Nanoemulsification Improves the Pharmaceutical Properties and Bioactivities of Niaouli Essential Oil (Melaleuca quinquenervia L.)
Abstract
1. Introduction
2. Results and Discussion
2.1. Pseudo-Ternary Phase Diagrams
2.2. Formulation Development
2.3. Characterization and Optimization of NEs
2.3.1. In Vitro Thermodynamic Stability Test
2.3.2. Droplet Diameter, Polydispersity Index (PDI), and Surface Charge Analysis
2.3.3. Rheology
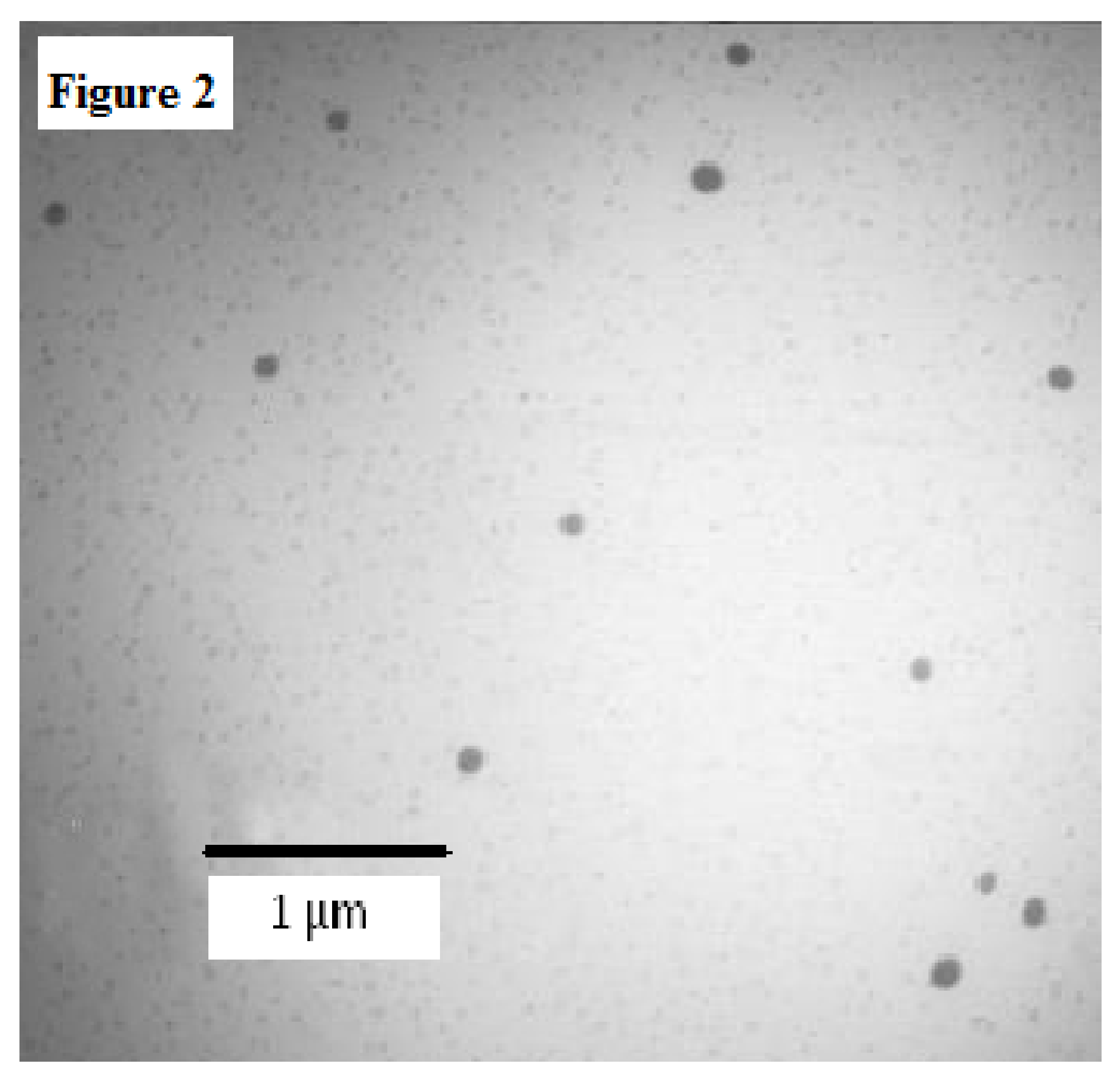
2.3.4. Transmission Electron Microscopy (TEM) Analysis
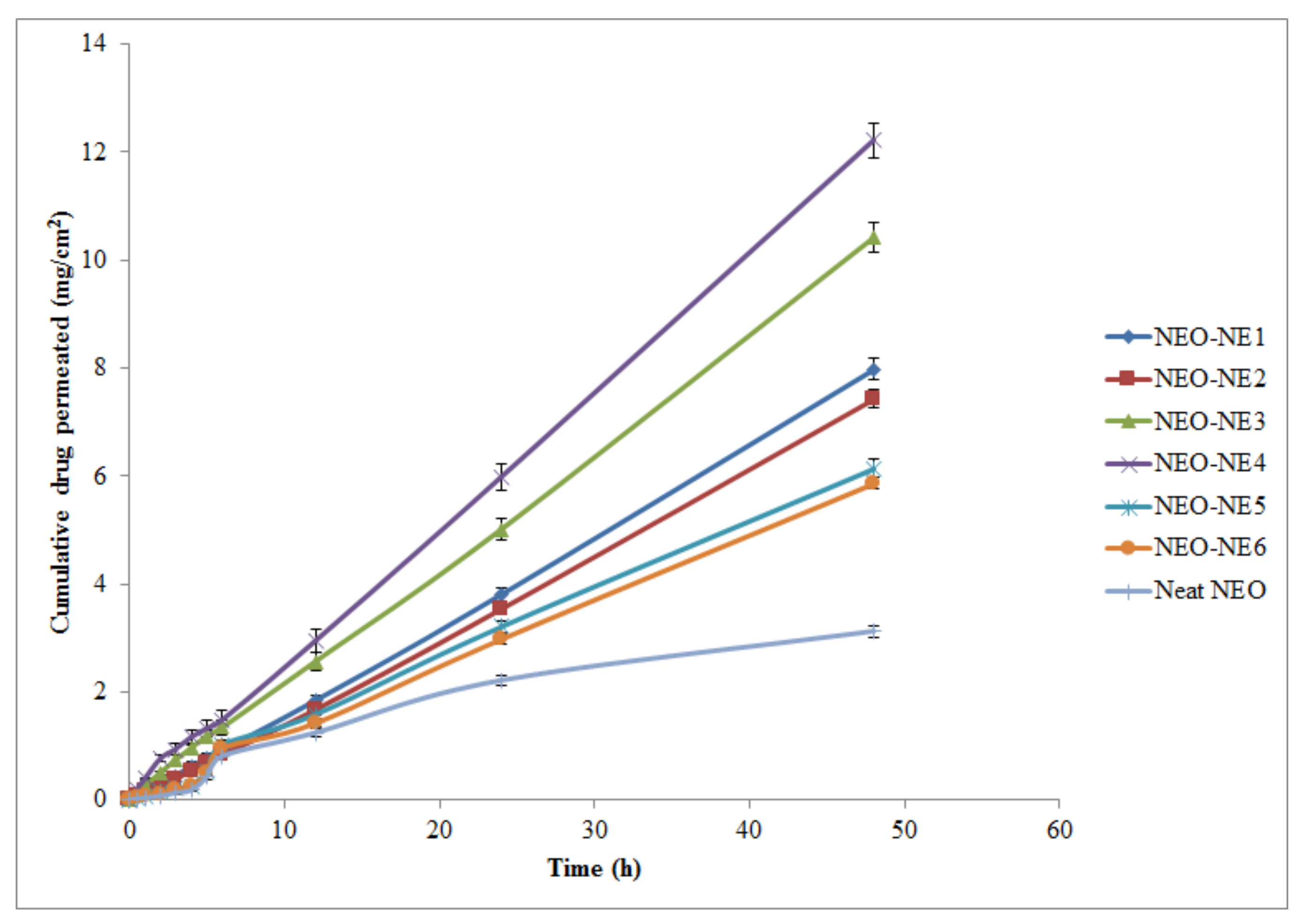
2.4. Ex Vivo Skin Permeation Studies
2.5. Colloidal Stability Evaluation
2.6. In Vitro Antiacne Study
3. Materials and Methods
3.1. Materials
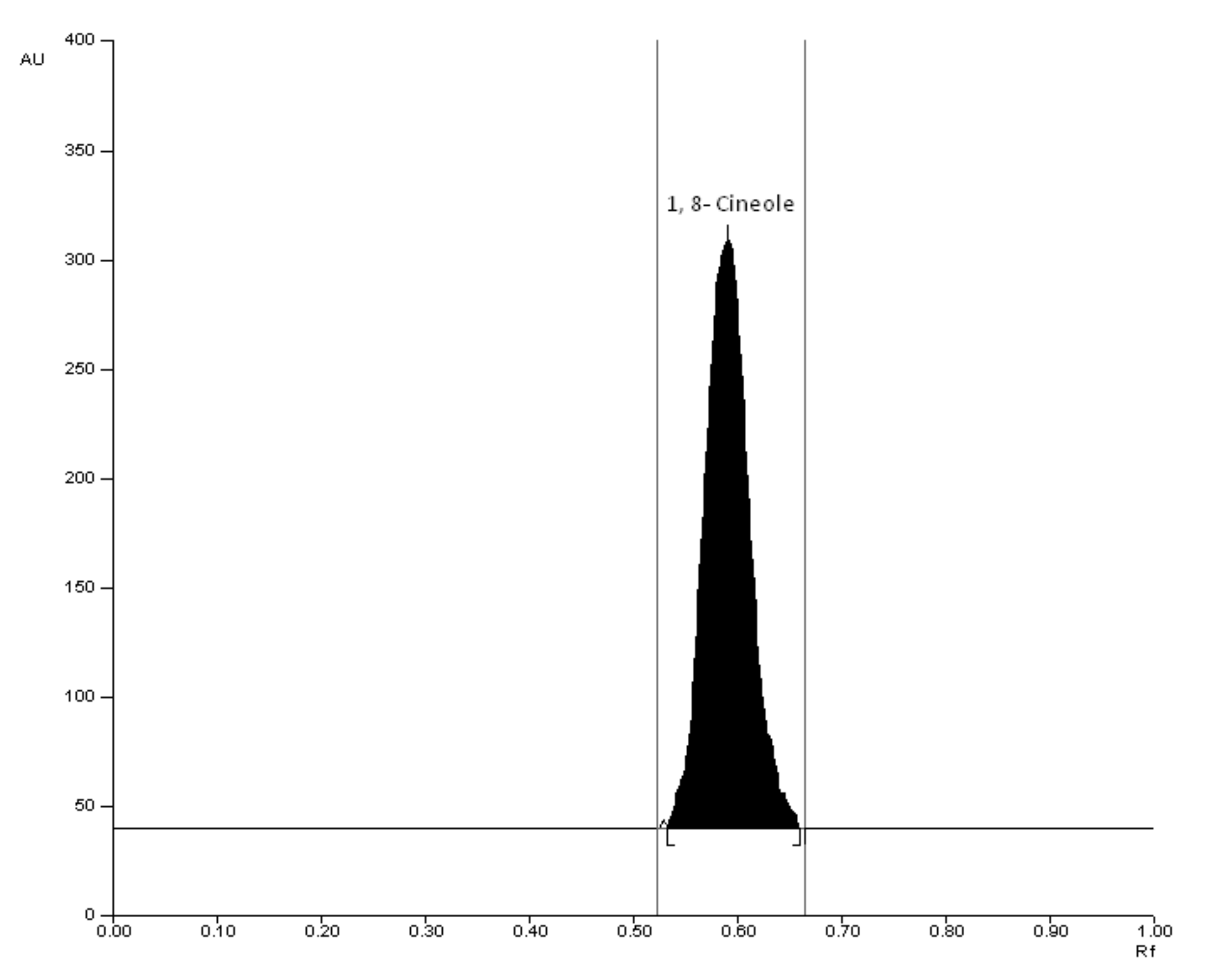
3.2. Analytical Methodology for the Analysis of NEO
3.3. Construction of Pseudo-Ternary Phase Diagrams
3.4. Formulation Development
3.5. Thermodynamic Stability Tests
3.6. Droplet diameter, PDI, and Surface Charge Analysis
3.7. Rheology
3.8. Refractive Index Determination
3.9. TEM Analysis
3.10. Ex Vivo Skin Permeation Studies
3.11. Colloidal Stability Evaluation
3.12. In Vitro Antiacne Study
3.13. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Sample Availability
References
- Ni, Z.J.; Wang, X.; Shen, Y.; Thakur, K.; Han, J.; Zhang, J.G.; Hu, F.; Wei, Z.J. Recent updates on the chemistry, bioactivities, mode of action, and industrial applications of plant essential oils. Trends Food Sci. Technol. 2021, 110, 78–89. [Google Scholar] [CrossRef]
- Shameen, J.B.; Mahomoodally, F.M.; Zengin, G.; Maggi, F. Essential oils as natural sources of fragrance compounds for cosmetics and cosmeceuticals. Molecules 2021, 26, 666. [Google Scholar] [CrossRef]
- Hellyer, R.O.; Lassak, E.V. The steam-volatile constituents of Melaleuca viridiflora Sol. ex Gaertn. Aust. J. Chem. 1968, 21, 2585–2587. [Google Scholar] [CrossRef][Green Version]
- Simsek, M.; Duman, R. Investigation of the effect of 1,8-cineole on antimicrobial activity of chlorhexidine gluconate. Pharmacogn. Res. 2017, 9, 234–237. [Google Scholar] [CrossRef]
- Mann, M.N.; Fisher, E.R. Investigation of antibacterial 1,8-cineole-derived thin films formed via plasma-enhanced chemical vapor deposition. ACS Appl. Mater. Interfaces 2017, 9, 36548–36560. [Google Scholar] [CrossRef]
- Lawrence, M.J.; Rees, G.D. Microemulsion based media as novel drug delivery systems. Adv. Drug Deliv. Rev. 2000, 45, 89–121. [Google Scholar] [CrossRef]
- El-Badry, M.; Fetih, G.; Shakeel, F. Comparative topical delivery of croconazole using liposome and micro-emulsion-based gel formulations. Drug Deliv. 2014, 21, 34–43. [Google Scholar] [CrossRef] [PubMed]
- Zakir, F.; Ahmad, A.; Farooq, U.; Mirza, M.A.; Tripathi, A.; Singh, D.; Shakeel, F.; Mohapatra, S.; Ahmad, F.J.; Kohli, K. Design and development of a commercially potential in situ nanoemulgel for the treatment of postmenopausal osteoporosis. Nanomed. 2020, 15, 1167–1187. [Google Scholar] [CrossRef] [PubMed]
- Altamimi, M.; Haq, N.; Alshehri, S.; Qamar, W.; Shakeel, F. Enhanced skin permeation of hydrocortisone using nanoemulsion as potential vehicle. ChemistrySelect 2019, 4, 10084–10091. [Google Scholar] [CrossRef]
- Shakeel, F.; Alam, P.; Anwer, M.K.; Alanazi, S.A.; Alsarra, I.A.; Alqarni, M.H. Wound healing evaluation of self-nanoemulsifying drug delivery system containing Piper cubeba essential oil. 3 Biotech. 2019, 9, E82. [Google Scholar] [CrossRef]
- Hussain, A.; Shakeel, F.; Singh, S.K.; Alsarra, I.A.; Faruk, A.; Alanazi, F.K.; Christoper, G.V.P. Solidified SNEDDS for the oral delivery of rifampicin: Evaluation, proof of concept, in vivo kinetics, and in silico GastroPlusTM simulation. Int. J. Pharm. 2019, 566, 203–217. [Google Scholar] [CrossRef] [PubMed]
- Faiyazuddin, M.; Baboota, S.; Ali, J.; Ahuja, A.; Ahmad, S. Characterization and in vitro bioactive studies of lemongrass oil phytonanoemulsion system in the treatment of acne vulgaris. Int. J. Essen. Oil Ther. 2009, 3, 13–21. [Google Scholar]
- Shakeel, F.; Shazly, G.A.; Raish, M.; Ahmad, A.; Kalam, M.A.; Ali, N.; Ansari, M.A.; Elosaily, G.M. Biological evaluation of a supersaturated self-nanoemulsifying drug delivery system of Piper cubeba essential oil. RSC Adv. 2015, 5, 105206–105217. [Google Scholar] [CrossRef]
- Alam, P.; Ansari, M.J.; Anwer, M.K.; Raish, M.; Kamal, Y.K.T.; Shakeel, F. Wound healing effects of nanoemulsion containing clove essential oil. Art Cells Nanomed. Biotechnol. 2017, 45, 591–597. [Google Scholar] [CrossRef]
- Alam, P.; Shakeel, F.; Anwer, M.K.; Foudah, A.I.; Alqarni, M.H. Wound healing study of eucalyptus essential oil containing nanoemulsion in rat model. J. Oleo Sci. 2018, 67, 957–968. [Google Scholar] [CrossRef]
- Bensouilah, J. Aetiology and management of acne vulgaris. Int. J. Aromather. 2002, 12, 99–104. [Google Scholar] [CrossRef]
- Holland, D.B.; Jeremy, A.H.T. The role of inflammation in the pathogenesis of acne and acne scarring. Sem. Cut. Med. Surg. 2005, 24, 79–83. [Google Scholar] [CrossRef]
- Monti, D.; Najarro, M.; Chetoni, P.; Burgalassi, S.; Saettone, M.F.; Boldrini, E. Niaouli oils as enhancer for transdermal permeation of estradiol evaluation of gel formulations on hairless rats in vivo. J. Drug Deliv. Sci. Technol. 2006, 16, 473–476. [Google Scholar] [CrossRef]
- Monti, D.; Tampucci, S.; Chetoni, P.; Burgalassi, S.; Bertoli, A.; Pistelli, L. Niaouli oils from different sources: Analysis and influence on cutaneous permeation of estradiol in vitro. Drug Deliv. 2009, 16, 237–242. [Google Scholar] [CrossRef] [PubMed]
- Myc, A.; Vanhecke, T.; Landers, J.J.; Hamouda, T.; Baker, J.R. The fungicidal activity of novel nanoemulsion (X8W60PC) against clinically important yeast and filamentous fungi. Mycopathol. 2001, 155, 195–201. [Google Scholar] [CrossRef] [PubMed]
- Flores, F.C.; de Lima, J.A.; Ribeiro, R.F.; Alves, S.H.; Rolim, C.M.M.; Beack, R.C.R.; da Silva, C.B. Antifungal activity of nanocapsule suspensions containing tea tree oil on the growth of Tricophyton rubrum. Mycopathologia 2013, 175, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Muta, T.; Parikh, A.; Kathawala, K.; Haidari, H.; Song, Y.; Thomas, J.; Garg, S. Quality-by-design approach for the development of tea tree oil formulation-impregnated biocompatible gel with antimicrobial properties. Pharmaceutics 2020, 12, 1091. [Google Scholar] [CrossRef]
- Wei, S.; Zhao, X.; Yu, J.; Yin, S.; Liu, M.; Bo, R.; Li, J. Characterization of tea tree oil nanoemulsion and its acute and subchronic toxicity. Reg. Toxicol. Pharmacol. 2021, 124, E104999. [Google Scholar] [CrossRef] [PubMed]
- Aziz, Z.A.A.; Nasir, H.M.; Ahmad, A.; Setapar, S.H.M.; Ahmad, H.; Noor, M.H.M.; Rafatullah, M.; Khatoon, A.; Kausar, M.A.; Ahmad, I.; et al. Enrichment of eucalyptus oil nanoemulsion by micellar nanotechnology: Transdermal analgesic activity using hot plate test in rats’ assay. Sci. Rep. 2019, 9, E13678. [Google Scholar] [CrossRef]
- Nirmala, M.J.; Durai, L.; Gopakumar, V.; Nagarajan, R. Preparation of celery essential oil-based nanoemulsion by ultrasonication and evaluation of its potential anticancer and antibacterial activity. Int. J. Nanomed. 2020, 15, 7651–7666. [Google Scholar] [CrossRef]
- Barradas, T.N.; Senna, J.P.; Cardoso, S.A.; Nicoli, S.; Padula, C.; Santi, P.; Rossi, F.; Silva, K.G.D.H.E.; Mansur, C.R.E. Hydrogel-thickened nanoemulsions based on essential oils for topical delivery of psoralen: Permeation and stability studies. Eur. J. Pharm. Biopharm. 2017, 116, 38–50. [Google Scholar] [CrossRef]
- Pathania, R.; Khan, H.; Kaushik, R.; Khan, M.A. Essential oil nanoemulsions and theier antimicrobial and food applications. Curr. Res. Nutr. Food Sci. 2018, 6, 626–643. [Google Scholar] [CrossRef]
- Faiyazuddin, M.; Akhtar, N.; Akhter, J.; Suri, S.; Shakeel, F.; Shafiq, S.; Mustafa, G. Production, characterization, in vitro and ex vivo studies of babchi oil-encapsulated nanostructure solid lipid carriers produced by a hot aqueous titration method. Pharmazie 2010, 65, 348–355. [Google Scholar] [PubMed]
- Danaei, M.; Dehghankhold, M.; Ataei, S.; Davarani, F.H.; Javanmard, R.; Dokhani, A.; Khorasani, S.; Mozafari, M.R. Impact of particle size and polydispersity index on the clinical applications of lipidic nanocarrier systems. Pharmaceutics 2018, 10, 57. [Google Scholar] [CrossRef] [PubMed]
- Shafiq, S.; Shakeel, F.; Talegaonkar, S.; Ahmad, F.J.; Khar, R.K.; Ali, M. Development and bioavailability assessment of ramipril nanoemulsion formulation. Eur. J. Pharm. Biopharm. 2007, 66, 227–243. [Google Scholar] [CrossRef]
- Craig, D.Q.M.; Barker, S.A.; Banning, D.; Booth, S.W. An investigation into the mechanisms of self-emulsification using particle size analysis and low frequency dielectric spectroscopy. Int. J. Pharm. 1995, 114, 103–110. [Google Scholar] [CrossRef]
- Freitas, C.; Muller, R.H. Effect of light and temperature on zeta potential and physical stability in solid lipid nanoparticle (SLN™) dispersions. Int. J. Pharm. 1998, 68, 221–229. [Google Scholar] [CrossRef]
- Shakeel, F.; Ramadan, W. Trnasdermal delivery of anticancer drug caffeine from water-in-oil nanoemulsions. Coll. Surface B. 2010, 75, 356–362. [Google Scholar] [CrossRef]
- Shakeel, F.; Haq, N.; Al-Dhfyan, A.; Alanazi, F.K.; Alsarra, I.A. Chemoprevention of skin cancer using low HLB surfactant nanoemulsion of 5-flourouracil: A preliminary study. Drug Deliv. 2015, 22, 573–580. [Google Scholar] [CrossRef]
- Shakeel, F.; Baboota, S.; Ahuja, A.; Ali, J.; Faisal, M.S.; Shafiq, S. Stability evaluation of celecoxib nanoemulsion containing Tween 80. Thai J. Pharm. Sci. 2008, 32, 4–9. [Google Scholar]
- Ali, M.S.; Alam, M.S.; Alam, N.; Anwer, T.; Safhi, M.M.A. Accelerated stability testing of a clobetasol propionate-loaded nanoemulsion as per ICH guidelines. Sci. Pharm. 2013, 81, 1089–1100. [Google Scholar] [CrossRef]
- Alam, M.S.; Ali, M.S.; Alam, M.I.; Anwer, T.; Safhi, M.M.A. Stability testing of beclamethasone dipropionate nanoemulsion. Trop. J. Pharm. Res. 2015, 14, 15–20. [Google Scholar] [CrossRef]
- Tucker, S.B.; Tausend, R.; Cochran, R.; Flannigan, S.A. Comparison of topical clindamycin phosphate, benzoyl peroxide, and a combination of the two for the treatment of acne vulgaris. Br. J. Dermatol. 1984, 110, 487–492. [Google Scholar] [CrossRef]
- Biju, S.S.; Ahuja, A.; Khar, R.K.; Chaudhry, R. Formulation and evaluation of an effective pH balanced topical antimicrobial product containing tea tree oil. Pharmazie 2005, 60, 208–211. [Google Scholar]
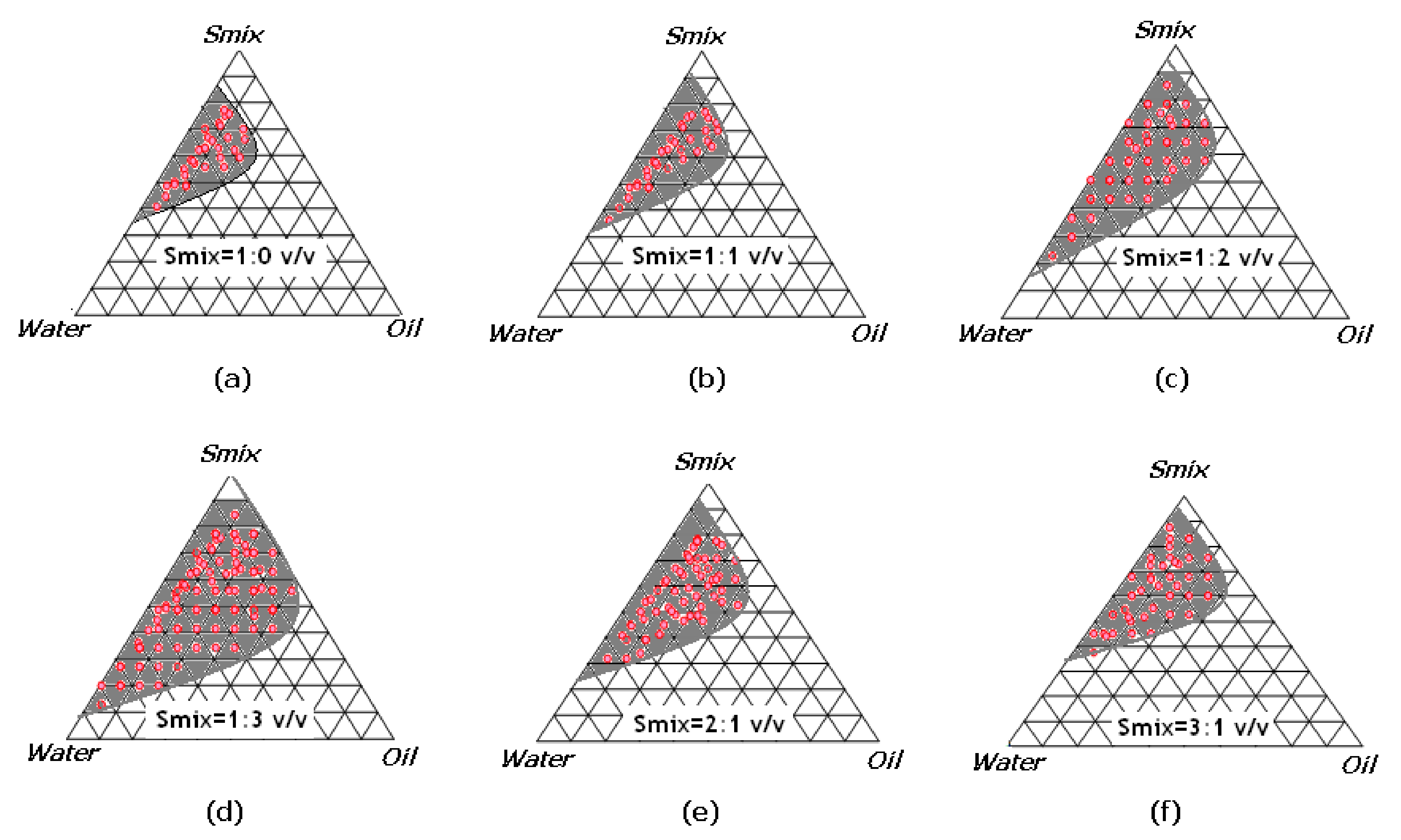
| Smix Ratio | Component (%) | Thermodynamic Stability Study | Inference | ||||
|---|---|---|---|---|---|---|---|
| Oil | Smix | Water | H/C | C/F | F/T | ||
| 1:0 (Figure 1a) | 10 | 46 | 44 | √ | √ | √ | P |
| 10 | 50 | 40 | √ | - | √ | F | |
| 12 | 53 | 35 | √ | √ | √ | P | |
| 12 | 55 | 33 | √ | - | - | F | |
| 15 | 57 | 28 | √ | - | - | F | |
| 1:1 (Figure 1b) | 10 | 36 | 54 | √ | √ | √ | P |
| 10 | 40 | 50 | √ | √ | √ | P | |
| 12 | 37 | 51 | √ | √ | √ | P | |
| 12 | 39 | 49 | √ | √ | √ | P | |
| 15 | 37 | 48 | - | - | - | F | |
| 1:2 (Figure 1c) | 10 | 41 | 49 | √ | √ | √ | P |
| 10 | 33 | 57 | √ | √ | √ | P | |
| 12 | 37 | 51 | √ | - | - | F | |
| 12 | 43 | 45 | √ | √ | √ | P | |
| 15 | 45 | 40 | - | √ | √ | F | |
| 1:3 (Figure 1d) | 10 | 36 | 54 | √ | - | √ | F |
| 10 | 31 | 59 | √ | √ | √ | P | |
| 12 | 41 | 49 | √ | √ | √ | P | |
| 12 | 43 | 47 | √ | √ | √ | P | |
| 15 | 44 | 41 | - | - | - | F | |
| 2:1 (Figure 1e) | 10 | 41 | 49 | √ | √ | √ | P |
| 10 | 46 | 44 | √ | √ | √ | P | |
| 12 | 51 | 37 | √ | √ | √ | P | |
| 12 | 49 | 39 | √ | √ | √ | P | |
| 15 | 40 | 45 | - | √ | √ | F | |
| 3:1 (Figure 1f) | 10 | 46 | 44 | √ | √ | √ | P |
| 10 | 49 | 41 | √ | √ | √ | P | |
| 12 | 53 | 35 | √ | √ | √ | P | |
| 12 | 48 | 40 | √ | √ | - | F | |
| 15 | 55 | 30 | √ | √ | X | F | |
| Code | Formulation Composition (% v/v) | Smix Combination | ||
|---|---|---|---|---|
| Oil Phase | Smix Phase | Water Phase | ||
| NEO-NE1 | 10 | 46 | 44 | 1:0 |
| NEO-NE2 | 10 | 36 | 54 | 1:1 |
| NEO-NE3 | 10 | 33 | 57 | 1:2 |
| NEO-NE4 | 10 | 31 | 59 | 1:3 |
| NEO-NE5 | 10 | 41 | 49 | 2:1 |
| NEO-NE6 | 10 | 46 | 44 | 3:1 |
| Formulation | Δdm # ± SD (nm) | ζ§ ± SD (mV) | PDI * | RI† ± SD | η$ ± SD (cps) |
|---|---|---|---|---|---|
| NEO-NE1 | 136.52 ± 4.08 | 29.28 ± 2.68 | 0.731 | 1.452 ± 0.005 | 134.94 ± 8.19 |
| NEO-NE2 | 138.61 ± 6.39 | 27.21 ± 1.98 | 0.648 | 1.460 ± 0.006 | 135.43 ± 7.41 |
| NEO-NE3 | 119.70 ± 4.71 | 30.57 ± 3.72 | 0.357 | 1.457 ± 0.008 | 128.52 ± 9.18 |
| NEO-NE4 | 95.86 ± 4.90 | 24.31 ± 4.81 | 0.252 | 1.453 ± 0.007 | 130.08 ± 6.87 |
| NEO-NE5 | 158.08 ± 3.54 | 28.60 ± 5.76 | 0.758 | 1.451 ± 0.010 | 143.44 ± 8.72 |
| NEO-NE6 | 162.41 ± 7.92 | 27.40 ± 3.91 | 0.819 | 1.468 ± 0.013 | 151.68 ± 6.07 |
| Matrices. | #Jss ± SD (mg/cm2/h) | †Kp ± SD (cm/h ×10−3) | ¶Er |
|---|---|---|---|
| * Neat NEO | 0.0698 ± 0.0012 | 1.442 ± 0.2101 | - |
| * NEO-NE1 | 0.1655 ± 0.0810 | 3.419 ± 0.2412 | 2.37 |
| * NEO-NE2 | 0.1546 ± 0.0720 | 3.194 ± 0.2234 | 2.21 |
| * NEO-NE3 | 0.2141 ± 0.0841 | 4.423 ± 0.3105 | 3.06 |
| * NEO-NE4 | 0.2507 ± 0.0910 | 5.179 ± 0.4104 | 3.59 |
| * NEO-NE5 | 0.1306 ± 0.0610 | 2.698 ± 0.2871 | 1.87 |
| * NEO-NE6 | 0.1245 ± 0.0501 | 2.572 ± 0.2152 | 1.78 |
| Formulation Matrices | T0 | 90th Day Sampling | ||
|---|---|---|---|---|
| Stability Chamber (40 ± 2 °C/75 ± 5% RH) ¶ | ||||
| Δdm ± SD (nm) | ζ ± SD (mV) | Δdm ± SD (nm) | ζ ± SD (Mv) | |
| NEO-NE1 | 136.52 ± 4.08 | 29.28 ± 2.68 | 151.22 ± 6.19 | 31.52 ± 4.96 |
| NEO-NE2 | 138.61 ± 6.39 | 27.21 ± 1.98 | 149.31 ± 5.23 | 32.46 ± 3.80 |
| NEO-NE3 | 119.70 ± 4.71 | 30.57 ± 3.72 | 127.57 ± 6.57 | 34.07 ± 2.47 |
| NEO-NE4 | 95.86 ± 4.90 | 24.31 ± 4.81 | 112.19 ± 5.78 | 27.46 ± 3.21 |
| NEO-NE5 | 158.08 ± 3.54 | 28.60 ± 5.76 | 173.44 ± 7.34 | 30.46 ± 3.48 |
| NEO-NE6 | 162.41 ± 7.92 | 27.40 ± 3.91 | 180.72 ± 6.55 | 31.65 ± 4.73 |
| Test Samples | Zone of Inhibition † (mm) ± SD | |
|---|---|---|
| S. epidermidis | P. acnes | |
| * Neat NEO (5% v/v in DMSO) | 7.3 ± 0.2 | 4.1 ± 0.4 |
| * Neat NEO (10% v/v in DMSO) | 9.8 ± 0.5 | 6.9 ± 0.5 |
| * Kolliphor EL | NA | NA |
| * Carbitol | 3.4 ± 0.7 | 2.2 ± 0.7 |
| * NEO-NE1 | 10.2 ± 0.5 | 7.1 ± 0.8 |
| * NEO-NE2 | 13.5 ± 0.6 | 9.6 ± 0.6 |
| * NEO-NE3 | 17.2 ± 0.6 | 11.8 ± 0.5 |
| * NEO-NE4 | 20.4 ± 1.5 | 12.2 ± 0.2 |
| * NEO-NE5 | 13.0 ± 0.3 | 7.5 ± 0.4 |
| * NEO-NE6 | 12.8 ± 0.6 | 7.0 ± 1.5 |
| Ingredients | Quantity Required for 1000 mL (g) |
|---|---|
| Protease peptone | 10.00 |
| Calf brain infusion | 200.00 |
| Sodium chloride | 5.00 |
| Dextrose | 2.00 |
| Beef heart infusion | 250.00 |
| Agar | 15.00 |
| Disodium phosphate | 2.50 |
| Human blood | 50.00 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shakeel, F.; Salem-Bekhit, M.M.; Haq, N.; Alshehri, S. Nanoemulsification Improves the Pharmaceutical Properties and Bioactivities of Niaouli Essential Oil (Melaleuca quinquenervia L.). Molecules 2021, 26, 4750. https://doi.org/10.3390/molecules26164750
Shakeel F, Salem-Bekhit MM, Haq N, Alshehri S. Nanoemulsification Improves the Pharmaceutical Properties and Bioactivities of Niaouli Essential Oil (Melaleuca quinquenervia L.). Molecules. 2021; 26(16):4750. https://doi.org/10.3390/molecules26164750
Chicago/Turabian StyleShakeel, Faiyaz, Mounir M. Salem-Bekhit, Nazrul Haq, and Sultan Alshehri. 2021. "Nanoemulsification Improves the Pharmaceutical Properties and Bioactivities of Niaouli Essential Oil (Melaleuca quinquenervia L.)" Molecules 26, no. 16: 4750. https://doi.org/10.3390/molecules26164750
APA StyleShakeel, F., Salem-Bekhit, M. M., Haq, N., & Alshehri, S. (2021). Nanoemulsification Improves the Pharmaceutical Properties and Bioactivities of Niaouli Essential Oil (Melaleuca quinquenervia L.). Molecules, 26(16), 4750. https://doi.org/10.3390/molecules26164750








