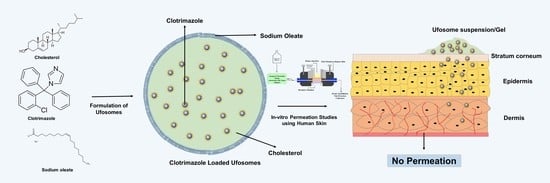
Clotrimazole Loaded Ufosomes for Topical Delivery: Formulation Development and In-Vitro Studies
Abstract
1. Introduction
2. Results and Discussion
2.1. Optimization of Clotrimazole Loaded Ufosomes
2.1.1. Determination of Size, Polydispersity Index, and Zeta Potential
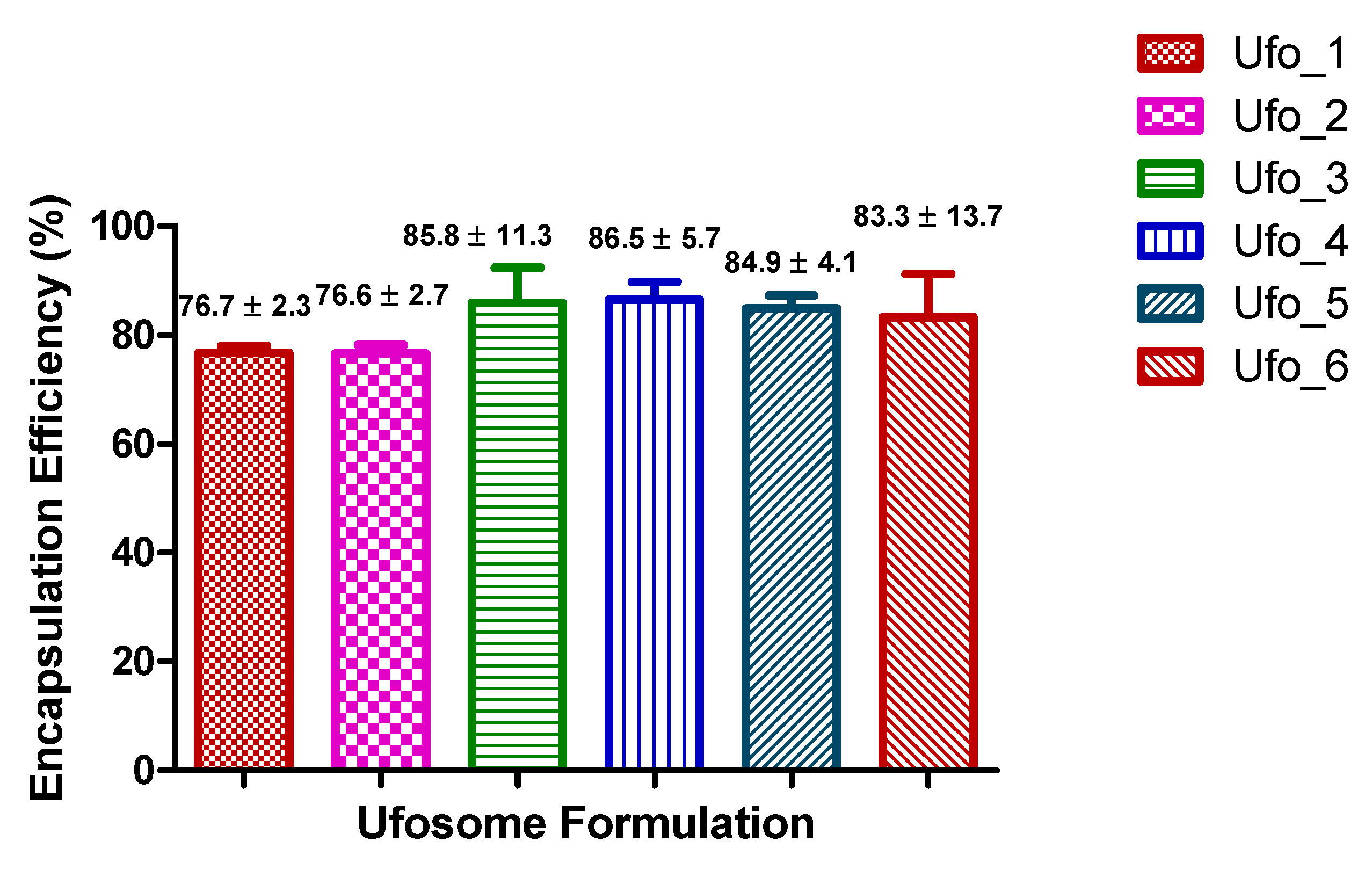
2.1.2. Determination of Entrapment Efficiency
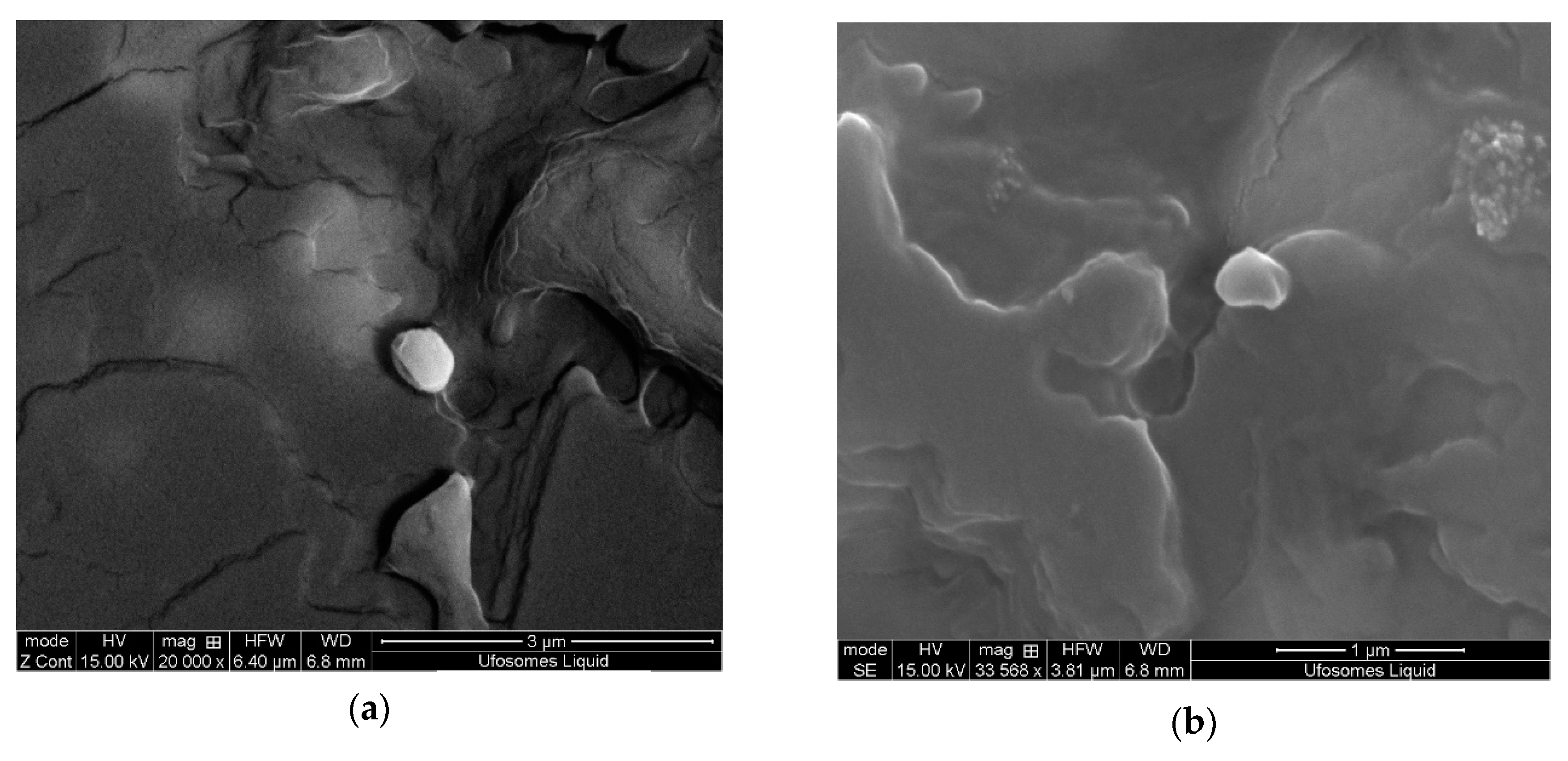
2.2. Surface Morphology
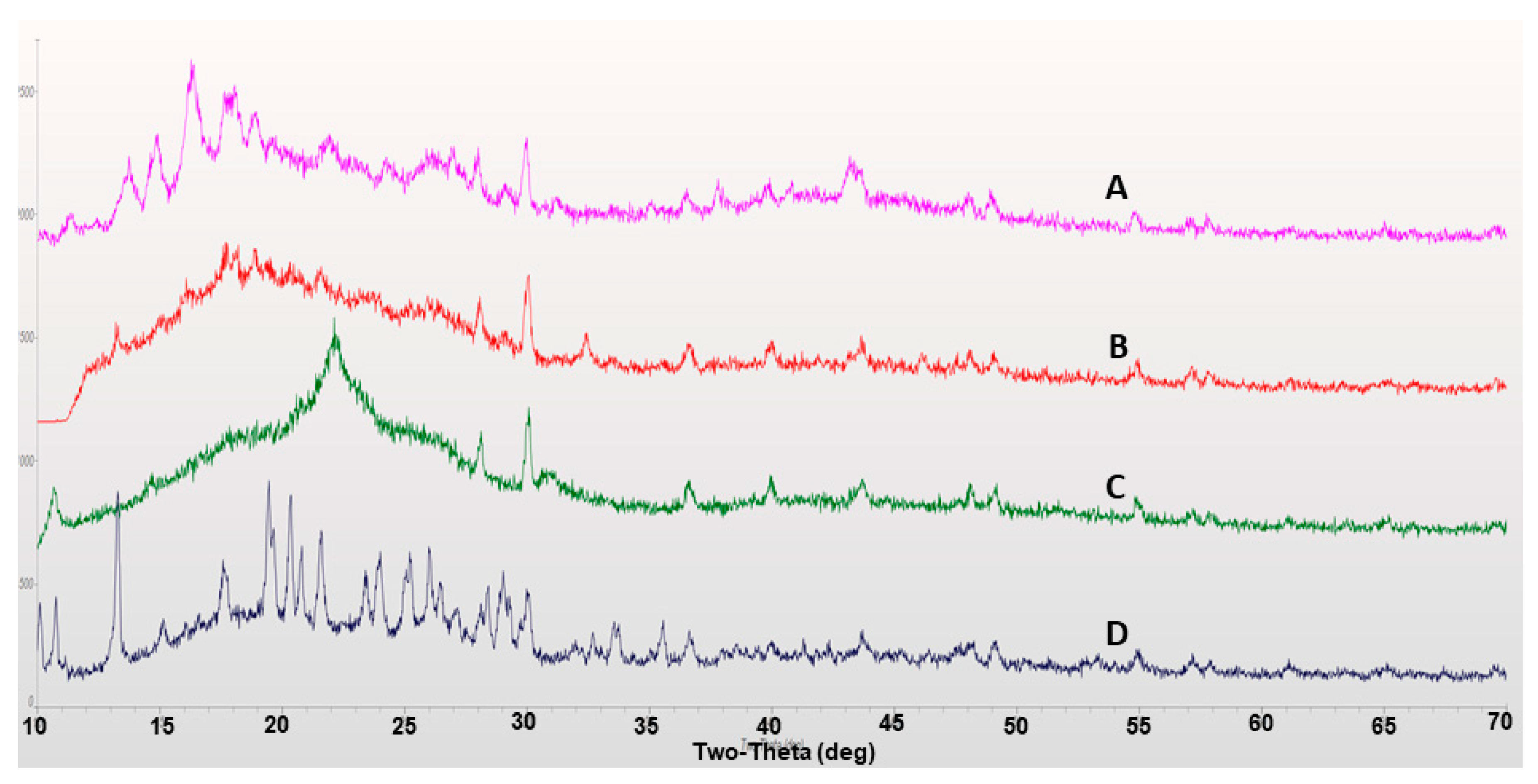
2.3. X-ray Diffraction
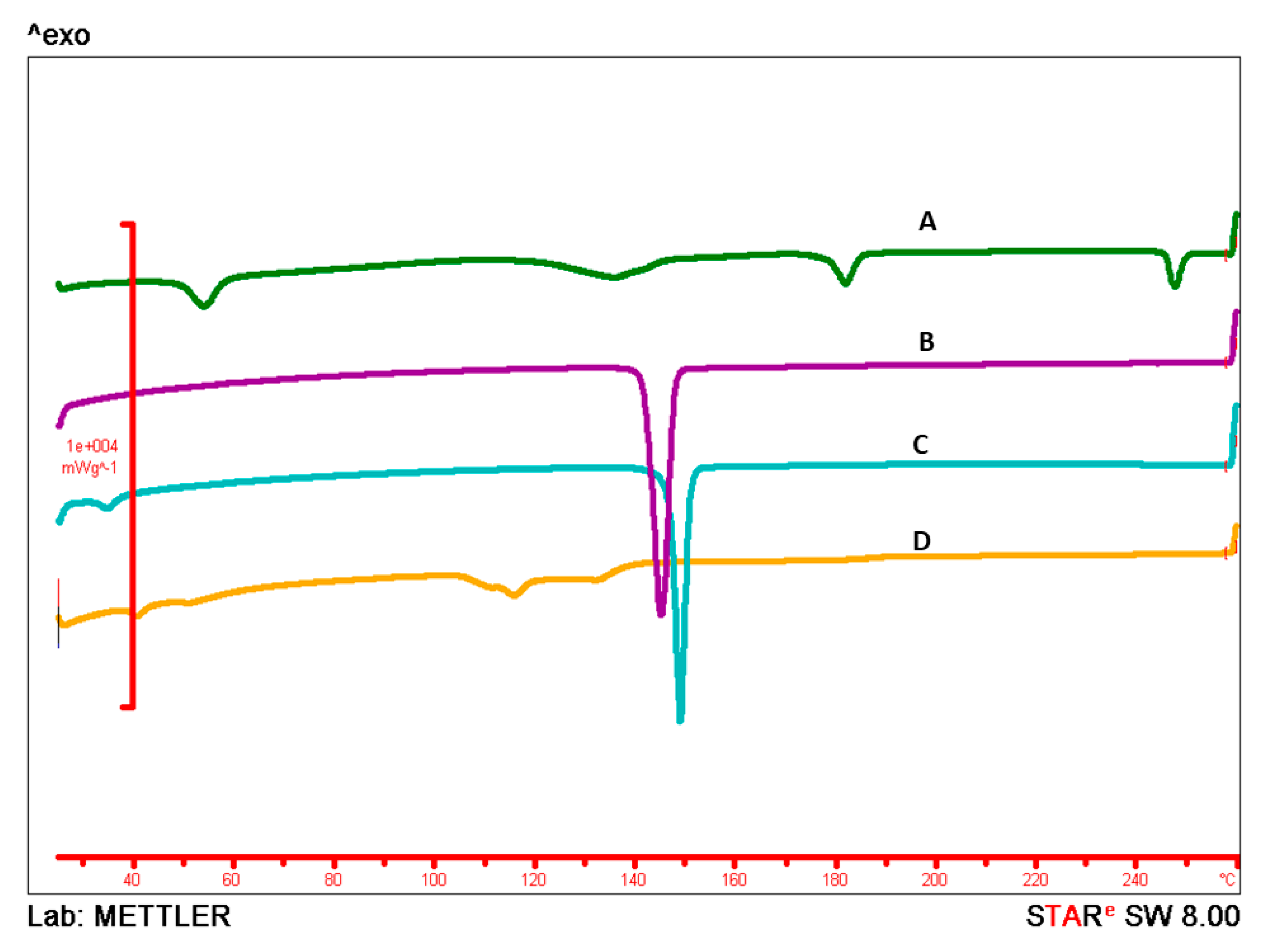
2.4. Differential Scanning Calorimetry
2.5. In-Vitro Permeation Studies
2.5.1. Skin Diffusion Studies
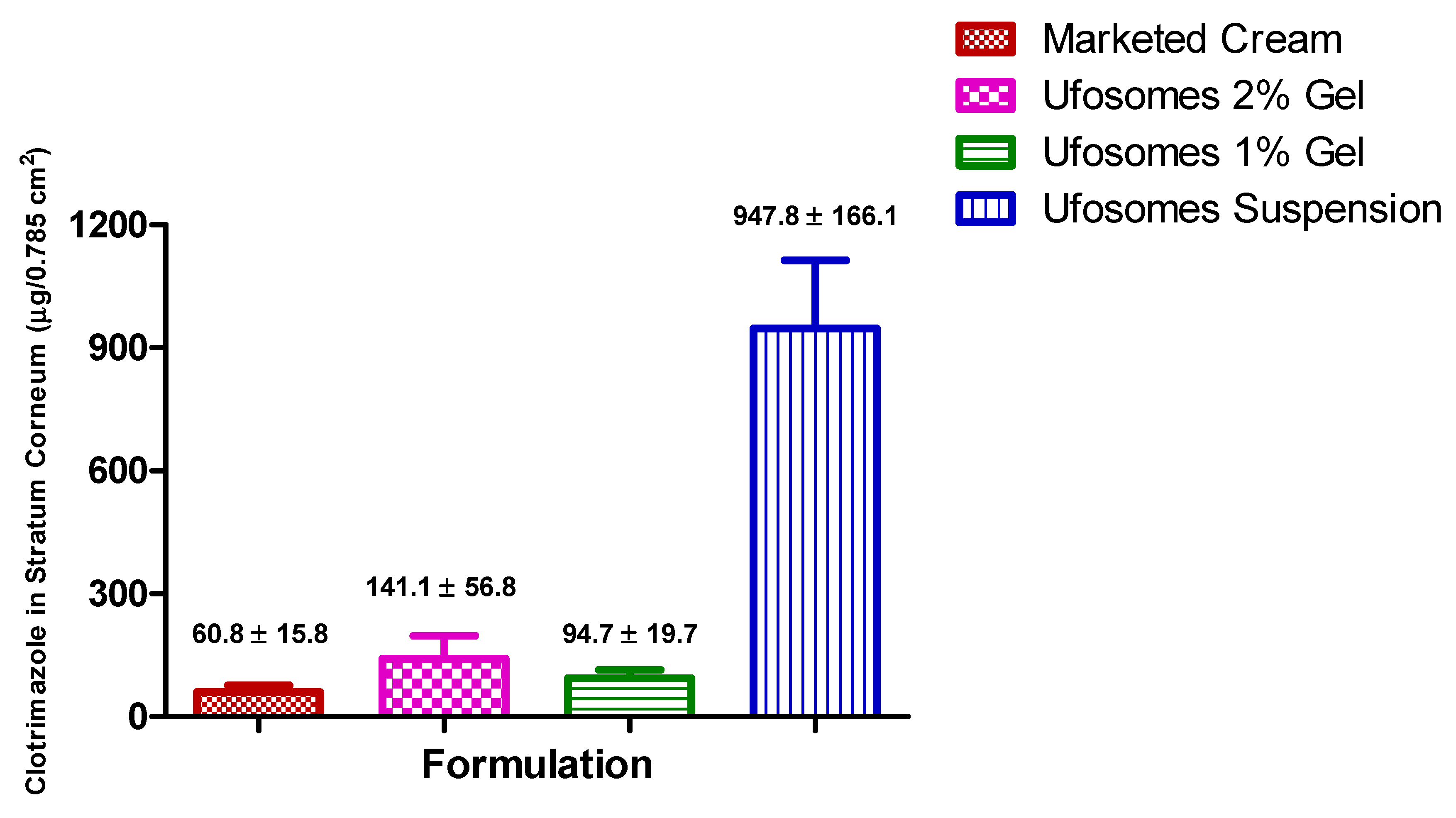
2.5.2. Skin Retention Study (Tape-Stripping)
3. Materials and Methods
3.1. Materials
3.2. Methods
3.2.1. Preparation of Ufosomes
3.2.2. Determination of Vesicle Size, Polydispersity Index, and Zeta Potential
3.2.3. Clotrimazole Quantification by HPLC
3.2.4. Determination of Entrapment Efficiency
3.2.5. Surface Morphology
3.2.6. XRD Analysis
3.2.7. DSC
3.2.8. In-Vitro Permeation Studies
Preparation of Skin
Automated Flow through Diffusion Cells
Tape Stripping
3.2.9. Statistical Analysis
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bongomin, F.; Gago, S.; Oladele, R.O.; Denning, W.D. Global and Multi-National Prevalence of Fungal Diseases—Estimate Precision. J. Fungi 2017, 3, 57. [Google Scholar] [CrossRef] [PubMed]
- AbouSamra, M.M.; Basha, M.; Awad, G.E.A.; Mansy, S.S. A promising nystatin nanocapsular hydrogel as an antifungal polymeric carrier for the treatment of topical candidiasis. J. Drug Deliv. Sci. Technol. 2019, 49, 365–374. [Google Scholar] [CrossRef]
- Gupta, M.; Sharma, V.; Chauhan, N.S. Chapter 11—Promising Novel Nanopharmaceuticals for Improving Topical Antifungal Drug Delivery. In Nano- and Microscale Drug Delivery Systems; Grumezescu, A.M., Ed.; Elsevier: Amsterdam, The Netherlands, 2017; pp. 197–228. [Google Scholar] [CrossRef]
- Shivakumar, H.N.; Juluri, A.; Desai, B.G.; Murthy, S.N. Ungual and transungual drug delivery. Drug Dev. Ind. Pharm. 2012, 38, 901–911. [Google Scholar] [CrossRef] [PubMed]
- Alam, M.A.; Al-Janoobi, F.I.; Alzahrani, K.A.; Al-Agamy, M.H.; Abdelgalil, A.A.; Al-Mohizea, A.M. In-vitro efficacies of topical microemulsions of clotrimazole and ketoconazole; and in-vivo performance of clotrimazole microemulsion. J. Drug Deliv. Sci. Technol. 2017, 39, 408–416. [Google Scholar] [CrossRef]
- Maheshwari, R.G.S.; Tekade, R.K.; Sharma, P.A.; Darwhekar, G.; Tyagi, A.; Patel, R.P.; Jain, D.K. Ethosomes and ultradeformable liposomes for transdermal delivery of clotrimazole: A comparative assessment. Saudi Pharm. J. 2012, 20, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Nami, S.; Aghebati-Maleki, A.; Morovati, H.; Aghebati-Maleki, L. Current antifungal drugs and immunotherapeutic approaches as promising strategies to treatment of fungal diseases. Biomed. Pharmacother. 2019, 110, 857–868. [Google Scholar] [CrossRef]
- Bseiso, E.A.; Nasr, M.; Sammour, O.; el Gawad, N.A.A. Recent advances in topical formulation carriers of antifungal agents. Indian J. Dermatol. Venereol. Leprol. 2015, 81, 457–463. [Google Scholar] [CrossRef]
- Gupta, P.N.; Mishra, V.; Rawat, A.; Dubey, P.; Mahor, S.; Jain, S.; Chatterji, D.P.; Vyas, S.P. Non-invasive vaccine delivery in transfersomes, niosomes and liposomes: A comparative study. Int. J. Pharm. 2005, 293, 73–82. [Google Scholar] [CrossRef]
- Juluri, A.; Modepalli, N.; Jo, S.; Repka, M.A.; Shivakumar, H.N.; Murthy, N.S. Minimally invasive transdermal delivery of iron-dextran. J. Pharm. Sci. 2013, 102, 987–993. [Google Scholar] [CrossRef]
- Juluri, S.A.; Murthy, N. Transdermal iontophoretic delivery of a liquid lipophilic drug by complexation with an anionic cyclodextrin. J. Control. Release 2014, 189, 11–18. [Google Scholar] [CrossRef]
- Pople, P.V.; Singh, K.K. Development and evaluation of colloidal modified nanolipid carrier: Application to topical delivery of tacrolimus. Eur. J. Pharm. Biopharm. 2011, 79, 82–94. [Google Scholar] [CrossRef] [PubMed]
- Santos, S.S.; Lorenzoni, A.; Ferreira, L.M.; Mattiazzi, J.; Adams, A.I.H.; Denardi, L.B.; Alves, S.H.; Schaffazick, S.R.; Cruz, L. Clotrimazole-loaded Eudragit® RS100 nanocapsules: Preparation, characterization and in vitro evaluation of antifungal activity against Candida species. Mater. Sci. Eng. C 2013, 33, 1389–1394. [Google Scholar] [CrossRef] [PubMed]
- Waugh, C.D. Clotrimazole. XPharm Compr. Pharmacol. Ref. 2007, 2011, 1–4. [Google Scholar] [CrossRef]
- Ravani, L.; Esposito, E.; Bories, C.; Moal, V.L.-L.; Loiseau, P.M.; Djabourov, M.; Cortesi, R.; Bouchemal, K. Clotrimazole-loaded nanostructured lipid carrier hydrogels: Thermal analysis and in vitro studies. Int. J. Pharm. 2013, 454, 695–702. [Google Scholar] [CrossRef] [PubMed]
- Esposito, E.; Ravani, L.; Contado, C.; Costenaro, A.; Drechsler, M.; Rossi, D.; Menegatti, E.; Grandini, A.; Cortesi, R. Clotrimazole nanoparticle gel for mucosal administration. Mater. Sci. Eng. C 2013, 33, 411–418. [Google Scholar] [CrossRef] [PubMed]
- Manca, M.L.; Usach, I.; Peris, J.E.; Ibba, A.; Orrù, G.; Valenti, D.; Escribano-Ferrer, E.; Gomez-Fernandez, J.C.; Aranda, F.J.; Fadda, A.M.; et al. Optimization of Innovative Three-Dimensionally-Structured Hybrid Vesicles to Improve the Cutaneous Delivery of Clotrimazole for the Treatment of Topical Candidiasis. Pharmaceutics 2019, 11, 263. [Google Scholar] [CrossRef] [PubMed]
- Csongradi, C.; du Plessis, J.; Aucamp, M.E.; Gerber, M. Topical delivery of roxithromycin solid-state forms entrapped in vesicles. Eur. J. Pharm. Biopharm. 2017, 114, 96–107. [Google Scholar] [CrossRef] [PubMed]
- Patel, D.M.; Patel, C.N.; Jani, R. Ufasomes: A vesicular drug delivery. Syst. Rev. Pharm. 2011, 2. [Google Scholar] [CrossRef]
- USFDA. Inactive Ingredient Search for Approved Drug Products. Available online: https://www.accessdata.fda.gov/scripts/cder/iig/index.cfm (accessed on 28 July 2019).
- 10 Final Report on the Safety Assessment of Cholesterol. J. Am. Coll. Toxicol. 1986, 5, 491–516. [CrossRef]
- Doppalapudi, S.; Jain, A.; Chopra, D.K.; Khan, W. Psoralen loaded liposomal nanocarriers for improved skin penetration and efficacy of topical PUVA in psoriasis. Eur. J. Pharm. Sci. 2017, 96, 515–529. [Google Scholar] [CrossRef] [PubMed]
- Kavian, Z.; Alavizadeh, S.H.; Golmohamadzadeh, S.; Badiee, A.; Khamesipour, A.; Jaafari, M.R. Development of topical liposomes containing miltefosine for the treatment of Leishmania major infection in susceptible BALB/c mice. Acta Trop. 2019, 196, 142–149. [Google Scholar] [CrossRef] [PubMed]
- Md, S.; Haque, S.; Madheswaran, T.; Zeeshan, F.; Meka, V.S.; Radhakrishnan, A.K.; Kesharwani, P. Lipid based nanocarriers system for topical delivery of photosensitizers. Drug Discov. Today 2017, 22, 1274–1283. [Google Scholar] [CrossRef] [PubMed]
- Roberts, M.S.; Mohammed, Y.; Pastore, M.N.; Namjoshi, S.; Yousef, S.; Alinaghi, A.; Haridass, I.N.; Abd, E.; Leite-Silva, V.R.; Benson, H.A.E.; et al. Topical and cutaneous delivery using nanosystems. J. Control. Release 2017, 247, 86–105. [Google Scholar] [CrossRef] [PubMed]
- Meng, S.; Sun, L.; Wang, L.; Lin, Z.; Liu, Z.; Xi, L.; Wang, Z.; Zheng, Y. Loading of water-insoluble celastrol into niosome hydrogels for improved topical permeation and anti-psoriasis activity. Colloids Surf. B Biointerfaces 2019, 182, 110352. [Google Scholar] [CrossRef] [PubMed]
- Kravchenko, I.; Boyko, Y.; Novikova, N.; Egorova, A.; Andronati, S. Influence of cholesterol and its esters on skin penetration in vivo and in vitro in rats and mice. Ukr. Bioorg. Acta 2011, 1, 17–21. [Google Scholar]
- Witteveen, F. Topical Flavouring Compositions Comprising Oleic Acid and Sodium Oleate. U.S. Patent US20180042289A1, 15 February 2018. Available online: https://patentimages.storage.googleapis.com/36/03/66/a8e8457f053715/US20180042289A1.pdf (accessed on 28 August 2019).
- Oliveira, M.B.; Calixto, G.; Graminha, M.; Cerecetto, H.; González, M.; Chorilli, M. Development, Characterization, and In Vitro Biological Performance of Fluconazole-Loaded Microemulsions for the Topical Treatment of Cutaneous Leishmaniasis. BioMed Res. Int. 2015, 2015, 396894. [Google Scholar] [CrossRef] [PubMed]
- Salama, A.H.; Aburahma, M.H. Ufasomes nano-vesicles-based lyophilized platforms for intranasal delivery of cinnarizine: Preparation, optimization, ex-vivo histopathological safety assessment and mucosal confocal imaging. Pharm. Dev. Technol. 2016, 21, 706–715. [Google Scholar] [CrossRef]
- Tavano, L.; Mazzotta, E.; Muzzalupo, R. Innovative topical formulations from diclofenac sodium used as surfadrug: The birth of Diclosomes. Colloids Surf. B Biointerfaces 2018, 164, 177–184. [Google Scholar] [CrossRef]
- Das, S.; Ng, W.K.; Tan, R.B.H. Are nanostructured lipid carriers (NLCs) better than solid lipid nanoparticles (SLNs): Development, characterizations and comparative evaluations of clotrimazole-loaded SLNs and NLCs? Eur. J. Pharm. Sci. 2012, 47, 139–151. [Google Scholar] [CrossRef]
- Bolla, P.K.; Kalhapure, R.S.; Rodriguez, V.A.; Ramos, D.V.; Dahl, A.; Renukuntla, J. Preparation of solid lipid nanoparticles of furosemide-silver complex and evaluation of antibacterial activity. J. Drug Deliv. Sci. Technol. 2019. [Google Scholar] [CrossRef]
- Renukuntla, J. FSE–Ag complex NS: Preparation and evaluation of antibacterial activity. IET Nanobiotechnol. 2018, 1, 1–5. [Google Scholar] [CrossRef]
- Jaiswal, M.K.; Pradhan, A.; Banerjee, R.; Bahadur, D. Dual pH and temperature stimuli-responsive magnetic nanohydrogels for thermo-chemotherapy. J. Nanosci. Nanotechnol. 2014, 14, 4082–4089. [Google Scholar] [CrossRef] [PubMed]
- Bose, S.; Michniak-Kohn, B. Preparation and characterization of lipid based nanosystems for topical delivery of quercetin. Eur. J. Pharm. Sci. 2013, 48, 442–452. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, L.N.M.; Franz-Montan, M.; Breitkreitz, M.C.; Alcântara, A.C.S.; Castro, S.R.; Guilherme, V.A.; Barbosa, E.; de Paula, R.M. Nanostructured lipid carriers as robust systems for topical lidocaine-prilocaine release in dentistry. Eur. J. Pharm. Sci. 2016, 93, 192–202. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, V.A.; Bolla, P.K.; Kalhapure, R.S.; Boddu, S.H.S.; Neupane, R.; Franco, J.; Renukuntla, J. Preparation and Characterization of Furosemide-Silver Complex Loaded Chitosan Nanoparticles. Processes 2019, 7, 206. [Google Scholar] [CrossRef]
- Buchiraju, R.; Sreekanth, D.N.; Bhargavi, S.; Rao, C.H.; Kommu, A.; Kishore, J.; Chebrolu, B.; Yedulapurapu, N.; Bosco, D. Vesicular Drug Delivery System -An Over View. Res. J. Pharm. Biol. Chem. Sci. 2013, 4, 462–474. Available online: https://www.researchgate.net/publication/255786699_Vesicular_Drug_Delivery_System_-An_Over_View (accessed on 28 August 2019).
- Ruela, A.L.M.; Figueiredo, E.C.; Perissinato, A.G.; Lima, A.C.Z.; AraÃ\textordmasculinejo, M.B.; Pereira, G.R. In vitro evaluation of transdermal nicotine delivery systems commercially available in Brazil, Brazilian. J. Pharm. Sci. 2013, 49, 579–588. Available online: http://www.scielo.br/scielo.php?script=sci_arttext&pid=S1984-82502013000300020&nrm=iso (accessed on 28 August 2019).
- Azarmi, S.; Roa, W.; Lobenberg, R. Current perspectives in dissolution testing of conventional and novel dosage forms. Int. J. Pharm. 2007, 328, 12–21. [Google Scholar] [CrossRef]
- Córdoba-Díaz, M.; Nova, M.; Elorza, B.; Córdoba-Díaz, D.; Chantres, J.R.; Córdoba-Borrego, M. Validation protocol of an automated in-line flow-through diffusion equipment for in vitro permeation studies. J. Control. Release 2000, 69, 357–367. [Google Scholar] [CrossRef]
- Kaewbanjong, J.; Amnuaikit, T.; Souto, E.B.; Boonme, P. Antidermatophytic Activity and Skin Retention of Clotrimazole Microemulsion and Microemulsion-Based Gel in Comparison to Conventional Cream. Skin Pharmacol. Physiol. 2018, 31, 292–297. [Google Scholar] [CrossRef]
- Dwivedi, A.; Mazumder, A.; Fox, L.T.; Brümmer, A.; Gerber, M.; du Preez, J.L.; Haynes, R.K.; du Plessis, J. In vitro skin permeation of artemisone and its nano-vesicular formulations. Int. J. Pharm. 2016, 503, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.; Bhardwaj, A.; Vij, M.; Bajpai, P.; Goutam, N.; Kumar, L. Oleic acid vesicles: A new approach for topical delivery of antifungal agent. Artif. Cells Nanomed. Biotechnol. 2014, 42, 95–101. [Google Scholar] [CrossRef] [PubMed]
- Barbero, A.M.; Frasch, H.F. Effect of Frozen Human Epidermis Storage Duration and Cryoprotectant on Barrier Function Using Two Model Compounds. Skin Pharmacol. Physiol. 2016, 29, 31–40. [Google Scholar] [CrossRef] [PubMed]
- Pere, C.P.P.; Economidou, S.N.; Lall, G.; Ziraud, C.; Boateng, J.S.; Alexander, B.D.; Lamprou, D.A.; Douroumis, D. 3D printed microneedles for insulin skin delivery. Int. J. Pharm. 2018, 544, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Hopf, N.B.; Berthet, A.; Vernez, D.; Langard, E.; Spring, P.; Gaudin, R. Skin permeation and metabolism of di(2-ethylhexyl) phthalate (DEHP). Toxicol. Lett. 2014, 224, 47–53. [Google Scholar] [CrossRef] [PubMed]
- De Leon, A.S.; Molina, M.; Wedepohl, S.; Munoz-Bonilla, A.; Rodriguez-Hernandez, J.; Calderon, M. Immobilization of Stimuli-Responsive Nanogels onto Honeycomb Porous Surfaces and Controlled Release of Proteins. Langmuir 2016, 32, 1854–1862. [Google Scholar] [CrossRef] [PubMed]
- Kahraman, E.; Neşetoğlu, N.; Güngör, S.; Ünal, D.Ş.; Özsoy, Y. The combination of nanomicelles with terpenes for enhancement of skin drug delivery. Int. J. Pharm. 2018, 551, 133–140. [Google Scholar] [CrossRef]
- Binder, L.; Jatschka, J.; Kulovits, E.M.; Seeböck, S.; Kählig, H.; Valenta, C. Simultaneous penetration monitoring of oil component and active drug from fluorinated nanoemulsions. Int. J. Pharm. 2018, 552, 312–318. [Google Scholar] [CrossRef]
Sample Availability: Not available. |



| Formulation | Clotrimazole:Cholesterol:Sodium Oleate | Vesicle Diameter (nm) | Polydispersity Index | Zeta Potential (mV) |
|---|---|---|---|---|
| Ufo_1 | 1:0.5:1 | 1177 ± 156 | 0.414 ± 0.164 | −74 ± 3 |
| Ufo_2 | 1:1:0.5 | 848 ± 239 | 0.638 ± 0.166 | −74 ± 3 |
| Ufo_3 | 1:1:1 | 432 ± 140 | 0.583 ± 0.069 | −74 ± 5 |
| Ufo_4 | 1:2:1 | 374 ± 67 | 0.589 ± 0.064 | −75 ± 7 |
| Ufo_5 | 1:1:2 | 752 ± 179 | 0.702 ± 0.067 | −101 ± 5 |
| Ufo_6 | 1:2:2 | 234 ± 59 | 0.581 ± 0.132 | −98 ± 3 |
| Formulation | Average Vesicle Diameter (nm) | Size Distribution (nm) (Mean ± SD) | Intensity (%) |
|---|---|---|---|
| Ufo_1 | 1282 | 1207 ± 342 | 93.7 |
| 128 ± 27 | 5.2 | ||
| 5560 | 1.1 | ||
| Ufo_2 | 894 | 947 ± 191 | 82.7 |
| 96 ± 17 | 17.3 | ||
| Ufo_3 | 493 | 396 ± 80 | 72.5 |
| 68 ± 12 | 27.5 | ||
| Ufo_4 | 367 | 546 ± 140 | 65 |
| 86 ± 21 | 35 | ||
| Ufo_5 | 720 | 808 ± 167 | 59.6 |
| 123 ± 28 | 40.4 | ||
| Ufo_6 | 207 | 144 ± 50 | 71.6 |
| 782 ± 194 | 19.4 | ||
| 42 ± 9 | 9 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bolla, P.K.; Meraz, C.A.; Rodriguez, V.A.; Deaguero, I.; Singh, M.; Yellepeddi, V.K.; Renukuntla, J. Clotrimazole Loaded Ufosomes for Topical Delivery: Formulation Development and In-Vitro Studies. Molecules 2019, 24, 3139. https://doi.org/10.3390/molecules24173139
Bolla PK, Meraz CA, Rodriguez VA, Deaguero I, Singh M, Yellepeddi VK, Renukuntla J. Clotrimazole Loaded Ufosomes for Topical Delivery: Formulation Development and In-Vitro Studies. Molecules. 2019; 24(17):3139. https://doi.org/10.3390/molecules24173139
Chicago/Turabian StyleBolla, Pradeep Kumar, Carlos A. Meraz, Victor A. Rodriguez, Isaac Deaguero, Mahima Singh, Venkata Kashyap Yellepeddi, and Jwala Renukuntla. 2019. "Clotrimazole Loaded Ufosomes for Topical Delivery: Formulation Development and In-Vitro Studies" Molecules 24, no. 17: 3139. https://doi.org/10.3390/molecules24173139
APA StyleBolla, P. K., Meraz, C. A., Rodriguez, V. A., Deaguero, I., Singh, M., Yellepeddi, V. K., & Renukuntla, J. (2019). Clotrimazole Loaded Ufosomes for Topical Delivery: Formulation Development and In-Vitro Studies. Molecules, 24(17), 3139. https://doi.org/10.3390/molecules24173139