Rhinovirus—A True Respiratory Threat or a Common Inconvenience of Childhood?
Abstract
:1. Introduction
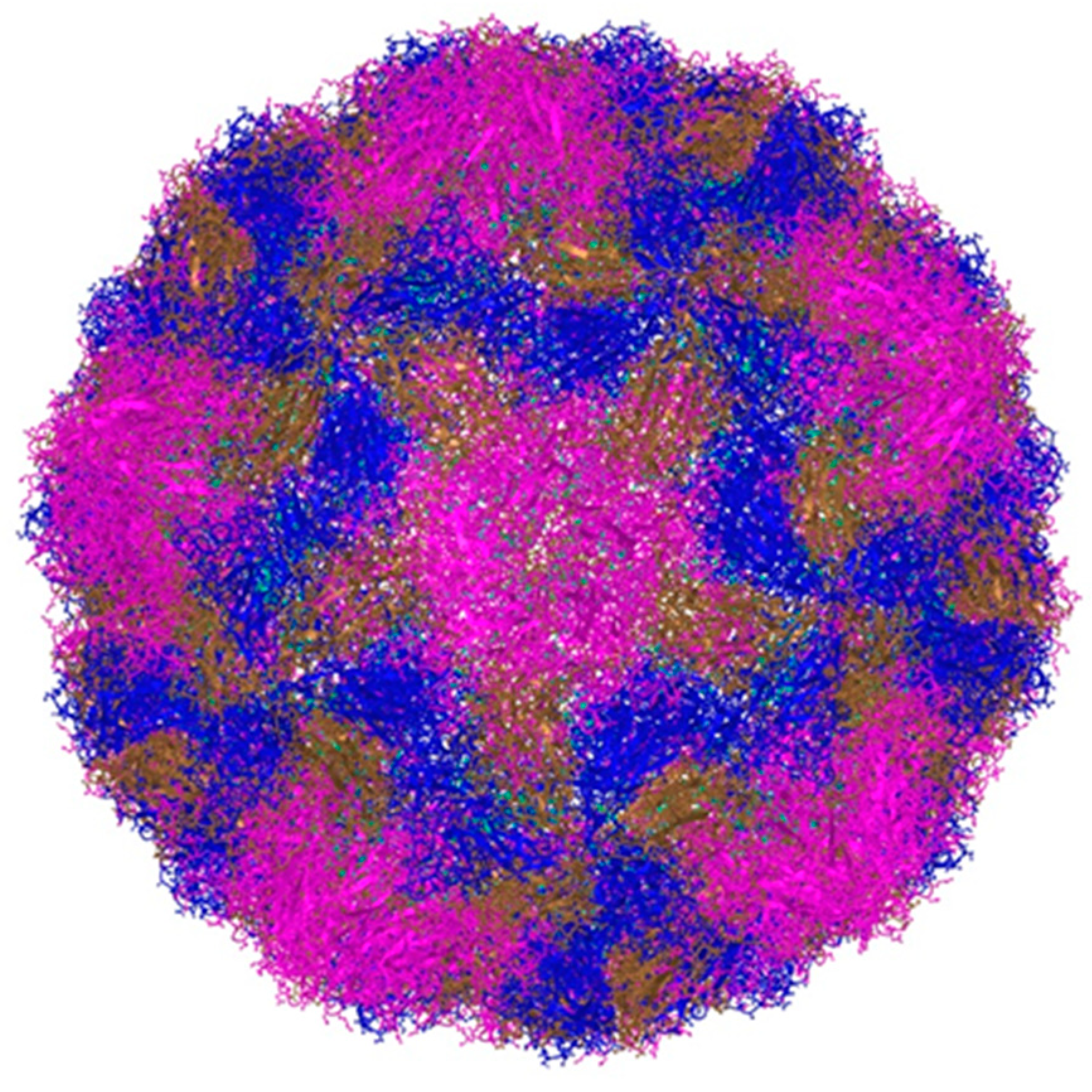
2. Classification and Main Characteristics
3. Modes of Transmission and Prevalence of Infection
4. The Link between Rhinovirus Epidemiology and Clinical Presentation
5. Risk Factors for the Development of a Severe Form of the Infection
6. Long-Term Consequences of Rhinovirus Infection
7. Pathogenesis of Asthma and Recurrent Wheezing Caused by Rhinoviruses
8. A Snapshot of Treatment Studies for Rhinovirus Infection
9. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gern, J.E. The ABCs of rhinoviruses, wheezing, and asthma. J. Virol. 2010, 84, 7418–7426. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vandini, S.; Biaggi, C.; Fischer, M.; Lanari, M. Impact of Rhinovirus Infections in Children. Viruses. 2019, 11, 521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bizot, E.; Bousquet, A.; Charpié, M.; Coquelin, F.; Lefevre, S.; Le Lorier, J.; Patin, M.; Sée, P.; Sarfati, E.; Walle, S.; et al. Rhinovirus: A Narrative Review on Its Genetic Characteristics, Pediatric Clinical Presentations, and Pathogenesis. Front. Pediatr. 2021, 9, 643219. [Google Scholar] [CrossRef] [PubMed]
- Neugebauer, F.; Bergs, S.; Liebert, U.G.; Hönemann, M. Human Rhinoviruses in Pediatric Patients in a Tertiary Care Hospital in Germany: Molecular Epidemiology and Clinical Significance. Viruses. 2022, 14, 1829. [Google Scholar] [CrossRef] [PubMed]
- Price, W.H. The isolation of a new virus associated with respiratory clinical disease in humans. Proc. Natl. Acad. Sci. USA 1956, 42, 892–896. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gern, J.E.; Palmenberg, A.C. Rhinoviruses. In Fields Virology, 6th ed.; Knipe, D.M., Howley, P.M., Eds.; Wolters Kluwer/Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013. [Google Scholar]
- Jacobs, S.E.; Lamson, D.M.; George, K.S.; Walsh, T.J. Human rhinoviruses. Clin. Microbiol. Rev. 2013, 26, 135–162. [Google Scholar] [CrossRef] [Green Version]
- Simmonds, P.; Gorbalenya, A.E.; Harvala, H.; Hovi, T.; Knowles, N.J.; Lindberg, A.M.; Oberste, M.S.; Palmenberg, A.C.; Reuter, G.; Skern, T.; et al. Recommendations for the nomenclature of enteroviruses and rhinoviruses. Arch. Virol. 2020, 165, 793–797. [Google Scholar] [CrossRef] [Green Version]
- Royston, L.; Tapparel, C. Rhinoviruses and respiratory enteroviruses: Not as simple as ABC. Viruses 2016, 8, 16. [Google Scholar] [CrossRef] [Green Version]
- Basnet, S.; Palmenberg, A.C.; Gern, J.E. Rhinoviruses and Their Receptors. Chest 2019, 155, 1018–1025. [Google Scholar] [CrossRef]
- Palmenberg, A.C.; Gern, J.E. Classification and evolution of human rhinoviruses. Methods Mol. Biol. 2015, 1221, 1–10. [Google Scholar] [CrossRef] [Green Version]
- Esneau, C.; Duff, A.C.; Bartlett, N.W. Understanding Rhinovirus Circulation and Impact on Illness. Viruses 2022, 14, 141. [Google Scholar] [CrossRef] [PubMed]
- Lopez-Souza, N.; Favoreto, S.; Wong, H.; Ward, T.; Yagi, S.; Schnurr, D.; Finkbeiner, W.E.; Dolganov, G.M.; Widdicombe, J.H.; Boushey, H.A.; et al. In vitro susceptibility to rhinovirus infection is greater for bronchial than for nasal airway epithelial cells in human subjects. J. Allergy Clin. Immunol. 2009, 123, 1384–1390.e2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giardina, F.A.M.; Piralla, A.; Ferrari, G.; Zavaglio, F.; Cassaniti, I.; Baldanti, F. Molecular Epidemiology of Rhinovirus/Enterovirus and Their Role on Cause Severe and Prolonged Infection in Hospitalized Patients. Microorganisms 2022, 10, 755. [Google Scholar] [CrossRef]
- Savolainen-Kopra, C.; Korpela, T.; Simonen-Tikka, M.L.; Amiryousefi, A.; Ziegler, T.; Roivainen, M.; Hovi, T. Single treatment with ethanol hand rub is ineffective against human rhinovirus hand washing with soap and water removes the virus efficiently. J. Med. Virol. 2012, 84, 543–547. [Google Scholar] [CrossRef] [PubMed]
- Stott, E.J.; Heath, G.F. Factors affecting the growth of rhinovirus 2 in suspension cultures of L132 cells. J. Gen. Virol. 1970, 6, 15–24. [Google Scholar] [CrossRef]
- Papadopoulos, N.; Sanderson, G.; Hunter, J.; Johnston, S. Rhinoviruses replicate effectively at lower airway temperatures. J. Med. Virol. 1999, 58, 100–104. [Google Scholar] [CrossRef]
- Kreger, J.E.; Hershenson, M.B. Effects of COVID-19 and Social Distancing on Rhinovirus Infections and Asthma Exacerbations. Viruses 2022, 14, 2340. [Google Scholar] [CrossRef]
- Papadopoulos, N.G.; Bates, P.J.; Bardin, P.G.; Papi, A.; Leir, S.H.; Fraenkel, D.J.; Meyer, J.; Lackie, P.M.; Sanderson, G.; Holgate, S.T.; et al. Rhinoviruses infect the lower airways. J. Infect. Dis. 2000, 181, 1875–1884. [Google Scholar] [CrossRef] [Green Version]
- Mosser, A.G.; Vrtis, R.; Burchell, L.; Lee, W.-M.; Dick, C.R.; Weisshaar, E.; Bock, D.; Swenson, C.A.; Cornwell, R.D.; Meyer, K.C.; et al. Quantitative and qualitative analysis of rhinovirus infection in bronchial tissues. Am. J. Respir. Crit. Care Med. 2005, 171, 645–651. [Google Scholar] [CrossRef]
- Halabi, K.C.; Stockwell, M.S.; Alba, L.; Vargas, C.; Reed, C.; Saiman, L.; Mobile Surveillance for Acute Respiratory Infection/Influenza-like Illness in the Community (MoSAIC) Study Team. Clinical and socioeconomic burden of rhinoviruses/enteroviruses in the community. Influenza Other Respir. Viruses. 2022, 16, 891–896. [Google Scholar] [CrossRef]
- Jin, X.; Ren, J.; Li, R.; Gao, Y.; Zhang, H.; Li, J.; Zhang, J.; Wang, X.; Wang, G. Global burden of upper respiratory infections in 204 countries and territories, from 1990 to 2019. EClinicalMedicine 2021, 37, 100986. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.T.; Tan, K.B.; Abisheganaden, J.; Dickens, B.L. Forecasting upper respiratory tract infection burden using high-dimensional time series data and forecast combinations. PLoS Comput. Biol. 2023, 19, e1010892. [Google Scholar] [CrossRef]
- Takashita, E.; Kawakami, C.; Momoki, T.; Saikusa, M.; Shimizu, K.; Ozawa, H.; Kumazaki, M.; Usuku, S.; Tanaka, N.; Okubo, I.; et al. Increased risk of rhinovirus infection in children during the coronavirus disease-19 pandemic. Influenza Other Respir. Viruses 2021, 15, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Nickbakhsh, S.; Mair, C.; Matthews, L.; Reeve, R.; Johnson, P.C.D.; Thorburn, F.; von Wissmann, B.; Reynolds, A.; McMenamin, J.; Gunson, R.N.; et al. Virus-virus interactions impact the population dynamics of influenza and the common cold. Proc. Natl. Acad. Sci. USA 2019, 116, 27142–27150. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dee, K.; Goldfarb, D.M.; Haney, J.; Amat, J.A.R.; Herder, V.; Stewart, M.; Szemiel, A.M.; Baguelin, M.; Murcia, P.R. Human Rhinovirus Infection Blocks Severe Acute Respiratory Syndrome Coronavirus 2 Replication Within the Respiratory Epithelium: Implications for COVID-19 Epidemiology. J. Infect. Dis. 2021, 224, 31–38. [Google Scholar] [CrossRef]
- Essaidi-Laziosi, M.; Alvarez, C.; Puhach, O.; Sattonnet-Roche, P.; Torriani, G.; Tapparel, C.; Kaiser, L.; Eckerle, I. Sequential infections with rhinovirus and influenza modulate the replicative capacity of SARS-CoV-2 in the upper respiratory tract. Emerg. Microbes Infect. 2022, 11, 412–423. [Google Scholar] [CrossRef]
- Kenmoe, S.; Kengne-Nde, C.; Ebogo-Belobo, J.T.; Mbaga, D.S.; Fatawou Modiyinji, A.; Njouom, R. Systematic review and meta-analysis of the prevalence of common respiratory viruses in children < 2 years with bronchiolitis in the pre-COVID-19 pandemic era. PLoS ONE 2020, 15, e0242302. [Google Scholar] [CrossRef]
- Pratt, M.T.G.; Abdalla, T.; Richmond, P.C.; Moore, H.C.; Snelling, T.L.; Blyth, C.C.; Bhuiyan, M.U. Prevalence of respiratory viruses in community-acquired pneumonia in children: A systematic review and meta-analysis. Lancet Child. Adolesc. Health 2022, 6, 555–570. [Google Scholar] [CrossRef]
- Krumbein, H.; Kümmel, L.S.; Fragkou, P.C.; Thölken, C.; Hünerbein, B.L.; Reiter, R.; Papathanasiou, K.A.; Renz, H.; Skevaki, C. Respiratory viral co-infections in patients with COVID-19 and associated outcomes: A systematic review and meta-analysis. Rev. Med. Virol. 2023, 33, e2365. [Google Scholar] [CrossRef]
- Jartti, T.; Lehtinen, P.; Vuorinen, T.; Koskenvuo, M.; Ruuskanen, O. Persistence of rhinovirus and enterovirus RNA after acute respiratory illness in children. J. Med. Virol. 2004, 72, 695–699. [Google Scholar] [CrossRef]
- Heymann, P.W.; Platts-Mills, T.A.; Johnston, S.L. Role of viral infections, atopy and antiviral immunity in the etiology of wheezing exacerbations among children and young adults. Pediatr. Infect. Dis. J. 2005, 24, S217–S222. [Google Scholar] [CrossRef]
- Singleton, R.J.; Bulkow, L.R.; Miernyk, K.; DeByle, C.; Pruitt, L.; Hummel, K.B.; Bruden, D.; Englund, J.A.; Anderson, L.J.; Lucher, L.; et al. Viral respiratory infections in hospitalized and community control children in Alaska. J. Med. Virol. 2010, 82, 1282–1290. [Google Scholar] [CrossRef] [PubMed]
- Calvo, C.; Casas, I.; Garcia-Garcia, M.L.; Pozo, F.; Reyes, N.; Cruz, N.; García-Cuenllas, L.; Pérez-Breña, P. Role of rhinovirus C respiratory infections in sick and healthy children in Spain. Pediatr. Infect. Dis. J. 2010, 29, 717–720. [Google Scholar] [CrossRef] [PubMed]
- Basharat, U.; Aiche, M.M.; Kim, M.M.; Sohal, M.; Chang, E.H. Are rhinoviruses implicated in the pathogenesis of sinusitis and chronic rhinosinusitis exacerbations? A comprehensive review. Int. Forum Allergy Rhinol. 2019, 9, 1159–1188. [Google Scholar] [CrossRef]
- Zhao, Y.; Shen, J.; Wu, B.; Liu, G.; Lu, R.; Tan, W. Genotypic Diversity and Epidemiology of Human Rhinovirus Among Children With Severe Acute Respiratory Tract Infection in Shanghai, 2013–2015. Front. Microbiol. 2018, 9, 1836. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ljubin-Sternak, S.; Meštrović, T.; Ivković-Jureković, I.; Kolarić, B.; Slović, A.; Forčić, D.; Tot, T.; Mijač, M.; Vraneš, J. The Emerging Role of Rhinoviruses in Lower Respiratory Tract Infections in Children—Clinical and Molecular Epidemiological Study From Croatia, 2017-2019. Front. Microbiol. 2019, 10, 2737. [Google Scholar] [CrossRef] [Green Version]
- Esposito, S.; Daleno, C.; Prunotto, G.; Scala, A.; Tagliabue, C.; Borzani, I.; Fossali, E.; Pelucchi, C.; Principi, N. Impact of viral infections in children with community-acquired pneumoniae: Results of a study of 17 respiratory viruses. Influenza Other Respir. Viruses 2013, 7, 18–26. [Google Scholar] [CrossRef] [Green Version]
- Ning, G.; Wang, X.; Wu, D.; Yin, Z.; Li, Y.; Wang, H.; Yang, W. The etiology of community-acquired pneumonia among children under 5 years of age in mainland China, 2001–2015: A systematic review. Hum. Vaccines Immunother. 2017, 13, 2742–2750. [Google Scholar] [CrossRef]
- Čivljak, R.; Tot, T.; Falsey, A.R.; Huljev, E.; Vraneš, J.; Ljubin-Sternak, S. Viral pathogens associated with acute respiratory illness in hospitalized adults and elderly from Zagreb, Croatia, 2016 to 2018. J. Med. Virol. 2019, 91, 1202–1209. [Google Scholar] [CrossRef] [Green Version]
- Esposito, S.; Daleno, C.; Tagliabue, C.; Scala, A.; Tenconi, R.; Borzani, I.; Fossali, E.; Pelucchi, C.; Piralla, A.; Principi, N. Impact of rhinoviruses on pediatric community-acquired pneumonia. Eur. J. Clin. Microbiol. Infect. Dis. 2012, 31, 1637–1645. [Google Scholar] [CrossRef]
- Hartiala, M.; Lahti, E.; Forsström, V.; Vuorinen, T.; Ruuskanen, O.; Peltola, V. Characteristics of Hospitalized Rhinovirus-Associated Community-Acquired Pneumonia in Children, Finland, 2003-2014. Front. Med. 2019, 6, 235. [Google Scholar] [CrossRef] [PubMed]
- Bahabri, I.; Abdulaal, A.; Alanazi, T.; Alenazy, S.; Alrumih, Y.; Alqahtani, R.; Bosaeed, M.; Al-Dorzi, H.M. Characteristics, Management, and Outcomes of Community-Acquired Pneumonia Due to Human Rhinovirus-A Retrospective Study. Can. Respir. J. 2022, 2022, 1349994. [Google Scholar] [CrossRef] [PubMed]
- Tsagarakis, N.J.; Sideri, A.; Makridis, P.; Triantafyllou, A.; Stamoulakatou, A.; Papadogeorgaki, E. Age-related prevalence of common upper respiratory pathogens, based on the application of the filmarray respiratory panel in a tertiary hospital in Greece. Medicine 2018, 97, e10903. [Google Scholar] [CrossRef] [PubMed]
- Feddema, J.J.; Claassen, E. Prevalence of Viral Respiratory Infections Amongst Asthmatics: Results of a Meta-Regression Analysis. Respir. Med. 2020, 173, 106020. [Google Scholar] [CrossRef]
- Kotaniemi-Syrjänen, A.; Reijonen, T.M.; Korhonen, K.; Waris, M.; Vainionpää, R.; Korppi, M. Wheezing due to rhinovirus infection in infancy: Bronchial hyperresponsiveness at school age. Pediatr. Int. 2008, 50, 506–510. [Google Scholar] [CrossRef]
- Turunen, R.; Koistinen, A.; Vuorinen, T.; Arku, B.; Söderlund-Venermo, M.; Ruuskanen, O.; Jartti, T. The first wheezing episode: Respiratory virus etiology, atopic characteristics, and illness severity. Pediatr. Allergy Immunol. 2014, 25, 796–803. [Google Scholar] [CrossRef]
- Jartti, T.; Gern, J.E. Role of viral infections in the development and exacerbation of asthma in children. J. Allergy Clin. Immunol. 2017, 140, 895–906. [Google Scholar] [CrossRef] [Green Version]
- Liu, L.; Pan, Y.; Zhu, Y.; Song, Y.; Su, X.; Yang, L.; Li, M. Association between rhinovirus wheezing illness and the development of childhood asthma: A metaanalysis. BMJ Open 2017, 7, e013034. [Google Scholar] [CrossRef] [Green Version]
- Drysdale, S.B.; Mejias, A.; Ramilo, O. Rhinovirus—Not just the common cold. J. Infect. 2017, 74, S41–S46. [Google Scholar] [CrossRef]
- Jartti, T.; Lehtinen, P.; Vuorinen, T.; Ruuskanen, O. Bronchiolitis: Age and previous wheezing episodes are linked to viral etiology and atopic characteristics. Pediatr. Infect. Dis. J. 2009, 28, 311–317. [Google Scholar] [CrossRef]
- Hyvarinen, M.K.; Kotaniemi-Syrjanen, A.; Reijonen, T.M.; Korhonen, K.; Korppi, M.O. Teenage asthma after severe early childhood wheezing: An 11-year prospective follow-up. Pediatr. Pulmonol. 2005, 40, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Jackson, D.J.; Gangnon, R.E.; Evans, M.D.; Roberg, K.A.; Anderson, E.L.; Pappas, T.E.; Printz, M.C.; Lee, W.M.; Shult, P.A.; Reisdorf, E.; et al. Wheezing rhinovirus illnesses in early life predict asthma development in high-risk children. Am. J. Respir. Crit. Care Med. 2008, 178, 667–672. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Midulla, F.; Nicolai, A.; Ferrara, M.; Gentile, F.; Pierangeli, A.; Bonci, E.; Scagnolari, C.; Moretti, C.; Antonelli, G.; Papoff, P. Recurrent wheezing 36 months after bronchiolitis is associated with rhinovirus infections and blood eosinophilia. Acta Paediatr. 2014, 103, 1094–1099. [Google Scholar] [CrossRef]
- Kusel, M.M.; de Klerk, N.H.; Holt, P.G.; Kebadze, T.; Johnston, S.L.; Sly, P.D. Role of respiratory viruses in acute upper and lower respiratory tract illness in the first year of life: A birth cohort study. Pediatr. Infect. Dis. J. 2006, 25, 680–686. [Google Scholar] [CrossRef]
- Jartti, T.; Smits, H.H.; Bønnelykke, K.; Bircan, O.; Elenius, V.; Konradsen, J.R.; Maggina, P.; Makrinioti, H.; Stokholm, J.; Hedlin, G.; et al. EAACI task force on clinical practice recommendations on preschool wheeze. Bronchiolitis needs a revisit: Distinguishing between virus entities and their treatments. Allergy 2019, 74, 40–52. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dumas, O.; Hasegawa, K.; Mansbach, J.M.; Sullivan, A.F.; Piedra, P.A.; Camargo, C.A., Jr. Severe bronchiolitis profiles and risk of recurrent wheeze by age 3 years. J. Allergy Clin. Immunol. 2019, 143, 1371–1379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Takeyama, A.; Hashimoto, K.; Sato, M.; Sato, T.; Tomita, Y.; Maeda, R.; Ito, M.; Katayose, M.; Kawasaki, Y.; Hosoya, M. Clinical and epidemiologic factors related to subsequent wheezing after virus-induced lower respiratory tract infections in hospitalized pediatric patients younger than 3 years. Eur. J. Pediatr. 2014, 173, 959–966. [Google Scholar] [CrossRef]
- Bergroth, E.; Aakula, M.; Elenius, V.; Remes, S.; Piippo-Savolainen, E.; Korppi, M.; Piedra, P.A.; Bochkov, Y.A.; Gern, J.E.; Camargo, C.A., Jr.; et al. Rhinovirus Type in Severe Bronchiolitis and the Development of Asthma. J. Allergy Clin. Immunol. Pract. 2020, 8, 588–595.e4. [Google Scholar] [CrossRef]
- Nanishi, M.; Chandran, A.; Li, X.; Stanford, J.B.; Alshawabkeh, A.N.; Aschner, J.L.; Dabelea, D.; Dunlop, A.L.; Elliott, A.J.; Gern, J.E. Association of Severe Bronchiolitis during Infancy with Childhood Asthma Development: An Analysis of the ECHO Consortium. Biomedicines 2022, 11, 23. [Google Scholar] [CrossRef]
- van Benten, I.; Koopman, L.; Niesters, B.; Hop, W.; van Middelkoop, B.; de Waal, L.; van Drunen, K.; Osterhaus, A.; Neijens, H.; Fokkens, W. Predominance of rhinovirus in the nose of symptomatic and asymptomatic infants. Pediatr. Allergy Immunol. 2003, 14, 363–370. [Google Scholar] [CrossRef]
- Jackson, D.J.; Gern, J.E. Rhinovirus infections and their roles in asthma: Etiology and exacerbations. J. Allergy Clin. Immunol. Pract. 2022, 10, 673–681. [Google Scholar] [CrossRef] [PubMed]
- Nakagome, K.; Bochkov, Y.A.; Ashraf, S.; Brockman-Schneider, R.A.; Evans, M.D.; Pasic, T.R.; Gern, J.E. Effects of rhinovirus species on viral replication and cytokine production. J. Allergy Clin. Immunol. 2014, 134, 332–341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choi, T.; Devries, M.; Bacharier, L.B.; Busse, W.; Camargo, C.A.; Cohen, R.; Demuri, G.P.; Evans, M.D.; Fitzpatrick, A.M.; Gergen, P.J.; et al. Enhanced Neutralizing Antibody Responses to Rhinovirus C and Age-Dependent Patterns of Infection. Am. J. Respir. Crit. Care Med. 2021, 203, 822–830. [Google Scholar] [CrossRef]
- Bruning, A.H.L.; Thomas, X.V.; van der Linden, L.; Wildenbeest, J.G.; Minnaar, R.P.; Jansen, R.R.; de Jong, M.D.; Sterk, P.J.; van der Schee, M.P.; Wolthers, K.C.; et al. Clinical, virological and epidemiological characteristics of rhinovirus infections in early childhood: A comparison between non-hospitalised and hospitalised children. J. Clin. Virol. 2015, 73, 120–126. [Google Scholar] [CrossRef]
- Sayama, A.; Okamoto, M.; Tamaki, R.; Saito-Obata, M.; Saito, M.; Kamigaki, T.; Sayama, Y.; Lirio, I.; Manalo, J.I.G.; Tallo, V.L.; et al. Comparison of Rhinovirus A-, B-, and C-Associated Respiratory Tract Illness Severity Based on the 5′-Untranslated Region Among Children Younger Than 5 Years. Open Forum Infect. Dis. 2022, 9, ofac387. [Google Scholar] [CrossRef] [PubMed]
- Çalışkan, M.; Bochkov, Y.A.; Kreiner-Møller, E.; Bønnelykke, K.; Stein, M.M.; Du, G.; Bisgaard, H.; Jackson, D.J.; Gern, J.E.; Lemanske, R.F., Jr.; et al. Rhinovirus wheezing illness and genetic risk of childhood-onset asthma. N. Engl. J. Med. 2013, 368, 1398–1407. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Y.; Willis-Owen, S.A.G.; Spiegel, S.; Lloyd, C.M.; Moffatt, M.F.; Cookson, W.O.C.M. The ORMDL3 Asthma Gene Regulates ICAM1 and Has Multiple Effects on Cellular Inflammation. Am. J. Respir. Crit. Care Med. 2019, 199, 478–488. [Google Scholar] [CrossRef]
- Bønnelykke, K.; Sleiman, P.; Nielsen, K.; Kreiner-Møller, E.; Mercader, J.M.; Belgrave, D. A genome-wide association study identifies CDHR3 as a susceptibility locus for early childhood asthma with severe exacerbations. Nat. Genet. 2014, 46, 51–55. [Google Scholar] [CrossRef]
- Kanazawa, J.; Masuko, H.; Yatagai, Y.; Sakamoto, T.; Yamada, H.; Kaneko, Y. Genetic association of the functional CDHR3 genotype with early-onset adult asthma in Japanese populations. Allergol. Int. 2017, 66, 563–567. [Google Scholar] [CrossRef]
- Shigemasa, R.; Masuko, H.; Hyodo, K.; Kitazawa, H.; Kanazawa, J.; Yatagai, Y.; Iijima, H.; Naito, T.; Saito, T.; Hirota, T.; et al. Genetic impact of CDHR3 on the adult onset of asthma and COPD. Clin. Exp. Allergy 2020, 50, 1223–1229. [Google Scholar] [CrossRef]
- Palmenberg, A.C. Rhinovirus C, Asthma, and Cell Surface Expression of Virus Receptor CDHR3. J. Virol. 2017, 91, e00072-17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, W.M.; Lemanske, R.F., Jr.; Evans, M.D.; Vang, F.; Pappas, T.; Gangnon, R.; Jackson, D.J.; Gern, J.E. Human rhinovirus species and season of infection determine illness severity. Am. J. Respir. Crit. Care Med. 2012, 186, 886–891. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Restori, K.H.; Srinivasa, B.T.; Ward, B.J.; Fixman, E.D. Neonatal Immunity, Respiratory Virus Infections, and the Development of Asthma. Front. Immunol. 2018, 9, 1249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gern, J.E. Viral respiratory infection and the link to asthma. Pediatr. Infect. Dis. J. 2004, 23 (Suppl. 1), S78–S86. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kotaniemi-Syrjanen, A.; Vainionpaa, R.; Reijonen, T.M.; Waris, M.; Korhonen, K.; Korppi, M. Rhinovirus-induced wheezing in infancy—The first sign of childhood asthma? J. Allergy Clin. Immunol. 2003, 111, 66–71. [Google Scholar] [CrossRef] [PubMed]
- Da Silva Sena, C.R.; Morten, M.; Meredith, J.; Kepreotes, E.; Murphy, V.E.; Gibson, G.P.; Robinson, P.D.; Sly, P.D.; Whitehead, B.; Karmaus, W.; et al. Rhinovirus bronchiolitis, maternal asthma, and the development of asthma and lung function impairments. Pediatr. Pulmonol. 2021, 56, 362–370. [Google Scholar] [CrossRef] [PubMed]
- De Winter, J.J.; Bont, L.; Wilbrink, B.; van der Ent, C.K.; Smit, H.A.; Houben, M.L. Rhinovirus wheezing illness in infancy is associated with medically attended third year wheezing in low risk infants: Results of a healthy birth cohort study. Immun. Inflamm. Dis. 2015, 3, 398–405. [Google Scholar] [CrossRef]
- Makrinioti, H.; Hasegawa, K.; Lakoumentas, J.; Xepapadaki, P.; Tsolia, M.; Castro-Rodriguez, J.A.; Feleszko, W.; Jartti, T.; Johnston, S.L.; Bush, A.; et al. The role of respiratory syncytial virus- and rhinovirus-induced bronchiolitis in recurrent wheeze and asthma-A systematic review and meta-analysis. Pediatr. Allergy Immunol. 2022, 33, e13741. [Google Scholar] [CrossRef]
- Miller, E.K.; Edwards, K.M.; Weinberg, G.A.; Iwane, M.K.; Griffin, M.R.; Hall, C.B.; Zhu, Y.; Szilagyi, P.G.; Morin, L.L.; Heil, L.H.; et al. New Vaccine Surveillance Network. A novel group of rhinoviruses is associated with asthma hospitalizations. J. Allergy Clin. Immunol. 2009, 123, 98–104.e1. [Google Scholar] [CrossRef]
- Hasegawa, K.; Mansbach, J.M.; Bochkov, Y.A.; Gern, J.E.; Piedra, P.A.; Bauer, C.S.; Teach, S.J.; Wu, S.; Sullivan, A.F.; Camargo, C.A., Jr. Association of Rhinovirus C Bronchiolitis and Immunoglobulin E Sensitization During Infancy with Development of Recurrent Wheeze. JAMA Pediatr. 2019, 173, 544–552. [Google Scholar] [CrossRef]
- Liew, K.Y.; Koh, S.K.; Hooi, S.L.; Ng, M.K.L.; Chee, H.Y.; Harith, H.H.; Israf, D.A.; Tham, C.L. Rhinovirus-Induced Cytokine Alterations with Potential Implications in Asthma Exacerbations: A Systematic Review and Meta-Analysis. Front. Immunol. 2022, 13, 782936. [Google Scholar] [CrossRef] [PubMed]
- Rajput, C.; Han, M.; Ishikawa, T.; Lei, J.; Goldsmith, A.M.; Jazaeri, S.; Stroupe, C.C.; Bentley, J.K.; Hershenson, M.B. Rhinovirus C Infection Induces Type 2 Innate Lymphoid Cell Expansion and Eosinophilic Airway Inflammation. Front. Immunol. 2021, 12, 649520. [Google Scholar] [CrossRef] [PubMed]
- Arden, K.E.; McErlean, P.; Nissen, M.D.; Sloots, T.P.; Mackay, I.M. Frequent detection of human rhinoviruses, paramyxoviruses, coronaviruses, and bocavirus during acute respiratory tract infections. J. Med. Virol. 2006, 78, 1232–1240. [Google Scholar] [CrossRef] [PubMed]
- Lau, S.K.; Yip, C.C.; Woo, P.C.; Yuen, K.Y. Human rhinovirus C: A newly discovered human rhinovirus species. Emerg. Health Threat. J. 2010, 3, e2. [Google Scholar] [CrossRef] [Green Version]
- Bochkov, Y.A.; Watters, K.; Ashraf, S.; Griggs, T.F.; Devries, M.K.; Jackson, D.J.; Palmenberg, A.C.; Gern, J.E. Cadherin-related family member 3, a childhood asthma susceptibility gene product, mediates rhinovirus C binding and replication. Proc. Natl. Acad. Sci. USA 2015, 112, 5485–5490. [Google Scholar] [CrossRef] [Green Version]
- Beale, J.; Jayaraman, A.; Jackson, D.J.; Macintyre, J.D.; Edwards, M.R.; Walton, R.P.; Zhu, J.; Ching, Y.M.; Shamji, B.; Edwards, M.; et al. Rhinovirus-induced IL-25 in asthma exacerbation drives type 2 immunity and allergic pulmonary inflammation. Sci. Transl. Med. 2014, 6, 256ra134. [Google Scholar] [CrossRef] [Green Version]
- Fonseca, W.; Lukacs, N.W.; Elesela, S.; Malinczak, C.A. Role of ILC2 in Viral-Induced Lung Pathogenesis. Front. Immunol. 2021, 12, 675169. [Google Scholar] [CrossRef]
- Nguyen-Thi-Dieu, T.; Le-Thi-Thu, H.; Le-Thi-Minh, H.; Pham-Nhat, A.; Duong-Quy, S. Study of Clinical Characteristics and Cytokine Profiles of Asthmatic Children with Rhinovirus Infection during Acute Asthma Exacerbation at National Hospital of Pediatrics. Can. Respir. J. 2018, 2018, 9375967. [Google Scholar] [CrossRef] [Green Version]
- Jiang, M.; Liu, H.; Li, Z.; Wang, J.; Zhang, F.; Cao, K.; Li, F.; Ding, J. ILC2s Induce Adaptive Th2-Type Immunity in Acute Exacerbation of Chronic Obstructive Pulmonary Disease. Mediat. Inflamm. 2019, 2019, 3140183. [Google Scholar] [CrossRef]
- Mehta, A.K.; Duan, W.; Doerner, A.M.; Traves, S.L.; Broide, D.H.; Proud, D.; Zuraw, B.L.; Croft, M. Rhinovirus infection interferes with induction of tolerance to aeroantigens through OX40 ligand, thymic stromal lymphopoietin, and IL-33. J. Allergy Clin. Immunol. 2016, 137, 278–288.e6. [Google Scholar] [CrossRef] [Green Version]
- Xatzipsalti, M.; Psarros, F.; Konstantinou, G.; Gaga, M.; Gourgiotis, D.; Saxoni-Papageorgiou, P.; Papadopoulos, N.G. Modulation of the epithelial inflammatory response to rhinovirus in an atopic environment. Clin. Exp. Allergy 2008, 38, 466–472. [Google Scholar] [CrossRef] [PubMed]
- Baraldo, S.; Contoli, M.; Bonato, M.; Snijders, D.; Biondini, D.; Bazzan, E.; Cosio, M.G.; Barbato, A.; Papi, A.; Saetta, M. Deficient Immune Response to Viral Infections in Children Predicts Later Asthma Persistence. Am. J. Respir. Crit. Care Med. 2018, 197, 673–675. [Google Scholar] [CrossRef]
- Dissanayake, T.K.; Schäuble, S.; Mirhakkak, M.H.; Wu, W.L.; Ng, A.C.; Yip, C.C.Y.; López, A.G.; Wolf, T.; Yeung, M.L.; Chan, K.H.; et al. Comparative Transcriptomic Analysis of Rhinovirus and Influenza Virus Infection. Front. Microbiol. 2020, 11, 1580. [Google Scholar] [CrossRef] [PubMed]
- Raita, Y.; Camargo, C.A., Jr.; Bochkov, Y.A.; Celedón, J.C.; Gern, J.E.; Mansbach, J.M.; Rhee, E.P.; Freishtat, R.J.; Hasegawa, K. Integrated-omics endotyping of infants with rhinovirus bronchiolitis and risk of childhood asthma. J. Allergy Clin. Immunol. 2021, 147, 2108–2117. [Google Scholar] [CrossRef] [PubMed]
- Bauer, L.; Lyoo, H.; van der Schaar, H.M.; Strating, J.R.; van Kuppeveld, F.J. Direct-acting antivirals and host-targeting strategies to combat enterovirus infections. Curr. Opin. Virol. 2017, 24, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Pevear, D.C.; Hayden, F.G.; Demenczuk, T.M.; Barone, L.R.; McKinlay, M.A.; Collett, M.S. Relationship of pleconaril susceptibility and clinical outcomes in treatment of common colds caused by rhinoviruses. Antimicrob. Agents Chemother. 2005, 49, 4492–4499. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayden, F.G.; Hipskind, G.J.; Woerner, D.H.; Eisen, G.F.; Janssens, M.; Janssen, P.A.; Andries, K. Intranasal pirodavir (R77,975) treatment of rhinovirus colds. Antimicrob. Agents Chemother. 1995, 39, 290–294. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mello, C.; Aguayo, E.; Rodriguez, M.; Lee, G.; Jordan, R.; Cihlar, T.; Birkus, G. Multiple classes of antiviral agents exhibit in vitro activity against human rhinovirus type C. Antimicrob. Agents Chemother. 2014, 58, 1546–1655. [Google Scholar] [CrossRef] [Green Version]
- Binford, S.L.; Maldonado, F.; Brothers, M.A.; Weady, P.T.; Zalman, L.S.; Meador, J.W., 3rd; Matthews, D.A.; Patick, A.K. Conservation of amino acids in human rhinovirus 3C protease correlates with broad-spectrum antiviral activity of rupintrivir, a novel human rhinovirus 3C protease inhibitor. Antimicrob. Agents Chemother. 2005, 49, 619–626. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Z.; Yang, E.; Hu, C.; Cheng, H.; Chen, C.Y.; Huang, D.; Wang, R.; Zhao, Y.; Rong, L.; Vignuzzi, M.; et al. Cell-Based High-Throughput Screening Assay Identifies 2′,2′-Difluoro-2′-deoxycytidine Gemcitabine as a Potential Antipoliovirus Agent. ACS Infect. Dis. 2017, 3, 45–53. [Google Scholar] [CrossRef] [Green Version]
- Lembo, D.; Cagno, V.; Civra, A.; Poli, G. Oxysterols: An emerging class of broad spectrum antiviral effectors. Mol. Asp. Med. 2016, 49, 23–30. [Google Scholar] [CrossRef] [PubMed]
- Civra, A.; Cagno, V.; Donalisio, M.; Biasi, F.; Leonarduzzi, G.; Poli, G.; Lembo, D. Inhibition of pathogenic non-enveloped viruses by 25-hydroxycholesterol and 27-hydroxycholesterol. Sci. Rep. 2014, 4, 7487. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Civra, A.; Francese, R.; Gamba, P.; Testa, G.; Cagno, V.; Poli, G.; Lembo, D. 25-Hydroxycholesterol and 27-hydroxycholesterol inhibit human rotavirus infection by sequestering viral particles into late endosomes. Redox Biol. 2018, 19, 318–330. [Google Scholar] [CrossRef] [PubMed]
- Gomes, B.; Sanna, G.; Madeddu, S.; Hollmann, A.; Santos, N.C. Combining 25-Hydroxycholesterol with an HIV Fusion Inhibitor Peptide: Interaction with Biomembrane Model Systems and Human Blood Cells. ACS Infect. Dis. 2019, 5, 582–591. [Google Scholar] [CrossRef]
- Zu, S.; Deng, Y.Q.; Zhou, C.; Li, J.; Li, L.; Chen, Q.; Li, X.F.; Zhao, H.; Gold, S.; He, J.; et al. 25-Hydroxycholesterol is a potent SARS-CoV-2 inhibitor. Cell Res. 2020, 30, 1043–1045. [Google Scholar] [CrossRef]
- Roulin, P.S.; Lötzerich, M.; Torta, F.; Tanner, L.B.; van Kuppeveld, F.J.; Wenk, M.R.; Greber, U.F. Rhinovirus uses a phosphatidylinositol 4-phosphate/cholesterol counter-current for the formation of replication compartments at the ER-Golgi interface. Cell Host Microbe 2014, 16, 677–690. [Google Scholar] [CrossRef] [Green Version]
- Civra, A.; Costantino, M.; Cavalli, R.; Adami, M.; Volante, M.; Poli, G.; Lembo, D. 27-Hydroxycholesterol inhibits rhinovirus replication in vitro and on human nasal and bronchial histocultures without selecting viral resistant variants. Antivir. Res. 2022, 204, 105368. [Google Scholar] [CrossRef]
- Rutaganira, F.U.; Fowler, M.L.; McPhail, J.A.; Gelman, M.A.; Nguyen, K.; Xiong, A.; Dornan, G.L.; Tavshanjian, B.; Glenn, J.S.; Shokat, K.M.; et al. Design and Structural Characterization of Potent and Selective Inhibitors of Phosphatidylinositol 4 Kinase IIIβ. J. Med. Chem. 2016, 59, 1830–1839. [Google Scholar] [CrossRef] [Green Version]
- Lamarche, M.J.; Borawski, J.; Bose, A.; Capacci-Daniel, C.; Colvin, R.; Dennehy, M.; Ding, J.; Dobler, M.; Drumm, J.; Gaither, L.A.; et al. Anti-hepatitis C virus activity and toxicity of type III phosphatidylinositol-4-kinase beta inhibitors. Antimicrob. Agents Chemother. 2012, 56, 5149–5156. [Google Scholar] [CrossRef] [Green Version]
| Authors | Publication Year | Population Examined | Final Number of Included Studies | Sample Size | Rhinovirus Prevalence |
|---|---|---|---|---|---|
| Kenmoe et al. | 2020 | Children < 2 years with bronchiolitis | 51 | 79,803 | 19.29% * (95% CI 16.67–22.04%) * |
| Pratt et al. | 2022 | Children with community-acquired pneumonia | 186 | 152,209 | 22.1% (95% CI 19.5–24.7%) |
| Krubmein et al. | 2023 | Children and adults with COVID-19 | 59 | 149,319 | 1.32% (95% CI 1.15–1.52%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ljubin-Sternak, S.; Meštrović, T. Rhinovirus—A True Respiratory Threat or a Common Inconvenience of Childhood? Viruses 2023, 15, 825. https://doi.org/10.3390/v15040825
Ljubin-Sternak S, Meštrović T. Rhinovirus—A True Respiratory Threat or a Common Inconvenience of Childhood? Viruses. 2023; 15(4):825. https://doi.org/10.3390/v15040825
Chicago/Turabian StyleLjubin-Sternak, Sunčanica, and Tomislav Meštrović. 2023. "Rhinovirus—A True Respiratory Threat or a Common Inconvenience of Childhood?" Viruses 15, no. 4: 825. https://doi.org/10.3390/v15040825
APA StyleLjubin-Sternak, S., & Meštrović, T. (2023). Rhinovirus—A True Respiratory Threat or a Common Inconvenience of Childhood? Viruses, 15(4), 825. https://doi.org/10.3390/v15040825







