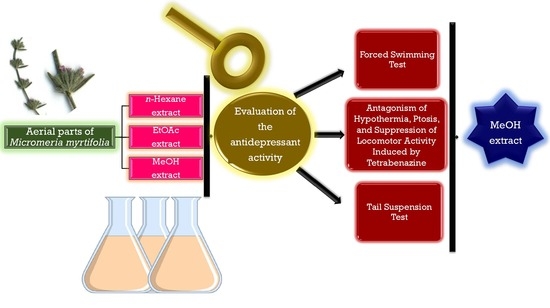
Assessment of Antidepressant Effect of the Aerial Parts of Micromeria myrtifolia Boiss. & Hohen on Mice
Abstract
:1. Introduction
2. Results
2.1. Biological Activity Studies
2.2. NMR Data of Isolated Compounds
3. Discussion
4. Materials and Methods
4.1. Plant Material
4.2. Extraction, Fractionation, and Isolation Process
4.2.1. Fractionation of MeOH Extract
4.2.2. Determination of the Structure of Compounds
4.3. Biological Activity Tests
4.3.1. Animals
4.3.2. Preparation of Test Samples for Bioassay
4.3.3. Forced Swimming Test (Behavioral Despair Test)
4.3.4. Tail Suspension Test
4.3.5. Antagonism of Hypothermia and Ptosis Induced by Tetrabenazine
4.3.6. The Inhibitory Activity on the MAO A&B
Author Contributions
Funding
Conflicts of Interest
References
- Mental Health. Available online: https://www.who.int/mental_health/world-mental-health-day/2017/en/ (accessed on 8 April 2019).
- Burden of Mental and Behavioural Disorders. Available online: https://www.who.int/whr/2001/chapter2/en/index4.html (accessed on 8 April 2019).
- The Global Burden of Disease 2004 Update. Available online: http://www.who.int/healthinfo/global_burden_disease/GBD_ report_2004update_full.pdf (accessed on 16 June 2012).
- Kashani, J.H.; Barbero, G.J.; Bolander, F.D. Depression in hospitalized pediatric patients. J. Am. Acad. Child Psychiatry 1981, 20, 123–134. [Google Scholar] [CrossRef]
- Ohayon, M.M. Specific characteristics of the pain/depression association in the general population. J. Clin. Psychiatry 2004, 65, 5–9. [Google Scholar]
- Zuckerman, B.; Amaro, H.; Bauchner, H.; Cabral, H. Depressive symptoms during pregnancy—Relationship to poor health behaviors. Am. J. Obstet. Gynecol. 1989, 160, 1107–1111. [Google Scholar] [CrossRef]
- Sevilla-Gonzalez, M.D.; Quintana-Mendoza, B.M.; Aguilar-Salinas, C.A. Interaction between depression, obesity, and type 2 diabetes: A complex picture. Arch. Med. Res. 2017, 48, 582–591. [Google Scholar] [CrossRef]
- Goodwin, G.M. Depression and associated physical diseases and symptoms. Dialogues Clin. Neurosci. 2006, 8, 259. [Google Scholar] [PubMed]
- Bisschop, M.I.; Knegsman, D.M.W.; Beekman, A.T.F.; Deeg, D.J.H. Chronic diseases and depression: The modifying role of psychosocial resources. Soc. Sci. Med. 2004, 59, 721–733. [Google Scholar] [CrossRef]
- Huang, C.Q.; Dong, B.R.; Lu, Z.C.; Yue, J.R.; Liu, Q.X. Chronic diseases and risk for depression in old age: A meta-analysis of published literature. Ageing Res. Rev. 2010, 9, 131–141. [Google Scholar] [CrossRef] [PubMed]
- Rabiei, Z.; Rabiei, S. A review on antidepressant effect of medicinal plants. Bangladesh J. Pharmacol. 2017, 12, 1–11. [Google Scholar] [CrossRef]
- Antai-Otong, D. Antidepressant-induced insomnia: Treatment options. Perspect. Psychiatr. Care 2004, 40, 29–33. [Google Scholar] [CrossRef]
- Baldwin, D.; Mayers, A. Sexual side-effects of antidepressant and antipsychotic drugs. Adv. Psychiatr. Treat. 2003, 9, 202–210. [Google Scholar] [CrossRef] [Green Version]
- Park, J.S.; Grow, J.M. The social reality of depression: DTC advertising of antidepressants and perceptions of the prevalence and lifetime risk of depression. J. Bus. Ethics 2008, 79, 379–393. [Google Scholar] [CrossRef]
- Redrobe, J.P.; Bourin, M. Augmentation of antidepressant pharmacotherapy: A preclinical approach using the mouse forced swimming test. CNS Spectrum 1999, 4, 73–81. [Google Scholar] [CrossRef]
- Sargin, S.A. Ethnobotanical survey of medicinal plants in Bozyazi district of Mersin, Turkey. J. Ethnopharmacol. 2015, 173, 105–126. [Google Scholar] [CrossRef] [PubMed]
- Davis, P.H. Micromeria Benth. In Flora of Turkey and the East Aegean Islands; Davis, P.H., Ed.; Edinburgh University Press: Edinburgh, UK, 1982; Volume 7, pp. 329–331. [Google Scholar]
- Said, O.; Khalil, K.; Fulder, S.; Azaizeh, H. Ethnopharmacological survey of medicinal herbs in Israel, the Golan Heights and the West Bank region. J. Ethnopharmacol. 2002, 83, 251–265. [Google Scholar] [CrossRef]
- El-Seedi, H.R.; Khattab, A.; Gaara, A.H.M.; Mohamed, T.K.; Hassan, N.A.; El-Kattan, A.E. Essential oil analysis of Micromeria nubigena HBK and its antimicrobial activity. J. Essent. Oil Res. 2008, 20, 452–456. [Google Scholar] [CrossRef]
- Duru, M.E.; Ozturk, M.; Ugur, A.; Ceylan, O. The constituents of essential oil and in vitro antimicrobial activity of Micromeria cilicica from Turkey. J. Ethnopharmacol. 2004, 94, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Vladimir-Knezevic, S.; Blazekovic, B.; Stefan, M.B.; Alegro, A.; Koszegi, T.; Petrik, J. Antioxidant activities and polyphenolic contents of three selected Micromeria species from Croatia. Molecules 2011, 16, 1454–1470. [Google Scholar] [CrossRef]
- Ozturk, M.; Kolak, U.; Duru, M.E.; Harmandar, M. GC-MS analysis of the antioxidant active fractions of Micromeria juliana with anticholinesterase activity. Nat. Prod. Commun. 2009, 4, 1271–1276. [Google Scholar]
- Abu-Gharbieh, E.; Shehab, N.G.; Khan, S.A. Anti-inflammatory and gastroprotective activities of the aqueous extract of Micromeria fruticosa (L.) Druce ssp serpyllifolia in mice. Pak. J. Pharm. Sci. 2013, 26, 799–803. [Google Scholar]
- Abu-Gharbieh, E.; Ahmed, N.G. Bioactive content, hepatoprotective and antioxidant activities of whole plant extract of Micromeria fruticosa (L) Druce ssp. serpyllifolia F Lamiaceae against carbon tetrachloride-induced hepatotoxicity in mice. Trop. J. Pharm. Res. 2016, 15, 2099–2106. [Google Scholar] [CrossRef]
- Koc, K.; Ozdemir, O.; Kizilkaya, O.F.; Sengul, M.; Turkez, H. Cytotoxic activity of the aqueous extract of Micromeria fruticosa (L.) Druce subsp serpyllifolia on human U-87 MG cell lines. Arch. Biol. Sci. 2017, 69, 449–453. [Google Scholar] [CrossRef]
- Ambreen, M.; Ahmad, M. Phytochemical analysis of selected medicinal plants used for dermatological infections. Sci. Int. (Lahore) 2016, 28, 4207–4210. [Google Scholar]
- Marin, P.D.; Grayer, R.J.; Veitch, N.C.; Kite, G.C.; Harborne, J.B. Acacetin glycosides as taxonomic markers in Calamintha and Micromeria. Phytochemistry 2001, 58, 943–947. [Google Scholar] [CrossRef]
- Nikolova, M.; Aneva, I.; Zhelev, P.; Dimitrova, M. Flavonoid compounds and antioxidant activity of Bulgarian species of Micromeria. In Proceedings of the Youth Scientific Conference “Kliment’s Days”, Sofia, Bulgaria, 17 November 2017. [Google Scholar]
- Tomasbarberan, F.A.; Gil, M.I.; Marin, P.D.; Tomaslorente, F. Flavonoids from some Yugoslavian Micromeria Species—Chemotaxonomical aspects. Biochem. Syst. Ecol. 1991, 19, 697–698. [Google Scholar] [CrossRef]
- Vukelić, D. Phytochemical Characterization of Polyphenols from Micromeria frivaldszkyana (Deg.)Vel. (Lamiaceae). Master’s Thesis, University of Zagreb Faculty of Pharmacy and Biochemistry, Zagreb, Croatia, 2015. [Google Scholar]
- Sargin, S.A.; Selvi, S.; Büyükcengiz, M. Ethnomedicinal plants of Aydincik district of Mersin, Turkey. J. Ethnopharmacol. 2015, 174, 200–216. [Google Scholar] [CrossRef] [PubMed]
- Formisano, C.; Oliviero, F.; Rigano, D.; Saab, A.M.; Senatore, F. Chemical composition of essential oils and in vitro antioxidant properties of extracts and essential oils of Calamintha origanifolia and Micromeria myrtifolia, two Lamiaceae from the Lebanon flora. Ind. Crops Prod. 2014, 62, 405–411. [Google Scholar] [CrossRef]
- Ozcan, M. Antifungal effects of Micromeria myrtifolia Boiss. & Hohen. in Boiss. and Prangos uechtritzii Boiss. Hawsskn decoctions. Acta Aliment. Hung. 1999, 28, 355–360. [Google Scholar]
- Porsolt, R.; Bertin, A.; Jalfre, M. Behavioral despair in mice: A primary screening test for antidepressants. Arch. Int. Pharmacodyn. Ther. 1977, 229, 327–336. [Google Scholar] [PubMed]
- Rottenberg, J. The Depths: The Evolutionary Origins of the Depression Epidemic; Basic Books (AZ): New York, NY, USA, 2014. [Google Scholar]
- Alpermann, H.G.; Schacht, U.; Usinger, P.; Hock, F.J. Pharmacological effects of Hoe-249: A new potential antidepressant. Drug Dev. Res. 1992, 25, 267–282. [Google Scholar] [CrossRef]
- Delgado, P.L. Depression: The case for a monoamine deficiency. J. Clin. Psychiatry 2000, 61, 7–11. [Google Scholar]
- Johannes, M.; Altmann, K.H. A ring-closing metathesis-based approach to the synthesis of (+/−)-tetrabenazine. Org. Lett. 2012, 14, 3752–3755. [Google Scholar] [CrossRef]
- Guay, D.R.P. Tetrabenazine, a monoamine-depleting drug used in the treatment of hyperkinetic movement disorders. Am. J. Geriatr. Pharmacother. 2010, 8, 331–373. [Google Scholar] [CrossRef]
- Garcia-Salas, P.; Morales-Soto, A.; Segura-Carretero, A.; Fernandez-Gutierrez, A. Phenolic-compound-extraction systems for fruit and vegetable samples. Molecules 2010, 15, 8813–8826. [Google Scholar] [CrossRef]
- Khurana, S.; Venkataraman, K.; Hollingsworth, A.; Piche, M.; Tai, T.C. Polyphenols: Benefits to the cardiovascular system in health and in aging. Nutrients 2013, 5, 3779–3827. [Google Scholar] [CrossRef]
- Farzaei, M.H.; Abbasabadi, Z.; Shams-Ardekani, M.R.; Abdollahi, M.; Rahimi, R. A Comprehensive review of plants and their active constituents with wound healing activity in traditional Iranian medicine. Wounds 2014, 26, 197–206. [Google Scholar]
- Kumar, G.; Jalaluddin, M.; Rout, P.; Mohanty, R.; Dileep, C.L. Emerging trends of herbal care in dentistry. J. Clin. Diagn. Res. 2013, 7, 1827. [Google Scholar]
- Bjorkholm, C.; Monteggia, L.M. BDNF—A key transducer of antidepressant effects. Neuropharmacology 2016, 102, 72–79. [Google Scholar] [CrossRef]
- Meng, X.; Zeng, N.; Zhang, Y.; Lai, X.; Ren, C.; Cheng, L. Effect of active constituents of Herba Epimedii on hypothalamic monoamine neurotransmitters and other brain functions in aging rats. Zhongguo Zhong Yao Za Zhi 1996, 21, 683–685. [Google Scholar]
- Saraceni, M.M.; Venci, J.V.; Gandhi, M.A. Levomilnacipran (Fetzima) a new serotonin-norepinephrine reuptake inhibitor for the treatment of major depressive disorder. J. Pharm. Pract. 2014, 27, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Shen, Z.; Chen, Y.; Huang, J.; Hu, Z. The gene expression profile in hypothalamus-pituitary-adrenal-thymus (HPAT) axis from EF-treated old rats. Chin. J. Immunol. 2004, 20, 59–62. [Google Scholar]
- Wedzony, K.; Chocyk, A.; Mackowiak, M. Potential roles of NCAM/PSA-NCAM proteins in depression and the mechanism of action of antidepressant drugs. Pharmacol. Rep. 2013, 65, 1471–1478. [Google Scholar] [CrossRef]
- Xiong, Z.; Jiang, B.; Wu, P.F.; Tian, J.; Shi, L.L.; Gu, J.; Hu, Z.L.; Fu, H.; Wang, F.; Chen, J.G. Antidepressant effects of a plant-derived flavonoid baicalein involving extracellular signal-regulated kinases cascade. Biol. Pharm. Bull. 2011, 34, 253–259. [Google Scholar] [CrossRef]
- Zhu, W.L.; Ma, S.P.; Qu, R.; Kang, D.L.; Liu, Y.D. Antidepressant effect of baicalin extracted from the root of Scutellaria baicalensis in mice and rats. Pharm. Biol. 2006, 44, 503–510. [Google Scholar] [CrossRef]
- Souza, L.C.; de Gomes, M.G.; Goes, A.T.; Del Fabbro, L.; Carlos Filho, B.; Boeira, S.P.; Jesse, C.R. Evidence for the involvement of the serotonergic 5-HT1A receptors in the antidepressant-like effect caused by hesperidin in mice. Prog. Neuropsychopharmacol. Biol. Psychiatry 2013, 40, 103–109. [Google Scholar] [CrossRef]
- Rinwa, P.; Kumar, A. Quercetin suppress microglial neuroinflammatory response and induce antidepressent-like effect in olfactory bulbectomized rats. Neuroscience 2013, 255, 86–98. [Google Scholar] [CrossRef]
- Machado, D.G.; Bettio, L.E.B.; Cunha, M.P.; Santos, A.R.S.; Pizzolatti, M.G.; Brighente, I.M.C.; Rodrigues, A.L.S. Antidepressant-like effect of rutin isolated from the ethanolic extract from Schinus molle L. in mice: Evidence for the involvement of the serotonergic and noradrenergic systems. Eur. J. Pharmacol. 2008, 587, 163–168. [Google Scholar] [CrossRef]
- Park, S.H.; Sim, Y.B.; Han, P.L.; Lee, J.K.; Suh, H.W. Antidepressant-like effect of kaempferol and quercitirin, isolated from Opuntia ficus-indica var. saboten. Exp. Neurobiol. 2010, 19, 30–38. [Google Scholar] [CrossRef]
- Nakazawa, T.; Yasuda, T.; Ueda, J.; Ohsawa, K. Antidepressant-like effects of apigenin and 2,4,5-trimethoxycinnamic acid from Perilla frutescens in the forced swimming test. Biol. Pharm. Bull. 2003, 26, 474–480. [Google Scholar] [CrossRef]
- Yi, L.T.; Li, H.M.; Li, Y.C.; Pan, Y.; Xu, Q.; Kong, L.D. Antidepressant-like behavioral and neurochemical effects of the citrus-associated chemical apigenin. Life Sci. 2008, 82, 741–751. [Google Scholar] [CrossRef]
- Li, R.P.; Zhao, D.; Qu, R.; Fu, Q.; Ma, S.P. The effects of apigenin on lipopolysaccharide-induced depressive-like behavior in mice. Neurosci. Lett. 2015, 594, 17–22. [Google Scholar] [CrossRef]
- Weng, L.J.; Guo, X.H.; Li, Y.; Yang, X.; Han, Y.Y. Apigenin reverses depression-like behavior induced by chronic corticosterone treatment in mice. Eur. J. Pharmacol. 2016, 774, 50–54. [Google Scholar] [CrossRef]
- Ma, Z.G.; Wang, G.L.; Cui, L.; Wang, Q.M. Myricetin attenuates depressant-like behavior in mice subjected to repeated restraint stress. Int. J. Mol. Sci. 2015, 16, 28377–28385. [Google Scholar] [CrossRef]
- Yi, L.T.; Li, C.F.; Zhan, X.; Cui, C.C.; Xiao, F.; Zhou, L.P.; Xie, Y. Involvement of monoaminergic system in the antidepressant-like effect of the flavonoid naringenin in mice. Prog. Neuropsychopharmacol. Biol. Psychiatry 2010, 34, 1223–1228. [Google Scholar] [CrossRef] [PubMed]
- Yi, L.T.; Li, J.; Li, H.C.; Su, D.X.; Quan, X.B.; He, X.C.; Wang, X.H. Antidepressant-like behavioral, neurochemical and neuroendocrine effects of naringenin in the mouse repeated tail suspension test. Prog. Neuropsychopharmacol. Biol. Psychiatry 2012, 39, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Yi, L.T.; Liu, B.B.; Li, J.; Luo, L.; Liu, Q.; Geng, D.; Tang, Y.; Xia, Y.; Wu, D. BDNF signaling is necessary for the antidepressant-like effect of naringenin. Prog. Neuropsychopharmacol. Biol. Psychiatry 2014, 48, 135–141. [Google Scholar] [CrossRef]
- Ito, N.; Yabe, T.; Gamo, Y.; Nagai, T.; Oikawa, T.; Yamada, H.; Hanawa, T. Rosmarinic acid from Perillae Herba produces an antidepressant-like effect in mice through cell proliferation in the hippocampus. Biol. Pharm. Bull. 2008, 31, 1376–1380. [Google Scholar] [CrossRef] [PubMed]
- Jin, X.; Liu, P.; Yang, F.; Zhang, Y.H.; Miao, D. Rosmarinic acid ameliorates depressive-like behaviors in a rat model of CUS and up-regulates BDNF levels in the hippocampus and hippocampal-derived astrocytes. Neurochem. Res. 2013, 38, 1828–1837. [Google Scholar] [CrossRef]
- Kondo, S.; El Omri, A.; Han, J.; Isoda, H. Antidepressant-like effects of rosmarinic acid through mitogen-activated protein kinase phosphatase-1 and brain-derived neurotrophic factor modulation. J. Funct. Foods 2015, 14, 758–766. [Google Scholar] [CrossRef] [Green Version]
- Petersen, M.; Simmonds, M.S.J. Rosmarinic acid. Phytochemistry 2003, 62, 121–125. [Google Scholar] [CrossRef]
- Semwal, D.K.; Semwal, R.B.; Combrinck, S.; Viljoen, A. Myricetin: A dietary molecule with diverse biological activities. Nutrients 2016, 8, 90. [Google Scholar] [CrossRef]
- Osigwe, C.C.; Akah, P.A.; Nworu, C.S.; Okoye, F.B.C. Apigenin: A methanol fraction component of Newbouldia laevis leaf, as a potential antidiabetic agent. J. Phytopharmacol. 2017, 6, 38–44. [Google Scholar]
- Guragac Dereli, F.T.; Ilhan, M.; Kupeli Akkol, E. Discovery of new antidepressant agents: In vivo study on Anthemis wiedemanniana Fisch. & Mey. J. Ethnopharmacol. 2018, 226, 11–16. [Google Scholar]
- Steru, L.; Chermat, R.; Thierry, B.; Simon, P. The tail suspension test—A new method for screening antidepressants in mice. Psychopharmacology 1985, 85, 367–370. [Google Scholar] [CrossRef]
- Hwang, K.H. Monoamine oxidase inhibitory activities of Korean medicinal plants classified to cold drugs by the theory of KIMI. Food Sci. Biotechnol. 2003, 12, 238–241. [Google Scholar]
Sample Availability: Samples of the compounds are available from the authors. |

| Material | Dose (mg/kg p.o.) | Duration of Immobility (s) (Mean ± S.E.M.) |
|---|---|---|
| Control | - | 187.22 ± 6.16 |
| n-Hexane extract | 100 | 199.51 ± 7.74 |
| EtOAc extract | 173.08 ± 8.13 | |
| MeOH extract | 115.34 ± 5.12 * | |
| Imipramine | 30 | 109.61 ± 4.23 ** |
| 50 | 94.26 ± 4.01 *** | |
| Control | - | 173.12 ± 5.01 |
| Fr. A | 100 | 192.31 ± 3.96 |
| Fr. B | 105.18 ± 3.26 ** | |
| Fr. C | 98.15 ± 2.07 *** | |
| Fr. D | 162.45 ± 2.93 | |
| Fr. E | 181.26 ± 4.12 | |
| Imipramine | 30 | 112.73 ± 2.84 ** |
| 50 | 93.28 ± 2.85 ** | |
| Control | - | 191.89 ± 9.68 |
| Rosmarinic acid | 25 | 119.76 ± 6.49 ** |
| Myricetin | 118.19 ± 4.62 ** | |
| Apigenin | 132.15 ± 7.06 ** | |
| Naringenin | 136.63 ± 6.81 * | |
| Imipramine | 30 | 128.00 ± 5.19 ** |
| 50 | 97.02 ± 3.74 ** |
| Material | Dose (mg/kg p.o.) | Duration of Immobility (s) (Mean ± S.E.M.) |
|---|---|---|
| Control | - | 172.68 ± 6.14 |
| n-Hexane extract | 100 | 191.41 ± 11.23 |
| EtOAc extract | 154.80 ± 7.59 | |
| MeOH extract | 111.82 ± 5.62 * | |
| Imipramine | 30 | 105.41 ± 3.62 ** |
| 50 | 91.56 ± 2.48 *** | |
| Control | - | 195.75 ± 10.63 |
| Fr. A | 100 | 182.03 ± 9.21 |
| Fr. B | 123.92 ± 5.04 * | |
| Fr. C | 131.37 ± 6.89 | |
| Fr. D | 184.91 ± 10.17 | |
| Fr. E | 197.66 ± 12.28 | |
| Imipramine | 30 | 108.82 ± 4.90 ** |
| 50 | 95.42 ± 3.20 *** | |
| Control | - | 220.49 ± 17.04 |
| Rosmarinic acid | 25 | 119.83 ± 11.91 * |
| Myricetin | 189.72 ± 15.26 | |
| Apigenin | 176.17 ± 12.03 | |
| Naringenin | 142.58 ± 14.45 | |
| Imipramine | 30 | 101.64 ± 4.77 ** |
| 50 | 84.90 ± 2.49 *** |
| Material | Dose (mg/kg p.o.) | Ptosis Mean Score (30 min) (Mean ± S.E.M.) | Mean Decrease in Rectal Temperature (°C) (Mean ± S.E.M.) |
|---|---|---|---|
| Control | - | 3.19 ± 0.63 | 4.88 ± 0.32 |
| n-Hexane extract | 100 | 3.24 ± 0.52 | 4.91 ± 0.74 |
| EtOAc extract | 2.71 ± 0.49 | 4.07 ± 0.52 | |
| MeOH extract | 2.13 ± 0.21 * | 2.46 ± 0.21 * | |
| Fluoxetine | 25 | 0.00 ± 0.00 *** | 0.43 ± 0.17 ** |
| Control | - | 4.16 ± 0.92 | 5.93 ± 0.48 |
| Fr. A | 100 | 3.96 ± 0.38 | 4.82 ± 0.54 |
| Fr. B | 2.34 ± 0.21 * | 2.82 ± 0.10 * | |
| Fr. C | 2.91 ± 0.18 * | 3.06 ± 0.27 * | |
| Fr. D | 4.29 ± 0.63 | 5.11 ± 0.82 | |
| Fr. E | 4.57 ± 0.51 | 6.12 ± 0.43 | |
| Fluoxetine | 25 | 0.00 ± 0.00 *** | 0.49 ± 0.11 *** |
| Control | - | 3.95 ± 0.83 | 6.18 ± 1.07 |
| Rosmarinic acid | 25 | 2.18 ± 0.66 * | 3.11 ± 0.74 * |
| Myricetin | 2.53 ± 0.48 * | 2.49 ± 0.42 * | |
| Apigenin | 2.31 ± 0.45 * | 2.62 ± 0.58 * | |
| Naringenin | 3.22 ± 0.94 | 3.34 ± 0.87 | |
| Fluoxetine | 0.00 ± 0.00 *** | 0.36 ± 0.15 *** |
| Material | IC50 (mg/mL) | |
|---|---|---|
| MAO-A | MAO-B | |
| Control | >10 | >10 |
| n-Hexane extract | >10 | 7.3 |
| EtOAc extract | >10 | 8.9 |
| MeOH extract | 4.7 | 1.4 |
| Fr. A | >10 | >10 |
| Fr. B | 5.9 | 4.8 |
| Fr. C | 4.1 | 2.2 |
| Fr. D | >10 | >10 |
| Fr. E | >10 | >10 |
| Rosmarinic acid | 6.5 | 5.3 |
| Myricetin | 4.4 | 2.7 |
| Apigenin | 3.1 | 1.6 |
| Naringenin | 5.9 | 1.9 |
| Caffeine | 0.2 | 0.5 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Küpeli Akkol, E.; Gürağaç Dereli, F.T.; Ilhan, M. Assessment of Antidepressant Effect of the Aerial Parts of Micromeria myrtifolia Boiss. & Hohen on Mice. Molecules 2019, 24, 1869. https://doi.org/10.3390/molecules24101869
Küpeli Akkol E, Gürağaç Dereli FT, Ilhan M. Assessment of Antidepressant Effect of the Aerial Parts of Micromeria myrtifolia Boiss. & Hohen on Mice. Molecules. 2019; 24(10):1869. https://doi.org/10.3390/molecules24101869
Chicago/Turabian StyleKüpeli Akkol, Esra, Fatma Tuğçe Gürağaç Dereli, and Mert Ilhan. 2019. "Assessment of Antidepressant Effect of the Aerial Parts of Micromeria myrtifolia Boiss. & Hohen on Mice" Molecules 24, no. 10: 1869. https://doi.org/10.3390/molecules24101869