Family-Based Obesity Prevention Interventions among Hispanic Children and Families: A Scoping Review
Abstract
1. Introduction
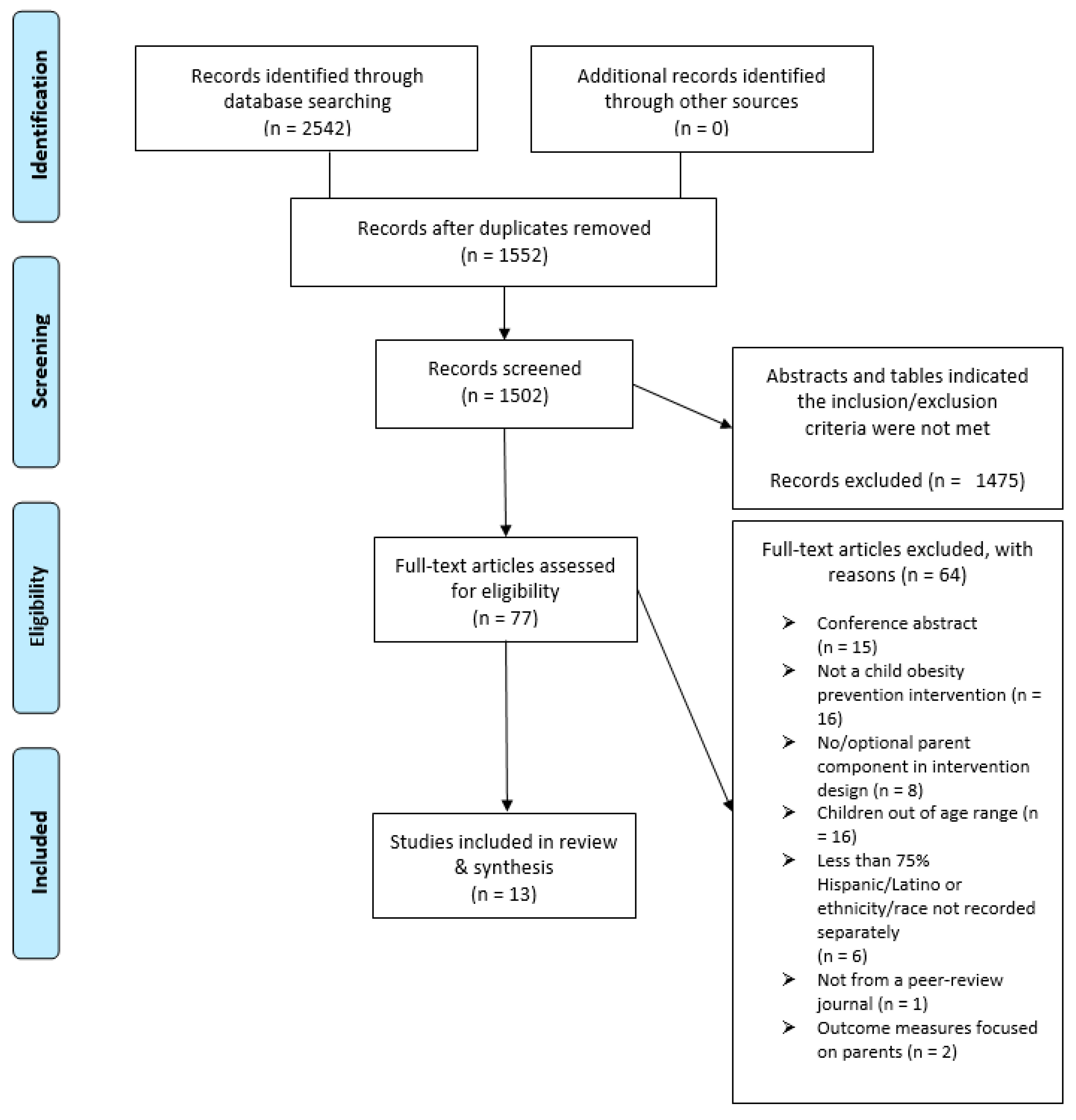
2. Methods
2.1. Identifying the Research Questions
2.2. Identifying Relevant Studies
2.3. Selecting Studies
2.4. Chart the Data
2.5. Synthesize and Summarize the Results
3. Results
3.1. Intervention Characteristics
3.2. Sample Characteristics
3.3. Integration of SDoH and Community Collaboration
4. Discussion
4.1. Intervention Gaps and Implications for Future Research
4.1.1. Targeting Multiple Health Behaviors
4.1.2. Lack of Studies with Adolescents
4.1.3. Theoretical Mechanisms
4.1.4. Defining and Evaluating Family
4.1.5. Acknowledging SDoH
4.1.6. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Skinner, A.C.; Ravanbakht, S.N.; Skelton, J.A.; Perrin, E.M.; Armstrong, S.C. Prevalence of obesity and severe obesity in US children, 1999–2016. Pediatrics 2018, 141, e20173459. [Google Scholar] [CrossRef] [PubMed]
- Miller, J.M.; Kaylor, M.B.; Johannsson, M.; Bay, C.; Churilla, J.R. Prevalence of metabolic syndrome and individual criterion in US adolescents: 2001-2010 National Health and Nutrition Examination Survey. Metab. Syndr. Relat. Disord. 2014, 12, 527–532. [Google Scholar] [CrossRef]
- Lorenzo, C.; Okoloise, M.; Williams, K.; Stern, M.P.; Haffner, S.M. The metabolic syndrome as predictor of type 2 diabetes: The San Antonio Heart Study. Diabetes Care 2003, 26, 3153–3159. [Google Scholar] [CrossRef]
- Menke, A.; Casagrande, S.; Geiss, L.; Cowie, C.C. Prevalence of and trends in diabetes among adults in the United States, 1988–2012. Jama 2015, 314, 1021–1029. [Google Scholar] [CrossRef] [PubMed]
- Black, W.R.; Borner, K.B.; Beauchamp, M.T.; Davis, A.M.; Dreyer Gillette, M.L.; Sweeney, B.; Hampl, S.E. Health-related quality of life across recent pediatric obesity classification recommendations. Children 2021, 8, 303. [Google Scholar] [CrossRef]
- van den Berg, P.; Neumark-Sztainer, D.; Eisenberg, M.E.; Haines, J. Racial/ethnic differences in weight-related teasing in adolescents. Obesity 2008, 16 (Suppl. 2), S3–S10. [Google Scholar] [CrossRef]
- Morales, D.X.; Prieto, N.; Grineski, S.E.; Collins, T.W. Race/ethnicity, obesity, and the risk of being verbally bullied: A national multilevel study. J. Racial Ethn. Health Disparities 2019, 6, 245–253. [Google Scholar] [CrossRef]
- Passel, J.; Cohn, D. U.S. Population Projections: 2005–2050. Available online: https://www.pewresearch.org/hispanic/2008/02/11/us-population-projections-2005-2050/ (accessed on 1 June 2021).
- Wilson, D.K. New perspectives on health disparities and obesity interventions in youth. J. Pediatric Psychol. 2009, 34, 231–244. [Google Scholar] [CrossRef]
- Toro-Morn, M.I. Familismo. In Encyclopedia of Immigrant Health; Loue, S., Sajatovic, M., Eds.; Springer: New York, NY, USA, 2012; pp. 672–674. [Google Scholar]
- Sleddens, E.F.; Gerards, S.M.; Thijs, C.; de Vries, N.K.; Kremers, S.P. General parenting, childhood overweight and obesity-inducing behaviors: A review. Int. J. Pediatric Obes. 2011, 6, e12–e27. [Google Scholar] [CrossRef]
- Viner, R.M.; Ozer, E.M.; Denny, S.; Marmot, M.; Resnick, M.; Fatusi, A.; Currie, C. Adolescence and the social determinants of health. Lancet 2012, 379, 1641–1652. [Google Scholar] [CrossRef]
- Scaglioni, S.; De Cosmi, V.; Ciappolino, V.; Parazzini, F.; Brambilla, P.; Agostoni, C. Factors influencing children’s eating behaviours. Nutrients 2018, 10, 706. [Google Scholar] [CrossRef]
- Ochoa, A.; Berge, J.M. Home environmental influences on childhood obesity in the Latino population: A decade review of literature. J. Immigr. Minority Health 2017, 19, 430–447. [Google Scholar] [CrossRef]
- Hammons, A.J.; Wiley, A.R.; Fiese, B.H.; Teran-Garcia, M. Six-week Latino family prevention pilot program effectively promotes healthy behaviors and reduces obesogenic behaviors. J. Nutr. Educ. Behav. 2013, 45, 745–750. [Google Scholar] [CrossRef]
- Eichen, D.M.; Rhee, K.E.; Strong, D.R.; Boutelle, K.N. Impact of race and ethnicity on weight-loss outcomes in pediatric family-based obesity treatment. J. Racial Ethn. Health Disparities 2020, 7, 643–649. [Google Scholar] [CrossRef]
- Prado, G.; Fernandez, A.; St George, S.M.; Lee, T.K.; Lebron, C.; Tapia, M.I.; Velazquez, M.R.; Messiah, S.E. Results of a family-based intervention promoting healthy weight strategies in overweight Hispanic adolescents and parents: An RCT. Am. J. Prev. Med. 2020, 59, 658–668. [Google Scholar] [CrossRef] [PubMed]
- Tripicchio, G.L.; Ammerman, A.S.; Ward, D.S.; Faith, M.S.; Truesdale, K.P.; Burger, K.S.; Dean, K.; Dumenci, L.; Davis, A. Clinical-community collaboration: A strategy to improve retention and outcomes in low-income minority youth in family-based obesity treatment. Child. Obes. 2018, 14, 141–148. [Google Scholar] [CrossRef]
- Ash, T.; Agaronov, A.; Young, T.; Aftosmes-Tobio, A.; Davison, K.K. Family-based childhood obesity prevention interventions: A systematic review and quantitative content analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 113. [Google Scholar] [CrossRef]
- Jin, J. Screening for obesity in children and adolescents. Jama 2017, 317, 2460. [Google Scholar] [CrossRef][Green Version]
- Resnicow, K.; Baranowski, T.; Ahluwalia, J.S.; Braithwaite, R.L. Cultural sensitivity in public health: Defined and demystified. Ethn. Dis. 1999, 9, 10–21. [Google Scholar]
- Engler-Stringer, R.; Le, H.; Gerrard, A.; Muhajarine, N. The community and consumer food environment and children’s diet: A systematic review. BMC Public Health 2014, 14, 522. [Google Scholar] [CrossRef]
- Weinstein, J.N.; Geller, A.; Negussie, Y.; Baciu, A. Communities in Action: Pathways to Health Equity; The National Academies Press: Washington, DC, USA, 2017. [Google Scholar]
- Philbin, M.M.; Flake, M.; Hatzenbuehler, M.L.; Hirsch, J.S. State-level immigration and immigrant-focused policies as drivers of Latino health disparities in the United States. Soc. Sci. Med. 2018, 199, 29–38. [Google Scholar] [CrossRef] [PubMed]
- Haire-Joshu, D.; Hill-Briggs, F. The next generation of diabetes translation: A path to health equity. Annu. Rev. Public Health 2019, 40, 391–410. [Google Scholar] [CrossRef]
- Braveman, P.A.; Kumanyika, S.; Fielding, J.; Laveist, T.; Borrell, L.N.; Manderscheid, R.; Troutman, A. Health disparities and health equity: The issue is justice. Am. J. Public Health 2011, 101 (Suppl. 1), S149–S155. [Google Scholar] [CrossRef] [PubMed]
- Clarke, A.R.; Goddu, A.P.; Nocon, R.S.; Stock, N.W.; Chyr, L.C.; Akuoko, J.A.; Chin, M.H. Thirty years of disparities intervention research: What are we doing to close racial and ethnic gaps in health care? Med. Care 2013, 51, 1020–1026. [Google Scholar] [CrossRef]
- Walker, R.J.; Smalls, B.L.; Campbell, J.A.; Strom Williams, J.L.; Egede, L.E. Impact of social determinants of health on outcomes for type 2 diabetes: A systematic review. Endocrine 2014, 47, 29–48. [Google Scholar] [CrossRef]
- Lee, R.M.; Ramanadhan, S.; Kruse, G.R.; Deutsch, C. A mixed methods approach to evaluate partnerships and implementation of the Massachusetts Prevention and Wellness Trust Fund. Front. Public Health 2018, 6, 150. [Google Scholar] [CrossRef] [PubMed]
- Wickremasinghe, D.; Kuruvilla, S.; Mays, N.; Avan, B.I. Taking knowledge users’ knowledge needs into account in health: An evidence synthesis framework. Health Policy Plan. 2016, 31, 527–537. [Google Scholar] [CrossRef]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Pawson, R. Evidence-based policy: In search of a method. Evaluation 2002, 8, 157–181. [Google Scholar] [CrossRef]
- Perdew, M.; Liu, S.; Naylor, P.J. Family-based nutrition interventions for obesity prevention among school-aged children: A systematic review. Transl. Behav. Med. 2021, 11, 709–723. [Google Scholar] [CrossRef] [PubMed]
- Agaronov, A.; Ash, T.; Sepulveda, M.; Taveras, E.M.; Davison, K.K. Inclusion of sleep promotion in family-based interventions to prevent childhood obesity. Child. Obes. 2018, 14, 485–500. [Google Scholar] [CrossRef] [PubMed]
- Rosenberger, M.E.; Fulton, J.E.; Buman, M.P.; Troiano, R.P.; Grandner, M.A.; Buchner, D.M.; Haskell, W.L. The 24-hour activity cycle: A new paradigm for physical activity. Med. Sci. Sports Exerc. 2019, 51, 454–464. [Google Scholar] [CrossRef] [PubMed]
- Tamayo, M.C.; Dobbs, P.D.; Pincu, Y. Family-centered interventions for treatment and prevention of childhood obesity in Hispanic families: A systematic review. J. Community Health 2021, 46, 635–643. [Google Scholar] [CrossRef] [PubMed]
- Sung-Chan, P.; Sung, Y.W.; Zhao, X.; Brownson, R.C. Family-based models for childhood-obesity intervention: A systematic review of randomized controlled trials. Obes. Rev. 2013, 14, 265–278. [Google Scholar] [CrossRef] [PubMed]
- Goran, M.I.; Ball, G.D.; Cruz, M.L. Obesity and risk of type 2 diabetes and cardiovascular disease in children and adolescents. J. Clin. Endocrinol. Metab. 2003, 88, 1417–1427. [Google Scholar] [CrossRef]
- Fraguela-Vale, R.; Varela-Garrote, L.; Carretero-García, M.; Peralbo-Rubio, E.M. Basic psychological needs, physical self-concept, and physical activity among adolescents: Autonomy in focus. Front. Psychol. 2020, 11, 491. [Google Scholar] [CrossRef]
- Soltero, E.G.; Olson, M.L.; Williams, A.N.; Konopken, Y.P.; Castro, F.G.; Arcoleo, K.J.; Keller, C.S.; Patrick, D.L.; Ayers, S.L.; Barraza, E.; et al. Effects of a community-based diabetes prevention program for Latino youth with obesity: A randomized controlled trial. Obesity 2018, 26, 1856–1865. [Google Scholar] [CrossRef]
- Contento, I.R.; Koch, P.A.; Lee, H.; Calabrese-Barton, A. Adolescents demonstrate improvement in obesity risk behaviors after completion of choice, control & change, a curriculum addressing personal agency and autonomous motivation. J. Am. Diet. Assoc. 2010, 110, 1830–1839. [Google Scholar] [CrossRef]
- Bandura, A. Social cognitive theory of self-regulation. Organ. Behav. Hum. Decis. Process. 1991, 50, 248–287. [Google Scholar] [CrossRef]
- Enright, G.; Allman-Farinelli, M.; Redfern, J. Effectiveness of family-based behavior change interventions on obesity-related behavior change in children: A realist synthesis. Int. J. Environ. Res. Public Health 2020, 17, 4099. [Google Scholar] [CrossRef]
- Soltero, E.G.; Ayers, S.L.; Avalos, M.A.; Peña, A.; Williams, A.N.; Olson, M.L.; Konopken, Y.P.; Castro, F.G.; Arcoleo, K.J.; Keller, C.S.; et al. Theoretical mediators of diabetes risk and quality of life following a diabetes prevention program for Latino youth with obesity. Am. J. Health Promot. 2021, 1–9. [Google Scholar] [CrossRef]
- Bagherniya, M.; Taghipour, A.; Sharma, M.; Sahebkar, A.; Contento, I.R.; Keshavarz, S.A.; Mostafavi Darani, F.; Safarian, M. Obesity intervention programs among adolescents using social cognitive theory: A systematic literature review. Health Educ. Res. 2018, 33, 26–39. [Google Scholar] [CrossRef]
- Branscum, P.; Sharma, M. A systematic analysis of childhood obesity prevention interventions targeting Hispanic children: Lessons learned from the previous decade. Obes. Rev. 2011, 12, e151–e158. [Google Scholar] [CrossRef]
- Alvidrez, J.; Stinson, N., Jr. Sideways progress in intervention research is not sufficient to eliminate health disparities. Am. J. Public Health 2019, 109, S102–S104. [Google Scholar] [CrossRef] [PubMed]
- Davis, R.; Campbell, R.; Hildon, Z.; Hobbs, L.; Michie, S. Theories of behaviour and behaviour change across the social and behavioural sciences: A scoping review. Health Psychol. Rev. 2015, 9, 323–344. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.T.; Goran, M.I. Prevention of type 2 diabetes in young people: A theoretical perspective. Pediatric Diabetes 2003, 4, 38–56. [Google Scholar] [CrossRef]
- Michie, S.; Johnston, M.; Francis, J.; Hardeman, W.; Eccles, M. From theory to intervention: Mapping theoretically derived behavioural determinants to behaviour change techniques. Appl. Psychol. 2008, 57, 660–680. [Google Scholar] [CrossRef]
- Pérez-Morales, M.E.; Bacardí-Gascón, M.; Jiménez-Cruz, A. Childhood overweight and obesity prevention interventions among Hispanic children in the United States: Systematic review. Nutr. Hosp. 2012, 27, 1415–1421. [Google Scholar] [CrossRef]
- Abbott, R.K. The changing definition of family. Compens. Benefits Rep. 2002, 16, 3–4. [Google Scholar]
- Walsh, F. Applying a family resilience framework in training, practice, and research: Mastering the art of the possible. Fam. Process. 2016, 55, 616–632. [Google Scholar] [CrossRef]
- Blendon, R.J.; Benson, J.M.; Gorski, M.T.; Weldon, K.J.; Pérez, D.J.; Mann, F.; Miller, C.E.; Ben-Porath, E.N. The perspectives of six Latino heritage groups about their health care. J. Immigr. Minority Health 2015, 17, 1347–1354. [Google Scholar] [CrossRef] [PubMed]
- Landale, N.S.; Oropesa, R.S.; Bradatan, C. Hispanic families in the United States: Family structure and process in an era of family change. In National Research Council (US) Panel on Hispanics and the Future of America; Tienda, M., Mitchell, F., Eds.; National Academies Press: Washington, DC, USA, 2006; Chapter 5. [Google Scholar]
- Sharma, R. The family and family structure classification redefined for the current times. J. Fam. Med. Prim. Care 2013, 2, 306–310. [Google Scholar] [CrossRef]
- James, K.S.; Connelly, C.D.; Rutkowski, E.; McPherson, D.; Gracia, L.; Mareno, N.; Zirkle, D. Family-based weight management with Latino mothers and children. J. Spec. Pediatric Nurs. 2008, 13, 249–262. [Google Scholar] [CrossRef]
- O’Connor, T.M.; Perez, O.; Beltran, A.; Colon Garcia, I.; Arredondo, E.; Parra Cardona, R.; Cabrera, N.; Thompson, D.; Baranowski, T.; Morgan, P.J. Cultural adaptation of ‘Healthy Dads, Healthy Kids’ for Hispanic families: Applying the ecological validity model. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 52. [Google Scholar] [CrossRef] [PubMed]
- Cordova, D.; Heinze, J.; Mistry, R.; Hsieh, H.F.; Stoddard, S.; Salas-Wright, C.P.; Zimmerman, M.A. Family functioning and parent support trajectories and substance use and misuse among minority urban adolescents: A latent class growth analysis. Subst. Use Misuse 2014, 49, 1908–1919. [Google Scholar] [CrossRef]
- Gray, L.A.; Hernandez Alava, M.; Kelly, M.P.; Campbell, M.J. Family lifestyle dynamics and childhood obesity: Evidence from the Millennium Cohort Study. BMC Public Health 2018, 18, 500. [Google Scholar] [CrossRef]
- Butler, A.M. Social determinants of health and racial/ethnic disparities in type 2 diabetes in youth. Curr. Diabetes Rep. 2017, 17, 60. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.M.; Okumura, M.J.; Davis, M.M.; Herman, W.H.; Gurney, J.G. Prevalence and determinants of insulin resistance among U.S. adolescents: A population-based study. Diabetes Care 2006, 29, 2427–2432. [Google Scholar] [CrossRef]
- Yusuf, Z.I.; Dongarwar, D.; Yusuf, R.A.; Bell, M.; Harris, T.; Salihu, H.M. Social determinants of overweight and obesity among children in the United States. Int. J. MCH AIDS 2020, 9, 22–33. [Google Scholar] [CrossRef]
- Barrera, M., Jr.; Berkel, C.; Castro, F.G. Directions for the advancement of culturally adapted preventive interventions: Local adaptations, engagement, and sustainability. Prev. Sci. 2017, 18, 640–648. [Google Scholar] [CrossRef]
- Falbe, J.; Cadiz, A.A.; Tantoco, N.K.; Thompson, H.R.; Madsen, K.A. Active and healthy families: A randomized controlled trial of a culturally tailored obesity intervention for Latino children. Acad. Pediatrics 2015, 15, 386–395. [Google Scholar] [CrossRef]
- Horton, L.A.; Parada, H.; Slymen, D.J.; Arredondo, E.; Ibarra, L.; Ayala, G.X. Targeting children’s dietary behaviors in a family intervention: ‘Entre familia: Reflejos de salud’. Salud Publica Mex. 2013, 55 (Suppl. 3), 397–405. [Google Scholar] [PubMed]
- Crespo, N.C.; Talavera, G.A.; Campbell, N.R.; Shadron, L.M.; Behar, A.I.; Slymen, D.; Ayala, G.X.; Wilfley, D.; Elder, J.P. A randomized controlled trial to prevent obesity among Latino paediatric patients. Pediatric Obes. 2018, 13, 697–704. [Google Scholar] [CrossRef]
- Soltero, E.G.; Ramos, C.; Williams, A.N.; Hooker, E.; Mendez, J.; Wildy, H.; Davis, K.; Hernandez, V.; Contreras, O.A.; Silva, M.; et al. ¡Viva Maryvale!: A multilevel, multisector model to community-based diabetes prevention. Am. J. Prev. Med. 2019, 56, 58–65. [Google Scholar] [CrossRef] [PubMed]
- López-Cevallos, D.F.; Harvey, S.M.; Warren, J.T. Medical mistrust, perceived discrimination, and satisfaction with health care among young-adult rural Latinos. J. Rural. Health 2014, 30, 344–351. [Google Scholar] [CrossRef]
- Falbe, J.; Friedman, L.E.; Sokal-Gutierrez, K.; Thompson, H.R.; Tantoco, N.K.; Madsen, K.A. “She gave me the confidence to open up”: Bridging communication by promotoras in a childhood obesity intervention for Latino families. Health Educ. Behav. 2017, 44, 728–737. [Google Scholar] [CrossRef] [PubMed]
- Balcázar, H.G.; de Heer, H.D.; Wise Thomas, S.; Redelfs, A.; Rosenthal, E.L.; Burgos, X.; Duarte, M.O. Promotoras can facilitate use of recreational community resources: The Mi Corazón Mi Comunidad cohort study. Health Promot. Pract. 2016, 17, 343–352. [Google Scholar] [CrossRef]
- Gonzalez, G. Primary care interventions to reduce childhood obesity in Latino families. J. Pediatric Health Care 2016, 30, 471–479. [Google Scholar] [CrossRef] [PubMed]
| n (%) | |
|---|---|
| Geographic Region | |
| United States | 12 (92.3%) |
| Mexico | 1 (7.6%) |
| Study Design * | |
| RCT | 9 (69.2%) |
| Quasi-Experimental | 4 (38.5%) |
| Intervention Setting * | |
| Home | 2 (15.4%) |
| Primary care/health clinic | 3 (23.1%) |
| Community Organization | 2 (15.4%) |
| School | 2 (15.4%) |
| University | 1 (7.7%) |
| Multi-setting | 1 (7.7%) |
| Not specified | 2 (15.4%) |
| Length of Intervention | |
| ≤10 weeks | 3 (23.1%) |
| 11–52 weeks | 7 (53.8%) |
| >53 weeks | 3 (23.1%) |
| Health Behaviors Targeted * | |
| Diet | 12 (92.3%) |
| Physical Activity | 9 (69.2%) |
| Screen Use | 2 (15.4%) |
| Sleep | 1 (7.7%) |
| Sedentary Behaviors | 6 (46.2%) |
| Theoretical Framework * | |
| Social Cognitive Theory | 6 (46.2%) |
| Transtheoretical Model of Behavior Change | 1 (7.7%) |
| Family Systems Theory | 2 (15.4%) |
| Behavioral Choice Theory | 1 (7.7%) |
| Food Preference Theory | 1 (7.7%) |
| Socioeconomic Model for Latino Health Promotion | 1 (7.7%) |
| Sociocultural approach | 1 (7.7%) |
| Cross-cultural psychology | 1 (7.7%) |
| Family resilience approach | 1 (7.7%) |
| Health Belief model | 1 (7.7%) |
| Structural model of health behavior | 1 (7.7%) |
| Ecological Model | 1 (7.7%) |
| Not stated | 3 (23.1%) |
| Focus of Evaluation * | |
| Child | 13 (100%) |
| Parent | 11 (84.6%) |
| Retention Rates | |
| 0–70% | 4 (30.8%) |
| 71–80% | 4 (30.8%) |
| 81–90% | 4 (30.8%) |
| ≥91% | 1 (7.7%) |
| n (%) | |
|---|---|
| Age of Target Child * | |
| 5–10 years | 13 (100%) |
| 11–13 years | 9 (69.2%) |
| Sample Size | |
| 0–100 | 4 (30.8%) |
| 101–200 | 2 (15.4%) |
| 201–300 | 3 (23.1%) |
| >300 | 4 (30.8%) |
| Family Socioeconomic Status | |
| Low Socioeconomic Status | 8 (61.5%) |
| Not Specified | 5 (38.5%) |
| Family Engagement | |
| Parent-child dyad | 3 (23.1%) |
| Whole Family | 10 (76.9%) |
| Measured Acculturation | |
| Yes | 3 (23.1%) |
| Not Measured | 10 (76.9%) |
| Hispanic Subgroups * | |
| Mexican/Mexican American | 10 (76.9%) |
| Central American | 3 (23.1%) |
| Latin America | 2 (15.4%) |
| Latino/Hispanic Non-specific | 5 (38.5%) |
| Other | 4 (30.8%) |
| n (%) | |
|---|---|
| Formative Work with Stakeholders | |
| Yes | 7 (53.8%) |
| Not Specified | 6 (46.2%) |
| Program Implementers | |
| Physicians/Providers | 4 (30.8%) |
| Health Educators/Promotoras | 6 (46.2%) |
| Trained Research Staff | 4 (30.8%) |
| Language | |
| Spanish | 3 (23.1%) |
| Bilingual | 8 (61.5%) |
| Not specified | 2 (15.4%) |
| Cultural Adaptations | |
| Yes | 9 (69.2%) |
| Not Specified | 4 (30.8%) |
| Acknowledged SDoH | |
| Yes | 6 (46.2%) |
| Not Specified | 7 (53.8%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soltero, E.G.; Peña, A.; Gonzalez, V.; Hernandez, E.; Mackey, G.; Callender, C.; Dave, J.M.; Thompson, D. Family-Based Obesity Prevention Interventions among Hispanic Children and Families: A Scoping Review. Nutrients 2021, 13, 2690. https://doi.org/10.3390/nu13082690
Soltero EG, Peña A, Gonzalez V, Hernandez E, Mackey G, Callender C, Dave JM, Thompson D. Family-Based Obesity Prevention Interventions among Hispanic Children and Families: A Scoping Review. Nutrients. 2021; 13(8):2690. https://doi.org/10.3390/nu13082690
Chicago/Turabian StyleSoltero, Erica G., Armando Peña, Veronica Gonzalez, Edith Hernandez, Guisela Mackey, Chishinga Callender, Jayna M. Dave, and Debbe Thompson. 2021. "Family-Based Obesity Prevention Interventions among Hispanic Children and Families: A Scoping Review" Nutrients 13, no. 8: 2690. https://doi.org/10.3390/nu13082690
APA StyleSoltero, E. G., Peña, A., Gonzalez, V., Hernandez, E., Mackey, G., Callender, C., Dave, J. M., & Thompson, D. (2021). Family-Based Obesity Prevention Interventions among Hispanic Children and Families: A Scoping Review. Nutrients, 13(8), 2690. https://doi.org/10.3390/nu13082690








