Curcumin and Resveratrol in the Management of Cognitive Disorders: What is the Clinical Evidence?
Abstract
:1. Introduction
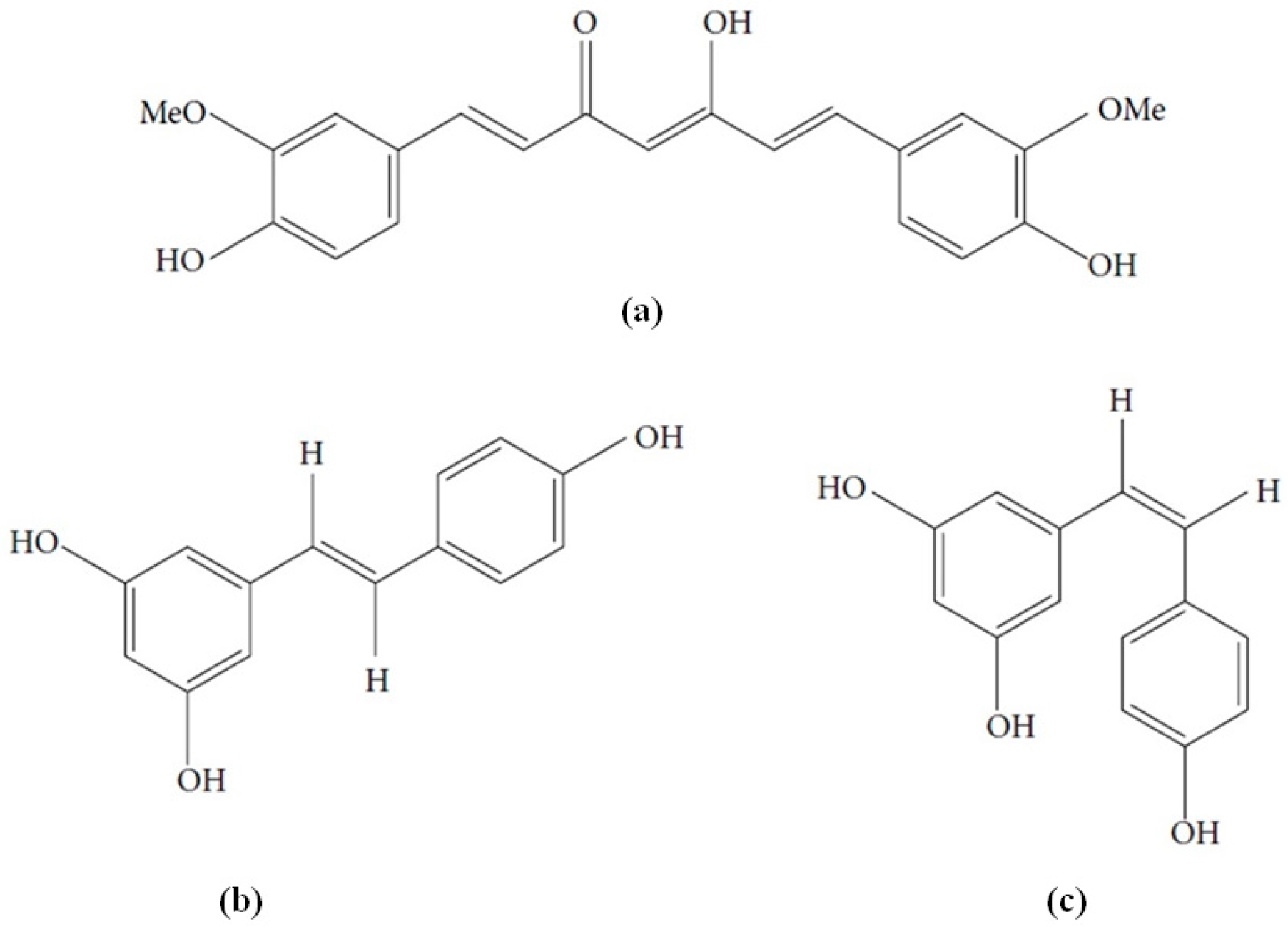
2. Mechanism of Neuroprotective Action of Curcumin and Resveratrol
3. Methods
4. Results
4.1. Curcumin
4.2. Resveratrol
5. Discussion
6. Conclusions
Acknowledgments
Conflicts of Interest
Abbreviations
| AD | Alzheimer disease |
| ADAS-Cog | Alzheimer’s Disease Assessment Scale-Cognitive subscale |
| ADCS-ADL | Alzheimer’s Disease Co-operative Study-Activities of Daily Living |
| AEs | Adverse Events |
| Aβ | Amyloid β |
| AUC | Area under the curve |
| BDPP | Bioactive Dietary Polyphenol Preparation |
| CANTAB | Cambridge Neuropsychological Test Automated Battery |
| CBF | Cerebral Blood Flow |
| CDB | Cognitive Demand Battery |
| CDR | Clinical Dementia Rating |
| CGIC | Clinical Global Impression of Change |
| CVR | Cerebral Vasodilator Responsiveness |
| DNMT1 | DNA Methyltransferase |
| EFSA | European Food Safety Authority |
| FDA | Food and Drug Administration |
| FDG-PET | 2-Deoxy-2-[fluorine-18]fluoro-d-glucose Positron Emission Tomography |
| FMD | Flow Mediated Dilatation |
| fMRI | functional Magnetic Resonance Imaging |
| HAT | Histone Acetyltransferases |
| HO-1 | Heme oxygenase-1 |
| iNOS | Inducible Nitric Oxide Synthase |
| MAPK | p38 Mitogen-activated protein kinase |
| MCI | Mild Cognitive Impairment |
| MMSE | Mini-Mental Status Examination |
| NF-kB | Nuclear factor kappa-light-chain-enhancer of activated B cells |
| NIRS | Near-Infrared Spectroscopy |
| NPI | Neuropsychiatric Inventory |
| NPI-Q | Neuropsychiatric Inventory-brief Questionnaire |
| PET | Positron Emission Tomography |
| RAI | Retinal Amyloid Index |
| RNS | Reactive Nitrogen Species |
| ROS | Reactive Oxygen Species |
| SAEs | Serious Adverse Events |
| SIRT-1 | Sirtuin-1 |
| STAT1 | Signal Transducer and Activator of Transcription 1 |
| STAT3 | Signal Transducer and Activator of Transcription 3 |
| TNF-α | Tumour Necrosis Factor α |
References
- Spagnuolo, C.; Napolitano, M.; Tedesco, I.; Moccia, S.; Milito, A.; Russo, G.L. Neuroprotective role of natural polyphenols. Curr. Top. Med. Chem. 2016, 16, 1943–1950. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.J.; Gan, R.Y.; Li, S.; Zhou, Y.; Li, A.N.; Xu, D.P.; Li, H.B. Antioxidant phytochemicals for the prevention and treatment of chronic diseases. Molecules 2015, 20, 21138–21156. [Google Scholar] [CrossRef] [PubMed]
- Alzheimer’s Disease International. The Global Voice on Dementia. Available online: https://www.alz.co.uk/research/WorldAlzheimerReport2015.pdf (accessed on 22 August 2016).
- World Health Organization. Available online: http://www.who.int/medicines/areas/priority_medicines/BP6_11Alzheimer.pdf (accessed on 22 August 2016).
- Dorszewska, J.; Prendecki, M.; Oczkowska, A.; Dezor, M.; Kozubski, W. Molecular basis of familial and sporadic Alzheimer’s disease. Curr. Alzheimer Res. 2016, 13, 952–963. [Google Scholar] [CrossRef] [PubMed]
- Apetz, N.; Munch, G.; Govindaraghavan, S.; Gyengesi, E. Natural compounds and plant extracts as therapeutics against chronic inflammation in Alzheimer’s disease—A translational perspective. CNS Neurol. Disord. Drug Targets 2014, 13, 1175–1191. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Singh, A.; Ekavali. A review on Alzheimer’s disease pathophysiology and its management: An update. Pharmacol. Rep. 2015, 67, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Goozee, K.G.; Shah, T.M.; Sohrabi, H.R.; Rainey-Smith, S.R.; Brown, B.; Verdile, G.; Martins, R.N. Examining the potential clinical value of curcumin in the prevention and diagnosis of Alzheimer’s disease. Br. J. Nutr. 2016, 115, 449–465. [Google Scholar] [CrossRef] [PubMed]
- Libro, R.; Giacoppo, S.; Soundara Rajan, T.; Bramanti, P.; Mazzon, E. Natural phytochemicals in the treatment and prevention of dementia: An overview. Molecules 2016, 21, 518. [Google Scholar] [CrossRef] [PubMed]
- Reddy, P.H.; Tripathi, R.; Troung, Q.; Tirumala, K.; Reddy, T.P.; Anekonda, V.; Shirendeb, U.P.; Calkins, M.J.; Reddy, A.P.; Mao, P.; et al. Abnormal mitochondrial dynamics and synaptic degeneration as early events in Alzheimer’s disease: Implications to mitochondria-targeted antioxidant therapeutics. Biochim. Biophys. Acta 2012, 1822, 639–649. [Google Scholar] [CrossRef] [PubMed]
- Noda, M. Dysfunction of glutamate receptors in microglia may cause neurodegeneration. Curr. Alzheimer Res. 2016, 13, 381–386. [Google Scholar] [CrossRef] [PubMed]
- Goedert, M.; Klug, A.; Crowther, R.A. Tau protein, the paired helical filament and Alzheimer disease. J. Alzheimers Dis. 2006, 9, 195–207. [Google Scholar] [PubMed]
- Di Domenico, F.; Pupo, G.; Giraldo, E.; Badìa, M.C.; Monllor, P.; Lloret, A.; Schininà, M.E.; Giorgi, A.; Cini, C.; Tramutola, A.; et al. Oxidative signature of cerebrospinal fluid from mild cognitive impairment and Alzheimer disease patients. Free Radic. Biol. Med. 2016, 91, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Sliwinska, A.; Kwiatkowski, D.; Czarny, P.; Toma, M.; Wigner, P.; Drzewoski, J.; Fabianowska-Majewska, K.; Szemraj, J.; Maes, M.; Galecki, P.; et al. The levels of 7,8-dihydrodeoxyguanosine (8-oxoG) and 8-oxoguanine DNA glycosylase 1 (OGG1)—A potential diagnostic biomarkers of Alzheimer’s disease. J. Neurol. Sci. 2016, 368, 155–159. [Google Scholar] [CrossRef] [PubMed]
- Faller, P.; Hureau, C.; Berthoumieu, O. Role of metal ions in the self-assembly of the Alzheimer’s amyloid-β peptide. Inorg. Chem. 2013, 52, 12193–12206. [Google Scholar] [CrossRef] [PubMed]
- Gella, A.; Durany, N. Oxidative stress in Alzheimer disease. Cell Adh. Migr. 2009, 3, 88–93. [Google Scholar] [CrossRef] [PubMed]
- McGeer, P.L.; McGeer, E.G. Local neuroinflammation and the progression of Alzheimer’s disease. J. Neurovirol. 2002, 8, 529–538. [Google Scholar] [CrossRef] [PubMed]
- Steiner, N.; Balez, R.; Karunaweera, N.; Lind, J.M.; Munch, G.; Ooi, L. Neuroprotection of Neuro2a cells and the cytokine suppressive and anti-inflammatory mode of action of resveratrol in activated RAW264.7 macrophages and C8-B4 microglia. Neurochem. Int. 2015, 95, 46–54. [Google Scholar] [CrossRef] [PubMed]
- Daniilidou, M.; Koutroumani, M.; Tsolaki, M. Epigenetic mechanisms in Alzheimer’s disease. Curr. Med. Chem. 2011, 18, 1751–1756. [Google Scholar] [CrossRef] [PubMed]
- Mastroeni, D.; Grover, A.; Delvaux, E.; Whiteside, C.; Coleman, P.D.; Rogers, J. Epigenetic mechanisms in Alzheimer’s disease. Neurobiol. Aging 2011, 32, 1161–1180. [Google Scholar] [CrossRef] [PubMed]
- Smith, A.R.; Smith, R.G.; Condliffe, D.; Hannon, E.; Schalkwyk, L.; Mill, J.; Lunnon, K. Increased DNA methylation near TREM2 is consistently seen in the superior temporal gyrus in Alzheimer’s disease brain. Neurobiol. Aging 2016, 47, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Shindikar, A.; Singh, A.; Nobre, M.; Kirolikar, S. Curcumin and resveratrol as promosing natural remedies with nanomedicine approach for the effective treatment of triple negative breast cancer. J. Oncol. 2016, 2016, 9750785. [Google Scholar] [CrossRef] [PubMed]
- Du, Q.; Hu, B.; An, H.M.; Shen, K.P.; Xu, L.; Deng, S.; Wei, M.M. Synergistic anticancer effects of curcumin and resveratrol in Hepa1-6 hepatocellular carcinoma cells. Oncol. Rep. 2013, 29, 1851–1858. [Google Scholar] [PubMed]
- Masuelli, L.; di Stefano, E.; Fantini, M.; Mattera, R.; Benvenuto, M.; Marzocchella, L.; Sacchetti, P.; Focaccetti, C.; Bernardini, R.; Tresoldi, I.; et al. Resveratrol potentiates the in vitro and in vivo anti-tumoral effects of curcumin in head and neck carcinomas. Oncotarget 2014, 5, 10745–10762. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, B.B.; Sundaram, C.; Malani, N.; Ichikawa, H. Curcumin: The Indian solid gold. Adv. Exp. Med. Biol. 2007, 595, 1–75. [Google Scholar] [PubMed]
- Gupta, S.C.; Sung, B.; Kim, J.H.; Prasad, S.; Li, S.; Aggarwal, B.B. Multitargeting by turmeric, the golden spice: From kitchen to clinic. Mol. Nutr. Food Res. 2013, 57, 1510–1528. [Google Scholar] [CrossRef] [PubMed]
- Rajakrishnan, V.; Viswanathan, P.; Rajasekharan, K.N.; Menon, V.P. Neuroprotective role of curcumin from Curcuma longa on ethanol-induced brain damage. Phytother. Res. 1999, 13, 571–574. [Google Scholar] [CrossRef]
- Shytle, R.D.; Tan, J.; Bickford, P.C.; Rezai-Zadeh, K.; Hou, L.; Zeng, J.; Sanberg, P.R.; Sanberg, C.D.; Alberte, R.S.; Fink, R.C.; et al. Optimized turmeric extract reduces β-amyloid and phosphorylated tau protein burden in Alzheimer’s transgenic mice. Curr. Alzheimer Res. 2012, 9, 500–506. [Google Scholar] [CrossRef] [PubMed]
- Ganguli, M.; Chandra, V.; Kamboh, M.I.; Johnston, J.M.; Dodge, H.H.; Thelma, B.K.; Juyal, R.C.; Pandav, R.; Belle, S.H.; DeKosky, S.T. Apolipoprotein E polymorphism and Alzheimer disease: The Indo-US cross-national dementia study. Arch. Neurol. 2000, 57, 824–830. [Google Scholar] [CrossRef] [PubMed]
- Chandra, V.; Pandav, R.; Dodge, H.H.; Johnston, J.M.; Belle, S.H.; DeKosky, S.T.; Ganguli, M. Incidence of Alzheimer’s disease in a rural community in India: the Indo-US study. Neurology 2001, 57, 985–989. [Google Scholar] [CrossRef] [PubMed]
- Shaji, S.; Bose, S.; Verghese, A. Prevalence of dementia in an urban population in Kerala, India. Br. J. Psychiatry 2005, 186, 136–140. [Google Scholar] [CrossRef] [PubMed]
- Ng, T.P.; Chiam, P.C.; Lee, T.; Chua, H.C.; Lim, L.; Kua, E.H. Curry consumption and cognitive function in the elderly. Am. J. Epidemiol. 2006, 164, 898–906. [Google Scholar] [CrossRef] [PubMed]
- Cvejic, J.M.; Djekic, S.V.; Petrovic, A.V.; Atanackovic, M.T.; Jovic, S.M.; Brceski, I.D.; Gojkovic-Bukarica, L.C. Determination of trans- and cis-Resveratrol in Serbian Commercial Wines. J. Chromatogr. Sci. 2010, 48, 229–234. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; He, M.; Cao, J.; Wang, H.; Ding, J.; Jiao, Y.; Li, R.; He, J.; Wang, D.; Wang, Y. The comparative analysis of the potential relationship between resveratrol and stilbene synthase gene family in the development stages of grapes (Vitis quinquangularis and Vitis vinifera). Plant Physiol. Biochem. 2014, 74, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Moreno, M.; Castro, E.; Falqué, E. Evolution of trans- and cis- resveratrol content in red grapes (Vitis vinifera L. cv Menciá, Albarello and Merenzao) during ripening. Eur. Food Res. Technol. 2008, 227, 667–674. [Google Scholar] [CrossRef]
- Trela, B.C.; Waterhouse, A.L. Resveratrol: Isomeric molar absorptivities and stability. J. Agric. Food Chem. 1996, 44, 1253–1257. [Google Scholar] [CrossRef]
- Smoliga, J.M.; Baur, J.A.; Hausenblas, H.A. Resveratrol and health—A comprehensive review of human clinical trials. Mol. Nutr. Food Res. 2011, 55, 1129–1141. [Google Scholar] [CrossRef] [PubMed]
- Luchsinger, J.A.; Noble, J.M.; Scarmeas, N. Diet and Alzheimer’s disease. Curr. Neurol. Neurosci. Rep. 2007, 7, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Orgogozo, J.M.; Dartigues, J.F.; Lafont, S.; Letenneur, L.; Commenges, D.; Salamon, R.; Renaud, S.; Breteler, M.B. Wine consumption and dementia in the elderly: A prospective community study in the Bordeaux area. Rev. Neurol. 1997, 153, 185–192. [Google Scholar] [PubMed]
- Ono, K.; Hasegawa, K.; Naiki, H.; Yamada, M. Curcumin has potent anti-amyloidogenic effects for Alzheimer’s β-amyloid fibrils in vitro. J. Neurosci. Res. 2004, 75, 742–750. [Google Scholar] [CrossRef] [PubMed]
- Lim, G.P.; Chu, T.; Yang, F.; Beech, W.; Frautschy, S.A.; Cole, G.M. The curry spice curcumin reduces oxidative damage and amyloid pathology in an Alzheimer transgenic mouse. J. Neurosci. 2001, 21, 8370–8377. [Google Scholar] [PubMed]
- Fu, Z.; Aucoin, D.; Ahmed, M.; Ziliox, M.; van Nostrand, W.E.; Smith, S.O. Capping of Aβ42 oligomers by small molecule inhibitors. Biochemistry 2014, 53, 7893–7903. [Google Scholar] [CrossRef] [PubMed]
- Mithu, V.S.; Sarkar, B.; Bhowmik, D.; Das, A.K.; Chandrakesan, M.; Maiti, S.; Madhu, P.K. Curcumin alters the salt bridge-containing turn region in amyloid β(1-42) aggregates. J. Biol. Chem. 2014, 289, 11122–11131. [Google Scholar] [CrossRef] [PubMed]
- Frautschy, S.A.; Hu, W.; Kim, P.; Miller, S.A.; Chu, T.; Harris-White, M.E.; Cole, G.M. Phenolic anti-inflammatory antioxidant reversal of Aβ-induced cognitive deficits and neuropathology. Neurobiol. Aging 2001, 22, 993–1005. [Google Scholar] [CrossRef]
- Ahmed, T.; Enam, S.A.; Gilani, A.H. Curcuminoids enhance memory in an amyloid-infused rat model of Alzheimer’s disease. Neuroscience 2010, 169, 1296–1306. [Google Scholar] [CrossRef] [PubMed]
- Belviranlı, M.; Okudan, N.; Atalık, K.E.; Öz, M. Curcumin improves spatial memory and decreases oxidative damage in aged female rats. Biogerontology 2013, 14, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Marambaud, P.; Zhao, H.; Davies, P. Resveratrol promotes clearance of Alzheimer’s disease amyloid-β peptides. J. Biol. Chem. 2005, 280, 37377–37382. [Google Scholar] [CrossRef] [PubMed]
- Bastianetto, S.; Ménard, C.; Quirion, R. Neuroprotective action of resveratrol. Biochim. Biophys. Acta 2015, 1852, 1195–1201. [Google Scholar] [CrossRef] [PubMed]
- Richard, T.; Poupard, P.; Nassra, M.; Papastamoulis, Y.; Iglesias, M.L.; Krisa, S.; Waffo-Teguo, P.; Merillon, J.M.; Monti, J.P. Protective effect of epsilon-viniferin on betaamyloid peptide aggregation investigated by electrospray ionization mass spectrometry. Bioorg. Med. Chem. 2011, 19, 3152–3155. [Google Scholar] [CrossRef] [PubMed]
- Granzotto, A.; Zatta, P. Resveratrol acts not through anti-aggregative pathways but mainly via its scavenging properties against Aβ and Aβ-metal complexes toxicity. PLoS ONE 2011, 6, e21565. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Lee, H.J.; Lee, K.W. Naturally occurring phytochemicals for the prevention of Alzheimer’s disease. J. Neurochem. 2010, 112, 1415–1430. [Google Scholar] [CrossRef] [PubMed]
- Wahlster, L.; Arimon, M.; Nasser-Ghodsi, N.; Post, K.L.; Serrano-Pozo, A.; Uemura, K.; Berezovska, O. Presenilin-1 adopts pathogenic conformation in normal aging and in sporadic Alzheimer’s disease. Acta Neuropathol. 2013, 125, 187–199. [Google Scholar] [CrossRef] [PubMed]
- Wei, Q.Y.; Chen, W.F.; Zhou, B.; Yang, L.; Liu, Z.L. Inhibition of lipid peroxidation and protein oxidation in rat liver mitochondria by curcumin and its analogues. Biochim. Biophys. Acta 2006, 1760, 70–77. [Google Scholar] [CrossRef] [PubMed]
- Agnihotri, N.; Mishra, P.C. Scavenging mechanism of curcumin toward the hydroxyl radical: A theoretical study of reactions producing ferulic acid and vanillin. J. Phys. Chem. A 2011, 115, 14221–14232. [Google Scholar] [CrossRef] [PubMed]
- Baum, L.; Ng, A. Curcumin interaction with copper and iron suggests one possible mechanism of action in Alzheimer’s disease animal models. J. Alzheimers Dis. 2004, 6, 367–377. [Google Scholar] [PubMed]
- Banerjee, R. Effect of curcumin on the metal ion induced fibrillization of amyloid-β peptide. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2014, 117, 798–800. [Google Scholar] [CrossRef] [PubMed]
- Nishinaka, T.; Ichijo, Y.; Ito, M.; Kimura, M.; Katsuyama, M.; Iwata, K.; Miura, T.; Terada, T.; Yabe-Nishimura, C. Curcumin activates human glutathione S-transferase P1 expression through antioxidant response element. Toxicol. Lett. 2007, 170, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Ishrat, T.; Hoda, M.N.; Khan, M.B.; Yousuf, S.; Ahmad, M.; Khan, M.M.; Ahmad, A.; Islam, F. Amelioration of cognitive deficits and neurodegeneration by curcumin in rat model of sporadic dementia of Alzheimer’s type (SDAT). Eur. Neuropsychopharmacol. 2009, 19, 636–647. [Google Scholar] [CrossRef] [PubMed]
- Motterlini, R.; Foresti, R.; Bassi, R.; Green, C.J. Curcumin, an antioxidant and anti-inflammatory agent, induces heme oxygenase-1 and protects endothelial cells against oxidative stress. Free Radic. Biol. Med. 2000, 28, 1303–1312. [Google Scholar] [CrossRef]
- González-Reyes, S.; Guzmán-Beltrán, S.; Medina-Campos, O.N.; Pedraza-Chaverri, J. Curcumin pretreatment induces Nrf2 and an antioxidant response and prevents hemin-induced toxicity in primary cultures of cerebellar granule neurons of rats. Oxid. Med. Cell Longev. 2013, 2013, 801418. [Google Scholar] [CrossRef] [PubMed]
- Begum, A.N.; Jones, M.R.; Lim, G.P.; Morihara, T.; Kim, P.; Heath, D.D.; Rock, C.L.; Pruitt, M.A.; Yang, F.; Hudspeth, B.; et al. Curcumin structure-function, bioavailability, and efficacy in models of neuroinflammation and Alzheimer’s disease. J. Pharmacol. Exp. Ther. 2008, 326, 196–208. [Google Scholar] [CrossRef] [PubMed]
- Zhuang, H.; Kim, Y.S.; Koehler, R.C.; Dore, S. Potential mechanism by which resveratrol, a red wine constituent, protects neurons. Ann. N. Y. Acad. Sci. 2003, 993, 276–286. [Google Scholar] [CrossRef] [PubMed]
- Candelario-Jalil, E.; de Oliveira, A.C.; Graf, S.; Bhatia, H.S.; Hull, M.; Munoz, E.; Fiebich, B.L. Resveratrol potently reduces prostaglandin E2production and free radical formation in lipopolysaccharide-activated primary rat microglia. J. Neuroinflam. 2007, 4, 25. [Google Scholar] [CrossRef] [PubMed]
- Jang, J.H.; Surh, Y.J. Protective effect of resveratrol on β-amyloid- induced oxidative PC12 cell death. Free Radic. Biol. Med. 2003, 34, 1100–1110. [Google Scholar] [CrossRef]
- Kwon, K.J.; Kim, H.J.; Shin, C.Y.; Han, S.H. Melatonin potentiates the neuroprotective properties of resveratrol against betaamyloid-induced neurodegeneration by modulating AMP activated protein kinase pathways. J. Clin. Neurol. 2010, 6, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Koukoulitsa, C.; Villalonga-Barber, C.; Csonka, R.; Alexi, X.; Leonis, G.; Dellis, D.; Hamelink, E.; Belda, O.; Steele, B.R.; Micha-Screttas, M.; et al. Biological and computational evaluation of resveratrol inhibitors against Alzheimer’s disease. J. Enzyme Inhib. Med. Chem. 2016, 31, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.; Li, Y. Potent induction of cellular antioxidants and phase 2 enzymes by resveratrol in cardiomyocytes: Protection against oxidative and electrophilic injury. Eur. J. Pharmacol. 2004, 489, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Kwon, K.J.; Kim, J.N.; Kim, M.K.; Lee, J.; Ignarro, L.J.; Kim, H.J.; Shin, C.Y.; Han, S.H. Melatonin synergistically increases resveratrolinduced heme oxygenase-1 expression through the inhibition of ubiquitin-dependent proteasome pathway: A possible role in neuroprotection. J. Pineal Res. 2011, 50, 110–123. [Google Scholar] [PubMed]
- Sharma, M.; Gupta, Y.K. Chronic treatment with trans-resveratrol prevents intracerebroventricular streptozotocin induced cognitive impairment and oxidative stress in rats. Life Sci. 2002, 71, 2489–2498. [Google Scholar] [CrossRef]
- Kumar, A.; Naidu, P.S.; Seghal, N.; Padi, S.S. Neuroprotective effects of resveratrol against intracerebroventricular colchicine-induced cognitive impairment and oxidative stress in rats. Pharmacology 2007, 79, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Sadigh-Eteghad, S.; Majdi, A.; Mahmoudi, J.; Golzari, S.E.; Talebi, M. Astrocytic and microglial nicotinic acetylcholine receptors: An overlooked issue in Alzheimer’s disease. J. Neural. Transm. 2016. [Google Scholar] [CrossRef] [PubMed]
- Nanji, A.A.; Jokelainen, K.; Tipoe, G.L.; Rahemtulla, A.; Thomas, P.; Dannenberg, A.J. Curcumin prevents alcohol-induced liver disease in rats by inhibiting the expression of NF-κB-dependent genes. Am. J. Physiol. Gastrointest. Liver Physiol. 2003, 284, G321–G327. [Google Scholar] [CrossRef] [PubMed]
- Bengmark, S. Curcumin, an atoxic antioxidant and natural NF-κB, cyclooxygenase-2, lipooxygenase, and inducible nitric oxide synthase inhibitor: A shield against acute and chronic diseases. J. Parenter. Enter. Nutr. 2006, 30, 45–51. [Google Scholar] [CrossRef]
- Sandur, S.K.; Ichikawa, H.; Pandey, M.K.; Kunnumakkara, A.B.; Sung, B.; Sethi, G.; Aggarwal, B.B. Role of pro-oxidants and antioxidants in the anti-inflammatory and apoptotic effects of curcumin (diferuloylmethane). Free Radic. Biol. Med. 2007, 43, 568–580. [Google Scholar] [CrossRef] [PubMed]
- Karunaweera, N.; Raju, R.; Gyengesi, E.; Münch, G. Plant polyphenols as inhibitors of NF-κB induced cytokine production—A potential antiinflammatory treatment for Alzheimer’s disease? Front. Mol. Neurosci. 2015, 8, 24. [Google Scholar] [CrossRef] [PubMed]
- Millington, C.; Sonego, S.; Karunaweera, N.; Rangel, A.; Aldrich-Wright, J.R.; Campbell, I.L.; Gyengesi, E.; Münch, G. Chronic neuroinflammation in Alzheimer’s disease: New perspectives on animal models and promising candidate drugs. BioMed Res. Int. 2014, 2014, 309129. [Google Scholar] [CrossRef] [PubMed]
- Venigalla, M.; Sonego, S.; Gyengesi, E.; Sharman, M.J.; Münch, G. Novel promising therapeutics against chronic neuroinflammation and neurodegeneration in Alzheimer’s disease. Neurochem. Int. 2016, 95, 63–74. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Xu, J.; Rottinghaus, G.E.; Simonyi, A.; Lubahn, D.; Sun, G.Y.; Sun, A.Y. Resveratrol protects against global cerebral ischemic injury in gerbils. Brain Res. 2002, 958, 439–447. [Google Scholar] [CrossRef]
- Bi, X.L.; Yang, J.Y.; Dong, Y.X.; Wang, J.M.; Cui, Y.H.; Ikeshima, T.; Zhao, Y.Q.; Wu, C.F. Resveratrol inhibits nitric oxide and TNF-α production by lipopolysaccharide-activated microglia. Int. Immunopharmacol. 2005, 5, 185–193. [Google Scholar] [CrossRef] [PubMed]
- Cheng, X.; Wang, Q.; Li, N.; Zhao, H. Effects of resveratrol on hippocampal astrocytes and expression of TNF-α in Alzheimer’s disease model rate. J. Hyg. Res. 2015, 44, 610–614. [Google Scholar]
- Rahman, I.; Biswas, S.K.; Kirkham, P.A. Regulation of inflammation and redox signaling by dietary polyphenols. Biochem. Pharmacol. 2006, 72, 1439–1452. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.C.; Lu, K.T.; Wo, Y.Y.; Wu, Y.J.; Yang, Y.L. Resveratrol protects rats from Aβ-induced neurotoxicity by the reduction of iNOS expression and lipid peroxidation. PLoS ONE 2011, 6, e29102. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Li, J.; Niu, Y.; Yu, J.Q.; Yan, L.; Miao, Z.H.; Zhao, X.X.; Li, Y.J.; Yao, W.X.; Zheng, P.; et al. Resveratrol inhibits oligomeric Aβ-induced microglial activation via NADPH oxidase. Mol. Med. Rep. 2015, 12, 6133–6139. [Google Scholar] [PubMed]
- Capiralla, H.; Vingtdeux, V.; Zhao, H.; Sankowski, R.; Al-Abed, Y.; Davies, P.; Marambaud, P. Resveratrol mitigates lipopolysaccharide- and Aβ-mediated microglial inflammation by inhibiting the TLR4/NF-κB/STAT signaling cascade. J. Neurochem. 2012, 120, 461–472. [Google Scholar] [CrossRef] [PubMed]
- Sezgin, Z.; Dincer, Y. Alzheimer’s disease and epigenetic diet. Neurochem. Int. 2014, 78, 105–116. [Google Scholar] [CrossRef] [PubMed]
- Boyanapalli, S.S.; Tony Kong, A.N. “Curcumin, the king of spices”: Epigenetic regulatory mechanisms in the prevention of cancer, neurological, and inflammatory diseases. Curr. Pharmacol. Rep. 2015, 1, 129–139. [Google Scholar] [CrossRef] [PubMed]
- Hardy, M.T.; Tollefsbol, T.O. Epigenetic diet: Impact on the epigenome and cancer. Epigenomics 2011, 3, 503–518. [Google Scholar] [CrossRef] [PubMed]
- Feng, J.; Zhou, Y.; Campbell, S.L.; Le, T.; Li, E.; Sweatt, J.D.; Silva, A.J.; Fan, G. Dnmt1 and Dnmt3a maintain DNA methylation and regulate synaptic function in adult forebrain neurons. Nat. Neurosci. 2010, 13, 423–430. [Google Scholar] [CrossRef] [PubMed]
- Fan, G.; Beard, C.; Chen, R.Z.; Csankovszki, G.; Sun, Y.; Siniaia, M.; Biniszkiewicz, D.; Bates, B.; Lee, P.P.; Kuhn, R.; et al. DNA hypomethylation perturbs the function and survival of CNS neurons in postnatal animals. J. Neurosci. 2001, 21, 788–797. [Google Scholar] [PubMed]
- Iskandar, B.J.; Rizk, E.; Meier, B.; Hariharan, N.; Bottiglieri, T.; Finnell, R.H.; Jarrard, D.F.; Banerjee, R.V.; Skene, J.H.; Nelson, A.; et al. Folate regulation of axonal regeneration in the rodent central nervous system through DNA methylation. J. Clin. Investig. 2010, 120, 1603–1616. [Google Scholar] [CrossRef] [PubMed]
- Huber, K.; Superti-Furga, G. After the grape rush: Sirtuins as epigenetic drug targets in neurodegenerative disorders. Bioorg. Med. Chem. 2011, 19, 3616–3624. [Google Scholar] [CrossRef] [PubMed]
- Porquet, D.; Grinan-Ferre, C.; Ferrer, I.; Camins, A.; Sanfeliu, C.; del Valle, J.; Pallàs, M. Neuroprotective role of trans-resveratrol in a murine model of familial Alzheimer’s disease. J. Alzheimers Dis. 2014, 42, 1209–1220. [Google Scholar] [PubMed]
- National Institutes of Health, Clinical Trials.gov. Available online: https://clinicaltrials.gov/ (accessed on 15 June 2016).
- Australian New Zealand Clinical Trials Registry. Available online: http://anzctr.org.au (accessed on 15 June 2016).
- Lamport, D.J.; Pal, D.; Moutsiana, C.; Field, D.T.; Williams, C.M.; Spencer, J.P.; Butler, L.T. The effect of flavanol-rich cocoa on cerebral perfusion in healthy older adults during conscious resting state: A placebo controlled, crossover, acute trial. Psychopharmacology 2015, 232, 3227–3234. [Google Scholar] [CrossRef] [PubMed]
- Baum, L.; Lam, C.W.; Cheung, S.K.; Kwok, T.; Lui, V.; Tsoh, J.; Lam, L.; Leung, V.; Hui, E.; Ng, C.; et al. Six-month randomized, placebo-controlled, double-blind, pilot clinical trial of curcumin in patients with Alzheimer disease. J. Clin. Psychopharmacol. 2008, 28, 110–113. [Google Scholar] [CrossRef] [PubMed]
- Ringman, J.M.; Frautschy, S.A.; Teng, E.; Begum, A.N.; Bardens, J.; Beigi, M.; Gylys, K.H.; Badmaev, V.; Heath, D.D.; Apostolova, L.G.; et al. Oral curcumin for Alzheimer’s disease: Tolerability and efficacy in a 24-week randomized, double blind, placebo-controlled study. Alzheimers Res. Ther. 2012, 4, 43. [Google Scholar] [CrossRef] [PubMed]
- Hishikawa, N.; Takahashi, Y.; Amakusa, Y.; Tanno, Y.; Tuji, Y.; Niwa, H.; Murakami, N.; Krishna, U.K. Effects of turmeric on Alzheimer’s disease with behavioral and psychological symptoms of dementia. AYU 2012, 33, 499–504. [Google Scholar] [CrossRef] [PubMed]
- Cox, K.H.; Pipingas, A.; Scholey, A.B. Investigation of the effects of solid lipid curcumin on cognition and mood in a healthy older population. J. Psychopharmacol. 2015, 29, 642–651. [Google Scholar] [CrossRef] [PubMed]
- Rainey-Smith, S.R.; Brown, B.M.; Sohrabi, H.R.; Shah, T.; Goozee, K.G.; Gupta, V.B.; Martins, R.N. Curcumin and cognition: A randomised, placebo-controlled, double-blind study of community-dwelling older adults. Br. J. Nutr. 2016, 115, 2106–2113. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health, Clinical Trials.gov. Early Intervention in Mild Cognitive Impairment (MCI) With Curcumin + Bioperine. Available online: https://clinicaltrials.gov/ct2/show/NCT00595582 (accessed on 15 June 2016).
- National Institutes of Health, Clinical Trials.gov. Efficacy and Safety of Curcumin Formulation in Alzheimer’s Disease. Available online: https://clinicaltrials.gov/ct2/show/NCT01001637 (accessed on 15 June 2016).
- National Institutes of Health, Clinical Trials.gov. 18-Month Study of Curcumin (Curcumin). Available online: https://clinicaltrials.gov/ct2/show/NCT01383161 (accessed on 15 June 2016).
- National Institutes of Health, Clinical Trials.gov. Curcumin and Yoga Therapy for Those at Risk for Alzheimer’s Disease. Available online: https://clinicaltrials.gov/ct2/show/NCT01811381 (accessed on 15 June 2016).
- Australian New Zealand Clinical Trials Registry. Investigation of the Effects of Longvida Curcumin on Cognitive Function, Mood and Biomarkers of Health. Available online: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=370499 (accessed on 15 June 2016).
- Australian New Zealand Clinical Trials Registry. McCusker KARVIAH: Curcumin in Alzheimer’s Disease Prevention. Available online: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?ACTRN=12613000681752 (accessed on 15 June 2016).
- Australian New Zealand Clinical Trials Registry. The Epigenetic Effect of Curcumin as Measured in the Blood and Seen within Lifestyle, for the Prevention of Alzheimer’s Disease. Available online: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=366926 (accessed on 15 June 2016).
- Australian New Zealand Clinical Trials Registry. This Study Will Evaluate if an Eye Examination Can Identify Changes in the Structure of the Retina Which May Help in the Early Detection of Alzheimer’s Disease. Available online: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=363949 (accessed on 15 June 2016).
- Australian New Zealand Clinical Trials Registry. Imaging of Retinal Amyloid Plaques in Alzheimer’s Disease—Longitudinal Study. Available online: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=368267 (accessed on 15 June 2016).
- Australian New Zealand Clinical Trials Registry. Imaging of Retinal Amyloid Plaques in Alzheimer’s Disease—Middle Aged Controls Study. Available online: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=368764 (accessed on 15 June 2016).
- Kennedy, D.; Wightman, E.L.; Reay, J.L.; Lietz, G.; Okello, E.J.; Wilde, A.; Haskell, C.F. Effects of resveratrol on cerebral blood flow variables and cognitive performance in humans: A double-blind, placebo-controlled, crossover investigation. Am. J. Clin. Nutr. 2010, 91, 1590–1597. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.H.; Berry, N.M.; Coates, A.M.; Buckley, J.D.; Bryan, J.; Kunz, I.; Howe, P.R. Chronic resveratrol consumption improves brachial flow-mediated dilatation in healthy obese adults. J. Hypertens. 2013, 31, 1819–1827. [Google Scholar] [CrossRef] [PubMed]
- Witte, A.V.; Kerti, L.; Margulies, D.S.; Flöel, A. Effects of resveratrol on memory performance, hippocampal functional connectivity, and glucose metabolism in healthy older adults. J. Neurosci. 2014, 34, 7862–7870. [Google Scholar] [CrossRef] [PubMed]
- Wightman, E.L.; Reay, JL.; Haskell, CF.; Williamson, G.; Dew, T.P.; Kennedy, D.O. Effects of resveratrol alone or in combination with piperine on cerebral blood flow parameters and cognitive performance in human subjects: A randomised, double-blind, placebo-controlled, cross-over investigation. Br. J. Nutr. 2014, 112, 203–213. [Google Scholar] [CrossRef] [PubMed]
- Turner, R.S.; Thomas, R.G.; Craft, S.; van Dyck, C.H.; Mintzer, J.; Reynolds, B.A.; Brewer, J.B.; Rissman, R.A.; Raman, R.; Aisen, P.S. Alzheimer’s disease cooperative study. A randomized, double-blind, placebo-controlled trial of resveratrol for Alzheimer disease. Neurology 2015, 85, 1383–1391. [Google Scholar] [CrossRef] [PubMed]
- Wong, R.H.; Nealon, R.S.; Scholey, A.; Howe, P.R. Low dose resveratrol improves cerebrovascular function in type 2 diabetes mellitus. Nutr. Metab. Cardiovasc. Dis. 2016, 26, 393–399. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health, Clinical Trials.gov. Pilot Study of the Effects of Resveratrol Supplement in Mild-to-moderate Alzheimer’s Disease. Available online: https://clinicaltrials.gov/ct2/show/NCT00743743 (accessed on 15 June 2016).
- National Institutes of Health, Clinical Trials.gov. Randomized Trial of a Nutritional Supplement in Alzheimer’s Disease. Available online: https://clinicaltrials.gov/ct2/show/NCT00678431 (accessed on 15 June 2016).
- National Institutes of Health, Clinical Trials.gov. Resveratrol for Improved Performance in the Elderly (RIPE). Available online: https://clinicaltrials.gov/ct2/show/NCT01126229 (accessed on 15 June 2016).
- Anton, S.D.; Embry, C.; Marsiske, M.; Lu, X.; Doss, H.; Leeuwenburgh, C.; Manini, T.M. Safety and metabolic outcomes of resveratrol supplementation in older adults: Results of a twelve-week, placebo-controlled pilot study. Exp. Gerontol. 2014, 57, 181–187. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health, Clinical Trials.gov. Cognitive Effects of 500 mg Trans-resveratrol. Available online: https://clinicaltrials.gov/ct2/show/NCT01794351 (accessed on 15 June 2016).
- National Institutes of Health, Clinical Trials.gov. Effects of Dietary Interventions on the Brain in Mild Cognitive Impairment (MCI). Available online: https://clinicaltrials.gov/ct2/show/NCT01219244 (accessed on 15 June 2016).
- National Institutes of Health, Clinical Trials.gov. Cerebrovascular and Cognitive Improvement by Resveratrol (resVida) and Fruitflow-II (CCIRF-II) (CCIRF-II). Available online: https://clinicaltrials.gov/ct2/show/NCT01766180 (accessed on 15 June 2016).
- National Institutes of Health, Clinical Trials.gov. Impact of Resveratrol on Brain Function and Structure. Available online: https://clinicaltrials.gov/ct2/show/NCT02621554 (accessed on 15 June 2016).
- National Institutes of Health, Clinical Trials.gov. BDPP Treatment for Mild Cognitive Impairment (MCI) and Prediabetes (BDPP). Available online: https://clinicaltrials.gov/ct2/show/NCT02502253 (accessed on 15 June 2016).
- Australian New Zealand Clinical Trials Registry. The Effect of Resveratrol in Red Wine on Cognitive Function in Older Adults: Preliminary Study. Available online: https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=347694 (accessed on 15 June 2016).
- Lovibond, P.F.; Lovibond, S.H. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behav. Res. Ther. 1995, 3, 335–343. [Google Scholar] [CrossRef]
- Nasreddine, Z.S.; Phillips, N.A.; Bédirian, V.; Charbonneau, S.; Whitehead, V.; Collin, I.; Cummings, J.L.; Chertkow, H. The Montreal Cognitive Assessment, MoCA: A brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 2005, 53, 695–699. [Google Scholar] [CrossRef] [PubMed]
- National Institutes of Health, Clinical Trials.gov. Early Detection of Mild Cognitive Impairment in Individual Patients. Available online: https://clinicaltrials.gov/ct2/show/study/NCT00243451 (accessed on 15 June 2016).
- Ahmed, T.; Javed, S.; Javed, S.; Tariq, A.; Šamec, D.; Tejada, S.; Nabavi, S.F.; Braidy, N.; Nabavi, S.M. Resveratrol and Alzheimer’s disease: Mechanistic insights. Mol. Neurobiol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Cheng, A.L.; Hsu, C.H.; Lin, J.K.; Hsu, M.M.; Ho, Y.F.; Shen, T.S.; Ko, J.Y.; Lin, J.T.; Lin, B.R.; Ming-Shiang, W.; et al. Phase I clinical trial of curcumin, a chemopreventive agent, in patients with high-risk or pre-malignant lesions. Anticancer Res. 2001, 21, 2895–2900. [Google Scholar] [PubMed]
- Cottart, C.H.; Nivet-Antoine, V.; Beaudeux, J.L. Review of recent data on the metabolism, biological effects, and toxicity of resveratrol in humans. Mol. Nutr. Food Res. 2014, 58, 7–21. [Google Scholar] [CrossRef] [PubMed]
- Kanai, M. Therapeutic applications of curcumin for patients with pancreatic cancer. World J. Gastroenterol. 2014, 20, 9384–9391. [Google Scholar] [PubMed]
- Erdogan, C.S.; Vang, O. Challenges in analyzing the biological effects of resveratrol. Nutrients 2016, 8, 353. [Google Scholar] [CrossRef] [PubMed]
- Morbidelli, L. Polyphenol-based nutraceuticals for the control of angiogenesis: Analysis of the critical issues for human use. Pharmacol. Res. 2016, 111, 384–393. [Google Scholar] [CrossRef] [PubMed]
- Prasad, S.; Tyagi, A.K.; Aggarwal, B.B. Recent developments in delivery, bioavailability, absorption and metabolism of curcumin: the Golden pigment from golden spice. Cancer Res. Treat. 2014, 46, 2–18. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.J.; Nihal, M.; Siddiqui, I.A.; Scarlett, C.O.; Bailey, H.H.; Mukhtar, H.; Ahmad, N. Enhancing the bioavailability of resveratrol by combining it with piperine. Mol. Nutr. Food Res. 2011, 55, 1169–1176. [Google Scholar] [CrossRef] [PubMed]
- Nahar, P.P.; Slitt, A.L.; Seeram, N.P. Anti-inflammatory effects of novel standardized solid lipid curcumin formulations. J. Med. Food 2015, 18, 786–792. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, H.; Sunagawa, Y.; Takahashi, K.; Imaizumi, A.; Fukuda, H.; Hashimoto, T.; Wada, H.; Katanasaka, Y.; Kakeya, H.; Fujita, M.; et al. Innovative preparation of curcumin for improved oral bioavailability. Biol. Pharm. Bull. 2011, 34, 660–665. [Google Scholar] [CrossRef] [PubMed]
- Antony, B.; Merina, B.; Iyer, V.S.; Judy, N.; Lennertz, K.; Joyal, S. A pilot cross-over study to evaluate human oral bioavailability of BCM-95®CG (Biocurcumax™), a novel bioenhanced preparation of curcumin. Indian J. Pharm. Sci. 2008, 70, 445–449. [Google Scholar] [CrossRef] [PubMed]
- Aggarwal, B.B.; Yuan, W.; Li, S.; Gupta, S.C. Curcumin-free turmeric exhibits anti-inflammatory and anticancer activities: Identification of novel components of turmeric. Mol. Nutr. Food Res. 2013, 57, 1529–1542. [Google Scholar] [CrossRef] [PubMed]
- Ryu, E.K.; Choe, Y.S.; Lee, K.H.; Choi, Y.; Kim, BT. Curcumin and dehydrozingerone derivatives: Synthesis, radiolabeling, and evaluation for β-amyloid plaque imaging. J. Med. Chem. 2006, 49, 6111–6119. [Google Scholar] [CrossRef] [PubMed]
- Koronyo-Hamaoui, M.; Koronyo, Y.; Ljubimov, A.V.; Miller, C.A.; Ko, M.K.; Black, K.L.; Schwartz, M.; Farkas, D.L. Identification of amyloid plaques in retinas from Alzheimer’s patients and noninvasive in vivo optical imaging of retinal plaques in a mouse model. Neuroimage 2011, 54, S204–S217. [Google Scholar] [CrossRef] [PubMed]
| Reference and/or ID (Location) | Study Design Phase | Curcumin Preparation and Dose [Other Medication] | Duration | Subjects n Age Disorder/Status | Primary Purpose | Main Results | Adverse Events | Status |
|---|---|---|---|---|---|---|---|---|
| Baum et al. [96] (Hong Kong, China) NCT00164749 | R, DB, PC NR | Curcumin 1 or 4 g/day (standardized ginkgo extract 120 mg/day) | 6 months | 34 ≥50 years Probable or possible AD | Effect in AD | No significant differences between curcumin and PL | No differences between curcumin and PL | Published |
| Ringman et al. [97] (Westwood, CA, USA) NCT00099710 | R, DB, PC Phase 2 | Curcumin C3 Complex® 2 or 4 g/day (1.9 or 3.8 g/day curcuminoids) a (AchE-Is and memantine) | 24 weeks with an open-label extension to 48 weeks | 36 ≥49 years Mild-to-moderate AD | Safety and efficacy with regard to cognition | No significant differences between curcumin and PL | No significant differences between curcumin and PL | Published |
| Hishikawa et al. [98] (Kariya, Japan) | Single cases | Turmeric 764 mg/day (curcumin 100 mg/day) (Yokukansan 2/3 subjects; donezepil 3/3) | 12 weeks | 3 79–83-84 years Progressive dementia | Effect on some symptoms of AD | Improvement in behavioral symptoms and quality of life | NR | Published |
| Cox et al. [99] (Melbourne, Australia) ACTRN12612001027808 | R, DB, PC Phase 3/Phase 4 | Longvida® Optimized Curcumin 400 mg (80 mg curcumin) | 4 weeks | 60 60–85 years Healthy | Effect on cognitive function | Improvement of cognitive functions | Treatment was well tolerated | Published |
| Rainey-Smith et al. [100] (Jondalup, Australia) ACTRN12611000437965 | R, DB, PC | BCM-95®CG (Biocurcumax™) 1500 mg/day (1320 mg/day curcuminoids) | 12 months | 160 40–90 years Healthy | Prevention of cognitive decline | No changes in cognitive performance | Gastrointestinal complaints in 23 subjects | Published |
| NCT00595582 [101] Shreveport, LA, USA | Open-label NR | Curcumin 5.4 g/day (bioperine) | 24 months | 10 55–85 years MCI or mild AD | Effect on MCI or mild AD | None patient terminated the study | Two patients showed dyspepsia | Terminated |
| NCT01001637 [102] (Mumbai, Maharashtra, India) | R, DB, PC Phase 2 | Longvida® 4 or 6 g/day | 2 months | 26 50–80 years Probable AD | Safety and effect on AD | ------- | ------- | Unknown |
| NCT01383161 [103] (Los Angeles, CA, USA) | R, DB, PC Phase 2 | Theracurmin™ 2.79 g/day (180 mg/day curcumin) | 18 months | 132 50–90 years MCI | Effect on age-related cognitive impairment | ------- | ------- | Active, not recruiting |
| NCT01811381 [104] (Los Angeles, CA, USA) | R, DB, PC Phase 2 | Longvida Curcumin® (800 mg/day of curcumin) | 12 months | 80 55–90 years MCI | Effect of curcumin alone or combined with yoga on AD | ------- | ------- | Recruiting |
| ACTRN12616000484448 [105] (Hawthorn, Australia) | R, DB, PC Phase 3/Phase 4 | Longvida® Optimized Curcumin 400 mg/day (80–90 mg curcumin) | 12 weeks | 80 50–85 years Healthy | Effects on cognition, mood and well-being | ------- | ------- | Not yet recruiting |
| ACTRN12613000681752 [106] (NSW, Australia) | R, DB, PC Phase 2 | Curcumin (Biocurcumax™): from 500 mg/day then 1 g/day then 1.5 g/day onwards | 12 months | 100 65–90 years Healthy but at high risk of AD | Prevention of AD | ------- | ------- | Recruiting |
| ACTRN12614001024639 [107] (sub study of ACTRN12613000681752) [106] (NSW, Australia) | R, B, PC Phase 2 | Curcumin 1.5 g/day | 3–6 months | 48 65–90 years Healthy and MCI | Influence on the expression of inflammatory genetic markers | ------- | ------- | Not yet recruiting |
| ACTRN12613000367741 [108] (Nedlands, Australia) | Open study, not randomized Phase 2 | Curcumin 20 gm/day (Vitamin E 500 IU/day) | 7 days | 40 ≥50 years AD, MCI, and healthy | Earlier detection of AD | ------- | ------- | Not yet recruiting |
| ACTRN12615000465550 [109] (Nedlands, Australia) | Open study, not randomised, unblended Phase 2/Phase 3 | Longvida® 20 g/day (4 g/day curcumin) (Vitamin E 500 IU/day for 8 days) | 7 days | 100 ≥50 years Healthy and MCI | Earlier detection of AD | ------- | ------- | Recruiting |
| ACTRN12615000677505 [110] (Nedlands, Australia) | Open study, not randomised, Phase 2 | Longvida® 20 g/day (containing 4 g curcumin)for 7 days (Vitamin E 500 IU/day for 8 days) | 7 days | 40 40–60 years Healthy | Earlier detection of AD | ------- | ------- | Not yet recruiting |
| Reference or ID (Location) | Study Design | Resveratrol Preparation and Dose [Other Medication] | Duration | Subjects n Age Disorder/Status | Purpose Outcome Measures | Main Results | Adverse Events | Status |
|---|---|---|---|---|---|---|---|---|
| Kennedy et al. [111] (Newcastle upon Tyne, UK) | R, DB, PC, CO | Trans-resveratrol from Biotivia Bioceuticals (Vienna, Austria) 250 mg or 500 mg | 21 days | 24 18–25 years Healthy 9 further subjects underwent bioavailability assessment | To investigate the ability to modulate mental function and increase cerebral blood flow | Cognitive function not affected. Increase in cerebral flow | Not assessed | Published |
| Wong et al. [112] (Adelaide, Australia) ACTRN12611000060943 | R, DB, PC, CO | Resvida (resveratrol 75 mg/day) | 12 weeks | 28 45–70 years Obese but otherwise healthy | Effects of resveratrol on circulatory function and cognitive performance in obese adults | Increase of circulatory function. No effects on blood pressure, arterial compliance, and cognitive function | Resveratrol appears safe and well tolerated | Published |
| Witte et al. [113] (Berlin, Germany) | R, DB, PC, | Resveratrol 200 mg/day in a formula with quercetin | 26 weeks | 46 50–80 years Healthy overweight | To investigate the ability to enhance cognitive performance | Significant retention of memory, significant increase of hyppocampal FC, improvement of glucose metabolism | Not assessed | Published |
| Wightman et al. [114] (Newcastle upon Tyne, UK) | R, DB, PC, CO | Trans-resveratrol 250 mg/day or trans-resveratrol 250 mg/day with 20 mg piperine | 21 days | 23 19–34 years Healthy 6 healthy men underwent bioavailability assessment | To assess if piperine affects the efficacy and bioavailability of resveratrol | Piperine henances the effect of resveratrol on cerebral blood flow but not the cognitive performance and bioavailability | Not assessed | Published |
| Turner et al. [115] (Georgetown, USA) NCT01504854 | R, DB, PC, MC Phase 2 | Resveratrol 500 mg/day with dose excalation by 500 mg increments ending with 2 g/day | 52 weeks | 119 >49 years Mild-to-moderate AD | To assess safety and efficacy | Decrease of CSF and plasma Aβ40 levels. No significant effects on cognitive score | Resveratrol appears safe and well tolerated | Published |
| Wong et al. [116] ACTRN12614000891628 (Newcastle, Australia) | R, DB, PC, CO Phase 2 | Resvida 75 mg/day, 150 mg/day, 300 mg/day | 4 weeks | 36 40–80 years Type 2 diabetes mellitus | Improvement of cerebrovascular responsiveness | Increase of cerebrovascular responsiveness | None | Published |
| NCT00743743 [117] (Milwaukee, WI, USA) | R, DB, PC Phase 3 | Longevinex brand resveratrol supplement (resveratrol 215 mg/day) | 52 weeks | 50 50–90 years Mild-to-moderate AD on standard therapy | Effects on cognitive and global functioning | ------- | ------- | Withdrawn prior to enrollment |
| NCT00678431 [118] (Bronx, NY, USA) | R, DB, PC Phase 3 | Resveratrol with glucose and malate | 12 months | 27 50–90 years Mild-to-moderate AD | To assess the ability to slow the progression of AD | Not available | Not available | Completed in June 2011 |
| NCT01126229 [119] (Gainesville, FL, USA) | R, DB, PC Phase 1 | Resveratrol 300 mg/day or 1000 mg/day | 12 weeks | 32 ≥65 years old | To assess the longer-term safety (3 months) and efficacy on age-related health conditions | Not available | Resveratrol appears safe and well tolerated [120] | Completed in December 2012 |
| NCT01794351 [121] (Newcastle upon Tyne, UK) | R, DB, PC, CO | Trans-resveratrol 500 mg in unique dose | 14 days | 50 18–35 years Healthy | To assess the potential cognitive enhancement | Not available | ------- | Completed in December 2012 |
| NCT01219244 [122] (Berlin, Germany) | R, DB, PC Phase 4 | Resveratrol or omega-3 supplementation or caloric restriction | 6 months | 330 50–80 years MCI | Effects on brain functions | ------- | ------- | Recruiting |
| NCT01766180 [123] (Lutherville, MD, USA) | R, DB, PC | ResVida (resveratrol 150 mg/day) alone or associated with Fruitflow a-II 150 mg/day | 3 months | 80 50–80 years Subjects with memory impairment | Efficacy in treating memory problems | ------- | ------- | Recruiting |
| NCT02621554 [124] (Leipzig, Germany) | R, DB, PC Phase 2/Phase 3 | Resveratrol (dose not reported) | 12 months | 60 ≥50 years Healthy or with subjective memory complaints | Effects on memory and on brain structures and functions | ------- | ------- | Recruiting |
| NCT02502253 [125] (Baltimore, MD, USA) | R, DB Phase 1 | Bioactive Dietary Polyphenol Preparation (BDPP) at low, moderate and high dose | 4 months | 48 55–85 years MCI | Safety and efficacy in treating mild cognitive impairment and prediabetes | ------- | ------- | Recruiting |
| ACTRN12611001288910 [126] (Hawthorn, Australia) | R, DB, PC, CO Phase 1/Phase 2 | 100mg of grape derived resveratrol in 100ml red wine | 8 days (washout 7 days) | 20 ≥65years Healthy | To assess the effect of resveratrol in red wine on cognitive function in older adults | ------- | ------- | Recruitment completed |
© 2016 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license ( http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mazzanti, G.; Di Giacomo, S. Curcumin and Resveratrol in the Management of Cognitive Disorders: What is the Clinical Evidence? Molecules 2016, 21, 1243. https://doi.org/10.3390/molecules21091243
Mazzanti G, Di Giacomo S. Curcumin and Resveratrol in the Management of Cognitive Disorders: What is the Clinical Evidence? Molecules. 2016; 21(9):1243. https://doi.org/10.3390/molecules21091243
Chicago/Turabian StyleMazzanti, Gabriela, and Silvia Di Giacomo. 2016. "Curcumin and Resveratrol in the Management of Cognitive Disorders: What is the Clinical Evidence?" Molecules 21, no. 9: 1243. https://doi.org/10.3390/molecules21091243
APA StyleMazzanti, G., & Di Giacomo, S. (2016). Curcumin and Resveratrol in the Management of Cognitive Disorders: What is the Clinical Evidence? Molecules, 21(9), 1243. https://doi.org/10.3390/molecules21091243





