Assessment of Sarcopenia in the Intensive Care Unit and 1-Year Mortality in Survivors of Critical Illness
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Setting and Populations
2.2. Data Collection
2.3. Ultrasound Measurement
2.4. Definition of Sarcopenia in the ICU
2.5. Endpoints
2.6. Statistical Methods
3. Results
3.1. Patient Characteristics
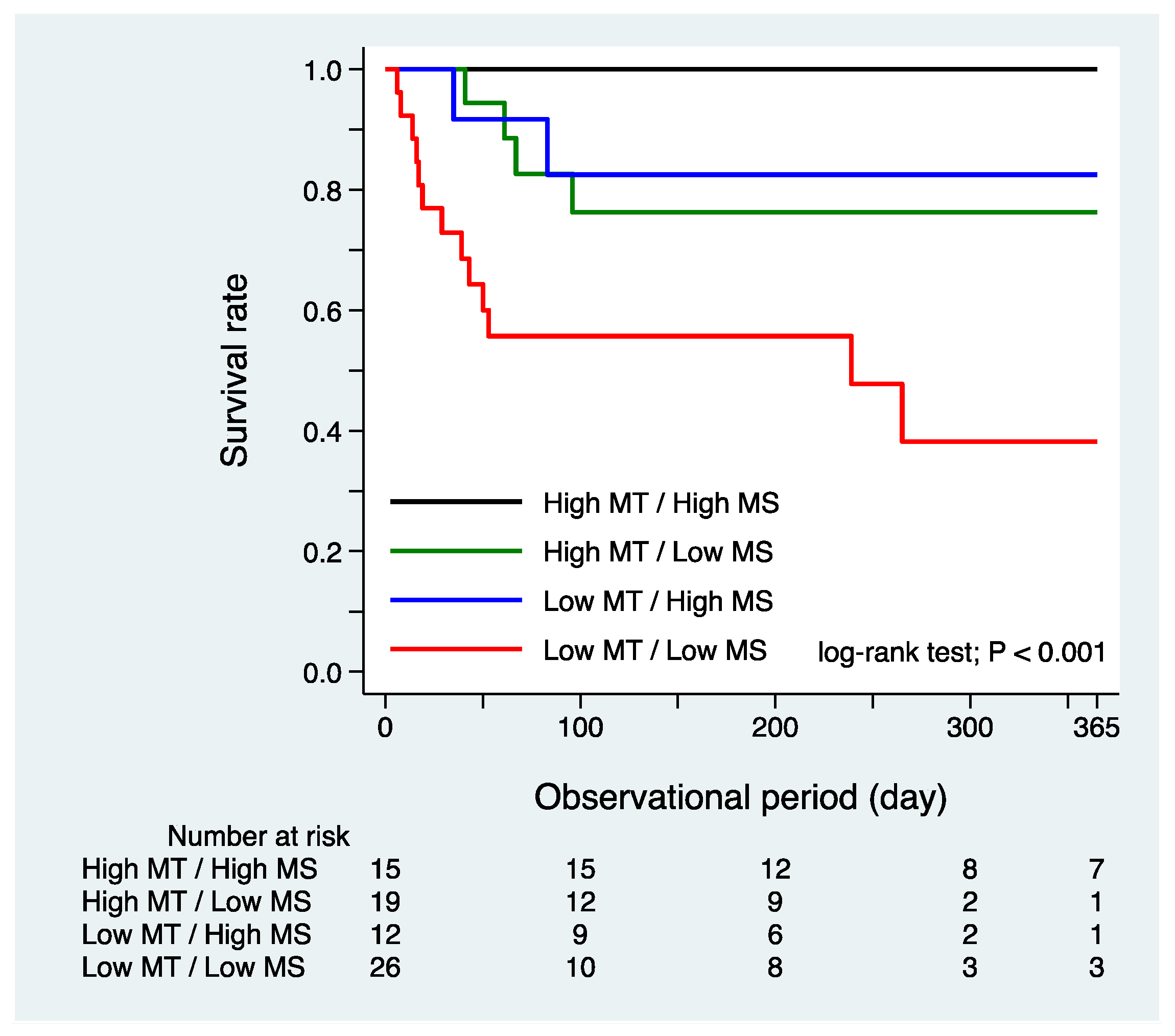
3.2. Sarcopenia in the ICU and 1-Year Mortality
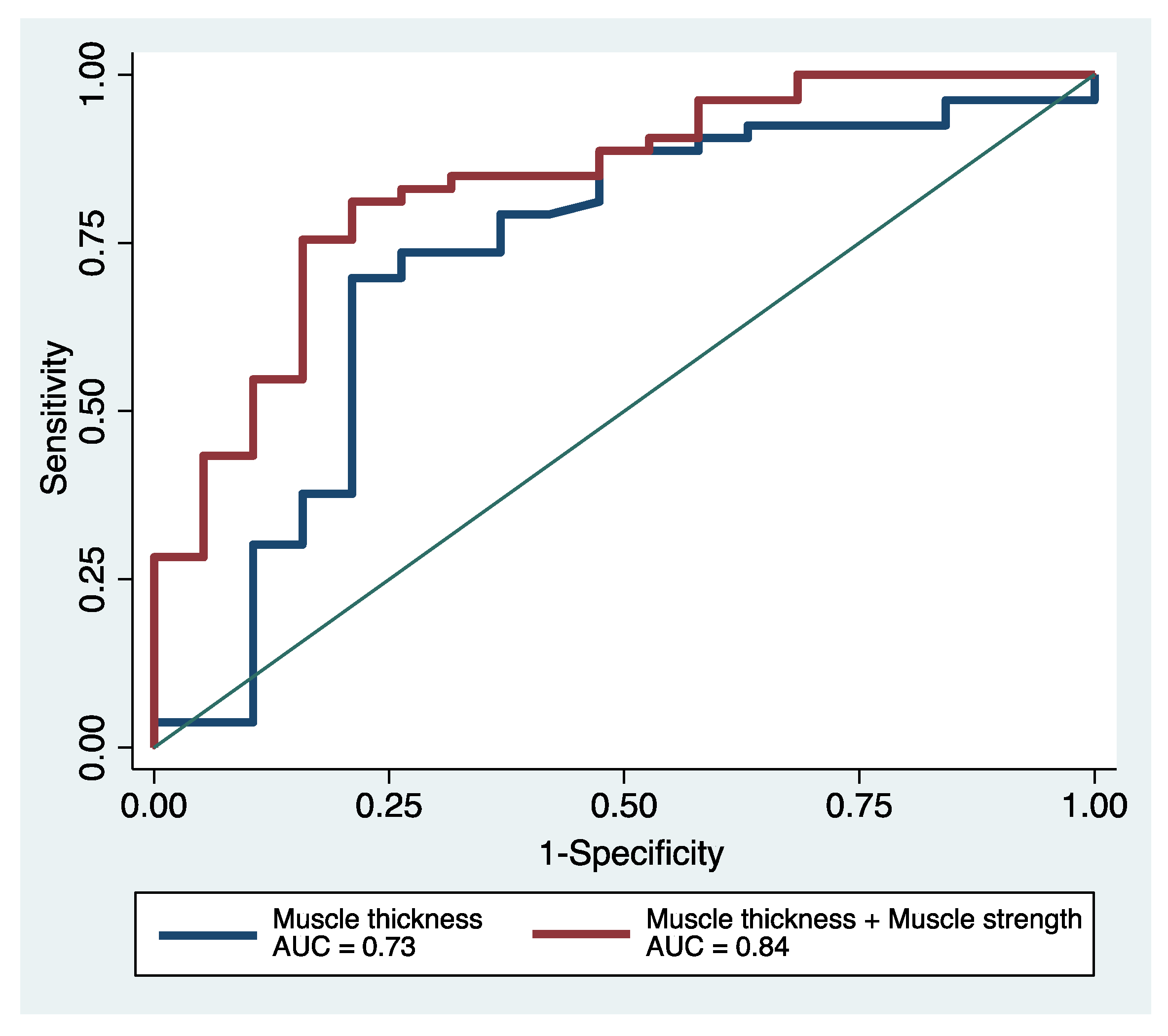
3.3. Additive Prognostic Predictive Capabilities of Sarcopenia Assessment in the ICU
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Kress, J.P.; Hall, J.B. ICU-acquired weakness and recovery from critical illness. N. Engl. J. Med. 2014, 370, 1626–1635. [Google Scholar] [CrossRef] [Green Version]
- Wieske, L.; Dettling-Ihnenfeldt, D.S.; Verhamme, C.; Nollet, F.; van Schaik, I.N.; Schultz, M.J.; Horn, J.; van der Schaaf, M. Impact of ICU-acquired weakness on post-ICU physical functioning: A follow-up study. Crit. Care 2015, 19, 196. [Google Scholar] [CrossRef] [Green Version]
- Van Aerde, N.; Meersseman, P.; Debaveye, Y.; Wilmer, A.; Gunst, J.; Casaer, M.P.; Bruyninckx, F.; Wouters, P.J.; Gosselink, R.; Van den Berghe, G.; et al. Five-year impact of ICU-acquired neuromuscular complications: A prospective, observational study. Intensive Care Med. 2020, 46, 1184–1193. [Google Scholar] [CrossRef]
- Puthucheary, Z.A.; Rawal, J.; McPhail, M.; Connolly, B.; Ratnayake, G.; Chan, P.; Hopkinson, N.S.; Padhke, R.; Dew, T.; Sidhu, P.S.; et al. Acute skeletal muscle wasting in critical illness. JAMA 2013, 310, 1591–1600. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weijs, P.J.; Looijaard, W.G.; Dekker, I.M.; Stapel, S.N.; Girbes, A.R.; Straaten, H.M.O.-V.; Beishuizen, A. Low skeletal muscle area is a risk factor for mortality in mechanically ventilated critically ill patients. Crit. Care 2014, 18, R12. [Google Scholar] [CrossRef] [Green Version]
- Jaitovich, A.; Dumas, C.L.; Itty, R.; Chieng, H.C.; Khan, M.M.H.S.; Naqvi, A.; Fantauzzi, J.; Hall, J.B.; Feustel, P.J.; Judson, M.A. ICU admission body composition: Skeletal muscle, bone, and fat effects on mortality and disability at hospital discharge-a prospective, cohort study. Crit. Care 2020, 24, 566. [Google Scholar] [CrossRef]
- Schefold, J.C.; Wollersheim, T.; Grunow, J.J.; Luedi, M.M.; Z’Graggen, W.J.; Weber-Carstens, S. Muscular weakness and muscle wasting in the critically ill. J. Cachexia Sarcopenia Muscle 2020, 11, 1399–1412. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.K.; Woo, J.; Assantachai, P.; Auyeung, T.-W.; Chou, M.-Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus update on sarcopenia diagnosis and treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e2. [Google Scholar] [CrossRef] [PubMed]
- Cruz-Jentoft, A.J.; Sayer, A.A. Sarcopenia. Lancet 2019, 393, 2636–2646. [Google Scholar] [CrossRef]
- Mueller, N.; Murthy, S.; Tainter, C.R.; Lee, J.; Riddell, K.; Fintelmann, F.J.; Grabitz, S.D.; Timm, F.P.; Levi, B.; Kurth, T.; et al. Can Sarcopenia Quantified by Ultrasound of the Rectus Femoris Muscle Predict Adverse Outcome of Surgical Intensive Care Unit Patients as well as Frailty? A Prospective, Observational Cohort Study. Ann. Surg. 2016, 264, 1116–1124. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kashani, K.B.; Frazee, E.N.; Kukralova, L.; Sarvottam, K.; Herasevich, V.; Young, P.M.; Kashyap, R.; Lieske, J.C. Evaluating Muscle Mass by Using Markers of Kidney Function: Development of the Sarcopenia Index. Crit. Care Med. 2017, 45, e23–e29. [Google Scholar] [CrossRef] [PubMed]
- Toptas, M.; Yalcin, M.; Akkoc, I.; Demir, E.; Metin, C.; Savas, Y.; Kalyoncuoglu, M.; Can, M.M. The Relation between Sarcopenia and Mortality in Patients at Intensive Care Unit. Biomed. Res. Int. 2018, 2018, 5263208. [Google Scholar] [CrossRef] [PubMed]
- Kizilarslanoglu, M.C.; Kuyumcu, M.E.; Yesil, Y.; Halil, M. Sarcopenia in critically ill patients. J. Anesth. 2016, 30, 884–890. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gotzsche, P.C.; Vandenbroucke, J.P.; Initiative, S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS Med. 2007, 4, e296. [Google Scholar] [CrossRef] [Green Version]
- Banks, J.L.; Marotta, C.A. Outcomes validity and reliability of the modified Rankin Scale: Implications for stroke clinical trials: A literature review and synthesis. Stroke 2007, 38, 1091–1096. [Google Scholar] [CrossRef] [Green Version]
- Knaus, W.A.; Draper, E.A.; Wagner, D.P.; Zimmerman, J.E. Apache II: A severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef] [PubMed]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonça, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef] [PubMed]
- Vanpee, G.; Hermans, G.; Segers, J.; Gosselink, R. Assessment of limb muscle strength in critically ill patients: A systematic review. Crit. Care Med. 2014, 42, 701–711. [Google Scholar] [CrossRef]
- Sessler, C.N.; Gosnell, M.S.; Grap, M.J.; Brophy, G.M.; O’Neal, V.; Keane, K.A.; Tesoro, E.P.; Elswick, R.K. The Richmond Agitation-Sedation Scale: Validity and reliability in adult intensive care unit patients. Am. J. Respir. Crit. Care Med. 2002, 166, 1338–1344. [Google Scholar] [CrossRef]
- Fan, E.; Cheek, F.; Chlan, L.; Gosselink, R.; Hart, N.; Herridge, M.S.; Hopkins, R.O.; Hough, C.L.; Kress, J.P.; Latronico, N.; et al. A ATS Committee on ICU-acquired Weakness in Adults, American Thoracic Society ATS Committee: An official American Thoracic Society clinical practice guideline: The diagnosis of intensive care unit-acquired weakness in adults. Am. J. Respir. Crit. Care Med. 2014, 190, 1437–1446. [Google Scholar] [CrossRef]
- Rubin, D.B. Estimating causal effects from large data sets using propensity scores. Ann. Intern. Med. 1997, 127, 757–763. [Google Scholar] [CrossRef]
- Delong, E.R.; Delong, D.M.; Clarkepearson, D.I. Comparing the Areas under 2 or More Correlated Receiver Operating Characteristic Curves—A Nonparametric Approach. Biometrics 1988, 44, 837–845. [Google Scholar] [CrossRef]
- Pencina, M.J.; D’Agostino, R.B., Sr.; D’Agostino, R.B., Jr.; Vasan, R.S. Evaluating the added predictive ability of a new marker: From area under the ROC curve to reclassification and beyond. Stat. Med. 2008, 27, 157–172; discussion 112–207. [Google Scholar] [CrossRef] [PubMed]
- Kou, H.-W.; Yeh, C.-H.; Tsai, H.-I.; Hsu, C.-C.; Hsieh, Y.-C.; Chen, W.-T.; Cheng, H.-T.; Yu, M.-C.; Lee, C.-W. Sarcopenia is an effective predictor of difficult-to-wean and mortality among critically ill surgical patients. PLoS ONE 2019, 14, e0220699. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Joyce, P.R.; O’Dempsey, R.; Kirby, G.; Anstey, C. A retrospective observational study of sarcopenia and outcomes in critically ill patients. Anaesth. Intensive Care 2020, 48, 229–235. [Google Scholar] [CrossRef] [PubMed]
- De Jonghe, B.; Sharshar, T.; Lefaucheur, J.-P.; Authier, F.-J.; Durand-Zaleski, I.; Boussarsar, M.; Cerf, C.; Renaud, E.; Mesrati, F.; Carlet, J.; et al. Paresis Acquired in the Intensive Care Unit: A Prospective Multicenter Study. JAMA 2002, 288, 2859–2867. [Google Scholar] [CrossRef] [Green Version]
- Garnacho-Montero, J.; Madrazo-Osuna, J.; García-Garmendia, J.L.; Ortiz-Leyba, C.; Jiménez-Jiménez, F.J.; Barrero-Almodóvar, A.; Garnacho-Montero, M.C.; Moyano-Del-Estad, M.R. Critical Illness Polyneuropathy: Risk Factors and Clinical Consequences. A Cohort Study in Septic Patients. Intensive Care Med. 2001, 27, 1288–1296. [Google Scholar] [CrossRef]
- Yanagi, N.; Kamiya, K.; Hamazaki, N.; Matsuzawa, R.; Nozaki, K.; Ichikawa, T.; Valley, T.S.; Nakamura, T.; Yamashita, M.; Maekawa, E.; et al. Post-Intensive Care Syndrome as a Predictor of Mortality in Patients with Critical Illness: A Cohort Study. PLoS ONE 2021, 16, e0244564. [Google Scholar] [CrossRef]
- Parry, S.M.; El-Ansary, D.; Cartwright, M.S.; Sarwal, A.; Berney, S.; Koopman, R.; Annoni, R.; Puthucheary, Z.; Gordon, I.R.; Morris, P.E.; et al. Ultrasonography in the intensive care setting can be used to detect changes in the quality and quantity of muscle and is related to muscle strength and function. J. Crit. Care 2015, 30, e9–e1151. [Google Scholar] [CrossRef]
- Mayer, K.P.; Bastin, M.L.T.; Montgomery-Yates, A.A.; Pastva, A.M.; Dupont-Versteegden, E.E.; Parry, S.M.; Morris, P.E. Acute skeletal muscle wasting and dysfunction predict physical disability at hospital discharge in patients with critical illness. Crit. Care 2020, 24, 637. [Google Scholar] [CrossRef]
| Characteristics | Overall (n = 72) | |
|---|---|---|
| Age (years), median [IQR] | 70 | (60–76) |
| Male, n (%) | 57 | (79) |
| BMI (kg/m2), median [IQR] | 23.6 | (20.8–26.6) |
| Reason for ICU admission, n (%) | ||
| Sepsis | 23 | (32) |
| Cardiac surgery | 23 | (32) |
| Respiratory failure | 20 | (28) |
| Others | 6 | (8) |
| ICU LOS (days), median [IQR] | 8 | (4–12) |
| mRS prior to admission, median [IQR] | 2 | (1–2) |
| APACHE II score at admission, median [IQR] | 23 | (18–28) |
| Maximum SOFA score, median [IQR] | 11 | (8–14) |
| ECMO, n (%) | 4 | (6) |
| Noradrenaline, n (%) | 33 | (46) |
| MRC sum score, median [IQR] | 42 | (36–48) |
| Muscle thickness (mm), median [IQR] | 20.9 | (16.0–27.1) |
| Death, n (%) | 19 | (26) |
| Characteristics | High MT and MS (n = 15) | High MT and Low MS (n = 19) | Low MT and High MS (n = 12) | Low MT and Low MS (Sarcopenia) (n = 26) | p Value | ||||
|---|---|---|---|---|---|---|---|---|---|
| Age (years), median [IQR] | 60 | (51–74) | 70 | (53–73) | 70 | (62–73) | 73 | (69–77) | 0.051 |
| Male, n (%) | 11 | (73) | 16 | (84) | 9 | (75) | 21 | (81) | 0.857 |
| BMI (kg/m2), median [IQR] | 25.1 | (21.4–27.3) | 26.2 | (24.1–28.3) | 20.2 | (19.0–23.5) | 22.8 | (19.8–25.2) | 0.004 |
| Reason of ICU admission, n (%) | |||||||||
| Sepsis | 1 | (7) | 6 | (32) | 5 | (42) | 11 | (42) | 0.006 |
| Cardiac Surgery | 7 | (47) | 8 | (42) | 1 | (8) | 6 | (23) | 0.220 |
| Respiratory Failure | 4 | (27) | 3 | (16) | 2 | (17) | 7 | (27) | 0.795 |
| Others | 3 | (20) | 2 | (11) | 4 | (33) | 2 | (8) | 0.072 |
| ICU LOS (days), median [IQR] | 4 | (3–5) | 11 | (7–15) | 5 | (4–9) | 10 | (7–12) | 0.014 |
| mRS prior to admission, median [IQR] | 1 | (0–3) | 1 | (0–2) | 2 | (1–2) | 3 | (2–3) | 0.588 |
| APACHE II score at admission, median [IQR] | 21 | (10–26) | 24 | (9–13) | 22 | (19–26) | 23 | (19–26) | 0.164 |
| Maximum SOFA score, median [IQR] | 8 | (5–13) | 11 | (9–13) | 11 | (7–13) | 12 | (10–15) | 0.087 |
| ECMO, n (%) | 0 | (0) | 1 | (5) | 1 | (8) | 2 | (8) | 0.732 |
| Noradrenaline, n (%) | 2 | (13) | 8 | (42) | 7 | (58) | 16 | (62) | 0.016 |
| Death, n (%) | 0 | (0) | 4 | (21) | 2 | (17) | 13 | (50) | 0.002 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yanagi, N.; Koike, T.; Kamiya, K.; Hamazaki, N.; Nozaki, K.; Ichikawa, T.; Matsunaga, A.; Kuroiwa, M.; Arai, M. Assessment of Sarcopenia in the Intensive Care Unit and 1-Year Mortality in Survivors of Critical Illness. Nutrients 2021, 13, 2726. https://doi.org/10.3390/nu13082726
Yanagi N, Koike T, Kamiya K, Hamazaki N, Nozaki K, Ichikawa T, Matsunaga A, Kuroiwa M, Arai M. Assessment of Sarcopenia in the Intensive Care Unit and 1-Year Mortality in Survivors of Critical Illness. Nutrients. 2021; 13(8):2726. https://doi.org/10.3390/nu13082726
Chicago/Turabian StyleYanagi, Naoya, Tomotaka Koike, Kentaro Kamiya, Nobuaki Hamazaki, Kohei Nozaki, Takafumi Ichikawa, Atsuhiko Matsunaga, Masayuki Kuroiwa, and Masayasu Arai. 2021. "Assessment of Sarcopenia in the Intensive Care Unit and 1-Year Mortality in Survivors of Critical Illness" Nutrients 13, no. 8: 2726. https://doi.org/10.3390/nu13082726






