Enhanced Extraction Technique of Omarigliptin from Human Plasma—Applied to Biological Samples from Healthy Human Volunteers
Abstract
:1. Introduction
2. Methods
2.1. Chemicals and Reagents
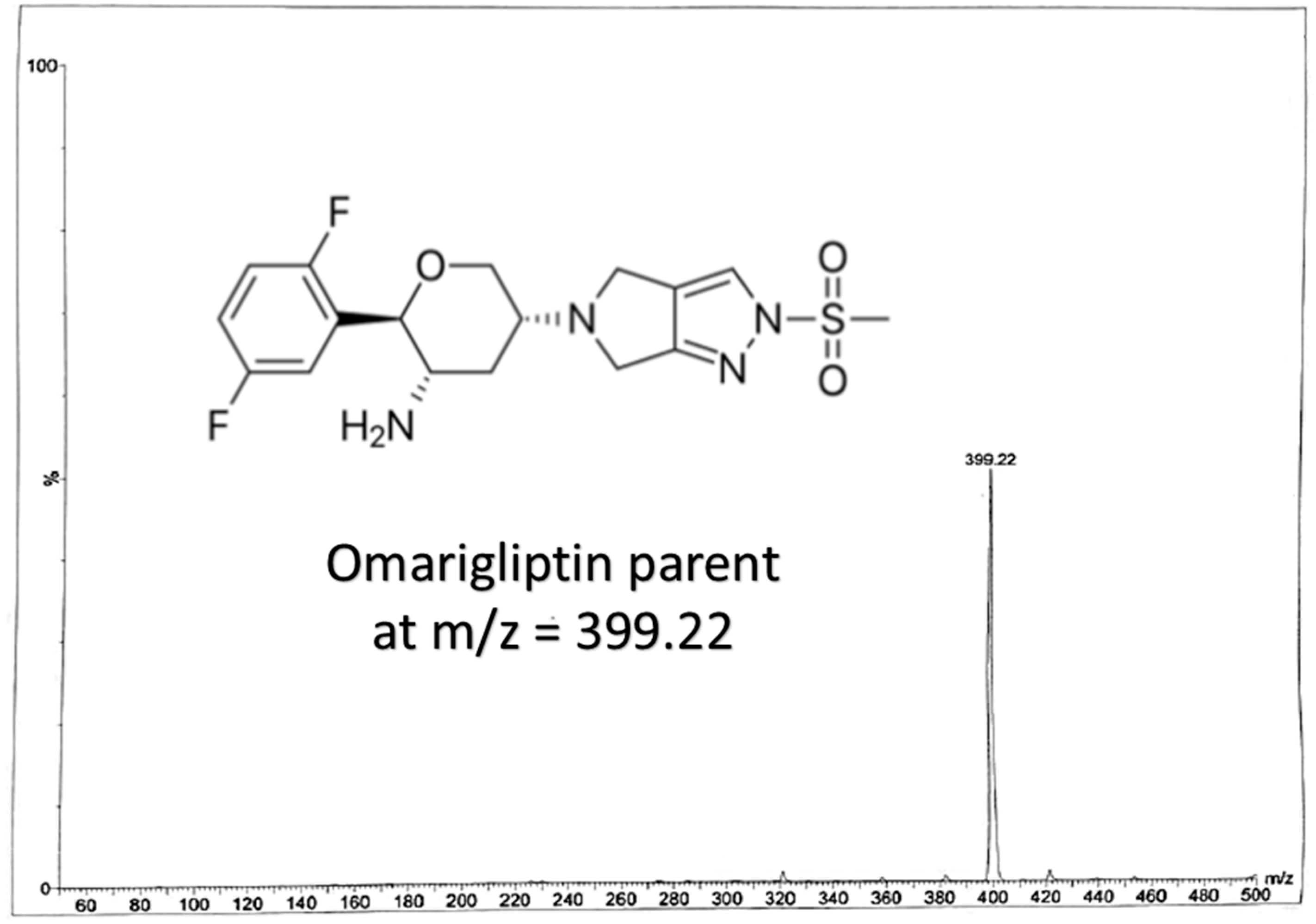
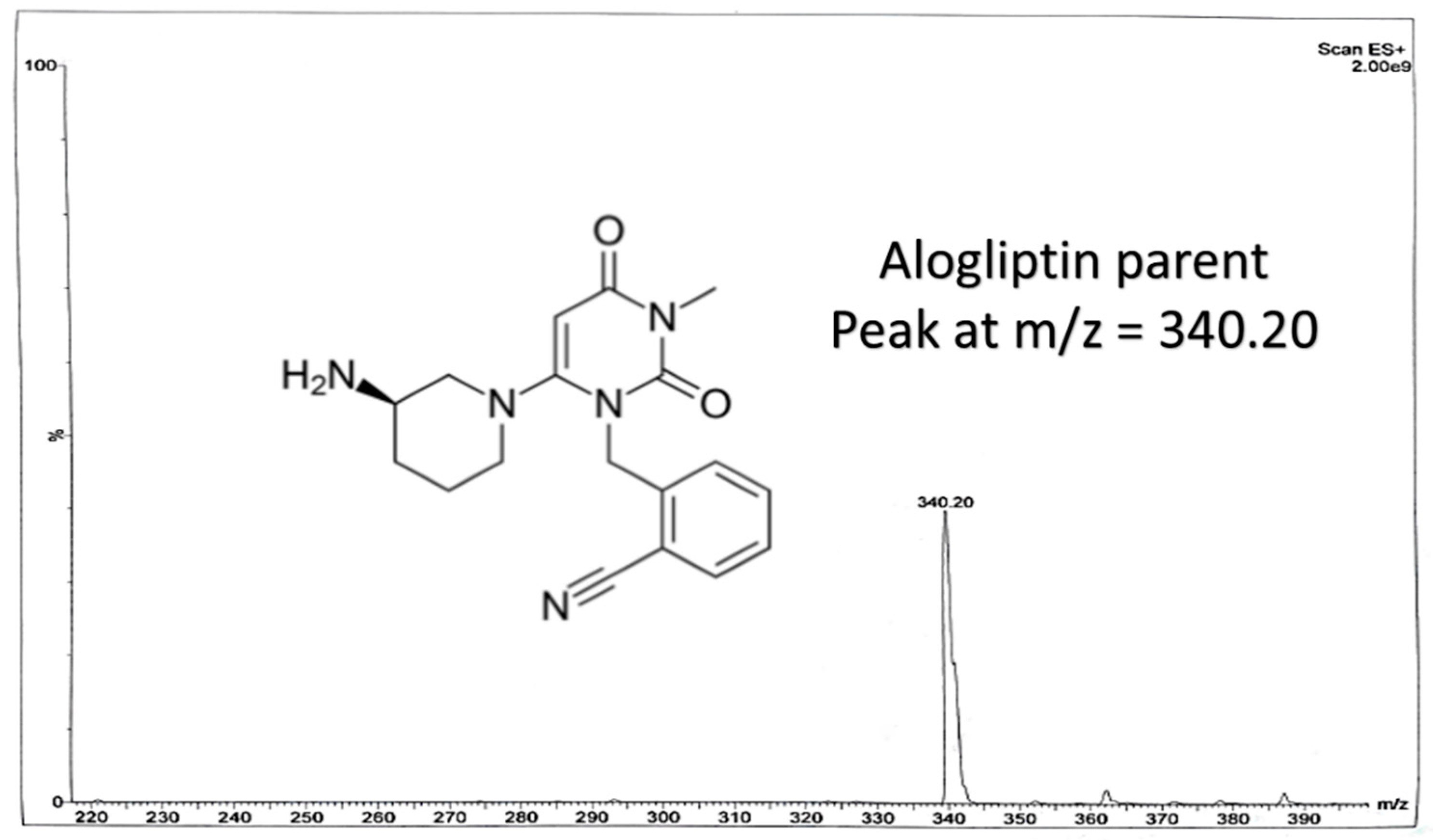
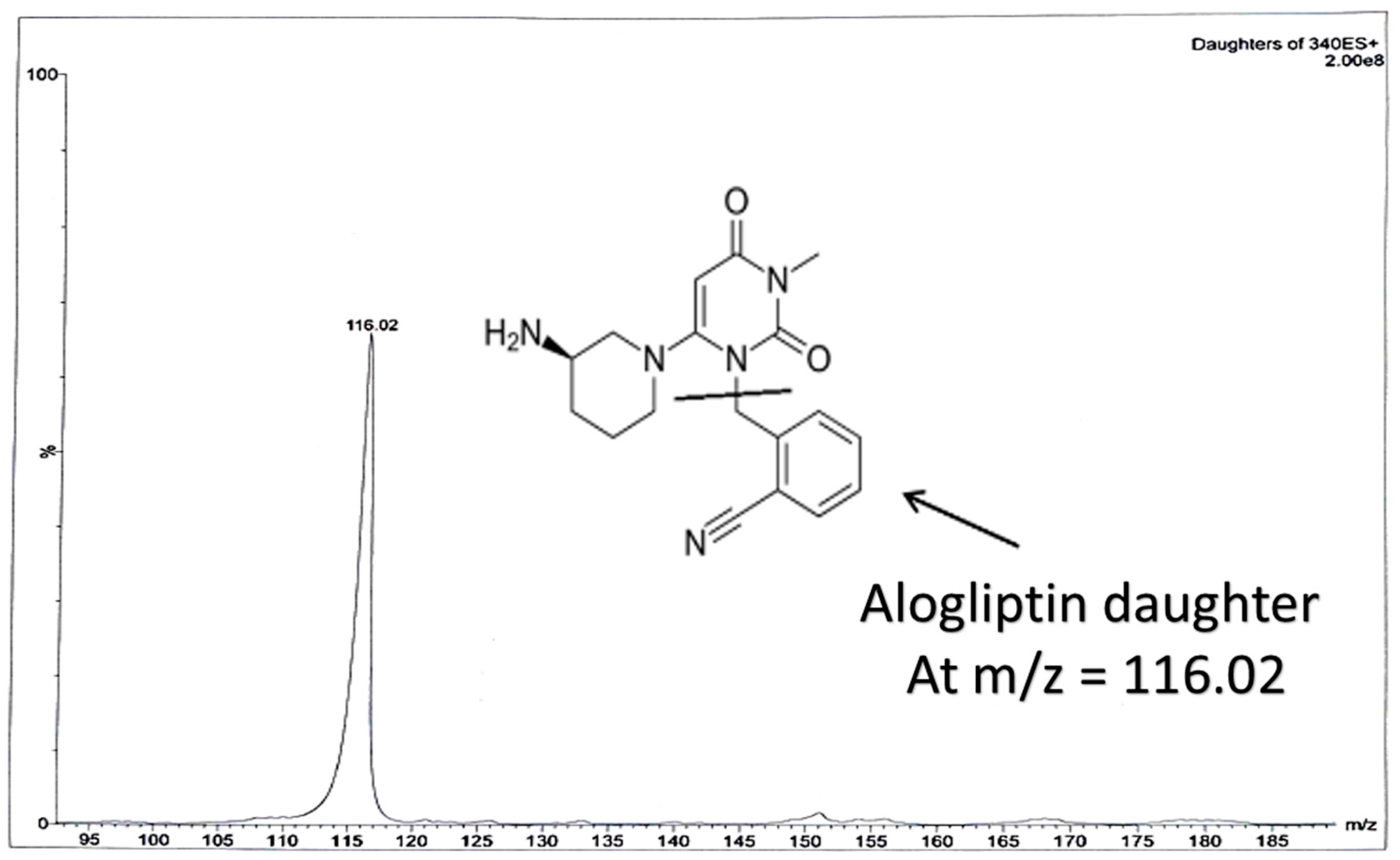
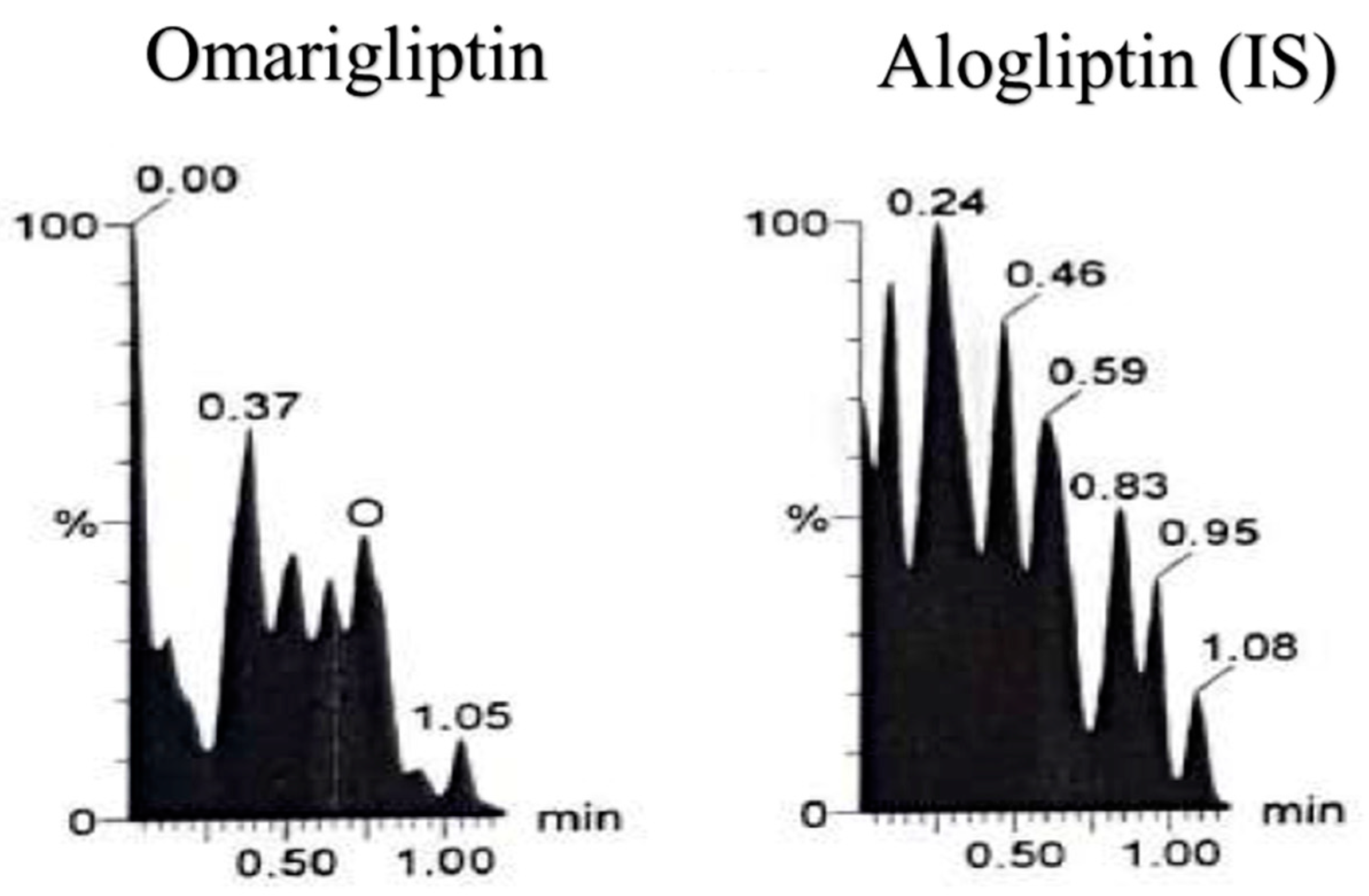
2.2. LC-MS/MS Conditions
2.3. Calibrators, QC Samples and Sample Preparation
2.4. Bioanalytical Validation
2.5. Biological Samples and Ethical Approval
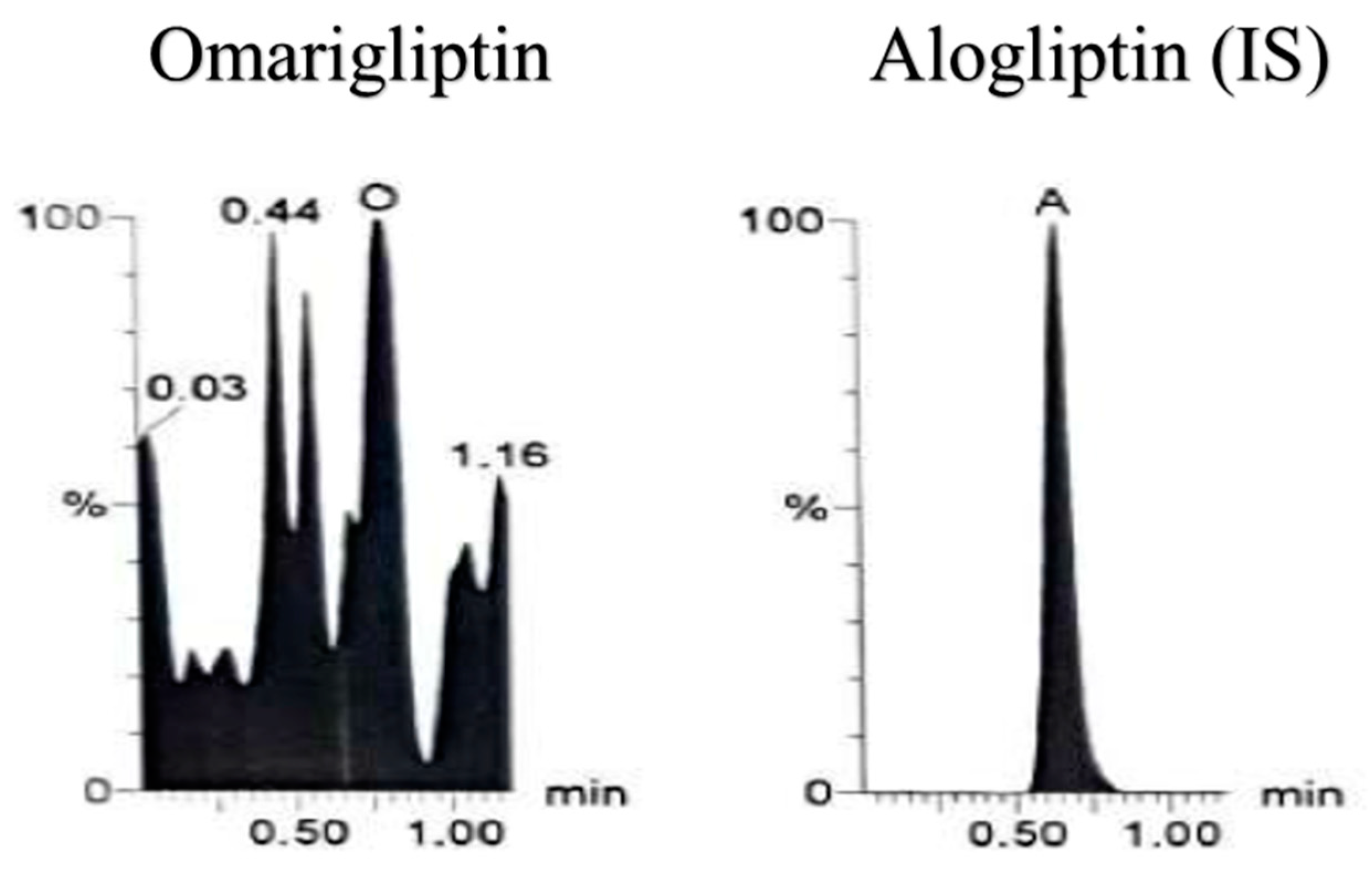
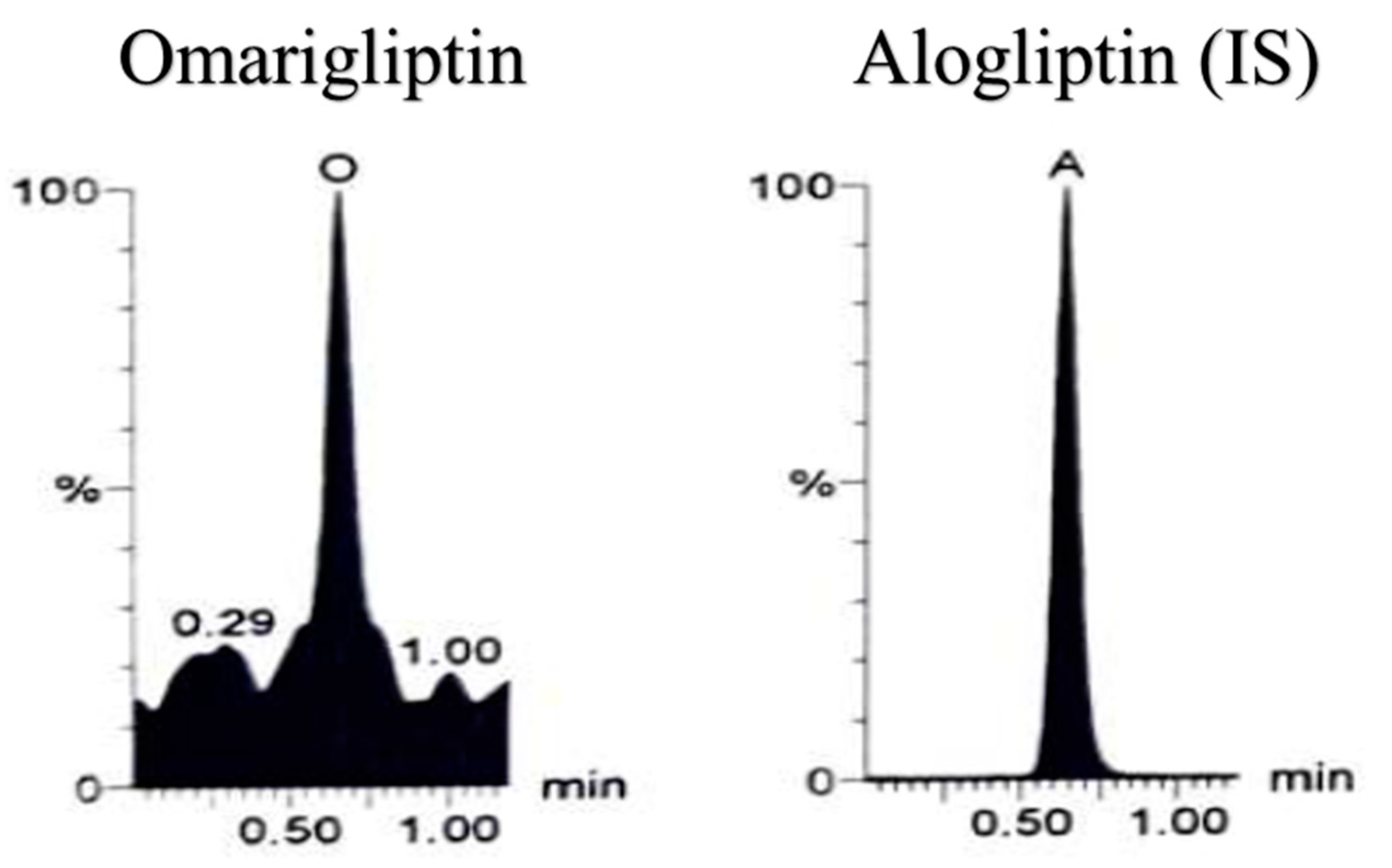
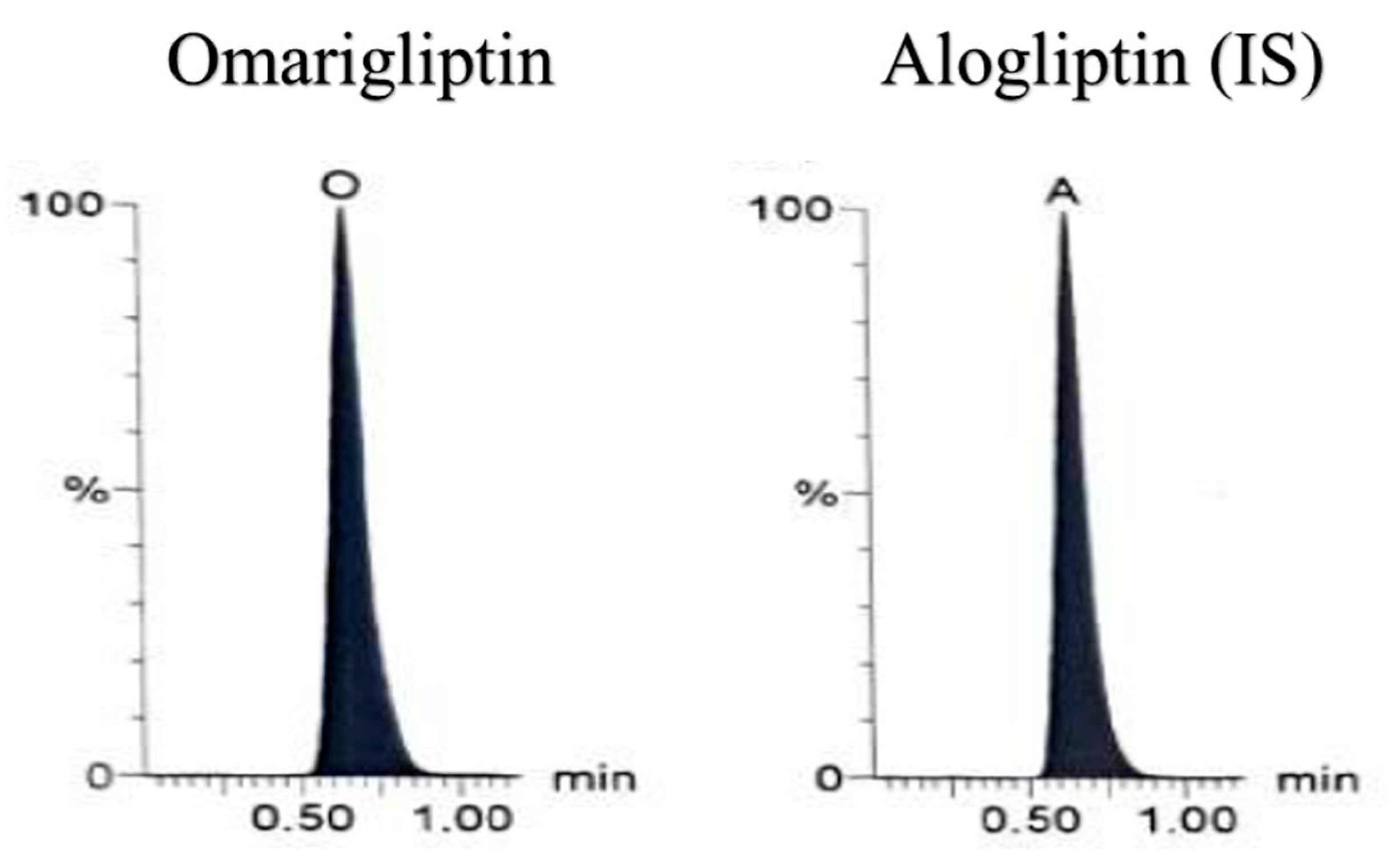
3. Results and Discussion
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Xia, J.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 2600, 30079–30085. [Google Scholar] [CrossRef] [Green Version]
- Gupta, R.; Ghosh, A.; Singh, A.K.; Misra, A. Clinical considerations for patients with diabetes in times of COVID-19 epidemic. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 211–212. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.K.; Feng, Y.; Yuan, M.Y.; Yuan, S.Y.; Fu, H.J.; Wu, B.Y.; Sun, G.Z.; Yang, G.R.; Zhang, X.L.; Wang, L.; et al. Plasma glucose levels and diabetes are independent predictors for mortality and morbidity in patients with SARS. Diabet. Med. 2006, 23, 623–628. [Google Scholar] [CrossRef] [PubMed]
- Schoen, K.; Horvat, N.; Guerreiro, N.F.C.; de Castro, I.; de Giassi, K.S. Spectrum of clinical and radiographic findings in patients with diagnosis of H1N1 and correlation with clinical severity. BMC Infect. Dis. 2019, 19, 964. [Google Scholar] [CrossRef] [Green Version]
- Galloway, I.; McKay, G.; Fisher, M. Omarigliptin. Pract. Diabetes 2017, 34, 70–71. [Google Scholar] [CrossRef]
- Tan, X. Omarigliptin for the treatment of type 2 diabetes. Endocrine 2016, 54, 24–31. [Google Scholar] [CrossRef]
- Wang, X.; Li, X.; Qie, S.; Zheng, Y.; Liu, Y.; Liu, G. The efficacy and safety of once-weekly DPP-4 inhibitor omarigliptin in patients with type 2 diabetes mellitus A systemic review and meta-analysis. Medicine 2018, 97, e11946. [Google Scholar] [CrossRef]
- Burness, C.B. Omarigliptin: First Global Approval. Drugs 2015, 75, 1947–1952. [Google Scholar] [CrossRef]
- Ito, Y.; Mori, M.; Matsumoto, Y.; Okamoto, T. Pharmacological action and clinical results of omarigliptin (MARIZEV® tablet), a novel dipeptidyl peptidase-4 inhibitor for once-weekly treatment of Type 2 diabetes. Folia Pharmacol. Jpn. 2017, 149, 128–137. [Google Scholar] [CrossRef] [Green Version]
- Jain, L.; Chain, A.S.Y.; Tatosian, D.A.; Hing, J.; Passarell, J.A.; Kauh, E.A.; Lai, E. Pharmacokinetic–pharmacodynamic (dipeptidyl peptidase-4 inhibition) model to support dose rationale in diabetes patients, including those with renal impairment, for once-weekly administered omarigliptin. Br. J. Clin. Pharmacol. 2019, 85, 2759–2771. [Google Scholar] [CrossRef]
- Ayoub, B.M.; Mowaka, S.; Safar, M.M.; Ashoush, N.; Arafa, M.G.; Michel, H.E.; Tadros, M.M.; Elmazar, M.M.; Mousa, S.A. Repositioning of omarigliptin as a once-weekly intranasal anti-parkinsonian agent. Sci. Rep. 2018, 8, 8959. [Google Scholar] [CrossRef]
- Tsuchiya, S.; Friedman, E.; Addy, C.; Wakana, A.; Tatosian, D.; Matsumoto, Y.; Suzuki, H.; Kauh, E. Single and multiple dose pharmacokinetics and pharmacodynamics of omarigliptin, a novel, once-weekly dipeptidyl peptidase-4 inhibitor, in healthy Japanese men. J. Diabetes Investig. 2017, 8, 84–92. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tatosian, D.A.; Cardillo Marricco, N.; Glasgow, X.S.; DeGroot, B.; Dunnington, K.; George, L.; Gendrano, I.N.; Johnson-Levonas, A.O.; Swearingen, D.; Kauh, E.A. Thorough QTc study confirms early pharmacokinetics/QTc Modeling: A supratherapeutic dose of omarigliptin, a once-weekly DPP-4 Inhibitor, does not prolong the QTc interval. Clin. Pharmacol. Drug Dev. 2016, 5, 383–392. [Google Scholar] [CrossRef] [PubMed]
- Addy, C.; Tatosian, D.A.; Glasgow, X.S.; Iii, I.N.G.; Sisk, C.M.; Kauh, E.A.; Stoch, S.A.; Wagner, J.A. Effects of age, sex, and obesity on the single-dose pharmacokinetics of omarigliptin in healthy subjects. Clin. Pharmacol. Drug Dev. 2016, 5, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Addy, C.; Tatosian, D.; Glasgow, X.S.; Gendrano, I.N., III; Kauh, E.; Martucci, A.; Johnson-Levonas, A.O.; Selverian, D.; Matthews, C.Z.; Gutierrez, M.; et al. Pharmacokinetic and pharmacodynamic effects of multiple-dose administration of omarigliptin, a once-weekly Dipeptidyl Peptidase-4 Inhibitor, in obese Participants with and without type 2 diabetes mellitus. Clin. Ther. 2016, 38, 516–530. [Google Scholar] [CrossRef] [PubMed]
- Krishna, R.; Addy, C.; Tatosian, D.; Glasgow, X.S.; Gendrano, I.N.; Robberechts, M.; Haazen, W.; de Hoon, J.N.; Depré, M.; Martucci, A.; et al. Pharmacokinetics and pharmacodynamics of omarigliptin, a once-weekly dipeptidyl peptidase-4 (DPP-4) inhibitor, after single and multiple doses in Healthy Subjects. J. Clin. Pharmacol. 2016, 56, 1528–1537. [Google Scholar] [CrossRef]
- Xu, S.; Tatosian, D.; Mcintosh, I.; Caceres, M.; Matthews, C.; Samuel, K.; Selverian, D.; Kumar, S.; Kauh, E. Absorption, metabolism and excretion of [14C] omarigliptin, a once-weekly DPP-4 inhibitor, in humans. Xenobiotica 2018, 48, 584–591. [Google Scholar] [CrossRef]
- Li, M.-F.; Hu, X.-X.; Ma, A.-Q. Ultra-high pressure liquid chromatography–tandem mass spectrometry method for the determination of omarigliptin in rat plasma and its application to a pharmacokinetic study in rats. Biomed. Chromatogr. 2017, 31, e3975. [Google Scholar] [CrossRef]
- Attallah, M.A.; Mowaka, S.; Elkady, E.F.; Fouad, M.; Ayoub, B. Analysis and bio-analysis of omarigliptin, trelagliptin and alogliptin: Applied to biological samples and degradation kinetic study. Microchem. J. 2019, 148, 253–261. [Google Scholar] [CrossRef]
- FDA Bioanalytical Method Validation, Guidance for Industry, U.S.Department of Health and Human Services Food and Drug Administration Center for Drug Evaluation and Research (CDER) Center for Veterinary Medicine (CVM). 2018. Available online: https://www.fda.gov/regulatory-information/search-fda-guidance-documents/bioanalytical-method-validation-guidance-industry (accessed on 15 July 2020).
- Fukunaga, S.; Kusama, M.; Arnold, F.L.; Ono, S. Ethnic differences in pharmacokinetics in new drug applications and approved doses in Japan. J. Clin. Pharmacol. 2011, 51, 1237–1240. [Google Scholar] [CrossRef]
- Limdi, N.A.; Brown, T.M.; Yan, Q.; Thigpen, J.L.; Shendre, A.; Liu, N.; Hill, C.E.; Arnett, D.K.; Beasley, T.M. Race influences warfarin dose changes associated with genetic factors. Blood 2015, 126, 539–545. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xue, Y.-J.; Pursley, J.; Arnold, M.E. A simple 96-well liquid–liquid extraction with a mixture of acetonitrile and methyl t-butyl ether for the determination of a drug in human plasma by high-performance liquid chromatography with tandem mass spectrometry. J. Pharm. Biomed. Anal. 2004, 34, 369–378. [Google Scholar] [CrossRef]
- Suresh, P.S.; Srinivas, N.R.; Mullangi, R. A concise review of the bioanalytical methods for the quantitation of sitagliptin, an important dipeptidyl peptidase-4 (DPP4) inhibitor, utilized for the characterization of the drug. Biomed. Chromatogr. 2016, 30, 749–771. [Google Scholar] [CrossRef]
Sample Availability: Samples of the compounds are not available from the authors. |

| Method | Extraction | LLOQ | Application | Reference |
|---|---|---|---|---|
| LC-MS/MS | Liquid-Liquid using TBME-DEE | 25 nM (9.96 ng/mL) | Human plasma | Underlying investigation |
| LC-MS/MS | Direct precipitation using Acetonitrile | 50 ng/mL | Rats’ plasma | [11] |
| LC-MS/MS | Liquid-Liquid using Ethyl acetate after pH adjustment | 2 ng/mL | Human plasma | [12,13,14,15,16,17] |
| LC-MS/MS | Direct precipitation using Acetonitrile | 4 ng/mL | Rats’ plasma | [18] |
| UPLC-UV | Liquid-Liquid using DEE | 2.5 µg/mL | Rats’ plasma | [19] |
| Accuracy and Precision (n = 5, Three days) | LLOQ (25 nM) | MQC (500 nM) | HQC (800 nM) | |
|---|---|---|---|---|
| 1st day Intraday | Bias (mean, n = 5) | 15.41 | −6.30 | −1.09 |
| Average Percent Recovery | 115.41% | 93.70% | 98.91% | |
| S.D. | 14.55 | 2.01 | 3.57 | |
| % R.S.D | 12.61 | 2.14 | 3.64 | |
| 2nd day Intraday | Bias (mean, n = 5) | 10.34 | 1.49 | −0.10 |
| Average Percent Recovery | 110.34% | 101.49% | 99.90% | |
| S.D. | 15.37 | 1.90 | 1.82 | |
| % R.S.D | 13.92 | 1.87 | 1.82 | |
| 3rd day Intraday | Bias (mean, n = 5) | 13.80 | 0.98 | −0.91 |
| Average Percent Recovery | 113.80% | 100.98% | 99.09% | |
| S.D. | 9.57 | 1.83 | 2.62 | |
| % R.S.D | 8.41 | 1.81 | 2.64 | |
| Interday | Bias (mean, n = 15) | 13.40 | −1.30 | −1.01 |
| Average Percent Recovery | 113.40% | 98.70% | 98.99% | |
| S.D. | 13.41 | 4.02 | 2.89 | |
| % R.S.D | 11.83 | 4.07 | 2.92 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mowaka, S.; Ashoush, N.; Tadros, M.; El Zahar, N.; Ayoub, B. Enhanced Extraction Technique of Omarigliptin from Human Plasma—Applied to Biological Samples from Healthy Human Volunteers. Molecules 2020, 25, 4232. https://doi.org/10.3390/molecules25184232
Mowaka S, Ashoush N, Tadros M, El Zahar N, Ayoub B. Enhanced Extraction Technique of Omarigliptin from Human Plasma—Applied to Biological Samples from Healthy Human Volunteers. Molecules. 2020; 25(18):4232. https://doi.org/10.3390/molecules25184232
Chicago/Turabian StyleMowaka, Shereen, Nermeen Ashoush, Mariam Tadros, Noha El Zahar, and Bassam Ayoub. 2020. "Enhanced Extraction Technique of Omarigliptin from Human Plasma—Applied to Biological Samples from Healthy Human Volunteers" Molecules 25, no. 18: 4232. https://doi.org/10.3390/molecules25184232
APA StyleMowaka, S., Ashoush, N., Tadros, M., El Zahar, N., & Ayoub, B. (2020). Enhanced Extraction Technique of Omarigliptin from Human Plasma—Applied to Biological Samples from Healthy Human Volunteers. Molecules, 25(18), 4232. https://doi.org/10.3390/molecules25184232






