A Systematic Review and Meta-Analysis of the Impact of Different Intensity of Dietary Counselling on Cardiometabolic Health in Middle-Aged and Older Adults
Abstract
:1. Introduction
2. Materials and Methods
2.1. Registration
2.2. Search Strategy and Inclusion Criteria
2.3. Articles Selection and Data Extraction
2.4. Risk of Bias Assessment
2.5. Calculation and Statistical Analysis
3. Results
3.1. Study Selection and Subject Characteristics
3.2. Risk of Bias Assessment
3.3. Results of Systematic Review
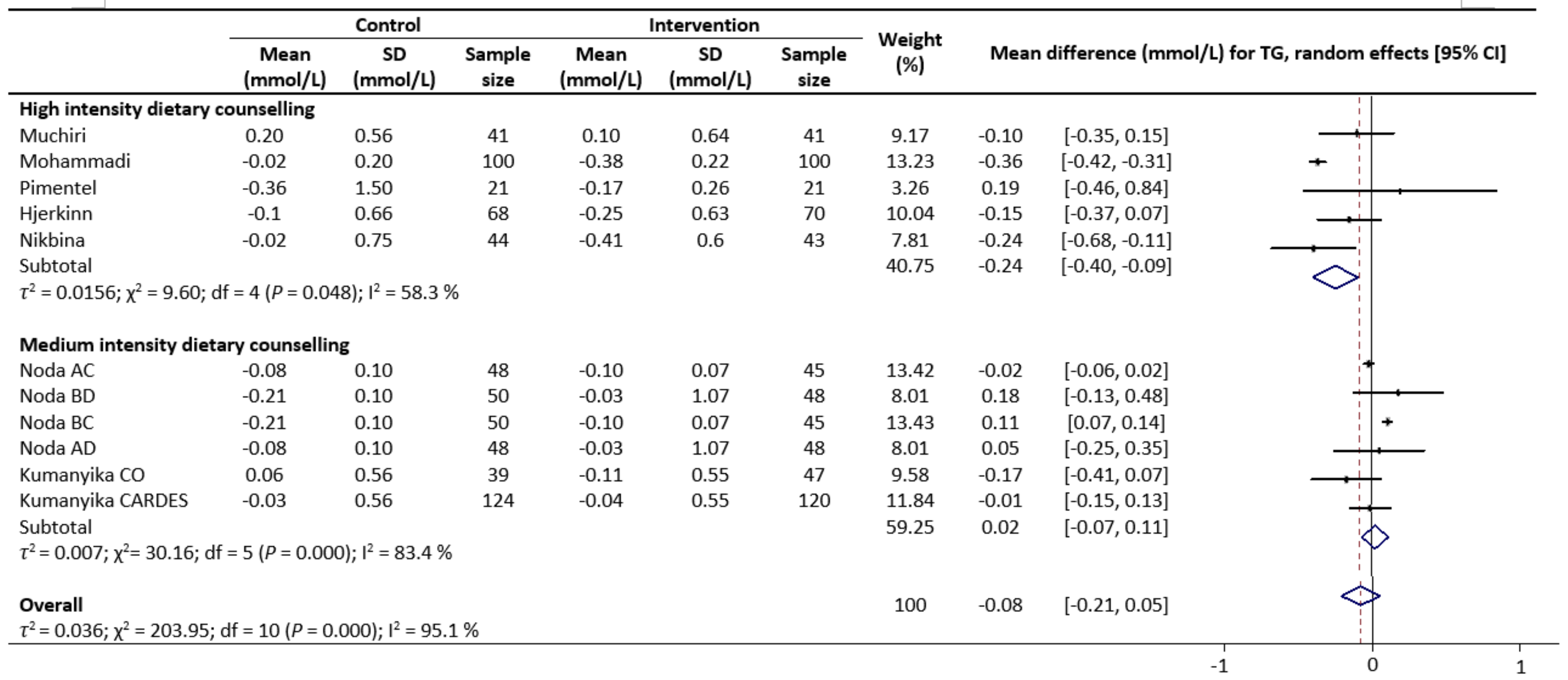
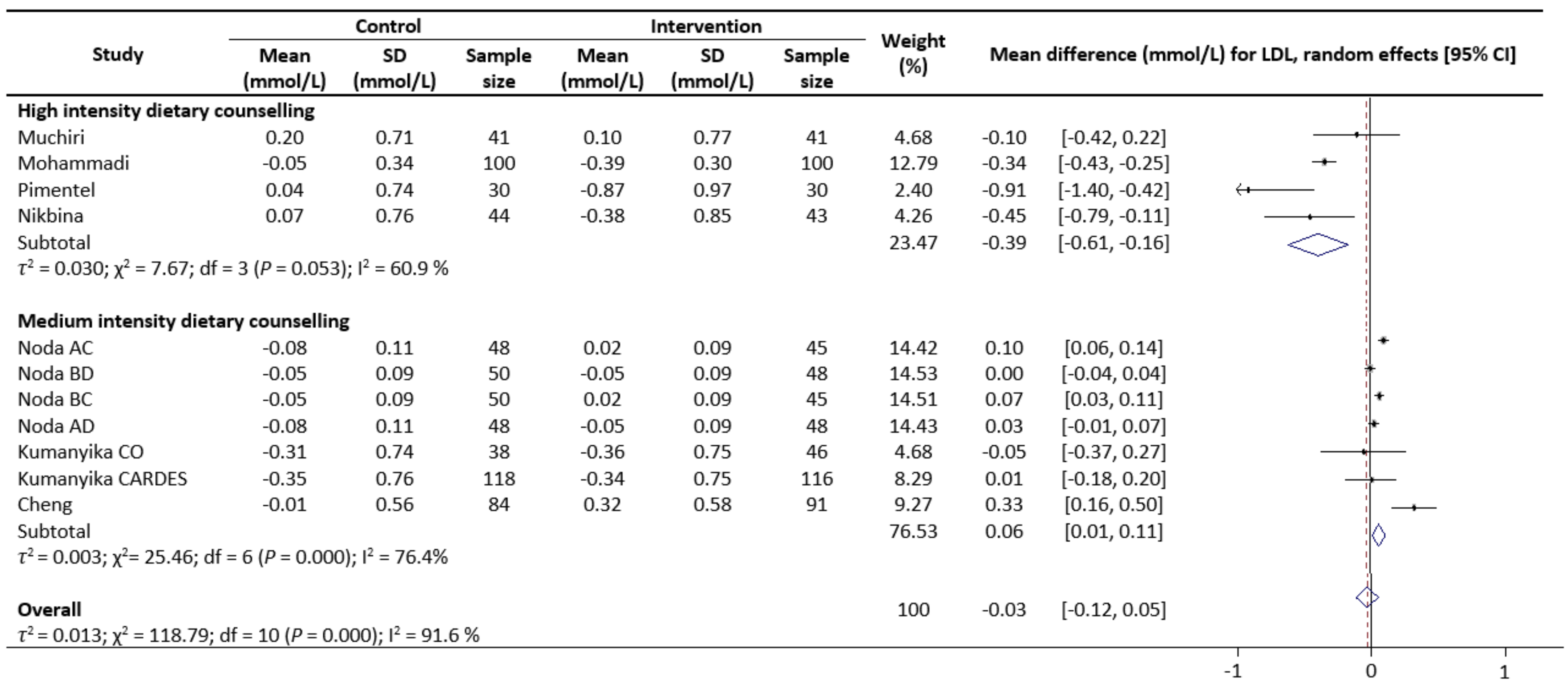
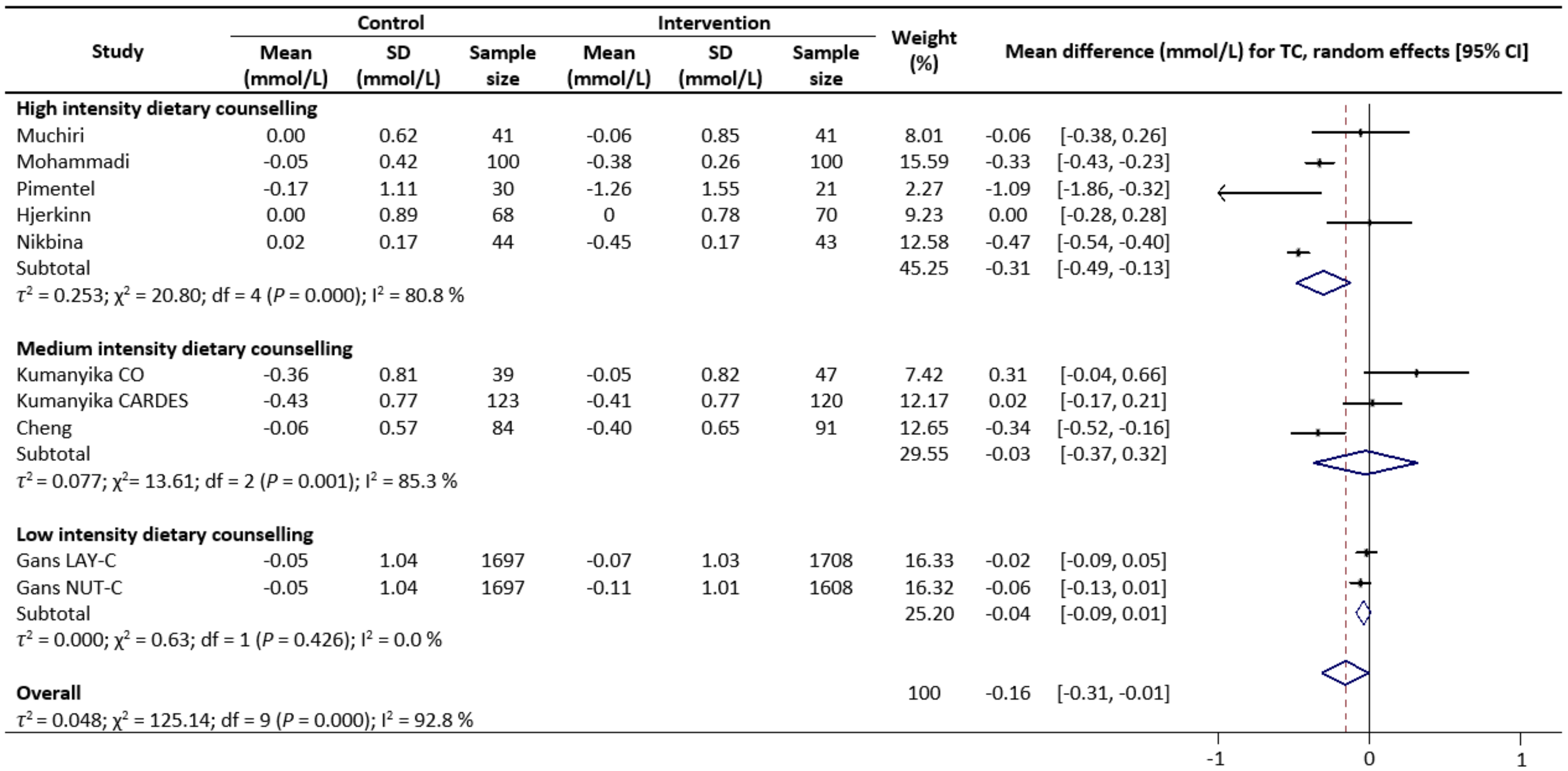
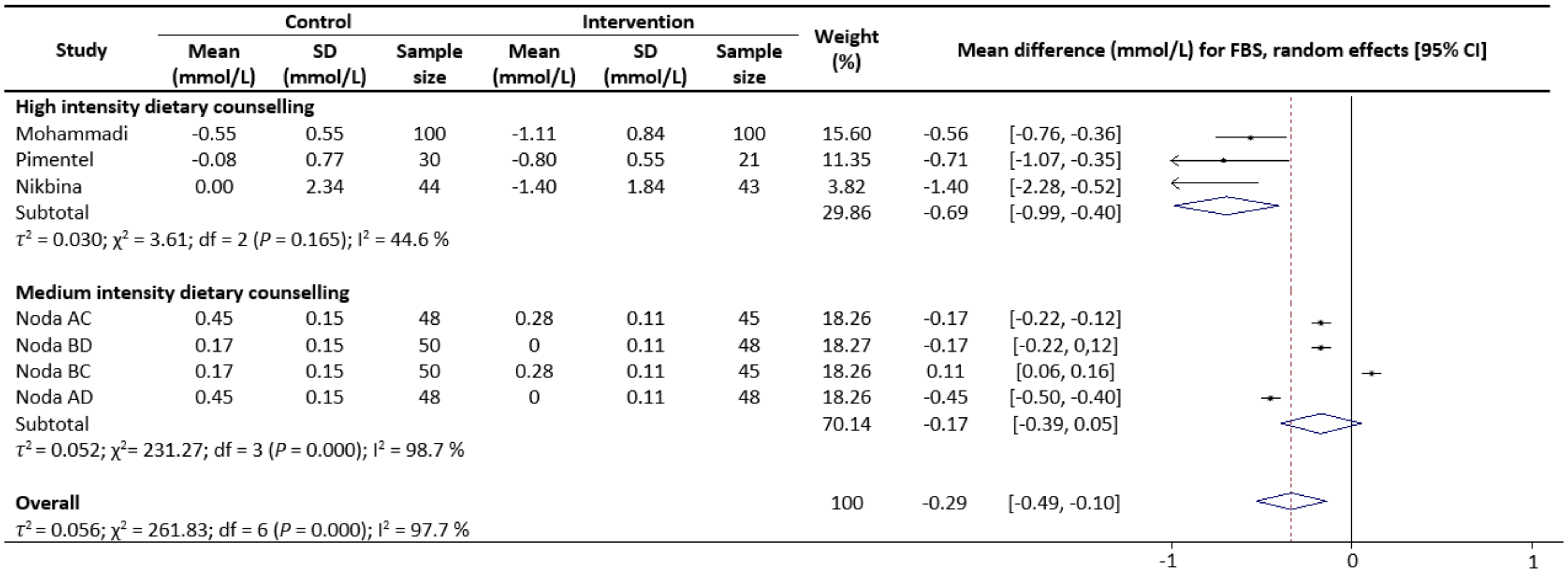
3.4. Results of Meta-Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- United Nations. World Population Ageing 2019; United Nations: New York, NY, USA, 2019. [Google Scholar]
- Machado-Oliveira, G.; Ramos, C.; Marques, A.R.A.; Vieira, O.V. Cell Senescence, Multiple Organelle Dysfunction and Atherosclerosis. Cells 2020, 9, 2146. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Tang, X.; Shen, P.; Si, Y.; Liu, X.; Xu, Z.; Wu, J.; Zhang, J.; Lu, P.; Lin, H.; et al. Multimorbidity of cardiometabolic diseases: Prevalence and risk for mortality from one million Chinese adults in a longitudinal cohort study. BMJ Open 2019, 9, e024476. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Reedy, J.; Krebs-Smith, S.M.; Miller, P.E.; Liese, A.D.; Kahle, L.L.; Park, Y.; Subar, A.F. Higher Diet Quality Is Associated with Decreased Risk of All-Cause, Cardiovascular Disease, and Cancer Mortality among Older Adults. J. Nutr. 2014, 144, 881–889. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwingshackl, L.; Hoffmann, G. Diet Quality as Assessed by the Healthy Eating Index, the Alternate Healthy Eating Index, the Dietary Approaches to Stop Hypertension Score, and Health Outcomes: A Systematic Review and Meta-Analysis of Cohort Studies. J. Acad. Nutr. Diet. 2015, 115, 780–800. [Google Scholar] [CrossRef]
- Xu, Z.; Steffen, L.M.; Selvin, E.; Rebholz, C.M. Diet quality, change in diet quality and risk of incident CVD and diabetes. Publ. Health Nutr. 2020, 23, 329–338. [Google Scholar] [CrossRef] [PubMed]
- Repas, T.B. Challenges and strategies in managing cardiometabolic risk. J. Am. Osteopath. Assoc. 2007, 107, 4–11. [Google Scholar]
- Esposito, K.; Pontillo, A.; Di Palo, C.; Giugliano, G.; Masella, M.; Marfella, R.; Giugliano, D. Effect of Weight Loss and Lifestyle Changes on Vascular Inflammatory Markers in Obese Women: A Randomized Trial. J. Am. Med. Assoc. 2003, 289, 1799–1804. [Google Scholar] [CrossRef] [Green Version]
- Yesilbursa, D.; Serdar, A.; Heper, Y.; Sarac, M.; Coskun, S.; Kazazoglu, A.R.; Cordan, J. The effect of orlistat-induced weight loss on interleukin-6 and C-reactive protein levels in obese subjects. Acta Cardiol. 2005, 60, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Monzillo, L.U.; Hamdy, O.; Horton, E.S.; Ledbury, S.; Mullooly, C.; Jarema, C.; Porter, S.; Ovalle, K.; Moussa, A.; Mantzoros, C.S. Effect of lifestyle modification on adipokine levels in obese subjects with insulin resistance. Obes. Res. 2003, 11, 1048–1054. [Google Scholar] [CrossRef] [Green Version]
- Grundy, S.M. Drug therapy of the metabolic syndrome: Minimizing the emerging crisis in polypharmacy. Nat. Rev. Drug Discov. 2006, 5, 295–309. [Google Scholar] [CrossRef]
- Vasiloglou, M.F.; Fletcher, J.; Poulia, K.A. Challenges and Perspectives in Nutritional Counselling and Nursing: A Narrative Review. J. Clin. Med. 2019, 8, 1489. [Google Scholar] [CrossRef] [Green Version]
- ADA Policy statement on licensure. J. Am. Diet. Assoc. 1991, 91, 985.
- Talib, R.; Ali, O.; Arshad, F.; Kadir, K.A. The effectiveness of group dietary counselling among non insulin dependent diabetes mellitus (NIDDM) patients in resettlement scheme areas in Malaysia. Asia Pac. J. Clin. Nutr. 1997, 6, 84–87. [Google Scholar]
- Nguyen, H.T.; Pavey, T.G.; Collins, P.F.; Nguyen, N.V.; Pham, T.D.; Gallegos, D. Effectiveness of Tailored Dietary Counseling in Treating Malnourished Outpatients with Chronic Obstructive Pulmonary Disease: A Randomized Controlled Trial. J. Acad. Nutr. Diet. 2020, 120, 778–791. [Google Scholar] [CrossRef]
- Ross, L.J.; Barnes, K.A.; Ball, L.E.; Mitchell, L.J.; Sladdin, I.; Lee, P.; Williams, L.T. Effectiveness of dietetic consultation for lowering blood lipid levels in the management of cardiovascular disease risk: A systematic review and meta-analysis of randomised controlled trials. Nutr. Diet. 2019, 76, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Razaz, J.M.; Rahmani, J.; Varkaneh, H.K.; Thompson, J.; Clark, C.; Abdulazeem, H.M. The health effects of medical nutrition therapy by dietitians in patients with diabetes: A systematic review and meta-analysis: Nutrition therapy and diabetes. Prim. Care Diabetes 2019, 13, 399–408. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.C.S.; Wang, H.H.X.; Kwan, M.W.M.; Fong, B.C.Y.; Chan, W.M.; Zhang, D.X.; Li, S.T.S.; Yan, B.P.; Coats, A.J.S.; Griffiths, S.M. Dietary counselling has no effect on cardiovascular risk factors among Chinese Grade 1 hypertensive patients: A randomized controlled trial. Eur. Heart J. 2015, 36, 2598–2607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lin, J.S.; O’Connor, E.; Whitlock, E.P.; Beil, T.L. Behavioral counseling to promote physical activity and a healthful diet to prevent cardiovascular disease in adults: A systematic review for the U.S. Preventive Services Task Force. Ann. Intern. Med. 2010, 153, 736–750. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Decoster, J.; Hall, G.P. Meta-Analysis Notes; University of Alabama: Tuscaloosa, AL, USA, 2004. [Google Scholar]
- Higgins, J.P.T.; Altman, D.G. Assessing Risk of Bias in Included Studies. Cochrane Handb. Syst. Rev. Interv. 2008, 187–241. [Google Scholar] [CrossRef]
- Mohammadi, S.; Karim, N.A.; Talib, R.A.; Amani, R. The impact of self-efficacy education based on the health belief model in Iranian patients with type 2 diabetes: A randomised controlled intervention study. Asia Pac. J. Clin. Nutr. 2018, 27, 546–555. [Google Scholar] [CrossRef]
- Deeks, J.J.; Higgins, J.P.; Altman, D.G. Analysing Data and Undertaking Meta-Analyses. Cochrane Handb. Syst. Rev. Interv. Cochrane B Ser. 2008, 243–296. [Google Scholar] [CrossRef]
- Ammerman, A.; Pignone, M.; Fernandez, L.; Lohr, K.; Jacobs, A.D.; Nester, C.; Orleans, T.; Pender, N.; Woolf, S.; Sutton, S.F.; et al. Counseling to Promote a Healthy Diet. Agency Healthc. Res. Qual. 2002, 18, 40–55. [Google Scholar]
- Lindgarde, F. The effect of orlistat body weight and coronary heart disease risk profile in obese patients: The swedish multimorbidity study. J. Intern. Med. 2000, 248, 245–254. [Google Scholar] [CrossRef]
- Al-Shookri, A.; Khor, G.L.; Chan, Y.M.; Loke, S.C.; Al-Maskari, M. Effectiveness of medical nutrition treatment delivered by dietitians on glycaemic outcomes and lipid profiles of Arab, Omani patients with Type 2 diabetes. Diabet. Med. 2012, 29, 236–244. [Google Scholar] [CrossRef]
- Thomson, C.A.; Stopeck, A.T.; Bea, J.W.; Cussler, E.; Nardi, E.; Frey, G.; Thompson, P.A. Changes in body weight and metabolic indexes in overweight breast cancer survivors enrolled in a randomized trial of low-fat vs. reduced carbohydrate diets. Nutr. Cancer 2010, 62, 1142–1152. [Google Scholar] [CrossRef] [PubMed]
- Klein, G.A.; Stefanuto, A.; Boaventura, B.C.B.; De Morais, E.C.; Da Cavalcante, L.S.; De Andrade, F.; Wazlawik, E.; Di Pietro, P.F.; Maraschin, M.; Da Silva, E.L. Mate Tea (Ilex paraguariensis) Improves Glycemic and Lipid Profiles of Type 2 Diabetes and Pre-Diabetes Individuals: A Pilot Study. J. Am. Coll. Nutr. 2011, 30, 320–332. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.; Graziani, C.; Diamond, J.J. Cholesterol-lowering effect of the Food for Heart Nutrition Education Program. J. Am. Diet. Assoc. 2004, 104, 1868–1872. [Google Scholar] [CrossRef] [PubMed]
- Kaliora, A.C.; Kokkinos, A.; Diolintzi, A.; Stoupaki, M.; Gioxari, A.; Kanellos, P.T.; Dedoussis, G.V.Z.; Vlachogiannakos, J.; Revenas, C.; Ladas, S.D.; et al. The effect of minimal dietary changes with raisins in NAFLD patients with non-significant fibrosis: A randomized controlled intervention. Food Funct. 2016, 7, 4533–4544. [Google Scholar] [CrossRef]
- Samuelsson, O.; Attman, P.O.; Knight-Gibson, C.; Kron, B.; Larsson, R.; Mulec, H.; Weiss, L.; Alaupovic, P. Effect of gemfibrozil on lipoprotein abnormalities in chronic renal insufficiency: A controlled study in human chronic renal disease. Nephron 1997, 75, 286–294. [Google Scholar] [CrossRef]
- Wu, H.L.; Sung, J.M.; Kao, M.D.; Wang, M.C.; Tseng, C.C.; Chen, S.T. Nonprotein Calorie Supplement Improves Adherence to Low-Protein Diet and Exerts Beneficial Responses on Renal Function in Chronic Kidney Disease. J. Ren. Nutr. 2013, 23, 271–276. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Li, Z.; Liu, Y.; Lv, X.; Yang, W. Effects of pistachios on body weight in Chinese subjects with metabolic syndrome. Nutr. J. 2012, 11, 20. [Google Scholar] [CrossRef] [Green Version]
- Hjerkinn, E.M.; Abdelnoor, M.; Breivik, L.; Bergengen, L.; Ellingsen, I.; Seljeflot, I.; Aase, O.; Klemsdal, T.O.; Hjermann, I.; Arnesen, H. Effect of diet or very long chain ω-3 fatty acids on progression of atherosclerosis, evaluated by carotid plaques, intima-media thickness and by pulse wave propagation in elderly men with hypercholesterolaemia. Eur. J. Prev. Cardiol. 2006, 13, 325–333. [Google Scholar] [CrossRef]
- Gans, K.M.; Burkholder, G.J.; Risica, P.M.; Harrow, B.; Lasater, T.M. Cost-effectiveness of minimal contact education strategies for cholesterol change. Ethn. Dis. 2006, 16, 443–451. [Google Scholar] [PubMed]
- Henkin, Y.; Shai, I.; Zuk, R.; Brickner, D.; Zuilli, I.; Neumann, L.; Shany, S. Dietary treatment of hypercholesterolemia: Do dietitians do it better? A randomized, controlled trial. Am. J. Med. 2000, 109, 549–555. [Google Scholar] [CrossRef]
- Meuleman, Y.; Hoekstra, T.; Dekker, F.W.; Navis, G.; Vogt, L.; van der Boog, P.J.M.; Bos, W.J.W.; van Montfrans, G.A.; van Dijk, S.; Boeschoten, E.W.; et al. Sodium Restriction in Patients With CKD: A Randomized Controlled Trial of Self-management Support. Am. J. Kidney Dis. 2017, 69, 576–586. [Google Scholar] [CrossRef] [Green Version]
- Nikbina, M.; Mameneh, M.; Bakaeian, M.; Dehcheshmeh, N.F. Effectiveness of nutrition education and counseling on metabolic control parameters of diabetes mellitus type 2 patients in primary health care centers. Clin. Diabetol. 2020, 9, 293–299. [Google Scholar] [CrossRef]
- Muchiri, J.W.; Gericke, G.J.; Rheeder, P. Effect of a nutrition education programme on clinical status and dietary behaviours of adults with type 2 diabetes in a resource-limited setting in South Africa: A randomised controlled trial. Public Health Nutr. 2016, 19, 142–155. [Google Scholar] [CrossRef] [Green Version]
- Noda, K.; Zhang, B.; Iwata, A.; Nishikawa, H.; Ogawa, M.; Nomiyama, T.; Miura, S.-I.; Sako, H.; Matsuo, K.; Yahiro, E.; et al. Lifestyle changes through the use of delivered meals and dietary counseling in a single-blind study-the STYLIST study. Circ. J. 2012, 76, 1335–1344. [Google Scholar] [CrossRef] [Green Version]
- Kumanyika, S.K.; Adams-Campbell, L.; Van Horn, B.; Ten Have, T.R.; Treu, J.A.; Askov, E.; Williams, J.; Achterberg, C.; Zaghloul, S.; Monsegu, D.; et al. Outcomes of a cardiovascular nutrition counseling program in African- Americans with elevated blood pressure or cholesterol level. J. Am. Diet. Assoc. 1999, 99, 1380–1388. [Google Scholar] [CrossRef]
- Takahashi, Y.; Sasaki, S.; Okubo, S.; Hayashi, M.; Tsugane, S. Blood pressure change in a free-living population-based dietary modification study in Japan. J. Hypertens. 2006, 24, 451–458. [Google Scholar] [CrossRef]
- Schwab, U.; Louheranta, A.; Törrönen, A.; Uusitupa, M. Impact of sugar beet pectin and polydextrose on fasting and postprandial glycemia and fasting concentrations of serum total and lipoprotein lipids in middle-aged subjects with abnormal glucose metabolism. Eur. J. Clin. Nutr. 2006, 60, 1073–1080. [Google Scholar] [CrossRef] [PubMed]
- Pimentel, G.D.; Portero-Mclellan, K.C.; Oliveira, É.P.; Spada, A.P.M.; Oshiiwa, M.; Zemdegs, J.C.S.; Barbalho, S.M. Long-term nutrition education reduces several risk factors for type 2 diabetes mellitus in Brazilians with impaired glucose tolerance. Nutr. Res. 2010, 30, 186–190. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Morán, M.; Guerrero-Romero, F.; Lazcano-Burciaga, G. Lipid-and glucose-lowering efficacy of Plantago Psyllium in type II diabetes. J. Diabetes Complicat. 1998, 12, 273–278. [Google Scholar] [CrossRef]
- Tan, X.; Alén, M.; Wang, K.; Tenhunen, J.; Wiklund, P.; Partinen, M.; Cheng, S. Effect of six-month diet intervention on sleep among overweight and obese men with chronic insomnia symptoms: A randomized controlled trial. Nutrients 2016, 8, 751. [Google Scholar] [CrossRef]
- Holland-Carter, L.; Tuerk, P.W.; Wadden, T.A.; Fujioka, K.N.; Becker, L.E.; Miller-Kovach, K.; Hollander, P.L.; Garvey, W.T.; Weiss, D.; Rubino, D.M.; et al. Impact on psychosocial outcomes of a nationally available weight management program tailored for individuals with type 2 diabetes: Results of a randomized controlled trial. J. Diabetes Complicat. 2017, 31, 891–897. [Google Scholar] [CrossRef] [PubMed]
- Britton, B.; Baker, A.L.; Wolfenden, L.; Wratten, C.; Bauer, J.; Beck, A.K.; McCarter, K.; Harrowfield, J.; Isenring, E.; Tang, C.; et al. Eating As Treatment (EAT): A Stepped-Wedge, Randomized Controlled Trial of a Health Behavior Change Intervention Provided by Dietitians to Improve Nutrition in Patients With Head and Neck Cancer Undergoing Radiation Therapy (TROG 12.03). Int. J. Radiat. Oncol. Biol. Phys. 2019, 103, 353–362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Munk, T.; Tolstrup, U.; Beck, A.M.; Holst, M.; Rasmussen, H.H.; Hovhannisyan, K.; Thomsen, T. Individualised dietary counselling for nutritionally at-risk older patients following discharge from acute hospital to home: A systematic review and meta-analysis. J. Hum. Nutr. Diet. 2016, 29, 196–208. [Google Scholar] [CrossRef]
- Tosti, V.; Bertozzi, B.; Fontana, L. Health Benefits of the Mediterranean Diet: Metabolic and Molecular Mechanisms. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2018, 73, 318–326. [Google Scholar] [CrossRef] [Green Version]
- Tyson, C.C.; Nwankwo, C.; Lin, P.H.; Svetkey, L.P. The dietary approaches to stop hypertension (dash) eating pattern in special populations. Curr. Hypertens. Rep. 2012, 14, 388–396. [Google Scholar] [CrossRef] [Green Version]
- Ndanuko, R.N.; Tapsell, L.C.; Charlton, K.E.; Neale, E.P.; Batterham, M.J. Dietary patterns and blood pressure in adults: A systematic review and meta-analysis of randomized controlled trials. Adv. Nutr. 2016, 7, 76–89. [Google Scholar] [CrossRef] [PubMed]
- Fukagawa, N.K.; Anderson, J.W.; Hageman, G.; Young, V.R.; Minaker, K.L. High-carbohydrate, high-fiber diets increase peripheral insulin sensitivity in healthy young and old adults. Am. J. Clin. Nutr. 1990, 52, 524–528. [Google Scholar] [CrossRef] [PubMed]
- Aleixandre, A.; Miguel, M. Dietary fiber and blood pressure control. Food Funct. 2016, 7, 1864–1871. [Google Scholar] [CrossRef] [PubMed]
- Tarray, R.; Saleem, S.; Afroze, D.; Yousuf, I.; Gulnar, A.; Laway, B.; Verma, S. Role of insulin resistance in essential hypertension. Cardiovasc. Endocrinol. 2014, 3, 129–133. [Google Scholar] [CrossRef]
- Cleland, S.J.; Petrie, J.R.; Ueda, S.; Elliott, H.L.; Connell, J.M. Insulin as a vascular hormone: Implications for the pathophysiology of cardiovascular disease. Clin. Exp. Pharmacol. Physiol. 1998, 25, 175–184. [Google Scholar] [CrossRef] [PubMed]
- Bessesen, D.H. The role of carbohydrates in insulin resistance. J. Nutr. 2001, 131, 2782S–2786S. [Google Scholar] [CrossRef]
- Brock, D.W.; Davis, C.K.; Irving, B.A.; Rodriguez, J.; Barrett, E.J.; Weltman, A.; Taylor, A.G.; Gaesser, G.A. A high-carbohydrate, high-fiber meal improves endothelial function in adults with the metabolic syndrome. Diabetes Care 2006, 29, 2313–2315. [Google Scholar] [CrossRef] [Green Version]
- Kobayashi, J.; Ohtake, K.; Uchida, H. No-rich diet for lifestyle-related diseases. Nutrients 2015, 7, 4911–4937. [Google Scholar] [CrossRef] [Green Version]
- Micha, R.; Mozaffarian, D. Saturated fat and cardiometabolic risk factors, coronary heart disease, stroke, and diabetes: A fresh look at the evidence. Lipids 2010, 45, 893–905. [Google Scholar] [CrossRef] [Green Version]
- Rasmussen, B.M.; Vessby, B.; Uusitupa, M.; Berglund, L.; Pedersen, E.; Riccardi, G.; Rivellese, A.A.; Tapsell, L.; Hermansen, K. Effects of dietary saturated, monounsaturated, and n-3 fatty acids on blood pressure in healthy subjects. Am. J. Clin. Nutr. 2006, 83, 221–226. [Google Scholar] [CrossRef]
- Rijnaarts, I.; De Roos, N.M.; Wang, T.; Zoetendal, E.G.; Top, J.; Timmer, M.; Bouwman, E.P.; Hogenelst, K.; Witteman, B.; De Wit, N. Increasing dietary fibre intake in healthy adults using personalised dietary advice compared with general advice: A single-blind randomised controlled trial. Public Health Nutr. 2021, 24, 1117–1128. [Google Scholar] [CrossRef]
- Brennan, C.S. Dietary fibre, glycaemic response, and diabetes. Mol. Nutr. Food Res. 2005, 49, 560–570. [Google Scholar] [CrossRef] [PubMed]
- Kritchevsky, D. Dietary fibre and lipid metabolism. Int. J. Obes. 1987, 11 (Suppl. 1), 33–43. [Google Scholar] [PubMed]
- Post, R.E.; Mainous, A.G.; King, D.E.; Simpson, K.N. Dietary fiber for the treatment of type 2 diabetes mellitus: A meta-analysis. J. Am. Board Fam. Med. 2012, 25, 16–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, C.; Zeng, Y.; Xu, J.; Zheng, H.; Liu, J.; Fan, R.; Zhu, W.; Yuan, L.; Qin, Y.; Chen, S.; et al. Therapeutic effects of soluble dietary fiber consumption on type 2 diabetes mellitus. Exp. Ther. Med. 2016, 12, 1232–1242. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaizu, S.; Kishimoto, H.; Iwase, M.; Fujii, H.; Ohkuma, T.; Ide, H.; Jodai, T.; Kikuchi, Y.; Idewaki, Y.; Hirakawa, Y.; et al. Impact of leisure-time physical activity on glycemic control and cardiovascular risk factors in Japanese patients with type 2 diabetes mellitus: The Fukuoka Diabetes Registry. PLoS ONE 2014, 9, e98768. [Google Scholar] [CrossRef] [Green Version]
- Van Amelsvoort, J.M.M.; Van Der Beek, A.; Stam, J.J. Effects of the type of dietary fatty acid on the insulin receptor function in rat epididymal fat cells. Ann. Nutr. Metab. 1986, 30, 273–280. [Google Scholar] [CrossRef]
- Field, C.J.; Ryan, E.A.; Thomson, A.B.; Clandinin, M.T. Diet fat composition alters membrane phospholipid composition, insulin binding, and glucose metabolism in adipocytes from control and diabetic animals. J. Biol. Chem. 1990, 265, 11143–11150. [Google Scholar] [CrossRef]
- Rees, K.; Dyakova, M.; Wilson, N.; Ward, K.; Thorogood, M.; Brunner, E. Dietary advice for reducing cardiovascular risk. Cochrane Database Syst. Rev. 2013, 2013. [Google Scholar] [CrossRef] [Green Version]
- Sialvera, T.E.; Papadopoulou, A.; Efstathiou, S.P.; Trautwein, E.A.; Ras, R.T.; Kollia, N.; Farajian, P.; Goumas, G.; Dimakopoulos, I.; Papavasiliou, K.; et al. Structured advice provided by a dietitian increases adherence of consumers to diet and lifestyle changes and lowers blood low-density lipoprotein (LDL)-cholesterol: The Increasing Adherence of Consumers to Diet & Lifestyle Changes to Lower (LDL) Cholester. J. Hum. Nutr. Diet. 2018, 31, 197–208. [Google Scholar] [CrossRef]
- Weickert, M.; Möhlig, M.; Schöfl, C.; Arafat, A.; Otto, B.; Viehoff, H.; Koebnick, C.; Kohl, A.; Spranger, J.; Pfeiffer, A. Cereal fiber improves whole-body insulin. Diabetes Care 2006, 29, 773–780. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodgers, J.L.; Jones, J.; Bolleddu, S.I.; Vanthenapalli, S.; Rodgers, L.E.; Shah, K.; Karia, K.; Panguluri, S.K. Cardiovascular Risks Associated with Gender and Aging. J. Cardiovasc. Dev. Dis. 2019, 6, 19. [Google Scholar] [CrossRef] [Green Version]
- Houston, K.A. Systematic Review of Literature on the Effectiveness of Behavioral Weight Loss Programs to Achieve Weight Reduction. J. Obes. Weight Loss Ther. 2012, 3, 2. [Google Scholar] [CrossRef]
- Baldwin, C.; Weekes, C.E. Dietary counselling with or without oral nutritional supplements in the management of malnourished patients: A systematic review and meta-analysis of randomised controlled trials. J. Hum. Nutr. Diet. 2012, 25, 411–426. [Google Scholar] [CrossRef]
- Bauer, J.; Isenring, E.; Ferguson, M. Dietary counseling: Evidence in chemotherapy patients. J. Support. Oncol. 2008, 6, 354–355, author reply 355. [Google Scholar] [PubMed]
- Folsom, A.R. Classical and Novel Biomarkers for Cardiovascular Risk Prediction in the United States. J. Epidemiol. 2013, 23, 158–162. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Variable | Description |
|---|---|
| Population | Adults mean aged ≥50 years old |
| Intervention | Groups that underwent dietary counselling |
| Comparator | Groups that did not go through dietary counselling |
| Outcome | Changes in TC, TG, HDL, LDL, FBS and insulin concentrations, SBP and DBP levels |
| Study Design | Randomised Controlled Trials |
| Research Question | Does the intensity of dietary counselling impact on the cardiometabolic health in middle-aged and older adults? |
| First Author, Year | Country of Study, Intervention Duration (Weeks) | Population Size, Description, Mean Age (Years), BMI (kg/m2) | Characteristics of Intervention Group (Provider; Number of Visit; Length of Visit (Minutes); Content) | Characteristics of Control Group (Provider; Number of Visit; Length of Visit (Minutes); Content) | Dietary Compliance | Attrition Rate (%) | Outcomes Measured |
|---|---|---|---|---|---|---|---|
| Kaliora [31], 2016 | Greece, 24 | 55, Men and women with NAFLD, 52, 29.1 | Dietitian; NR; NR; Received dietary counselling on calorie restriction | Nil | Monitored via non-scheduled phone calls with 24-h dietary recall | 20.0 | TC, TG, LDL, HDL, SBP, DBP, FBS, Insulin |
| Muchiri [40], 2016 | South Africa, 48 | 82, Men and women with type 2 diabetes, 59, 31.5 | Dietitian and Research staff; 8; 120; Received educational materials and took part in nutritional education programme | Dietitian; 1; Not applicable; Received educational materials only and usual medical care. | Follow-up sessions (four monthly meetings and two bi-monthly meetings each lasting 90 min) | 7.3 | TC, LDL, HDL, TG, SBP DBP |
| Wu [33], 2013 | Taiwan, 24 | 135, Men and women with chronic kidney disease, NR | Registered Dietitian; 6; NR; Received dietary counselling as recommended by the Kidney Disease Outcomes Quality Initiative nutritional guidelines and consumed a packet of non-protein calorie supplement | Registered Dietitian; 6; NR; Received dietary counselling as recommended by the Kidney Disease Outcomes Quality Initiative nutritional guidelines | NR | 19.3 | TC, TG, LDL, HDL |
| Al-Shookri [27], 2012 | Oman, 24 | 100, Men and women with type 2 diabetes, 52, 28.4 | Dietitian; 3; 150; Received practice guidelines nutritional care for T2DM | Dietitian; 1; 60; Received usual nutritional care | If goals and behavioural objectives of educations are not met, a second follow-up appointment would be scheduled | 15.0 | TC, TG, LDL, HDL, FBS |
| Noda [41], 2012 | Japan, 4 | 200, Men and women with type 2 diabetes, 65, 26.2 | Registered Dietitian; 4; 30–60; Face to face dietary counselling on | Nil | 1 telephone counselling lasting 10–20 min in between study where the dietary performance is checked by the dietitian. | 6.5 | TG, HDL, LDL, SBP, DBP, FBS |
| Wang [34] 2012 | China, 12 | 90, Men and women with metabolic syndrome, 51, 28 | Research staff; 5; NR; Received dietary counselling based on the American Heart Association Step I diet | Nil | A random phone call once every 2 weeks was conducted to check on compliance. | 4.4 | TC, TG, LDL, FBS, Insulin |
| Klein [29], 2011 | Brazil, 15 | 66, Men and women with type 2 diabetes and pre-diabetes, 60, 29.8 | Research staff; NR; NR; Dietary counselling to improve glycaemic and lipid profiles based on the Brazilian and American Diabetes Associations guidelines | Nil | 3-day food record was collected during baseline and throughout study periods. | 12.1 | TC, TG, LDL, HDL |
| Pimentel [45], 2010 | Brazil, 48 | 67, Men and women who are at high risk of type 2 diabetes, 60, 28 | Nutritionists; 36; 30–90; Individual and group counselling session including written and oral didactic instructions to improve diet quality | Nil | NR | 23.9 | TC, TG, LDL, HDL, FBS, Insulin |
| Thomson [28], 2010 | United States, 24 | 40; overweight postmenopausal breast cancer survivors, 56, 31.8 | Dietitian; 6; 45; Face to face dietary counselling for either low-fat or low-carbohydrate diet | Nil | A review of gram intake log and a 24-h recall to assess adherence to targeted diet. | 0.0 | TC, TG, LDL, HDL, SBP, DBP, FBS, Insulin |
| Gans [36], 2006 | England, 24 | 10,144, NR, 50, 26.9 | Trained lay person or Nutritionist; 1; 10–12; Dietary counselling provided according to the National Cholesterol Education Program | Received feedback tips sheet only OR Received tip sheet plus Rate Your Plate OR Received all materials along with CD audio intervention | Follow-up and assessed at baseline, 3 months, and 12 months. | NR | TC |
| Hjerkinn [35], 2006 | Europe, 144 | 278, Men with high cardiovascular risks, 70, 26.5 | Clinical nutritionist; 6; 30–45; Dietary counselling provided according to the European guidelines | Nil | Additional follow-up for subjects with poor adherence. | 15.1 | TC, TG, HDL, SBP, DBP |
| Schwab [44], 2006 | Finland, 12 | 68, Men and women with type 2 diabetes, 53, 28.8 | Nutritionist; 4; NR; Dietary counselling aimed to meet the generally recommended dietary goals for the prevention of cardiovascular diseases | Nil | 4-day food record was kept monitoring food intake during the third and the seventh week for personal nutrition counselling. | 2.9 | TC, TG, LDL, HDL, SBP, DBP, FBS |
| Takahashi [43], 2006 | Japan, 48 | 550, Generally healthy men and women, 56, 23.4 | Research staff; 4; 15; Individual and group session with individualized dietary counselling | Research staff; 1; 15; Tailored dietary education | A second dietary assessment was performed, and the same individual dietary counselling was given to each subject. | 18.5 | SBP, DBP |
| Cheng [30], 2004 | United States, 16 | 208, Men and women who are hypercholesterolemic, 54, 31.8 | Research assistant; 4; 5–50; Received nutrition counselling using the Food For Heart Program curriculum | Nil | Every visit featured a quiz and advice sheets for each subject individually and a dietary risk assessment completed for all visits | 15.9 | TC, LDL, HDL |
| Lindgärde [26], 2001 | Sweden, 54 | 382, Men and women with at least one of the obesity-associated CHD risk factors, 53, 33.2 | Practice nurse; 8; NR; Self-help weight control educational package with leaflets and videotape | Nil | Each visit subjects have to update on their frequency of watching the video | 1.6 | SBP, DBP, TC, TG, LDL, HDL, FBS |
| Henkin [37], 2000 | Israel, 48 | 136, Men and women with hyper cholesterol, 50, 27 136, Men and women with hyper cholesterol, 51, 26 | Physicians and Dietitians; 1; 30; Counselling focused on smoking cessation, physical activity, weight control, and dietary modifications conforming to the Step I diet Physicians and Dietitians; 2–4; 30; Face to face dietary counselling session on general information about hyper- cholesterolemia, guidelines, as well as specific dietary recommendations | Nil | 3-day food diary Detailed analysis of nutrient intake and eating habits guided by 3-day food diary and provision of more specific dietary recommendations. | 13.2 | TC, TG, LDL, HDL |
| Kumanyika [42], 1999 | United States, 48 | 330, Men and women with either hypercholesterolemia or hypertension, NR, NR | Nutritionist; 4; NR; Received baseline counselling using the Cardiovascular Dietary Education System which aimed to educate about cardiovascular disease | Nutritionist; NR; NR; Received baseline counselling | Followed-up visits was given to reinforce self-directed learning. | 22.7 | TG, TC, LDL, HDL |
| Rodríguez-Morán [46], 1998 | Mexico, 12 | 60, Men and women with type 2 diabetes, 57, 28.6 | Research staff; NR; NR; NR | Nil | NR | 0.0 | TC, TG, LDL, HDL |
| Samuelsson [32], 1997 | Sweden, 48 | 28, Men and women with non-diabetic primary renal disease and moderately advanced renal insufficiency, 50, 26.9 | Dietitian; NR; NR; Received tailored dietary counselling for diabetes | Nil | Telephone follow-up after 1 month | 10.7 | TC, TG, LDL, HDL, vLDL |
| Nikbina [39], 2020 | Iran, 16 | 90, Men and women with type 2 diabetes, 52, NR | Nutritionist; 5; 45–90; Educational content included healthy nutrition that focused on balance, diversity and diet, proper food replacement technique, how to use the healthy eating plate and cook healthy food | Received only routine care | Telephone follow-up over a period of 4 months on a weekly basis conducted by a nutritionist | 3.3 | SBP, DBP, TC, TG, LDL, HDL, FBS |
| Mohammadi [23], 2018 | Iran, 12 | 240, Men and women with type 2 diabetes, 51, 27 | Researcher; 8; 120; Received dietary counselling and education booklet, complications, self-care and self-efficacy behaviour, physical activity, healthy diet, medication adherence and to self-monitor their blood glucose level | Researcher; NR; NR; Received conventional dietary counselling with no additional details | NR | 16.7 | TC, TG, LDL, HDL, FBS |
| Meuleman [38], 2017 | Netherlands, 24 | 151, men and women with moderately decreased kidney functions, 55; 29.7 | Dietitian; 2; 60; Received regular care according to the Dutch Federation of Nephrology treatment guidelines and self-management intervention with personal coaches including psychologists | Received only regular care according to the Dutch Federation of Nephrology treatment guidelines | Feedbacks via telephone from coach to discuss progression, achievements, barriers, and possible solutions | 8.6 | SBP, DBP |
| Outcome (Unit) | Post | Change | ||
|---|---|---|---|---|
| Control | Intervention | Control | Intervention | |
| TC (mmol/L) | 5.25 | 5.41 | −0.10 | −0.19 |
| [4.23, 5.94] | [4.25, 6.24] | [−0.36, 0.02] | [−1.26, 0.17] | |
| TG (mmol/L) | 1.76 | 1.85 | −0.10 | −0.11 |
| [1.49, 2.16] | [0.95, 4.76] | [−0.42, 0.20] | [−0.41, 0.18] | |
| LDL (mmol/L) | 3.16 | 3.34 | −0.12 | −0.15 |
| [2.65, 4.09] | [2.49, 4.62] | [−0.36, 0.07] | [−0.88, 0.37] | |
| HDL (mmol/L) | 1.25 | 1.31 | −0.01 | 0.06 |
| [1.02, 1.44] | [0.91, 1.63] | [−0.09 0.10] | [−0.11, 0.20] | |
| SBP (mmHg) | 136.7 | 132.0 | −0.10 | −4.86 |
| [128.5, 143] | [121.8, 142] | [−5.00, 4.00] | [−11.80, −0.80] | |
| DBP (mmHg) | 81.0 | 78.9 | −0.94 | −2.94 |
| [75.9, 89.0] | [74.8, 85.1] | [−4.00, 1.00] | [−7.50, 1.60] | |
| Glucose (mmol/L) | 7.00 | 6.76 | −0.02 | −0.39 |
| [5.05, 9.17] | [5.08, 11.90] | [−0.08, 0.02] | [−2.05, 0.32] | |
| Insulin (μU/mL) a | 14.5 | 14.6 | −1.10 | −1.43 |
| - | [11.40, 18.70] | - | [−4.50, 1.93] | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Low, J.H.M.; Toh, D.W.K.; Ng, M.T.T.; Fam, J.; Kua, E.H.; Kim, J.E. A Systematic Review and Meta-Analysis of the Impact of Different Intensity of Dietary Counselling on Cardiometabolic Health in Middle-Aged and Older Adults. Nutrients 2021, 13, 2936. https://doi.org/10.3390/nu13092936
Low JHM, Toh DWK, Ng MTT, Fam J, Kua EH, Kim JE. A Systematic Review and Meta-Analysis of the Impact of Different Intensity of Dietary Counselling on Cardiometabolic Health in Middle-Aged and Older Adults. Nutrients. 2021; 13(9):2936. https://doi.org/10.3390/nu13092936
Chicago/Turabian StyleLow, Jasmine Hui Min, Darel Wee Kiat Toh, Magdeline Tao Tao Ng, Johnson Fam, Ee Heok Kua, and Jung Eun Kim. 2021. "A Systematic Review and Meta-Analysis of the Impact of Different Intensity of Dietary Counselling on Cardiometabolic Health in Middle-Aged and Older Adults" Nutrients 13, no. 9: 2936. https://doi.org/10.3390/nu13092936






