Pharmacodynamics of Five Anthraquinones (Aloe-emodin, Emodin, Rhein, Chysophanol, and Physcion) and Reciprocal Pharmacokinetic Interaction in Rats with Cerebral Ischemia
Abstract
1. Introduction
2. Results
2.1. Pharmacodynamic Results
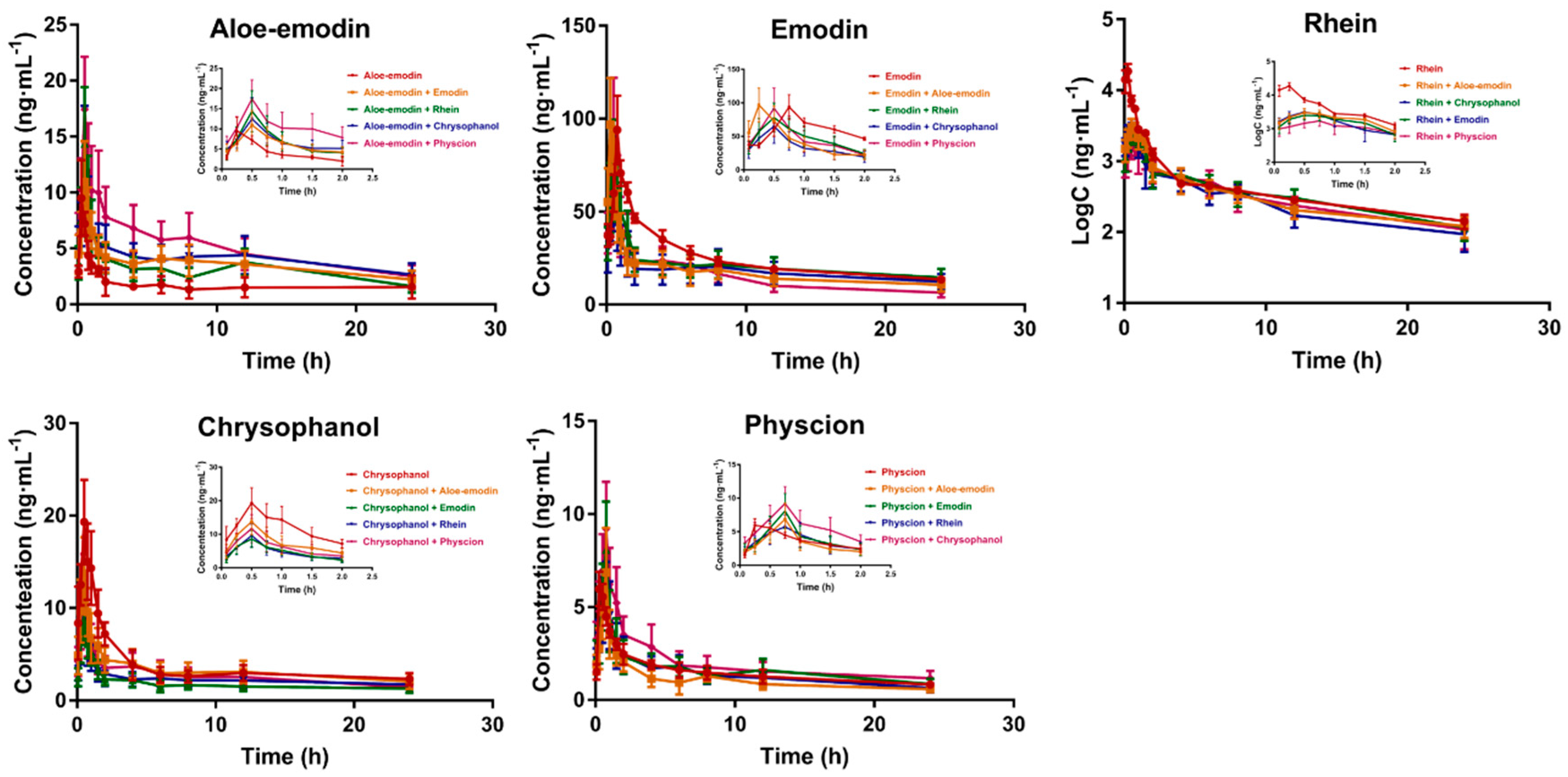
2.2. Pharmacokinetics Interaction Studies
3. Discussion
4. Materials and Methods
4.1. Material
4.1.1. Chemicals and Materials
4.1.2. Animals and Cerebral Ischemia Reperfusion Model in Rats
4.2. Pharmacodynamic Study of Anticerebral Ischemia-Reperfusion Injury
4.2.1. Grouping and Administration
4.2.2. Measurement and Evaluation
4.3. Pharmacokinetic Interaction among Anthraquinone Aglycones in Model Rats
4.3.1. Apparatus and Operation Conditions
4.3.2. Plasma Sample Preparation
4.3.3. Standard Solution Preparation and Sample Quality Control
4.3.4. Administration and Sample Collection
4.4. Statistical Methods
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Russo, T.; Felzani, G.; Marini, C. Stroke in the very old: A systematic review of studies on incidence, outcome, and resource use. J. Aging Res. 2011, 2011, 108785. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; Lees, K.R.; Ringleb, P.A.; Bladin, C.; Collas, D.; Toni, D.; Ford, G.A. Outcome after stroke thrombolysis in patients >80 years treated within 3 hours vs. > 3–4.5 hours. Neurology 2017, 89, 1561–1568. [Google Scholar] [CrossRef]
- Liang, J.; Qi, Z.F.; Liu, W.L.; Wang, P.; Shi, W.J.; Dong, W.; Ji, X.M.; Luo, Y.M.; Liu, K.J. Normobaric hyperoxia slows blood-brain barrier damage and expands the therapeutic time window for tissue-type plasminogen activator treatment in cerebral ischemia. Stroke 2015, 46, 1344–1351. [Google Scholar] [CrossRef] [PubMed]
- Donnan, G.A.; Davis, S.M.; Parsons, M.W.; Ma, H.; Dewey, H.M.; Howells, D.W. How to make better use of thrombolytic therapy in acute ischemic stroke. Nat. Rev. Neurol 2011, 7, 400–409. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, N.; Kellert, L.; Lees, K.R.; Mikulik, R.; Tatlisumak, T.; Toni, D. Results of intravenous thrombolysis within 4.5 to 6 hours and updated results within 3 to 4.5 hours of onset of acute ischemic stroke recorded in the Safe Implementation of Treatment in Stroke International Stroke Thrombolysis Register (SITS-ISTR): An observational study. JAMA Neurol. 2013, 70, 837–844. [Google Scholar] [PubMed]
- Puyal, J.; Ginet, V.; Clarke, P.G. Multiple interacting cell death mechanisms in the mediation of excitotoxicity and ischemic brain damage: A challenge for neuroprotection. Prog. Neurobiol. 2013, 105, 24–48. [Google Scholar] [CrossRef] [PubMed]
- Miao, X.L.; Huang, Y.; Pei, J.; Yang, Y.S.; Wang, X.Z.; Tan, J.L.; Li, J.; Gu, W.; Cao, X.L.; Dong, M.J.; et al. The Regression Analysis on Syndromes Grade for Yin-yang Syndrome Differentiation of in Acute Phase of Ischemic Stroke. Chin. J. Integr. Trad. West. Med. 2007, 5, 1166–1167. [Google Scholar]
- Wang, Y.; Ren, Q.Y.; Zhang, X.; Lu, H.L.; Chen, J. Neuroprotective Mechanisms of Calycosin Against Focal Cerebral Ischemia and Reperfusion Injury in Rats. Cell Physiol. Biochem. 2018, 45, 537–546. [Google Scholar]
- Liu, P.; Zhao, H.P.; Wang, R.L.; Wang, P.; Tao, Z.; Gao, L.; Yan, F.; Liu, X.G.; Yu, S.; Ji, X.M.; et al. MicroRNA-424 protects against focal cerebral ischemia and reperfusion injury in mice by suppressing oxidative stress. Stroke 2015, 46, 513–519. [Google Scholar] [CrossRef]
- Zhang, N.; Zhang, X.J.; Liu, X.X.; Wang, H.; Xue, J.; Yu, J.Y.; Kang, N.; Wang, X.L. Chrysophanol inhibits NALP3 inflammasome activation and ameliorates cerebral ischemia/reperfusion in mice. Mediat. Inflamm. 2014, 2014, 370530. [Google Scholar]
- Abu-Amara, M.; Yang, S.Y.; Quaglia, A.; Rowley, P.; Fuller, B.; Seifalian, A.; Davidson, B. Role of endothelial nitric oxide synthase in remote ischemic preconditioning of the mouse liver. Liver Transpl. 2011, 17, 610–619. [Google Scholar] [CrossRef]
- Chen, S.D.; Yang, D.I.; Lin, T.K.; Shaw, F.Z.; Liou, C.W.; Chuang, Y.C. Roles of oxidative stress, apoptosis, PGC-1 alpha and mitochondrial biogenesis in cerebral ischemia. Int. J. Mol. Sci. 2011, 12, 7199–7215. [Google Scholar] [CrossRef] [PubMed]
- Kadiiska, M.B.; Peddada, S.; Herbert, R.A.; Basu, S.; Hensley, K.; Jones, D.P.; Hatch, G.E.; Mason, R.P. Biomarkers of oxidative stress study VI. Endogenous plasma antioxidants fail as useful biomarkers of endotoxin-induced oxidative stress. Free Radic. Biol. Med. 2015, 81, 100–106. [Google Scholar] [CrossRef]
- Pejin, B.; Jovanović, K.K.; Mojović, M.; Savić, A.G. New and highly potent antitumor natural products from marine-derived fungi: Covering the period from 2003 to 2012. Curr. Top. Med. Chem. 2013, 13, 2745–2766. [Google Scholar] [CrossRef]
- Wang, J.; Gou, L.L.; Yang, G.; Wang, Y.Y. Methodology and prospects of study on theory of compatibility of prescriptions in traditional Chinese medicine. World Sci. Tech./Mod. Trad. Chin. Med. Mater. Med. 2006, 8, 1–5. [Google Scholar]
- Yu, C.P.; Shia, C.S.; Lin, H.J.; Hsieh, Y.W.; Lin, S.P.; Hou, Y.C. Analysis of the pharmacokinetics and metabolism of aloe-emodin following intravenous and oral administrations in rats. Biomed. Chromatogr. 2016, 30, 1641–1647. [Google Scholar] [CrossRef]
- Ullah, H.M.A.; Kim, J.; Rehman, N.U.; Kim, H.J.; Ahn, M.J.; Chuang, H.J. A Simple and Sensitive Liquid Chromatography with Tandem Mass Spectrometric Method for the Simultaneous Determination of Anthraquinone Aglycones and Their Aglycones in Rat Plasma: Application to a Pharmacokinetic Study of Rumex acetosa Extract. Pharmaceutics 2018, 10, 100. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Luo, G.W.; Xiang, Z.; Cai, X.J.; Chen, D.H. Pharmacokinetics and pharmacodynamics study of rhein treating renal fibrosis based on metabonomics approach. Phyto. Med. 2016, 23, 1661–1670. [Google Scholar] [CrossRef] [PubMed]
- Sun, H.; Yin, Q.W.; Zhang, A.H.; Wang, X.J. UPLC-MS/MS performing pharmacokinetic and biodistribution studies of rhein. J. Sep. Sci. 2012, 35, 2063–2068. [Google Scholar] [CrossRef]
- Shia, C.S.; Hou, Y.C.; Tsai, S.Y.; Huieh, P.H.; Leu, Y.L.; Chao, P.W.L. Differences in pharmacokinetics and ex vivo antioxidant activity following intravenous and oral administrations of emodin to rats. J. Pharm. Sci. 2010, 99, 2185–2195. [Google Scholar] [CrossRef]
- Li, J.S.; Liu, J.X.; Zhang, W.Y.; Liang, S.W.; Wang, D.; Fang, J. Preventive effects of emodin on cerebral ischemia injury and expression of the inflammtory factors in rats with cerebral ischemia. China J. Chin. Mater. Med. 2005, 30, 1939–1943. [Google Scholar]
- Liu, T.; Hu, H.T.; Sun, Q.R. Neuroprotective effects of emodin on primary rat cortical neurons apoptosis induced by hydrogen peroxide. Chin. Med. Met. 2010, 33, 1116–1119. [Google Scholar]
- Ma, B.L.; Ma, Y.M.; Yan, D.M.; Zhou, H.; Shi, R.; Wang, T.M.; Yang, Y.; Wang, C.H.; Zhang, N. Effective constituents in xiexin decoction for anti-inflammation. J. Ethnopharmacol. 2009, 125, 151–156. [Google Scholar] [CrossRef]
- Lu, K.; Zhang, C.; Wu, W.J.; Zhou, M.; Tang, Y.M.; Peng, Y. Rhubarb extract has a protective role against radiation-induced brain injury and neuronal cell apoptosis. Mol. Med. Rep. 2015, 12, 2689–2694. [Google Scholar] [CrossRef]
- Guidance for Industy, Bioanalytical Method Validation; US Department of Health and Human Services Food and Drug Administration, Center for Drug Evaluation and Research (CDER), Center for Veterinary Medicine (CV): Washington, DC, USA, 2001; pp. 4–10.
- Xue, J.T.; Shi, Y.L.; Ye, L.M.; Yang, Q.M.; Li, C.Y.; Chen, X.Y.; Jing, Y. Near-infrared spectroscopy for rapid and simultaneous determination of five main active components in rhubarb of different geographical origins and processing. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2018, 205, 419–427. [Google Scholar]
- Feng, S.X.; Li, J.S.; Qu, L.B.; Shi, Y.M.; Zhao, D. Comparative pharmacokinetics of five rhubarb anthraquinones in normal and thrombotic focal cerebral ischemia-induced rats. Phytother. Res. 2013, 27, 1489–1494. [Google Scholar] [CrossRef]
- Song, R.; Lin, H.; Zhang, Z.; Li, Z.; Xu, L.; Dong, H.; Tian, Y. Profiling the metabolic differences of anthraquinone derivatives using liquid chromatography/tandem mass spectrometry with data-dependent acquisition. Rapid Commun. Mass Spectrom. 2009, 23, 537–547. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.; Wang, S.; Li, F.J. Effects of chrysophanol on antioxidative stress andAQP4 in brain tissue of mice induced by cerebral ischemia-reperfusion injury. Chin. Pharmacol. Bull. 2015, 31, 1477–1478. [Google Scholar]
- Wang, S.H.; Liang, C.L.; Zhang, H.H.; Wang, S. Effects of chrysophanol on NO of brain tissue and anti-anoxia in mice with cerebral ischemia-reperfusion injury. Tianjin Med. J. 2017, 45, 593–595. [Google Scholar]
- Wang, S.; Zhang, H.H.; Xue, G.P. Effects of Emodin on Exploratory and Cognitive Function of Mice Experiencing Cerebral Ischemia Reperfusion. Acta Neuropharmacol. 2013, 3, 8–13. [Google Scholar]
- Dong, X.; Fu, J.; Yin, X.B.; Cao, S.; Li, X.C.; Lin, L.F.; Huyiligeqi; Ni, J. Emodin: A Review of its Pharmacology, Toxicity and Pharmacokinetics. Phytother. Res. 2016, 30, 1207–1218. [Google Scholar] [CrossRef]
- Zhao, Y.; Fang, Y.; Zhao, H.; Li, J.; Duan, Y.; Shi, W.; Huang, Y.; Gao, L.; Luo, Y. Chrysophanol inhibits endoplasmic reticulum stress in cerebral ischemia and reperfusion mice. Eur. J. Pharmacol. 2018, 818, 1–9. [Google Scholar] [CrossRef]
- Zhao, Y.; Huang, Y.; Fang, Y.; Zhao, H.; Shi, W.; Li, J.; Duan, Y.; Sun, Y.; Gao, L.; Luo, Y. Chrysophanol attenuates nitrosative/oxidative stress injury in a mouse model of focal cerebral ischemia/reperfusion. J. Pharmacol. Sci. 2018, 138, 16–22. [Google Scholar] [CrossRef]
- Bian, H.T.; Hu, Q.; Liang, X.P.; Chen, D.; Li, B.; Tang, J.P.; Zhang, J.H. Hyperbaric oxygen preconditioning attenuates hemorrhagic transformation through increasing PPARγ in hyperglycemic MCAO rats. Exp. Neurol. 2015, 265, 22–29. [Google Scholar] [CrossRef]
- Matel, N.; Camara, J.; McBride, D.; Camara, R.; Xu, N.; Tang, J.P.; Zhang, J.H. Intranasal wnt3a Attenuates Neuronal Apoptosis through Frz1/PIWIL1a/FOXM1 Pathway in MCAO Rats. J. Neurosci. 2018, 38, 6787–6801. [Google Scholar]
- McBride, D.W.; Zhang, J.H. Precision Stroke Animal Models: The permanent MCAO Model Should Be the Primary Model, Not Transient MCAO. Transl. Stroke Res. 2017, 8, 397–404. [Google Scholar] [CrossRef]
- Yang, J.; Yan, H.; Li, S.; Zhang, M. Berberine Ameliorates MCAO Induced Cerebral Ischemia/Reperfusion Injury via Activation of the BDNF-TrkB-PI3K/Akt Signaling Pathway. Neurochem. Res. 2018, 43, 702–710. [Google Scholar] [CrossRef]
- Morris, G.P.; Wright, A.L.; Tan, R.P.; Gladbach, A.; Ittner, M.; Vissel, B. A Comparative Study of Variables Influencing Ischemic Injury in the Longa and Koizumi Methods of Intraluminal Filament Middle Cerebral Artery Occlusion in Mice. PLoS ONE 2016, 11, e0148503. [Google Scholar] [CrossRef]
- Bachour, S.P.; Hevesi, M.; Bachour, O.; Sweis, B.M.; Mahmoudi, J.; Brekke, J.A.; Divani, A.A. Comparisons between Garcia, Modo, and Longa rodent stroke scales: Optimizing resource allocation in rat models of focal middle cerebral artery occlusion. J. Neurol. Sci. 2016, 364, 136–140. [Google Scholar] [CrossRef]
- Sun, T.; Zeng, G.R.; Jiang, D.J. Neurological behavior in pharmacology and toxicology evaluation. Cent. South Pharm. 2014, 12, 732–734. [Google Scholar]
- Gong, Z.G.; Hu, J.; Wu, X.; Xu, Y.J. The Recent Developments in Sample Preparation for Mass Spectrometry-Based Metabolomics. Crit. Rev. Anal. Chem. 2017, 47, 325–331. [Google Scholar] [CrossRef] [PubMed]
- Jin, Q.Z.; Wang, N.; Liu, Y.F. Study on the Pretreatment of Biological Samples of Traditional Chinese Medicine. Asia-Pac. Tradit. Med. 2014, 10, 67–69. [Google Scholar]
Sample Availability: Samples of the compounds are not available from the authors. |
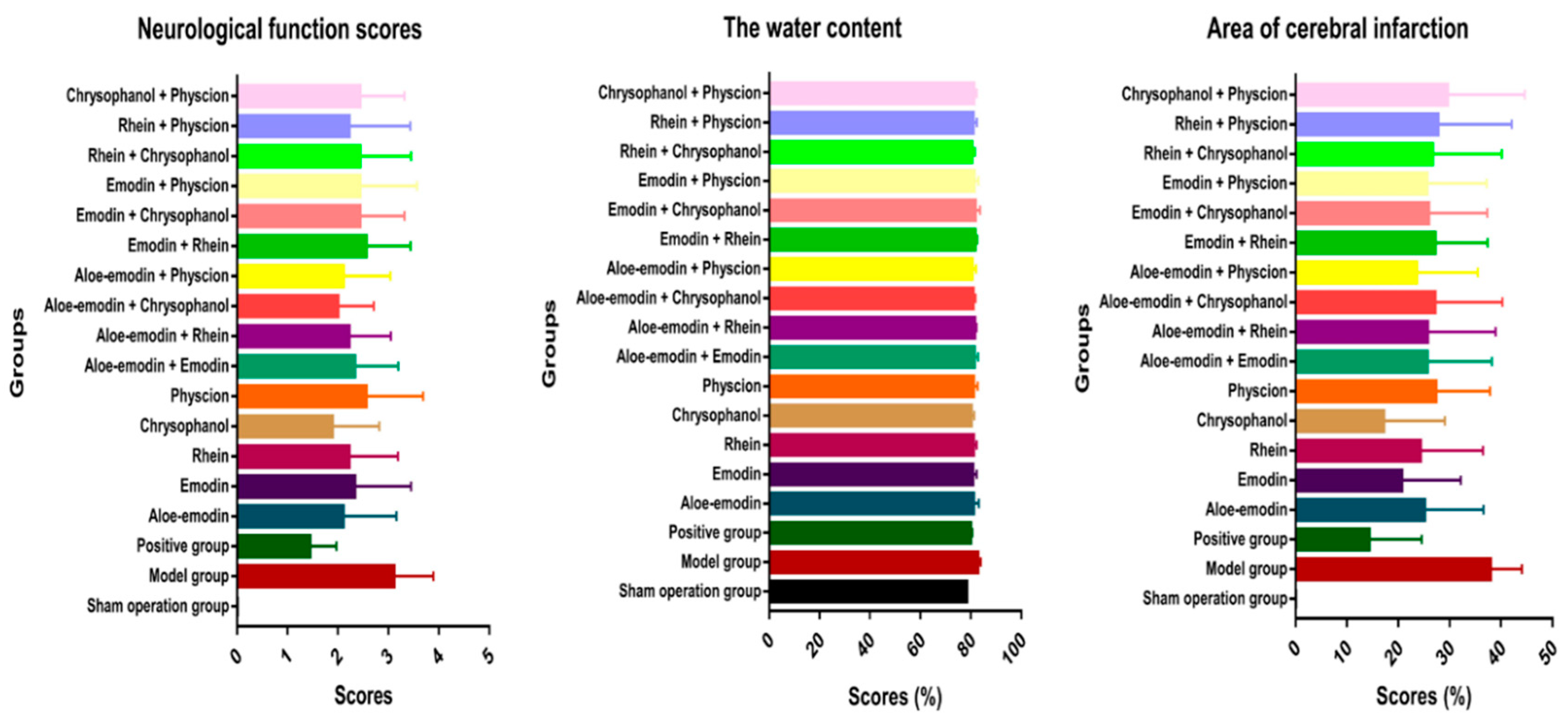
| Group | Neurological Function Score | The Water Content (%) | Area of Cerebral Infarction (%) |
|---|---|---|---|
| Sham operation group | - | 78.40 ± 0.28 | - |
| Model group | 3.11 ± 0.78 ΔΔ | 82.84 ± 1.08 ΔΔ | 37.95 ± 6.13 ΔΔ |
| Positive group | 1.44 ± 0.53 ** | 79.91 ± 0.64 ** | 14.36 ± 10.20 ** |
| Aloe-emodin | 2.11 ± 1.05 * | 81.03 ± 2.15 ** | 25.09 ± 11.47 ** |
| Emodin | 2.33 ± 1.12 | 80.78 ± 1.52 ** | 20.65 ± 11.51 ** |
| Rhein | 2.22 ± 0.97 * | 81.08 ± 1.21 ** | 24.31 ± 12.19 ** |
| Chrysophanol | 1.89 ± 0.93 ** | 80.10 ± 1.21 ** | 17.16 ± 11.94 ** |
| Physcion | 2.56 ± 1.13 | 81.02 ± 1.64 * | 27.32 ± 10.57 * |
| Aloe-emodin + Emodin | 2.33 ± 0.87 | 81.42 ± 1.45 * | 25.62 ± 12.61 * |
| Aloe-emodin + Rhein | 2.22 ± 0.83 * | 81.52 ± 0.70 * | 25.72 ± 13.21 * |
| Aloe-emodin + Chrysophanol | 2.00 ± 0.71 ** | 80.91 ± 0.91 ** | 27.14 ± 13.14 |
| Aloe-emodin + Physcion | 2.11 ± 0.93 * | 80.52 ± 1.53 ** | 23.56 ± 11.92 * |
| Emodin + Rhein | 2.56 ± 0.88 | 81.65 ± 0.91 * | 27.16 ± 10.25 |
| Emodin + Chrysophanol | 2.44 ± 0.88 | 81.69 ± 1.98 * | 25.91 ± 11.41 * |
| Emodin + Physcion | 2.44 ± 1.13 | 81.34 ± 1.66 ** | 25.57 ± 11.63 * |
| Rhein + Chrysophanol | 2.44 ± 1.01 | 80.38 ± 1.27 ** | 26.66 ± 13.49 * |
| Rhein + Physcion | 2.22 ± 1.21 * | 80.89 ± 1.52 * | 27.70 ± 14.38 |
| Chrysophanol + Physcion | 2.44 ± 0.88 | 81.18 ± 1.11 * | 29.58 ± 15.04 |
| Group | Parameters | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| t1/2 (h) | Tmax (h) | Cmax (ng/mL) | AUC0-t | AUC0-∞ | AUMC0-∞ | MRT0-∞ (h) | V/F (L) | Cl/F (L/h) | ||
| (ng·h/mL) | (ng·h/mL) | (ng·h2/mL) | ||||||||
| Aloe-emodin | Aloe-emodin | 14.98 ± 6.48 | 0.32 ± 0.12 | 9.88 ± 2.9 | 42.77 ± 10.09 | 63.18 ± 24.20 | 1524 ± 566.3 | 21.73 ± 8.35 | 4287 ± 1948 | 244.2 ± 118.0 |
| Aloe-emodin + Emodin | 33.26 ± 6.4 ** | 0.45 ± 0.11 | 10.85 ± 1.45 | 88.02 ± 8.32 ** | 214.4 ± 14.32 ** | 9303 ± 703.5 ** | 45.3 ± 6.39 ** | 2857 ± 171.6 * | 59.6 ± 7.76 ** | |
| Aloe-emodin + Rhein | 21.51 ± 6.36 | 0.55 ± 0.11 ** | 14.1 ± 3.04 * | 77.58 ± 7.3 ** | 126.6 ± 15.53 ** | 3323 ± 240.7 ** | 26.61 ± 5.61 | 3181 ± 271.5 | 104.0 ± 12.18 ** | |
| Aloe-emodin+ Chrysophanol | 28.34 ± 4.72 ** | 0.45 ± 0.11 | 12.41 ± 2.53 | 99.62 ± 11.7 ** | 210.4 ± 18.37 ** | 7955 ± 508.8 ** | 38.15 ± 5.3 ** | 2488 ± 330.0 ** | 62.78 ± 5.30 ** | |
| Aloe-emodin + Physcion | 15.49 ± 3.64 | 0.55 ± 0.11 ** | 17.8 ± 4.18 ** | 121.5 ± 19.59 ** | 177.7 ± 16.70 ** | 3641 ± 261.1 ** | 21.2 ± 6.57 | 1556 ± 262.4 ** | 75.65 ± 15.29 ** | |
| Emodin | Emodin | 23.13 ± 3.56 | 0.75 ± 0.00 | 91.65 ± 16.82 | 624.7 ± 73.35 | 1108 ± 191.1 | 33673 ± 10503 | 29.90 ± 4.71 | 1052 ± 119.8 | 31.99 ± 5.15 |
| Emodin + Aloe-emodin | 26.13 ± 4.44 | 0.3 ± 0.11 ** | 95.15 ± 5.47 | 419.5 ± 21.62 ** | 798.8 ± 40.85 ** | 27693 ± 2767 | 32.5 ± 5.44 | 1550 ± 113.0 ** | 44.82 ± 5.12 ** | |
| Emodin + Rhein | 28.97 ± 6.17 * | 0.45 ± 0.11 ** | 77.83 ± 6.2 * | 511.8 ± 40.91 ** | 1194 ± 226.7 | 45531 ± 5933 ** | 41.11 ± 5.04 ** | 1282 ± 165.4 ** | 30.98 ± 4.08 | |
| Emodin + Chrysophanol | 26.73 ± 3.18 | 0.45 ± 0.11 ** | 65.19 ± 4.96 ** | 433.4 ± 33.69 ** | 906.6 ± 29.35 * | 33509 ± 3389 | 38.18 ± 4.87 ** | 1475 ± 151.6 ** | 37.92 ± 4.57 | |
| Emodin + Physcion | 5.49 ± 0.78 ** | 0.5 ± 0 ** | 91.21 ± 8.89 | 373.3 ± 54.31 ** | 397.4 ± 82.77 ** | 3464 ± 655.3 ** | 8.64 ± 0.83 ** | 689.7 ± 49.64 ** | 87.65 ± 7.74 ** | |
| Rhein | Rhein | 10.20 ± 2.50 | 0.23 ± 0.06 | 19290 ± 5420 | 18866 ± 1739 | 20893 ± 2262 | 157175 ± 52352 | 7.44 ± 1.87 | 12.08 ± 2.07 | 0.83 ± 0.09 |
| Rhein + Aloe-emodin | 5.21 ± 0.89 ** | 0.6 ± 0.29 ** | 3136 ± 412.6 ** | 10272 ± 1478 ** | 10909 ± 1119 ** | 71400 ± 5075 | 7.17 ± 0.78 | 13.51 ± 1.46 | 1.56 ± 0.53 ** | |
| Rhein + Emodin | 9.26 ± 0.87 | 0.5 ± 0 ** | 2554 ± 511.0 ** | 10861 ± 1055 ** | 11515 ± 1366 ** | 116864 ± 16106 ** | 10.76 ± 1.10 ** | 18.33 ± 1.19 ** | 1.47 ± 0.55 * | |
| Rhein + Chrysophanol | 8.98 ± 0.74 | 0.5 ± 0.18 ** | 3076 ± 299.8 ** | 8914 ± 535.7 ** | 10548 ± 1333 ** | 92427 ± 5960 * | 10.07 ± 1.54 ** | 21.9 ± 2.25 ** | 1.98 ± 0.28 ** | |
| Rhein + Physcion | 10.8 ± 1.12 | 0.75 ± 0.18 ** | 1746 ± 102.8 ** | 8857 ± 845.1 ** | 10500 ± 1367 ** | 124300 ± 17430 ** | 11.42 ± 1.61 ** | 24.18 ± 2.45 ** | 1.72 ± 0.54 ** | |
| Chrysophanol | Chrysophanol | 37.47 ± 14.54 | 0.54 ± 0.10 | 19.01 ± 3.93 | 88.97 ± 10.58 | 185.2 ± 56.36 | 8755 ± 3200 | 42.24 ± 23.55 | 10372 ± 2880 | 236.8 ± 97.59 |
| Chrysophanol + Aloe-emodin | 34.61 ± 4.86 | 0.65 ± 0.11 ** | 15.22 ± 4.55 | 75.17 ± 8.9 ** | 173.6 ± 11.3 | 7441 ± 368 | 44.73 ± 5.03 | 10815 ± 1527 | 248.6 ± 40.56 | |
| Chrysophanol + Emodin | 47.34 ± 11.03 | 0.62 ± 0.15 ** | 8.74 ± 2.09 ** | 45.87 ± 7.42 ** | 121.8 ± 15.29 ** | 7125 ± 450 | 54.53 ± 9.19 | 20629 ± 2753 ** | 313.0 ± 42.9 * | |
| Chrysophanol + Rhein | 38.18 ± 5.76 | 0.72 ± 0.12 ** | 9.17 ± 1.49 ** | 52.47 ± 3.07 ** | 160.2 ± 4.80 | 8390 ± 418 | 57.27 ± 6.35 | 14625 ± 1072 ** | 241.8 ± 19.13 | |
| Chrysophanol + Physcion | 15.75 ± 2.18 ** | 0.67 ± 0.13 ** | 11.8 ± 2.36 ** | 59.38 ± 4.14 ** | 96.01 ± 11.77 ** | 2478 ± 345.7 ** | 19.06 ± 2.38 ** | 9866 ± 1354 | 416.4 ± 48.03 ** | |
| Physcion | Physcion | 30.47 ± 14.4 | 0.38 ± 0.14 | 6.24 ± 0.59 | 36.38 ± 5.58 | 72.50 ± 41.70 | 4492 ± 2151 | 41.50 ± 17.65 | 13170 ± 6030 | 433.4 ± 161.6 |
| Physcion + Aloe-emodin | 26.38 ± 4.99 | 0.75 ± 0.16 ** | 6.78 ± 0.81 | 26.71 ± 4.72 ** | 48.29 ± 6.73 * | 1556 ± 220 | 32.09 ± 5.62 | 20255 ± 4540 ** | 545.1 ± 52.62 * | |
| Physcion + Emodin | 16.65 ± 3.17 | 0.7 ± 0.11 ** | 8.05 ± 0.56 ** | 39.51 ± 2.23 | 60.89 ± 3.57 | 1359 ± 156.28 | 22.82 ± 6.99 | 10336 ± 1131 | 436.5 ± 38.8 | |
| Physcion + Rhein | 12.88 ± 4.28 | 0.75 ± 0 ** | 5.82 ± 0.7 | 34.51 ± 3.92 | 45.52 ± 4.41 * | 759.2 ± 34.69 | 16.52 ± 2.82 | 10773 ± 1823 | 580.0 ± 46.03 ** | |
| Physcion + Chrysophanol | 27.49 ± 2.62 | 0.75±0 ** | 9.14 ± 0.37 ** | 48.45 ± 3.47 ** | 94.39 ± 5.18 | 3346 ± 260 | 35.89 ± 4.75 | 10747 ± 1803 | 276.7 ± 16.66 ** | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, R.-R.; Liu, X.-F.; Feng, S.-X.; Shu, S.-N.; Wang, P.-Y.; Zhang, N.; Li, J.-S.; Qu, L.-B. Pharmacodynamics of Five Anthraquinones (Aloe-emodin, Emodin, Rhein, Chysophanol, and Physcion) and Reciprocal Pharmacokinetic Interaction in Rats with Cerebral Ischemia. Molecules 2019, 24, 1898. https://doi.org/10.3390/molecules24101898
Li R-R, Liu X-F, Feng S-X, Shu S-N, Wang P-Y, Zhang N, Li J-S, Qu L-B. Pharmacodynamics of Five Anthraquinones (Aloe-emodin, Emodin, Rhein, Chysophanol, and Physcion) and Reciprocal Pharmacokinetic Interaction in Rats with Cerebral Ischemia. Molecules. 2019; 24(10):1898. https://doi.org/10.3390/molecules24101898
Chicago/Turabian StyleLi, Rong-Rong, Xue-Fang Liu, Su-Xiang Feng, Sheng-Nan Shu, Pei-Yang Wang, Na Zhang, Jian-Sheng Li, and Ling-Bo Qu. 2019. "Pharmacodynamics of Five Anthraquinones (Aloe-emodin, Emodin, Rhein, Chysophanol, and Physcion) and Reciprocal Pharmacokinetic Interaction in Rats with Cerebral Ischemia" Molecules 24, no. 10: 1898. https://doi.org/10.3390/molecules24101898
APA StyleLi, R.-R., Liu, X.-F., Feng, S.-X., Shu, S.-N., Wang, P.-Y., Zhang, N., Li, J.-S., & Qu, L.-B. (2019). Pharmacodynamics of Five Anthraquinones (Aloe-emodin, Emodin, Rhein, Chysophanol, and Physcion) and Reciprocal Pharmacokinetic Interaction in Rats with Cerebral Ischemia. Molecules, 24(10), 1898. https://doi.org/10.3390/molecules24101898





