Memantine Prevents the WIN 55,212-2 Evoked Cross-Priming of Ethanol-Induced Conditioned Place Preference (CPP)
Abstract
1. Introduction
2. Results
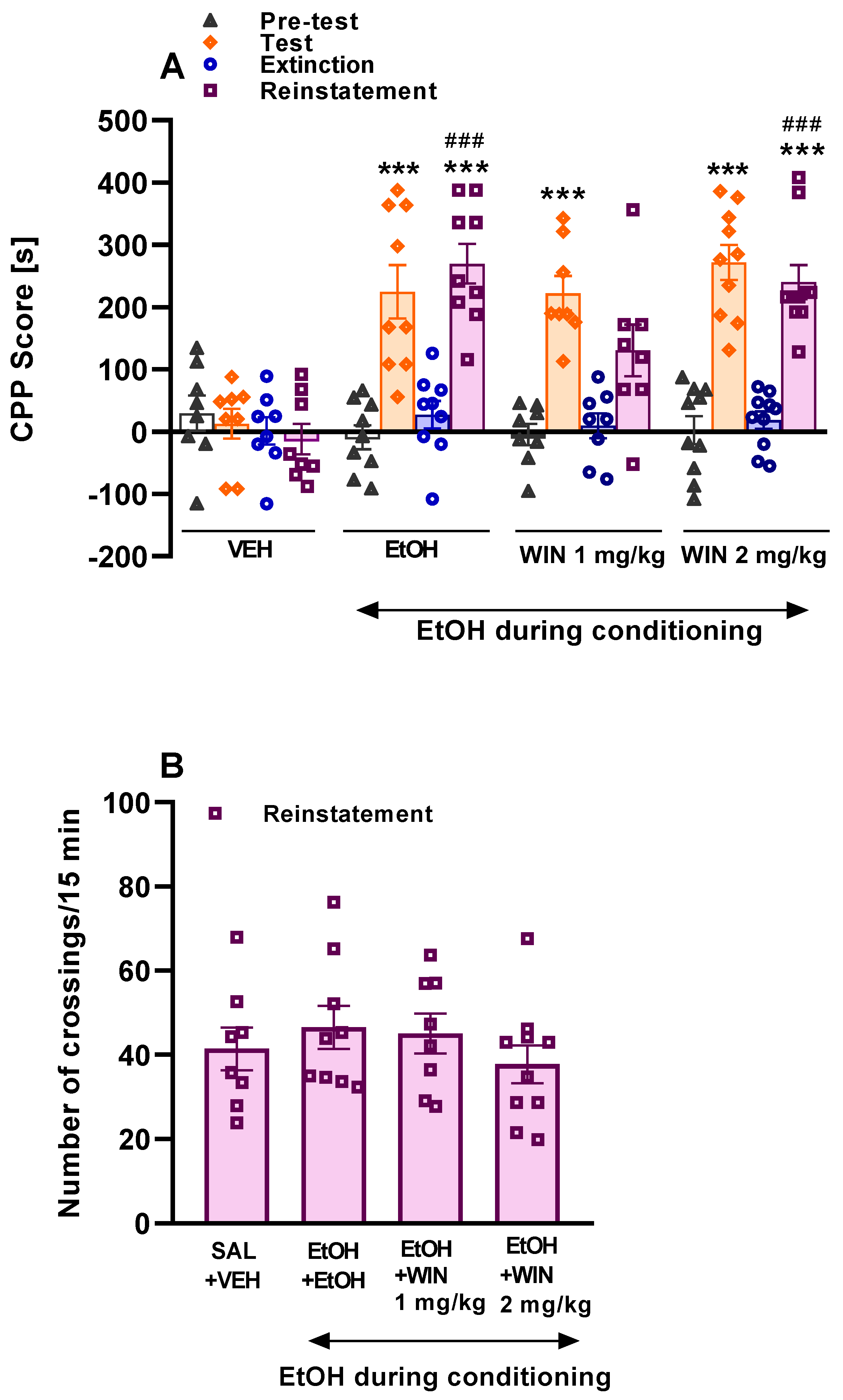
2.1. The Effect of Ethanol and WIN 55,212-2 on the Reinstatement of Ethanol-CPP
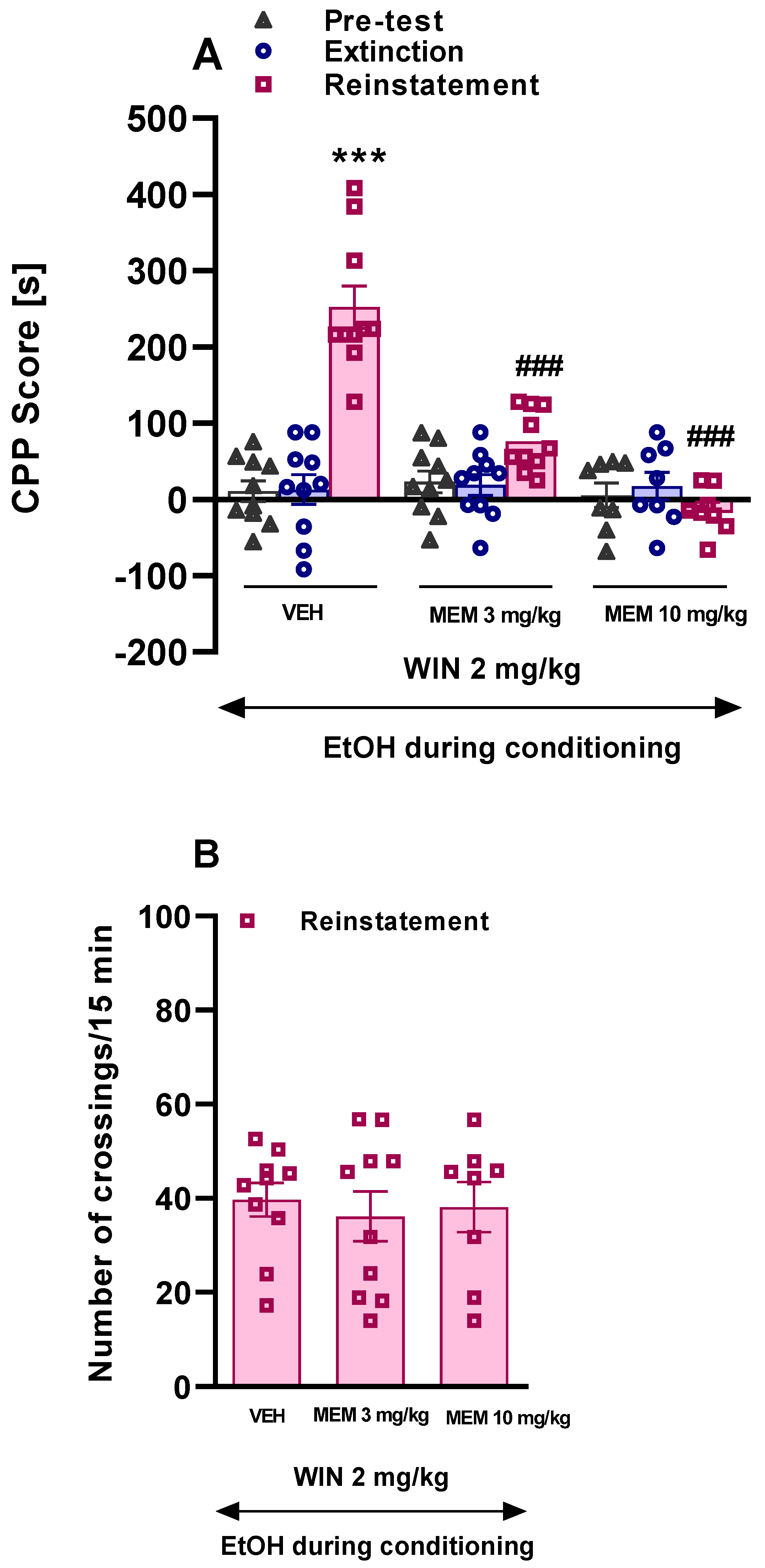
2.2. The Influence of Memantine on the Effect of WIN 55,212-2 on the Reinstatement of Ethanol CPP
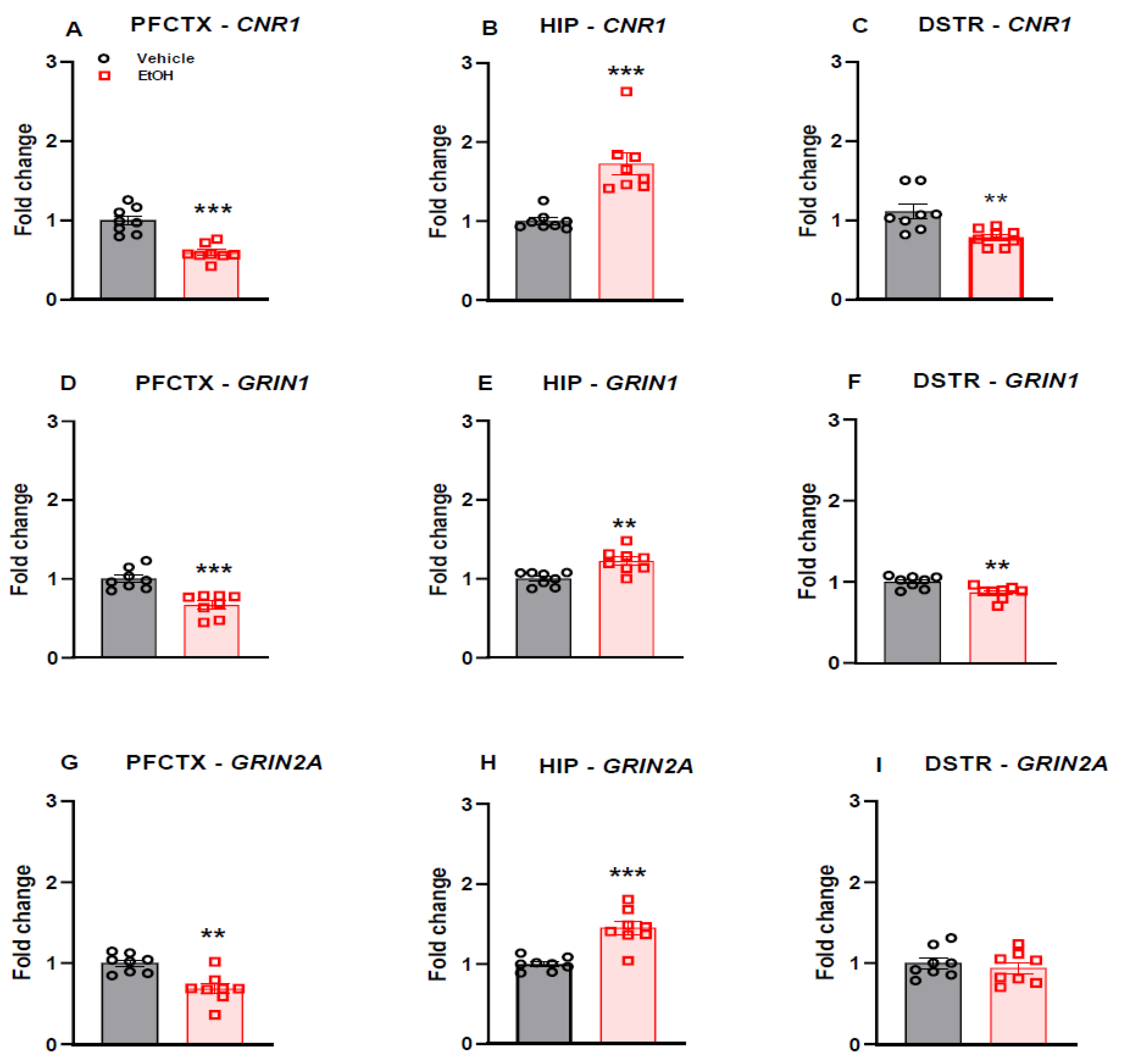
2.3. CNR1 Gene Expression
2.4. NMDA Receptor Subunit Gene Expression
3. Discussion
4. Materials and Methods
4.1. Animals
4.2. Drugs
4.3. CPP Apparatus
4.4. CPP Procedure
4.4.1. The Effect of Ethanol and WIN 55,212-2 on the Reinstatement of Ethanol CPP
4.4.2. The Influence of Memantine Pretreatment on the Effect of WIN 55,212-2 on the Reinstatement of Ethanol CPP
4.4.3. The Effect of WIN 55,212-2 and Memantine on Locomotor Activity
4.5. Molecular Analyses
4.5.1. RNA Isolation
4.5.2. RT-qPCR Analyses
4.6. Statistical Analysis
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hunt, W.A.; Majchrowicz, E.; Dalton, T.K. Alterations in High-Affinity Choline Uptake in Brain After Acute and Chronic Ethanol Treatment. J. Pharmacol. Exp. Ther. 1979, 210, 259–263. [Google Scholar]
- O’Brien, C.P. A Range of Research-Based Pharmacotherapies for Addiction. Sci. 1997, 278, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Brigham, J.; Henningfield, J.E.; Stitzer, M.L. Smoking Relapse: A Review. Int. J. Addict. 1991, 25 (Suppl. 9), 1239–1255. [Google Scholar] [CrossRef] [PubMed]
- Kassel, J.D.; Stroud, L.R.; Paronis, C.A. Smoking, Stress, and Negative Affect: Correlation, Causation, and Context across Stages of Smoking. Psychol. Bull. 2003, 129, 270–304. [Google Scholar] [CrossRef]
- Stewart, J.; de Wit, H. Reinstatement of Drug-Taking Behavior As a Method of Assessing Incentive Motivational Properties of Drugs. In Methods of Assessing the Reinforcing Properties of Abused Drugs; Springer Science and Business Media LLC: Berlin, Germany, 1987; pp. 211–227. [Google Scholar] [CrossRef]
- Peters, E.N.; Hughes, J.R. Daily Marijuana Users With past Alcohol Problems Increase Alcohol Consumption During Marijuana Abstinence. Drug Alcohol Depend. 2010, 106, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Norton, R.; Colliver, J. Prevalence and Patterns of Combined Alcohol and Marijuana Use. J. Stud. Alcohol 1988, 49, 378–380. [Google Scholar] [CrossRef]
- Reiman, A. Cannabis As a Substitute for Alcohol and Other Drugs. Harm Reduct. J. 2009, 6, 35. [Google Scholar] [CrossRef]
- Substance Abuse and Mental Health Services Administration. Treatment Episode Data Set (TEDS) National Admissions to Substance Abuse Treatment Services. Rockville, MD: Department of Health and Human Services; 1992–2002; Department of Health and Human Services: Victoria, Australia, 2004; Publication No SMA 04–3965. [Google Scholar]
- Subbaraman, M.S. Substitution and Complementarity of Alcohol and Cannabis: A Review of the Literature. Subst. Use Misuse 2016, 51, 1399–1414. [Google Scholar] [CrossRef]
- Kogan, N.M.; Mechoulam, R. The Chemistry of Endocannabinoids. J. Endocrinol. Invest. 2006, 29 (Suppl. 3), 3–14. [Google Scholar]
- Van Sickle, M.D.; Duncan, M.; Kingsley, P.J.; Mouihate, A.; Urbani, P.; Mackie, K.; Stella, N.; Makriyannis, A.; Piomelli, D.; Davison, J.S.; et al. Identification and Functional Characterization of Brainstem Cannabinoid CB2 Receptors. Science 2005, 310, 329–332. [Google Scholar] [CrossRef]
- Tsou, K.; Brown, S.; Sañudo-Peña, M.; Mackie, K.; Walker, J. Immunohistochemical Distribution of Cannabinoid CB1 Receptors in the Rat Central Nervous System. Neuroscience 1998, 83, 393–411. [Google Scholar] [CrossRef]
- Marsicano, G.; Lutz, B. Expression of the Cannabinoid Receptor CB1 in Distinct Neuronal Subpopulations in the Adult Mouse Forebrain. Eur. J. Neurosci. 1999, 11, 4213–4225. [Google Scholar] [CrossRef] [PubMed]
- López-Moreno, J.A.; González-Cuevas, G.; Moreno, G.; Navarro, M. The Pharmacology of the Endocannabinoid System: Functional and Structural Interactions With Other Neurotransmitter Systems and Their Repercussions in Behavioral Addiction. Addict. Biol. 2008, 13, 160–187. [Google Scholar] [CrossRef] [PubMed]
- Wilson, R.I. Endocannabinoid Signaling in the Brain. Science 2002, 296, 678–682. [Google Scholar] [CrossRef]
- Schlicker, E.; Kathmann, M. Modulation of Transmitter Release via Presynaptic Cannabinoid Receptors. Trends Pharmacol. Sci. 2001, 22, 565–572. [Google Scholar] [CrossRef]
- Davis, S.F.; Linn, C.L. Activation of NMDA Receptors Linked to Modulation of Voltage-Gated Ion Channels and Functional Implications. Am. J. Physiol. Physiol. 2003, 284, C757–C768. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, P.L. NMDA Receptors in Alcoholism. Int. Rev. Neurobiol. 2003, 56, 35–82. [Google Scholar] [CrossRef]
- Nagy, J. Alcohol Related Changes in Regulation of NMDA Receptor Functions. Curr. Neuropharmacol. 2008, 6, 39–54. [Google Scholar] [CrossRef]
- Nagy, J.; Kolok, S.; Boros, A.; Dezso, P. Role of Altered Structure and Function of NMDA Receptors in Development of Alcohol Dependence. Curr. Neuropharmacol. 2005, 3, 281–297. [Google Scholar] [CrossRef]
- Tzschentke, T.M.; Schmidt, W.J. Glutamatergic Mechanisms in Addiction. Mol. Psychiatry 2003, 8, 373–382. [Google Scholar] [CrossRef]
- Kretschmer, B.D. Modulation of the Mesolimbic Dopamine System by Glutamate. J. Neurochem. 2002, 73, 839–848. [Google Scholar] [CrossRef]
- Ong, W.Y.; Mackie, K. A Light and Electron Microscopic Study of the CB1 Cannabinoid Receptor in Primate Brain. Neurosci. 1999, 92, 1177–1191. [Google Scholar] [CrossRef]
- Robbe, D.; Alonso, G.; Duchamp, F.; Bockaert, J.; Manzoni, O. Localization and Mechanisms of Action of Cannabinoid Receptors at the Glutamatergic Synapses of the Mouse Nucleus Accumbens. J. Neurosci. 2001, 21, 109–116. [Google Scholar] [CrossRef] [PubMed]
- Hajos, N.; Freund, T. Pharmacological Separation of Cannabinoid Sensitive Receptors on Hippocampal Excitatory and Inhibitory Fibers. Neuropharmacology 2002, 43, 503–510. [Google Scholar] [CrossRef]
- Hoffman, A.F.; Öz, M.; Yang, R.; Lichtman, A.H.; Lupica, C.R. Opposing Actions of Chronic 9-Tetrahydrocannabinol and Cannabinoid Antagonists on Hippocampal Long-Term Potentiation. Learn. Mem. 2007, 14, 63–74. [Google Scholar] [CrossRef]
- Laaris, N.; Good, C.H.; Lupica, C.R. Δ9-Tetrahydrocannabinol Is a Full Agonist at CB1 Receptors on GABA Neuron Axon Terminals in the Hippocampus. Neuropharmacology 2010, 59, 121–127. [Google Scholar] [CrossRef] [PubMed]
- De Witte, P. Imbalance Between Neuroexcitatory and Neuroinhibitory Amino Acids Causes Craving for Ethanol. Addict. Behav. 2004, 29, 1325–1339. [Google Scholar] [CrossRef] [PubMed]
- Spanagel, R.; Rosenwasser, A.M.; Schumann, G.; Sarkar, D.K. Alcohol Consumption and the Body’s Biological Clock. Alcohol. Clin. Exp. Res. 2005, 29, 1550–1557. [Google Scholar] [CrossRef]
- Becker, J.B.; Hu, M. Sex Differences in Drug Abuse. Front. Neuroendocr. 2008, 29, 36–47. [Google Scholar] [CrossRef]
- Anthony, J.C.; Warner, L.A.; Kessler, R.C. Comparative Epidemiology of Dependence on Tobacco, Alcohol, Controlled Substances, and Inhalants: Basic Findings from the National Comorbidity Survey. Exp. Clin. Psychopharmacol. 1994, 2, 244–268. [Google Scholar] [CrossRef]
- Hitschfeld, M.J.; Schneekloth, T.D.; Ebbert, J.O.; Hall-Flavin, D.K.; Karpyak, V.; Abulseoud, O.A.; Patten, C.A.; Geske, J.R.; Frye, M.A. Female Smokers Have the Highest Alcohol Craving in a Residential Alcoholism Treatment Cohort. Drug Alcohol Depend. 2015, 150, 179–182. [Google Scholar] [CrossRef]
- Kippin, T.E.; Fuchs, R.A.; Mehta, R.H.; Case, J.M.; Parker, M.P.; Bimonte-Nelson, H.A.; See, R.E. Potentiation of Cocaine-Primed Reinstatement of Drug Seeking in Female Rats During Estrus. Psychopharmacology 2005, 182, 245–252. [Google Scholar] [CrossRef]
- Rubonis, A.V.; Colby, S.M.; Monti, P.M.; Rohsenow, D.J.; Gulliver, S.B.; Sirota, A.D. Alcohol Cue Reactivity and Mood Induction in Male and Female Alcoholics. J. Stud. Alcohol 1994, 55, 487–494. [Google Scholar] [CrossRef]
- Economidou, D.; Mattioli, L.; Cifani, C.; Perfumi, M.C.; Massi, M.; Cuomo, V.; Trabace, L.; Ciccocioppo, R. Effect of the Cannabinoid CB1 Receptor Antagonist SR-141716A on Ethanol Self-Administration and Ethanol-Seeking Behaviour in Rats. Psychopharmacology 2005, 183, 394–403. [Google Scholar] [CrossRef]
- Hansson, A.C.; Bermúdez-Silva, F.J.; Malinen, H.; Hyytiä, P.; Sanchez-Vera, I.; Rimondini, R.; De Fonseca, F.R.; Kunos, G.; Sommer, W.H.; Heilig, M. Genetic Impairment of Frontocortical Endocannabinoid Degradation and High Alcohol Preference. Neuropsychopharmacology 2006, 32, 117–126. [Google Scholar] [CrossRef]
- Hungund, B.L.; Szakall, I.; Adam, A.; Basavarajappa, B.; Vadasz, C. Cannabinoid CB1 Receptor Knockout Mice Exhibit Markedly Reduced Voluntary Alcohol Consumption and Lack Alcohol-Induced Dopamine Release in the Nucleus Accumbens. J. Neurochem. 2003, 84, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Lallemand, F.; Soubrié, P.H.; De Witte, P.H. Effects of CB1 Cannabinoid Receptor Blockade on Ethanol Preference After Chronic Ethanol Administration. Alcohol Clin. Exp. Res. 2001, 25, 1317–1323. [Google Scholar] [CrossRef] [PubMed]
- Lallemand, F.; De Witte, P. SR147778, a CB1 Cannabinoid Receptor Antagonist, Suppresses Ethanol Preference in Chronically Alcoholized Wistar Rats. Alcohol 2006, 39, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Liu, J.; Harvey-White, J.; Zimmer, A.; Kunos, G. Endocannabinoid Signaling via Cannabinoid Receptor 1 Is Involved in Ethanol Preference and Its Age-Dependent Decline in Mice. Proc. Natl. Acad. Sci. USA 2003, 100, 1393–1398. [Google Scholar] [CrossRef] [PubMed]
- Basavarajappa, B.S.; Saito, M.; Cooper, T.B.; Hungund, B.L. Chronic Ethanol Inhibits the Anandamide Transport and Increases Extracellular Anandamide Levels in Cerebellar Granule Neurons. Eur. J. Pharmacol. 2003, 466, 73–83. [Google Scholar] [CrossRef]
- Alvarez-Jaimes, L.; Stouffer, D.G.; Parsons, L.H. Chronic Ethanol Treatment Potentiates Ethanol-Induced Increases in Interstitial Nucleus Accumbens Endocannabinoid Levels in Rats. J. Neurochem. 2009, 111, 37–48. [Google Scholar] [CrossRef] [PubMed]
- Caillé, S.; Alvarez-Jaimes, L.; Polis, I.; Stouffer, D.G.; Parsons, L.H. Specific Alterations of Extracellular Endocannabinoid Levels in the Nucleus Accumbens by Ethanol, Heroin, and Cocaine Self-Administration. J. Neurosci. 2007, 27, 3695–3702. [Google Scholar] [CrossRef]
- Vinod, K.; Yalamanchili, R.; Xie, S.; Cooper, T.; Hungund, B. Effect of Chronic Ethanol Exposure and Its Withdrawal on the Endocannabinoid System. Neurochem. Int. 2006, 49, 619–625. [Google Scholar] [CrossRef]
- Serrano, A.; Rivera, P.; Pavon, F.J.; Decara, J.; Suárez, J.; de Fonseca, F.R.; Parsons, L.H. Differential Effects of Single Versus Repeated Alcohol Withdrawal on the Expression of Endocannabinoid System-Related Genes in the Rat Amygdala. Alcohol. Clin. Exp. Res. 2012, 36, 984–994. [Google Scholar] [CrossRef] [PubMed]
- Rimondini, R.; Arlinde, C.; Sommer, W.; Heilig, M. Long-lasting Increase in Voluntary Ethanol Consumption and Transcriptional Regulation in the Rat Brain After Intermittent Exposure to Alcohol. FASEB J. 2002, 16, 27–35. [Google Scholar] [CrossRef]
- Mitrirattanakul, S.; Lopez-Valdes, H.E.; Liang, J.; Matsuka, Y.; Mackie, K.; Faull, K.F.; Spigelman, I. Bidirectional Alterations of Hippocampal Cannabinoid 1 Receptors and Their Endogenous Ligands in a Rat Model of Alcohol Withdrawal and Dependence. Alcohol. Clin. Exp. Res. 2007, 31, 855–867. [Google Scholar] [CrossRef]
- Ceccarini, J.; Casteels, C.; Koole, M.; Bormans, G.; Van Laere, K. Transient Changes in the Endocannabinoid System After Acute and Chronic Ethanol Exposure and Abstinence in the Rat: A Combined PET and Microdialysis Study. Eur. J. Nucl. Med. Mol. Imaging 2013, 40, 1582–1594. [Google Scholar] [CrossRef] [PubMed]
- Coelhoso, C.C.; Engelke, D.S.; Filev, R.; Silveira, D.X.; Mello, L.E.; Junior, J.G.D.S. Temporal and Behavioral Variability in Cannabinoid Receptor Expression in Outbred Mice Submitted to Ethanol-Induced Locomotor Sensitization Paradigm. Alcohol. Clin. Exp. Res. 2013, 37, 1516–1526. [Google Scholar] [CrossRef] [PubMed]
- Gremel, C.M.; Cunningham, C.L. Involvement of Amygdala Dopamine and Nucleus Accumbens NMDA Receptors in Ethanol-Seeking Behavior in Mice. Neuropsychopharmacology 2008, 34, 1443–1453. [Google Scholar] [CrossRef] [PubMed]
- Hyman, S.E.; Malenka, R.C. Addiction and the Brain: The Neurobiology of Compulsion and Its Persistence. Nat. Rev. Neurosci. 2001, 2, 695–703. [Google Scholar] [CrossRef] [PubMed]
- Kauer, J.A. Learning Mechanisms in Addiction: Synaptic Plasticity in the Ventral Tegmental Area As a Result of Exposure to Drugs of Abuse. Annu. Rev. Physiol. 2004, 66, 447–475. [Google Scholar] [CrossRef] [PubMed]
- Gremel, C.M.; Cunningham, C.L. Roles of the Nucleus Accumbens and Amygdala in the Acquisition and Expression of Ethanol-Conditioned Behavior in Mice. J. Neurosci. 2008, 28, 1076–1084. [Google Scholar] [CrossRef] [PubMed]
- Fattore, L.; Fadda, P.; Spano, M.S.; Pistis, M.; Fratta, W. Neurobiological Mechanisms of Cannabinoid Addiction. Mol. Cell En-Docrinol. 2008, 286, S97–S107. [Google Scholar] [CrossRef] [PubMed][Green Version]
- McCool, B.A.; Christian, D.T.; Diaz, M.; Läck, A.K. Glutamate Plasticity in the Drunken Amygdala. Int. Rev. Neurobiol. 2010, 91, 205–233. [Google Scholar] [CrossRef] [PubMed]
- Koob, G.F.; Le Moal, M. Neurobiological Mechanisms for Opponent Motivational Processes in Addiction. Philos. Trans. R. Soc. B Biol. Sci. 2008, 363, 3113–3123. [Google Scholar] [CrossRef]
- Houchi, H.; Babovic, D.; Pierrefiche, O.; Ledent, C.; Daoust, M.; Naassila, M. CB1 Receptor Knockout Mice Display Reduced Ethanol-Induced Conditioned Place Preference and Increased Striatal Dopamine D2 Receptors. Neuropsychopharmacology 2004, 30, 339–349. [Google Scholar] [CrossRef]
- Katona, I.; Rancz, E.A.; Acsády, L.; Ledent, C.; Mackie, K.; Hajos, N.; Freund, T.F. Distribution of CB1 Cannabinoid Receptors in the Amygdala and Their Role in the Control of GABAergic Transmission. J. Neurosci. 2001, 21, 9506–9518. [Google Scholar] [CrossRef]
- Roberts, A.J.; Heyser, C.J.; Cole, M.; Griffin, P.; Koob, G.F. Excessive Ethanol Drinking Following a History of Dependence Animal Model of Allostasis. Neuropsychopharmacology 2000, 22, 581–594. [Google Scholar] [CrossRef]
- Palazzo, E.; Marabese, I.; De Novellis, V.; Oliva, P.; Rossi, F.; Berrino, L.; Maione, S. Metabotropic and NMDA Glutamate Receptors Participate in the Cannabinoid-Induced Antinociception. Neuropharmacology 2001, 40, 319–326. [Google Scholar] [CrossRef]
- Sánchez-Blázquez, P.; Rodriguez-Muñoz, M.; Vicente-Sánchez, A.; Garzón, J. Cannabinoid Receptors Couple to NMDA Receptors to Reduce the Production of NO and the Mobilization of Zinc Induced by Glutamate. Antioxidants Redox Signal. 2013, 19, 1766–1782. [Google Scholar] [CrossRef]
- Thorat, S.N.; Bhargava, H.N. Effects of NMDA Receptor Blockade and Nitric Oxide Synthase Inhibition on the Acute and Chronic Actions of Δ9-Tetrahydrocannabinol in Mice. Brain Res. 1994, 667, 77–82. [Google Scholar] [CrossRef]
- Derkinderen, P.; Valjent, E.; Toutant, M.; Corvol, J.-C.; Enslen, H.; Ledent, C.; Trzaskos, J.; Caboche, J.; Girault, J.-A. Regulation of Extracellular Signal-Regulated Kinase by Cannabinoids in Hippocampus. J. Neurosci. 2003, 23, 2371–2382. [Google Scholar] [CrossRef] [PubMed]
- Marsicano, G.; Goodenough, S.; Monory, K.; Hermann, H.; Eder, M.; Cannich, A.; Azad, S.C.; Cascio, M.G.; Ortega-Gutiérrez, S.; Van Der Stelt, M.; et al. CB1 Cannabinoid Receptors and On-Demand Defense Against Excitotoxicity. Science 2003, 302, 84–88. [Google Scholar] [CrossRef]
- Liu, Q.; Bhat, M.; Bowen, W.D.; Cheng, J. Signaling Pathways from Cannabinoid Receptor-1 Activation to Inhibition of N-Methyl-D-Aspartic Acid Mediated Calcium Influx and Neurotoxicity in Dorsal Root Ganglion Neurons. J. Pharmacol. Exp. Ther. 2009, 331, 1062–1070. [Google Scholar] [CrossRef] [PubMed]
- Brown, T.M.; Brotchie, J.M.; Fitzjohn, S.M. Cannabinoids Decrease Corticostriatal Synaptic Transmission via an Effect on Glutamate Uptake. J. Neurosci. 2003, 23, 11073–11077. [Google Scholar] [CrossRef]
- Melis, M. Endocannabinoids Mediate Presynaptic Inhibition of Glutamatergic Transmission in Rat Ventral Tegmental Area Dopamine Neurons through Activation of CB1 Receptors. J. Neurosci. 2004, 24, 53–62. [Google Scholar] [CrossRef]
- Li, Q.; Yan, H.; Wilson, W.A.; Swartzwelder, H.S. Modulation of NMDA and AMPA-Mediated Synaptic Transmission by CB1 Receptors in Frontal Cortical Pyramidal Cells. Brain Res. 2010, 1342, 127–137. [Google Scholar] [CrossRef]
- Hampson, R.; Miller, F.; Palchik, G.; Deadwyler, S.A. Cannabinoid Receptor Activation Modifies NMDA Receptor Mediated Release of Intracellular Calcium: Implications for Endocannabinoid Control of Hippocampal Neural Plasticity. Neuropharmacology 2011, 60, 944–952. [Google Scholar] [CrossRef] [PubMed]
- Kashiwagi, K.; Masuko, T.; Nguyen, C.D.; Kuno, T.; Tanaka, I.; Igarashi, K.; Williams, K. Channel Blockers Acting AtN-Methyl-D-Aspartate Receptors: Differential Effects of Mutations in the Vestibule and Ion Channel Pore. Mol. Pharmacol. 2002, 61, 533–545. [Google Scholar] [CrossRef]
- Alén, F.; Santos, A.; Moreno-Sanz, G.; González-Cuevas, G.; Giné, E.; Franco-Ruiz, L.; Navarro, M.; López-Moreno, J.A. Canna-Binoid-Induced Increase in Relapse-Like Drinking Is Prevented by the Blockade of the Glycine-Binding Site of N-Methyl-D-Aspartate Receptors. Neuroscience 2009, 158, 465–473. [Google Scholar] [CrossRef]
- Haspula, D.; Clark, M.A. Cannabinoid Receptors: An Update on Cell Signaling, Pathophysiological Roles and Therapeutic Opportunities in Neurological, Cardiovascular, and Inflammatory Diseases. Int. J. Mol. Sci. 2020, 21, 7693. [Google Scholar] [CrossRef]
- Marszalek-Grabska, M.; Gawel, K.; Matosiuk, D.; Gibula-Tarlowska, E.; Listos, J.; Kotlinska, J.H. Effects of the Positive Allosteric Modulator of Metabotropic Glutamate Receptor 5, VU-29, on Maintenance Association Between Environmental Cues and Rewarding Properties of Ethanol in Rats. Biomolecules 2020, 10, 793. [Google Scholar] [CrossRef] [PubMed]
- Gibula-Tarlowska, E.; Grochecki, P.; Silberring, J.; Kotlinska, J.H. The Kisspeptin Derivative Kissorphin Reduces the Acquisition, Expression, and Reinstatement of Ethanol-Induced Conditioned Place Preference in Rats. Alcohol 2019, 81, 11–19. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marszalek-Grabska, M.; Smaga, I.; Surowka, P.; Grochecki, P.; Slowik, T.; Filip, M.; Kotlinska, J.H. Memantine Prevents the WIN 55,212-2 Evoked Cross-Priming of Ethanol-Induced Conditioned Place Preference (CPP). Int. J. Mol. Sci. 2021, 22, 7940. https://doi.org/10.3390/ijms22157940
Marszalek-Grabska M, Smaga I, Surowka P, Grochecki P, Slowik T, Filip M, Kotlinska JH. Memantine Prevents the WIN 55,212-2 Evoked Cross-Priming of Ethanol-Induced Conditioned Place Preference (CPP). International Journal of Molecular Sciences. 2021; 22(15):7940. https://doi.org/10.3390/ijms22157940
Chicago/Turabian StyleMarszalek-Grabska, Marta, Irena Smaga, Paulina Surowka, Pawel Grochecki, Tymoteusz Slowik, Malgorzata Filip, and Jolanta H. Kotlinska. 2021. "Memantine Prevents the WIN 55,212-2 Evoked Cross-Priming of Ethanol-Induced Conditioned Place Preference (CPP)" International Journal of Molecular Sciences 22, no. 15: 7940. https://doi.org/10.3390/ijms22157940
APA StyleMarszalek-Grabska, M., Smaga, I., Surowka, P., Grochecki, P., Slowik, T., Filip, M., & Kotlinska, J. H. (2021). Memantine Prevents the WIN 55,212-2 Evoked Cross-Priming of Ethanol-Induced Conditioned Place Preference (CPP). International Journal of Molecular Sciences, 22(15), 7940. https://doi.org/10.3390/ijms22157940







