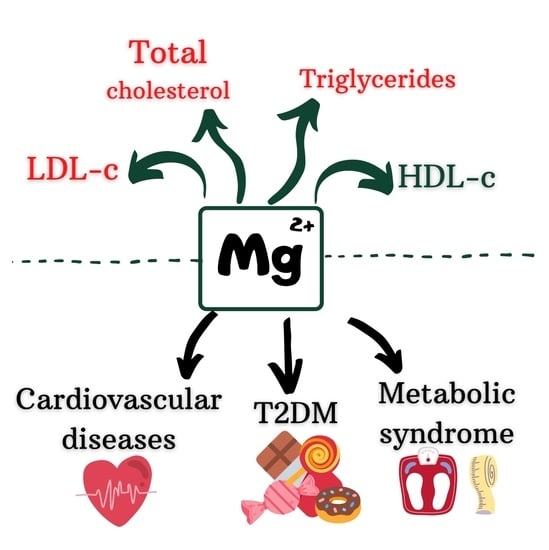
Crosstalk of Magnesium and Serum Lipids in Dyslipidemia and Associated Disorders: A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Crosstalk of Magnesium, Serum Lipids, and Dyslipidemia
3.1.1. Magnesium, Serum Lipids, and Dyslipidemia
3.1.2. Magnesium, Serum Lipids, and the Diet/dietary Interventions
3.1.3. Magnesium, Serum Lipids, and Overweight and (or) Obesity
3.1.4. Magnesium, Serum Lipids, and Polycystic Ovary Syndrome (PCOS)
3.1.5. Magnesium, Serum Lipids, and Nonalcoholic Fatty Liver Disease (NAFLD)
3.2. Crosstalk of Magnesium, Serum Lipids, and Metabolic Syndrome
3.3. Magnesium, Serum Lipids, and Type 2 Diabetes Mellitus (T2DM)
3.3.1. Hypomagnesemia
3.3.2. Magnesium Supplementation in RCTs and Interventional Studies
3.4. Crosstalk of Magnesium, Serum Lipids and Cardiovascular Disorders
3.4.1. Atherosclerosis, Angina Pectoris and Acute Myocardial Infarction
3.4.2. Coronary Heart Disease
3.4.3. Coronary Artery Calcifications
3.4.4. Hypertension
3.5. Crosstalk of Magnesium, Chronic Kidney Disease, and Hemodialysis
3.5.1. Chronic Kidney Disease
3.5.2. Hemodialysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Lu, Y.; Wang, P.; Zhou, T.; Lu, J.; Spatz, E.S.; Nasir, K.; Jiang, L.; Krumholz, H.M. Comparison of Prevalence, Awareness, Treatment, and Control of Cardiovascular Risk Factors in China and the United States. J. Am. Heart Assoc. 2018, 7, e007462. [Google Scholar] [CrossRef] [PubMed]
- Epingeac, M.E.; Gaman, M.A.; Diaconu, C.C.; Gaman, A.M. Crosstalk between Oxidative Stress and Inflammation in Obesity. Rev. Chim. 2020, 71, 228–232. [Google Scholar] [CrossRef]
- Munteanu, M.A.; Gheorghe, G.; Stanescu, A.M.A.; Bratu, O.G.; Diaconu, C.C. What Is New Regarding the Treatment of Dyslipidemia in the 2019 European Society of Cardiology Guidelines? Arch. Balk. Med. Union 2019, 54, 749–752. [Google Scholar] [CrossRef]
- Orlova, S.; Dikke, G.; Pickering, G.; Konchits, S.; Starostin, K.; Bevz, A. Magnesium Deficiency Questionnaire: A New Non-Invasive Magnesium Deficiency Screening Tool Developed Using Real-World Data from Four Observational Studies. Nutrients 2020, 12, 2062. [Google Scholar] [CrossRef] [PubMed]
- Piuri, G.; Zocchi, M.; Della Porta, M.; Ficara, V.; Manoni, M.; Zuccotti, G.V.; Pinotti, L.; Maier, J.A.; Cazzola, R. Magnesium in Obesity, Metabolic Syndrome, and Type 2 Diabetes. Nutrients 2021, 13, 320. [Google Scholar] [CrossRef]
- Rosanoff, A.; Costello, R.B.; Johnson, G.H. Effectively Prescribing Oral Magnesium Therapy for Hypertension: A Categorized Systematic Review of 49 Clinical Trials. Nutrients 2021, 13, 195. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Barragán, R.; Llopis, J.; Portolés, O.; Sorlí, J.V.; Coltell, O.; Rivas-García, L.; Asensio, E.M.; Ortega-Azorín, C.; Corella, D.; Sánchez-González, C. Influence of Demographic and Lifestyle Variables on Plasma Magnesium Concentrations and Their Associations with Cardiovascular Risk Factors in a Mediterranean Population. Nutrients 2020, 12, 1018. [Google Scholar] [CrossRef]
- Bersohn, I.; Oelofse, P.J. Correlation of Serum-Magnesium and Serum-Cholesterol Levels in South African Bantu and European Subjects. Lancet 1957, 269, 1020–1021. [Google Scholar] [CrossRef]
- Petersen, B.; Christiansen, C.; Hansen, P.F. Treatment of Hypercholesterolaemia and Hypertriglyceridaemia with Magnesium. Acta Med. Scand. 1976, 200, 59–61. [Google Scholar] [CrossRef]
- Liu, A.; Xu, P.; Gong, C.; Zhu, Y.; Zhang, H.; Nie, W.; Zhou, X.; Liang, X.; Xu, Y.; Huang, C.; et al. High Serum Concentration of Selenium, but Not Calcium, Cobalt, Copper, Iron, and Magnesium, Increased the Risk of Both Hyperglycemia and Dyslipidemia in Adults: A Health Examination Center Based Cross-Sectional Study. J. Trace Elem. Med. Biol. 2020, 59, 126470. [Google Scholar] [CrossRef]
- Jin, H.; Nicodemus-Johnson, J. Gender and Age Stratified Analyses of Nutrient and Dietary Pattern Associations with Circulating Lipid Levels Identify Novel Gender and Age-Specific Correlations. Nutrients 2018, 10, 1760. [Google Scholar] [CrossRef] [PubMed]
- Itoh, K.; Kawasaka, T.; Nakamura, M. The Effects of High Oral Magnesium Supplementation on Blood Pressure, Serum Lipids and Related Variables in Apparently Healthy Japanese Subjects. Br. J. Nutr. 1997, 78, 737–750. [Google Scholar] [CrossRef]
- Marken, P.A.; Weart, C.W.; Carson, D.S.; Gums, J.G.; Lopes-Virella, M.F. Effects of Magnesium Oxide on the Lipid Profile of Healthy Volunteers. Atherosclerosis 1989, 77, 37–42. [Google Scholar] [CrossRef]
- Randell, E.W.; Mathews, M.; Gadag, V.; Zhang, H.; Sun, G. Relationship between Serum Magnesium Values, Lipids and Anthropometric Risk Factors. Atherosclerosis 2008, 196, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Guerrero-Romero, F.; Rodríguez-Morán, M. The Ratio Potassium-to-Magnesium Intake and High Blood Pressure. Eur. J. Clin. Invest. 2019, 49, e13093. [Google Scholar] [CrossRef]
- de Valk, H.W.; Bianchi, R.; van Rijn, H.J.; Erkelens, D.W. Acute Exogenous Elevation of Plasma Free Fatty Acids Does Not Influence the Plasma Magnesium Concentration. Clin. Chem. Lab. Med. 1998, 36, 115–117. [Google Scholar] [CrossRef]
- Aslanabadi, N.; Habibi Asl, B.; Bakhshalizadeh, B.; Ghaderi, F.; Nemati, M. Hypolipidemic Activity of a Natural Mineral Water Rich in Calcium, Magnesium, and Bicarbonate in Hyperlipidemic Adults. Adv. Pharm. Bull. 2014, 4, 303–307. [Google Scholar]
- Fu, Z.-Y.; Yang, F.L.; Hsu, H.-W.; Lu, Y.-F. Drinking Deep Seawater Decreases Serum Total and Low-Density Lipoprotein-Cholesterol in Hypercholesterolemic Subjects. J. Med. Food 2012, 15, 535–541. [Google Scholar] [CrossRef] [PubMed]
- Nerbrand, C.; Agréus, L.; Lenner, R.A.; Nyberg, P.; Svärdsudd, K. The Influence of Calcium and Magnesium in Drinking Water and Diet on Cardiovascular Risk Factors in Individuals Living in Hard and Soft Water Areas with Differences in Cardiovascular Mortality. BMC Public Health 2003, 3, 21. [Google Scholar] [CrossRef]
- Luoma, H.; Helminen, S.K.J.; Ranta, H.; Rytömaa, I.; Meurman, J.H. Relationships between the Fluoride and Magnesium Concentrations in Drinking Water and Some Components in Serum Related to Cardiovascular Diseases in Men from Four Rural Districts in Finland. Scand. J. Clin. Lab. Investig. 1973, 32, 217–224. [Google Scholar] [CrossRef] [PubMed]
- Balliett, M.; Burke, J.R. Changes in Anthropometric Measurements, Body Composition, Blood Pressure, Lipid Profile, and Testosterone in Patients Participating in a Low-Energy Dietary Intervention. J. Chiropr. Med. 2013, 12, 3–14. [Google Scholar] [CrossRef] [PubMed][Green Version]
- de Los Rios, M.G. Serum Magnesium and Serum Cholesterol Changes in Man. Am. J. Clin. Nutr. 1961, 9, 315–319. [Google Scholar] [CrossRef]
- Cocate, P.G.; Natali, A.J.; de Oliveira, A.; Longo, G.Z.; Rita de Cássia, G.A.; Maria do Carmo, G.P.; dos Santos, E.C.; Buthers, J.M.; de Oliveira, L.L.; Hermsdorff, H.H.M. Fruit and Vegetable Intake and Related Nutrients Are Associated with Oxidative Stress Markers in Middle-Aged Men. Nutrition 2014, 30, 660–665. [Google Scholar] [CrossRef]
- Ruel, G.; Shi, Z.; Zhen, S.; Zuo, H.; Kröger, E.; Sirois, C.; Lévesque, J.-F.; Taylor, A.W. Association between Nutrition and the Evolution of Multimorbidity: The Importance of Fruits and Vegetables and Whole Grain Products. Clin. Nutr. 2014, 33, 513–520. [Google Scholar] [CrossRef] [PubMed]
- Bain, L.K.M.; Myint, P.K.; Jennings, A.; Lentjes, M.A.H.; Luben, R.N.; Khaw, K.-T.; Wareham, N.J.; Welch, A.A. The Relationship between Dietary Magnesium Intake, Stroke and Its Major Risk Factors, Blood Pressure and Cholesterol, in the EPIC-Norfolk Cohort. Int. J. Cardiol. 2015, 196, 108–114. [Google Scholar] [CrossRef]
- Samavarchi Tehrani, S.; Khatami, S.H.; Saadat, P.; Sarfi, M.; Ahmadi Ahangar, A.; Daroie, R.; Firouzjahi, A.; Maniati, M. Association of Serum Magnesium Levels with Risk Factors, Severity and Prognosis in Ischemic and Hemorrhagic Stroke Patients. Caspian J. Intern. Med. 2020, 11, 83–91. [Google Scholar] [PubMed]
- Kim, D.S.; Burt, A.A.; Ranchalis, J.E.; Jarvik, L.E.; Eintracht, J.F.; Furlong, C.E.; Jarvik, G.P. Effects of Dietary Components on High-Density Lipoprotein Measures in a Cohort of 1,566 Participants. Nutr. Metab. 2014, 11, 44. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.-H.; Choi, M.-K. Seven Dietary Minerals (Ca, P, Mg, Fe, Zn, Cu, and Mn) and Their Relationship with Blood Pressure and Blood Lipids in Healthy Adults with Self-Selected Diet. Biol. Trace Elem. Res. 2013, 153, 69–75. [Google Scholar] [CrossRef]
- Cao, Y.; Wang, C.; Guan, K.; Xu, Y.; Su, Y.-X.; Chen, Y.-M. Association of Magnesium in Serum and Urine with Carotid Intima-Media Thickness and Serum Lipids in Middle-Aged and Elderly Chinese: A Community-Based Cross-Sectional Study. Eur. J. Nutr. 2016, 55, 219–226. [Google Scholar] [CrossRef]
- López-González, B.; Molina-López, J.; Florea, D.I.; Quintero-Osso, B.; Pérez de la Cruz, A.; Planells del Pozo, E.M. Association between Magnesium-Deficient Status and Anthropometric and Clinical-Nutritional Parameters in Posmenopausal Women. Nutr. Hosp. 2014, 29, 658–664. [Google Scholar] [PubMed]
- Yamori, Y.; Sagara, M.; Mizushima, S.; Liu, L.; Ikeda, K.; Nara, Y.; CARDIAC Study Group. An Inverse Association between Magnesium in 24-h Urine and Cardiovascular Risk Factors in Middle-Aged Subjects in 50 CARDIAC Study Populations. Hypertens. Res. 2015, 38, 219–225. [Google Scholar] [CrossRef] [PubMed]
- Guerrero-Romero, F.; Rodriguez-Moran, M. Serum Magnesium in the Metabolically-Obese Normal-Weight and Healthy-Obese Subjects. Eur. J. Intern. Med. 2013, 24, 639–643. [Google Scholar] [CrossRef] [PubMed]
- Lefebvre, P.; Letois, F.; Sultan, A.; Nocca, D.; Mura, T.; Galtier, F. Nutrient Deficiencies in Patients with Obesity Considering Bariatric Surgery: A Cross-Sectional Study. Surg. Obes. Relat. Dis. 2014, 10, 540–546. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Moran, M.; Guerrero-Romero, F. Oral Magnesium Supplementation Improves the Metabolic Profile of Metabolically Obese, Normal-Weight Individuals: A Randomized Double-Blind Placebo-Controlled Trial. Arch. Med. Res. 2014, 45, 388–393. [Google Scholar] [CrossRef]
- Joris, P.J.; Plat, J.; Bakker, S.J.L.; Mensink, R.P. Effects of Long-Term Magnesium Supplementation on Endothelial Function and Cardiometabolic Risk Markers: A Randomized Controlled Trial in Overweight/Obese Adults. Sci. Rep. 2017, 7, 106. [Google Scholar] [CrossRef]
- Guerrero-Romero, F.; Flores-García, A.; Saldaña-Guerrero, S.; Simental-Mendía, L.E.; Rodríguez-Morán, M. Obesity and Hypomagnesemia. Eur. J. Intern. Med. 2016, 34, 29–33. [Google Scholar] [CrossRef]
- Solati, M.; Kazemi, L.; Shahabi Majd, N.; Keshavarz, M.; Pouladian, N.; Soltani, N. Oral Herbal Supplement Containing Magnesium Sulfate Improve Metabolic Control and Insulin Resistance in Non-Diabetic Overweight Patients: A Randomized Double Blind Clinical Trial. Med. J. Islam. Repub. Iran 2019, 33, 2. [Google Scholar] [CrossRef]
- Farsinejad-Marj, M.; Azadbakht, L.; Mardanian, F.; Saneei, P.; Esmaillzadeh, A. Clinical and Metabolic Responses to Magnesium Supplementation in Women with Polycystic Ovary Syndrome. Biol. Trace Elem. Res. 2020, 196, 349–358. [Google Scholar] [CrossRef]
- Cutler, D.A.; Pride, S.M.; Cheung, A.P. Low Intakes of Dietary Fiber and Magnesium Are Associated with Insulin Resistance and Hyperandrogenism in Polycystic Ovary Syndrome: A Cohort Study. Food Sci. Nutr. 2019, 7, 1426–1437. [Google Scholar] [CrossRef]
- Jamilian, M.; Sabzevar, N.K.; Asemi, Z. The Effect of Magnesium and Vitamin E Co-Supplementation on Glycemic Control and Markers of Cardio-Metabolic Risk in Women with Polycystic Ovary Syndrome: A Randomized, Double-Blind, Placebo-Controlled Trial. Horm. Metab. Res. 2019, 51, 100–105. [Google Scholar] [CrossRef] [PubMed]
- Jamilian, M.; Maktabi, M.; Asemi, Z. A Trial on the Effects of Magnesium-Zinc-Calcium-Vitamin D Co-Supplementation on Glycemic Control and Markers of Cardio-Metabolic Risk in Women with Polycystic Ovary Syndrome. Arch. Iran. Med. 2017, 20, 640–645. [Google Scholar] [PubMed]
- Karandish, M.; Tamimi, M.; Shayesteh, A.A.; Haghighizadeh, M.H.; Jalali, M.T. The Effect of Magnesium Supplementation and Weight Loss on Liver Enzymes in Patients with Nonalcoholic Fatty Liver Disease. J. Res. Med. Sci. 2013, 18, 573–579. [Google Scholar] [PubMed]
- Ali, R.; Lee, E.T.; Knehans, A.W.; Zhang, Y.; Yeh, J.; Rhoades, E.R.; Jobe, J.B.; Ali, T.; Johnson, M.R. Dietary Intake among American Indians with Metabolic Syndrome—Comparison to Dietary Recommendations: The Balance Study. Int. J. Health Nutr. 2013, 4, 33–45. [Google Scholar]
- Vajdi, M.; Farhangi, M.A.; Nikniaz, L. Diet-Derived Nutrient Patterns and Components of Metabolic Syndrome: A Cross-Sectional Community- Based Study. BMC Endocr. Disord. 2020, 20, 69. [Google Scholar] [CrossRef]
- Akbarzade, Z.; Amini, M.R.; Djafari, F.; Yarizadeh, H.; Mohtashaminia, F.; Majdi, M.; Bazshahi, E.; Djafarian, K.; Clark, C.C.T.; Shab-Bidar, S. Association of Nutrient Patterns with Metabolic Syndrome and Its Components in Iranian Adults. Clin. Nutr. Res. 2020, 9, 318–331. [Google Scholar] [CrossRef]
- Mottaghian, M.; Salehi, P.; Teymoori, F.; Mirmiran, P.; Hosseini-Esfahani, F.; Azizi, F. Nutrient Patterns and Cardiometabolic Risk Factors among Iranian Adults: Tehran Lipid and Glucose Study. BMC Public Health 2020, 20, 653. [Google Scholar] [CrossRef]
- Choi, M.-K.; Bae, Y.-J. Relationship between Dietary Magnesium, Manganese, and Copper and Metabolic Syndrome Risk in Korean Adults: The Korea National Health and Nutrition Examination Survey (2007–2008). Biol. Trace Elem. Res. 2013, 156, 56–66. [Google Scholar] [CrossRef] [PubMed]
- Cano-Ibáñez, N.; Gea, A.; Ruiz-Canela, M.; Corella, D.; Salas-Salvadó, J.; Schröder, H.; Navarrete-Muñoz, E.M.; Romaguera, D.; Martínez, J.A.; Barón-López, F.J.; et al. Diet Quality and Nutrient Density in Subjects with Metabolic Syndrome: Influence of Socioeconomic Status and Lifestyle Factors. A Cross-Sectional Assessment in the PREDIMED-Plus Study. Clin. Nutr. 2020, 39, 1161–1173. [Google Scholar] [CrossRef]
- Choi, W.-S.; Kim, S.-H.; Chung, J.-H. Relationships of Hair Mineral Concentrations with Insulin Resistance in Metabolic Syndrome. Biol. Trace Elem. Res. 2014, 158, 323–329. [Google Scholar] [CrossRef] [PubMed]
- Vanaelst, B.; Huybrechts, I.; Michels, N.; Flórez, M.R.; Aramendía, M.; Balcaen, L.; Resano, M.; Vanhaecke, F.; Bammann, K.; Bel-Serrat, S.; et al. Hair Minerals and Metabolic Health in Belgian Elementary School Girls. Biol. Trace Elem. Res. 2013, 151, 335–343. [Google Scholar] [CrossRef]
- Sun, X.; Du, T.; Huo, R.; Yu, X.; Xu, L. Impact of HbA1c Criterion on the Definition of Glycemic Component of the Metabolic Syndrome: The China Health and Nutrition Survey 2009. BMC Public Health 2013, 13, 1045. [Google Scholar] [CrossRef] [PubMed]
- Lima de Souza, E.; Silva, M.d.L.; Cruz, T.; Rodrigues, L.E.; Ladeia, A.M.; Bomfim, O.; Olivieri, L.; Melo, J.; Correia, R.; Porto, M.; et al. Magnesium Replacement Does Not Improve Insulin Resistance in Patients with Metabolic Syndrome: A 12-Week Randomized Double-Blind Study. J. Clin. Med. Res. 2014, 6, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Rotter, I.; Kosik-Bogacka, D.; Dołęgowska, B.; Safranow, K.; Lubkowska, A.; Laszczyńska, M. Relationship between the Concentrations of Heavy Metals and Bioelements in Aging Men with Metabolic Syndrome. Int. J. Environ. Res. Public Health 2015, 12, 3944–3961. [Google Scholar] [CrossRef]
- Ghasemi, A.; Zahediasl, S.; Syedmoradi, L.; Azizi, F. Low Serum Magnesium Levels in Elderly Subjects with Metabolic Syndrome. Biol. Trace Elem. Res. 2010, 136, 18–25. [Google Scholar] [CrossRef]
- Evangelopoulos, A.A.; Vallianou, N.G.; Panagiotakos, D.B.; Georgiou, A.; Zacharias, G.A.; Alevra, A.N.; Zalokosta, G.J.; Vogiatzakis, E.D.; Avgerinos, P.C. An Inverse Relationship between Cumulating Components of the Metabolic Syndrome and Serum Magnesium Levels. Nutr. Res. 2008, 28, 659–663. [Google Scholar] [CrossRef]
- Guerrero-Romero, F.; Rodríguez-Morán, M. Low Serum Magnesium Levels and Metabolic Syndrome. Acta Diabetol. 2002, 39, 209–213. [Google Scholar] [CrossRef]
- Yuan, Z.; Liu, C.; Tian, Y.; Zhang, X.; Ye, H.; Jin, L.; Ruan, L.; Sun, Z.; Zhu, Y. Higher Levels of Magnesium and Lower Levels of Calcium in Whole Blood Are Positively Correlated with the Metabolic Syndrome in a Chinese Population: A Case-Control Study. Ann. Nutr. Metab. 2016, 69, 125–134. [Google Scholar] [CrossRef]
- Rotter, I.; Kosik-Bogacka, D.; Dołęgowska, B.; Safranow, K.; Karakiewicz, B.; Laszczyńska, M. Relationship between Serum Magnesium Concentration and Metabolic and Hormonal Disorders in Middle-Aged and Older Men. Magnes. Res. 2015, 28, 99–107. [Google Scholar] [CrossRef]
- van Dijk, P.R.; Schutten, J.C.; Jeyarajah, E.J.; Kootstra-Ros, J.E.; Connelly, M.A.; Bakker, S.J.L.; Dullaart, R.P.F. Blood Mg2+ Is More Closely Associated with Hyperglycaemia than with Hypertriacylglycerolaemia: The PREVEND Study. Diabetologia 2019, 62, 1732–1734. [Google Scholar] [CrossRef]
- Rusu, M.; Cristea, V.; Frenţiu, T.; Măruţoiu, C.; Rusu, L.D. Magnesium and Selenium in Diabetics with Peripheral Artery Disease of the Lower Limbs. Clujul Med. 2013, 86, 235–239. [Google Scholar]
- Spiga, R.; Mannino, G.C.; Mancuso, E.; Averta, C.; Paone, C.; Rubino, M.; Sciacqua, A.; Succurro, E.; Perticone, F.; Andreozzi, F.; et al. Are Circulating Mg2+ Levels Associated with Glucose Tolerance Profiles and Incident Type 2 Diabetes? Nutrients 2019, 11, 2460. [Google Scholar] [CrossRef]
- Esmeralda, C.A.C.; David, P.E.; Maldonado, I.C.; Ibrahim, S.N.A.; David, A.S.; Escorza, M.A.Q.; Dealmy, D.G. Deranged Fractional Excretion of Magnesium and Serum Magnesium Levels in Relation to Retrograde Glycaemic Regulation in Patients with Type 2 Diabetes Mellitus. Curr. Diabetes Rev. 2021, 17, 91–100. [Google Scholar] [CrossRef] [PubMed]
- Niranjan, G.; Srinivasan, A.R.; Srikanth, K.; Pruthu, G.; Reeta, R.; Ramesh, R.; Anitha, R.; Valli, V.M. Evaluation of Circulating Plasma VEGF-A, ET-1 and Magnesium Levels as the Predictive Markers for Proliferative Diabetic Retinopathy. Indian J. Clin. Biochem. 2019, 34, 352–356. [Google Scholar] [CrossRef]
- Hruby, A.; Guasch-Ferré, M.; Bhupathiraju, S.N.; Manson, J.E.; Willett, W.C.; McKeown, N.M.; Hu, F.B. Magnesium Intake, Quality of Carbohydrates, and Risk of Type 2 Diabetes: Results from Three U.s. Cohorts. Diabetes Care 2017, 40, 1695–1702. [Google Scholar] [CrossRef]
- Anetor, J.I.; Senjobi, A.; Ajose, O.A.; Agbedana, E.O. Decreased Serum Magnesium and Zinc Levels: Atherogenic Implications in Type-2 Diabetes Mellitus in Nigerians. Nutr. Health 2002, 16, 291–300. [Google Scholar] [CrossRef]
- Corica, F.; Corsonello, A.; Ientile, R.; Cucinotta, D. Serum ionized magnesium levels in relation to metabolic syndrome in type 2 diabetic patients. J. Am. Col. Nutr. 2006, 25, 210–215. [Google Scholar] [CrossRef]
- Guerrero-Romero, F.; Rodríguez-Morán, M. Hypomagnesemia Is Linked to Low Serum HDL-Cholesterol Irrespective of Serum Glucose Values. J. Diabetes Complicat. 2000, 14, 272–276. [Google Scholar] [CrossRef]
- Yu, L.; Zhang, J.; Wang, L.; Li, S.; Zhang, Q.; Xiao, P.; Wang, K.; Zhuang, M.; Jiang, Y. Association between Serum Magnesium and Blood Lipids: Influence of Type 2 Diabetes and Central Obesity. Br. J. Nutr. 2018, 120, 250–258. [Google Scholar] [CrossRef]
- Kurstjens, S.; de Baaij, J.H.F.; Bouras, H.; Bindels, R.J.M.; Tack, C.J.J.; Hoenderop, J.G.J. Determinants of Hypomagnesemia in Patients with Type 2 Diabetes Mellitus. Eur. J. Endocrinol. 2017, 176, 11–19. [Google Scholar] [CrossRef]
- Rasheed, H.; Elahi, S.; Ajaz, H. Serum Magnesium and Atherogenic Lipid Fractions in Type II Diabetic Patients of Lahore, Pakistan. Biol. Trace Elem. Res. 2012, 148, 165–169. [Google Scholar] [CrossRef]
- Srinivasan, A.R.; Niranjan, G.; Kuzhandai Velu, V.; Parmar, P.; Anish, A. Status of Serum Magnesium in Type 2 Diabetes Mellitus with Particular Reference to Serum Triacylglycerol Levels. Diabetes Metab. Syndr. 2012, 6, 187–189. [Google Scholar] [CrossRef]
- Pokharel, D.R.; Khadka, D.; Sigdel, M.; Yadav, N.K.; Kafle, R.; Sapkota, R.M.; Jha, S.K. Association of Serum Magnesium Level with Poor Glycemic Control and Renal Functions in Nepalese Patients with Type 2 Diabetes Mellitus. Diabetes Metab. Syndr. 2017, 11, S417–S423. [Google Scholar] [CrossRef]
- Hyassat, D.; Al Sitri, E.; Batieha, A.; El-Khateeb, M.; Ajlouni, K. Prevalence of Hypomagnesaemia among Obese Type 2 Diabetic Patients Attending the National Center for Diabetes, Endocrinology and Genetics (NCDEG). Int. J. Endocrinol. Metab. 2014, 12, e17796. [Google Scholar] [CrossRef]
- Waanders, F.; Dullaart, R.P.F.; Vos, M.J.; Hendriks, S.H.; van Goor, H.; Bilo, H.J.G.; van Dijk, P.R. Hypomagnesaemia and Its Determinants in a Contemporary Primary Care Cohort of Persons with Type 2 Diabetes. Endocrine 2020, 67, 80–86. [Google Scholar] [CrossRef]
- Huang, J.-H.; Lu, Y.-F.; Cheng, F.-C.; Lee, J.N.-Y.; Tsai, L.-C. Correlation of Magnesium Intake with Metabolic Parameters, Depression and Physical Activity in Elderly Type 2 Diabetes Patients: A Cross-Sectional Study. Nutr. J. 2012, 11, 41. [Google Scholar] [CrossRef]
- Corsonello, A.; Ientile, R.; Buemi, M.; Cucinotta, D.; Mauro, V.N.; Macaione, S.; Corica, F. Serum Ionized Magnesium Levels in Type 2 Diabetic Patients with Microalbuminuria or Clinical Proteinuria. Am. J. Nephrol. 2000, 20, 187–192. [Google Scholar] [CrossRef]
- Shardha, A.K.; Vaswani, A.S.; Faraz, A.; Alam, M.T.; Kumar, P. Frequency and Risk Factors Associated with Hypomagnesaemia in Hypokalemic Type-2 Diabetic Patients. J. Coll. Physicians Surg. Pak. 2014, 24, 830–835. [Google Scholar]
- Song, Y.; He, K.; Levitan, E.B.; Manson, J.E.; Liu, S. Effects of Oral Magnesium Supplementation on Glycaemic Control in Type 2 Diabetes: A Meta-Analysis of Randomized Double-Blind Controlled Trials: Review Article. Diabet. Med. 2006, 23, 1050–1056. [Google Scholar] [CrossRef]
- Hamedifard, Z.; Farrokhian, A.; Reiner, Ž.; Bahmani, F.; Asemi, Z.; Ghotbi, M.; Taghizadeh, M. The Effects of Combined Magnesium and Zinc Supplementation on Metabolic Status in Patients with Type 2 Diabetes Mellitus and Coronary Heart Disease. Lipids Health Dis. 2020, 19, 112. [Google Scholar] [CrossRef]
- Al-Daghri, N.M.; Alkharfy, K.M.; Khan, N.; Alfawaz, H.A.; Al-Ajlan, A.S.; Yakout, S.M.; Alokail, M.S. Vitamin D Supplementation and Serum Levels of Magnesium and Selenium in Type 2 Diabetes Mellitus Patients: Gender Dimorphic Changes. Int. J. Vitam. Nutr. Res. 2014, 84, 27–34. [Google Scholar] [CrossRef]
- Rashvand, S.; Mobasseri, M.; Tarighat-Esfanjani, A. Effects of Choline and Magnesium Concurrent Supplementation on Coagulation and Lipid Profile in Patients with Type 2 Diabetes Mellitus: A Pilot Clinical Trial. Biol. Trace Elem. Res. 2020, 194, 328–335. [Google Scholar] [CrossRef]
- Whitfield, P.; Parry-Strong, A.; Walsh, E.; Weatherall, M.; Krebs, J.D. The Effect of a Cinnamon-, Chromium- and Magnesium-Formulated Honey on Glycaemic Control, Weight Loss and Lipid Parameters in Type 2 Diabetes: An Open-Label Cross-over Randomised Controlled Trial. Eur. J. Nutr. 2016, 55, 1123–1131. [Google Scholar] [CrossRef]
- Dehbalaei, M.G.; Ashtary-Larky, D.; Amarpoor Mesrkanlou, H.; Talebi, S.; Asbaghi, O. The Effects of Magnesium and Vitamin E Co-Supplementation on Some Cardiovascular Risk Factors: A Meta-Analysis. Clin. Nutr. Espen 2021, 41, 110–117. [Google Scholar] [CrossRef]
- Yokota, K.; Kato, M.; Lister, F.; Ii, H.; Hayakawa, T.; Kikuta, T.; Kageyama, S.; Tajima, N. Clinical Efficacy of Magnesium Supplementation in Patients with Type 2 Diabetes. J. Am. Coll. Nutr. 2004, 23, 506S–509S. [Google Scholar] [CrossRef] [PubMed]
- Djurhuus, M.S.; Klitgaard, N.A.; Pedersen, K.K.; Blaabjerg, O.; Altura, B.M.; Altura, B.T.; Henriksen, J.E. Magnesium Reduces Insulin-Stimulated Glucose Uptake and Serum Lipid Concentrations in Type 1 Diabetes. Metabolism 2001, 50, 1409–1417. [Google Scholar] [CrossRef]
- Ham, J.Y.; Shon, Y.H. Natural Magnesium-Enriched Deep-Sea Water Improves Insulin Resistance and the Lipid Profile of Prediabetic Adults: A Randomized, Double-Blinded Crossover Trial. Nutrients 2020, 12, 515. [Google Scholar] [CrossRef]
- Cosaro, E.; Bonafini, S.; Montagnana, M.; Danese, E.; Trettene, M.S.; Minuz, P.; Delva, P.; Fava, C. Effects of Magnesium Supplements on Blood Pressure, Endothelial Function and Metabolic Parameters in Healthy Young Men with a Family History of Metabolic Syndrome. Nutr. Metab. Cardiovasc. Dis. 2014, 24, 1213–1220. [Google Scholar] [CrossRef]
- Asemi, Z.; Karamali, M.; Jamilian, M.; Foroozanfard, F.; Bahmani, F.; Heidarzadeh, Z.; Benisi-Kohansal, S.; Surkan, P.J.; Esmaillzadeh, A. Magnesium Supplementation Affects Metabolic Status and Pregnancy Outcomes in Gestational Diabetes: A Randomized, Double-Blind, Placebo-Controlled Trial. Am. J. Clin. Nutr. 2015, 102, 222–229. [Google Scholar] [CrossRef]
- Navarrete-Cortes, A.; Ble-Castillo, J.L.; Guerrero-Romero, F.; Cordova-Uscanga, R.; Juárez-Rojop, I.E.; Aguilar-Mariscal, H.; Tovilla-Zarate, C.A.; Lopez-Guevara, M.D.R. No Effect of Magnesium Supplementation on Metabolic Control and Insulin Sensitivity in Type 2 Diabetic Patients with Normomagnesemia. Magnes. Res. 2014, 27, 48–56. [Google Scholar] [CrossRef]
- Guerrero-Romero, F.; Simental-Mendía, L.E.; Hernández-Ronquillo, G.; Rodriguez-Morán, M. Oral Magnesium Supplementation Improves Glycaemic Status in Subjects with Prediabetes and Hypomagnesaemia: A Double-Blind Placebo-Controlled Randomized Trial. Diabetes Metab. 2015, 41, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Solati, M.; Ouspid, E.; Hosseini, S.; Soltani, N.; Keshavarz, M.; Dehghani, M. Oral Magnesium Supplementation in Type II Diabetic Patients. Med. J. Islam. Repub. Iran 2014, 28, 67. [Google Scholar]
- de Valk, H.W.; Verkaaik, R.; van Rijn, H.J.; Geerdink, R.A.; Struyvenberg, A. Oral Magnesium Supplementation in Insulin-Requiring Type 2 Diabetic Patients. Diabet. Med. 1998, 15, 503–507. [Google Scholar] [CrossRef]
- Eriksson, J.; Kohvakka, A. Magnesium and Ascorbic Acid Supplementation in Diabetes Mellitus. Ann. Nutr. Metab. 1995, 39, 217–223. [Google Scholar] [CrossRef]
- Talari, H.R.; Zakizade, M.; Soleimani, A.; Bahmani, F.; Ghaderi, A.; Mirhosseini, N.; Eslahi, M.; Babadi, M.; Mansournia, M.A.; Asemi, Z. Effects of Magnesium Supplementation on Carotid Intima-Media Thickness and Metabolic Profiles in Diabetic Haemodialysis Patients: A Randomised, Double-Blind, Placebo-Controlled Trial. Br. J. Nutr. 2019, 121, 809–817. [Google Scholar] [CrossRef] [PubMed]
- Afzali, H.; Jafari Kashi, A.H.; Momen-Heravi, M.; Razzaghi, R.; Amirani, E.; Bahmani, F.; Gilasi, H.R.; Asemi, Z. The Effects of Magnesium and Vitamin E Co-Supplementation on Wound Healing and Metabolic Status in Patients with Diabetic Foot Ulcer: A Randomized, Double-Blind, Placebo-Controlled Trial: Supplementation and Diabetic Foot. Wound Repair Regen. 2019, 27, 277–284. [Google Scholar] [CrossRef]
- Brandão-Lima, P.N.; Carvalho, G.B.d.; Santos, R.K.F.; Santos, B.D.C.; Dias-Vasconcelos, N.L.; Rocha, V.D.S.; Barbosa, K.B.F.; Pires, L.V. Intakes of Zinc, Potassium, Calcium, and Magnesium of Individuals with Type 2 Diabetes Mellitus and the Relationship with Glycemic Control. Nutrients 2018, 10, 1948. [Google Scholar] [CrossRef]
- Karamali, M.; Bahramimoghadam, S.; Sharifzadeh, F.; Asemi, Z. Magnesium–Zinc–Calcium–Vitamin D Co-Supplementation Improves Glycemic Control and Markers of Cardiometabolic Risk in Gestational Diabetes: A Randomized, Double-Blind, Placebo-Controlled Trial. Appl. Physiol. Nutr. Metab. 2018, 43, 565–570. [Google Scholar] [CrossRef]
- Sadeghian, M.; Azadbakht, L.; Khalili, N.; Mortazavi, M.; Esmaillzadeh, A. Oral Magnesium Supplementation Improved Lipid Profile but Increased Insulin Resistance in Patients with Diabetic Nephropathy: A Double-Blind Randomized Controlled Clinical Trial. Biol. Trace Elem. Res. 2020, 193, 23–35. [Google Scholar] [CrossRef]
- An, G.; Du, Z.; Meng, X.; Guo, T.; Shang, R.; Li, J.; An, F.; Li, W.; Zhang, C. Association between Low Serum Magnesium Level and Major Adverse Cardiac Events in Patients Treated with Drug-Eluting Stents for Acute Myocardial Infarction. PLoS ONE 2014, 9, e98971. [Google Scholar] [CrossRef]
- Qazmooz, H.A.; Smesam, H.N.; Mousa, R.F.; Al-Hakeim, H.K.; Maes, M. Trace Element, Immune and Opioid Biomarkers of Unstable Angina, Increased Atherogenicity and Insulin Resistance: Results of Machine Learning. J. Trace Elem. Med. Biol. 2021, 64, 126703. [Google Scholar] [CrossRef]
- Brown, D. Magnesium-Lipid Relations in Health and in Patients with Myocardial Infarction. Lancet 1958, 272, 933–935. [Google Scholar] [CrossRef]
- Mahalle, N.; Kulkarni, M.V.; Naik, S.S. Is Hypomagnesaemia a Coronary Risk Factor among Indians with Coronary Artery Disease? J. Cardiovasc. Dis. Res. 2012, 3, 280–286. [Google Scholar] [CrossRef]
- Liao, F.; Folsom, A.R.; Brancati, F.L. Is Low Magnesium Concentration a Risk Factor for Coronary Heart Disease? The Atherosclerosis Risk in Communities (ARIC) Study. Am. Heart J. 1998, 136, 480–490. [Google Scholar] [CrossRef]
- Farshidi, H.; Sobhani, A.R.; Eslami, M.; Azarkish, F.; Eftekhar, E.; Keshavarz, M.; Soltani, N. Magnesium Sulfate Administration in Moderate Coronary Artery Disease Patients Improves Atherosclerotic Risk Factors: A Double-Blind Clinical Trial Study. J. Cardiovasc. Pharmacol. 2020, 76, 321–328. [Google Scholar] [CrossRef] [PubMed]
- Petersen, B.; Schroll, M.; Christiansen, C.; Transbol, I. Serum and Erythrocyte Magnesium in Normal Elderly Danish People. Relationship to Blood Pressure and Serum Lipids. Acta Med. Scand. 1977, 201, 31–34. [Google Scholar] [CrossRef] [PubMed]
- Posadas-Sánchez, R.; Posadas-Romero, C.; Cardoso-Saldaña, G.; Vargas-Alarcón, G.; Villarreal-Molina, M.T.; Pérez-Hernández, N.; Rodríguez-Pérez, J.M.; Medina-Urrutia, A.; Jorge-Galarza, E.; Juárez-Rojas, J.G.; et al. Serum Magnesium Is Inversely Associated with Coronary Artery Calcification in the Genetics of Atherosclerotic Disease (GEA) Study. Nutr. J. 2015, 15, 22. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.Y.; Hyun, Y.Y.; Lee, K.B.; Kim, H. Low Serum Magnesium Is Associated with Coronary Artery Calcification in a Korean Population at Low Risk for Cardiovascular Disease. Nutr. Metab. Cardiovasc. Dis. 2015, 25, 1056–1061. [Google Scholar] [CrossRef]
- Zemel, P.C.; Zemel, M.B.; Urberg, M.; Douglas, F.L.; Geiser, R.; Sowers, J.R. Metabolic and Hemodynamic Effects of Magnesium Supplementation in Patients with Essential Hypertension. Am. J. Clin. Nutr. 1990, 51, 665–669. [Google Scholar] [CrossRef]
- Motoyama, T.; Sano, H.; Fukuzaki, H. Oral Magnesium Supplementation in Patients with Essential Hypertension. Hypertension 1989, 13, 227–232. [Google Scholar] [CrossRef]
- Guerrero-Romero, F.; Rodríguez-Morán, M. The Effect of Lowering Blood Pressure by Magnesium Supplementation in Diabetic Hypertensive Adults with Low Serum Magnesium Levels: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial. J. Hum. Hypertens. 2009, 23, 245–251. [Google Scholar] [CrossRef]
- Esfandiari, S.; Bahadoran, Z.; Mirmiran, P.; Tohidi, M.; Azizi, F. Adherence to the Dietary Approaches to Stop Hypertension Trial (DASH) Diet Is Inversely Associated with Incidence of Insulin Resistance in Adults: The Tehran Lipid and Glucose Study. J. Clin. Biochem. Nutr. 2017, 61, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Cunha, A.R.; D’El-Rei, J.; Medeiros, F.; Umbelino, B.; Oigman, W.; Touyz, R.M.; Neves, M.F. Oral Magnesium Supplementation Improves Endothelial Function and Attenuates Subclinical Atherosclerosis in Thiazide-Treated Hypertensive Women. J. Hypertens. 2017, 35, 89–97. [Google Scholar] [CrossRef]
- Karppanen, H.; Tanskanen, A.; Tuomilehto, J.; Puska, P.; Vuori, J.; Jäntti, V.; Seppänen, M.-L. Safety and Effects of Potassium- and Magnesium-Containing Low Sodium Salt Mixtures. J. Cardiovasc. Pharmacol. 1984, 6, S236. [Google Scholar] [CrossRef]
- Delva, P.; Pastori, C.; Degan, M.; Montesi, G.; Lechi, A. Intralymphocyte Free Magnesium and Plasma Triglycerides. Life Sci. 1998, 62, 2231–2240. [Google Scholar] [CrossRef]
- Toprak, O.; Sarı, Y.; Koç, A.; Sarı, E.; Kırık, A. The Impact of Hypomagnesemia on Erectile Dysfunction in Elderly, Non-Diabetic, Stage 3 and 4 Chronic Kidney Disease Patients: A Prospective Cross-Sectional Study. Clin. Interv. Aging 2017, 12, 437–444. [Google Scholar] [CrossRef]
- Khatami, M.R.; Mirchi, E.; Khazaeipour, Z.; Abdollahi, A.; Jahanmardi, A. Association between Serum Magnesium and Risk Factors of Cardiovascular Disease in Hemodialysis Patients. Iran. J. Kidney Dis. 2013, 7, 47–52. [Google Scholar]
- Dey, R.; Rajappa, M.; Parameswaran, S.; Revathy, G. Hypomagnesemia and Atherogenic Dyslipidemia in Chronic Kidney Disease: Surrogate Markers for Increased Cardiovascular Risk. Clin. Exp. Nephrol. 2015, 19, 1054–1061. [Google Scholar] [CrossRef]
- Cambray, S.; Ibarz, M.; Bermudez-Lopez, M.; Marti-Antonio, M.; Bozic, M.; Fernandez, E.; Valdivielso, J.M. Magnesium Levels Modify the Effect of Lipid Parameters on Carotid Intima Media Thickness. Nutrients 2020, 12, 2631. [Google Scholar] [CrossRef]
- Gupta, B.K.; Glicklich, D.; Tellis, V.A. Magnesium Repletion Therapy Improves Lipid Metabolism in Hypomagnesemic Renal Transplant Recipients: A Pilot Study. Transplantation 1999, 67, 1485–1487. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Zhang, X.; Qi, H.; Wang, J.; Wang, M.; Zhang, Y.; Yan, H.; Zhuang, S. Correlation of Serum Magnesium with Cardiovascular Risk Factors in Maintenance Hemodialysis Patients--a Cross-Sectional Study. Magnes. Res. 2013, 26, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Han, Z.; Zhou, L.; Liu, R.; Feng, L. The Effect of Hemodialysis on Serum Magnesium Concentration in Hemodialysis Patients. Ann. Palliat. Med. 2020, 9, 1134–1143. [Google Scholar] [CrossRef] [PubMed]
- Mortazavi, M.; Moeinzadeh, F.; Saadatnia, M.; Shahidi, S.; McGee, J.C.; Minagar, A. Effect of Magnesium Supplementation on Carotid Intima-Media Thickness and Flow-Mediated Dilatation among Hemodialysis Patients: A Double-Blind, Randomized, Placebo-Controlled Trial. Eur. Neurol. 2013, 69, 309–316. [Google Scholar] [CrossRef]
- Shimohata, H.; Yamashita, M.; Ohgi, K.; Tsujimoto, R.; Maruyama, H.; Takayasu, M.; Hirayama, K.; Kobayashi, M. The Relationship between Serum Magnesium Levels and Mortality in Non-Diabetic Hemodialysis Patients: A 10-Year Follow-up Study. Hemodial. Int. 2019, 23, 369–374. [Google Scholar] [CrossRef]
- Robles, N.R.; Escola, J.M.; Albarran, L.; Espada, R. Correlation of Serum Magnesium and Serum Lipid Levels in Hemodialysis Patients. Nephron 1998, 78, 118–119. [Google Scholar] [CrossRef] [PubMed]
- Tamura, T.; Unagami, K.; Okazaki, M.; Komatsu, M.; Nitta, K. Serum Magnesium Levels and Mortality in Japanese Maintenance Hemodialysis Patients. Blood Purif. 2019, 47 (Suppl. 2), 88–94. [Google Scholar] [CrossRef]
- Ansari, M.R.; Maheshwari, N.; Shaikh, M.A.; Laghari, M.S.; Lal, K.; Ahmed, K. Correlation of Serum Magnesium with Dyslipidemia in Patients on Maintenance Hemodialysis. Saudi J. Kidney Dis. Transpl. 2012, 23, 21–25. [Google Scholar]
- Nasri, H.; Baradaran, A. Correlation of Serum Magnesium with Dyslipidemia in Maintenance Hemodialysis Patients. Acta Med. (Hradec Kral.) 2004, 47, 263–265. [Google Scholar] [CrossRef][Green Version]
- Ikee, R.; Toyoyama, T.; Endo, T.; Tsunoda, M.; Hashimoto, N. Impact of Sevelamer Hydrochloride on Serum Magnesium Concentrations in Hemodialysis Patients. Magnes. Res. 2016, 29, 184–190. [Google Scholar] [CrossRef]
- Mitwalli, A.H. Why Are Serum Magnesium Levels Lower in Saudi Dialysis Patients? J. Taibah Univ. Med. Sci. 2017, 12, 41–46. [Google Scholar] [CrossRef]
- Cai, K.; Luo, Q.; Dai, Z.; Zhu, B.; Fei, J.; Xue, C.; Wu, D. Hypomagnesemia Is Associated with Increased Mortality among Peritoneal Dialysis Patients. PLoS ONE 2016, 11, e0152488. [Google Scholar] [CrossRef]
- Barbagallo, M.; Veronese, N.; Dominguez, L.J. Magnesium in Aging, Health and Diseases. Nutrients 2021, 13, 463. [Google Scholar] [CrossRef]
- Barbagallo, M.; Di Bella, G.; Brucato, V.; D’Angelo, D.; Damiani, P.; Monteverde, A.; Belvedere, M.; Dominguez, L.J. Serum Ionized Magnesium in Diabetic Older Persons. Metabolism 2014, 63, 502–509. [Google Scholar] [CrossRef]
- Veronese, N.; Demurtas, J.; Pesolillo, G.; Celotto, S.; Barnini, T.; Calusi, G.; Caruso, M.G.; Notarnicola, M.; Reddavide, R.; Stubbs, B.; et al. Magnesium and Health Outcomes: An Umbrella Review of Systematic Reviews and Meta-Analyses of Observational and Intervention Studies. Eur. J. Nutr. 2020, 59, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Fiorentini, D.; Cappadone, C.; Farruggia, G.; Prata, C. Magnesium: Biochemistry, Nutrition, Detection, and Social Impact of Diseases Linked to Its Deficiency. Nutrients 2021, 13, 1136. [Google Scholar] [CrossRef] [PubMed]
- Găman, M.-A.; Cozma, M.-A.; Dobrică, E.-C.; Bacalbașa, N.; Bratu, O.G.; Diaconu, C.C. Dyslipidemia: A Trigger for Coronary Heart Disease in Romanian Patients with Diabetes. Metabolites 2020, 10, 195. [Google Scholar] [CrossRef] [PubMed]
- Frank, J.; Kisters, K.; Stirban, O.A.; Obeid, R.; Lorkowski, S.; Wallert, M.; Egert, S.; Podszun, M.C.; Eckert, G.P.; Pettersen, J.A.; et al. The Role of Biofactors in the Prevention and Treatment of Age-Related Diseases. Biofactors 2021. [Google Scholar] [CrossRef] [PubMed]
- Stepura, O.B.; Martynow, A.I. Magnesium Orotate in Severe Congestive Heart Failure (MACH). Int. J. Cardiol. 2009, 131, 293–295. [Google Scholar] [CrossRef] [PubMed]
- Kisters, K.; Gremmler, B.; Gröber, U. Magnesium deficiency in hypertensive heart disease. J. Hypertens. 2015, 33, e273. [Google Scholar] [CrossRef]

| Author and Year | Condition | Number of Patients | Method of Mg Determination | Main Results |
|---|---|---|---|---|
| Barragán et al. (2020) [8] | Cardiometabolic risk factors: T2DM, hypercholesterolemia, hypertension | 492 | Serum, urine (spectrometry) | Prevalence of hypoMg = 19% Hypercholesterolemia: Mg ↑; T2DM: Mg ↓ HypoMg-T2DM association (OR: 3.36, 95% CI: 1.26–8.96, p = 0.016) TC, LDL-C associated with Mg quartiles ↑ Hypercholesterolemia in 4th versus 1st quartile of Mg levels (OR: 3.12; 95% CI: 1.66–5.85, p < 0.001) |
| Bersohn and Oelofse (1957) [9] | Healthy | 100 | Serum (spectrophotometry) | Normal TC—normal Mg ↓ TC–↑ Mg Hypercholesterolemia: ↓ Mg |
| Petersen et al. (1976) [10] | Hypercholesterolemia Hypertriglyceridemia | 17 | Serum (spectrophotometry) | 3 g/day of MgO for 6 weeks: no effect on TC, TG |
| Liu et al. (2020) [11] | Dyslipidemia | 1466 | Serum (spectrophotometry) | ↑ TC, TG, HDL-C and LDL-C (p < 0.001) ↓ Mg (p = 0.002) ↑ Dyslipidemia in the 4th versus 1st Mg quartile (OR = 1.4, 95% CI 1.0–1.9, p = 0.023) |
| Jin and Nicodemus-Johnson (2018) [12] | Healthy | 12,284 | Serum (method unspecified) | (+) association of Mg intake and HDL-C in ♀ (−) association of Mg intake and TC/HDL-C ratio in ♀ (−) association of Mg intake and TG in ♀ and ♂ |
| Randell et al. (2008) [15] | Healthy | 1318 | Serum (spectroscopy) | (+) association of Mg and TC, HDL-C, LDL-C, TG |
| Guerrero-Romero et al. (2019) [16] | Healthy | 529 | Serum (method unspecified) | Mg and K supplementation ↓ TG |
| Fu et al. (2012) [19] | Healthy | 42 | Serum (method unspecified) | deep sea water (395 Mg mg/L) ↓ TC, LDL-C and HDL-C versus MgCl2 fortified (386 Mg mg/L) or reverse osmotic water |
| Nerbrand et al. (2003) [20] | CV risk factors | 207 | Serum, whole blood, muscle, urine (method unspecified) | No correlation of Mg content in water and CV risk factors |
| Luoma et al. (1973) [21] | CV risk factors | 300 | Serum (method unspecified) | No correlation of Mg in drinking water and CV risk factors (TG, TC) |
| Balliett et al. (2013) [22] | Healthy | 49 | Serum (method unspecified) | Low-energy dietary interventions (+ Mg) ↓ TC, LDL-C, TG and HDL-C |
| de Los Rios (1963) [23] | Schizophrenia | 28 | Serum (method unspecified) | Controlled diet (Mg > RDV): no associations of ΔTC and ΔMg |
| Cocate et al. (2013) [24] | Healthy | 296 | Serum (method unspecified) | Association of ↑Mg intake and oxLDL |
| Ruel et al. (2014) [25] | Multimorbidity, Hypercholesterolemia | 1020 | Serum (method unspecified) | ↑ consumption of cereals (r = 0.60, p < 0.0001), fruits and vegetables (r = 0.49, p < 0.0001) associated with ↑ Mg and ↓ multimorbidity |
| Bain et al. (2015) [26] | Healthy | 4443 | Serum (method unspecified) | Inverse correlation of Mg intake and TC in ♂ (p = 0.02) and ♀ (p = 0.04) |
| Samavarchi Tehrani et al. (2020) [27] | Dyslipidemia | 447 | Serum (method unspecified) | Mg levels associated with dyslipidemia in embolic stroke (p = 0.012) |
| Kim et al. (2014) [28] | Healthy | 1566 | Serum (method unspecified) | (+) association of Mg intake and HDL-C (p = 0.001), HDL-2 (p = 0.018), HDL-3 (p = 0.013) |
| Kim and Choi (2013) [29] | Healthy | 258 | Serum (method unspecified) | ↑ Mg intake, ↑ TG (p < 0.05), ↓ HDL-C (p < 0.01), ↑ AIP (p < 0.001) in ♂ |
| Cao et al. (2015) [30] | Healthy | 2837 | Serum, urine (method unspecified) | (+) association of ↑ serum Mg and TC (p < 0.001), HDL-C (p < 0.001), LDL-C (p = 0.001), TG (p < 0.001) (−) association of ↑ serum Mg and non-HDL-C/HDL-C (p = 0.003) (+) association of Mg/creatinine ratio in urine and TC (p = 0.004), HDL-C (p = 0.003) and LDL-C (p = 0.009) |
| López-González et al. (2014) [31] | Post-menopause | 78 | Serum (method unspecified) | Mg in red blood cells, not serum Mg, correlates with TG (r = 0.287, p = 0.011) |
| Yamori et al. [32] | Hypercholesterolemia | 4211 | Serum, urine (method unspecified) | ↑ hypercholesterolemia, ↑ TC in lower versus higher 24-h urinary Mg/creatinine ratios (p < 0.001 for trend for both) ↑ hypercholesterolemia in the lowest versus the highest quintiles of 24-h Mg/creatinine urinary ratios (OR = 2.73; 95% CI 2.03 to 3.67; p < 0.001) |
| Guerrero-Romero and Rodriguez-Moran (2013) [33] | Overweight/obesity | 427 | Serum (method unspecified) | NW and MHO: ↑ Mg (p = 0.04 and p = 0.01, respectively), ↓ TG (p < 0.0005 for both) MONW: (−) Mg-TG correlation Obese and non-obese: ↓ Mg associated with hypertriglyceridemia (OR = 1.61, 95% CI: 1.5–2.46 and OR = 6.67, 95% CI 2.1–20.4, respectively) |
| Lefebvre et al. (2014) [34] | Obesity | 267 | Serum (method unspecified) | No Mg-TG correlation in candidates for bariatric surgery |
| Guerrero-Romero et al. (2016) [37] | Obesity | 681 | Serum (method unspecified) | ↓ HDL-C, ↑ TG in ↓ Mg versus normal Mg groups |
| Farsinejad-Marj et al. (2020) [39] | PCOS | 60 | Serum (method unspecified) | 250 mg/day Mg oxide for 8 weeks: no effect on TC, HDL-C, LDL-C, TG, TC/HDL-C, TG/HDL-C |
| Cutler et al. (2019) [40] | PCOS | 137 | Serum (method unspecified) | Mg-rich diet ↓ insulin resistance and ↑ HDL-C (p = 0.02 for both) |
| Author and Year | Number of Patients | Method of Mg Determination | Main Results |
|---|---|---|---|
| Ali et al. (2013) [44] | 213 | Unspecified | 90% ♂ Mg intake < daily recommended dose (↓ whole grains, vegetable intake) |
| Vajdi et al. (2020) [45] | 588 | Unspecified | ↓ odds of MetS (p = 0.01), ↓ LDL-C (p = 0.04), in the 1st versus 4th quartile of plant source-based diets (↑ Mg) |
| Akbarzade et al. (2020) [46] | 850 | Unspecified | No association of nutrient patterns with ↑ Mg intake and MetS components |
| Mottaghian et al. (2020) [47] | 1637 | Unspecified | No association of Mg-rich dietary pattern and lipid profile changes ↑ TG (p < 0.05 for trend) across the quartiles of the Mg-rich nutrient pattern |
| Choi and Bae (2013) [48] | 5136 | Unspecified | ♀ and ♂: ↓ Mg intake, no link with MetS ♀ with ↓ HDL-C: ↓ Mg intake ♀ and ♂ with ↑ TG: no link with Mg intake |
| Cano-Ibáñez et al. (2019) [49] | 6646 | Unspecified | MetS: ↓ Mg intake ↓ Mg intake in ♂ and ↓ education |
| Choi et al. (2014) [50] | 456 | Serum (automatic analytical analyzer) | serum Mg similar in MetS versus controls ↓ hair Mg levels (p = 0.046) ↑ Na/Mg ratio (p = 0.013) in MetS (−) correlation of hair Mg and TG (r = −0.125, p < 0.05) |
| Vanaelst et al. (2012) [51] | 166 | Unspecified | (−) correlations of serum Mg and non-HDL-C (r = −0.170, p = 0.030), metabolic score (r = −0.257, p = 0.001) ↓ hair Mg (p = 0.015) in ♀ with metabolic score > 3 points |
| Sun et al. (2013) [52] | 7641 | Serum (biochemical analyzer) | ↓ Mg (p < 0.001), ↓ HDL-C, ↑ TC, ↑ TG, ↑ LDL-C |
| Rotter et al. (2015) [54] | 313 | Serum and whole blood (spectrometry) | ↓ Mg in MetS (p = 0.02), T2DM (p = 0.0001), HTN (p = 0.0001) (+) associations of Mg and TC (r = 0.25; p < 0.001), LDL-C (r = 0.26; p < 0.001) |
| Ghasemi et al. (2010) [55] | 137 | Serum (spectrometry) | ↓ Mg in patients > 60 years with MetS, T2DM and hyperglycemia |
| Evangelopoulos et al. (2008) [56] | 117 | Serum (colorimetric reaction) | (+) Mg-HDL-C association (r = 0.18; p = 0.05) |
| Guerrero-Romero and Rodríguez-Morán (2002) [57] | 576 | Serum (colorimetric assay) | (+) Mg-HDL-C association (r = 0.36, p < 0.05) (−) Mg-TC association (r = −0.29, p < 0.05) |
| Yuan et al. (2016) [58] | 408 | Serum (spectrometry) | (+) correlations: Mg-BMI (r = 0.128, p < 0.05), Mg-TC (r = 0.254, p < 0.05), Mg-LDL-C (r = 0.280, p < 0.05) |
| Rotter et al. (2016) [59] | 313 | Serum (spectrometry) | (+) correlations: Mg-TC (r = 0.25, p < 0.0001), Mg-LDL-C (r = 0.26, p < 0.0001) |
| Author and Year | Number of Patients | Method of Mg Determination | Main Results |
|---|---|---|---|
| van Dijk et al. (2019) [60] | 5568 | Serum (xylidyl blue test) | (−) correlation of Mg (measured by nuclear magnetic resonance spectroscopy and colorimetric assays) and TG (r = −0.184, p = 0.002 and r = −0.194, p = 0.001, respectively) |
| Rusu et al. (2013) [61] | 154 | Serum (automated multianalyzer) | T2DM + peripheral arterial disease: ↓ Mg (p < 0.01), ↓ HDL-C, ↑ TG, ↑ TC |
| Spiga et al. (2019) [62] | 589 | Serum (colorimetric assay) | ↓ Mg, ↓ HDL-C, ↑ TG in normal glucose tolerance → impaired fasting glucose → T2DM (p < 0.02, p < 0.01 and p < 0.001, respectively) (+) correlations: Mg and TC (r = 0.154, p < 0.001), HDL-C (r = 0.113, p < 0.01), LDL-C (r = 0.170, p < 0.001) ↑ Mg: ↓ risk of T2DM (OR = 0.765, 95% CI 0.629–0.932, p < 0.01) |
| Esmeralda et al. (2021) [63] | 62 | Serum and urine analysis (methods unspecified) | T2DM: ↑ TG (p = 0.004), ↑ fractional excretion of Mg (p = 0.01), ↓ serum Mg (p = 0.001) versus controls |
| Gopal et al. (2019) [64] | 90 | Serum (calmagite colorimetric test) | Mg concentrations predict proliferative retinopathy development in T2DM (optimum cut-off 1.7 mg/dL, sensitivity 92.86%, specificity 77.14%, AUC 0.837, SEM 0.06, 95% CI 0.70–0.92) Mg ↓: no retinopathy → non-proliferative retinopathy → proliferative retinopathy (p < 0.01) proliferative retinopathy: ↑ HDL-C (p < 0.05), similar TC, TG, LDL-C, VLDL |
| Hruby et al. (2017) [65] | 202,743 | Unspecified | 15% T2DM-risk ↓ in individuals with ↑ dietary intake of Mg ↑ Hypercholesterolemia in the 5th (12.7% for 427–498 mg/day) versus 1st first (8.7% for 242–275 mg/day) quartile of Mg intake |
| Anetor et al. (2002) [66] | 60 | Serum (spectrophotometry) | (+) association of Mg and TC (r = 0.6; p < 0.001) |
| Corica et al. (2006) [67] | 290 | Serum (ion selective analyzer) | ↓ Mg: ↓ HDL-C (p < 0.001) and ↑ TG (p < 0.001) |
| Romero and Moran (2000) [68] | 390 | Serum (chemical autoanalyzer) | ↓ Mg associated with ↓ HDL-C (p = 0.01 in T2DM; p = 0.05 in IFG; p = 0.03 for controls) |
| Yu et al. (2018) [69] | 8163 | Serum (xylidyl blue test) | ↑ serum lipids, except for HDL-C, across progressive Mg concentrations (from ↓ Mg of ≤0.65 mmol/L, normal 0.65–0.95 mmol/L, ↑ levels ≥0.95 mmol/L) (p < 0.05) ↑ TG, TC, HDL-C and LDL-C (Mg ≥0.95 mmol/L versus ↓ Mg, p < 0.05) |
| Kurstjens et al. (2016) [70] | 395 | Serum (spectrophotometry) | (−) negative correlation of Mg and TG (r = −0.273, p < 0.001) (+) positive correlation of Mg and HDL-C (r = 0.156, p = 0.002) |
| Author and Year | Number of Patients | Method of Mg Determination | Main Results |
|---|---|---|---|
| Rasheed et al. (2012) [71] | 319 | Serum (spectrophotometry) | ↑ prevalence of hypoMg in T2DM hypoMg: ↑ TG, ↑ LDL-C, ↓ HDL-C |
| Srinivasan el al. (2012) [72] | 30 | Serum (calmagite colorimetric test) | association of hypoMg and TG (p < 0.05) |
| Pokharel et al. (2017) [73] | 300 | Serum (xylidyl blue test) | ↑ prevalence of hypoMg in T2DM: 50% (−) correlation of Mg and TC (r = −0.219; p < 0.01), LDL-C (r = −0.168; p < 0.05) |
| Hyassat et al. (2014) [74] | 1105 | Serum (colorimetric assay) | ↑ prevalence of hypoMg in overweight/obese T2DM: 19% dyslipidemia, statin use associated with hypoMg (p = 0.022 and p < 0.001, respectively) hypoMg-statin use association (OR = 1.56, 95% CI: 1.1–2.2) |
| Waanders et al. (202p) [75] | 929 | Serum (colorimetric assay) | (+) associations of Mg and TC (r = 0.142, p < 0.001), TC/HDL-C ratio (r = 0.114, p < 0.001), LDL-C (r = 0.166, p < 0.001) stepwise multivariable regression: Mg associated with LDL-C (β = 0.141, p = 0.001) |
| Huang et al. (2012) [76] | 210 | Serum (methylthymol blue method) | T2DM, >65 years: insufficient Mg intake (>88%), hypoMg (37%) (+) association of Mg intake and HDL-C (r = 0.192; p = 0.005) |
| Corsonello et al. (2000) [77] | 110 | Serum (ion selective analyzer) | ↓ Mg, ↑ TG with the ↑ urinary protein loss (p < 0.001) hypoMg: ↑ TC |
| Shardha et al. (2014) [78] | 358 | Serum (method unspecified) | ↑ TG (p = 0.001), ↑ LDL-C (p < 0.001), ↓ HDL-C (p < 0.001) in T2DM + hypoK + hypoMg |
| Author and Year | Condition | Number of Patients | Method of Mg Determination | Main Results |
|---|---|---|---|---|
| Qazmooz et al. (2020) [101] | atherosclerosis versus unstable angina | 178 | Serum (spectrophotometry) | ↑ Mg in atherosclerosis versus controls and unstable angina Mg explained the variance in AIP (β = −0.205, t = −3.036, p = 0.003), Castelli index 1 (β = −0.179, t = −2.633, p = 0.009), Castelli index 2 (β = −0.143, t = −1.983, p = 0.049), HDL-C (β = 0.157, t = 2.106, p = 0.037) |
| Brown et al. (1958) [102] | myocardial infarction | 1225 | Serum (spectrophotometry) | Mg not associated with serum cholesterol, total lipids, α/β lipoproteins |
| Mahalle el al. (2012) [103] | cardiovascular disease | 300 | Serum (xylidyl blue test) | ↓ Mg: ↑ TC, ↑ LDL-C, ↑ VLDL, ↑ TG and ↓ HDL-C |
| Liao et al. (1998) [104] | CHD | 13,922 | Serum (calmagite colorimetric test) | ↑ Mg = ↑ TC, ↑ HDL-C, ↓ LDL-C |
| Petersen et al. (1977) [106] | CHD | 73 | Serum, erythrocytes (spectrophotometry) | (+) correlation of erythrocyte Mg and TC (r = 0.25, p < 0.05) |
| Posadas-Sanchez et al. (2016) [107] | CAC | 1276 | Serum (xylidyl blue test) | hypoMg and normoMg: similar LDL-C, HDL-C, TG, apolipoprotein A/B |
| Lee et al. (2015) [108] | CAC | 34,553 | Serum (colorimetric assay) | no TC, LDL-C, HDL-C difference across Mg subgroups: ↓ < 1.9 mg/dL, normal 1.9–2.3 mg/dL, ↑ > 2.3 mg/dL |
| Esfandiari et al. (2017) [112] | HTN | 927 | Unspecified | ↑ questionnaire-assessed DASH score = ↑ Mg and ↓ TC (p < 0.05) |
| Karppanen et al. (1984) [114] | HTN | 126 | Serum (method unspecified) | KCl–NaCl–MgCl2 salts versus common table salt (NaCl) ↑ Mg but no effect on TC, TG |
| Delva et al. (1998) [115] | HTN | 52 | Intralymphocyte (fluorimetric test) | ↓ intra-lymphocytic Mg associated with ↑ TG |
| Author and Year | Condition | Number of Patients | Method of Mg Determination | Main Results |
|---|---|---|---|---|
| Toprak et al. (2017) [116] | stage 3 and 4 CKD, erectile dysfunction | 372 | Unspecified | hypoMg: ↑ obesity (p = 0.003), ↑ MetS (p = 0.026), ↓ HDL-C (p = 0.009) |
| Khatami et al. (2013) [117] | end-stage renal disease + HD | 103 | Serum (spectrophotometry) | ↑ Mg = ↑ TC (p = 0.03), ↑ TG (p = 0.04) |
| Dey et al. (2015) [118] | CKD | 180 | Serum (chemical autoanalyzer) | ↓ serum and urinary Mg ↑ TC, LDL-C, non-HDL-C (p < 0.001 for all) (+) correlation of serum Mg and HDL-C (r = 0.326, p = 0.002) (−) correlations of serum Mg and TC (r = −0.247, p = 0.019), LDL-C (r = −0.303, p = 0.004), non-HDL-C (r = −0.289, p = 0.006), Framingham risk score (r = −0.939, p < 0.001), the presence of MetS (r = −0.830, p < 0.001), CKD severity (r = −0.245, p = 0.02) |
| Cambray et al. (2020) [119] | CKD | 1754 | Serum (Mg reagent) | ↑ CKD severity = ↑ Mg and ↑ TG (p < 0.001 for trend) ↑ CKD severity = ↓ TC, LDL-C, HDL-C (p < 0.001 for) associations of Mg with T2DM (r = −0.070, p = 0.003), HTN (r = 0.053, p = 0.028), BMI (r = −0.053, p = 0.027) association of CIMT and Mg-TC (β = 0.008, SE = 0.003, p = 0.011), Mg-HDL-C (β = −0.007, SE = 0.003, p = 0.016), Mg-LDL-C (β = −0.007, SE = 0.003, p = 0.03), Mg-TG (β = −0.0014, SE = 0.0005, p = 0.01) interactions |
| Gupta et al. (1999) [120] | kidney transplant | 14 | Serum (method unspecified) | MgO in hypoMg: ↓ TC, ↓ LDL-C |
| Liu et al. (2013) [121] | HD | 98 | Serum (colorimetric assay) | ↑ HDL-C (p < 0.05) in hypo- versus hyperMg similar LDL-C, TC, TG, lipoprotein-a (−) Mg-HDL-C correlation (r = −0.028, p = 0.024) |
| Han et al. (2020) [122] | HD | 148 | Serum (toluidine blue assay) | HD ↓ Mg (p < 0.05) pre-HD Mg correlated with TC [β = 0.03 (0.006, 0.05), p = 0.016; β = −0.003 (−0.004, −0.0009), p = 0.003; β = 0.03 (0.006, 0.05), p = 0.02] |
| Shimohata et al. (2019) [124] | HD | 83 | Serum (chemical autoanalyzer) | Mg-HDL-C association (r = 0.284, p = 0.009) multiple regression: no Mg-HDL-C (coefficient: 0.004; β = 0.196; p = 0.105) ↑ mortality for Mg < 2.5 versus ≥2.5 mg/dL (log rank = 4.951; p = 0.026) |
| Robles et al. (1997) [125] | HD | 25 | Serum (method unspecified) | ↓ Mg correlated with ↑ LDL-C, ↑ VLDL-C, ↑ apoB (p < 0.001) |
| Tamura et al. (2019) [126] | HD | 392 | Serum (method unspecified) | ↓ Mg associated with ↑ mortality (+) Mg–TC (p = 0.257) and Mg–TG (p = 0.0279) associations |
| Ansari et al. (2012) [127] | HD | 50 | Serum (standard method) | (+) correlations of Mg and lipoprotein-a (r = 0.40, p < 0.007), HDL-C (r = 0.31, p < 0.01), TG (r = 0.35, p < 0.005) |
| Baradaran and Nasri (2004) [128] | HD | 36 | Dialysis fluid (method unspecified) | (+) correlations of Mg and lipoprotein (a) (r = 0.65, p < 0.05), TG (r = 0.32, p < 0.05) |
| Ikee et al. (2016) [129] | HD | 86 | Serum (xylidyl blue test) | (+) association of Mg and. HDL-C (r = 0.315, p = 0.003) |
| Mitwalli et al. (2016) [130] | HD, PD | 115 | Dialysis fluid (Mg reagent) | Mg in PD compared to HD no associations of Mg and TC or TG variations |
| Cai et al. (2016) [131] | PD | 253 | Dialysis fluid (chemical autoanalyzer) | (+) association of hypoMg and TG (r = 0.160, p = 0.011) |
| Authors and Year | Country | Intervention | Duration | Condition | No. Subjects | Effects on the Lipid Profile |
|---|---|---|---|---|---|---|
| Itoh et al. (1997) [13] | Japan | Mg(OH)2 ~411–548 mg Mg/day | 4 weeks | Healthy | 33 | HDL-C, apoA1: ↑ LDL-C, TC/HDL-C: ↓ |
| Marken et al. (1989) [14] | USA | 800 mg/day MgO | 60 days | Healthy | 50 | TC, HDL-C, LDL-C, VLDL, TG: no effect |
| Aslanabadi et al. (2014) [18] | Iran | 1L/day Mg-rich miner water | 1 month | Dyslipidemia | 69 | TC, HDL-C, LDL-C, TG: no effect |
| Rodriguez-Moran and Guerrero-Romero (2014) [35] | Mexico | 30 mL/day MgCl2 5% solution ~382 mg Mg | 4 months | MONW + Hypomagnesemia | 47 | HDL-C: ↑ TG: ↓ |
| Joris et al. (2017) [36] | The Netherlands | 350 mg/day Mg | 24 weeks | Overweight/Obesity | 52 | TC, HDL-C, LDL-C, TG, non-esterified fatty acids: no effect |
| Solati et al. (2019) [38] | Iran | herbal supplement ~300 mg/day MgSO4 | 6 months | Overweight | 70 | HDL-C, HDL-C/TG: ↑ LDL-C, TG: ↓ |
| Jamilian et al. (2019) [41] | Iran | 250 mg/day Mg + 400 mg/day vitamin E | 12 weeks | PCOS | 60 | TG, VLDL: ↓ HDL-C, LDL-C, TC/HDL-C: no effect |
| Jamilian et al. (2017) [42] | Iran | 200 mg/day Mg + 800 mg/day Ca + 8 mg/day Zn + 400 IU vitamin D | 12 weeks | PCOS | 60 | TC, TG, VLDL: ↓ HDL-C, LDL-C: no effect |
| Karandish et al. (2013) [43] | Iran | 350 mg/day Mg + low-calorie diet + physical exercise | 90 days | NAFLD | 68 | TC, HDL-C, LDL-C, TG: no effect |
| de Lourdes Lima de Souza e Silva (2014) [53] | Brazil | 400 mg/day Mg chelate | 12 weeks | MetS | 72 | TC, HDL-C, LDL-C, TG: no effect |
| Hamedifard et al. (2020) [80] | Iran | 250 mg/day MgO + 150 mg/day ZnSO4 | 12 weeks | T2DM + CHD | 60 | HDL-C: ↑ TC, TC/HDL-C, LDL-C, VLDL, TG: no effect |
| Rashvand et al. (2019) [82] | Iran | 500 mg/day MgO + 1000 mg/day choline bitartrate | 2 months | T2DM | 96 | HDL-C: ↑ TG: ↓ TC, LDL-C/HDL-C, LDL-C: no effect |
| Whitfield et al. (2016) [83] | New Zealand | 53.5 g Mg, Cr, cinnamon enriched honey | 40 days | T2DM | 12 | TC, LDL-C: ↓ HDL-C, TG: no effect |
| Ham and Shon (2020) [87] | Korea | 440 mL/day Mg-enriched deep sea water | 8 weeks | Prediabetes | 74 | TC, LDL-C: ↓ HDL-C, TG: no effect |
| Cosaro et al. (2014) [88] | Italy | 16.2 mmol/day Mg pidolate | 8 weeks | Healthy men with a positive family history for T2DM/MetS | 14 | TC, HDL-C, LDL-C, TG: no effect |
| Asemi et al. (2015) [89] | Iran | 250 mg/day MgO | 6 weeks | Gestational diabetes + Mg deficiency | 70 | HDL-C, LDL-C, TC/HDL-C: no effect |
| Navarrete-Cortes et al. (2014) [90] | Mexico | 360 mg/day Mg lactate | 3 months | T2DM + normomagnesemia | 98 | TC, HDL-C, LDL-C, TG: no effect |
| Guerrero-Romero et al. (2015) [91] | Mexico | 30 mL/day MgCl2 5% solution ~382 mg of Mg | 4 months | Prediabetes + hypomagnesemia | 116 | HDL-C: ↑ TG: ↓ |
| Solati et al. (2014) [92] | Iran | 300 mg/day MgSO4 | 3 months | T2DM | 54 | LDL-C, non-HDL-C: ↓ TC, HDL-C, TG: no effect |
| De Valk et al. (1998) [93] | The Netherlands | 15 mmol/day Mg aspartate | 3 months | Controlled T2DM | 50 | TC, HDL-C, TG: no effect |
| Talari et al. (2019) [95] | Iran | 250 mg/day MgO | 24 weeks | T2DM + HD | 54 | TC, LDL-C ↓ |
| Afzali et al. (2019) [96] | Iran | 250 mg/day MgO + 400 IU/day vitamin E | 12 weeks | T2DM + diabetic foot | 57 | HDL-C: ↑ LDL-C, TG: ↓ |
| Karamali M. et al. (2018) [98] | Iran | 200 mg/day Mg + 800 mg/day Ca + 8 mg/day Zn + 400 IU vitamin D | 6 weeks | Gestational diabetes | 60 | VLDL, TG: ↓ |
| Sadeghian et al. (2020) [99] | Iran | 250 mg/day MgO | 12 weeks | T2DM nephropathy | 80 | TC, LDL-C, HDL-C, TC/HDL-C, TG: no effect |
| Farshidi et al. (2020) [105] | Iran | 300 mg/day MgSO4 | 6 months | CHD | 64 | HDL-C: ↑ oxLDL, TC/HDL-C, LDL-C: ↓ |
| Zemel et al. (1990) [109] | USA | 40 mmol/day Mg aspartate | 3 months | Hypertension | 13 | TC, HDL-C, LDL-C, TG: no effect |
| Guerrero-Romero and Rodriguez-Moran (2008) [111] | Mexico | 2.5 g/day MgCl2 (450 mg Mg) | 4 months | Hypertension | 82 | HDL-C: ↑ TG: no effect |
| Cunha et al. (2016) [113] | Brazil | 1200 mg/day Mg chelate | 6 months | Hypertension in women prescribed thiazides | 35 | HDL-C, LDL-C: no effect |
| Mortazavi et al. (2013) [123] | Iran | 440 mg MgO x3/week | 6 months | HD | 54 | LDL-C: ↓ TC, HDL-C, TG: no effect |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Găman, M.-A.; Dobrică, E.-C.; Cozma, M.-A.; Antonie, N.-I.; Stănescu, A.M.A.; Găman, A.M.; Diaconu, C.C. Crosstalk of Magnesium and Serum Lipids in Dyslipidemia and Associated Disorders: A Systematic Review. Nutrients 2021, 13, 1411. https://doi.org/10.3390/nu13051411
Găman M-A, Dobrică E-C, Cozma M-A, Antonie N-I, Stănescu AMA, Găman AM, Diaconu CC. Crosstalk of Magnesium and Serum Lipids in Dyslipidemia and Associated Disorders: A Systematic Review. Nutrients. 2021; 13(5):1411. https://doi.org/10.3390/nu13051411
Chicago/Turabian StyleGăman, Mihnea-Alexandru, Elena-Codruța Dobrică, Matei-Alexandru Cozma, Ninel-Iacobus Antonie, Ana Maria Alexandra Stănescu, Amelia Maria Găman, and Camelia Cristina Diaconu. 2021. "Crosstalk of Magnesium and Serum Lipids in Dyslipidemia and Associated Disorders: A Systematic Review" Nutrients 13, no. 5: 1411. https://doi.org/10.3390/nu13051411
APA StyleGăman, M.-A., Dobrică, E.-C., Cozma, M.-A., Antonie, N.-I., Stănescu, A. M. A., Găman, A. M., & Diaconu, C. C. (2021). Crosstalk of Magnesium and Serum Lipids in Dyslipidemia and Associated Disorders: A Systematic Review. Nutrients, 13(5), 1411. https://doi.org/10.3390/nu13051411