Applying the Stages of Change Model in a Nutrition Education Programme for the Promotion of Fruit and Vegetable Consumption among People with Severe Mental Disorders (DIETMENT)
Abstract
1. Introduction
2. Materials and Methods
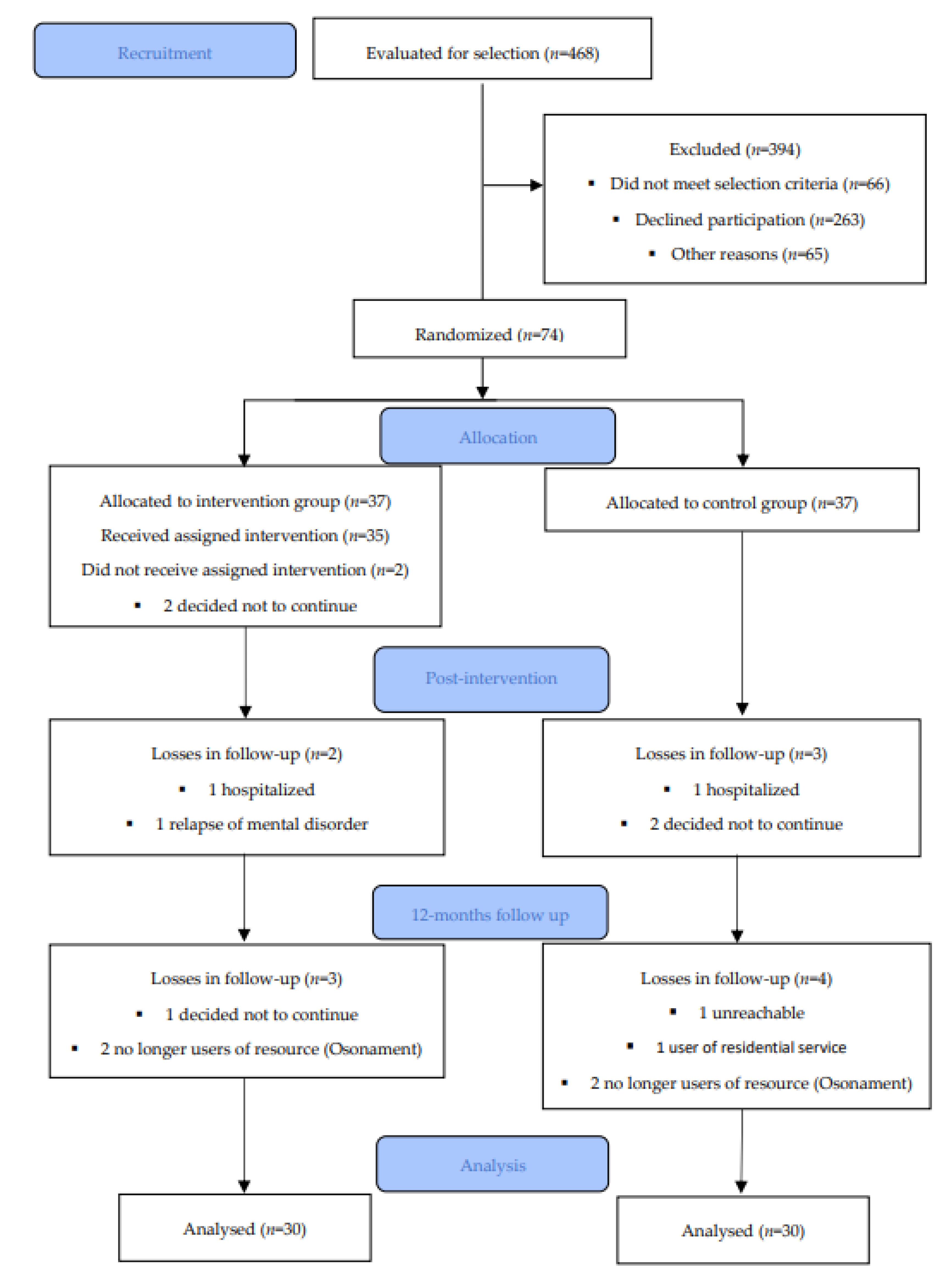
2.1. Study Design and Participants
2.2. Intervention
2.3. Measures
2.3.1. Sociodemographic Characteristics
2.3.2. Clinical Characteristics
2.3.3. The Consumption of F&V
2.3.4. Stages of Change
2.4. Statistical Analysis
3. Results
3.1. Sociodemographic and Clinical Characteristics
3.2. Sociodemographic and Clinical Characteristics Related to the Intake of F&V
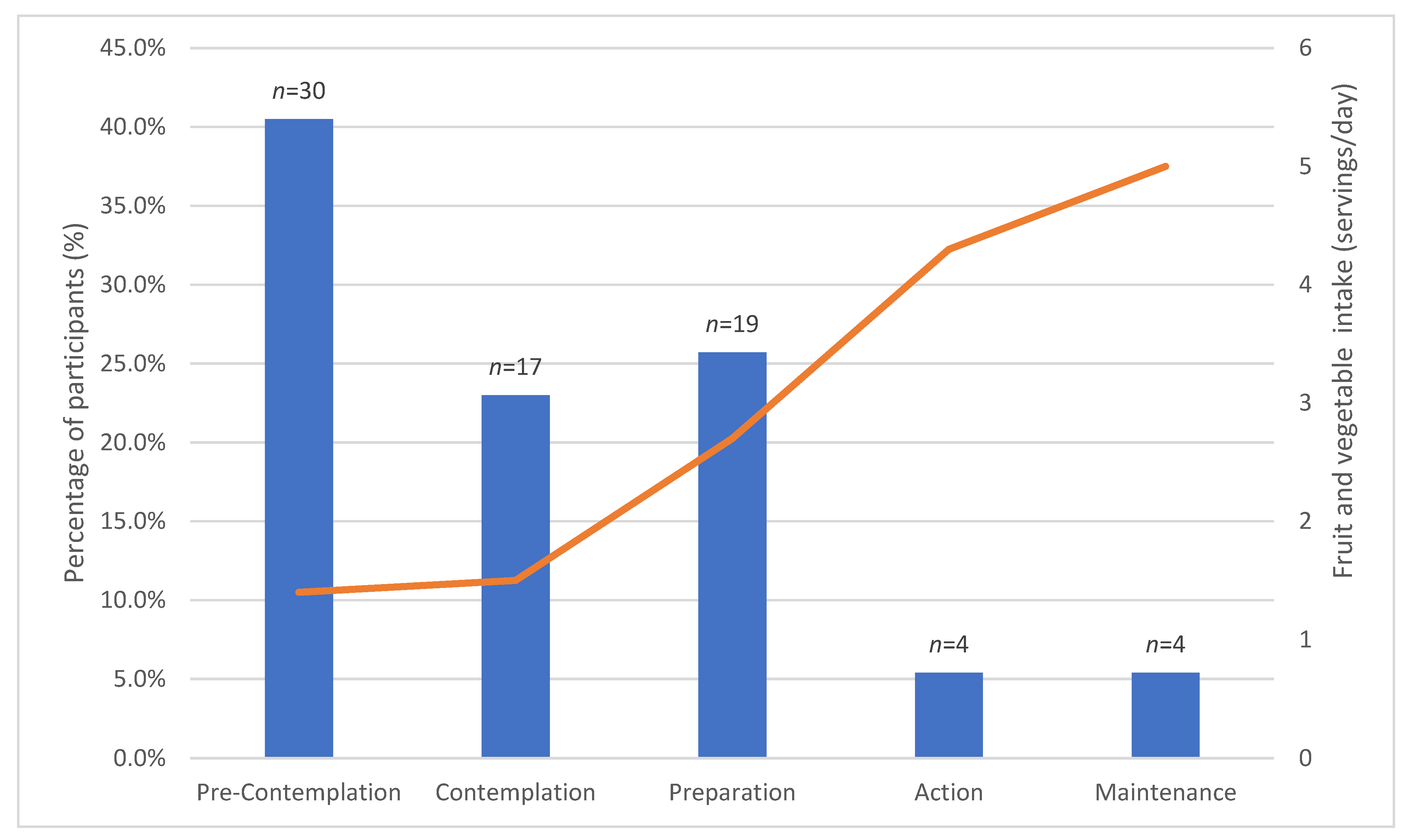
3.3. Association between Stages of Change and the Intake of F&V
3.4. Consumption of F&V at Baseline and Impact of the Intervention
3.5. Impact of Intervention on Motivation to Change
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Characteristics | Servings F&V | p-Value |
|---|---|---|
| Mean (SD) | ||
| Gender | ||
| Men | 1.9 (1.8) | 0.319 a |
| Women | 2.3 (1.7) | |
| Marital status | ||
| Single | 1.9 (1.7) | 0.365 b |
| Separated or divorced | 1.6 (1.8) | |
| Married or has a partner | 2.3 (1.9) | |
| Level of education | ||
| No schooling | 1 | 0.841 b |
| Secondary | 2.2 (1.8) | |
| Upper secondary or VT | 2.1 (1.6) | |
| Further education | 1.8 (2.1) | |
| ADL support | ||
| No support | 1.9 (1.7) | 0.022 b,* |
| Family or non-professional | 1.8 (1.6) | |
| Professional | 3.2 (1.5) | |
| Main diagnosis | ||
| Schizophrenia and other psychotic disorders | 2.3 (1.8) | 0.784 b |
| Bipolar disorder | 2.3 (1.8) | |
| Depressive disorders | 1.8 (1.6) | |
| Personality disorder | 2 (1.4) | |
| Obsessive-compulsive disorder | 1.3 (1.5) |
| F&V | Age | Weight | BMI | FAST | SCIP-S | Subjective Well-Being | |
|---|---|---|---|---|---|---|---|
| Servings | |||||||
| Age (years) | |||||||
| r | 0.185 | 1 | −0.107 | 0.079 | 0.028 | 0.436 | 0.036 |
| p-value | 0.115 | 0.369 | 0.509 | 0.812 | <0.001 *** | 0.765 | |
| Weight (kg) | |||||||
| r | −0.158 | −0.107 | 1 | 0.852 | 0.071 | −0.002 | 0.159 |
| p-value | 0.184 | 0.369 | <0.001 *** | 0.554 | 0.99 | 0.192 | |
| BMI (Kg/m2) | |||||||
| r | −0.098 | 0.079 | 0.852 | 1 | 0.087 | 0.083 | 0.194 |
| p-value | 0.411 | 0.509 | <0.001 *** | 0.469 | 0.508 | 0.111 | |
| FAST | |||||||
| r | 0.067 | 0.028 | 0.071 | 0.087 | 1 | −0.121 | 0.087 |
| p-value | 0.571 | 0.812 | 0.554 | 0.469 | 0.329 | 0.468 | |
| SCIP-S | |||||||
| r | 0.114 | 0.436 | −0.002 | 0.083 | −0.121 | 1 | −0.220 |
| p-value | 0.243 | <0.001 *** | 0.99 | 0.508 | 0.329 | 0.074 | |
| Subjective | |||||||
| well-being | 1 | ||||||
| r | −0.035 | 0.036 | 0.159 | 0.194 | 0.087 | −0.220 | |
| p-value | 0.77 | 0.765 | 0.192 | 0.111 | 0.468 | 0.074 |
References
- Aune, D.; Giovannucci, E.; Boffetta, P.; Fadnes, L.T.; Keum, N.; Norat, T.; Greenwood, D.C.; Riboli, E.; Vatten, L.J.; Tonstad, S. Fruit and vegetable intake and the risk of cardiovascular disease, total cancer and all-cause mortality—a systematic review and dose-response meta-analysis of prospective studies. Int. J. Epidemiol. 2017, 46, 1029–1056. [Google Scholar] [CrossRef] [PubMed]
- Wallace, T.C.; Bailey, R.L.; Blumberg, J.B.; Burton-Freeman, B.; Chen, C.-Y.O.; Crowe-White, K.M.; Drewnowski, A.; Hooshmand, S.; Johnson, E.; Lewis, R.; et al. Fruits, vegetables, and health: A comprehensive narrative, umbrella review of the science and recommendations for enhanced public policy to improve intake. Crit. Rev. Food Sci. Nutr. 2020, 60, 2174–2211. [Google Scholar] [CrossRef]
- Alissa, E.M.; Ferns, G.A. Dietary Fruits and Vegetables and Cardiovascular Diseases Risk. Crit. Rev. Food Sci. Nutr. 2017, 57, 1950–1962. [Google Scholar] [CrossRef]
- Bradbury, K.E.; Appleby, P.N.; Key, T.J. Fruit, vegetable, and fiber intake in relation to cancer risk: Findings from the European Prospective Investigation into Cancer and Nutrition (EPIC). Am. J. Clin. Nutr. 2014, 100, 394S–398S. [Google Scholar] [CrossRef] [PubMed]
- Głąbska, D.; Guzek, D.; Groele, B.; Gutkowska, K. Fruit and Vegetable Intake and Mental Health in Adults: A Systematic Review. Nutrients 2020, 12, 115. [Google Scholar] [CrossRef]
- Adan, R.A.; van der Beek, E.M.; Buitelaar, J.K.; Cryan, J.F.; Hebebrand, J.; Higgs, S.; Schellekens, H.; Dickson, S.L. Nutritional psychiatry: Towards improving mental health by what you eat. Eur. Neuropsychopharmacol. 2019, 29, 1321–1332. [Google Scholar] [CrossRef]
- Tuck, N.-J.; Farrow, C.; Thomas, J.M. Assessing the effects of vegetable consumption on the psychological health of healthy adults: A systematic review of prospective research. Am. J. Clin. Nutr. 2019, 110, 196–211. [Google Scholar] [CrossRef]
- WHO. FAO/WHO Fruit and Vegetables for Health. Report of a Joint FAO/OMS Workshop, 1–3 September 2004, Kobe, Japan; WHO: Kobe, Japan, 2004. [Google Scholar]
- Agència de Salut Pública de Catalunya (ASPCAT). Petits Canvis per Menjar Millor; Agència de Salut Pública de Catalunya: Barcelona, Spain, 2019. [Google Scholar]
- Sociedad Española de Nutrición Comunitaria (SENC). Guía de la Alimentación Saludable para Atención Primaria y Colectivos Ciudadanos; Planeta: Barcelona, Spain, 2019. [Google Scholar]
- Stea, T.H.; Nordheim, O.; Bere, E.; Stornes, P.; Eikemo, T.A. Fruit and vegetable consumption in Europe according to gender, educational attainment and regional affiliation—A cross-sectional study in 21 European countries. PLoS ONE 2020, 15, e0232521. [Google Scholar] [CrossRef] [PubMed]
- Hahn, L.A.; Galletly, A.C.; Foley, D.L.; Mackinnon, A.; Watts, G.F.; Castle, D.J.; Waterreus, A.; Morgan, A.V. Inadequate fruit and vegetable intake in people with psychosis. Aust. N. Z. J. Psychiatry 2014, 48, 1025–1035. [Google Scholar] [CrossRef]
- Teasdale, S.B.; Ward, P.B.; Samaras, K.; Firth, J.; Stubbs, B.; Tripodi, E.; Burrows, T.L. Dietary intake of people with severe mental illness: Systematic review and meta-analysis. Br. J. Psychiatry 2019, 214, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Costa, R.; Teasdale, S.; Abreu, S.; Bastos, T.; Probst, M.; Rosenbaum, S.; Ward, P.B.; Corredeira, R. Dietary Intake, Adherence to Mediterranean Diet and Lifestyle-Related Factors in People with Schizophrenia. Issues Ment. Health Nurs. 2019, 40, 851–860. [Google Scholar] [CrossRef]
- Ruggeri, M.; Leese, M.; Thornicroft, G.; Bisoffi, G.; Tansella, M. Definition and prevalence of severe and persistent mental illness. Br. J. Psychiatry 2000, 177, 149–155. [Google Scholar] [CrossRef]
- Liu, N.H.; Daumit, G.L.; Dua, T.; Aquila, R.; Charlson, F.; Cuijpers, P.; Druss, B.; Dudek, K.; Freeman, M.; Fujii, C.; et al. Excess mortality in persons with severe mental disorders: A multilevel intervention framework and priorities for clinical practice, policy and research agendas. World Psychiatry 2017, 16, 30–40. [Google Scholar] [CrossRef]
- Holt, R.I.G. Cardiovascular Disease and Severe Mental Illness. In Comorbidity of Mental and Physical Disorders; Sartorius, N., Holt, R.I.G., Maj, M., Eds.; Karger: Basel, Swirzerland, 2015; Volume 179, pp. 54–65. ISBN 978-3-31-802603-0. [Google Scholar]
- De Hert, M.; Correll, C.U.; Bobes, J.; Cetkovich-Bakmas, M.; Cohen, D.; Asai, I.; Detraux, J.; Gautam, S.; Möller, H.-J.; Ndetei, D.M.; et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry 2011, 10, 52–77. [Google Scholar] [CrossRef] [PubMed]
- Jahrami, H.A.; Faris, M.A.-I.E.; Saif, Z.Q.; Hammad, L.H. Assessing dietary and lifestyle risk factors and their associations with disease comorbidities among patients with schizophrenia: A case–control study from Bahrain. Asian J. Psychiatry 2017, 28, 115–123. [Google Scholar] [CrossRef] [PubMed]
- Contento, I.R. Foundation in Theory and Research: Facilitating the Ability to take Action. In Nutrition Education: Linking Research, Theory and Practice; Jones and Bartlett Publishers: Sudbury, ON, Canada, 2011. [Google Scholar]
- Prochaska, J.O.; Velicer, W.F. The Transtheoretical Model of Health Behavior Change. Am. J. Health Promot. 1997, 12, 38–48. [Google Scholar] [CrossRef]
- Prochaska, J.O.; Redding, C.A.; Evers, K.E. The Transtheoretical Model and stages of change. In Health Behavior and Health Education: Theory, Research, and Practice; Glanz, K., Rimer, B.K., Viswanath, K., Eds.; Jossey-Bass: Hoboken, NJ, USA, 2008; pp. 97–117. [Google Scholar]
- Hashemzadeh, M.; Rahimi, A.; Zare-Farashbandi, F.; Alavi-Naeini, A.M.; Daei, A. Transtheoretical Model of Health Behavioral Change: A Systematic Review. Iran J. Nurs. Midwifery Res 2019, 24, 83. [Google Scholar]
- Spencer, L.; Wharton, C.; Moyle, S.; Adams, T. The transtheoretical model as applied to dietary behaviour and outcomes. Nutr. Res. Rev. 2007, 20, 46–73. [Google Scholar] [CrossRef] [PubMed]
- Teasdale, S.B.; Ward, P.B.; Rosenbaum, S.; Samaras, K.; Stubbs, B. Solving a weighty problem: Systematic review and meta-analysis of nutrition interventions in severe mental illness. Br. J. Psychiatry 2017, 210, 110–118. [Google Scholar] [CrossRef]
- American Psychiatric Association (APA). DSM-IV TR. Manual Diagnóstico y Estadístico de los Trastornos Mentales, 4th ed.; American Psychiatric Publishing: Washington, DC, USA, 2000. [Google Scholar]
- World Health Organization (WHO). Obesity: Preventing and Managing the Global Epidemic. Report of a WHO Consultation; WHO: Geneva, Switzerland, 2000; Volume 894. [Google Scholar]
- Rosa, A.R.; Sánchez-Moreno, J.; Martínez-Aran, A.; Salamero, M.; Torrent, C.; Reinares, M.; Comes, M.; Colom, F.; Van Riel, W.; Ayuso-Mateos, J.L.; et al. Validity and reliability of the Functioning Assessment Short Test (FAST) in bipolar disorder. Clin. Pr. Epidemiol. Ment. Health 2007, 3, 5. [Google Scholar] [CrossRef]
- Pino, O.; Guilera, G.; Rojo, J.E.; Gómez-Benito, J.; Bernardo, M.; Crespo-Facorro, B.; Cuesta, M.J.; Franco, M.; Martinez-Aran, A.; Segarra, N.; et al. Spanish version of the Screen for Cognitive Impairment in Psychiatry (SCIP-S): Psychometric properties of a brief scale for cognitive evaluation in schizophrenia. Schizophr. Res. 2008, 99, 139–148. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Blazquez, C.; Frades-Payo, B.; Forjaz, M.J.; Ayala, A.; Martinez-Martin, P.; Fernandez-Mayoralas, G.; Rojo-Perez, F. Psychometric properties of the International Wellbeing Index in community-dwelling older adults. Int. Psychogeriatr. 2010, 23, 161–169. [Google Scholar] [CrossRef] [PubMed]
- LaForge, R.G.; Greene, G.W.; Prochaska, J.O. Psychosocial factors influencing low fruit and vegetable consumption. J. Behav. Med. 1994, 17, 361–374. [Google Scholar] [CrossRef] [PubMed]
- Simonelli-Muñoz, A.J.; Fortea, M.I.; Salorio, P.; Gallego-Gomez, J.I.; Bautista, S.S.; Balanza, S. Dietary habits of patients with schizophrenia: A self-reported questionnaire survey. Int. J. Ment. Health Nurs. 2012, 21, 220–228. [Google Scholar] [CrossRef]
- Contento, I.R. Overview of determinants of food choice and dietary change: Implications for nutrition education. In Nutrition Education: Linking Research, Theory and Practice; Jones and Bartlett Publishers: Sudbury, ON, Canada, 2011. [Google Scholar]
- Vilamala-Orra, M.; Vaqué-Crusellas, C.; Saéz, R.D.R. Valoración de los factores que condicionan la adquisición de hábitos alimentarios saludables en personas con trastorno mental grave (tmg): Aproximación cualitativa desde una perspectiva en primera persona y de los profesionales. New Trends Qual. Res. 2020, 3, 318–330. [Google Scholar] [CrossRef]
- Barre, L.K.; Ferron, J.C.; Davis, K.E.; Whitley, R. Healthy eating in persons with serious mental illnesses: Understanding and barriers. Psychiatry Rehabil. J. 2011, 34, 304–310. [Google Scholar] [CrossRef]
- Yen, W.C.; Shariff, Z.M.; Kandiah, M.; Taib, M.N.M. Stages of change to increase fruit and vegetable intake and its relationships with fruit and vegetable intake and related psychosocial factors. Nutr. Res. Pr. 2014, 8, 297–303. [Google Scholar] [CrossRef]
- Zeidan, B.; Partridge, S.R.; Balestracci, K.; Allman-Farinelli, M. Congruence of stage-of-change for fruit, vegetables and take-out foods with consumption. Nutr. Food Sci. 2018, 48, 483–497. [Google Scholar] [CrossRef]
- Naslund, J.A.; Whiteman, K.L.; McHugo, G.J.; Aschbrenner, K.A.; Marsch, L.A.; Bartels, S.J. Lifestyle interventions for weight loss among overweight and obese adults with serious mental illness: A systematic review and meta-analysis. Gen. Hosp. Psychiatry 2017, 47, 83–102. [Google Scholar] [CrossRef]
- Gur, K.; Erol, S.; Kadioglu, H.; Ergun, A.; Boluktas, R. The impact on adolescents of a Transtheoretical Model-based programme on fruit and vegetable consumption. Public Health Nutr. 2019, 22, 2500–2508. [Google Scholar] [CrossRef]
- Nakabayashi, J.; Melo, G.R.-I.; Toral, N. Transtheoretical model-based nutritional interventions in adolescents: A systematic review. BMC Public Health 2020, 20, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Kristal, A.R.; Glanz, K.; Curry, S.J.; E Patterson, R. How Can Stages of Change be Best Used in Dietary Interventions? J. Am. Diet. Assoc. 1999, 99, 679–684. [Google Scholar] [CrossRef]

| Stages of Change | Session | Objective | Process of Change | Session Content |
|---|---|---|---|---|
| Pre-contemplation | 1st, 2nd session | Raise awareness of the need for change | Consciousness-raising Dramatic relief | Debate on beliefs and attitudes towards healthy eating (1st session) Identify facilitating elements and barriers to habit change (1st session) Present news items on the health impacts of adopting unhealthy eating behaviours (1st session) Role of emotional state in eating behaviours and food selection (2nd session) |
| Contemplation | 3rd, 4th, 5th session | Motivate and increase confidence in the ability to change | Consciousness-raising Self-reevaluation | Self-reevaluation of current eating habits via a dietary record (24 h reminder) (3rd session) Presentation and debate about false beliefs related to food (4th session) Benefits of the consumption of F&V (4th session) Workshop on the amount of sugar in foods and healthy alternatives (5th session) |
| Preparation | 6th, 7th session | Work on knowledge and skills | Self-liberation | Individual assessment of possible modifications to be introduced in eating habits (6th session) Set specific short-term goals (6th session) Seasonality of F&V and strategies to increase their intake (7th session) Suggestions for healthy breakfasts and snacks (7th session) |
| Action | 8th, 9th, 10th, 11th, 12th, 13th session | Increase self-confidence and enhance autonomy (skills training) | Counterconditioning Stimulus or environmental control | Cooking workshop (servings and recipes) (8th and 13th session) Producing a healthy recipe book according to the season (9th session) Creating an individual diet plan (9th session) Workshop on purchase planning (10th session) Food remaining management workshop (11th session) Disposable tablecloth design with messages promoting consumption of F&V (12th session) |
| Maintenance | 14th, 15th session | Work on social support Preventing relapse into unhealthy eating behaviours | Environmental re-evaluation Helping relationships | Self-assessment of current eating habits and comparison with dietary record completed at the beginning of the programme (14th session) Sharing experiences (peer support) (15th session) Group sessions aimed at relatives and flat/housemates |
| Characteristics | Total Population (n = 74) | IG (n = 37) | CG (n = 37) |
|---|---|---|---|
| Age (years), mean (SD) | 48.7 (10.8) | 49.8 (11.4) | 47.7 (10.3) |
| Gender, n (%) | |||
| Men | 41 (55.4) | 21 (56.8) | 20 (54.1) |
| Women | 33 (44.6) | 16 (43.2) | 17 (45.9) |
| Marital status, n (%) | |||
| Single | 46 (63) | 19 (52.8) | 27 (73) |
| Separated or divorced | 18 (24.7) | 13 (36.1) | 5 (13.5) |
| Married or has a partner | 9 (12.3) | 4 (11.1) | 5 (13.5) |
| Level of education, n (%) | |||
| No schooling | 1 (1.4) | 1 (2.7) | - |
| Secondary | 32 (43.2) | 12 (32.4) | 20 (54.1) |
| Upper secondary or VT | 31 (41.9) | 19 (51.4) | 12 (32.4) |
| Further education | 10 (13.5) | 5 (13.5) | 5 (13.4) |
| ADL support, n (%) | |||
| No support | 39 (52.7) | 19 (51.4) | 20 (54.1) |
| Family or non-professional | 20 (27) | 10 (27) | 10 (27) |
| Professional | 15 (20.3) | 8 (21.6) | 7 (18.9) |
| Main diagnosis, n (%) | |||
| Schizophrenia and other psychotic disorders | 28 (37.8) | 12 (32.4) | 16 (43.2) |
| Bipolar disorder | 22 (29.7) | 12 (32.4) | 10 (27) |
| Depressive disorders | 19 (25.7) | 10 (27) | 9 (24.3) |
| Personality disorders | 3 (4.1) | 1 (2.7) | 2 (5.4) |
| Obsessive-compulsive disorder | 2 (2.7) | 2 (5.4) | - |
| Weight (kg), mean (SD) | 84.2 (18.1) | 87.1 (17.5) | 81.3 (18.5) |
| BMI (kg/m2), mean (SD) | 29.6 (6.3) | 30.6 (5.6) | 28.7 (6.8) |
| FAST, mean (SD) | 34.4 (13.1) | 32 (14) | 36.8 (11.9) |
| SCIP-S (PT), mean (SD) | 36.3 (7.7) | 37.1 (8.1) | 35.5 (7.3) |
| Subjective well-being, mean (SD) | 57.3 (19.3) | 53.8 (19.6) | 61.1 (18.6) |
| Stage of Change | F&V | p-Value 1 | p-Value 2 | ||||
|---|---|---|---|---|---|---|---|
| Mean (SD) | Pre-Contemplation | Contemplation | Preparation | Action | Maintenance | ||
| Pre-contemplation | 1.4 (1.7) | <0.001 | - | 1.0 | 0.031 * | 0.004 * | <0.001 * |
| Contemplation | 1.5 (1, 0) | 1.0 | - | 0.092 | 0.007 * | <0.001 * | |
| Preparation | 2.7 (1.4) | 0.031 * | 0.092 | - | 0.279 | 0.034 * | |
| Action | 4.3 (0.9) | 0.004 * | 0.007 * | 0.279 | - | 0.945 | |
| Maintenance | 5 (1.4) | <0.001 * | <0.001 * | 0.034 * | 0.945 | - | |
| Baseline (T0) (n = 60) | Post Intervention (T1) (n = 60) | 12-Month Follow-up (T2) (n = 60) | p1 | Difference from T0 to T1 p-Value 2 | Difference from T1 to T2 p-Value 2 | |
|---|---|---|---|---|---|---|
| Result | Median (P25–75) | Median (P25–75) | Median (P25-75) | |||
| IG | ||||||
| Fruit | 1 (0–2) | 2 (1–3) | 2 (1–3) | 0.012 * | 0.007 * | 0.088 |
| Vegetables | 1 (0–2) | 1 (0–2) | 1 (0–2) | 0.219 | 0.432 | 0.251 |
| F&V | 2 (1–3.3) | 3 (2–4.3) | 3 (2–4) | 0.081 | 0.005 * | 0.447 |
| CG | ||||||
| Fruit | 1 (0–2) | 2 (1–2.3) | 1 (0–2) | 0.086 | 0.098 | 0.095 |
| Vegetables | 1 (0–1) | 1 (0–1) | 1 (0–2) | 0.439 | 0.527 | 0.653 |
| F&V | 2 (0.8–3) | 3 (1.3–3) | 2 (1–4) | 0.237 | 0.212 | 0.243 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vilamala-Orra, M.; Vaqué-Crusellas, C.; Foguet-Boreu, Q.; Guimerà Gallent, M.; del Río Sáez, R. Applying the Stages of Change Model in a Nutrition Education Programme for the Promotion of Fruit and Vegetable Consumption among People with Severe Mental Disorders (DIETMENT). Nutrients 2021, 13, 2105. https://doi.org/10.3390/nu13062105
Vilamala-Orra M, Vaqué-Crusellas C, Foguet-Boreu Q, Guimerà Gallent M, del Río Sáez R. Applying the Stages of Change Model in a Nutrition Education Programme for the Promotion of Fruit and Vegetable Consumption among People with Severe Mental Disorders (DIETMENT). Nutrients. 2021; 13(6):2105. https://doi.org/10.3390/nu13062105
Chicago/Turabian StyleVilamala-Orra, Mireia, Cristina Vaqué-Crusellas, Quintí Foguet-Boreu, Marta Guimerà Gallent, and Ruben del Río Sáez. 2021. "Applying the Stages of Change Model in a Nutrition Education Programme for the Promotion of Fruit and Vegetable Consumption among People with Severe Mental Disorders (DIETMENT)" Nutrients 13, no. 6: 2105. https://doi.org/10.3390/nu13062105
APA StyleVilamala-Orra, M., Vaqué-Crusellas, C., Foguet-Boreu, Q., Guimerà Gallent, M., & del Río Sáez, R. (2021). Applying the Stages of Change Model in a Nutrition Education Programme for the Promotion of Fruit and Vegetable Consumption among People with Severe Mental Disorders (DIETMENT). Nutrients, 13(6), 2105. https://doi.org/10.3390/nu13062105






