Rationally Designed α-Conotoxin Analogues Maintained Analgesia Activity and Weakened Side Effects
Abstract
1. Introduction
2. Results
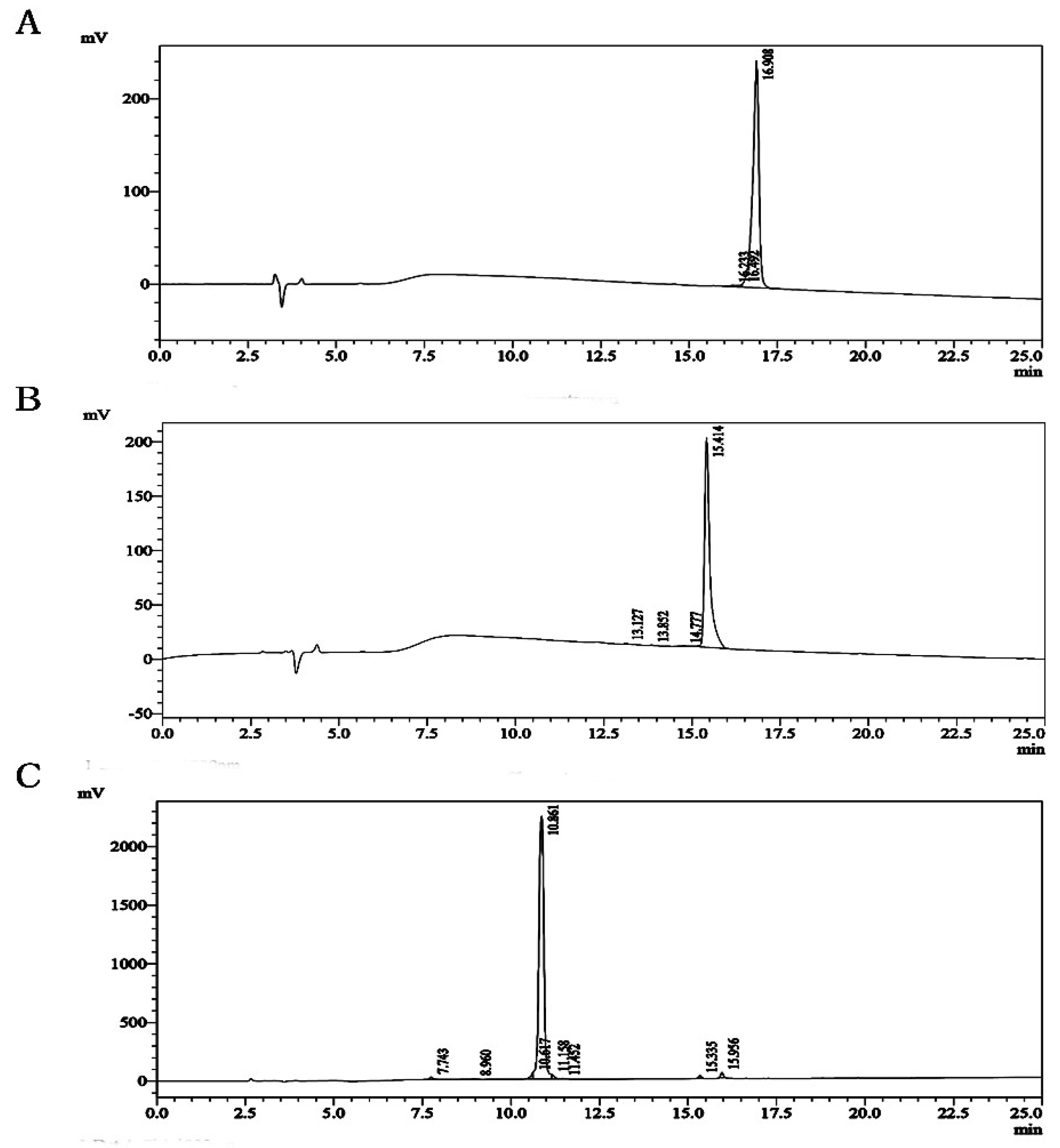
2.1. Virtual Screening and HPLC Chromatography of Analogues
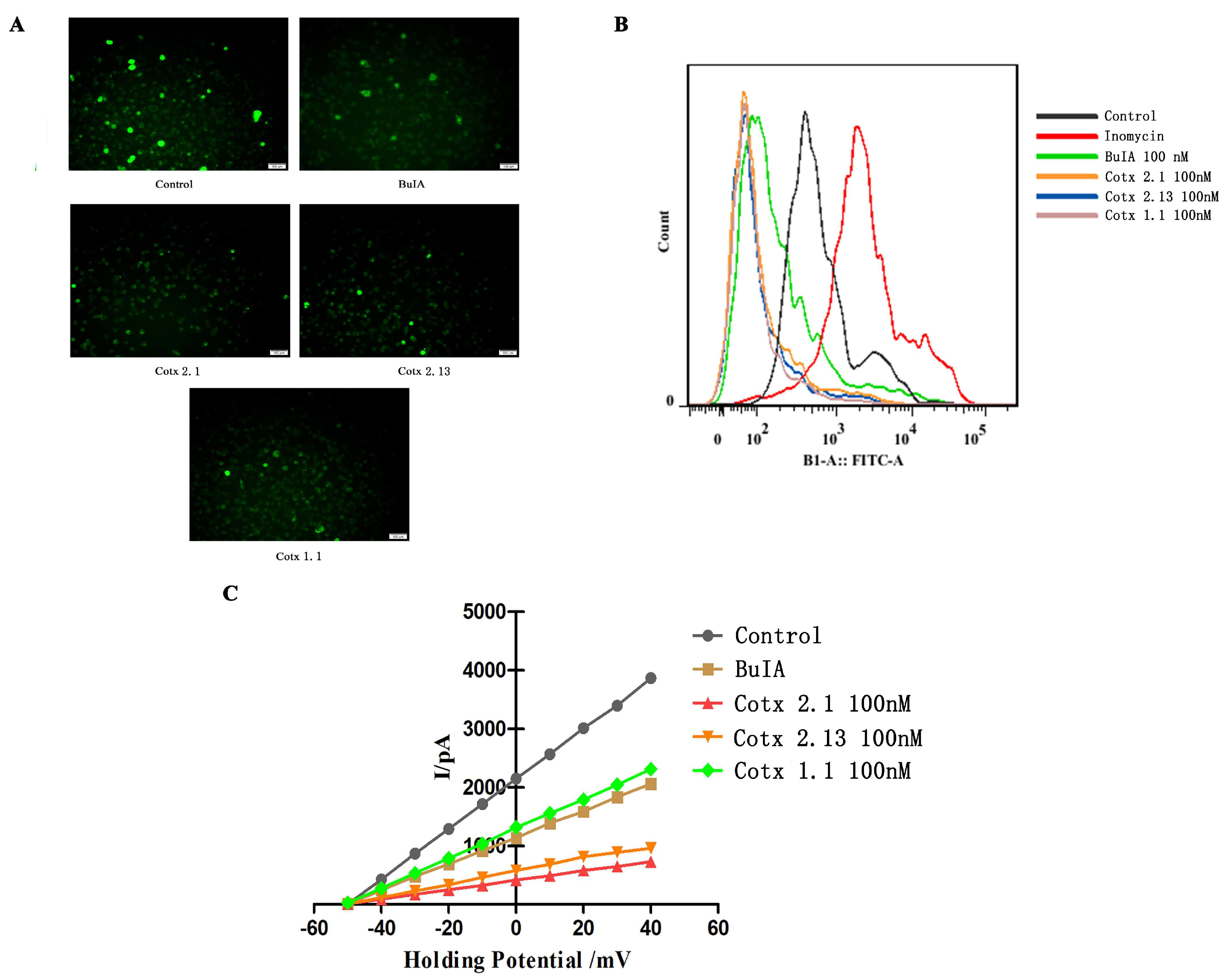
2.2. Affinity and Activity of BuIA and Analogues
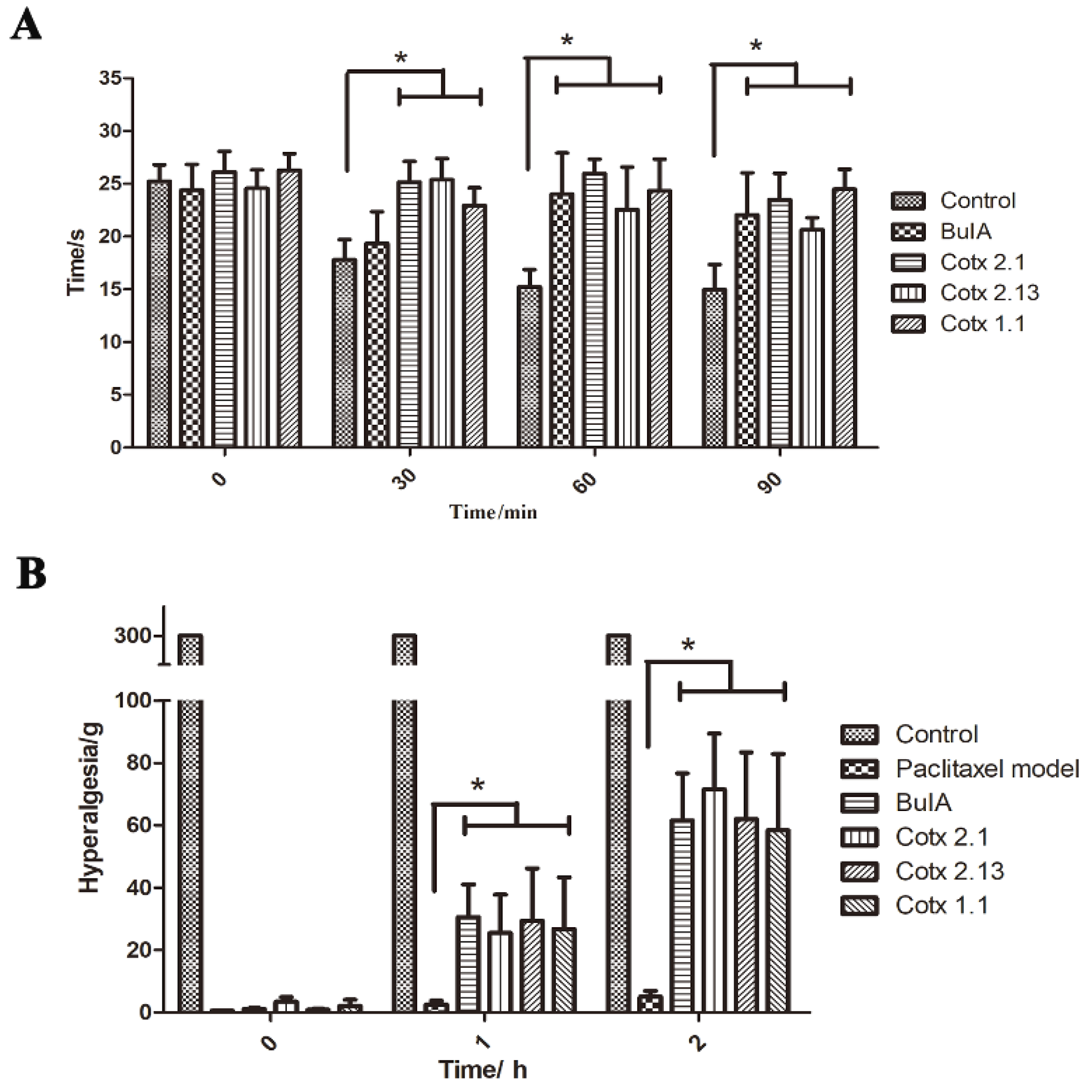
2.3. Analgesic Activity of BuIA and Analogues In Vivo
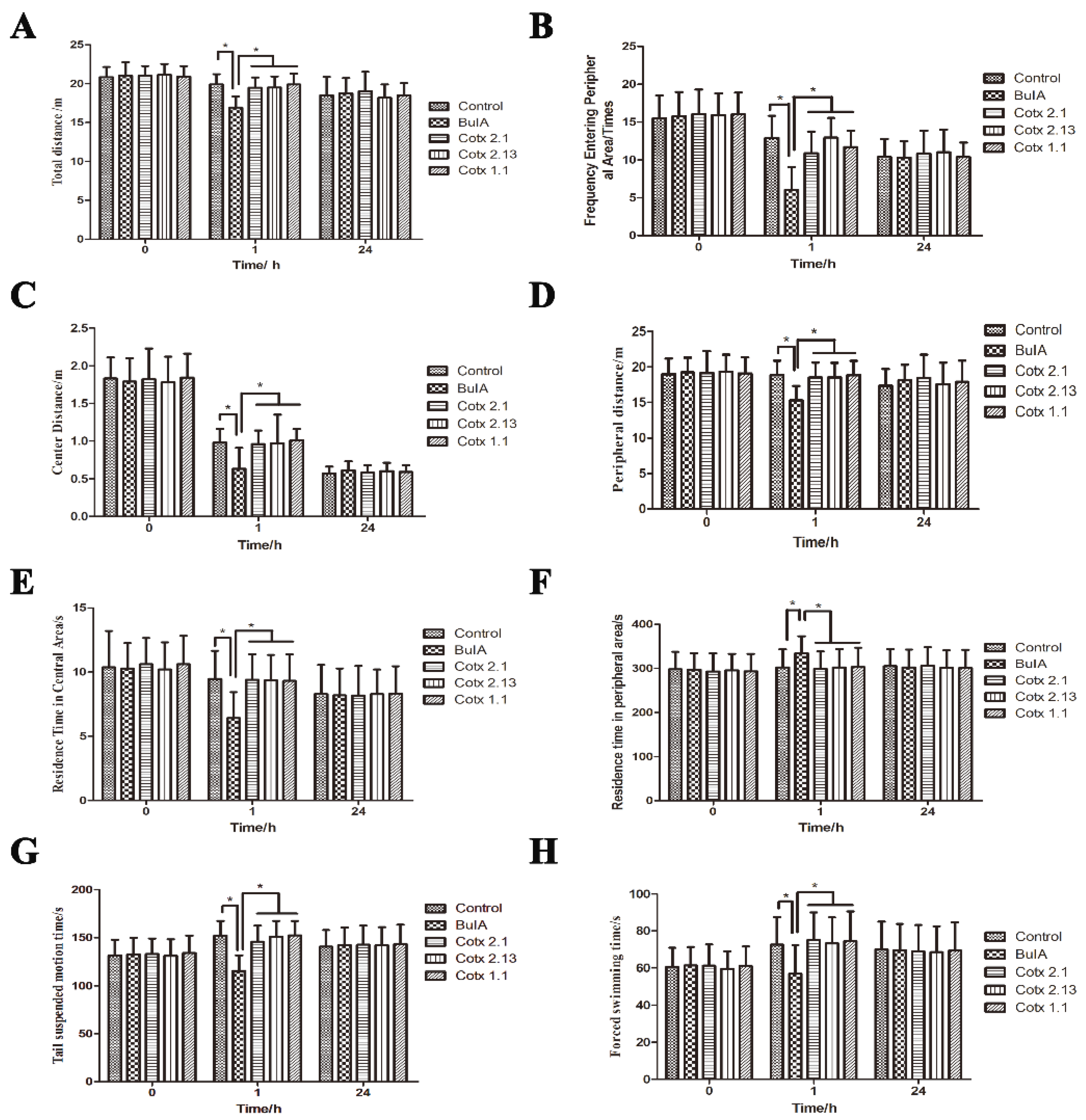
2.4. Adverse Reactions to BuIA and Analogues
3. Discussion
4. Materials and Methods
4.1. Analogue Design and Siftings
4.2. Peptide Preparation
4.3. Microscale Thermophoresis Analysis
4.4. Dorsal Root Ganglion Neuron Cell Preparation
4.5. Fluorescence Imaging Analysis
4.6. Flow Cytometer Analysis
4.7. Patch Clamp Electrophysiology
4.8. Animals
4.8.1. Hot-Plate model Test
4.8.2. Paclitaxel-Induced Peripheral Neuropathy Model
4.9. Detection of Side Reaction Activity
4.9.1. Tail Suspension Test
4.9.2. Forced Swimming Test
4.9.3. Open Field Test
4.10. Data Analysis
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Brady, K.T.; McCauley, J.L.; Back, S.E. Prescription Opioid Misuse, Abuse, and Treatment in the United States: An Update. Am. J. Psychiatry 2016, 173, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Romero, H.K.; Christensen, S.B.; Di Cesare Mannelli, L.; Gajewiak, J.; Ramachandra, R.; Elmslie, K.S.; Vetter, D.E.; Ghelardini, C.; Iadonato, S.P.; Mercado, J.L.; et al. Inhibition of alpha9alpha10 nicotinic acetylcholine receptors prevents chemotherapy-induced neuropathic pain. Proc. Natl. Acad. Sci. USA 2017, 114, E1825–E1832. [Google Scholar] [CrossRef] [PubMed]
- Olivera, B.M. Conus peptides: Biodiversity-based discovery and exogenomics. J. Biol. Chem. 2006, 281, 31173–31177. [Google Scholar] [CrossRef] [PubMed]
- Terlau, H.; Olivera, B.M. Conus venoms: A rich source of novel ion channel-targeted peptides. Physiol. Rev. 2004, 84, 41–68. [Google Scholar] [CrossRef] [PubMed]
- Akondi, K.B.; Muttenthaler, M.; Dutertre, S.; Kaas, Q.; Craik, D.J.; Lewis, R.J.; Alewood, P.F. Discovery, synthesis, and structure-activity relationships of conotoxins. Chem. Rev. 2014, 114, 5815–5847. [Google Scholar] [CrossRef] [PubMed]
- Bingham, J.P.; Mitsunaga, E.; Bergeron, Z.L. Drugs from slugs--past, present and future perspectives of omega-conotoxin research. Chem.-Biol. Interact. 2010, 183, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Kress, H.G.; Simpson, K.H.; Marchettini, P.; Ver Donck, A.; Varrassi, G. Intrathecal therapy: What has changed with the introduction of ziconotide. Pain Pract. 2009, 9, 338–347. [Google Scholar] [CrossRef] [PubMed]
- Sanford, M. Intrathecal Ziconotide: A Review of Its Use in Patients with Chronic Pain Refractory to Other Systemic or Intrathecal Analgesics. CNS Drugs 2013, 27, 989–1002. [Google Scholar] [CrossRef] [PubMed]
- Smit, A.B.; Syed, N.I.; Schaap, D.; van Minnen, J.; Klumperman, J.; Kits, K.S.; Lodder, H.; van der Schors, R.C.; van Elk, R.; Sorgedrager, B.; et al. A glia-derived acetylcholine-binding protein that modulates synaptic transmission. Nature 2001, 411, 261–268. [Google Scholar] [CrossRef]
- Nicke, A.; Wonnacott, S.; Lewis, R.J. Alpha-conotoxins as tools for the elucidation of structure and function of neuronal nicotinic acetylcholine receptor subtypes. Eur. J. Biochem. 2004, 271, 2305–2319. [Google Scholar] [CrossRef] [PubMed]
- Azam, L.; McIntosh, J.M. Alpha-conotoxins as pharmacological probes of nicotinic acetylcholine receptors. Acta Pharmacol. Sin. 2009, 30, 771–783. [Google Scholar] [CrossRef] [PubMed]
- Gao, B.; Peng, C.; Yang, J.; Yi, Y.; Zhang, J.; Shi, Q. Cone Snails: A Big Store of Conotoxins for Novel Drug Discovery. Toxins 2017, 9, 397. [Google Scholar] [CrossRef] [PubMed]
- Livett, B.G.; Sandall, D.W.; Keays, D.; Down, J.; Gayler, K.R.; Satkunanathan, N.; Khalil, Z. Therapeutic applications of conotoxins that target the neuronal nicotinic acetylcholine receptor. Toxicon 2006, 48, 810–829. [Google Scholar] [CrossRef]
- Sandall, D.W.; Satkunanathan, N.; Keays, D.A.; Polidano, M.A.; Liping, X.; Pham, V.; Down, J.G.; Khalil, Z.; Livett, B.G.; Gayler, K.R. A novel alpha-conotoxin identified by gene sequencing is active in suppressing the vascular response to selective stimulation of sensory nerves in vivo. Biochemistry 2003, 42, 6904–6911. [Google Scholar] [CrossRef] [PubMed]
- Satkunanathan, N.; Livett, B.; Gayler, K.; Sandall, D.; Down, J.; Khalil, Z. Alpha-conotoxin Vc1.1 alleviates neuropathic pain and accelerates functional recovery of injured neurones. Brain Res. 2005, 1059, 149–158. [Google Scholar] [CrossRef] [PubMed]
- Bencan, Z.; Levin, E.D. The role of alpha7 and alpha4beta2 nicotinic receptors in the nicotine-induced anxiolytic effect in zebrafish. Physiol. Behav. 2008, 95, 408–412. [Google Scholar] [CrossRef] [PubMed]
- Tsunoda, K.; Tsujino, I.; Koshi, R.; Sugano, N.; Sato, S.; Asano, M. Nicotine-Mediated Ca(2+)-Influx Induces IL-8 Secretion in Oral Squamous Cell Carcinoma Cell. J. Cell. Biochem. 2016, 117, 1009–1015. [Google Scholar] [CrossRef] [PubMed]
- Gong, S.; Liang, Q.; Zhu, Q.; Ding, D.; Yin, Q.; Tao, J.; Jiang, X. Nicotinic acetylcholine receptor alpha7 subunit is involved in the cobratoxin-induced antinociception in an animal model of neuropathic pain. Toxicon 2015, 93, 31–36. [Google Scholar] [CrossRef]
- Cuny, H.; Yu, R.; Tae, H.S.; Kompella, S.N.; Adams, D.J. alpha-Conotoxins active at alpha3-containing nicotinic acetylcholine receptors and their molecular determinants for selective inhibition. Br. J. Pharmacol. 2018, 175, 1855–1868. [Google Scholar] [CrossRef]
- Iwata, H.; Hirose, S.; Akiyoshi, H.; Kaneko, S.; Mitsudome, A. A novel intragenetic PvuII marker in the human neuronal nicotinic acetylcholine receptor a4 subunit gene (CHRNA4). Mutation and polymorphism report no. 62. Online. Hum. Mutat. 1999, 14, 93. [Google Scholar] [CrossRef]
- Azam, L.; Yoshikami, D.; McIntosh, J.M. Amino acid residues that confer high selectivity of the alpha6 nicotinic acetylcholine receptor subunit to alpha-conotoxin MII[S4A,E11A,L15A]. J. Biol. Chem. 2008, 283, 11625–11632. [Google Scholar] [CrossRef] [PubMed]
- Yu, R.; Craik, D.J.; Kaas, Q. Blockade of neuronal alpha7-nAChR by alpha-conotoxin ImI explained by computational scanning and energy calculations. PLOS Comput. Biol. 2011, 7, e1002011. [Google Scholar] [CrossRef] [PubMed]
- Yu, R.; Seymour, V.A.L.; Berecki, G.; Jia, X.; Akcan, M.; Adams, D.J.; Kaas, Q.; Craik, D.J. Less is More: Design of a Highly Stable Disulfide-Deleted Mutant of Analgesic Cyclic α-Conotoxin Vc1.1. Sci. Rep. 2015, 5, 13264. [Google Scholar] [CrossRef] [PubMed]
- Vink, S.; Alewood, P.F. Targeting voltage-gated calcium channels: Developments in peptide and small-molecule inhibitors for the treatment of neuropathic pain. Br. J. Pharmacol. 2012, 167, 970–989. [Google Scholar] [CrossRef] [PubMed]
- Azam, L.; Dowell, C.; Watkins, M.; Stitzel, J.A.; Olivera, B.M.; McIntosh, J.M. Alpha-conotoxin BuIA, a novel peptide from Conus bullatus, distinguishes among neuronal nicotinic acetylcholine receptors. J. Biol. Chem. 2005, 280, 80–87. [Google Scholar] [CrossRef]
- Servent, D.; Thanh, H.L.; Antil, S.; Bertrand, D.; Corringer, P.J.; Changeux, J.P.; Menez, A. Functional determinants by which snake and cone snail toxins block the alpha 7 neuronal nicotinic acetylcholine receptors. J. Physiol. 1998, 92, 107–111. [Google Scholar] [CrossRef]
- Eichinger, A.; Neumaier, I.; Pschenitza, M.; Niessner, R.; Knopp, D.; Skerra, A. Tight Molecular Recognition of Benzo[a]pyrene by a High-Affinity Antibody. Angew. Chem. 2017, 56, 10592–10597. [Google Scholar] [CrossRef]
- Traxler, L.; Rathner, P.; Fahrner, M.; Stadlbauer, M.; Faschinger, F.; Charnavets, T.; Muller, N.; Romanin, C.; Hinterdorfer, P.; Gruber, H.J. Detailed Evidence for an Unparalleled Interaction Mode between Calmodulin and Orai Proteins. Angew. Chem. 2017, 56, 15755–15759. [Google Scholar] [CrossRef]
- Mangat, A.K.; Oei, J.L.; Chen, K.; Quah-Smith, I.; Schmolzer, G.M. A Review of Non-Pharmacological Treatments for Pain Management in Newborn Infants. Children 2018, 5, 130. [Google Scholar] [CrossRef]
- Carstens, B.B.; Berecki, G.; Daniel, J.T.; Lee, H.S.; Jackson, K.A.; Tae, H.S.; Sadeghi, M.; Castro, J.; O’Donnell, T.; Deiteren, A.; et al. Structure-Activity Studies of Cysteine-Rich alpha-Conotoxins that Inhibit High-Voltage-Activated Calcium Channels via GABA(B) Receptor Activation Reveal a Minimal Functional Motif. Angew. Chem. 2016, 55, 4692–4696. [Google Scholar] [CrossRef]
- Bylund, D.B.; Toews, M.L. Radioligand binding methods: Practical guide and tips. Am. J. Physiol. 1993, 265, L421–L429. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Jo, H.; Lee, H.; Choo, H.; Kim, H.J.; Pae, A.N.; Cho, Y.S.; Min, S.J. Identification of Optically Active Pyrimidine Derivatives as Selective 5-HT2C Modulators. Molecules 2017, 22, 1416. [Google Scholar] [CrossRef]
- Pattnaik, P. Surface plasmon resonance: Applications in understanding receptor-ligand interaction. Appl. Biochem. Biotechnol. 2005, 126, 79–92. [Google Scholar] [CrossRef]
- Corbeski, I.; Horn, V.; van der Valk, R.A.; le Paige, U.B.; Dame, R.T.; van Ingen, H. Microscale Thermophoresis Analysis of Chromatin Interactions. Methods Mol. Biol. 2018, 1837, 177–197. [Google Scholar] [CrossRef]
- Murayama, C.; Watanabe, S.; Nakamura, M.; Norimoto, H. Inhibitory Activity of Yokukansankachimpihange against Nerve Growth Factor-Induced Neurite Growth in Cultured Rat Dorsal Root Ganglion Neurons. Molecules 2015, 20, 14959–14969. [Google Scholar] [CrossRef] [PubMed]
- Buhner, S.; Barki, N.; Greiter, W.; Giesbertz, P.; Demir, I.E.; Ceyhan, G.O.; Zeller, F.; Daniel, H.; Schemann, M. Calcium Imaging of Nerve-Mast Cell Signaling in the Human Intestine. Front. Physiol. 2017, 8, 971. [Google Scholar] [CrossRef]
- Spinelli, K.J.; Gillespie, P.G. Monitoring intracellular calcium ion dynamics in hair cell populations with Fluo-4 AM. PLoS ONE 2012, 7, e51874. [Google Scholar] [CrossRef]
- Gandini, M.A.; Sandoval, A.; Felix, R. Whole-cell patch-clamp recordings of Ca2+ currents from isolated neonatal mouse dorsal root ganglion (DRG) neurons. Cold Spring Harb. Protoc. 2014, 2014, 389–395. [Google Scholar] [CrossRef]
- Jiang, Y.J.; Lee, C.L.; Wang, Q.; Zhou, Z.W.; Yang, F.; Jin, C.; Fu, D.L. Establishment of an orthotopic pancreatic cancer mouse model: Cells suspended and injected in Matrigel. World J. Gastroenterol. 2014, 20, 9476–9485. [Google Scholar] [CrossRef]
- Haj-Mirzaian, A.; Kordjazy, N.; Amiri, S.; Haj-Mirzaian, A.; Amini-Khoei, H.; Ostadhadi, S.; Dehpour, A. Involvement of nitric oxide-cyclic guanosine monophosphate pathway in the antidepressant-like effect of tropisetron and ondansetron in mice forced swimming test and tail suspension test. Eur. J. Pharmacol. 2016, 780, 71–81. [Google Scholar] [CrossRef]
- Seredenin, S.B.; Nadorova, A.V.; Kolik, L.G.; Yarkova, M.A. Effects of phenazepam on the behavior of C57BL/6 and BALB/c mice in the open field test after naloxone pretreatment. Bull. Exp. Biol. Med. 2013, 155, 346–349. [Google Scholar] [CrossRef] [PubMed]
Sample Availability: Samples of the compounds (cotx 2.1, cotx 2.13 and cotx 1.1) are available from the authors. |
| Number | Sequence | α3 | α6 | β2 | β4 | α7 |
|---|---|---|---|---|---|---|
| BuIA | GCCSTPPCAVLYC (CysI–CysIII, CysII–CysVI) | −6.657 | −5.032 | −6.866 | −5.485 | −7.136 |
| Loop2 | ||||||
| cotx 2.1 | GSCSTPPSAVLYC (CysI–CysII) | −6.531 | −4.783 | −6.395 | −4.544 | −7.946 |
| cotx 2.2 | GDCSTPPDAVLYC (CysI–CysII) | −6.770 | −5.060 | −6.884 | −5.377 | −7.636 |
| cotx 2.3 | GQCSTPPQAVLYC (CysI–CysII) | −6.265 | −4.799 | −7.536 | −4.297 | −8.239 |
| cotx 2.4 | GMCSTPPMAVLYC (CysI–-CysII) | −6.878 | −4.652 | −7.407 | −4.472 | −8.766 |
| cotx 2.5 | GWCSTPPWAVLYC (CysI–CysII) | −7.265 | −7.348 | −7.333 | −6.083 | −8.073 |
| cotx 2.6 | GYCSTPPYAVLYC (CysI–CysII) | −7.106 | −5.128 | −7.123 | −6.265 | −7.541 |
| cotx 2.7 | GTCSTPPTAVLYC (CysI–CysII) | −6.259 | −4.150 | −7.186 | −4.711 | −7.857 |
| cotx 2.8 | GECSTPPEAVLYC (CysI–CysII) | −6.605 | −3.883 | −6.611 | −4.528 | −7.084 |
| cotx 2.9 | GHCSTPPHAVLYC (CysI–CysII) | −6.995 | −7.399 | −8.029 | −5.695 | −8.570 |
| cotx 2.10 | GKCSTPPKAVLYC (CysI–CysII) | −7.151 | −5.698 | −7.412 | −4.759 | −8.167 |
| cotx 2.11 | GRCSTPPRAVLYC (CysI–CysII) | −7.315 | −5.643 | −7.302 | −5.565 | −8.906 |
| cotx 2.12 | KCSTPPSAVLYC (CysI–CysII) | −7.267 | −5.625 | −6.204 | −5.173 | −7.719 |
| cotx 2.13 | KCSTPPDAVLYC (CysI–CysII) | −6.358 | −4.509 | −6.406 | −5.363 | −7.190 |
| cotx 2.14 | KCSTPPQAVLYC (CysI–CysII) | −6.448 | −6.270 | −6.617 | −4.347 | −7.755 |
| cotx 2.15 | HCSTPPSAVLYC (CysI–CysII) | −6.203 | −5.498 | −6.424 | −4.907 | −7.241 |
| cotx 2.16 | HCSTPPDAVLYC (CysI–CysII) | −6.451 | −5.757 | −6.406 | −5.069 | −7.774 |
| cotx 2.17 | HCSTPPQAVLYC (CysI–CysII) | −7.002 | −6.143 | −6.850 | −4.313 | −7.781 |
| cotx 2.18 | RCSTPPSAVLYC (CysI–CysII) | −7.177 | −4.840 | −6.789 | −4.531 | −8.072 |
| cotx 2.19 | RCSTPPDAVLYC (CysI–CysII) | −6.930 | Neg | Neg | −5.294 | Neg |
| cotx 2.20 | RCSTPPQAVLYC (CysI–CysII) | −7.354 | Neg | Neg | −5.259 | Neg |
| Loop1 | ||||||
| cotx 1.1 | GCSSTPPC (CysI–CysII) | −5.834 | −4.028 | −5.969 | −3.186 | −6.462 |
| cotx 1.2 | GCDSTPPC (CysI–CysII) | −5.983 | −4.161 | −5.718 | −3.390 | −6.376 |
| cotx 1.3 | GCQSTPPC (CysI–CysII) | −5.755 | −6.275 | −5.633 | −3.289 | −6.651 |
| cotx 1.4 | GCWSTPPC (CysI–CysII) | −6.281 | −6.187 | −5.403 | −4.900 | −6.966 |
| cotx 1.5 | GCYSTPPC (CysI–CysII) | −6.133 | −4.823 | −5.710 | −5.271 | −6.670 |
| cotx 1.6 | GCMSTPPC (CysI–CysII) | −6.233 | −6.329 | −5.454 | −3.633 | −6.392 |
| cotx 1.7 | GCTSTPPC (CysI–CysII) | −6.353 | −4.967 | −5.938 | −3.553 | −6.211 |
| cotx 1.8 | GCESTPPC (CysI–CysII) | −6.151 | −3.414 | −5.640 | −3.669 | −6.249 |
| cotx 1.9 | GCHSTPPC (CysI-CysII) | −6.045 | −6.565 | −5.506 | −3.648 | −6.010 |
| cotx 1.10 | GCKSTPPC (CysI–CysII) | −5.956 | −4.409 | −5.532 | −3.282 | −6.450 |
| cotx 1.11 | GCRSTPPC (CysI–CysII) | −6.373 | −6.403 | −5.770 | −4.116 | −6.370 |
| Peptide | EC50 (nM) |
|---|---|
| BuIA | 19.7 ± 2.85 |
| cotx 2.1 | 12.3 ± 1.07 |
| cotx 2.13 | 15.4 ± 1.6 |
| cotx 1.1 | 26.6 ± 4.8 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, C.; Wu, P.; Zhu, H.; Grieco, P.; Yu, R.; Gao, X.; Wu, G.; Wang, D.; Xu, H.; Qi, W. Rationally Designed α-Conotoxin Analogues Maintained Analgesia Activity and Weakened Side Effects. Molecules 2019, 24, 337. https://doi.org/10.3390/molecules24020337
Liu C, Wu P, Zhu H, Grieco P, Yu R, Gao X, Wu G, Wang D, Xu H, Qi W. Rationally Designed α-Conotoxin Analogues Maintained Analgesia Activity and Weakened Side Effects. Molecules. 2019; 24(2):337. https://doi.org/10.3390/molecules24020337
Chicago/Turabian StyleLiu, Chen, Pengxiang Wu, He Zhu, Paolo Grieco, Ruihe Yu, Xinmei Gao, Guiyue Wu, Dong Wang, Hanmei Xu, and Weiyan Qi. 2019. "Rationally Designed α-Conotoxin Analogues Maintained Analgesia Activity and Weakened Side Effects" Molecules 24, no. 2: 337. https://doi.org/10.3390/molecules24020337
APA StyleLiu, C., Wu, P., Zhu, H., Grieco, P., Yu, R., Gao, X., Wu, G., Wang, D., Xu, H., & Qi, W. (2019). Rationally Designed α-Conotoxin Analogues Maintained Analgesia Activity and Weakened Side Effects. Molecules, 24(2), 337. https://doi.org/10.3390/molecules24020337





