Determination of Bitterness of Andrographis Herba Based on Electronic Tongue Technology and Discovery of the Key Compounds of Bitter Substances
Abstract
:1. Introduction
2. Results and Discussion
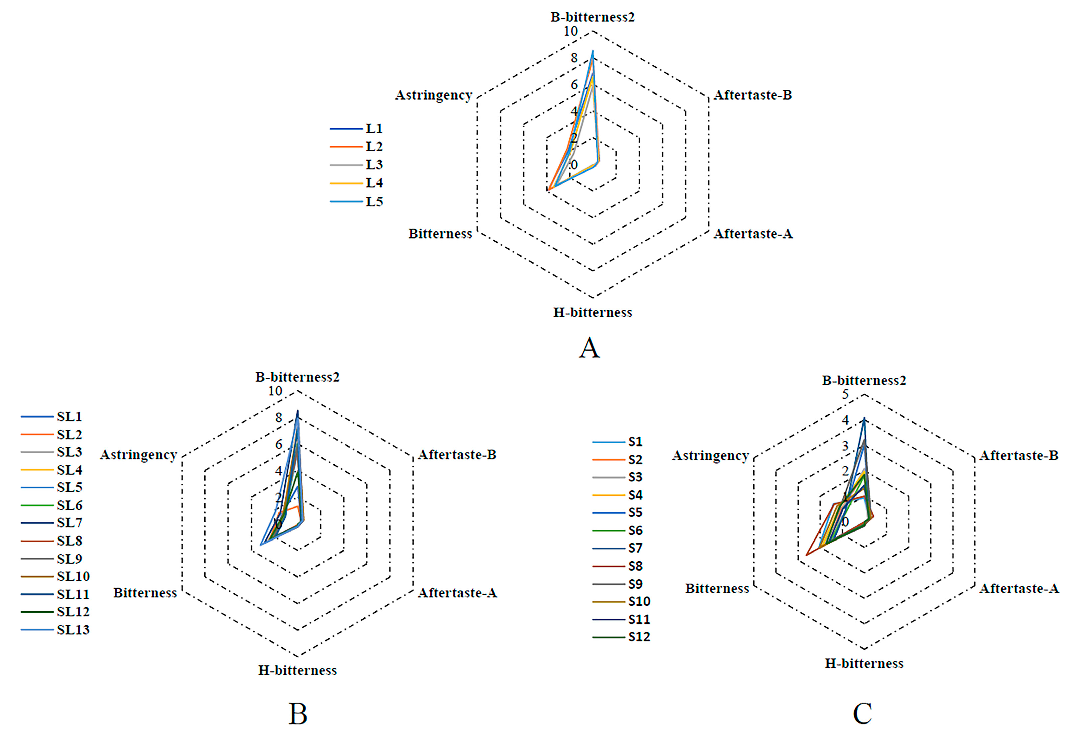
2.1. Bitterness AH Aample Analysis via Electronic Tongue
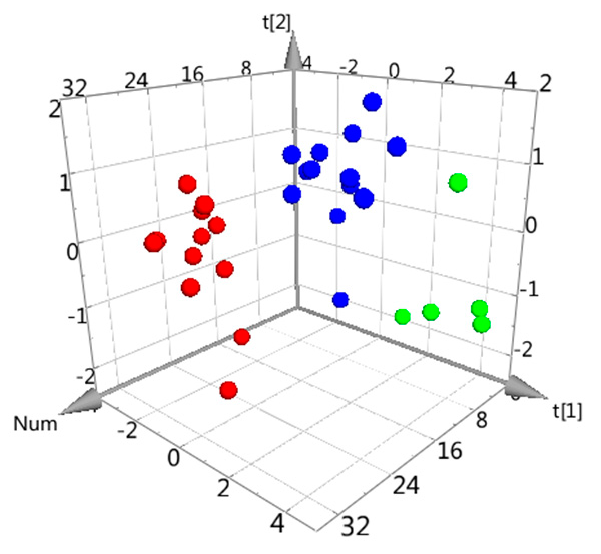
2.2. Principal Component Analysis of AH Samples’ Bitterness
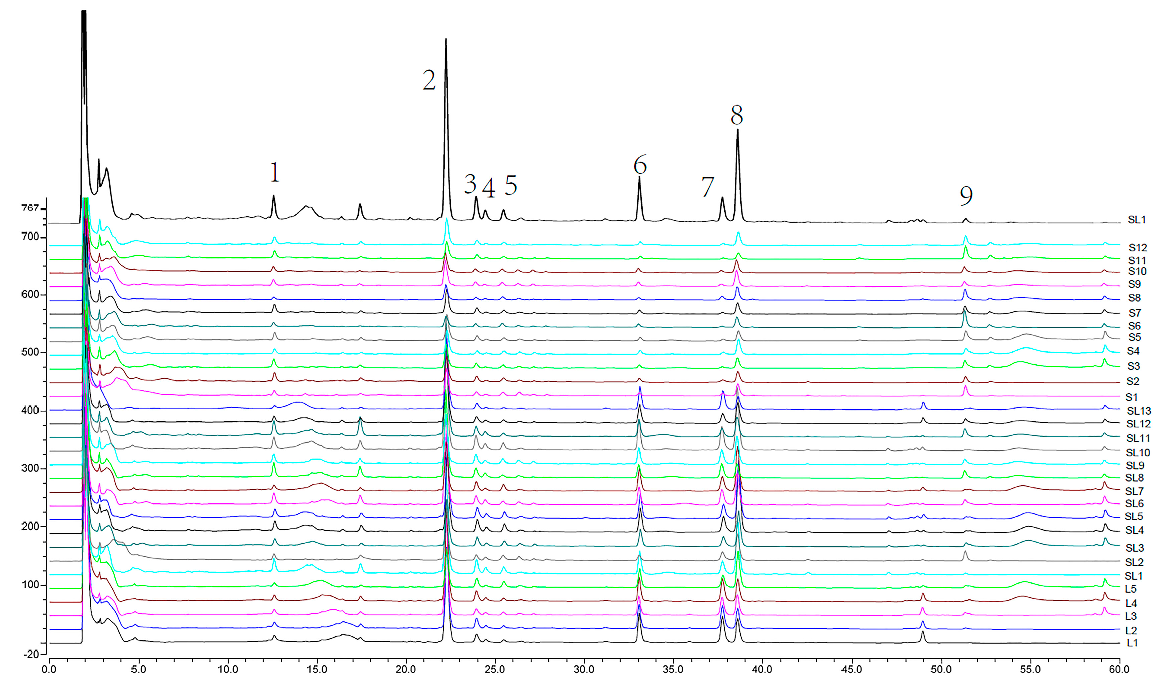
2.3. HPLC Fingerprint Analysis
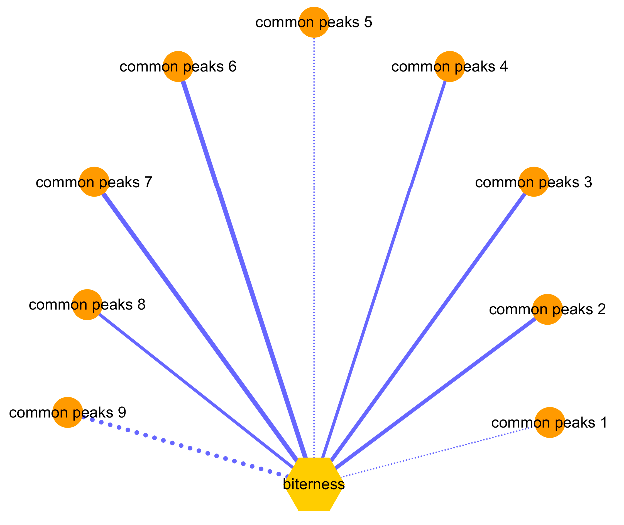
2.4. Spearman Correlation Analysis
3. Materials and Methods
3.1. Instruments and Chemicals
3.2. AH Sample Collection
3.3. Electronic Tongue Methods
3.3.1. Electronic Tongue Measurement Principle, Steps, and Conditions
3.3.2. Sample Preparation for the Electronic Tongue
3.3.3. Electronic Tongue Methodology Validation
3.4. HPLC Fingerprint Methods
3.4.1. Chromatographic Conditions
3.4.2. HPLC Sample Preparation
3.4.3. HPLC Methodology Validation
3.5. Data Analysis
3.5.1. PCA Analysis for Electronic Tongue Data
3.5.2. Fingerprint Data Processing
3.5.3. Correlation Analysis
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Sareer, O.; Ahad, A.; Umar, S. Prophylactic and lenitive effects of Andrographis Paniculata against common human ailments: An exhaustive and comprehensive reappraisal. J. Pharm. Res. Opin. 2012, 10, 138–162. [Google Scholar]
- Sareer, O.; Ahmad, S.; Umar, S. Andrographis paniculata: A critical appraisal of extraction, isolation and quantification of andrographolide and other active constituents. Nat. Prod. Res. 2014, 28, 2081–2101. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Tang, L.Y.; Wu, H.W.; Xu, M.Y.; Guo, R.X.; Yu, X.K.; Lu, Y.Q.; Luo, H.Y.; Liu, D.F.; Wang, Z.J.; et al. The newest research progresses of Andrographis Paniculate. Chin. J. Exp. Tradit. Med. Form. 2018, 24, 96–108. [Google Scholar]
- Committee for the Pharmacopoeia of China. Pharmacopoeia of China; Part I; China Medical Science and Technology Press: Beijing, China, 2015; pp. 268–269. [Google Scholar]
- Liu, C.X.; Zhang, T.J.; He, X.; Chen, C.Q.; Xu, J.; Tian, C.W. Study on chemistry and biology based on five-tastes and function-efficacy of Chinese materia medica with invigorating blood circulation and eliminating blood stasis. Chin. Tradit. Herbal Drugs 2015, 46, 615–624. [Google Scholar]
- Tang, D.C. Science of Chinese Materia Medica, 1st ed.; Shanghai University of Traditional Chinese Medicine Press: Shanghai, China, 2003; p. 5. ISBN 7–810810-658659. [Google Scholar]
- Bartoshuk, L.M. Comparing sensory experiences across individuals: Recent psychophysical advances illuminate genetic variation in taste perception. Chem. Senses 2000, 25, 447–460. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.Y.; Liu, X.L.; Zhou, S.P.; Tong, L.; Ding, L. Chemical fingerprinting of Andrographis Paniculata and quantitative analysis of four diterpenoids by UPLC-PDA. Chin. J. Chin. Mater. Med. 2014, 21, 4240–4245. [Google Scholar]
- Zhang, X.; Wu, H.W.; Yu, X.K.; Lu, Y.Q.; Luo, H.Y.; Yang, H.J.; Xu, M.Y.; Guo, R.X.; Li, Z.Y.; Tang, L.Y.; et al. Quality evaluation of Andrographis Paniculate based on electronic-eye technique. Chin. J. Exp. Tradit. Med. Form. 2018, 17, 1–7. [Google Scholar]
- Woertz, K.; Tissen, C.; Kleinebudde, P.; Breitkreutz, J. Taste sensing systems (electronic tongues) for pharmaceutical applications. Int. J. Pharm. 2011, 417, 256–271. [Google Scholar] [CrossRef]
- Tahara, Y.; Toko, K. Electronic Tongues-A Review. IEEE Sens. J. 2013, 13, 3001–3011. [Google Scholar] [CrossRef]
- Imamura, T.; Toko, K.; Yanagisawa, S.; Kume, T. Monitoring of fermentation process of miso (soybean paste) using multichannel taste sensor. Sensor. Actuat. B Chem. 1996, 37, 179–185. [Google Scholar] [CrossRef]
- Eckert, C.; Lutz, C.; Breitkreutz, J.; Woertz, K. Quality control of oral herbal products by an electronic tongue-Case study on sage lozenges. Sensor. Actuat. B Chem. 2011, 156, 204–212. [Google Scholar] [CrossRef]
- Kataoka, M.; Tokuyama, E.; Miyanaga, Y.; Uchida, T. The taste sensory evaluation of medicinal plants and Chinese medicines. Int. J. Pharm. 2008, 351, 36–44. [Google Scholar] [CrossRef]
- Woertz, K.; Tissen, C.; Kleinebudde, P.; Breitkreutz, J. Rational development of taste masked oral liquids guided by an electronic tongue. Int. J. Pharm. 2010, 400, 114–123. [Google Scholar] [CrossRef] [PubMed]
- Mohamed-Ahmed, A.H.A.; Soto, J.; Ernest, T.; Tuleu, C. Non-human tools for the evaluation of bitter taste in the design and development of medicines: A systematic review. Drug. Discov. Today 2016, 21, 1170–1180. [Google Scholar] [CrossRef] [PubMed]
- Woertz, K.; Tissen, C.; Kleinebudde, P.; Breitkreutz, J. A comparative study on two electronic tongues for pharmaceutical formulation development. J. Pharm. Biomed. Anal. 2011, 55, 272–281. [Google Scholar] [CrossRef] [PubMed]
- Ono, N.; Miyamoto, Y.; Ishiguro, T.; Motoyama, K.; Hirayama, F.; Iohara, D.; Seo, H.; Tsuruta, S.; Arima, H.; Uekama, K. Reduction of bitterness of antihistaminic drugs by complexation with β-cyclodextrins. J. Pharm. SCI-US 2011, 100, 1935–1943. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Xie, D.S.; Liu, H.M.; Fang, C.X.; Wei, C.; Guo, L.; Fu, C.M. Identification of Fritillaria cirrhosa powder and its adulterated products by electronic tongue technology. Chin. Tradit. Pat. Med. 2017, 39, 1977–1979. [Google Scholar]
- Anjiki, N.; Hosoe, J.; Fuchino, H.; Kiuchi, F.; Sekita, S.; Ikezaki, H.; Mikage, M.; Kawahara, N.; Goda, Y. Evaluation of the taste of crude drug and Kampo formula by a taste-sensing system (4): Taste of Processed Aconite Root. J. Nat. Med. 2011, 65, 293–300. [Google Scholar] [CrossRef]
- Fu, Z.H.; Li, S.J.; Hu, H.H.; Liu, P.; Sun, M.L. Taste comparison of unprocessed and processed Siegesbeckiae puescens based on electronic tongue. Chin. Tradit. Herbal Drugs 2017, 48, 673–680. [Google Scholar]
- Kobayashi, Y.; Habara, M.; Ikezazki, H.; Chen, R.; Naito, Y.; Toko, K. Advanced taste sensors based on artificial lipids with global selectivity to basic taste qualities and high correlation to sensory scores. Sensors 2010, 10, 3411–3443. [Google Scholar] [CrossRef]
- Letellier, T.; Durrieu, G.; Malgat, M.; Rossignol, R.; Antoch, J.; Deshouillers, J.M.; Coquet, M.; Lacombe, D.; Netter, J.C.; Pedespan, J.M.; et al. Statistical analysis of mitochondrial pathologies in childhood: Identification of deficiencies using principal component analysis. Lab. Investig. 2000, 80, 1019–1030. [Google Scholar] [CrossRef] [PubMed]
- Liang, X.G.; Wu, F.; Wang, Y.J.; Fu, Z.; Wang, Y.; Feng, Y.; Liang, S. Research on bitter substances of traditional Chinese medicine Coptis chinensis based on electronic tongue technology. Chin. J. Chin. Mater. Med. 2014, 39, 3326–3329. [Google Scholar]
- Wu, H.W.; Wang, P.; Liu, M.T.; Tang, L.Y.; Fang, J.; Zhao, Y.; Zhang, Y.; Li, D.F.; Xu, H.Y.; Yang, H.J. A 1H-NMR-Based Metabonomic Study on the Anti-Depressive Effect of the Total Alkaloid of Corydalis Rhizoma. Molecules 2015, 20, 10047–10064. [Google Scholar] [CrossRef] [PubMed]
- Liu, M.T.; Liu, X.; Wang, H.P.; Xiao, H.B.; Fang, J.; Tang, L.Y.; Li, D.F.; Zhang, Y.; Wu, H.W.; Yang, H.J. Metabolomics study on the effects of Buchang Naoxintong capsules for treating cerebral ischemia in rats using UPLC-Q/TOF-MS. J. Ethnopharmacol. 2016, 180, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Nian Shong Chok, M.S. Pearson’s versus Spearman’s and Kendall’s correlation coefficients for continuous data. Master’s Thesis, University of Pittsburgh, Auckland, PA, USA, 2010. [Google Scholar]
- Sun, M.M.; Li, L.; Wang, M.; van Wijk, E.; He, M.; van Wijk, R.; Koval, S.; Hankemeier, T.; van der Greef, J.; Wei, S.L. Effects of growth altitude on chemical constituents and delayed luminescence properties in medicinal rhubarb. J. Photochem. Photobiol. B 2016, 162, 24–33. [Google Scholar] [CrossRef] [PubMed]
- Franco, G.; De Nunzio, C.; Leonardo, C.; Tubaro, A.; Ciccariello, M.; De Dominicis, C.; Miano, L.; Laurenti, C. Ultrasound assessment of intravesical prostatic protrusion and detrusor wall thickness—new standards for noninvasive bladder outlet obstruction diagnosis? J. Urol. 2010, 183, 2270–2274. [Google Scholar] [CrossRef]
Sample Availability: Smples of the compounds are available from the authors. |

| Samples | B-Bitterness2 | Aftertaste-B | Aftertaste-A | H-Bitterness | Bitterness | Astringency | Radar Curve Area |
|---|---|---|---|---|---|---|---|
| L1 | 6.83 ± 0.01 | 0.55 ± 0.05 | 0.19 ± 0.03 | 0.13 ± 0.04 | 3.86 ± 0.03 | 2.12 ± 0.05 | 11.713 |
| L2 | 7.94 ± 0.05 | 0.51 ± 0.03 | 0.21 ± 0.08 | 0.11 ± 0.05 | 3.82 ± 0.03 | 2.25 ± 0.04 | 13.449 |
| L3 | 5.90 ± 0.04 | 0.47 ± 0.05 | 0.10 ± 0.06 | 0.04 ± 0.07 | 3.16 ± 0.05 | 1.66 ± 0.03 | 7.790 |
| L4 | 6.57 ± 0.02 | 0.49 ± 0.02 | 0.15 ± 0.07 | 0.09 ± 0.06 | 3.39 ± 0.06 | 1.94 ± 0.01 | 9.931 |
| L5 | 8.53 ± 0.06 | 0.41 ± 0.05 | 0.19 ± 0.06 | 0.24 ± 0.04 | 3.28 ± 0.06 | 1.99 ± 0.03 | 12.085 |
| ST1 | 2.79 ± 0.03 | 0.29 ± 0.05 | 0.07 ± 0.07 | 0.14 ± 0.07 | 2.06 ± 0.05 | 1.36 ± 0.06 | 3.344 |
| ST2 | 1.30 ± 0.04 | 0.30 ± 0.05 | 0.10 ± 0.06 | 0.08 ± 0.08 | 2.39 ± 0.04 | 1.62 ± 0.05 | 2.857 |
| ST3 | 6.07 ± 0.05 | 0.34 ± 0.03 | 0.09 ± 0.00 | 0.21 ± 0.07 | 2.14 ± 0.07 | 1.21 ± 0.09 | 5.411 |
| ST4 | 7.17 ± 0.01 | 0.42 ± 0.01 | 0.11 ± 0.09 | 0.25 ± 0.06 | 2.30 ± 0.06 | 1.23 ± 0.09 | 6.629 |
| ST5 | 5.48 ± 0.05 | 0.47 ± 0.05 | 0.09 ± 0.06 | 0.17 ± 0.06 | 2.38 ± 0.05 | 1.15 ± 0.04 | 5.229 |
| ST6 | 5.99 ± 0.03 | 0.30 ± 0.04 | 0.06 ± 0.05 | 0.18 ± 0.06 | 2.13 ± 0.06 | 1.14 ± 0.05 | 4.965 |
| ST7 | 8.51 ± 0.08 | 0.46 ± 0.07 | 0.16 ± 0.06 | 0.24 ± 0.09 | 2.88 ± 0.04 | 1.51 ± 0.05 | 9.490 |
| ST8 | 5.65 ± 0.03 | 0.25 ± 0.02 | 0.08 ± 0.08 | 0.17 ± 0.07 | 2.03 ± 0.03 | 1.26 ± 0.02 | 4.966 |
| ST9 | 5.83 ± 0.08 | 0.28 ± 0.08 | 0.10 ± 0.06 | 0.18 ± 0.03 | 2.05 ± 0.03 | 1.29 ± 0.02 | 5.288 |
| ST10 | 7.28 ± 0.01 | 0.52 ± 0.01 | 0.12 ± 0.05 | 0.19 ± 0.03 | 2.53 ± 0.02 | 1.26 ± 0.12 | 7.237 |
| ST11 | 7.21 ± 0.02 | 0.30 ± 0.05 | 0.08 ± 0.07 | 0.16 ± 0.06 | 1.90 ± 0.03 | 1.07 ± 0.04 | 5.305 |
| ST12 | 3.87 ± 0.08 | 0.41 ± 0.05 | 0.05 ± 0.12 | 0.19 ± 0.03 | 2.41 ± 0.01 | 1.23 ± 0.05 | 4.243 |
| ST13 | 7.92 ± 0.01 | 0.43 ± 0.04 | 0.12 ± 0.05 | 0.24 ± 0.07 | 3.23 ± 0.03 | 1.91 ± 0.01 | 11.067 |
| S1 | 0.93 ± 0.05 | 0.20 ± 0.05 | 0.05 ± 0.10 | 0.02 ± 0.00 | 2.07 ± 0.05 | 1.40 ± 0.06 | 1.922 |
| S2 | 1.87 ± 0.04 | 0.18 ± 0.06 | 0.02 ± 0.03 | 0.11 ± 0.05 | 1.58 ± 0.06 | 1.03 ± 0.08 | 1.762 |
| S3 | 2.08 ± 0.07 | 0.15 ± 0.07 | 0.01 ± 0.11 | 0.08 ± 0.07 | 1.38 ± 0.03 | 0.99 ± 0.08 | 1.667 |
| S4 | 1.96 ± 0.04 | 0.24 ± 0.08 | 0.06 ± 0.06 | 0.09 ± 0.06 | 1.90 ± 0.02 | 1.14 ± 0.07 | 2.192 |
| S5 | 3.03 ± 0.03 | 0.24 ± 0.09 | 0.04 ± 0.13 | 0.11 ± 0.05 | 1.42 ± 0.08 | 0.86 ± 0.06 | 2.046 |
| S6 | 1.82 ± 0.08 | 0.23 ± 0.07 | 0.05 ± 0.11 | 0.07 ± 0.09 | 1.56 ± 0.04 | 0.81 ± 0.05 | 1.421 |
| S7 | 4.09 ± 0.01 | 0.22 ± 0.05 | 0.03 ± 0.10 | 0.13 ± 0.08 | 1.38 ± 0.03 | 0.86 ± 0.05 | 2.509 |
| S8 | 1.00 ± 0.07 | 0.41 ± 0.05 | 0.07 ± 0.09 | 0.02 ± 0.00 | 2.63 ± 0.03 | 1.37 ± 0.03 | 2.367 |
| S9 | 3.21 ± 0.02 | 0.29 ± 0.08 | 0.09 ± 0.07 | 0.17 ± 0.09 | 1.76 ± 0.03 | 1.10 ± 0.04 | 2.932 |
| S10 | 1.31 ± 0.02 | 0.30 ± 0.03 | 0.05 ± 0.11 | 0.11 ± 0.09 | 2.03 ± 0.02 | 1.23 ± 0.03 | 2.055 |
| S11 | 1.43 ± 0.09 | 0.22 ± 0.00 | 0.02 ± 0.07 | 0.12 ± 0.05 | 1.60 ± 0.03 | 0.99 ± 0.02 | 1.521 |
| S12 | 1.84 ± 0.03 | 0.21 ± 0.07 | 0.01 ± 0.09 | 0.13 ± 0.04 | 1.71 ± 0.04 | 1.14 ± 0.01 | 2.017 |
| Common Peaks | Radar Curve Area | Common Peaks | Radar Curve Area |
|---|---|---|---|
| 1 | ρ = −0.125 (p = 0.510) | 6 | ρ = 0.854 (p < 0.01) |
| 2 | ρ = 0.725 (p < 0.01) | 7 | ρ = 0.890 (p < 0.01) |
| 3 | ρ = 0.729 (p < 0.01) | 8 | ρ = 0.691 (p < 0.01) |
| 4 | ρ = 0.629 (p < 0.01) | 9 | ρ=−0.826 (p < 0.01) |
| 5 | ρ = −0.014 (p = 0.942) |
| Samples | Origin | Collection Parts | Samples | Origin | Collection Parts |
|---|---|---|---|---|---|
| L1 | Anhui | Leaf | SL11 | Guangdong | Stem/Leaf |
| L2 | Anhui | Leaf | SL12 | Anhui | Stem/Leaf |
| L3 | Anhui | Leaf | SL13 | Anhui | Stem/Leaf |
| L4 | Anhui | Leaf | S1 | Jiangxi | Stem |
| L5 | Anhui | Leaf | S2 | Anhui | Stem |
| SL1 | Jiangxi | Stem/Leaf | S3 | Guangxi | Stem |
| SL2 | Jiangxi | Stem/Leaf | S4 | Guangxi | Stem |
| SL3 | Guangxi | Stem/Leaf | S5 | Guangxi | Stem |
| SL4 | Fujian | Stem/Leaf | S6 | Guangxi | Stem |
| SL5 | Guangxi | Stem/Leaf | S7 | Guangdong | Stem |
| SL6 | Guangxi | Stem/Leaf | S8 | Guangdong | Stem |
| SL7 | Guangxi | Stem/Leaf | S9 | Sichuan | Stem |
| SL8 | Guangdong | Stem/Leaf | S10 | Sichuan | Stem |
| SL9 | Guangdong | Stem/Leaf | S11 | Jiangsu | Stem |
| SL10 | Guangdong | Stem/Leaf | S12 | Jiangsu | Stem |
| Sensor Probes | Taste Information | |
|---|---|---|
| Initial Value | Aftertaste Value | |
| C00 | Bitterness | Aftertaste of anionic bitterness (aftertaste-B) |
| BT0 | - | Aftertaste of cationic bitterness (H-bitterness) |
| AN0 | - | Aftertaste of mineral bitterness (B-bitterness2) |
| AE1 | Astringency | Aftertaste of astringency (aftertaste-A) |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, X.; Wu, H.; Yu, X.; Luo, H.; Lu, Y.; Yang, H.; Li, X.; Li, Z.; Tang, L.; Wang, Z. Determination of Bitterness of Andrographis Herba Based on Electronic Tongue Technology and Discovery of the Key Compounds of Bitter Substances. Molecules 2018, 23, 3362. https://doi.org/10.3390/molecules23123362
Zhang X, Wu H, Yu X, Luo H, Lu Y, Yang H, Li X, Li Z, Tang L, Wang Z. Determination of Bitterness of Andrographis Herba Based on Electronic Tongue Technology and Discovery of the Key Compounds of Bitter Substances. Molecules. 2018; 23(12):3362. https://doi.org/10.3390/molecules23123362
Chicago/Turabian StyleZhang, Xiao, Hongwei Wu, Xiankuo Yu, Hanyan Luo, Yaqi Lu, Hongjun Yang, Xin Li, Zhiyong Li, Liying Tang, and Zhuju Wang. 2018. "Determination of Bitterness of Andrographis Herba Based on Electronic Tongue Technology and Discovery of the Key Compounds of Bitter Substances" Molecules 23, no. 12: 3362. https://doi.org/10.3390/molecules23123362
APA StyleZhang, X., Wu, H., Yu, X., Luo, H., Lu, Y., Yang, H., Li, X., Li, Z., Tang, L., & Wang, Z. (2018). Determination of Bitterness of Andrographis Herba Based on Electronic Tongue Technology and Discovery of the Key Compounds of Bitter Substances. Molecules, 23(12), 3362. https://doi.org/10.3390/molecules23123362





