A Narrative Review of Dietary Assessment Tools for Preschool-Aged Children in the Home Environment
Abstract
1. Introduction
| Dietary Assessment Tool | Description | Key Considerations for Use in Preschool-Aged Children | Respondent | Diet Intake Captured | Dietary Variable Outputs | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Single | Multiple | Habitual | Acute | Foods/ Food Groups | Energy | Macro-Nutrients | Micro- Nutrients | Score/Index | |||
| 24 h Recall | Facilitated interview by trained professional or automated software to capture amounts of foods and beverages consumed by respondent in past 24 h period. Sample period: 2–3 days, mix of weekday and weekend | Primary respondent may not be with child for all 24 h. Culturally specific foods can be captured due to open-ended nature of tool. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ||
| Food Record/ Diary | Written or electronic account of all foods and beverages consumed over a specified timeframe. Items may be weighed or non-weighed. Sample period: 3–7 consecutive days | Primary respondent may not be with child for all 24 h. Record may be completed across multiple settings (childcare/home, split households). Culturally specific foods can be captured due to open-ended nature of tool. | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | ✓ | |
| FFQ/ FFQ Screener | Defined list of foods and beverages; asks frequency of consumption over an extended timeframe. Respondents choose from close-ended, multiple-choice options. Usually self-administered but can be interviewer administered/assisted. FFQ contains a comprehensive list of items (~120–180 items). FFQ screeners contain an abbreviated list of the specified items (~20 items) and can be targeted to a specific food group or nutrient. Sample period: 1 W to 6 M (vs. 12 M for adults) | Complex to navigate and literacy level of respondent should be considered. The FFQ Screener provides only high-level view of intake. List of food items may not include foods commonly consumed in some cultures or child-friendly items. | ✓ | ✓ | ✓ | * | ✓ | ✓ | ✓ | ||
| Food Checklist | Defined list of foods and beverages for which respondents are asked to check which of the specified items were consumed over a specified time period. It may also ask about behavioral habits (e.g., reading nutrition labels). Portion sizes may be captured. Sample period: single or multiple days | Low participant burden, although literacy level of respondent should be considered. List of food items may not include foods commonly consumed in some cultures or child-friendly items. | ✓ | ✓ | ✓ | ✓ | ✓ | ||||
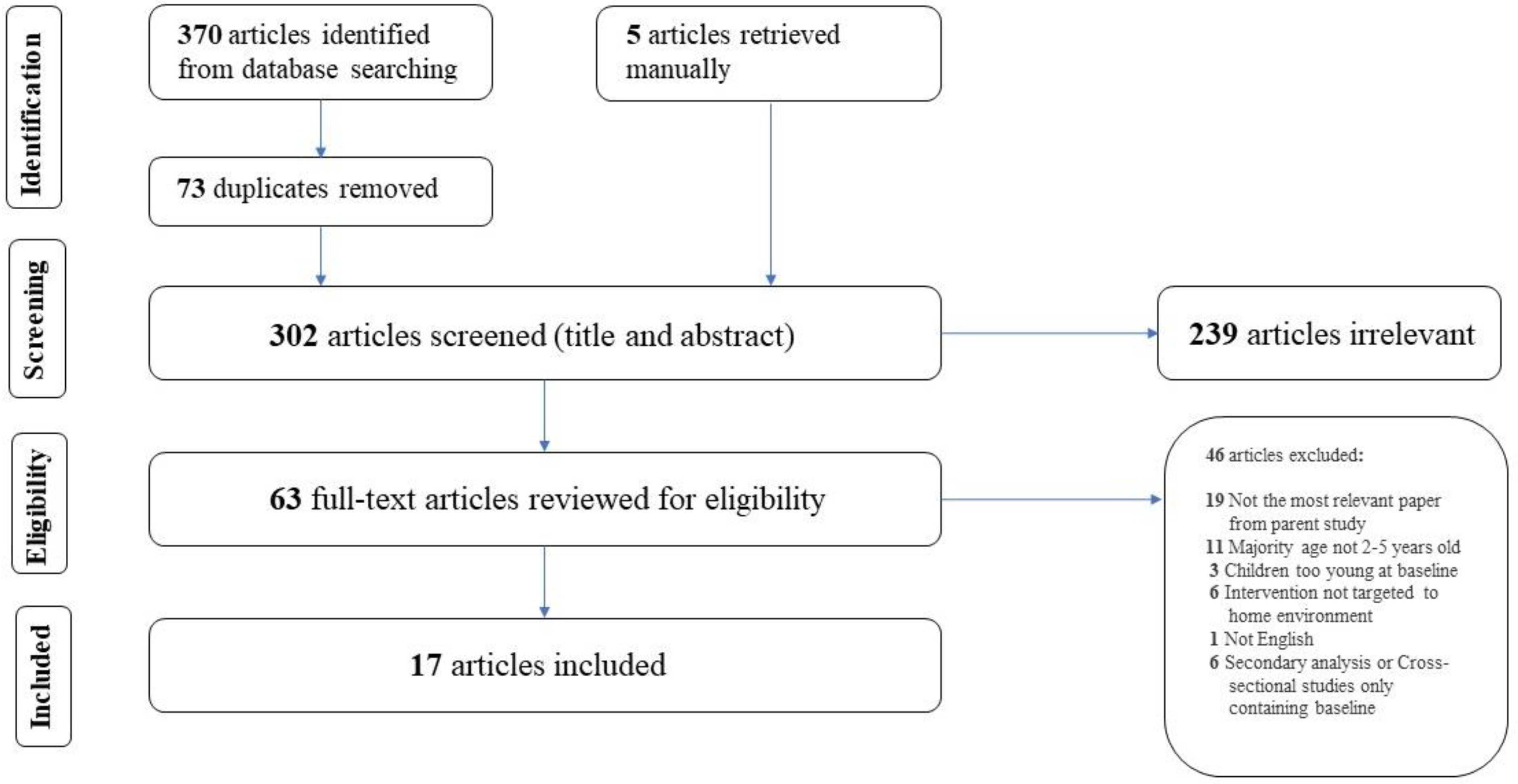
2. Materials and Methods
2.1. Data Sources and Searching Strategies
2.2. Inclusion and Exclusion Criteria
2.3. Selection of Studies
2.4. Data Extraction
3. Results
3.1. Study Characteristics
3.2. Participant Characteristics
3.3. Measurement Tools Used
3.4. Intervention Scope
3.5. Intervention Objectives
3.6. Key Findings
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
Appendix A.1. PubMed Search Terms
- Child, Preschool[MeSH] OR “young child*”[tiab] OR kid[tiab] OR preschool*[tiab] OR toddler*[tiab]
- “parents”[MeSH] OR “home environment”[MeSH] OR “home-based”[tiab] OR “home environment”[tiab] OR “home food environment”[tiab] OR “family meal”[tiab] OR “home food”[tiab] OR “food in home”[tiab] OR “family-based”[tiab] OR “family environment”[tiab] OR “family food environment”[tiab] OR caregiver[tiab] OR parent[tiab] OR famil*[tiab] OR mother[tiab] OR father[tiab] OR guardian[tiab]
- AND
- “diet recall*”[tiab] OR “food recall*”[tiab] OR “24 h recall*”[tiab] OR “food frequency questionnaire*”[tiab] OR FFQ[tiab] OR screener[tiab] OR “dietary questionnaire”[tiab] OR “food survey*”[tiab] OR “diet survey*”[tiab] OR “meal survey*”[tiab] OR “food record*”[tiab] OR “diet record*”[tiab] OR “food checklist*”[tiab] or “food behavior checklist*”[tiab] OR “diet checklist*”[tiab] OR “food photo*”[tiab] OR “photo assisted diet assessment*”[tiab] OR PADA[tiab] OR “image based food record*”[tiab] OR IBFR[tiab] OR “dietary observ*”[tiab] OR “meal observ*”[tiab] or “food observ*”[tiab] OR “diet assess*”[tiab] OR “food assess*”[tiab] OR “meal assess*”[tiab] OR “weighed record*”[tiab] OR “plate waste”[tiab] OR “direct weighing method*”[tiab] OR “food diar*”[tiab] OR “meal diar*”[tiab]
- AND
- “food intake”[tiab] OR “energy intake”[tiab] OR “nutrition intake”[tiab] OR “dietary intake”[tiab] OR consumption[tiab] OR “diet quality”[tiab] OR “diet variety”[tiab] OR “food group”[tiab] OR calorie[tiab] OR kcal[tiab] OR “energy density”[tiab] OR adequa*[tiab] OR “healthy eating”[tiab]
- AND
- Interven*[tiab] OR trial[tiab] OR RCT[tiab] OR “randomized control trial”[tiab] OR “randomized control trial”[tiab] OR “quasi experiment*”[tiab] OR “behavior change”[tiab]
Appendix A.2. Web of Science Search Terms
- TS = (“young child*” OR kid OR preschool* OR toddler*)
- AND
- TS = (“parent” OR “home environment” OR “home-based” OR “home food environment” OR “family meal” OR “home food” OR “food in home” OR “family-based” OR “family environment” OR “family food environment” OR caregiver OR parent OR famil* OR mother OR father OR guardian)
- AND
- TS = (“diet recall*” OR “food recall*” OR “24 h recall*” OR “food frequency questionnaire*” OR FFQ OR “screener” OR “dietary questionnaire” OR “food survey*” OR “diet survey*” OR “meal survey*” OR “food record*” OR “diet record*” OR “food checklist*” or “food behavior checklist*” OR “diet checklist*” OR “food photo*” OR “photo assisted diet assessment*” OR PADA OR “image based food record*” OR IBFR OR “dietary observ*” OR “meal observ*” or “food observ*” OR “diet assess*” OR “food assess*” OR “meal assess*” OR “weighed record*” OR “plate waste” OR “direct weighing method*” OR “food diar*” OR “meal diar*”)
- AND
- TS = (Interven* OR trial OR RCT OR “randomized control trial” OR “randomized control trial” OR “quasi experiment*” OR “behavior change”)
References
- Interagency Committee on Human Nutrition Research. National Nutrition Research Roadmap 2016–2021: Advancing Nutrition Research to Improve and Sustain Health; Interagency Committee on Human Nutrition Research: Washington, DC, USA, 2016. [Google Scholar]
- U.S. Department of Agriculture; U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2020–2025, 9th ed.; U.S. Department of Agriculture: Washington, DC, USA; U.S. Department of Health and Human Services: Washington, DC, USA, 2020.
- 2020 Dietary Guidelines Advisory Committee and Data Analysis Team. Data Supplement for Food Group and Nutrient Distribution: All Life Stages; 2020 Dietary Guidelines Advisory Committee Project; U.S. Department of Agriculture: Washington, DC, USA; U.S. Department of Health and Human Services: Washington, DC, USA, 2020.
- Centers for Disease Control and Prevention. National Center for Health Statistics National Health and Nutrition Examination Survey (NHANES) 2017–2018 Dietary Data; Atlanta, GA, USA, 2020. Available online: https://www.cdc.gov/nchs/nhanes/index.htm (accessed on 14 October 2022).
- Fisher, J.; Lumeng, J.; Miller, L.; Smethers, A.; Lott, M. Evidence Based Recommendations and Best Practices for Promoting Healthy Eating Behaviors in Children 2 to 8 Years 2021. Healthy Eating Research; Robert Wood Johnson Foundation: Durham, NC, USA, 2021. [Google Scholar]
- Bekelman, T.A.; Bellows, L.L.; Johnson, S.L. Are Family Routines Modifiable Determinants of Preschool Children’s Eating, Dietary Intake, and Growth? A Review of Intervention Studies. Curr. Nutr. Rep. 2017, 6, 171–189. [Google Scholar] [CrossRef]
- Golan, M.; Weizman, A. Familial Approach to the Treatment of Childhood Obesity: Conceptual Model. J. Nutr. Educ. 2001, 33, 102–107. [Google Scholar] [CrossRef]
- Ventura, A.K.; Birch, L.L. Does Parenting Affect Children’s Eating and Weight Status? Int. J. Behav. Nutr. Phys. Act. 2008, 5, 15. [Google Scholar] [CrossRef]
- Reid, M.; Worsley, A.; Mavondo, F. The Obesogenic Household: Factors Influencing Dietary Gatekeeper Satisfaction with Family Diet. Psychol. Mark. 2015, 32, 544–557. [Google Scholar] [CrossRef]
- Boles, R.E.; Johnson, S.L.; Burdell, A.; Davies, P.L.; Gavin, W.J.; Bellows, L.L. Home Food Availability and Child Intake among Rural Families Identified to Be At-Risk for Health Disparities. Appetite 2019, 134, 135–141. [Google Scholar] [CrossRef]
- Gebremariam, M.K.; Vaqué-Crusellas, C.; Andersen, L.F.; Stok, F.M.; Stelmach-Mardas, M.; Brug, J.; Lien, N. Measurement of Availability and Accessibility of Food among Youth: A Systematic Review of Methodological Studies. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 22. [Google Scholar] [CrossRef]
- Vollmer, R.L.; Mobley, A.R. Parenting Styles, Feeding Styles, and Their Influence on Child Obesogenic Behaviors and Body Weight. A Review. Appetite 2013, 71, 232–241. [Google Scholar] [CrossRef]
- Draxten, M.; Fulkerson, J.A.; Friend, S.; Flattum, C.F.; Schow, R. Parental Role Modeling of Fruits and Vegetables at Meals and Snacks Is Associated with Children’s Adequate Consumption. Appetite 2014, 78, 1–7. [Google Scholar] [CrossRef]
- Robson, S.M.; Couch, S.C.; Peugh, J.L.; Glanz, K.; Zhou, C.; Sallis, J.F.; Saelens, B.E. Parent Diet Quality and Energy Intake Are Related to Child Diet Quality and Energy Intake. J. Acad. Nutr. Diet. 2016, 116, 984–990. [Google Scholar] [CrossRef]
- Rex, S.M.; Kopetsky, A.; Bodt, B.; Robson, S.M. Relationships among the Physical and Social Home Food Environments, Dietary Intake, and Diet Quality in Mothers and Children. J. Acad. Nutr. Diet. 2021, 121, 2013–2020. [Google Scholar] [CrossRef]
- Vilela, S.; Severo, M.; Moreira, T.; Ramos, E.; Lopes, C. Evaluation of a Short Food Frequency Questionnaire for Dietary Intake Assessment among Children. Eur. J. Clin. Nutr. 2019, 73, 679–691. [Google Scholar] [CrossRef]
- Tugault-Lafleur, C.N.; Black, J.L.; Barr, S.I. A Systematic Review of Methods to Assess Children’s Diets in the School Context. Adv. Nutr. 2017, 8, 63–79. [Google Scholar] [CrossRef]
- Dao, M.C.; Subar, A.F.; Warthon-Medina, M.; Cade, J.E.; Burrows, T.; Golley, R.K.; Forouhi, N.G.; Pearce, M.; Holmes, B.A. Dietary Assessment Toolkits: An Overview. Public Health Nutr. 2019, 22, 404–418. [Google Scholar] [CrossRef] [PubMed]
- National Center for Education Statistics Enrollment Rates of Young Children. Available online: https://nces.ed.gov/programs/coe/indicator/cfa/enrollment-of-young-children (accessed on 7 October 2022).
- National Cancer Institute Comparing Dietary Assessment Instruments. Available online: https://dietassessmentprimer.cancer.gov/profiles/table.html (accessed on 14 October 2022).
- Callahan, E.A. Approaches to Assessing Intake of Food and Dietary Supplements in Pregnant Women and Children 2 to 11 Years of Age; Proceedings of a Workshop Series; National Academies Press: Washington, DC, USA, 2022; ISBN 978-0-309-27160-8. [Google Scholar]
- Cade, J.E.; Warthon-Medina, M.; Albar, S.; Alwan, N.A.; Ness, A.; Roe, M.; Wark, P.A.; Greathead, K.; Burley, V.J.; Finglas, P.; et al. DIET@NET: Best Practice Guidelines for Dietary Assessment in Health Research. BMC Med. 2017, 15, 202. [Google Scholar] [CrossRef] [PubMed]
- NIHR Cambridge Biomedical Research Centre DAPA Measurement Toolkit. Available online: https://dapa-toolkit.mrc.ac.uk/diet/subjective-methods/introduction (accessed on 14 October 2022).
- Nutritools Dietary Assessment Tools. Available online: https://www.nutritools.org/tools/24#t1 (accessed on 14 October 2022).
- Burrows, T.L.; Martin, R.J.; Collins, C.E. A Systematic Review of the Validity of Dietary Assessment Methods in Children When Compared with the Method of Doubly Labeled Water. J. Am. Diet. Assoc. 2010, 110, 1501–1510. [Google Scholar] [CrossRef] [PubMed]
- McPherson, R.S.; Hoelscher, D.M.; Alexander, M.; Scanlon, K.S.; Serdula, M.K. Dietary Assessment Methods among School-Aged Children: Validity and Reliability. Prev. Med. 2000, 31, S11–S33. [Google Scholar] [CrossRef]
- Rockett, H.R.H.; Berkey, C.S.; Colditz, G.A. Evaluation of Dietary Assessment Instruments in Adolescents. Curr. Opin. Clin. Nutr. Metab. Care 2003, 6, 557–562. [Google Scholar] [CrossRef]
- Bell, L.K.; Golley, R.K.; Magarey, A.M. Short Tools to Assess Young Children’s Dietary Intake: A Systematic Review Focusing on Application to Dietary Index Research. J. Obes. 2013, 2013, 709626. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. PLoS Med. 2021, 18, e1003583. [Google Scholar] [CrossRef]
- Bakırcı-Taylor, A.L.; Reed, D.B.; McCool, B.; Dawson, J.A. MHealth Improved Fruit and Vegetable Accessibility and Intake in Young Children. J. Nutr. Educ. Behav. 2019, 51, 556–566. [Google Scholar] [CrossRef]
- Barkin, S.L.; Heerman, W.J.; Sommer, E.C.; Martin, N.C.; Buchowski, M.S.; Schlundt, D.; Po’e, E.K.; Burgess, L.E.; Escarfuller, J.; Pratt, C.; et al. Effect of a Behavioral Intervention for Underserved Preschool-Age Children on Change in Body Mass Index: A Randomized Clinical Trial. JAMA 2018, 320, 450–460. [Google Scholar] [CrossRef]
- Davison, K.K.; Jurkowski, J.M.; Li, K.; Kranz, S.; Lawson, H.A. A Childhood Obesity Intervention Developed by Families for Families: Results from a Pilot Study. Int. J. Behav. Nutr. Phys. Act. 2013, 10, 3. [Google Scholar] [CrossRef] [PubMed]
- Fisher, J.O.; Serrano, E.L.; Foster, G.D.; Hart, C.N.; Davey, A.; Bruton, Y.P.; Kilby, L.; Harnack, L.; Ruth, K.J.; Kachurak, A.; et al. Efficacy of a Food Parenting Intervention for Mothers with Low Income to Reduce Preschooler’s Solid Fat and Added Sugar Intakes: A Randomized Controlled Trial. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 6. [Google Scholar] [CrossRef] [PubMed]
- Ling, J.; Robbins, L.B.; Zhang, N.; Kerver, J.M.; Lyons, H.; Wieber, N.; Zhang, M. Using Facebook in a Healthy Lifestyle Intervention: Feasibility and Preliminary Efficacy. West. J. Nurs. Res. 2018, 40, 1818–1842. [Google Scholar] [CrossRef]
- Natale, R.A.; Messiah, S.E.; Asfour, L.; Uhlhorn, S.B.; Delamater, A.; Arheart, K.L. Role Modeling as an Early Childhood Obesity Prevention Strategy: Effect of Parents and Teachers on Preschool Children’s Healthy Lifestyle Habits. J. Dev. Behav. Pediatr. 2014, 35, 378–387. [Google Scholar] [CrossRef] [PubMed]
- Mirotta, J.A.; Darlington, G.A.; Buchholz, A.C.; Haines, J.; Ma, D.W.L.; Duncan, A.M. Guelph Family Health Study’s Home-Based Obesity Prevention Intervention Increases Fibre and Fruit Intake in Preschool-Aged Children. Can. J. Diet. Pract. Res. 2018, 79, 86–90. [Google Scholar] [CrossRef] [PubMed]
- Ashton, L.M.; Morgan, P.J.; Grounds, J.A.; Young, M.D.; Rayward, A.T.; Barnes, A.T.; Pollock, E.R.; Kennedy, S.-L.; Saunders, K.L.; Collins, C.E. Dietary Outcomes of the ‘Healthy Youngsters, Healthy Dads’ Randomised Controlled Trial. Nutrients 2021, 13, 3306. [Google Scholar] [CrossRef] [PubMed]
- Duncanson, K.; Burrows, T.; Collins, C. Effect of a Low-Intensity Parent-Focused Nutrition Intervention on Dietary Intake of 2- to 5-Year Olds. J. Pediatr. Gastroenterol. Nutr. 2013, 57, 728–734. [Google Scholar] [CrossRef]
- Poelman, A.A.M.; Delahunty, C.M.; Broch, M.; de Graaf, C. Multiple vs Single Target Vegetable Exposure to Increase Young Children’s Vegetable Intake. J. Nutr. Educ. Behav. 2019, 51, 985–992. [Google Scholar] [CrossRef]
- Wyse, R.; Wolfenden, L.; Campbell, E.; Campbell, K.J.; Wiggers, J.; Brennan, L.; Fletcher, A.; Bowman, J.; Heard, T.R. A Cluster Randomized Controlled Trial of a Telephone-Based Parent Intervention to Increase Preschoolers’ Fruit and Vegetable Consumption. Am. J. Clin. Nutr. 2012, 96, 102–110. [Google Scholar] [CrossRef]
- Ray, C.; Figuereido, R.; Vepsäläinen, H.; Lehto, R.; Pajulahti, R.; Skaffari, E.; Sainio, T.; Hiltunen, P.; Lehto, E.; Korkalo, L.; et al. Effects of the Preschool-Based Family-Involving DAGIS Intervention Program on Children’s Energy Balance-Related Behaviors and Self-Regulation Skills: A Clustered Randomized Controlled Trial. Nutrients 2020, 12, 2599. [Google Scholar] [CrossRef]
- Somaraki, M.; Eli, K.; Sorjonen, K.; Ek, A.; Sandvik, P.; Nowicka, P. Changes in Parental Feeding Practices and Preschoolers’ Food Intake Following a Randomized Controlled Childhood Obesity Trial. Appetite 2020, 154, 104746. [Google Scholar] [CrossRef] [PubMed]
- Aktaç, Ş.; Kızıltan, G.; Avcı, S. The Effect of Family Participation in Nutrition Education Intervention on the Nutritional Status of Preschool Age Children. Educ. Sci. 2019, 44, 415–431. [Google Scholar] [CrossRef]
- Reale, S.; Kearney, C.; Hetherington, M.; Croden, F.; Cecil, J.; Carstairs, S.; Rolls, B.; Caton, S. The Feasibility and Acceptability of Two Methods of Snack Portion Control in United Kingdom (UK) Preschool Children: Reduction and Replacement. Nutrients 2018, 10, 1493. [Google Scholar] [CrossRef] [PubMed]
- Sirasa, F.; Mitchell, L.; Azhar, A.; Chandrasekara, A.; Harris, N. A 6-Week Healthy Eating Intervention with Family Engagement Improves Food Knowledge and Preferences but Not Dietary Diversity among Urban Preschool Children in Sri Lanka. Public Health Nutr. 2021, 24, 4328–4338. [Google Scholar] [CrossRef] [PubMed]
- Roche, M.L.; Ambato, L.; Sarsoza, J.; Kuhnlein, H.V. Mothers’ Groups Enrich Diet and Culture through Promoting Traditional Quichua Foods. Matern. Child Nutr. 2017, 13, e12530. [Google Scholar] [CrossRef] [PubMed]
- Börnhorst, C.; Huybrechts, I.; Ahrens, W.; Eiben, G.; Michels, N.; Pala, V.; Molnár, D.; Russo, P.; Barba, G.; Bel-Serrat, S.; et al. Prevalence and Determinants of Misreporting among European Children in Proxy-Reported 24 h Dietary Recalls. Br. J. Nutr. 2013, 109, 1257–1265. [Google Scholar] [CrossRef]
- Boushey, C.J.; Spoden, M.; Zhu, F.M.; Delp, E.J.; Kerr, D.A. New Mobile Methods for Dietary Assessment: Review of Image-Assisted and Image-Based Dietary Assessment Methods. Proc. Nutr. Soc. 2017, 76, 283–294. [Google Scholar] [CrossRef]
- Nicklas, T.; Saab, R.; Islam, N.G.; Wong, W.; Butte, N.; Schulin, R.; Liu, Y.; Apolzan, J.W.; Myers, C.A.; Martin, C.K. Validity of the Remote Food Photography Method Against Doubly Labeled Water Among Minority Preschoolers: Dietary Assessment of Preschoolers. Obesity 2017, 25, 1633–1638. [Google Scholar] [CrossRef]
- Elliott, S.; McCloskey, M.L.; Johnson, S.L.; Mena, N.Z.; Swindle, T.; Bellows, L.L. Food Photography as a Tool to Assess Type, Quantity, and Quality of Foods in Parent-Packed Lunches for Preschoolers. J. Nutr. Educ. Behav. 2021, 53, 164–173. [Google Scholar] [CrossRef]
- McCloskey, M.L.; Johnson, S.L.; Bekelman, T.A.; Martin, C.K.; Bellows, L.L. Beyond Nutrient Intake: Use of Digital Food Photography Methodology to Examine Family Dinnertime. J. Nutr. Educ. Behav. 2019, 51, 547–555.e1. [Google Scholar] [CrossRef] [PubMed]
- Bekelman, T.A.; Bellows, L.L.; McCloskey, M.L.; Martin, C.K.; Johnson, S.L. Assessing Dinner Meals Offered at Home among Preschoolers from Low-income Families with the Remote Food Photography Method. Pediatr. Obes. 2019, 14, e12558. [Google Scholar] [CrossRef] [PubMed]
- Kasper, N.; Mandell, C.; Ball, S.; Miller, A.L.; Lumeng, J.; Peterson, K.E. The Healthy Meal Index: A Tool for Measuring the Healthfulness of Meals Served to Children. Appetite 2016, 103, 54–63. [Google Scholar] [CrossRef] [PubMed]
- Williams, P.A.; Cates, S.C.; Blitstein, J.L.; Hersey, J.; Gabor, V.; Ball, M.; Kosa, K.; Wilson, H.; Olson, S.; Singh, A. Nutrition-Education Program Improves Preschoolers’ At-Home Diet: A Group Randomized Trial. J. Acad. Nutr. Diet. 2014, 114, 1001–1008. [Google Scholar] [CrossRef] [PubMed]
- Wyse, R.; Wolfenden, L.; Bisquera, A. Characteristics of the Home Food Environment That Mediate Immediate and Sustained Increases in Child Fruit and Vegetable Consumption: Mediation Analysis from the Healthy Habits Cluster Randomised Controlled Trial. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 118. [Google Scholar] [CrossRef] [PubMed]
| Study | Design | Child Participant | Adult Respondent | Dietary Assessment Tool | Dietary Variables Reported | Psychometric Properties | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample Size | Age (y) Mean (SD) | Role Gender | Race/ Ethnicity | Income | Type | # Items | Sample Period | ||||
| Wyse et al. (2012), Australia [40] | RCT | n = 394 | 4.3 (0.6) | Parents 96% female | Indigenous (2%) | Mixed | FFQ | NR | Previous 1 d, 7 d |
| Tool psychometrics reportedOriginal source cited (pre-K) |
| Davison et al. (2013), USA [32] | Quasi-Exp | n = 423 | 3.6 (1.0) | Parents/Grandparents 92% female | White (68%) Black (22%) | Low | 24 h Recall | - | 2 d(1 Wd, 1 We) |
| Original source cited (pre-K) |
| Duncanson et al. (2013), Australia [38] | RCT | n = 146 | 4.0 (0.1) I 4.0 (0.9) C | Parents 99% female | Indigenous (2%) | NR | FFQ | 120 | Previous 6 M |
| Original source cited (pre-K) |
| Natale et al. (2014), USA [35] | RCT | n = 1211 | 3.9 (0.9) | Caregivers 90% female | Hispanic (56%) Black (33%) | Low | Food Checklis | 32 | NR |
| Original source cited (pre-K) |
| Roche et al. (2017), Ecuador [46] | Quasi-Exp | NR | NR | Mothers | Indigenous (% NR) | NR | FFQ | NR | Previous 2 W |
| NR |
| Barkin et al. (2018), USA [31] | RCT | n = 610 | 4.3 (0.9) | Parents 98% female | Hispanic (91%) | Low | 24 h Recall | - | 3 d(2 Wd, 1 We) |
| NR |
| Ling et al. (2018), USA [34] | Pilot | n = 69 | 4.5 (0.5) | Caregivers 96% female | White (48%) Black (39%) | Low | FFQ Screener | 41 | Previous 1 W |
| Original source cited (other)Sample specific data provided |
| Mirotta et al. (2018), Canada [36] | Pilot | n = 45 | 3.2 (0.2) | Parents | White (81%) | Mixed | Food Record(non-weighed) | - | 3 d(2 Wd, 1 We) |
| NR |
| Reale et al. (2018), UK [44] | Pilot | n = 46 | 3.1 (0.8) | Mothers | White British, mixed or other (94%) | Mixed | FFQ | NR | NR |
| NR |
| Food Record (weighed) | - | 4 d(1 We) |
| NR | |||||||
| Aktaç et al. (2019), Turkey [43] | Quasi-Exp | n = 74 | 5.5 (0.5) I-1 5.7 (0.2) I-2 5.1 (0.6) C | Parents 51% female | NR | NR | Food Record | - | 3 d(2 Wd, 1 We) |
| NR |
| Bakirci-Taylor et al. (2019), USA [30] | Pilot | n = 30 | 3.6 (1.4) I 3.8 (0.8) C | Parents 100% female | White (73%) Hispanic (13%) | Mixed | Food Checklist | 10 | NR |
| Original source cited (pre-K) |
| Food Photography | - | 3 d(2 Wd, 1 We) |
| NR | |||||||
| Veggie Meter | - | - |
| Original source cited (other) | |||||||
| Fisher et al. (2019), USA [33] | RCT | n = 119 | 3.7 (0.8) | Mothers (biological) | Black (91%) | Low | 24 h Recall | - | 3 d(2 Wd, 1 We) |
| NR |
| Poelman et al. (2019), Australia [39] | Pilot | n = 32 | 5.2 (0.8) I-1 5.1 (0.7) I-2 5.0 (1.1) C | Parents 67% female | NR | NR | FFQ | NR | NR |
| Original source cited (other) |
| Food Record (weighed) | - | 3 d(2 Wd, 1 We) |
| NR | |||||||
| Weighed Dinner Meal | - | 1 meal |
| NR | |||||||
| Ray et al. (2020), Finland [41] | RCT | n = 802 | 5.2 (1.1) I 5.1 (1.0) C | Parents | NR | NR | FFQ | 51 | Previous 1 W |
| Original source cited (pre-K) |
| Somaraki et al. (2020), Sweden [42] | RCT | n = 174 | 5.2 (0.8) | Parents | NR | NR | FFQ | NR | NR |
| Original source cited (pre-K)Adaptions cite original source (other) |
| Ashton et al. (2021), Australia [37] | RCT | n = 125 | 3.9 (0.5) | Mothers | NR | Unclear | FFQ | 120 | Previous 2 M |
| Original source cited (pre-K) |
| Sirasa et al. (2021), Sri Lanka [45] | RCT | n= 345 | NR | Parents/Caregivers 86% female | Sinhalese (76%) Muslim (21%) | Unclear | Food Checklist | NR | Previous 1 W |
| Checklist: NRScoring: Original source cited (pre-K) |
| Study | Diet-Related Intervention Objective(s) | Intervention Duration | Assessment Tool(s) (Sample Period) | Data Collection Time Points | Key Findings |
|---|---|---|---|---|---|
| Overall Diet | |||||
| Aktaç et al. (2019), Turkey [43] | Evaluate the effectiveness of family participation in nutrition education on the nutritional status of preschool-aged children. | 10 W | Food Record (3 d) | B, 10 W | The intervention led to positive changes in consumption patterns in the Family Participation Group (FPG) and Education Group (EG), with greater changes in FPG (e.g., energy percentage from proteins). |
| Ashton et al. (2021), Australia [37] | Evaluate the efficacy of a family-based lifestyle intervention on change in dietary intake in fathers and their preschool-aged children and; investigate associations in father–child dietary intakes. | 8 W | FFQ (Previous 2 M) | B, 10 W, 9 M | Medium group-by-time effect sizes identified at 10 W for sodium and energy from core foods, energy-dense, nutrient-poor foods and prepacked snacks; sustained at 9 M follow-up. Moderate to strong associations existed in father–child dietary intakes for some dietary variables (e.g., fast foods). |
| Duncanson et al. (2013), Australia [38] | Determine if provision of quality nutrition information to rural parents using self-directed, technology-based education resources has an effect on the dietary patterns of 2–5-year-old children. | 12 M | FFQ (Previous 6 M) | B, 3 M, 12 M | Total reported energy from nutrient-dense food groups and percentage energy from energy-dense, nutrient-poor foods were high at baseline relative to estimated total energy expenditure for child age. No intervention effect. |
| Natale et al. (2014), USA [35] | Assess the effectiveness of a child care-based parent and teacher healthy lifestyle role-modeling program on child nutrition and PA outcomes. | 1 School Year | Food Checklist (NR) | B, Post-intervention | Intervention group significantly increased child FV consumption. Junk food consumption significantly decreased in the intervention group, increased in the control group. |
| Ray et al. (2020), Finland [41] | Evaluate the effects of a preschool-based family intervention on children’s energy balance-related behaviors such as food consumption and screen time, as well as PA and self-regulation skills. | 5 M | FFQ (Previous 1 W) | B, 5 M | No significant differences were detected between intervention and control groups for energy balance-related behaviors, self-regulation skills, or for consumption frequencies of sugary everyday foods and beverages, sugary treats, and FV. |
| Roche et al. (2017), Ecuador [46] | Assess the nutritional, social, and cultural potential of mothers’ cooking clubs that promoted Quichua culture and foods (leafy greens) to improve children’s nutrition. | 12 M | FFQ (Previous 2 W) | 12 M | Mothers in the intervention group were ~10 times more likely to feed their children the leafy greens than controls. Dietary diversity scores for all promoted foods were significantly greater for intervention children than for control children. |
| Sirasa et al. (2021), Sri Lanka [45] | Evaluate the effectiveness of a multicomponent intervention of child nutrition education plus family engagement, compared to a single component and control, on children’s dietary diversity. | 6 W | Food Checklist (Previous 1 W) | B, 6 W | Neither the Multicomponent nor Single Component groups showed significant differences in average dietary diversity score of children between baseline and post-intervention. |
| Specific Food Groups | |||||
| Bakirci-Taylor et al. (2019), USA [30] | Explore the effect of a parent-focused intervention with three mHealth technologies on the accessibility and intake of FV in young children. | 10 W | Food Checklist (NR) | B, 10 W | Screener data showed intervention children had higher vegetable consumption than control. Food photos showed no significant effects for week x treatment or treatment of frequency of FV. Significant week x treatment interaction values in children’s Veggie Meter values were found in the intervention group compared to control at mid- and post-intervention. |
| Food Photography (3 d) | B, 5 W, 10 W | ||||
| Veggie Meter | B, 5 W, 10 W | ||||
| Fisher et al. (2019), USA [33] | Evaluate the efficacy of an authoritative food parenting intervention for low-income mothers to reduce preschool-aged children’s intake of calories from SoFAS. | 12 W | 24 h Recall (3 d) | B, 12 W | At post-intervention, children in the intervention group consumed ~ 94 kcal or 23% less daily energy from SoFAS than control group. Child total daily energy intake did not significantly differ between groups post-intervention. |
| Poelman et al. (2019), Australia [39] | Evaluate the effectiveness of repeated exposure to multiple vs. single target vegetables in increasing young children’s vegetable intake. | 5 W | FFQ, (NR) | B, 4 M | FFQ data showed usual vegetable intake increased in the multiple target group from 0.6 to 1.2 servings/day and did not change in other groups. Food record data were not significant. Vegetable intake from the weighed dinner meal was not significantly different between groups. |
| Food Record (3 d) | B, 5 W, 4 M | ||||
| Weighed Dinner Meal | B, 5 W | ||||
| Wyse et al. (2012), Australia [40] | Assess the efficacy of a telephone-based intervention for parents to increase FV consumption in their 3–5-year-old children. | 4 W | FFQ (Previous 1 d, 7 d) | B, 2 M, 6 M | FV scores were significantly higher in the intervention group than control group at 2 M and 6 M. Sensitivity analysis showed intervention effect at 2 M but not 6 M. |
| Eating Occasion | |||||
| Reale et al. (2018), UK [44] | Explore the preliminary efficacy of two strategies of snack portion control (reduction and replacement) and; examine the efficacy of these two methods to improve diet in preschoolers. | 3 W | FFQ, (NR) | 1 W, 7–9 W | Snack replacement resulted in increased vegetable intake and decreased total daily energy intake when compared to snack reduction (Food Record). No significant changes to the frequency of snack intake pre- and post-intervention (FFQ). |
| Food Record (4 d) | 1 W, 2 W, 3 W | ||||
| Obesity Prevention and Treatment | |||||
| Barkin et al. (2018), USA [31] | Test the effect of a multicomponent behavioral intervention on child BMI growth trajectories among preschool children at risk for obesity. | 36 M | 24 h Recall (3 d) | B, 12 M, 24 M, 36 M | The intervention resulted in a statistically significant reduction in mean child daily energy intake and higher percentage of energy from protein compared with control. |
| Davison et al. (2013), USA [32] | Test initial efficacy of a parent-centered, community-based participatory research approach for obesity prevention for improving food, PA, and media-related parenting, as well as child behavioral and weight outcomes. | 6 M | 24 h Recall (2 d) | B, 8 M | At post-intervention, children had significantly lower total energy intake and macronutrient intake (fat, protein, and carbohydrate) compared with pre-intervention. |
| Ling et al. (2018), USA [34] | Examine the feasibility and preliminary efficacy of using Facebook in a lifestyle intervention to improve healthy behaviors and reduce BMI. | 10 W | FFQ Screener (Previous 1 W) | B, 10 W | The intervention resulted in small but nonsignificant effects on children’s FV intake. |
| Mirotta et al. (2018), Canada [36] | Examine the effectiveness of a home-based obesity prevention intervention on health behaviors, obesity risk and dietary intakes. | 6 M | Food Record (3 d) | B, 6 M | Post-intervention, the 4 home visits (HV) group had significantly higher fiber intake. The 4 HV and 2 HV groups had significantly higher fruit intake compared to control. |
| Somaraki et al. (2020), Sweden [42] | Evaluate the effects of two approaches (a parent support program with and without booster sessions and standard treatment) to treat obesity in preschoolers. | 12 M | FFQ (NR) | B, 3 M, 6 M, 12 M | Changes in intake did not differ between children by treatment. Within group changes in cookies/buns decreased over time among children in two treatment groups. Control children significantly decreased consumption of sweets/ chocolate. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bellows, L.L.; Lou, Y.; Nelson, R.; Reyes, L.I.; Brown, R.C.; Mena, N.Z.; Boles, R.E. A Narrative Review of Dietary Assessment Tools for Preschool-Aged Children in the Home Environment. Nutrients 2022, 14, 4793. https://doi.org/10.3390/nu14224793
Bellows LL, Lou Y, Nelson R, Reyes LI, Brown RC, Mena NZ, Boles RE. A Narrative Review of Dietary Assessment Tools for Preschool-Aged Children in the Home Environment. Nutrients. 2022; 14(22):4793. https://doi.org/10.3390/nu14224793
Chicago/Turabian StyleBellows, Laura L., Yuanying Lou, Rachel Nelson, Ligia I. Reyes, Renae C. Brown, Noereem Z. Mena, and Richard E. Boles. 2022. "A Narrative Review of Dietary Assessment Tools for Preschool-Aged Children in the Home Environment" Nutrients 14, no. 22: 4793. https://doi.org/10.3390/nu14224793
APA StyleBellows, L. L., Lou, Y., Nelson, R., Reyes, L. I., Brown, R. C., Mena, N. Z., & Boles, R. E. (2022). A Narrative Review of Dietary Assessment Tools for Preschool-Aged Children in the Home Environment. Nutrients, 14(22), 4793. https://doi.org/10.3390/nu14224793





