Food Consumption Pattern and the Intake of Sugar, Salt, and Fat in the South Jakarta City—Indonesia
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. Estimation of Added Sugar, Salt, and Fat Intake
2.3.1. Estimation of Added Sugar Intake
2.3.2. Estimation of Salt Intake
2.3.3. Estimation of Fat Intake
2.4. Data Analysis
3. Results and Discussion
3.1. Subjects Characteristics
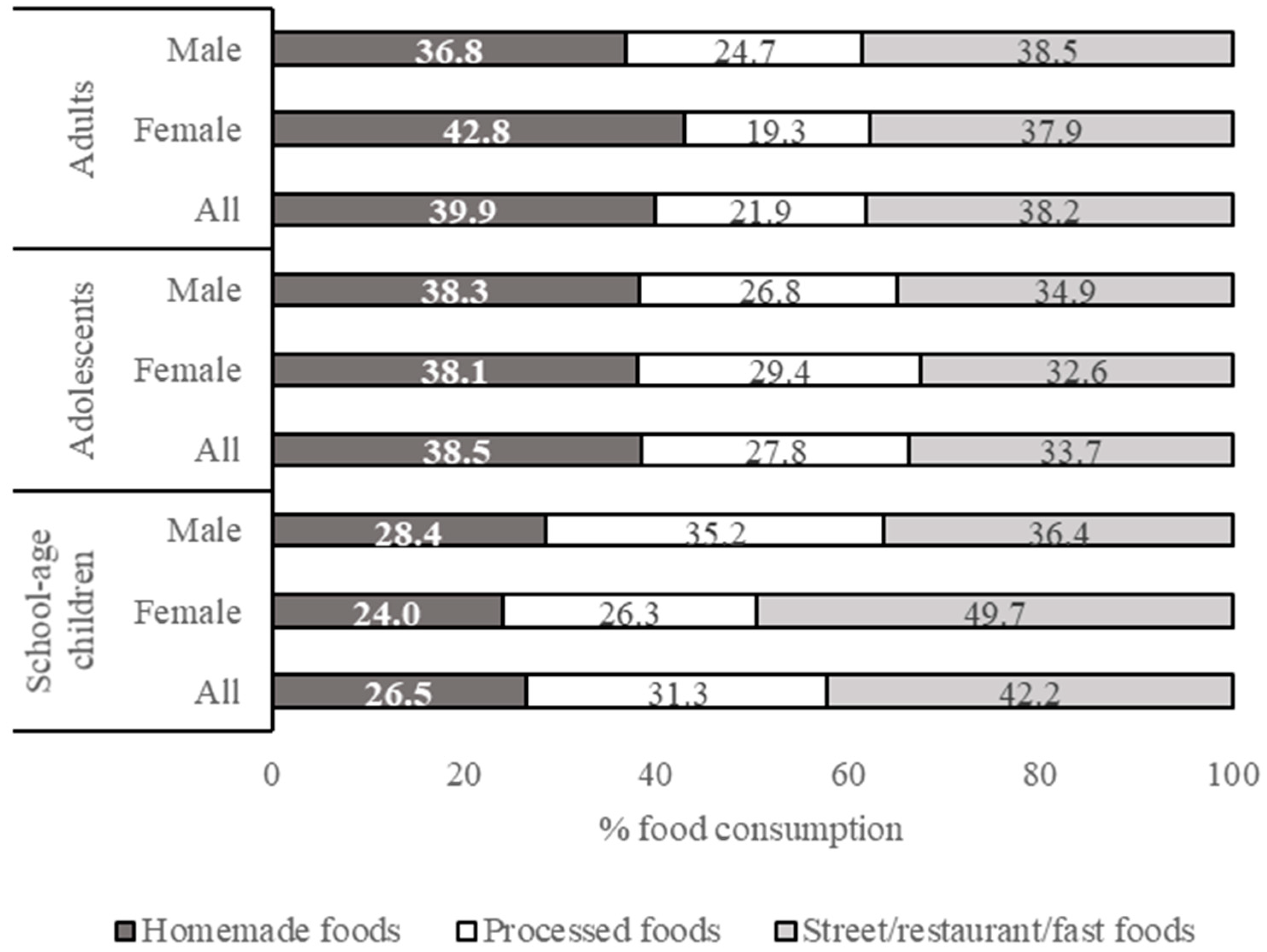
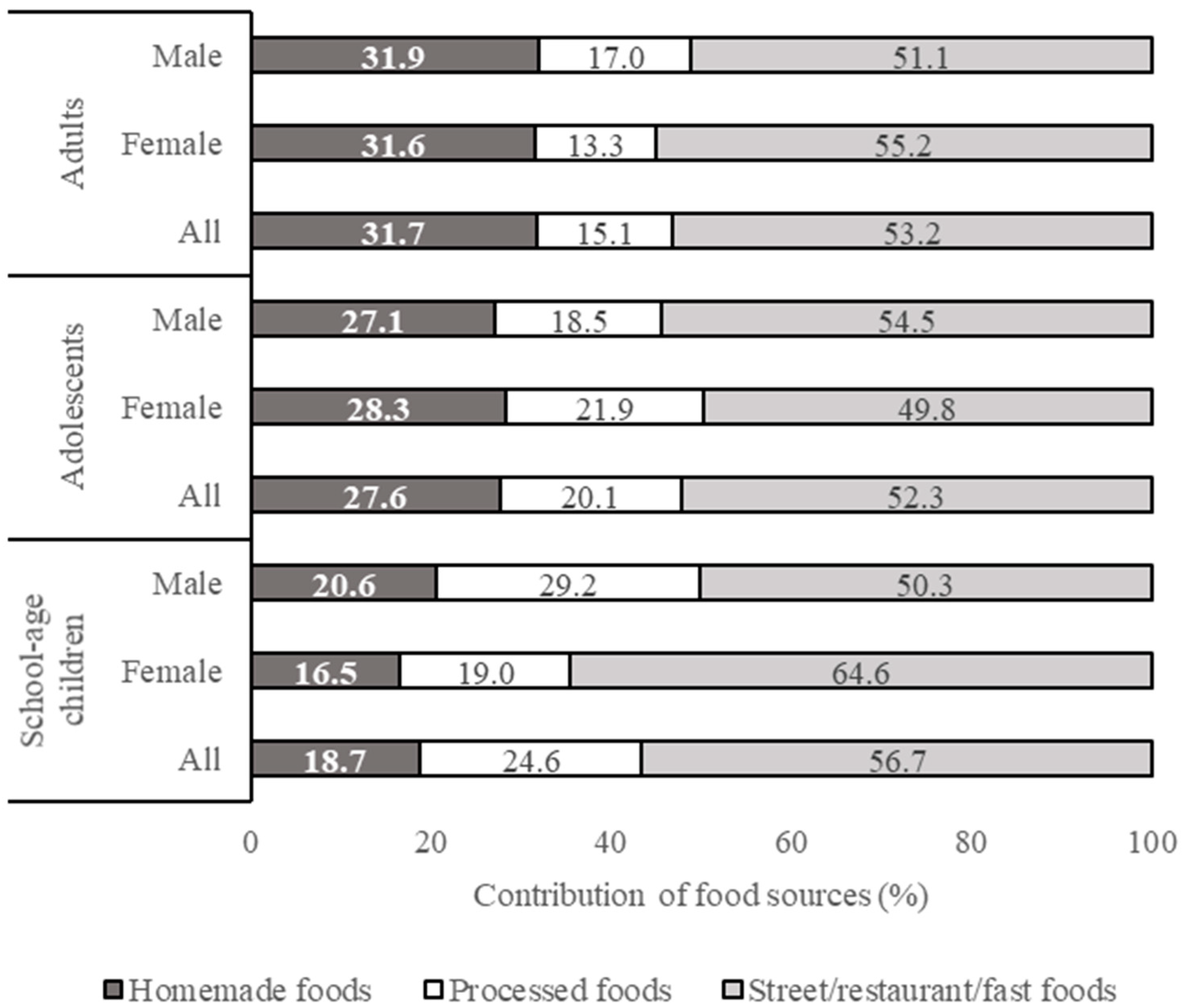
3.2. Food Consumption Pattern
3.3. Total Daily Intake of Sugar, Salt, and Fat
3.3.1. Added Sugar Intake
3.3.2. Salt Intake
3.3.3. Fat Intake
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Noncommunicable Diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 22 January 2021).
- Balitbangkes Kemenkes RI. Badan Penelitian dan Pengembangan Kesehatan; Riset Kesehatan Dasar (Kemenkes): Jakarta, Indonesia, 2007.
- Balitbangkes Kemenkes RI. Badan Penelitian dan Pengembangan Kesehatan; Riset Kesehatan Dasar (Kemenkes): Jakarta, Indonesia, 2013.
- Balitbangkes Kemenkes RI. Badan Penelitian dan Pengembangan Kesehatan; Riset Kesehatan Dasar (Kemenkes): Jakarta, Indonesia, 2018.
- Indonesian Ministry of Health. Penyakit Tidak Menular Kini Ancam Usia Muda. Available online: https://www.kemkes.go.id/article/view/20070400003/penyakit-tidak-menular-kini-ancam-usia-muda.html (accessed on 1 October 2020).
- Pervin, R.; Hossain, M.A.; Debnath, D.; Nath, B.D. Epidemiological perspectives of dietary sugars, salts and fats. In Dietary Sugar, Salt and Fat in Human Health; Preuss, H.G., Bagchi, D., Eds.; Academic Press: Cambridge, UK, 2020; pp. 3–23. [Google Scholar]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
- Hatma, R.D.; Lukito, W.; Rumawas, Y.S.P. Fatty acids intake among diverse ethnic groups in Indonesia. Med. J. Indones. 2005, 14, 242–248. [Google Scholar] [CrossRef][Green Version]
- Mustafa, A.; Muslimatun, S.; Untoro, J.; Lan, M.C.P.J.; Kristianto, Y. Determination of discretionary salt intake in an iodine deficient area of East Java-Indonesia using three different methods. Asia Pac. J. Clin. Nutr. 2006, 15, 362–367. [Google Scholar]
- Atmarita, A.; Jahari, A.B.; Sudikno, S.; Soekatri, M. Asupan gula, garam, dan lemak di Indonesia: Analisis survei konsumsi makanan individu (SKMI) 2014. Gizi Indones. 2017, 39, 1. [Google Scholar] [CrossRef]
- Atmarita, A.; Imanningsih, N.; Jahari, A.B.; Permaesih, I.D.; Chan, P.; Amarra, M.S. Consumption and sources of added sugar in Indonesia: A review. Asia Pac. J. Clin. Nutr. 2018, 27, 47–64. [Google Scholar] [PubMed]
- Daya, M.; Pujianto, D.A.; Witjaksono, F.; Priliani, L.; Susanto, J.; Lukito, W.; Malik, S.G. Obesity risk and preference for high dietary fat intake are determined by FTO rs9939609 gene polymorphism in selected Indonesian adults. Asia Pac. J. Clin. Nutr. 2019, 28, 183–191. [Google Scholar]
- Triandhini, R.L.N.K.R.; Rahardjo, M.; Putranti, M. Sugar, salt and fat consumption of population in Batur Kidul Village Getasan Subdistrict Semarang Regency Gambaran. J. Health 2018, 5, 1–11. [Google Scholar] [CrossRef][Green Version]
- Anisyah, A.; Andarwulan, N.; Hariyadi, P. Tartrazine exposure assessment by using food frequency method in North Jakarta, Indonesia. Food Nutr. Sci. 2011, 2, 458–463. [Google Scholar]
- Torheim, L.E.; Barikmo, I.; Hatløy, A.; Diakité, M.; Solvoll, K.; Diarra, M.M.; Oshaug, A. Validation of a quantitative food-frequency questionnaire for use in Western Mali. Public Health Nutr. 2001, 4, 1267–1277. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Parr, C.L.; Barikmo, I.; Torheim, L.E.; Ouattara, F.; Kaloga, A.; Oshaug, A. Validation of the second version of a quantitative food-frequency questionnaire for use in Western Mali. Public Health Nutr. 2002, 5, 769–781. [Google Scholar] [CrossRef] [PubMed]
- Torheim, L.E.; Barikmo, I.; Parr, C.L.; Hatløy, A.; Ouattara, F.; Oshaug, A. Validation of food variety as an indicator of diet quality assessed with a food frequency questionnaire for Western Mali. Eur. J. Clin. Nutr. 2003, 57, 1283–1291. [Google Scholar] [CrossRef] [PubMed]
- Food and Agriculture Organization. Dietary Assessment: A Resource Guide to Method Selection and Application in Low Resource Settings; Food and Agriculture Organization: Rome, Italy, 2018. [Google Scholar]
- Persatuan Ahli Gizi Indonesia (PERSAGI). Food Composition Table-Indonesia (Daftar Komposisi Bahan Makanan); Direktorat Gizi Departemen Kesehatan R.I. Penerbit Bhratara: Djakarta, Indonesia, 2005. [Google Scholar]
- Nutrient Data Laboratory, Agricultural Research Service, US Department of Agriculture (USDA). National Nutrient Database for Standard Reference; US Department of Agriculture: Washington, DC, USA, 2015.
- Singapore: Nutrition Unit. Ministry of Health. Food Composition Table of Foods Commonly Used in Singapore; Ministry of Health: Singapore, 1977.
- Pomeranz, Y.; Meloan, C.E. Food Analysis Theory and Practice; Aspen Publishers Inc.: Gaithersburg, MD, USA, 2000. [Google Scholar]
- AOAC International. Official Methods of Analysis, 18th ed.; AOAC International: Gaithersburg, MD, USA, 2005. [Google Scholar]
- World Health Organization. Body Mass Index. Available online: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi (accessed on 1 October 2020).
- World Health Organization. Waist Circumference and Waist–Hip Ratio. Report of a WHO Expert Consultation; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- American Heart Association (AHA). High Blood Pressure. Available online: https://www.heart.org/en/health-topics/high-blood-pressure (accessed on 1 October 2020).
- de Onis, M.; Onyango, A.W.; Borghi, A.W.; Siyam, A.; Nishidaa, C.; Siekmann, J. Development of a WHO growth reference for school-aged children and adolescents. Bull. World Health Organ. 2007, 85, 660–667. [Google Scholar] [CrossRef] [PubMed]
- National Cancer Institute. Usual Dietary Intakes: U.S. Population, 2007–2010; National Cancer Institute: Bethesda, MD, USA, 2019.
- Fisberg, M.; Kovalskys, I.; Gómez, G.; Rigotti, A.; Sanabria, L.Y.C.; García, M.C.Y.; Torres, R.G.P.; Herrera-Cuenca, M.; Zimberg, I.Z.; Koletzko, B.; et al. Total and added sugar intake: Assessment in eight Latin American countries. Nutrients 2018, 10, 389. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline: Sugars Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Johnson, R.K.; Appel, L.J.; Brands, M.; Howard, B.V.; Lefevre, M.; Lustig, R.H.; Sacks, F.; Steffen, L.M.; Wylie-Rosett, J. Dietary sugars intake and cardiovascular health a scientific statement from the american heart association. Circulation 2009, 120, 1011–1020. [Google Scholar] [CrossRef] [PubMed]
- Thout, S.R.; Santos, J.A.; McKenzie, B.; Trieu, K.; Johnson, C.; McLean, R.; Arcand, J.A.; Campbell, N.R.C.; Webster, J. The Science of Salt: Updating the evidence on global estimates of salt intake. J. Clin. Hypertens. 2019, 21, 710–721. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guideline: Sodium Intake for Adults and Children; World Health Organization: Geneva, Switzerland, 2012. [Google Scholar]
- He, F.J.; MacGregor, G.A. Reducing population salt intake worldwide: From evidence to implementation. Prog. Cardiovasc. Dis. 2010, 52, 363–382. [Google Scholar] [CrossRef] [PubMed]
- Elliott, P.; Brown, I. Sodium Intakes around the World; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- World Health Organization. Interim Summary of Conclusions and Dietary Recommendations on Total Fat & Fatty Acids; World Health Organization: Geneva, Switzerland, 2008. [Google Scholar]
- Harika, R.K.; Eilander, A.; Alssema, M.; Osendarp, S.J.M.; Zock, P.L. Intake of fatty acids in general populations worldwide does not meet dietary recommendations to prevent coronary heart disease: A systematic review of data from 40 countries. Ann. Nutr. Metab. 2013, 63, 229–238. [Google Scholar] [CrossRef] [PubMed]
- Micha, R.; Khatibzadeh, S.; Shi, P.; Fahimi, S.; Lim, S.; Andrews, K.G.; Engell, R.E.; Powles, J.; Ezzati, M.; Mozaffarian, D. Global, regional, and national consumption levels of dietary fats and oils in 1990 and 2010: A systematic analysis including 266 country-specific nutrition surveys. BMJ 2014, 348, 1–20. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Healthy Diets. Available online: https://www.who.int/news-room/fact-sheets/detail/healthy-diet (accessed on 1 October 2020).


| Subject | Male | Female | Total |
|---|---|---|---|
| School-age children (6–12 years) | 59 | 52 | 111 |
| Adolescents (13–18 years) | 51 | 56 | 107 |
| Adults (≥19 years) | 47 | 58 | 105 |
| Total | 157 | 166 | 323 |
| Characteristic | Male | Female | All |
|---|---|---|---|
| Nutritional status (BMI) 1 | |||
| Underweight (<18.5), in % | 8.5 | 3.4 | 5.7 |
| Normal weight (18.5–24.9), in % | 42.6 | 53.4 | 48.6 |
| Overweight (25–29.9), in % | 42.6 | 31 | 36.2 |
| Obesity (>30), in % | 6.4 | 12.1 | 9.5 |
| Average BMI, mean ± SD in kg/m2 | 24.2 ± 4.3 | 24.9 ± 4.3 | 24.6 ± 4.3 |
| Min. to max. value of BMI in kg/m2 | 15.3–34.5 | 11.6–33.8 | 11.6–34.5 |
| Status of waist to hip ratio (WHR) 2 | |||
| Normal (<0.95 for male, <0.8 for female), in % | 29.8 | 34.5 | 32.4 |
| Risk (≥0.95 for male, ≥0.8 for female), in % | 70.2 | 65.5 | 67.6 |
| Average value, mean ± SD | 0.9 ± 0.1 | 0.9 ± 0.1 | 0.9 ± 0.1 |
| Min. to max. value of WHR | 0.7–1.1 | 0.7–1.2 | 0.7–1.2 |
| Blood pressure status (systole/diastole in mmHg) 3 | |||
| Normal (<120/<80), in % | 55.3 | 70.7 | 63.8 |
| Pre-hypertension (120–129/<80), in % | 31.9 | 20.7 | 25.7 |
| Hypertension stage 1 (130–139/80–89), in % | 10.6 | 6.9 | 8.6 |
| Hypertension stage 2 (≥140/≥90), in % | 2.1 | 1.7 | 1.9 |
| Diabetes Mellitus (DM) history of family member | |||
| Yes, in % | 25.5 | 32.8 | 29.5 |
| No, in % | 74.5 | 67.2 | 70.5 |
| Hypertension history of family member | |||
| Yes, in % | 21.3 | 37.9 | 30.5 |
| No, in % | 78.7 | 62.1 | 69.5 |
| Cardiovascular (CVD) disease history of family member | |||
| Yes, in % | 21.3 | 12.1 | 11.4 |
| No, in % | 89.4 | 87.9 | 88.6 |
| Suffering from DM | |||
| Yes, in % | 0 | 3.4 | 1.9 |
| No, in % | 100 | 96.6 | 98.1 |
| Suffering from hypertension | |||
| Yes, in % | 0 | 3.4 | 3.8 |
| No, in % | 95.7 | 96.6 | 96.2 |
| Suffering from CVD | |||
| Yes, in % | 0 | 0 | 0 |
| No, in % | 100 | 100 | 100 |
| Characteristic | Adolescents (13–18 Years Old) | School-Age Children (6–12 Years Old) | ||||
|---|---|---|---|---|---|---|
| Male | Female | All | Male | Female | All | |
| Body height status 1 by age, in % | ||||||
| Stunted | 9.8 | 1.8 | 5.6 | 5.1 | 11.5 | 8.1 |
| Normal | 90.2 | 98.2 | 94.4 | 89.8 | 88.5 | 89.2 |
| Tall | 0 | 0 | 0 | 5.1 | 0 | 0 |
| BMI status by age 1, in % | ||||||
| Underweight | 13.7 | 7.2 | 10.2 | 6.8 | 5.8 | 6.3 |
| Normal | 66.7 | 83.9 | 75.7 | 76.3 | 84.6 | 80.2 |
| Overweight | 19.6 | 5.4 | 12.1 | 16.9 | 9.6 | 13.5 |
| Obese | 0 | 3.6 | 1.9 | 0 | 0 | 0 |
| Blood pressure status 2, in % | ||||||
| Normal | 90.2 | 98.2 | 94.4 | 98.3 | 98.1 | 98.2 |
| Pre-hypertension | 7.8 | 0 | 3.7 | 1.7 | 1.9 | 1.8 |
| Hypertension | 2 | 1.8 | 1.9 | 0 | 0 | 0 |
| Diabetes Mellitus (DM) history of family member | ||||||
| Yes, in % | 15.7 | 17.9 | 16.8 | 22 | 23.1 | 22.5 |
| No, in % | 84.3 | 82.1 | 83.2 | 78 | 76.9 | 77.5 |
| Hypertension history of family member | ||||||
| Yes, in % | 15.7 | 23.2 | 19.6 | 23.7 | 26.9 | 25.2 |
| No, in % | 84.3 | 76.8 | 94.4 | 76.3 | 73.1 | 74.8 |
| Cardiovascular (CVD) disease history of family member | ||||||
| Yes, in % | 3.9 | 7.1 | 5.6 | 10.2 | 11.5 | 10.8 |
| No, in % | 96.1 | 92.9 | 94.4 | 89.8 | 88.5 | 89.2 |
| Suffering from DM | ||||||
| Yes, in % | 0 | 0 | 0 | 0 | 0 | 0 |
| No, in % | 100 | 100 | 100 | 100 | 100 | 100 |
| Suffering from hypertension | ||||||
| Yes, in % | 3.9 | 0 | 1.9 | 0 | 0 | 0 |
| No, in % | 96.1 | 100 | 98.1 | 100 | 100 | 100 |
| Suffering from CVD | ||||||
| Yes, in % | 0 | 0 | 0 | 0 | 0 | 0 |
| No, in % | 100 | 100 | 100 | 100 | 100 | 100 |
| No | Food Group | Food Consumption (g/capita/day) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Adults (Mean ± SD) | Adolescents (Mean ± SD) | School-Age Group (Mean ± SD) | ||||||||
| Male | Female | All | Male | Female | All | Male | Female | All | ||
| 1 | Bakery products | 18.5 ± 32.8 | 15.5 ± 29.1 | 16.9 ± 30.7 | 18.4 ± 31.2 | 32.5 ± 111 | 25.7 ± 82.9 | 19.0 ± 30.5 | 21 ± 33.1 | 19.9 ± 31.6 |
| 2 | Beverages | 1186 ± 612 | 1215 ± 669 | 1202 ± 644 | 1077 ± 692 | 941 ± 444 | 1006 ± 577 | 1055 ± 665 | 889 ± 442 | 977 ± 575 |
| 3 | Cereals and cereal products | 635 ± 235 | 523 ± 216 | 573 ± 231 | 704 ± 285 | 552 ± 181 | 624 ± 247 | 563 ± 253 | 504 ± 157 | 535 ± 214 |
| 4 | Eggs and egg products | 35.1 ± 44.8 | 15.6 ± 20.0 | 24.3 ± 34.7 | 28.4 ± 41.4 | 21.4 ± 24.3 | 24.8 ± 33.6 | 30.3 ± 33.2 | 42.3 ± 39.9 | 35.9 ± 36.8 |
| 5 | Fish and fish products (incl. seafood) | 34.8 ± 50.2 | 25.0 ± 46.0 | 29.4 ± 47.9 | 28.0 ± 47.3 | 19.5 ± 29.1 | 23.5 ± 38.9 | 16.9 ± 28.2 | 17.5 ± 30.7 | 17.2 ± 29.3 |
| 6 | Fruits and fruit products | 75 ± 159 | 55.6 ± 76.8 | 64.3 ± 121 | 37.1 ± 66.8 | 35.1 ± 71.4 | 36.0 ± 68.9 | 14.9 ± 35.5 | 31.5 ± 63.3 | 22.7 ± 50.7 |
| 7 | Legumes and legume products | 53.2 ± 64.3 | 52.1 ± 91.5 | 52.6 ± 80.1 | 22.7 ± 33.4 | 28.8 ± 41.3 | 25.9 ± 37.7 | 34.9 ± 81.5 | 20.0 ± 45.5 | 27.9 ± 67.2 |
| 8 | Meat and meat products | 20 ± 41.0 | 25.8 ± 69.0 | 23.2 ± 58.2 | 22.0 ± 56 | 23.8 ± 45.1 | 23 ± 50.3 | 17.6 ± 47.1 | 8.8 ± 21.1 | 13.5 ± 37.3 |
| 9 | Milk and dairy products | 22.5 ± 70.5 | 16.8 ± 58.7 | 19.4 ± 64 | 84.4 ± 124 | 101 ± 170.5 | 93 ± 150 | 186 ± 167 | 139 ± 185 | 164 ± 176 |
| 10 | Chicken and poultry products | 55.7 ± 69.7 | 57.7 ± 77.2 | 56.8 ± 73.6 | 62.5 ± 68.9 | 60.9 ± 71.5 | 61.6 ± 69.9 | 71.4 ± 71.8 | 60.0 ± 57.1 | 66.1 ± 65.3 |
| 11 | Snacks | 75.1 ± 99.1 | 81.7 ± 81.7 | 78.7 ± 88.6 | 57.1 ± 70.4 | 76.4 ± 91.6 | 67.2 ± 82.4 | 96.3 ± 109 | 76.7 ± 83.9 | 87.1 ± 98.2 |
| 12 | Vegetables and vegetable products | 124 ± 96.7 | 111 ± 97.2 | 117 ± 96.8 | 80.6 ± 101 | 68 ± 68 | 74 ± 85.3 | 65.3 ± 60.4 | 58.0 ± 59.2 | 61.9 ± 59.7 |
| 13 | Supplements | 0 | 0 | 0 | 0.0 ± 0.2 | 0.0 ± 0.1 | 0.0 ± 0.1 | 0 | 0 | 0 |
| Total | 2334 | 2195 | 2257 | 2222 | 1960 | 2084 | 2169 | 1868 | 2028 | |
| Data Sources | Fat Content | Sugar Content | Salt Content | |||
|---|---|---|---|---|---|---|
| Number of Food Items | % | Number of Food Items | % | Number of Food Items | % | |
| Food composition databases 1 | 37 | 8.03 | 8 | 1.74 | 1 | 0.22 |
| Recipe elaboration | 291 | 63.12 | 249 | 54.01 | 227 | 49.24 |
| Food labels 2 | 109 | 23.64 | 115 | 24.95 | 84 | 18.22 |
| Laboratory analysis | 0 | 0.00 | 22 | 4.77 | 40 | 8.68 |
| Assigned as zero | 4 | 0.87 | 67 | 14.53 | 109 | 23.64 |
| Unavailable data | 20 | 4.34 | 0 | 0.00 | 0 | 0.00 |
| Total | 461 | 100 | 461 | 100 | 461 | 100 |
| No. | Food Group | Added Sugar Intake (g/capita/day) 1 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Adults | Adolescents | School-Age Children | ||||||||
| Male | Female | All | Male | Female | All | Male | Female | All | ||
| 1 | Bakery products | 1.42 (0.28–13.5) 2 | 0.86 (0.29–11.7) | 1.11 (0.28–13.5) | 1.11 (0.52–7.32) | 1.45 (0.10–28.2) | 1.29 (0.10–28.2) | 1.63 (0.40–12.1) | 1.13 (0.52–20.3) | 1.40 (0.40–20.3) |
| 2 | Beverages | 25.9 (0–92.04) | 23.4 (0.10–101.9) | 24.5 (0–101.9) | 18.2 (0.11–81.1) | 19.4 (0.10–71.1) | 18.8 (0.10–81.1) | 17.1 (0–68.6) | 13.4 (0.21–51.5) | 15.4 (0–68.6) |
| 3 | Cereals and cereal products | 3.37 (0–45.3) | 2.36 (0–17.1) | 2.81 (0–45.3) | 3.55 (0–15.5) | 3.84 (0–38.7) | 3.70 (0–38.7) | 3.88 (0–17.9) | 2.29 (0–9.00) | 3.14 (0–17.9) |
| 4 | Eggs and egg products | 0.23 (0–1.24) | 0.08 (0–0.77) | 0.15 (0–1.24) | 0.21 (0–1.99) | 0.14 (0–0.83) | 0.18 (0–1.99) | 0.14 (0–0.687) | 0.23 (0–2.85) | 0.18 (0–2.85) |
| 5 | Fish and fish products (incl. seafood) | 0.16 (0–1.49) | 0.17 (0–2.04) | 0.17 (0–2.04) | 0.757 (0.000–16.562) | 0.114 (0.000–0.780) | 0.421 (0.000–16.562) | 0.085 (0.000–1.115) | 0.092 (0.000–0.884) | 0.088 (0.000–1.115) |
| 6 | Fruits and fruit products | 0 | 0.52 (0–14.3) | 0.29 (0–14.3) | 1.23 (0–22.0) | 0.27 (0–3.67) | 0.73 (0–22.0) | 1.88 (0–30.6) | 1.13 (0–19.5) | 1.53 (0–30.6) |
| 7 | Legumes and legume products | 1.43 (0–11.04) | 1.89 (0–48.5) | 1.68 (0–48.5) | 1.33 (0–22.0) | 0.63 (0–16.2) | 0.96 (0–22.0) | 2.64 (0–43.2) | 1.18 (0–19.5) | 1.96 (0–43.2) |
| 8 | Meat and meat products | 0.10 (0–1.48) | 0.21 (0–8.21) | 0.16 (0–8.21) | 0.13 (0–3.80) | 0.30 (0–3.80) | 0.22 (0–3.80) | 0.18 (0–3.75) | 0.06 (0–1.59) | 0.12 (0–3.75) |
| 9 | Milk and dairy products | 0.70 (0–15.5) | 2.24 (0–94.5) | 1.55 (0–94.5) | 4.39 (0–27.0) | 5.15 (0–35.5) | 4.79 (0–35.5) | 8.30 (0–30.20) | 6.42 (0–38.3) | 7.42 (0–38.3) |
| 10 | Chicken and poultry products | 0.42 (0–2.73) | 0.47 (0–3.80) | 0.45 (0–3.80) | 0.45 (0–2.72) | 0.49 (0–4.93) | 0.48 (0–4.93) | 0.40 (0–3.17) | 0.48 (0–6.03) | 0.44 (0–6.03) |
| 11 | Snacks | 9.84 (0–129) | 9.59 (0–48.2) | 9.71 (0–129) | 6.58 (0–60.9) | 7.9 (0–35.35) | 7.28 (0–60.9) | 10.7 (0–58.6) | 8.95 (0–66.8) | 9.88 (0–66.78) |
| 12 | Vegetables and vegetable products | 1.00 (0–6.03) | 1.31 (0–12.2) | 1.17 (0–12.2) | 1.38 (0.03–10.6) | 0.73 (0–3.16) | 1.04 (0–10.6) | 0.54 (0–2.86) | 0.44 (0–5.72) | 0.49 (0–5.72) |
| Total | 44.6a 3 | 43.1a | 43.8A 4 | 38.3a | 40.3a | 39.3A | 45.8a | 34.9b | 40.7A | |
| No. | Food Group | Salt Intake (g/capita/day) 1 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Adults | Adolescents | School-Age Children | ||||||||
| Male | Female | All | Male | Female | All | Male | Female | All | ||
| 1 | Bakery products | 0.18 (0–1.54) 2 | 0.15 (0–1.52) | 0.16 (0–1.54) | 0.17 (0.08–1.16) | 0.14 (0.02–1.04) | 0.16 (0.02–1.16) | 0.20 (0–2.86) | 0.15 (0–1.52) | 0.17 (0–2.86) |
| 2 | Beverages | 0.13 (0–1.49) | 0.04 (0–0.35) | 0.08 (0–1.49) | 0.16 (0–1.20) | 0.13 (0–1.05) | 0.15 (0–1.20) | 0.02 (0–0.23) | 0.04 (0–0.35) | 0.02 (0–0.23) |
| 3 | Cereals and cereal products | 2.23 (0–6.91) | 2.09 (0–10.5) | 2.15 (0–10.5) | 3.48 (0–9.23) | 2.78 (0–9.62) | 3.11 (0–9.62) | 2.23 (0–6.73) | 2.09 (0–10.52) | 2.46 (0.000–7.51) |
| 4 | Eggs and egg products | 0.52 (0.10–3.42) | 0.21 (0–1.56) | 0.35 (0–3.42) | 0.45 (0.06–2.96) | 0.33 (0.08–2.01) | 0.39 (0.06–2.92) | 0.60 (0–2.58) | 0.21 (0–1.56) | 0.51 (0–2.58) |
| 5 | Fish and fish products (incl. seafood) | 0.74 (0.04–7.60) | 0.41 (0.02–5.38) | 0.56 (0.02–7.60) | 0.54 (0.07–4.29) | 0.29 (0.05–3.83) | 0.41 (0.05–4.29) | 0.37 (0.06–3.60) | 0.41 (0.02–5.38) | 0.35 (0.06–3.60) |
| 6 | Fruits and fruit products | 0.003 (0–0.13) | 0.03 (0–0.91) | 0.02 (0–0.91) | 0.0003 (0–0.01) | 0.01 (0–0.35) | 0.004 (0–0.35) | 0.01 (0–0.50) | 0.03 (0–0.91) | 0.01 (0–0.50) |
| 7 | Legumes and legume products | 0.76 (0.17–2.89) | 0.60 (0.001–2.94) | 0.67 (0.001–2.94) | 0.42 (0.04–2.60) | 0.39 (0–2.61) | 0.41 (0–2.61) | 0.28 (0.001–3.22) | 0.60 (0.001–2.94) | 0.31 (0–3.22) |
| 8 | Meat and meat products | 0.12 (0.02–1.20) | 0.16 (0.05–1.77) | 0.14 (0.02–1.77) | 0.21 (0.03–2.34) | 0.22 (0.07–1.92) | 0.22 (0.03–2.34) | 0.07 (0.06–0.62) | 0.16 (0.05–1.77) | 0.15 (0.06–2.53) |
| 9 | Milk and dairy products | 0.02 (0–0.46) | 0.01 (0–0.34) | 0.01 (0–0.46) | 0.15 (0.04–0.80) | 0.18 (0–1.40) | 0.16 (0–1.40) | 0.01 (0–0.14) | 0.01 (0–0.34) | 0.01 (0–0.14) |
| 10 | Chicken and poultry products | 0.60 (0.12–3.63) | 0.56 (0.11–4.20) | 0.58 (0.11–4.20) | 0.70 (0.02–4.03) | 0.62 (0.10–3.38) | 0.66 (0.02–4.03) | 0.69 (0.13–2.27) | 0.56 (0.11–4.20) | 0.70 (0.05–2.75) |
| 11 | Snacks | 0.44 (0–2.28) | 0.51 (0–4.06) | 0.48 (0–4.06) | 0.48 (0–3.35) | 0.54 (0.04–2.18) | 0.51 (0–3.35) | 0.53 (0–4.08) | 0.51 (0–4.06) | 0.61 (0–4.15) |
| 12 | Vegetables and vegetable products | 0.62 (0–1.84) | 0.69 (0.06–2.55) | 0.66 (0–2.55) | 0.66 (0.01–5.18) | 0.48 (0–2.79) | 0.56 (0–5.18) | 0.59 (0–4.03) | 0.69 (0.06–2.55) | 0.54 (0–5.22) |
| Total | 6.36a 3 | 5.46a | 5.86B 4 | 7.43a | 6.11b | 6.74A | 6.02a | 5.60a | 5.83B | |
| No. | Food Group | Fat Intake (g/capita/day) 1 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Adults | Adolescents | School-Age Children | ||||||||
| Male | Female | All | Male | Female | All | Male | Female | All | ||
| 1 | Bakery products | 2.04 (0.28–17.6) 2 | 1.96 (0.71–25.4) | 1.99 (0.28–25.4) | 1.98 (1.62–19.3) | 2.57 (1.74–25.4) | 2.30 (1.62–25.4) | 2.63 (0.89–4.15) | 4.15 (0.63–30.6) | 3.34 (0.63–30.6) |
| 2 | Beverages | 5.33 (0–75.3) | 3.16 (0–86.6) | 4.13 (0–86.6) | 0.96 (0–19.8) | 2.50 (0–61.9) | 1.77 (0–61.9) | 3.00 (0–61.9) | 1.00 (0–11.4) | 2.06 (0–61.9) |
| 3 | Cereals and cereal products | 11.7 (0.54–53.9) | 9.69 (0.41–30.5) | 10.59 (0.41–53.99) | 23.56 (0–0.59) | 16.3 (0.47–79.6) | 19.8 (0.47–86.3) | 13.6 (0.51–56.1) | 11.7 (0.55–42.2) | 12.7 (0.51–56.1) |
| 4 | Eggs and egg products | 5.01 (2.64–19.60) | 2.52 (2.07–13.3) | 3.63 (2.07–19.6) | 4.23 (1.93–16.4) | 3.28 (1.88–17.6) | 3.73 (1.88–17.6) | 4.54 (1.76–20.4) | 6.19 (2.62–25.90) | 5.31 (1.76–25.90) |
| 5 | Fish and fish products (incl. seafood) | 4.74 (0.86–34.3) | 3.50 (0.61–25.8) | 4.05 (0.61–34.3) | 3.31 (1.26–26.4) | 2.60 (0.48–18.5) | 2.94 (0.48–26.37) | 2.84 (0.61–18.69) | 2.52 (0.73–28.2) | 2.69 (0.61–28.2) |
| 6 | Fruits and fruit products | 0.23 (0.02–2.76) | 0.49 (0–8.70) | 0.37 (0–8.70) | 0.11 (0–1.03) | 0.20 (0–7.04) | 0.16 (0–7.04) | 0.18 (0–4.98) | 0.22 (0–6.99) | 0.20 (0–6.99) |
| 7 | Legumes and legume products | 5.93 (1.50–35.1) | 4.08 (0–28.8) | 4.91 (0–35.1) | 2.49 (0.01–25.5) | 2.91 (0–15.8) | 2.71 (0–25.50) | 2.14 (0–13.4) | 2.20 (0–44.5) | 2.17 (0–44.5) |
| 8 | Meat and meat products | 3.61 (0.60–45.4) | 3.15 (0.37–72.7) | 3.36 (0.37–72.7) | 3.84 (0.37–51.2) | 2.65 (0.08–53.7) | 3.22 (0.08–53.7) | 2.05 (1.33–33.6) | 1.85 (0.77–36.6) | 1.96 (0.77–36.6) |
| 9 | Milk and dairy products | 0.25 (0–3.57) | 0.44 (0.91–14.6) | 0.35 (0–14.58) | 1.88 (0.88–10.4) | 2.87 (0.15–21.3) | 2.40 (0.15–21.3) | 4.89 (0–18.13) | 3.28 (0.07–18.00) | 4.13 (0–18.13) |
| 10 | Chicken and poultry products | 7.60 (2.01–33.6) | 7.52 (1.81–57.2) | 7.56 (1.81–57.2) | 9.44 (3.42–48.9) | 9.83 (2.85–42.1) | 9.65 (2.85–48.9) | 9.79 (2.05–51.5) | 9.50 (2.09–43.0) | 9.65 (2.05–51.5) |
| 11 | Snacks | 7.36 (0.21–30.3) | 9.13 (0.04–8.34) | 8.34 (0.04–46.9) | 10.3 (0.92–43.7) | 9.81 (0.49–62.92) | 10.0 (0.49–62.9) | 14.8 (0.095–148) | 11.3 (0.37–64.7) | 13.1 (0.095–148) |
| 12 | Vegetables and vegetable products | 3.12 (0.02–8.35) | 3.39 (0.02–19.2) | 3.26 (0.02–19.2) | 3.01 (0–26.2) | 2.13 (0.01–12.4) | 2.55 (0–26.2) | 2.02 (0–9.16) | 2.13 (0.13–10.4) | 2.07 (0–10.4) |
| Total | 56.9a 3 | 49.0a | 52.6B 4 | 65.1a | 57.7a | 61.2A | 62.5a | 56.0a | 59.4A | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Andarwulan, N.; Madanijah, S.; Briawan, D.; Anwar, K.; Bararah, A.; Saraswati; Średnicka-Tober, D. Food Consumption Pattern and the Intake of Sugar, Salt, and Fat in the South Jakarta City—Indonesia. Nutrients 2021, 13, 1289. https://doi.org/10.3390/nu13041289
Andarwulan N, Madanijah S, Briawan D, Anwar K, Bararah A, Saraswati, Średnicka-Tober D. Food Consumption Pattern and the Intake of Sugar, Salt, and Fat in the South Jakarta City—Indonesia. Nutrients. 2021; 13(4):1289. https://doi.org/10.3390/nu13041289
Chicago/Turabian StyleAndarwulan, Nuri, Siti Madanijah, Dodik Briawan, Khoirul Anwar, Atikah Bararah, Saraswati, and Dominika Średnicka-Tober. 2021. "Food Consumption Pattern and the Intake of Sugar, Salt, and Fat in the South Jakarta City—Indonesia" Nutrients 13, no. 4: 1289. https://doi.org/10.3390/nu13041289
APA StyleAndarwulan, N., Madanijah, S., Briawan, D., Anwar, K., Bararah, A., Saraswati, & Średnicka-Tober, D. (2021). Food Consumption Pattern and the Intake of Sugar, Salt, and Fat in the South Jakarta City—Indonesia. Nutrients, 13(4), 1289. https://doi.org/10.3390/nu13041289








