A Step-by-Step Guide for the Novel Radiometal Production for Medical Applications: Case Studies with 68Ga, 44Sc, 177Lu and 161Tb
Abstract
1. Introduction
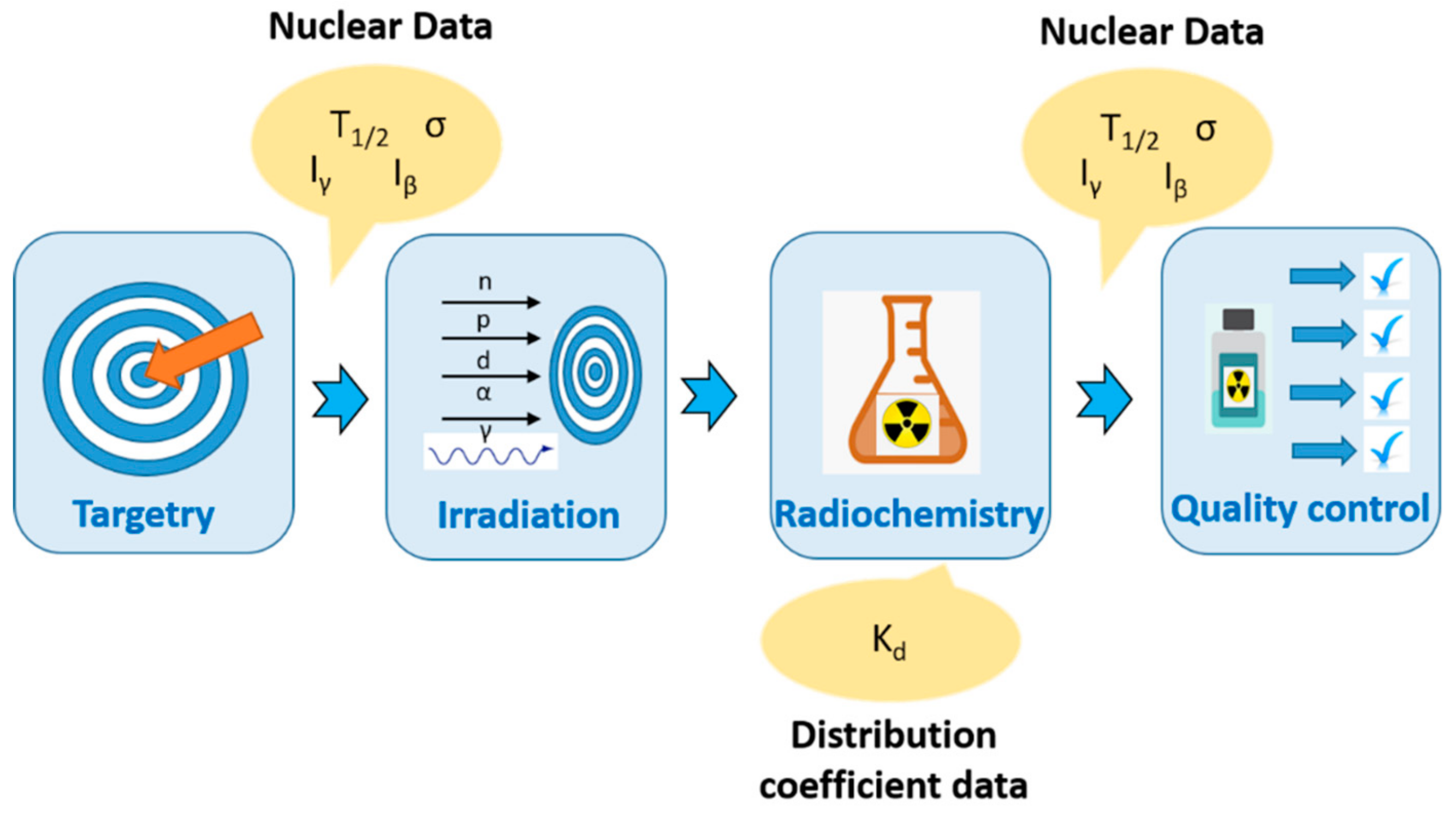
2. Radionuclide Production: A Step-by-Step Guide
- 1)
- Radiation characteristics such as the type(s) of decay emission(s), the energy of the emission(s), LET, physical half-life. If a gamma-ray photon is emitted in the decay process, its energy and branching ratio should be in the diagnostically useful range (dose received by the patients should be minimized, photon energy should be mostly less than 400 keV [38]). The physical half-life of the therapeutic radionuclides is extremely important for minimizing decay loss and provides logistical advantages for the shipment. Most of the novel radionuclides have relatively long half-lives, however, in some cases, due to their short half-life, irradiation facilities should be on-site.
- 2)
- The cost of the target material and stable long-term supply.
- 3)
- Availability of the facility (production capability and logistics).
- 4)
- A reasonable production cost.
- 5)
- The chemical separation method should be as simple as possible, for remote handling and to produce no-carrier-added (n.c.a.) products.
2.1. Targetry
2.1.1. Target Preparation for Cyclotrons
Solid Targets
Liquid Targets
2.1.2. Target Preparation for Reactors
2.2. Production
2.2.1. Cyclotrons
2.2.2. Nuclear Reactors
2.2.3. Alternative Production Routes
2.3. Radiochemistry
- 1)
- Adaptation of the separation using a remote/semi-automated operation system;
- 2)
- Separation processing time;
- 3)
- Product yield as a result of the separation process;
- 4)
- Recovery of enriched target material for recycling;
- 5)
- The chemical form of the final product;
- 6)
- Acidity and the volume of the final product;
- 7)
- Robustness and reproducibility of the process.
2.4. Quality Control of the Radionuclide for Preclinical Studies
2.5. Automation of the Labeling Procedure Towards GMP Production
- 1)
- appearance;
- 2)
- pH;
- 3)
- radiochemical purity/yield;
- 4)
- radionuclide identity/radionuclidic purity;
- 5)
- radioactivity concentration;
- 6)
- tracer identity/quantification;
- 7)
- molar activity;
- 8)
- chemical purity;
- 9)
- residual solvents;
- 10)
- bacterial endotoxins (BET);
- 11)
- sterility;
- 12)
- product stability;
- 1)
- the conjugate molecule;
- 2)
- the radionuclide;
- 3)
- a buffer to maintain pH;
- 4)
- a scavenging agent (such as ascorbic acid) to prevent radiolysis;
- 5)
- a quenching agent (such as EDTA) to complex any radionuclide that is not associated with the conjugate molecule;
- 6)
- diluent to formulate the preparation for administration to patients.
3. The Diagnostic Radionuclides 68Ga and 44Sc
3.1. Targetry/Production
3.1.1. 68. Ga Generator Production
3.1.2. 68. Ga Cyclotron Production
3.1.3. 44Sc Generator Production
3.1.4. 44. Sc Cyclotron Production
3.2. Radiochemistry
3.2.1. 68. Ge/68Ga Generator Production
3.2.2. 68. Ga Cyclotron Production
Recycling of 68Zn
3.2.3. 44. Sc Generator Production
3.2.4. 44. Sc Cyclotron Production
Recycling of 44Ca
3.3. Labeling Efficiency
3.3.1. 68. Ga
3.3.2. 44. Sc
3.4. Production for the Clinical Applications
3.4.1. 68. Ga
3.4.2. 44. Sc
4. Beta-Emitting Radionuclides: 161Tb and 177Lu
4.1. Targetry Production
4.1.1. 177Lu
Direct Method: Production of Carrier-Added (c.a.) 177Lu
Indirect Method: Production of No-Carrier-Added (n.c.a.) 177Lu
4.1.2. 161. Tb
4.2. Radiochemistry
4.2.1. 177. Lu
4.2.2. 161. Tb
4.3. Labeling Efficiency
4.4. Production for the Clinical Applications
4.4.1. 177. Lu
4.4.2. 161. Tb
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- European Commission. Supply of medical isotopes. Available online: https://ec.europa.eu/euratom/observatory_radioisotopes.html (accessed on 30 January 2020).
- Fior Markets, Global Radiopharmaceuticals/Nuclear Market by Type (Diagnostic, Therapeutic), procedure, Application, End User, Region, Global Industry Analysis, Market Size, Share, Growth, Trends, and Forecast 2018 to 2025. Available online: https://www.fiormarkets.com/report/global-radiopharmaceuticals-nuclear-market-by-type-diagnostic-therapeutic-procedure-376060.html (accessed on 30 January 2020).
- Ku, A.; Facca, V.J.; Cai, Z.; Reilly, R.M. Auger electrons for cancer therapy–a review. EJNMMI Radiopharma. Chem. 2019, 4, 1–36. [Google Scholar] [CrossRef] [PubMed]
- Kassis, A.I. Cancer Therapy with Auger Electrons: Are We Almost There ? J. Nucl. Med. 2003, 44, 1479–1482. [Google Scholar] [PubMed]
- Howell, R.W. Auger processes in the 21st century. Int. J. Radiat. Biol. 2008, 84, 959–975. [Google Scholar] [CrossRef] [PubMed]
- Kassis, A.I. Molecular and cellular radiobiological effects of Auger emitting radionuclides. Radiat. Prot. Dosimetry 2011, 143, 241–247. [Google Scholar] [CrossRef]
- Kassis, A.I. The amazing world of Auger electrons. Int. J. Radiat. Biol. 2004, 80, 789–803. [Google Scholar] [CrossRef]
- Ahmadzadehfar, H.; Eppard, E.; Kürpig, S.; Fimmers, R.; Yordanova, A.; Schlenkhoff, C.D.; Gärtner, F.; Rogenhofer, S.; Essler, M. Therapeutic response and side effects of repeated radioligand therapy with 177Lu-PSMA-DKFZ-617 of castrate-resistant metastatic prostate cancer. Oncotarget 2016, 7, 12477–12488. [Google Scholar] [CrossRef]
- Rahbar, K.; Ahmadzadehfar, H.; Kratochwil, C.; Haberkorn, U.; Sch, M.; Essler, M.; Baum, R.P.; Kulkarni, H.R.; Schmidt, M.; Drzezga, A.; et al. German Multicenter Study Investigating 177Lu-PSMA-617 Radioligand Therapy in Advanced Prostate Cancer. J. Nucl. Med. 2017, 58, 85–90. [Google Scholar] [CrossRef]
- Baum, R.P.; Kulkarni, H.R.; Schuchardt, C.; Singh, A.; Wirtz, M.; Wiessalla, S.; Schottelius, M.; Mueller, D.; Klette, I.; Wester, H.J. 177Lu-labeled prostate-specific membrane antigen radioligand therapy of metastatic castration-resistant prostate cancer: Safety and efficacy. J. Nucl. Med. 2016, 57, 1006–1013. [Google Scholar] [CrossRef]
- Pfeifer, A.K.; Gregersen, T.; Gronbaek, H.; Hansen, C.; Brand, J.M.; Bruun, K.H.; Krogh, K.; Kjaer, A.; Knigge, U. Peptide Receptor Radionuclide Therapy with Y-DOTATOC and 177Lu-DOTATOC in Advanced Neuroendocrine Tumors: Results from a Danish Cohort Treated in Switzerland. Neuroendocrinology 2011, 93, 189–196. [Google Scholar] [CrossRef]
- Mantry, P.S.; Mehta, A.; Madani, B.; Mejia, A.; Shahin, I. Selective internal radiation therapy using yttrium-90 resin microspheres in patients with unresectable hepatocellular carcinoma: A retrospective study. J. Gastrointest. Oncol. 2017, 8, 799–807. [Google Scholar] [CrossRef]
- Furubayashi, N.; Negishi, T.; Ura, S.; Hirai, Y.; Nakamura, M. Palliative effects and adverse events of strontium-89 for prostate cancer patients with bone metastasis. Mol. Clin. Oncol. 2015, 3, 257–263. [Google Scholar] [CrossRef] [PubMed]
- Yamada, K.; Yoshimura, M.; Kaise, H.; Ogata, A.; Ueda, N.; Tokuuye, K.; Kohno, N. Concurrent use of Sr-89 chloride with zoledronic acid is safe and effective for breast cancer patients with painful bone metastases. Exp. Ther. Med. 2012, 3, 226–230. [Google Scholar] [CrossRef] [PubMed]
- Dionisi, V.; Bellarosa, C.; Cardano, R.; Rizzini, E.L.; Ghedini, P.; Morganti, A.G.; Fanti, S.; Monari, F. Use of Radium-223 Dichloride in Patients With Osteonecrosis of the Jaw Induced by Zoledronic Acid: Report of 2 Cases. Clin. Genitourin. Cancer 2019, 17, e612–e617. [Google Scholar] [CrossRef] [PubMed]
- Den, R.B.; George, D.; Pieczonka, C.; McNamara, M. Ra-223 treatment for bone metastases in castrate-resistant prostate cancer: Practical management issues for patient selection. Am. J. Clin. Oncol. Cancer Clin. Trials 2019, 42, 399–406. [Google Scholar] [CrossRef] [PubMed]
- Carroll, P.R. NCCN Guidelines Insights Prostate cancer early detection, version 2.2016. J. Nat. Compr. Canc. Netw. 2016, 14, 509–519. [Google Scholar] [CrossRef] [PubMed]
- Kratochwil, C.; Fendler, W.; Eiber, M.; Baum, R.; Bozkurt, M.F.; Czernin, J.; Bolton, R.C.D.; Ezziddin, S.; Forrer, F.; Hicks, R.J. EANM procedure guidelines for radionuclide therapy with 177Lu-labelled PSMA-ligands ( 177Lu-PSMA-RLT ). Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 2536–2544. [Google Scholar] [CrossRef]
- Kuznetsov, R.A.; Bobrovskaya, K.S.; Svetukhin, V.V.; Fomin, A.N.; Zhukov, A. V Production of Lutetium-177: Process Aspects. Radiochemistry 2019, 61, 381–395. [Google Scholar] [CrossRef]
- Dash, A. Production of 177Lu for Targeted Radionuclide Therapy: Available Options. Nucl. Med. Mol Imaging 2015, 49, 85–107. [Google Scholar] [CrossRef]
- European Medicines Agency, EndolucinBeta International. Available online: https://www.ema.europa.eu/en/medicines/human/EPAR/endolucinbeta (accessed on 30 January 2020).
- NuDat 2.8, Decay radiation search. Available online: https://www.nndc.bnl.gov/nudat2/ (accessed on 30 January 2020).
- Hindie, E.; Zanotti-Fregonara, P.; Quinto, M.A.; Morgat, C.; Champion, C. Dose Deposits from 90Y, 177Lu, 111In, and 161Tb in Micrometastases of Various Sizes: Implications for Radiopharmaceutical Therapy. J. Nucl. Med. 2016, 57, 759–764. [Google Scholar] [CrossRef]
- Champion, C.; Quinto, M.A.; Morgat, C.; Zanotti-fregonara, P.; Hindié, E. Comparison between Three Promising ß-emitting Radionuclides, 67Cu, 47Sc and 161Tb, with Emphasis on Doses Delivered to Minimal Residual Disease. Theranostics 2016, 6, 1611–1618. [Google Scholar] [CrossRef]
- Müller, C.; Reber, J.; Haller, S.; Dorrer, H.; Bernhardt, P.; Zhernosekov, K.; Türler, A.; Schibli, R. Direct in vitro and in vivo comparison of 161Tb and 177Lu using a tumour-targeting folate conjugate. Eur J. Nucl. Med. Mol Imaging 2014, 41, 476–485. [Google Scholar] [CrossRef] [PubMed]
- Müller, C.; Umbricht, C.A.; Gracheva, N.; Tschan, V.J.; Pellegrini, G.; Bernhardt, P.; Zeevaart, J.R.; Köster, U.; Schibli, R.; Meulen, N.P. Van Der Terbium-161 for PSMA-targeted radionuclide therapy of prostate cancer. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 1919–1930. [Google Scholar] [CrossRef] [PubMed]
- Grünberg, J.; Lindenblatt, D.; Dorrer, H.; Cohrs, S.; Zhernosekov, K.; Köster, U. Anti-L1CAM radioimmunotherapy is more effective with the radiolanthanide terbium-161 compared to lutetium-177 in an ovarian cancer model. Eur J. Nucl. Med. Mol Imaging 2014, 41, 1907–1915. [Google Scholar] [CrossRef] [PubMed]
- Marin, I.; Ryden, T.; van Essen, M.; Svensson, J.; van der Meulen, N.P.; Gracheva, N.; Müller, C. Establishment of optimized SPECT/CT protocol for therapy with 161Tb demonstrate improved image quality with Monte Carlo based OSEM reconstruction. Eur J. Nucl. Med. Mol Imaging 2018, 45, S16. [Google Scholar]
- Müller, C.; Domnanich, K.A.; Umricht, C.A.; Van der Meulen, N. Theranostics and precision medicine special feature: Review Article Scandium and terbium radionuclides for radiotheranostics: Current state of development towards clinical application. Br. J. Radiol 2018, 91, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Qaim, S.M.; Scholten, B.; Neumaier, B. New developments in the production of theranostic pairs of radionuclides. J. Radioanal. Nucl. Chem. 2018, 318, 1493–1509. [Google Scholar] [CrossRef]
- Domnanich, K.A.; Müller, C.; Benešová, M.; Dressler, R.; Haller, S.; Köster, U.; Ponsard, B.; Schibli, R.; Türler, A.; van der Meulen, N.P. 47Sc as useful β–-emitter for the radiotheragnostic paradigm: A comparative study of feasible production routes. EJNMMI Radiopharm. Chem. 2017, 2, 1–17. [Google Scholar] [CrossRef]
- Müller, C.; Bunka, M.; Haller, S.; Köster, U.; Groehn, V.; Bernhardt, P.; Van Der Meulen, N.; Türler, A.; Schibli, R. Promising prospects for 44Sc-/47Sc-based theragnostics: Application of 47Sc for radionuclide tumor therapy in mice. J. Nucl. Med. 2014, 55, 1658–1664. [Google Scholar] [CrossRef]
- Siwowska, K.; Guzik, P.; Domnanich, K.A.; Rodríguez, J.M.M.; Bernhardt, P.; Ponsard, B.; Hasler, R.; Borgna, F.; Schibli, R.; Köster, U.; et al. Therapeutic potential of 47Sc in comparison to 177Lu and 90Y: Preclinical investigations. Pharmaceutics 2019, 11, 424. [Google Scholar] [CrossRef]
- Umbricht, C.A.; Benesova, M.; Schmid, R.M.; Türler, A.; Schibli, R.; van der Meulen, N.P.; Müller, C. Sc-PSMA-617 for radiotheragnostics in tandem with 177Lu-PSMA-617 — preclinical investigations in comparison with. EJNMMI Res. 2017, 7, 1–10. [Google Scholar] [CrossRef]
- Eppard, E.; de Fuente, A.; Benešová, M.; Khawar, A.; Bundschuh, R.A.; Gärtner, C.; Kreppel, B.; Kopka, K.; Essler, M.; Rösch, F. Clinical Translation and First In-Human Use of [ 44Sc ] Sc-PSMA-617 for PET Imaging of Metastasized Castrate-Resistant Prostate Cancer. Theranostics 2017, 7, 4359–4369. [Google Scholar] [CrossRef] [PubMed]
- Bunka, M.; Müller, C.; Vermeulen, C.; Haller, S.; Türler, A.; Schibli, R.; Meulen, N.P. van der Imaging quality of 44Sc in comparison with five other PET radionuclides using Derenzo phantoms and preclinical PET. Appl. Radiat. Isot. 2016, 110, 129–133. [Google Scholar] [CrossRef] [PubMed]
- García-Toraño, E.; Peyrés, V.; Roteta, M.; Sánchez-Cabezudo, A.I.; Romero, E.; Martínez Ortega, A. Standardization and precise determination of the half-life of 44Sc. Appl. Radiat. Isot. 2016, 115, 313. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.H.; Chen, J.C. Investigation of attenuation correction for small-animal single photon emission computed tomography. Comput. Math. Methods Med. 2013, 2013, 1–13. [Google Scholar] [CrossRef]
- Stolarz, A. Target preparation for research with charged projectiles. J. Radioanal Nucl. Chem 2014, 299, 913–931. [Google Scholar] [CrossRef]
- Skliarova, H.; Cisternino, S.; Cicoria, G.; Marengo, M.; Cazzola, E.; Gorgoni, G.; Palmieri, V. Medical Cyclotron Solid Target Preparation by Ultrathick Film Magnetron Sputtering Deposition. Instruments 2019, 3, 21. [Google Scholar] [CrossRef]
- SRIM. Stopping and Range of Ions in matter. Available online: http://www.srim.org/ (accessed on 30 January 2020).
- Alves, V.; do Carmo, S.; Alves, F.; Abrunhosa, A. Automated Purification of Radiometals Produced by Liquid Targets. Instruments 2018, 2, 17. [Google Scholar] [CrossRef]
- Do Carmo, S.J.C.; Scott, P.J.H.; Alves, F. Production of radiometals in liquid targets. EJNMMI Radiopharm. Chem. 2020, 5, 1–21. [Google Scholar] [CrossRef]
- Pandey, M.K.; Engelbrecht, H.P.; Byrne, J.P.; Packard, A.B.; DeGrado, T.R. Production of 89Zr via the 89Y(p,n)89Zr reaction in aqueous solution: Effect of solution composition on in-target chemistry. Nucl. Med. Biol. 2014, 41, 309–316. [Google Scholar] [CrossRef]
- Pawlak, D.; Parus, J.L.; Sasinowska, I.; Mikolajczak, R. Determination of elemental and radionuclidic impurities in 177Lu used for labeling of radiopharmaceuticals. J. Radioanal. Nucl. Chem. 2004, 261, 469–472. [Google Scholar] [CrossRef]
- Qaim, S.M. Nuclear data for production and medical application of radionuclides: Present status and future needs. Nucl. Med. Biol. 2017, 44, 31–49. [Google Scholar] [CrossRef] [PubMed]
- Tarkanyi, F.; Hermanne, A.; Ditroi, F.; Csikai, J.; Ignatyuk, A.V. Cross-section measurement of some deuteron induced reactions on 160Gd for possible production of the therapeutic radionuclide 161Tb. J. Radioanal Nucl Chem 2013, 298, 1385–1392. [Google Scholar] [CrossRef]
- Engle, J.W.; Ignatyuk, A.V.; Capote, R.; Carlson, B.V.; Hermanne, A.; Kellett, M.A.; Kib, T. Recommended Nuclear Data for the Production of Selected Therapeutic Radionuclides. Nucl. Data Sheets 2019, 155, 56–74. [Google Scholar] [CrossRef]
- Tarkanyi, F.T.; Ignatyuk, A.V.; Hermanne, A.; Capote, R.; Carlson, B.V.; Engle, J.W.; Kellett, M.; Kibedi, M.; Kondev, G.; Lebeda, M.; et al. Recommended nuclear data for medical radioisotope production: Diagnostic gamma emitters. J. Radioanal. Nucl. Chem. 2019, 319, 487–531. [Google Scholar] [CrossRef]
- Tarkanyi, F.T.; Ignatyuk, A.V.; Hermanne, A.; Engle, J.W.; Kellett, M.A.; Kibedi, T.; Kim, G.; Kondev, F.; Lebeda, O.; Verpelli, M. Recommended nuclear data for medical radioisotope production: Diagnostic positron emitters. J. Radioanal. Nucl. Chem. 2019, 319, 533–666. [Google Scholar] [CrossRef]
- Sajjad, M.; Lambrecht, M. Cyclotron targetry for medical radioisotope production. Nucl. Instruments Methods Phys. Res. B 1989, 41, 1100–1104. [Google Scholar] [CrossRef]
- Otuka, N.; Takács, S. Definitions of radioisotope thick target yields. Radiochim. Acta 2015, 103, 1–6. [Google Scholar] [CrossRef]
- Goethals, P.E.; Zimmermann, R. Cyclotrons used in Nuclear Medicine World Market. Report Directory. 2015. Available online: http://medraysintell.com/attachments/File/MEDraysintell_Cyclotron_Edition_2015_-_Summary_and_TOC.pdf (accessed on 30 January 2020).
- van der Meulen, N.P.; Eichler, R.; Grundler, P.V.; Hasler, R.; Hirzel, W.; Joray, S.; Kiselev, D.C.; Sommerhalder, A.; Talip, Z.; Zhang, H.; et al. The use of PSI’s IP2 beam line towards exotic radionuclide development and its application towards proof-of-principle preclinicaland clinical studies. In Proceedings of the 22th International Conference on Cyclotrons and their Applications, National Reseach Foundation, Cape Town, South Africa, 22–27 September 2019; p. 24. [Google Scholar]
- IAEA. Research Reactor Database. Available online: https://nucleus.iaea.org/RRDB/Content/Util/IsoTopes.aspx (accessed on 30 January 2020).
- Krijger, G.C.; Ponsard, B.; Harfensteller, M.; Wolterbeek, H.T.; Nijsen, J.W.F. The necessity of nuclear reactors for targeted radionuclide therapies. Trends Biotechnol. 2013, 31, 390–396. [Google Scholar] [CrossRef]
- Fedosseev, V.; Marsh, B.; Fedorov, D.V.; Koester, U. Ionization scheme development at the ISOLDE MLIS. Hyperfine Interact. 2005, 3, 1–13. [Google Scholar]
- Fedosseev, V.; Chrysalidis, K.; Goodacre, T.D.; Marsh, B.; Rothe, S.; Seiffert, C.; Wendt, K. Ion beam production and study of radioactive isotopes with the laser ion source at ISOLDE Ion. J. Phys. G Nucl. Part. Phys. 2017, 44, 1–26. [Google Scholar] [CrossRef]
- Santos Augusto, R.; Stora, T.; Buehler, L.; Lawson, Z.; Marzari, S.; Stachura, M.; Stora, T.; Collaboration, C.-M. CERN-MEDICIS (Medical Isotopes Collected from ISOLDE): A New Facility. Appl. Sci. 2014, 4, 265–281. [Google Scholar] [CrossRef]
- Gadelshin, V.; Cocolios, T.; Fedoseev, V.; Heinke, R.; Kieck, T.; March, B.; Naubereit, P.; Rothe, S.; Stora, T.; Studer, D.; et al. Laser resonance ionization spectroscopy on lutetium for the MEDICIS project. Hyperfine Interact. 2017, 238, 1–7. [Google Scholar] [CrossRef]
- Köster, U.; Assmann, W.; Bacri, C.; Faestermann, T.; Garrett, P.; Gernhäuser, R.; Tomandl, I. Electromagnetic isotope separation of gadolinium isotopes for the production of 152,155Tb for radiopharmaceutical applications. Nucl. Inst. Methods Phys. Res. B 2020, 463, 111–114. [Google Scholar] [CrossRef]
- Hoehr, C.; Bénard, F.; Buckley, K.; Crawford, J.; Gottberg, A.; Hanemaayer, V. Medical isotope production at TRIUMF – from imaging to treatment. Phys. Procedia 2017, 90, 200–208. [Google Scholar] [CrossRef]
- Baeten, P.; Schyns, M.; Fernandez, R.; de Bruyn, D.; Eynde, G. Van Den MYRRHA: A multipurpose nuclear research facility. In Proceedings of the EPJ Web of Conferences, Rhodes, Greece, 25–30 August 2013; EDP Sciences: Les Ulis, France, 2014; pp. 1–7. [Google Scholar]
- Formento-Cavaier, R.; Köster, U.; Crepieux, B.; Gadelshin, V.M.; Haddad, F.; Stora, T.; Wendt, K. Very high specific activity erbium 169Er production for potential receptor-targeted radiotherapy. Nucl. Instruments Methods Phys. Res. Sect. B Beam Interact. Mater. Atoms 2019, 463, 468–471. [Google Scholar] [CrossRef]
- Starovoitova, V.N.; Tchelidze, L.; Wells, D.P. Production of medical radioisotopes with linear accelerators. Appl. Radiat. Isot. 2014, 85, 39–44. [Google Scholar] [CrossRef]
- Jang, J.; Yamamoto, M.; Uesaka, M. Design of an X-band electron linear accelerator dedicated to decentralized 99Mo/99mTc supply: From beam energy selection to yield estimation. Phys. Rev. Accel. Beams 2017, 20, 104701–104709. [Google Scholar] [CrossRef]
- Jones, S.; JR Robinson, G.D.; Mcintyre, E. Tandem Van de Graaff Accelerator Production of Positron Labeled Radiopharmaceuticals for Routine Clinical Use. Int. J. Appl. Rdiat. Hot. Vol. 1984, 35, 721–729. [Google Scholar] [CrossRef]
- Bychenkov, V.Y.; Brantov, A.V.; Mourou, G. Tc-99m production with ultrashort intense laser pulses. Laser Part. Beams 2014, 32, 605–611. [Google Scholar] [CrossRef]
- Ledingham, K.; Mckenna, P.; Mccanny, T. High power laser production of short-lived isotopes for positron emission tomography. J. Phys. D Appl. Phys. 2004, 37, 2341–2345. [Google Scholar] [CrossRef]
- Lefebvre, E.D.; Humiere, E.; Fritzler, S.; Malka, V. Numerical simulation of isotope production for positron emission tomography with laser- accelerated ions. J. Appl. Phys. 2006, 100, 113308–113318. [Google Scholar] [CrossRef]
- Klug, J.; Buckley, K.R.; Zeisler, S.K.; Dodd, M.; Tsao, P.; Hoehr, C.; Economou, C.; Corsaut, J.; Appiah, J.P.; Kovacs, M.S.; et al. A New Transfer System for Solid Targets. In Proceedings of the 14th International Workshop on Targetry and Target Chemistry, Playa Del Carmen, Mexico, 26–29 August 2012; Volume 1509, pp. 146–151. [Google Scholar]
- Coenen, H.H.; Gee, A.D.; Adam, M.; Antoni, G.; Cutler, C.S.; Fujibayashi, Y.; Min, J.; Mach, R.H.; Mindt, T.L.; Pike, V.W.; et al. Consensus nomenclature rules for radiopharmaceutical chemistry — Setting the record straight. Nucl. Med. Biol. 2017, 55, 5–11. [Google Scholar] [CrossRef] [PubMed]
- International Atomic Energy Agency. Quality Assurance for Radioactivity Measurement in Nuclear Medicine; Technical report series no. 454; IAEA: Vienna, Austria, 2006; p. 81. [Google Scholar]
- Carey, J.E.; Byrne, P.; De, W.L.; Lieto, R. The Selection, Use, Calibration, and Quality Assurance of Radionuclide Calibrators Used in Nuclear Medicine; Report No: 181; Americal Association of Physicists in Medicine: Alexandria, VA, USA, 2012; p. 38. [Google Scholar]
- Council of Europe, European Pharmacopoeia. Available online: https://www.edqm.eu/en/european-pharmacopoeia-ph-eur-9th-edition (accessed on 30 January 2020).
- Bauwens, M.; Pooters, I.; Cobben, R.; Visser, M.; Schnerr, R.; Mottaghy, F.; Wildberger, J.; Wierts, R. A comparison of four radionuclide dose calibrators using various radionuclides and measurement geometries clinically used in nuclear medicine. Phys. Medica 2019, 60, 14–21. [Google Scholar] [CrossRef] [PubMed]
- Bochud, F.O.; Laedermann, J.P.; Baechler, S.; Kosinski, M.; Bailat, C.J. Usefulness of specific calibration coefficients for gamma-emitting sources measured by radionuclide calibrators in nuclear medicine. Med. Phys. 2011, 38, 4073–4080. [Google Scholar] [CrossRef]
- Breeman, W.A.P.; de Jong, M.; Visser, T.J.; Erion, J.L.; Krenning, E.P. Occasional survey Optimising conditions for radiolabelling of DOTA-peptides with 90Y, 111In and 177Lu at high specific activities. Eur J. Nucl Med. Mol Imaging 2003, 30, 917–920. [Google Scholar] [CrossRef]
- Asti, M.; Tegoni, M.; Farioli, D.; Iori, M.; Guidotti, C.; Cutler, C.S.; Mayer, P.; Versari, A.; Salvo, D. Influence of cations on the complexation yield of DOTATATE with yttrium and lutetium: A perspective study for enhancing the 90Y and Lu labeling conditions. Nucl. Med. Biol. 2012, 39, 509–517. [Google Scholar] [CrossRef]
- Chakravarty, R.; Chakraborty, S.; Dash, A.; Pillai, M.R.A. Detailed evaluation on the effect of metal ion impurities on complexation of generator eluted 68Ga with different bifunctional chelators. Nucl. Med. Biol. 2013, 40, 197–205. [Google Scholar] [CrossRef]
- Eppard, E.; Pèrez-malo, M.; Rösch, F. Improved radiolabeling of DOTATOC with trivalent radiometals for clinical application by addition of ethanol. EJNMMI Radiopharm. Chem. 2016, 6, 1–13. [Google Scholar] [CrossRef]
- European Pharmacopoeia 10.0. Radiopharmaceutical Preparations; European Directorate for the Quality of Medicines & HealthCare: Strasbourg, France, 2016; pp. 884–887. [Google Scholar]
- Pharmaceutical Legistration, EudraLex Volume 4, Good manufacturing practice (GMP) Guidelines. Available online: http://www.it-asso.com/gxp/eudralex_v27/contents/homev4.htm (accessed on 30 January 2020).
- EudraLex. The Rules Governing Medicinal Products in the European Union. In Volume 4 Good Manufacturing Practice Medicinal Products for Human and Veterinary Use; European Commission: Brussels, Belgium, 2012; pp. 1–9. [Google Scholar]
- Awasthi, V.; Watson, J.; Gali, H.; Matlock, G.; McFarland, A.; Bailey, J.; Anzellotti, A. A “dose on demand” Biomarker Generator for automated production of [18F]F-and [18F]FDG. Appl. Radiat. Isot. 2014, 89, 167–175. [Google Scholar] [CrossRef]
- Philippe, C.; Mairinger, S.; Pichler, V.; Stanek, J.; Nics, L.; Mitterhauser, M.; Hacker, M.; Wanek, T.; Langer, O.; Wadsak, W. Comparison of fully-automated radiosyntheses of [11C]erlotinib for preclinical and clinical use starting from in target produced [11C]CO2 or [11C]CH4. EJNMMI Radiopharm. Chem. 2018, 3, 8. [Google Scholar] [CrossRef]
- Schultz, M.K.; Mueller, D.; Baum, R.P.; Leonard Watkins, G.; Breeman, W.A.P. A new automated NaCl based robust method for routine production of gallium-68 labeled peptides. Appl. Radiat. Isot. 2013, 76, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Morley, T.J.; Dodd, M.; Gagnon, K.; Hanemaayer, V.; Wilson, J.; McQuarrie, S.A.; English, W.; Ruth, T.J.; Bénard, F.; Schaffer, P. An automated module for the separation and purification of cyclotron-produced 99mTcO4-. Nucl. Med. Biol. 2012, 39, 551–559. [Google Scholar] [CrossRef] [PubMed]
- Elsinga, P.; Todde, S.; Penuelas, I.; Meyer, G.; Farstad, B.; Faivre-Chauvet, A.; Mikolajczak, R.; Westera, G.; Gmeiner-Stopar, T.; Decristoforo, C. Guidance on current good radiopharmacy practice (cGRPP) for the small-scale preparation of radiopharmaceuticals. Eur. J. Nucl. Med. Mol. Imaging 2010, 37, 1049–1062. [Google Scholar] [CrossRef] [PubMed]
- Boschi, S.; Lodi, F.; Malizia, C.; Cicoria, G.; Marengo, M. Automation synthesis modules review. Appl. Radiat. Isot. 2013, 76, 38–45. [Google Scholar] [CrossRef] [PubMed]
- Petrik, M.; Knetsch, P.A.; Knopp, R.; Imperato, G.; Ocak, M.; Von Guggenberg, E.; Haubner, R.; Silbernagl, R.; Decristoforo, C. Radiolabelling of peptides for PET, SPECT and therapeutic applications using a fully automated disposable cassette system. Nucl. Med. Commun. 2011, 32, 887–895. [Google Scholar] [CrossRef]
- Ellison, D.; Kaufman, J.; Mather, S.J. Automated radiolabelling of monoclonal antibodies with the Modular Lab system. Nucl. Med. Commun. 2010, 31, 173–177. [Google Scholar] [CrossRef]
- Jensen, M.; Clark, J. Direct Production of Ga68 from bombardment of concentrated aqueous solutions of [Zn68] Zicn Chloride. In Proceedings of the 13th International Workshop on Targetry and Target Chemistry; Riso National Laboratory for Sustainable Energy: Roskilde, Denmark, 2011; pp. 288–290. [Google Scholar]
- Hoehr, C.; Oehlke, E.; Benard, F.; Lee, C.L.; Hou, X.; Badesso, B.; Ferguson, S.; Miao, Q.; Yang, H.; Buckley, K.; et al. 44gSc production using a water target on a 13 MeV cyclotron. Nucl. Med. Biol. 2014, 41, 401–406. [Google Scholar] [CrossRef]
- Pandey, M.K.; Byrne, J.F.; Jiang, H.; Packard, A.B.; Degrado, T.R. Cyclotron production of 68Ga via the 68Zn(p,n)68Ga reaction in aqueous solution. Am. J. Nucl Med. Mol Imaging 2014, 4, 303–310. [Google Scholar]
- Pandey, M.K.; Byrne, J.F.; Schlasner, K.N.; Schmit, N.R.; DeGrado, T.R. Cyclotron production of 68Ga in a liquid target: Effects of solution composition and irradiation parameters. Nucl. Med. Biol. 2019, 74–75, 49–55. [Google Scholar] [CrossRef]
- Oehlke, E.; Hoehr, C.; Hou, X.; Hanemaayer, V.; Zeisler, S.; Adam, M.J.; Ruth, T.J.; Celler, A.; Buckley, K.; Benard, F.; et al. Production of Y-86 and other radiometals for research purposes using a solution target system. Nucl. Med. Biol. 2015, 42, 842–849. [Google Scholar] [CrossRef]
- Abbasi, A.A.; Easwaramoorthy, B. Method and System for Producing Gallium-68 Radioisotope by Solid Targeting in a Cyclotro. Patent WO/2016/197084, 2016. Available online: https://patentscope2.wipo.int/search/en/detail.jsf?docId=WO2016197084 (accessed on 30 January 2020).
- van der Meulen, N.P.; Bunka, M.; Domnanich, K.A.; Müller, C.; Haller, S.; Vermeulen, C.; Türler, A.; Schibli, R. Cyclotron production of 44Sc: From bench to bedside. Nucl. Med. Biol. 2015, 42, 745–751. [Google Scholar] [CrossRef] [PubMed]
- Krajewski, B.S.; Cydzik, I.; Abbas, K.; Bulgheroni, A.; Simonelli, F.; Holzwarth, U.; Bilewicz, A. Cyclotron production of 44Sc for clinical application. Radiochim. Acta 2013, 101, 333–338. [Google Scholar] [CrossRef]
- Engle, J.W.; Lopez-Rodriguez, V.; Gaspar-Carcamo, R.E.; Valdovinos, H.F.; Gonzalez, M.V.-; Trejo-Ballado, F.; Severin, G.W.; Barnhart, T.E.; Nickles, R.J.; Rodriguez, M.A.A.-. Very high specific activity 66/68Ga from zinc targets for PET. Appl Radiat Isot 2012, 70, 1792–1796. [Google Scholar] [CrossRef] [PubMed]
- Sadeghi, M.; Kakavand, T.; Rajabifar, S.; Mokhtari, L.; Rahimi-Nezhad, A. Cyclotron production of 68Ga via proton-induced reaction on 68Zn target. Nukleonika 2009, 54, 25–28. [Google Scholar]
- Lin, M.; Waligorski, G.J.; Lepera, C.G. Production of curie quantities of 68Ga with a medical cyclotron via the 68Zn (p,n)68Ga reaction. Appl. Radiat. Isot. 2018, 133, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Laboratory of Radiochemistry. Annual Report, CaO target development for 44Sc Production; Paul Scherrer Institute: Villigen, Switzerland, 2017; p. 58. [Google Scholar]
- Chakravarty, R.; Chakraborty, S.; Ram, R.; Vatsa, R.; Bhusari, P.; Shukla, J.; Mittal, B.R.; Dash, A. Detailed evaluation of different 68Ge/68Ga generators: an attempt toward achieving efficient 68Ga radiopharmacy. J. Label Compd. Radiopharm. 2015, 59, 87–94. [Google Scholar] [CrossRef]
- Van der Meulen, N.P.; Dolley, S.G.; Steyn, G.F.; van der Walt, T.N.; Raubenheimer, H.G. The use of selective volatilization in the separation of 68Ge from irradiated Ga targets. Appl. Radiat. Isot. 2011, 69, 727–731. [Google Scholar] [CrossRef]
- Rösch, F. Maturation of a Key Resource – The Germanium-68/Gallium-68 Generator: Development and New Insights Maturation of a Key Resource – The Germanium-68/Gallium-68 Generator: Development and New Insights. Curr. Radiopharm. 2012, 5, 202–211. [Google Scholar] [CrossRef]
- Alnahwi, A.; Tremblay, S.; Ait-mohand, S.; Beaudoin, J.-F.; Guerin, B. Large-scale routine production of 68Ga using 68Zn-pressed target. J. Nucl. Med. 2019, 60, 634. [Google Scholar]
- Filosofov, B.D.V.; Loktionova, N.S.; Rösch, F. A 44Ti/44Sc radionuclide generator for potential application of 44Sc-based PET-radiopharmaceuticals. Radiochim. Acta 2010, 98, 149–156. [Google Scholar] [CrossRef]
- Pruszyn’ ski, M.; Loktionova, N.S.; Filosofov, D.V.; Roesch, F. Post-elution processing of Ti-44/Sc-44 generator-derived Sc-44 for clinical application. Appl. Radiat. Isot. 2010, 68, 1636–1641. [Google Scholar] [CrossRef] [PubMed]
- Yug, A.; Novgorodov, A.F.; Skripnik, A.V.; D.V., F.; Skripnik, A.V.; Kaplun, V.G.; Suzikov, A.G.; Eliseev, I.A.; Rösch, F. 44Ti: Investigation of target preparation, irradiation and yields in the 45Sc ( p, 2n ) process. Annu. Report. Inst. Nucl. Chem. Univ. Mainz. Available online: https://www.blogs.uni-mainz.de/fb09-kernchemie/files/2018/07/b3_05.pdf (accessed on 30 January 2020).
- Zaitseva, N.G.; Tchikalov, M.B.; Khalkin, V.A.; Rurarz, E.; Vobecky, M.; Popinenkova, L.M. Production Cross Sections and Yields of Long Lived 44Ti from 100 MeV Proton Bombardment of Vanadium. Radiochim. Acta 1994, 65, 157–160. [Google Scholar] [CrossRef]
- Sajjad, M.; Lambrecht, R.M. Separation of Tracer Titanium-44 from Vanadium. Anal. Chem. 1986, 58, 667–668. [Google Scholar] [CrossRef]
- Brodzinski, R.L.; Rancitelli, L.A.; Cooper, J.A.; Wogman, N.A. High-energy proton spallation of iron. Phys. Rev. C 1971, 4, 1257–1265. [Google Scholar] [CrossRef]
- Dash, A.; Chakravarty, R. Radionuclide generators: The prospect of availing PET radiotracers to meet current clinical needs and future research demands. Am. J. Nucl Med. Mol Imaging 2019, 9, 30–66. [Google Scholar] [PubMed]
- Rösch, F. Scandium-44: Benefits of a Long-Lived PET Radionuclide Available from the 44Ti/44Sc Generator System. Curr. Radiopharm. 2012, 5, 187–201. [Google Scholar] [CrossRef]
- Severin, G.W.; Engle, J.W.; Valdovinos, H.F.; Barnhart, T.E.; Nickles, R.J. Cyclotron produced Sc from natural calcium. Appl. Radiat. Isot. 2012, 70, 1526–1530. [Google Scholar] [CrossRef]
- Valdovinos, H.F.; Hernandez, R.; Barnhart, T.E.; Graves, S.; Cai, W.; Nickles, R.J. Separation of cyclotron-produced 44Sc from a natural calcium target using a dipentyl pentylphosphonate functionalized extraction resin. Appl Radiat Isot. 2016, 95, 23–29. [Google Scholar] [CrossRef]
- Duchemin, C.; Guertin, A.; Haddad, F.; Michel, N.; Métivier, V. Erratum: Production of scandium-44m and scandium-44g with deuterons on calcium-44: Cross section measurements and production yield calculations. Phys. Med. Biol. 2015, 60, 6847–6864. [Google Scholar] [CrossRef]
- Alliot, C.; Kerdjoudj, R.; Michel, N.; Haddad, F.; Huclier-Markai, S. Cyclotron production of high purity 44m,44Sc with deuterons from 44CaCO3 targets. Nucl. Med. Biol. 2015, 42, 524–529. [Google Scholar] [CrossRef]
- Szkliniarz, K.; Sitarz, M.; Walczak, R.; Jastrzębski, J.; Bilewicz, A.; Choiński, J.; Jakubowski, A.; Majkowska, A.; Stolarz, A.; Trzcińska, A.; et al. Production of medical Sc radioisotopes with an alpha particle beam. Appl. Radiat. Isot. 2016, 118, 182–189. [Google Scholar] [CrossRef] [PubMed]
- Dash, A.; Chakravarty, R. Pivotal role of separation chemistry in the development of radionuclide generators to meet. RSC Adv. 2014, 4, 42779–42803. [Google Scholar] [CrossRef]
- Asti, M.; De Pietri, G.; Fraternali, A.; Grassi, E.; Sghedoni, R.; Fioroni, F.; Roesch, F.; Versari, A.; Salvo, D. Validation of 68Ge/68Ga generator processing by chemical purification for routine clinical application of 68Ga-DOTATOC. Nucl. Med. Biol. 2008, 35, 721–724. [Google Scholar] [CrossRef] [PubMed]
- Meyer, G.J.; Mäcke, H.; Schuhmacher, J.; Knapp, W.H.; Hofmann, M. 68Ga-labelled DOTA-derivatised peptide ligands. Eur. J. Nucl. Med. Mol. Imaging 2004, 31, 1097–1104. [Google Scholar] [CrossRef]
- Lewis, M.R.; Reichert, D.E.; Laforest, R.; Margenau, W.H.; Shefer, R.E.; Klinkowstein, R.E.; Hughey, B.J.; Welch, M.J. Production and purification of gallium-66 for preparation of tumor-targeting radiopharmaceuticals. Nucl. Med. Biol. 2002, 29, 701–706. [Google Scholar] [CrossRef]
- Ugur, Ö.; Kothari, P.J.; Finn, R.D.; Zanzonico, P.; Ruan, S.; Guenther, I.; Maecke, H.R.; Larson, S.M. Ga-66 labeled somatostatin analogue DOTA-DPhe1-Tyr3-octreotide as a potential agent for positron emission tomography imaging and receptor mediated internal radiotherapy of somatostatin receptor positive tumors. Nucl. Med. Biol. 2002, 29, 147–157. [Google Scholar] [CrossRef]
- Tolmachew, V.; Lundqvist, H. Rapid Separation of Gallium from Zinc Targets by Thermal Diffusion. Appl. Radiat. Isot. 1996, 47, 297–299. [Google Scholar] [CrossRef]
- Sadeghi, M.; Mokhtari, L. Rapid separation of 67,68Ga from 68Zn target using precipitation technique. J. Radioanal. Nucl. Chem. 2010, 284, 471–473. [Google Scholar] [CrossRef]
- Wittwer, D.; Dressler, R.; Eichler, R.; Gäggeler, H.W.; Piguet, D.; Serov, A.; Türler, A.; Vögele, A. The thermal release of scandium from titanium metal-A simple way to produce pure 44Sc for PET application. Radiochim. Acta 2011, 99, 193–196. [Google Scholar] [CrossRef]
- Zhernosekov, K.P.; Filosofov, D.V.; Baum, R.P.; Aschoff, P.; Bihl, H.; Razbash, A.A.; Jahn, M.; Jennewein, M.; Rösch, F. Processing of generator-produced 68Ga for medical application. J. Nucl. Med. 2007, 48, 1741–1748. [Google Scholar] [CrossRef]
- Notni, J.; Wester, H.J. Re-thinking the role of radiometal isotopes: Towards a future concept for theranostic radiopharmaceuticals. J. Label. Compd. Radiopharm. 2017, 61, 141–153. [Google Scholar] [CrossRef] [PubMed]
- Ma, M.T.; Cullinane, C.; Waldeck, K.; Roselt, P.; Hicks, R.J.; Blower, P.J. Rapid kit-based 68Ga-labelling and PET imaging with THP-Tyr3-octreotate: A preliminary comparison with DOTA-Tyr3-octreotate. EJNMMI Res. 2015, 5, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Sinnes, J.P.; Nagel, J.; Waldron, B.P.; Maina, T.; Nock, B.A.; Bergmann, R.K.; Ullrich, M.; Pietzsch, J.; Bachmann, M.; Baum, R.P.; et al. Instant kit preparation of 68Ga-radiopharmaceuticals via the hybrid chelator DATA: Clinical translation of [68Ga]Ga-DATA-TOC. EJNMMI Res. 2019, 9, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Pruszynski, M.; Majkowska-Pilip, A.; Loktionova, N.S.; Eppard, E.; Roesch, F. Radiolabeling of DOTATOC with the long-lived positron emitter 44Sc. Appl. Radiat. Isot. 2012, 70, 974–979. [Google Scholar] [CrossRef]
- Huclier-Markai, S.; Kerdjoudj, R.; Alliot, C.; Bonraisin, A.C.; Michel, N.; Haddad, F.; Barbet, J. Optimization of reaction conditions for the radiolabeling of DOTA and DOTA-peptide with 44m/44Sc and experimental evidence of the feasibility of an in vivo PET generator. Nucl. Med. Biol. 2014, 41, 36–43. [Google Scholar] [CrossRef]
- Domnanich, K.A.; Müller, C.; Farkas, R.; Schmid, R.M.; Ponsard, B.; Schibli, R.; Türler, A.; van der Meulen, N.P. Sc for labeling of DOTA- and NODAGA- functionalized peptides: Preclinical in vitro and in vivo investigations. EJNMMI Radiopharm. Chem. 2016, 1–19. [Google Scholar]
- Majkowska-Pilip, A.; Bilewicz, A. Macrocyclic complexes of scandium radionuclides as precursors for diagnostic and therapeutic radiopharmaceuticals. J. Inorg. Biochem. 2011, 105, 313–320. [Google Scholar] [CrossRef]
- Bouyer, F.; Sanson, N.; Destarac, M.; Gérardin, C. Hydrophilic block copolymer-directed growth of lanthanum hydroxide nanoparticles. New, J. Chem. 2006, 30, 399–408. [Google Scholar] [CrossRef]
- Wood, S.A.; Samson, I.M. The aqueous geochemistry of gallium, germanium, indium and scandium. Ore Geol. Rev. 2006, 28, 57–102. [Google Scholar] [CrossRef]
- Pyrzyńska, K.; Kilian, K.; Pęgier, M. Separation and purification of scandium: From industry to medicine. Sep. Purif. Rev. 2019, 48, 65–77. [Google Scholar] [CrossRef]
- Velikyan, I. 68Ga-based radiopharmaceuticals: Production and application relationship. Molecules 2015, 20, 12913–12943. [Google Scholar] [CrossRef] [PubMed]
- Applied Radiology. FDA Approves First Gallium 68Ga-DOTATATE Radiopharmaceutical Tracer for PET Imaging of Neuroendocrine Tumors. Available online: https://appliedradiology.com/articles/fda-approves-first-gallium-68ga-dotatate-radiopharmaceutical-tracer-for-pet-imaging-of-neuroendocrine-tumors (accessed on 30 January 2020).
- Aslani, A.; Snowdon, G.M.; Bailey, D.L.; Schembri, G.P.; Bailey, E.A.; Roach, P.J. Gallium-68 DOTATATE Production with Automated PET Radiopharmaceutical Synthesis System: A Three Year Experience. Asia Ocean. J. Nucl. Med. Biol. 2014, 2, 75–86. [Google Scholar]
- Decristoforo, C.; Knopp, R.; von Guggenberg, E.; Rupprich, M.; Dreger, T.; Hess, A.; Virgolini, I.; Haubner, R. A fully automated synthesis for the preparation of 68Ga-labelled peptides. Nucl. Med. Commun. 2007, 28, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Ocak, M.; Antretter, M.; Knopp, R.; Kunkel, F.; Petrik, M.; Bergisadi, N.; Decristoforo, C. Full automation of 68Ga labelling of DOTA-peptides including cation exchange prepurification. Appl. Radiat. Isot. 2010, 68, 297–302. [Google Scholar] [CrossRef] [PubMed]
- Bailey, D.L.; Hofman, M.S.; Forwood, N.J.; O’Keefe, G.J.; Scott, A.M.; Van Wyngaardt, W.M.; Howe, B.; Kovacev, O.; Francis, R.J. Accuracy of dose calibrators for 68Ga PET imaging: Unexpected findings in a multicenter clinical pretrial assessment. J. Nucl. Med. 2018, 59, 636–638. [Google Scholar] [CrossRef] [PubMed]
- European Pharmacopoeia Organisation. Gallium (68Ga) Chloride Solution for Radiolabelling, European Pharmacopoeie 10.0; EDQM Council of Europe: Strasbourg, France, 2016; pp. 1206–1208. [Google Scholar]
- Radiopharmacy: An Update; A Technologist’s guide; EANM: Vienna, Austria, 2019; p. 149.
- Singh, A.; van der Meulen, N.P.; Müller, C.; Klette, I.; Kulkarni, H.R.; Tu, A.; Schibli, R.; Baum, R.P. First-in-Human PET/CT Imaging of Metastatic Neuroendocrine Neoplasms with Cyclotron-Produced 44Sc-DOTATOC: A Proof-of-Concept Study. Cancer Biother. Radiopharm. 2017, 32, 124–132. [Google Scholar] [CrossRef] [PubMed]
- Dvorakova, Z. Production and Chemical Processing of 177 Lu for Nuclear Medicine at the Munich Research Reactor FRM-II. Available online: https://www.researchgate.net/publication/36420376_Production_and_chemical_processing_of_Lu-177_for_nuclear_medicine_at_the_Munich_research_reactor_FRM-II (accessed on 30 January 2020).
- Lehenberger, S.; Barkhausen, C.; Cohrs, S.; Fischer, E.; Grünberg, J.; Hohn, A.; Köster, U.; Schibli, R.; Türler, A.; Zhernosekov, K. The low-energy β − and electron emitter 161Tb as an alternative to Lu for targeted radionuclide therapy. Nucl. Med. Biol. 2011, 38, 917–924. [Google Scholar] [CrossRef]
- Ferreira, K.M.; Collins, S.M.; Fenwick, A.J. Half-life measurement of the medical radioisotope 177Lu produced from the 176Yb(n, γ) reaction. EPJ Web Conf. 2017, 146, 1–5. [Google Scholar] [CrossRef]
- Duran, M.T.; Juget, F.; Nedjadi, Y.; Bochud, F.; Grundler, P.V.; Gracheva, G.; Müller, C. Determination of 161Tb half-life. J. Appl. Isot. 2020, in press. [Google Scholar] [CrossRef]
- Regulations for the Safe Transport of Radioactive Materials. IAEA Saf. Stand. 2012, SSR-6, 1–166.
- Nash, K.L.; Jensen, M.P. Analytical separations of the lanthanides: Basic chemistry and methods. Handb. Phys. Chem. Rare Earths 2000, 28, 311–371. [Google Scholar]
- Horwitz, E.P.; Mcalister, D.R.; Bond, A.H.; Barrans, R.E.; Williamson, J.M. A process for the separation of 177Lu from neutron irradiated 176Yb targets. Appl. Radiat. Isot. 63 2005, 63, 23–36. [Google Scholar] [CrossRef] [PubMed]
- van So, L.; Morcos, N.; Zaw, M.; Pellegrini, P.; Greguric, I. Alternative chromatographic processes for no-carrier added 177Lu radioisotope separation Part I. Multi-column chromatographic process for clinically applicable. J. Radioanal. Nucl. Chem. 2008, 277, 663–673. [Google Scholar]
- van So, L.; Morcos, N. New SPE column packing material: Retention assessment method and its application for the radionuclide chromatographic separation. J. Radioanal. Nucl. Chem. 2008, 277, 651–661. [Google Scholar]
- van So, L.; Morcos, N.; Zaw, M.; Pellegrini, P.; Greguric, I.; Nevissi, A. Alternative chromatographic processes for no-carrier added 177Lu radioisotope separation Part II. The conventional column chromatographic separation combined with HPLC for high purity. J. Radioanal. Nucl. Chem. 2008, 277, 675–683. [Google Scholar]
- Park, U.J.; Jae, U.; Lee, J.; Hyuk, K.; Soo, S.; Hyun, K. Lu-177 preparation for radiotherapy application. Appl. Radiat. Isot. 2016, 115, 8–12. [Google Scholar] [CrossRef]
- Marx, S.; Harfensteller, M.; Zhernosekov, K.; Nikula, T. Method of Manufacturing Non-Carrier Added High-Purity 177Lu Compounds as Well as Non-Carrier Added 177Lu Compounds. Patent US 2014/02, 2014. 1–8. Available online: https://patentimages.storage.googleapis.com/c2/d5/a3/32b542f3379064/US20140294700A1.pdf (accessed on 30 January 2020).
- Gracheva, N.; Müller, C.; Talip, Z.; Heinitz, S.; Köster, U.; Zeevaart, J.R.; Vögele, A.; Schibli, R.; van der Meulen, N.P. Production and characterization of no- carrier-added 161Tb as an alternative to the therapy. EJNMMI Radiopharm. Chem. 2019, 4, 1–16. [Google Scholar] [CrossRef]
- McAlister, D.R.; Horwitz, P.E. Characterization of extraction of chromatographic materials containing bis(2-ethyl-1-hexyl)phosphoric acid, 2-Ethyl-1-Hexyl (2-Ethyl-1-Hexyl) phosphonic acid, and bis(2,4,4-Trimethyl-1-Pentyl)phosphinic acid. Solvent Extr. Ion. Exch. 2007, 25, 757–769. [Google Scholar] [CrossRef]
- Horwitz, E.P.; McAlister, D.R.; Dietz, M.L. Extraction chromatography versus solvent extraction: How similar are they? Sep. Sci. Technol. 2006, 41, 2163–2182. [Google Scholar] [CrossRef]
- Starý, J. Separation of transplutonium elements. Talanta 1966, 13, 421–437. [Google Scholar] [CrossRef]
- Nayak, D.; Lahiri, S. Application of radioisotopes in the field of nuclear medicine. J. Radioanal. Nucl. Chem. 1999, 242, 423–432. [Google Scholar] [CrossRef]
- Cathy, C.; Jeffrey, S.; Ehrhardt, G.; Tyler, T.; Jurisson, S.; Deutsch, E. Current and Potential Therapeutic Uses of Lanthanide Radioisotope. Cancer Biother. Radiopharm. 2000, 15, 531–545. [Google Scholar]
- Rösch, F. Radiolanthanides in endoradiotherapy: An overview. Radiochim. Acta 2007, 95, 303–311. [Google Scholar] [CrossRef]
- Teo, R.D.; Termini, J.; Gray, H.B. Lanthanides: Applications in Cancer Diagnosis and Therapy Miniperspective. J. Med. Chem. 2016, 59, 6012–6024. [Google Scholar] [CrossRef] [PubMed]
- van de Voorde, M.; van Hecke, K.; Cardinaels, T.; Binnemans, K. Radiochemical processing of nuclear-reactor-produced radiolanthanides for medical applications. Coord. Chem. Rev. 2019, 382, 103–125. [Google Scholar] [CrossRef]
- Iori, M.; Capponi, P.C.; Rubagotti, S.; Esposizione, L.R.; Seemann, J.; Pitzschler, R.; Dreger, T.; Formisano, D.; Grassi, E.; Fioroni, F.; et al. Labelling of 90Y- and 177Lu-DOTA-Bioconjugates for targeted radionuclide Therapy: A comparison among manual, semiautomated, and fully automated synthesis. Contrast Media Mol. Imaging 2017, 2017, 1–12. [Google Scholar] [CrossRef]
- Aslani, A.; Snowdon, G.M.; Bailey, D.L.; Schembri, G.P.; Bailey, E.A.; Pavlakis, N.; Roach, P.J. Lutetium-177 DOTATATE Production with an Automated Radiopharmaceutical Synthesis System. Asia Ocean. J. Nucl. Med. Biol. 2015, 3, 107–10715. [Google Scholar]
- European Pharmacopoeia Organisation. European Pharmacopoeia, Lutetium (177Lu) Solution for Radiolabelling. 2016, pp. 1218–1219. Available online: https://www.esrr.info/wp-content/uploads/2016/04/Kroon.pdf (accessed on 30 January 2020).
| Radionuclide | Half-Life | Main Decay Mode | Eα [MeV] | Eβav [MeV] | Eγ [KeV] | Iγ [%] | Application |
|---|---|---|---|---|---|---|---|
| 64Cu | 12.70 h | β+ | 0.278 | 511 1345.8 | (annihil.) 0.48 | PET | |
| 67Ga | 9.26 d | γ | 93.3 184.6 300.2 393.5 208.9 | 38.8 21.4 16.6 4.6 2.5 | SPECT | ||
| 68Ga | 67.71 min | β+ | 0.830 | 511 1077.3 | (annihil.) 3.22 | PET | |
| 111In | 2.80 d | γ | 245.3 171.3 | 94.1 90.7 | SPECT | ||
| 177Lu | 6.65 d | β− | 0.134 | 208.4 112.9 | 10.4 6.2 | β−-Therapy | |
| 153Sm | 46.50 h | β− | 0.224 | 103.2 69.7 | 29.3 4.7 | Bone metastases | |
| 89Sr | 50.53 d | β− | 0.587 | Bone metastases | |||
| 223Ra | 11.43 d | α | 5.716 5.606 5.539 5.747 | 269.5 154.2 323.9 144.2 | 13.9 5.7 3.9 3.3 | α-Therapy | |
| 186Re | 3.72 d | β− | 0.347 | 137.2 | 9.5 | Bone metastases | |
| 99mTc | 6.01 h | γ | 140.5 | 89 | SPECT | ||
| 201Tl | 72.91 h | γ | 167.4 135.3 | 10.0 2.6 | SPECT | ||
| 90Y | 64.10 h | β− | 0.934 | β−-Therapy | |||
| 89Zr | 78.41 h | β+ | 0.396 | 511 909.1 | (annihil.) 99 | PET |
| Radionuclide | Half-life | Decay mode | Eγ (kev) | Main Production Route | Radionuclidic impurities |
|---|---|---|---|---|---|
| 68Ga | EC (11%) | 68Ge →68Ga generator | 68Ge 67Ga, 66Ga, | ||
| 67.71 min | β+ (88%) | 1077 (3%) | 68Zn(p,n)68Ga | ||
| Eβ+av: 830 keV | |||||
| 44Sc | EC (5%), | 44Ti → 44Sc generator | 48Sc, 44mSc | ||
| 4.04 h | β+ (95%) | 1157 (99.9%) | natCa(p, xn)44Sc | 44mSc, 47Sc, 48Sc | |
| Eβ+av: 632 keV | 44Ca(p, n)44Sc | 44mSc |
| 68Ga | References | 44Sc | References |
|---|---|---|---|
| Liquid Target | Liquid target | ||
| 68ZnCl2 | [93] | Ca(NO3)2 | [94] |
| 68Zn(NO3)2 | [42,95,96,97] | ||
| Solid Target | Solid target | ||
| 68Zn foil | [98] | 44CaCO3 | [99,100] |
| EP 68Zn | [101,102,103] | 44CaO | [104] |
| EP: Electroplated |
| Final product | 68GaCl3 |
|---|---|
| Appearance | Clear, colorless solution |
| pH | <2 |
| Radiolabeling Yield | >99% |
| TLC/HPLC | |
| Radionuclide Identity (γ-Spectrometry Approx. Half Life) | 511 keV 1077 keV |
| Radionuclidic purity (γ-spectrometry) | >99.9% |
| Radiochemical Purity (TLC) | >95% |
| 68Ge Breakthrough | <0.001% |
| Bacterial Endotoxins | <175IU/V |
| Iron | <10ug/GBq, each |
| Zinc |
| Final product | Generator-produced 68Ga | Cyclotron-produced 68Ga |
|---|---|---|
| 68Ga activity | Minimum 99.9% | Minimum 98.0% |
| 68Ge activity | Maximum 0.001% | n.a. |
| 66Ga and 67Ga | n.a. | Maximum 2.0% |
| Other radioimpurities | n.a. | Maximum 0.1% |
| n.a. not applicable |
| Radionuclide | Half-Life (d) | Eβ-av (MeV) | Eγ (kev) | Auger/Conversion e- | Production Route | |
|---|---|---|---|---|---|---|
| 177Lu | 6.64 [152] | 134 | 208 (10.4%) | Auger L | 6.3 (8.7%) | 176Lu(n,γ)177Lu |
| 113 (6.4%) | CE K | 47.6 (5.1%) | 176Yb(n,γ)177Yb →177Lu | |||
| 321 (0.219%) | CE L | 101.7 (6.8%) | ||||
| 161Tb | 6.96 [153] | 154 | 26 (23.2%) | CE K | 3.4 (17.5%) | 160Gd(n,γ)161Gd →161Tb |
| 29 (0.0365%) | CE L | 16.6 (41%) | ||||
| 44 (0.060%) | Auger L | 5.2 (87.9%) | ||||
| Target | % Natural Abundance | % Available Enrichment | Cross Section σ (Barn) | Activation Product | Decay Mode | T1/2 | Decay Product | Specific Activity (TBq/mg) |
|---|---|---|---|---|---|---|---|---|
| 176Lu2O3 | 2.59 | 84.6 | 2.8 | 177mLu | β, γ, IT | 160.4 d | 177Hf (78.6%) 177Lu (21.4%)→ | 3.9 TBq/mg |
| 2090 | 177Lu | β, γ | 6.65 d | 177Hf | ||||
| 176Yb2O3 | 12.76 | >99.6 | 2.85 | 177Yb | β, γ | 1.9 h | 177Lu | 740-1110 GBq/mg |
| 160Gd2O3 | 21.86 | 98.2 | 1.5 | 161Gd | β, γ | 3.66 m | 161Tb | to be optimized |
| Test | 177LuCl3 (EndolucinBeta) | 161TbCl3 |
|---|---|---|
| Specific activity (Dose calibrator) | 36–44 GBq/mL at ART | 11–21 GBq/mL |
| Appearance | Clear, colorless | Clear, colorless |
| pH (pH indicator strip) | 1–2 | 1–2 |
| Radiolabeling yield | >99.0% | >99.0% |
| TLC/HPLC (Based on radiolabeling with 177Lu or 161Tb of DOTA-derivate, molar ratio 1:4) | ||
| Identity (γ-spectrometry) | 113 keV 208 keV | 48.9 keV 74.6 keV |
| Radionuclidic purity (γ-spectrometry) | 175Yb ≤ 0.1% | 160Tb ≤ 0.007% |
| Radiochemical purity (radio-TLC) | >99.0% | >99.0% |
| Bacterial endotoxins | ≤175 IU/V |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Talip, Z.; Favaretto, C.; Geistlich, S.; Meulen, N.P.v.d. A Step-by-Step Guide for the Novel Radiometal Production for Medical Applications: Case Studies with 68Ga, 44Sc, 177Lu and 161Tb. Molecules 2020, 25, 966. https://doi.org/10.3390/molecules25040966
Talip Z, Favaretto C, Geistlich S, Meulen NPvd. A Step-by-Step Guide for the Novel Radiometal Production for Medical Applications: Case Studies with 68Ga, 44Sc, 177Lu and 161Tb. Molecules. 2020; 25(4):966. https://doi.org/10.3390/molecules25040966
Chicago/Turabian StyleTalip, Zeynep, Chiara Favaretto, Susanne Geistlich, and Nicholas P. van der Meulen. 2020. "A Step-by-Step Guide for the Novel Radiometal Production for Medical Applications: Case Studies with 68Ga, 44Sc, 177Lu and 161Tb" Molecules 25, no. 4: 966. https://doi.org/10.3390/molecules25040966
APA StyleTalip, Z., Favaretto, C., Geistlich, S., & Meulen, N. P. v. d. (2020). A Step-by-Step Guide for the Novel Radiometal Production for Medical Applications: Case Studies with 68Ga, 44Sc, 177Lu and 161Tb. Molecules, 25(4), 966. https://doi.org/10.3390/molecules25040966





