. [Google Scholar] [CrossRef]
- Abdel-Hafez, S.M.; Hathout, R.M.; Sammour, O.A. Curcumin-loaded ultradeformable nanovesicles as a potential delivery system for breast cancer therapy. Colloids Surf. B 2018, 167, 63–72. [Google Scholar] [CrossRef]
- Abdellatif, A.A.H.; Tawfeek, H.M. Transfersomal Nanoparticles for Enhanced Transdermal Delivery of Clindamycin. AAPS PharmSciTech 2016, 17, 1067–1074. [Google Scholar] [CrossRef] [PubMed]
- Batool, S.; Zahid, F.; Ud-Din, F.; Naz, S.S.; Dar, M.J.; Khan, M.W.; Zeb, A.; Khan, G.M. Macrophage targeting with the novel carbopol-based miltefosine-loaded transfersomal gel for the treatment of cutaneous leishmaniasis: In vitro and in vivo analyses. Drug Dev. Ind. Pharm. 2021, 47, 440–453. [Google Scholar] [CrossRef] [PubMed]
- Salim, M.W.; Shabbir, K.; Ud-Din, F.; Yousaf, A.M.; Choi, H.G.; Khan, G.M. Preparation, in-vitro and in-vivo evaluation of rifampicin and vancomycin co-loaded transfersomal gel for the treatment of cutaneous leishmaniasis. J. Drug Deliv. Sci. Technol. 2020, 60, 101996. [Google Scholar] [CrossRef]
- Kassem, M.A.; Aboul-Einien, M.H.; El Taweel, M.M. Dry gel containing optimized felodipine-loaded transferosomes: A promising transdermal delivery system to enhance drug bioavailability. AAPS PharmSciTech 2018, 19, 2155–2173. [Google Scholar] [CrossRef] [PubMed]
- Omar, M.M.; Eleraky, N.E.; El Sisi, A.M.; Hasan, O.A. Development and evaluation of in-situ nasal gel formulations of nanosized transferosomal sumatriptan: Design, optimization, in vitro and in vivo evaluation. Drug Des. Devel. Ther. 2019, 13, 4413–4430. [Google Scholar] [CrossRef] [PubMed]
- Nimisha, D.A.R.; Fatima, Z.; Neema, C.D.K. Antipsoriatic and anti-inflammatory studies of berberis aristata extract loaded nanovesicular gels. Pharmacogn. Mag. 2017, 13, 587–594. [Google Scholar] [CrossRef]
- Lu, K.; Xie, S.; Han, S.; Zhang, J.; Chang, X.; Chao, J.; Huang, Q.; Yuan, Q.; Lin, H.; Xu, L.; et al. Preparation of a nano emodin transfersome and study on its anti-obesity mechanism in adipose tissue of diet-induced obese rats. J. Transl. Med. 2014, 12, 72. [Google Scholar] [CrossRef]
- Salem, H.F.; Kharshoum, R.M.; Abou-Taleb, H.A.; Naguib, D.M. Nanosized transferosome-based intranasal in situ gel for brain targeting of resveratrol: Formulation, optimization, in vitro evaluation, and in vivo pharmacokinetic study. AAPS PharmSciTech 2019, 20, 181. [Google Scholar] [CrossRef] [PubMed]
- Salem, H.F.; Kharshoum, R.M.; Abou-Taleb, H.A.; Naguib, D.M. Brain targeting of resveratrol through intranasal lipid vesicles labelled with gold nanoparticles: In vivo evaluation and bioaccumulation investigation using computed tomography and histopathological examination. J. Drug Target. 2019, 27, 1127–1134. [Google Scholar] [CrossRef] [PubMed]
- Elkomy, M.H.; El Menshawe, S.F.; Abou-Taleb, H.A.; Elkarmalawy, M.H. Loratadine bioavailability via buccal transferosomal gel: Formulation, statistical optimization, in vitro/in vivo characterization, and pharmacokinetics in human volunteers. Drug Deliv. 2017, 24, 781–791. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, T.A. Study the pharmacokinetics, pharmacodynamics and hepatoprotective activity of rosuvastatin from drug loaded lyophilized orodispersible tablets containing transfersomes nanoparticles. J. Drug Deliv. Sci. Technol. 2021, 63, 102489. [Google Scholar] [CrossRef]
- Sousa, F.; Ferreira, D.; Reis, S.; Costa, P. Current insights on antifungal therapy: Novel nanotechnology approaches for drug delivery systems and new drugs from natural sources. Pharmaceuticals 2020, 13, 248. [Google Scholar] [CrossRef] [PubMed]
- Soliman, G.M. Nanoparticles as safe and effective delivery systems of antifungal agents: Achievements and challenges. Int. J. Pharm. 2017, 523, 15–32. [Google Scholar] [CrossRef] [PubMed]
- Salem, H.F.; Kharshoum, R.M.; Abou-Taleb, H.A.; AbouTaleb, H.A.; AbouElhassan, K.M. Progesterone-loaded nanosized transethosomes for vaginal permeation enhancement: Formulation, statistical optimization, and clinical evaluation in anovulatory polycystic ovary syndrome. J. Liposome Res. 2019, 29, 183–194. [Google Scholar] [CrossRef]
- Chen, Z.X.; Li, B.; Liu, T.; Wang, X.; Zhu, Y.; Wang, L.; Wang, X.H.; Niu, X.; Xiao, Y.; Sun, Q. Evaluation of paeonol-loaded transethosomes as transdermal delivery carriers. Eur. J. Pharm. Sci. 2017, 99, 240–245. [Google Scholar] [CrossRef] [PubMed]
- Garg, V.; Singh, H.; Bhatia, A.; Raza, K.; Singh, S.K.; Singh, B.; Beg, S. Systematic development of transethosomal gel system of piroxicam: Formulation optimization, in vitro evaluation, and ex vivo assessment. AAPS PharmSciTech 2017, 18, 58–71. [Google Scholar] [CrossRef]
- Nayak, D.; Tawale, R.M.; Aranjani, J.M.; Tippavajhala, V.K. Formulation, optimization and evaluation of novel ultra-deformable vesicular drug delivery system for an anti-fungal drug. AAPS PharmSciTech 2020, 21, 140. [Google Scholar] [CrossRef]
- Ansari, M.D.; Ahmed, S.; Imam, S.S.; Khan, I.; Singhal, S.; Sharma, M.; Sultana, Y. CCD based development and characterization of nano-transethosome to augment the antidepressant effect of agomelatine on Swiss albino mice. J. Drug Deliv. Sci. Technol. 2019, 54, 101234. [Google Scholar] [CrossRef]
- Rady, M.; Gomaa, I.; Afifi, N.; Abdel-Kader, M. Dermal delivery of Fe-chlorophyllin via ultradeformable nanovesicles for photodynamic therapy in melanoma animal model. Int. J. Pharm. 2018, 548, 480–490. [Google Scholar] [CrossRef] [PubMed]
- El-Kayal, M.; Nasr, M.; Elkheshen, S.; Mortada, N. Colloidal (-)-epigallocatechin-3-gallate vesicular systems for prevention and treatment of skin cancer: A comprehensive experimental study with preclinical investigation. Eur. J. Pharm. Sci. 2019, 137, 104972. [Google Scholar] [CrossRef] [PubMed]
- Albash, R.; Abdelbary, A.A.; Refai, H.; El-Nabarawi, M.A. Use of transethosomes for enhancing the transdermal delivery of olmesartan medoxomil: In vitro, ex vivo, and in vivo evaluation. Int. J. Nanomed. 2019, 14, 1953–1968. [Google Scholar] [CrossRef] [PubMed]
- Mahdi, M.; Rostami, H.; Mahdi, S.; Fathi, M. Food bioscience development and characterization of chitosan-coated nanoliposomes for encapsulation of caffeine. Food Biosci. 2021, 40, 100857. [Google Scholar] [CrossRef]
- Alavi, S.; Haeri, A.; Dadashzadeh, S. Utilization of chitosan-caged liposomes to push the boundaries of therapeutic delivery. Carbohydr. Polym. 2017, 157, 991–1012. [Google Scholar] [CrossRef]
- Hasanovic, A.; Hollick, C.; Fischinger, K.; Valenta, C. Improvement in physicochemical parameters of DPPC liposomes and increase in skin permeation of aciclovir and minoxidil by the addition of cationic polymers. Eur. J. Pharm. Biopharm. 2010, 75, 148–153. [Google Scholar] [CrossRef]
- Saidin, N.M.; Anuar, N.K.; Meor Mohd Affandi, M.M.R. Roles of polysaccharides in transdermal drug delivery system and future prospects. J. Appl. Pharm. Sci. 2018, 8, 141–157. [Google Scholar] [CrossRef][Green Version]
- Ali, A.; Ahmed, S. A review on chitosan and its nanocomposites in drug delivery. Int. J. Biol. Macromol. 2018, 109, 273–286. [Google Scholar] [CrossRef]
- Sivasankarapillai, V.S.; Das, S.S.; Sabir, F.; Sundaramahalingam, M.A.; Colmenares, J.C.; Prasannakumar, S.; Rajan, M.; Rahdar, A.; Kyzas, G.Z. Progress in natural polymer engineered biomaterials for transdermal drug delivery systems. Mater. Today Chem. 2021, 19, 100382. [Google Scholar] [CrossRef]
- He, W.; Guo, X.; Xiao, L.; Feng, M. Study on the mechanisms of chitosan and its derivatives used as transdermal penetration enhancers. Int. J. Pharm. 2009, 382, 234–243. [Google Scholar] [CrossRef]
- Mohammed, L.; Nourddine, H.; Saad, E.F.; Abdelali, D.; Hamid, R. Chitosan-covered liposomes as a promising drug transporter: Nanoscale investigations. RSC Adv. 2021, 11, 1503–1516. [Google Scholar] [CrossRef]
- Chen, Y.; Wang, M.; Fang, L. Biomaterials as novel penetration enhancers for transdermal and dermal drug delivery systems. Drug Deliv. 2013, 20, 199–209. [Google Scholar] [CrossRef] [PubMed]
- Sebaaly, C.; Trifan, A.; Sieniawska, E.; Greige-Gerges, H. Chitosan-coating effect on the characteristics of liposomes: A focus on bioactive compounds and essential oils: A review. Processes 2021, 9, 445. [Google Scholar] [CrossRef]
- Mititelu-Tartau, L.; Bogdan, M.; Pricop, D.A.; Buca, B.R.; Hilitanu, L.; Pauna, A.-M.; Dijmarescu, L.A.; Popa, E.G. Biocompatibility and pharmacological effects of innovative systems for prolonged drug release containing dexketoprofen in rats. Polymers 2021, 13, 1010. [Google Scholar] [CrossRef]
- Elsayad, M.K.; Mowafy, H.A.; Zaky, A.A.; Samy, A.M. Chitosan caged liposomes for improving oral bioavailability of rivaroxaban: In vitro and in vivo evaluation. Pharm. Dev. Technol. 2021, 26, 316–327. [Google Scholar] [CrossRef] [PubMed]
- Lopes Rocha Correa, V.; Assis Martins, J.; Ribeiro de Souza, T.; de Castro Nunes Rincon, G.; Pacheco Miguel, M.; Borges de Menezes, L.; Correa Amaral, A. Melatonin loaded lecithin-chitosan nanoparticles improved the wound healing in diabetic rats. Int. J. Biol. Macromol. 2020, 162, 1465–1475. [Google Scholar] [CrossRef]
- Caddeo, C.; Díez-Sales, O.; Pons, R.; Carbone, C.; Ennas, G.; Puglisi, G.; Fadda, A.M.; Manconi, M. Cross-linked chitosan/liposome hybrid system for the intestinal delivery of quercetin. J. Colloid Interface Sci. 2016, 461, 69–78. [Google Scholar] [CrossRef]
- Esposto, B.S.; Jauregi, P.; Tapia-Blácido, D.R.; Martelli-Tosi, M. Liposomes vs. chitosomes: Encapsulating food bioactives. Trends Food Sci. Technol. 2021, 108, 40–48. [Google Scholar] [CrossRef]
- Lee, E.H.; Lim, S.J.; Lee, M.K. Chitosan-coated liposomes to stabilize and enhance transdermal delivery of indocyanine green for photodynamic therapy of melanoma. Carbohydr. Polym. 2019, 224, 115143. [Google Scholar] [CrossRef] [PubMed]
- Li, L.; Zhang, Y.; Han, S.; Qu, Z.; Zhao, J.; Chen, Y.; Chen, Z.; Duan, J.; Pan, Y.; Tang, X. Penetration enhancement of lidocaine hydrochlorid by a novel chitosan coated elastic liposome for transdermal drug delivery. J. Biomed. Nanotechnol. 2011, 7, 704–713. [Google Scholar] [CrossRef] [PubMed]
- Park, S.N.; Jo, N.R.; Jeon, S.H. Chitosan-coated liposomes for enhanced skin permeation of resveratrol. J. Ind. Eng. Chem. 2014, 20, 1481–1485. [Google Scholar] [CrossRef]
- Yaroslavov, A.A.; Efimova, A.A.; Krasnikov, E.A.; Trosheva, K.S.; Popov, A.S.; Melik-Nubarov, N.S.; Krivtsov, G.G. Chitosan-based multi-liposomal complexes: Synthesis, biodegradability and cytotoxicity. Int. J. Biol. Macromol. 2021, 177, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Xiong, G.M.; Ali, Y.; Boehm, B.O.; Huang, Y.Y.; Venkatraman, S. Layer-by-layer coated nanoliposomes for oral delivery of insulin. Nanoscale 2021, 13, 776–789. [Google Scholar] [CrossRef]
- Mertins, O.; Dimova, R. Insights on the interactions of chitosan with phospholipid vesicles. Part I: Effect of polymer deprotonation. Langmuir 2013, 29, 14545–14551. [Google Scholar] [CrossRef]
- Quemeneur, F.; Rinaudo, M.; Pépin-Donat, B. Influence of molecular weight and pH on adsorption of chitosan at the surface of large and giant vesicles. Biomacromolecules 2008, 9, 396–402. [Google Scholar] [CrossRef]
- Tan, H.W.; Misran, M. Polysaccharide-anchored fatty acid liposome. Int. J. Pharm. 2013, 441, 414–423. [Google Scholar] [CrossRef]
- Seong, J.S.; Yun, M.E.; Park, S.N. Surfactant-stable and pH-sensitive liposomes coated with N-succinyl-chitosan and chitooligosaccharide for delivery of quercetin. Carbohydr. Polym. 2018, 181, 659–667. [Google Scholar] [CrossRef]
- Eh Suk, V.R.; Marlina, A.; Hussain, Z.; Misran, M. N-stearoyl chitosan as a coating material for liposomes encapsulating itraconazole. Arab. J. Sci. Eng. 2021, 46, 5645–5653. [Google Scholar] [CrossRef]
- Shukla, S.K.; Chan, A.; Parvathaneni, V.; Gupta, V. Metformin-loaded chitosomes for treatment of malignant pleural mesothelioma—A rare thoracic cancer. Int. J. Biol. Macromol. 2020, 160, 128–141. [Google Scholar] [CrossRef] [PubMed]
- Andersen, T.; Mishchenko, E.; Flaten, G.E.; Sollid, J.U.E.; Mattsson, S.; Tho, I.; Škalko-Basnet, N. Chitosan-based nanomedicine to fight genital Candida Infections: Chitosomes. Mar. Drugs 2017, 15, 64. [Google Scholar] [CrossRef]
- Hemmingsen, L.M.; Giordani, B.; Pettersen, A.K.; Vitali, B.; Basnet, P.; Škalko-Basnet, N. Liposomes-in-chitosan hydrogel boosts potential of chlorhexidine in biofilm eradication in vitro. Carbohydr. Polym. 2021, 262, 117939. [Google Scholar] [CrossRef] [PubMed]
- Zhao, G.; Hu, C.; Xue, Y. In vitro evaluation of chitosan-coated liposome containing both coenzyme Q10 and alpha-lipoic acid: Cytotoxicity, antioxidant activity, and antimicrobial activity. J. Cosmet. Dermatol. 2018, 17, 258–262. [Google Scholar] [CrossRef]
- Castro, N.R.; dos Santos Cerqueira Pinto, C.; de Campos, V.E.B.; Cardoso, V.; Vermelho, A.B.; dos Santos, E.P.; Mansur, C.R.E. Development of hybrid vesicular nanosystems composed of lipids and chitosan for octyl methoxycinnamate encapsulation. Colloids Surface. A 2021, 608, 125476. [Google Scholar] [CrossRef]
- El Menshawe, S.F.; Aboud, H.M.; Elkomy, M.H.; Kharshoum, R.M.; Abdeltwab, A.M. A novel nanogel loaded with chitosan decorated bilosomes for transdermal delivery of terbutaline sulfate: Artificial neural network optimization, in vitro characterization and in vivo evaluation. Drug Deliv. Transl. Res. 2020, 10, 471–485. [Google Scholar] [CrossRef]
- Lv, H.X.; Zhang, Z.H.; Wang, X.P.; Cheng, Q.Q.; Wang, W.; Huang, X.H.; Zhou, J.P.; Zhang, Q.; Hou, L.L.; Huo, W. A biomimetic chitosan derivates: Preparation, characterization and transdermal enhancement studies of n-arginine chitosan. Molecules 2011, 16, 6778–6790. [Google Scholar] [CrossRef] [PubMed]
- Garcia, B.B.M.; Mertins, O.; da Silva, E.R.; Mathews, P.D.; Han, S.W. Arginine-modified chitosan complexed with liposome systems for plasmid DNA delivery. Colloids Surf. B 2020, 193, 111131. [Google Scholar] [CrossRef]
- Deng, J.; Zhang, Z.; Liu, C.; Yin, L.; Zhou, J.; Lv, H. The studies of N-Octyl-N-arginine-chitosan coated liposome as an oral delivery system of cyclosporine A. J. Pharm. Pharmacol. 2015, 67, 1363–1370. [Google Scholar] [CrossRef] [PubMed]
- Jain, S.; Tripathi, S.; Tripathi, P.K. Invasomes: Potential vesicular systems for transdermal delivery of drug molecules. J. Drug Deliv. Sci. Technol. 2021, 61, 102166. [Google Scholar] [CrossRef]
- Ashtikar, M.; Nagarsekar, K.; Fahr, A. Transdermal delivery from liposomal formulations—Evolution of the technology over the last three decades. J. Control. Release 2016, 242, 126–140. [Google Scholar] [CrossRef] [PubMed]
- Amnuaikit, T.; Limsuwan, T.; Khongkow, P.; Boonme, P. Vesicular carriers containing phenylethyl resorcinol for topical delivery system; liposomes, transfersomes and invasomes. Asian, J. Pharm. Sci. 2018, 13, 472–484. [Google Scholar] [CrossRef]
- El-Kattan, A.F.; Asbill, C.S.; Kim, N.; Michniak, B.B. The effects of terpene enhancers on the percutaneous permeation of drugs with different lipophilicities. Int. J. Pharm. 2001, 215, 229–240. [Google Scholar] [CrossRef]
- Krishnaiah, Y.S.R.; Satyanarayana, V.; Karthikeyan, R.S. Penetration enhancing effect of menthol on the percutaneous flux of nicardipine hydrochloride through excised rat epidermis from hydroxypropyl cellulose gels. Pharm. Dev. Technol. 2002, 7, 305–315. [Google Scholar] [CrossRef]
- Aqil, M.; Ahad, A.; Sultana, Y.; Ali, A. Status of terpenes as skin penetration enhancers. Drug Discov. Today 2007, 12, 1061–1067. [Google Scholar] [CrossRef] [PubMed]
- Andega, S.; Kanikkannan, N.; Singh, M. Comparison of the effect of fatty alcohols on the permeation of melatonin between porcine and human skin. J. Control. Release 2001, 77, 17–25. [Google Scholar] [CrossRef]
- Anurova, M.N.; Demina, N.B.; Bakhrushina, E.O. Permeability enhancers in transdermal delivery system technology (review). Pharm. Chem. J. 2021, 54, 1162–1168. [Google Scholar] [CrossRef]
- Shah, S.M.; Ashtikar, M.; Jain, A.S.; Makhija, D.T.; Nikam, Y.; Gude, R.P.; Steiniger, F.; Jagtap, A.A.; Nagarsenker, M.S.; Fahr, A. LeciPlex, invasomes, and liposomes: A skin penetration study. Int. J. Pharm. 2015, 490, 391–403. [Google Scholar] [CrossRef]
- Dragicevic-Curic, N.; Gräfe, S.; Albrecht, V.; Fahr, A. Topical application of temoporfin-loaded invasomes for photodynamic therapy of subcutaneously implanted tumours in mice: A pilot study. J. Photoch. Photobiol. B 2008, 91, 41–50. [Google Scholar] [CrossRef]
- Abdollahi, D.; Jafariazar, Z.; Afshar, M. Effect of monoterpenes on ex vivo transungual delivery of itraconazole for the management of onychomycosis. J. Cosmet. Dermatol. 2020, 19, 2745–2751. [Google Scholar] [CrossRef]
- Amaral, B.R.; Argenta, D.F.; Kroth, R.; Caon, T. Transbuccal delivery of benznidazole associated with monoterpenes: Permeation studies and mechanistic insights. Eur. J. Pharm. Sci. 2020, 143, 105177. [Google Scholar] [CrossRef]
- Ahmed, O.A.A.; Badr-Eldin, S.M. Development of an optimized avanafil-loaded invasomal transdermal film: Ex vivo skin permeation and in vivo evaluation. Int. J. Pharm. 2019, 570, 118657. [Google Scholar] [CrossRef]
- Verma, D.D.; Fahr, A. Synergistic penetration enhancement effect of ethanol and phospholipids on the topical delivery of Cyclosporin a. J. Control. Release 2004, 97, 55–66. [Google Scholar] [CrossRef]
- Babaie, S.; Del Bakhshayesh, A.R.; Ha, J.W.; Hamishehkar, H.; Kim, K.H. Invasome: A novel nanocarrier for transdermal drug delivery. Nanomaterials 2020, 10, 341. [Google Scholar] [CrossRef]
- Haque, T.; Talukder, M.M.U. Chemical enhancer: A simplistic way to modulate barrier function of the stratum corneum. Adv. Pharm. Bull. 2018, 8, 169–179. [Google Scholar] [CrossRef]
- Qadri, G.R.; Ahad, A.; Aqil, M.; Imam, S.S.; Ali, A. Invasomes of isradipine for enhanced transdermal delivery against hypertension: Formulation, characterization, and in vivo pharmacodynamic study. Artif. Cells Nanomed. Biotechnol. 2017, 45, 139–145. [Google Scholar] [CrossRef]
- Badran, M. Effect of terpene liposomes on the transdermal delivery of hydrophobic model drug, nimesulide: Characterization, stability and in vitro skin permeation. Afr. J. Pharm. Pharmacol. 2012, 6, 3018–3026. [Google Scholar] [CrossRef]
- Kalpana, B.; Lakshmi, P.K. Transdermal permeation enhancement of tolterodine tartrate through invasomes and iontophoresis. Der Pharm. Lett. 2013, 5, 119–126. [Google Scholar]
- Lee, M.K. Clinical usefulness of liposomal formulations in cancer therapy: Lessons from the experiences of doxorubicin. J. Pharm. Investig. 2019, 49, 203–214. [Google Scholar] [CrossRef]
- Large, D.E.; Abdelmessih, R.G.; Fink, E.A.; Auguste, D.T. Liposome composition in drug delivery design, synthesis, characterization, and clinical application. Adv. Drug Deliv. Rev. 2021, 176, 113851. [Google Scholar] [CrossRef] [PubMed]
- Torchilin, V.P. Recent approaches to intracellular delivery of drugs and DNA and organelle targeting. Annu. Rev. Biomed. Eng. 2006, 8, 343–375. [Google Scholar] [CrossRef]
- Brown, B.S.; Patanam, T.; Mobli, K.; Celia, C.; Zage, P.E.; Bean, A.J.; Tasciotti, E. Etoposide-loaded immunoliposomes as active targeting agents for GD2-positive malignancies. Cancer Biol. Ther. 2014, 15, 851–861. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Jain, S.K. Stimuli-responsive smart liposomes in cancer targeting. Curr. Drug Targets 2018, 19, 259–270. [Google Scholar] [CrossRef]
- Li, M.; Du, C.; Guo, N.; Teng, Y.; Meng, X.; Sun, H.; Li, S.; Yu, P.; Galons, H. Composition design and medical application of liposomes. Eur. J. Med. Chem. 2019, 164, 640–653. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.-Q.; Yang, X.; Wu, X.-F.; Fan, Y.-B. Enhancing permeation of drug molecules across the skin via delivery in nanocarriers: Novel strategies for effective transdermal applications. Front. Bioeng. Biotechnol. 2021, 9, 6554. [Google Scholar] [CrossRef]
- Hasan, M.; Khatun, A.; Fukuta, T.; Kogure, K. Noninvasive transdermal delivery of liposomes by weak electric current. Adv. Drug Deliv. Rev. 2020, 154–155, 227–235. [Google Scholar] [CrossRef]
- Zorec, B.; Zupančič, Š.; Kristl, J.; Pavšelj, N. Combinations of nanovesicles and physical methods for enhanced transdermal delivery of a model hydrophilic drug. Eur. J. Pharm. Biopharm. 2018, 127, 387–397. [Google Scholar] [CrossRef]
- Ramkanth, S.; Anitha, P.; Gayathri, R.; Mohan, S.; Babu, D. Formulation and design optimization of nano-transferosomes using pioglitazone and eprosartan mesylate for concomitant therapy against diabetes and hypertension. Eur. J. Pharm. Sci. 2021, 162, 105811. [Google Scholar] [CrossRef]
- De Lima, P.H.C.; Butera, A.P.; Cabeça, L.F.; Ribeiro-Viana, R.M. Liposome surface modification by phospholipid chemical reactions. Chem. Phys. Lipids 2021, 237, 5084. [Google Scholar] [CrossRef]
- Anselmo, A.C.; Mitragotri, S. An overview of clinical and commercial impact of drug delivery systems. J. Control. Release 2014, 190, 15–28. [Google Scholar] [CrossRef]


| Composition | Loaded Drug | Route of Administration | Ref. |
|---|---|---|---|
| Span 40, 60, 80; Tween 40, 60; cholesterol | Pentoxifylline | topical drug delivery | [129] |
| Span 60; cholesterol; sodium carboxymethylcellulose | Insulin | transdermal drug delivery | [130] |
| Span 60; Tween 80; Cremophor RH40; cholesterol | Simvastatin | transdermal drug delivery | [131] |
| Span 20, 40, 60; Tween 20, 40; cholesterol; Carbopol 934 | Timolol Maleate | ocular drug delivery | [132] |
| Span 40; Tween 40; cholesterol; hydrophobin-1 | Doxorubicin | parenteral drug delivery | [133] |
| Span 60; cholesterol | Bromocriptin Mesylate | nose-to-brain drug delivery | [134] |
| Span 60; cholesterol; dicetyl phosphate | Withaferin–A | intraperitoneally | [135] |
| Span 80, 60; Tween 80, 20; cholesterol | Ondansetron HCl | trans-mucosal nasal drug delivery | [136] |
| Tween 65; Span 60; cholesterol; dodecyl sulfate sodium | Gemcitabine, Cisplatin | aerosolized drug delivery | [137] |
| Span 60; cholesterol | Doxycycline | ocular drug delivery | [138] |
| Span 40; cholesterol; Carbopol 934 | Betaxolol | ocular drug delivery | [139] |
| Tween 20; cholesterol; chitosan; dicetyl phosphate | Pentamidine | nose-to-brain drug delivery | [140] |
| Span 60, 80; Tween 40, 80; cholesterol | Artemether | parenteral drug delivery | [141] |
| Span 20; cholesterol; dicetyl phosphate; ketorolacatromethamine | Natamycin | topical ocular drug delivery | [142] |
| Span 60; cholesterol; Cremophor RH40 | Quercetin | transdermal drug delivery | [143] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gaynanova, G.; Vasileva, L.; Kashapov, R.; Kuznetsova, D.; Kushnazarova, R.; Tyryshkina, A.; Vasilieva, E.; Petrov, K.; Zakharova, L.; Sinyashin, O. Self-Assembling Drug Formulations with Tunable Permeability and Biodegradability. Molecules 2021, 26, 6786. https://doi.org/10.3390/molecules26226786
Gaynanova G, Vasileva L, Kashapov R, Kuznetsova D, Kushnazarova R, Tyryshkina A, Vasilieva E, Petrov K, Zakharova L, Sinyashin O. Self-Assembling Drug Formulations with Tunable Permeability and Biodegradability. Molecules. 2021; 26(22):6786. https://doi.org/10.3390/molecules26226786
Chicago/Turabian StyleGaynanova, Gulnara, Leysan Vasileva, Ruslan Kashapov, Darya Kuznetsova, Rushana Kushnazarova, Anna Tyryshkina, Elmira Vasilieva, Konstantin Petrov, Lucia Zakharova, and Oleg Sinyashin. 2021. "Self-Assembling Drug Formulations with Tunable Permeability and Biodegradability" Molecules 26, no. 22: 6786. https://doi.org/10.3390/molecules26226786
APA StyleGaynanova, G., Vasileva, L., Kashapov, R., Kuznetsova, D., Kushnazarova, R., Tyryshkina, A., Vasilieva, E., Petrov, K., Zakharova, L., & Sinyashin, O. (2021). Self-Assembling Drug Formulations with Tunable Permeability and Biodegradability. Molecules, 26(22), 6786. https://doi.org/10.3390/molecules26226786






