Clinical Usefulness of Anthropometric Indices to Predict the Presence of Prediabetes. Data from the ILERVAS Cohort
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design of the Study and Description of the Study Population
2.2. Prediabetes Screening
2.3. Anthropometry and Calculation of Indices
2.4. Statistical Analysis
2.5. Ethics Statement
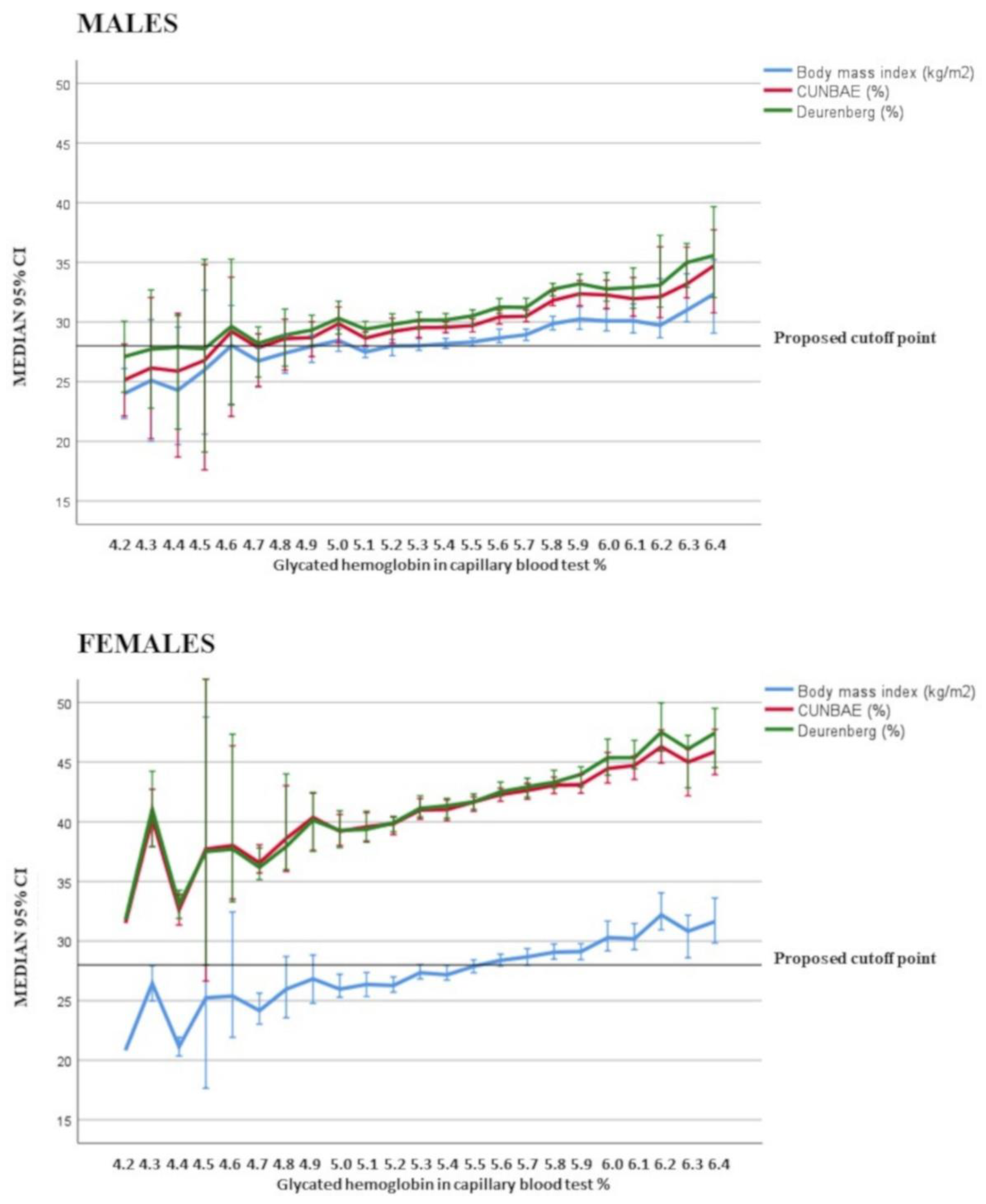
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cho, N.; Shaw, J.; Karuranga, S.; Huang, Y.; Fernandes, J.D.R.; Ohlrogge, A.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef]
- DeFronzo, R.A.; Abdul-Ghani, M.A. Preservation of β-Cell Function: The Key to Diabetes Prevention. J. Clin. Endocrinol. Metab. 2011, 96, 2354–2366. [Google Scholar] [CrossRef] [Green Version]
- Lee, C.C.; Perkins, B.A.; Kayaniyil, S.; Harris, S.B.; Retnakaran, R.; Gerstein, H.C.; Zinman, B.; Hanley, A.J. Peripheral Neuropathy and Nerve Dysfunction in Individuals at High Risk for Type 2 Diabetes: The PROMISE Cohort. Diabetes Care 2015, 38, 793–800. [Google Scholar] [CrossRef] [Green Version]
- Huang, Y.; Cai, X.; Mai, W.; Li, M.; Hu, Y. Association between prediabetes and risk of cardiovascular disease and all cause mortality: Systematic review and meta-analysis. BMJ 2016, 355, i5953. [Google Scholar] [CrossRef] [Green Version]
- Sánchez, E.; Collaborators, T.I.P.; Betriu, À.; López-Cano, C.; Hernández, M.; Fernández, E.; Purroy, F.; Bermúdez-López, M.; Farràs-Sallés, C.; Barril, S.; et al. Characteristics of atheromatosis in the prediabetes stage: A cross-sectional investigation of the ILERVAS project. Cardiovasc Diabetol. 2019, 18, 154. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sánchez, E.; Project, I.; Gutiérrez-Carrasquilla, L.; Barbé, F.; Betriu, À.; López-Cano, C.; Gaeta, A.M.; Purroy, F.; Pamplona, R.; Ortega, M.; et al. Lung function measurements in the prediabetes stage: Data from the ILERVAS Project. Acta Diabetol. 2019, 56, 1005–1012. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2021. Diabetes Care 2021, 44, S15–S33. [Google Scholar] [CrossRef]
- Machann, J.; Stefan, N.; Wagner, R.; Fritsche, A.; Bell, J.D.; Whitcher, B.; Häring, H.; Birkenfeld, A.L.; Nikolaou, K.; Schick, F.; et al. Normalized Indices Derived from Visceral Adipose Mass Assessed by Magnetic Resonance Imaging and Their Correlation with Markers for Insulin Resistance and Prediabetes. Nutrients 2020, 12, 2064. [Google Scholar] [CrossRef] [PubMed]
- Mahat, R.K.; Singh, N.; Arora, M.; Rathore, V. Health risks and interventions in prediabetes: A review. Diabetes Metab. Syndr. Clin. Res. Rev. 2019, 13, 2803–2811. [Google Scholar] [CrossRef]
- Zhao, X.; Zhu, X.; Zhang, H.; Zhao, W.; Li, J.; Shu, Y.; Li, S.; Yang, M.; Cai, L.; Zhou, J.; et al. Prevalence of diabetes and predictions of its risks using anthropometric measures in southwest rural areas of China. BMC Public Health 2012, 12, 821. [Google Scholar] [CrossRef] [Green Version]
- Li, S.; Xiao, J.; Ji, L.; Weng, J.; Jia, W.; Lu, J.; Zhou, Z.; Guo, X.; Liu, J.; Shan, Z.; et al. BMI and waist circumference are associated with impaired glucose metabolism and type 2 diabetes in normal weight Chinese adults. J. Diabetes its Complicat. 2014, 28, 470–476. [Google Scholar] [CrossRef] [Green Version]
- Haghighatdoost, F.; Amini, M.; Feizi, A.; Iraj, B. Are body mass index and waist circumference significant predictors of diabetes and prediabetes risk: Results from a population based cohort study. World J. Diabetes 2017, 8, 365–373. [Google Scholar] [CrossRef] [PubMed]
- Zhang, F.; Wan, Q.; Cao, H.; Tang, L.; Li, D.; Lü, Q.; Yan, Z.; Li, J.; Yang, Q.; Zhang, Y.; et al. Identical anthropometric characteristics of impaired fasting glucose combined with impaired glucose tolerance and newly diagnosed type 2 diabetes: Anthropometric indicators to predict hyperglycaemia in a community-based prospective cohort study in southwest China. BMJ Open. 2018, 8, e019735. [Google Scholar]
- Sangrós, F.J.; Torrecilla, J.; Giráldez-García, C.; Carrillo, L.; Mancera, J.; Mur, T.; Franch, J.; Díez, J.; Goday, A.; Serrano, R.; et al. Association of General and Abdominal Obesity With Hypertension, Dyslipidemia and Prediabetes in the PREDAPS Study. Rev. Española de Cardiol. (Engl. Ed.) 2018, 71, 170–177. [Google Scholar] [CrossRef]
- Blundell, J.E.; Dulloo, A.G.; Salvador, J.; Frühbeck, G. Beyond BMI-Phenotyping the Obesities. Obes. Facts 2014, 7, 322–328. [Google Scholar] [CrossRef] [PubMed]
- Ortega, F.B.; Sui, X.; Lavie, C.J.; Blair, S.N. Body Mass Index, the Most Widely Used but Also Widely Criticized Index: Would a Criteri-on Standard Measure of Total Body Fat Be a Better Predictor of Cardiovascular Disease Mortality? Mayo Clin. Proc. 2016, 91, 443–455. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kelly, T.L.; Wilson, K.E.; Heymsfield, S.B. Dual Energy X-Ray Absorptiometry Body Composition Reference Values from NHANES. PLoS ONE 2009, 4, e7038. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gomez-Ambrosi, J.; Silva, C.; Catalan, V.; Rodriguez, A.; Galofre, J.; Escalada, J.; Valenti, V.; Rotellar, F.; Romero, S.; Ramirez, B.; et al. Clinical Usefulness of a New Equation for Estimating Body Fat. Diabetes Care 2011, 35, 383–388. [Google Scholar] [CrossRef] [Green Version]
- Deurenberg, P.; Weststrate, J.A.; Seidell, J.C. Body mass index as a measure of body fatness: Age- and sex-specific prediction formulas. Br. J. Nutr. 1991, 65, 105–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Valdez, R. A simple model-based index of abdominal adiposity. J. Clin. Epidemiol. 1991, 44, 955–956. [Google Scholar] [CrossRef]
- Ashwell, M.; Gunn, P.; Gibson, S. Waist-to-height ratio is a better screening tool than waist circumference and BMI for adult cardiometabolic risk factors: Systematic review and meta-analysis. Obes. Rev. 2011, 13, 275–286. [Google Scholar] [CrossRef] [PubMed]
- Bonora, E.; Micciolo, R.; Ghiatas, A.A.; Lancaster, J.L.; Alyassin, A.; Muggeo, M.; DeFronzo, R.A. Is it possible to derive a reliable estimate of human visceral and subcutaneous abdominal adipose tissue from simple anthropometric measurements? Metabolism 1995, 44, 1617–1625. [Google Scholar] [CrossRef]
- Krakauer, N.Y.; Krakauer, J.C. A New Body Shape Index Predicts Mortality Hazard Independently of Body Mass Index. PLoS ONE 2012, 7, e39504. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.M.; Bredlau, C.; Bosy-Westphal, A.; Mueller, M.; Shen, W.; Gallagher, D.; Maeda, Y.; McDougall, A.; Peterson, C.M.; Ravussin, E.; et al. Relationships between body roundness with body fat and visceral adipose tissue emerging from a new geometrical model. Obesity 2013, 21, 2264–2271. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Després, J.P.; Couillard, C.; Gagnon, J.; Bergeron, J.; Leon, A.S.; Rao, D.C.; Skinner, J.S.; Wilmore, J.H.; Bouchard, C. Race, visceral adipose tissue, plasma lipids, and lipoprotein lipase activity in men and women: The Health, Risk Factors, Exercise Training, and Genetics (HERITAGE) family study. Arterioscler. Thromb. Vasc. Biol. 2000, 20, 1932–1938. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Betriu, À.; Farràs, C.; Abajo, M.; Martinez-Alonso, M.; Arroyo, D.; Barbé, F.; Buti, M.; Lecube, A.; Portero, M.; Purroy, F.; et al. Randomised intervention study to assess the prevalence of subclinical vascular disease and hidden kidney disease and its impact on morbidity and mortality: The ILERVAS project. Nefrología (Engl. Ed.) 2016, 36, 389–396. [Google Scholar] [CrossRef] [Green Version]
- Bermúdez-López, M.; Martínez-Alonso, M.; Castro-Boqué, E.; Betriu, À.; Cambray, S.; Farràs, C.; Barbé, F.; Pamplona, R.; Lecube, A.; Mauricio, D.; et al. Subclinical atheromatosis localization and burden in a low-to-moderate cardiovascular risk population: The ILERVAS study. Rev. Española de Cardiol. (Engl. Ed.) 2020, 27. [Google Scholar] [CrossRef]
- Lenters-Westra, E.; Slingerland, R.J. Three of 7 Hemoglobin A1c Point-of-Care Instruments Do Not Meet Generally Accepted Analytical Performance Criteria. Clin. Chem. 2014, 60, 1062–1072. [Google Scholar] [CrossRef]
- World Health Organization. Obesity: Preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ. Tech. Rep. Ser. 2000, 894, 1–253. [Google Scholar]
- Ma, W.-Y.; Yang, C.-Y.; Shih, S.-R.; Hsieh, H.-J.; Hung, C.S.; Chiu, F.-C.; Lin, M.-S.; Liu, P.-H.; Hua, C.-H.; Hsein, Y.-C.; et al. Measurement of Waist Circumference: Midabdominal or iliac crest? Diabetes Care 2013, 36, 1660–1666. [Google Scholar] [CrossRef] [Green Version]
- Ben-Noun, L.L.; Laor, A. Relationship between changes in neck circumference and cardiovascular risk factors. Exp. Clin. Cardiol. 2006, 11, 14–20. [Google Scholar]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.; Yngve, A.; Sallis, J.F.; et al. International physical activity questionnaire: 12-country reliability and validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [Green Version]
- Bermúdez, V.; Salazar, J.; Rojas, J.; Calvo, M.; Rojas, M.; Chávez-Castillo, M.; Añez, R.; Cabrera, M. Diabetes and Impaired Fasting Glucose Prediction Using Anthropometric Indices in Adults from Maracaibo City, Venezuela. J. Community Health 2016, 41, 1223–1233. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.O.; Galloway, J.M.; Goley, A.; Marrero, D.G.; Minners, R.; Montgomery, B.; Peterson, G.E.; Ratner, R.E.; Sanchez, E.; Aroda, V.R. Scientific Statement: Socioecological Determinants of Prediabetes and Type 2 Diabetes. Diabetes Care 2013, 36, 2430–2439. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Julian, V.; Blondel, R.; Pereira, B.; Thivel, D.; Boirie, Y.; Duclos, M. Body Composition Is Altered in Pre-Diabetic Patients with Impaired Fasting Glucose Tolerance: Results from the NHANES Survey. J. Clin. Med. Res. 2017, 9, 917–925. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Heber, S.D.; Hetterich, H.; Lorbeer, R.; Bayerl, C.; Machann, J.; Auweter, S.; Storz, C.; Schlett, C.L.; Nikolaou, K.; Reiser, M.; et al. Pancreatic fat content by magnetic resonance imaging in subjects with prediabetes, diabetes, and controls from a general population without cardiovascular disease. PLoS ONE 2017, 12, e0177154. [Google Scholar] [CrossRef] [PubMed]
- Carba, D.B.; Bas, I.N.; Gultiano, S.A.; Lee, N.R.; Adair, L.S. Waist circumference and the risk of hypertension and prediabetes among Filipino women. Eur. J. Nutr. 2012, 52, 825–832. [Google Scholar] [CrossRef] [PubMed]
- Borné, Y.; Nilsson, P.M.; Melander, O.; Hedblad, B.; Engström, G. Multiple anthropometric measures in relation to incidence of diabetes: A Swedish population-based cohort study. Eur. J. Public Health 2015, 25, 1100–1105. [Google Scholar] [CrossRef] [Green Version]
- Ramírez-Vélez, R.; Pérez-Sousa, M.Á.; González-Ruíz, K.; Cano-Gutierrez, C.A.; Schmidt-RioValle, J.; Correa-Rodríguez, M.; Izquierdo, M.; Romero-García, J.A.; Campos-Rodríguez, A.Y.; Triana-Reina, H.R.; et al. Obesity- and Lipid-Related Parameters in the Identification of Older Adults with a High Risk of Prediabetes According to the American Diabetes Association: An Analysis of the 2015 Health, Well-Being, and Aging Study. Nutrients 2019, 11, 2654. [Google Scholar] [CrossRef] [Green Version]
- Zhao, Q.; Zhang, K.; Li, Y.; Zhen, Q.; Shi, J.; Yu, Y.; Tao, Y.; Cheng, Y.; Liu, Y. Capacity of a body shape index and body roundness index to identify diabetes mellitus in Han Chinese people in Northeast China: A cross-sectional study. Diabet. Med. 2018, 35, 1580–1587. [Google Scholar] [CrossRef] [Green Version]
- Volaco, A.; Martins, C.M.; Soares, J.Q.; Cavalcanti, A.M.; Moyses, S.T.; Baena, C.P.; Precoma, D.B. Neck Circumference and its Correlation to Other Anthropometric Parameters and Finnish Diabetes Risk Score (FINDRISC). Curr. Diabetes Rev. 2018, 14, 464–471. [Google Scholar] [CrossRef] [PubMed]
- Joshipura, K.; Muñoz-Torres, F.; Vergara, J.; Palacios, C.; Pérez, C.M. Neck Circumference May Be a Better Alternative to Standard Anthropometric Measures. J. Diabetes Res. 2016, 2016, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Jung, S.H.; Ha, K.H.; Kim, D.J. Visceral Fat Mass Has Stronger Associations with Diabetes and Prediabetes than Other Anthropometric Obesity Indicators among Korean Adults. Yonsei Med. J. 2016, 57, 674–680. [Google Scholar] [CrossRef]
- Bala, M.; Meenakshi Aggarwal, S. Correlation of Body Mass Index and Waist/Hip Ratio with Glycated Hemoglobin in Prediabetes. EJIFCC 2019, 30, 317–324. [Google Scholar] [PubMed]
- Noudeh, Y.J.; Hadaegh, F.; Vatankhah, N.; Momenan, A.A.; Saadat, N.; Khalili, D.; Azizi, F. Wrist Circumference as a Novel Predictor of Diabetes and Prediabetes: Results of Cross-Sectional and 8.8-Year Follow-up Studies. J. Clin. Endocrinol. Metab. 2013, 98, 777–784. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Control Group (n = 5457) | Prediabetes (n = 2731) | p-Value | |
|---|---|---|---|
| Women, n (%) | 2616 (47.9) | 1551 (56.8) | <0.001 |
| Age (years) | 56 (52–62) | 59 (54–64) | <0.001 |
| Caucasian, n (%) | 5440 (99.7) | 2712 (99.3) | 0.013 |
| HbA1c (%) | 5.4 (5.2–5.5) | 5.8 (5.7–6.0) | <0.001 |
| Obesity, n (%) | 1580 (29.0) | 1094 (40.1) | <0.001 |
| Blood hypertension, n (%) | 2015 (36.9) | 1290 (47.2) | <0.001 |
| Systolic BP (mm Hg) | 129 (119–141) | 132 (121–143) | <0.001 |
| Diastolic BP (mm Hg) | 81 (75–88) | 82 (75–88) | 0.184 |
| Antihypertensive drugs, n (%) | 1569 (28.8) | 1103 (40.4) | <0.001 |
| Dyslipidemia, n (%) | 2798 (51.3) | 1622 (59.4) | <0.001 |
| Total cholesterol (mg/dL) | 202 (179–229) | 206 (183–232) | <0.001 |
| Lipid-lowering agents, n (%) | 831 (15.2) | 646 (23.7) | <0.001 |
| Antithrombotic drugs, n (%) | 141 (2.6) | 106 (3.9) | 0.001 |
| Male Subjects | Control Group (n = 2841) | Prediabetes (n = 1180) | p-Value |
|---|---|---|---|
| Total adiposity | |||
| BMI (Kg/m2) | 28.1 (25.6–31.0) | 29.8 (27.4–33.0) | <0.001 |
| CUN-BAE (%) | 29.5 (26.2–33.1) | 31.7 (28.7–35.3) | <0.001 |
| Deurenberg (%) | 30.1 (27.0–33.9) | 32.6 (29.3–36.4) | <0.001 |
| Visceral adipose tissue | |||
| WC (cm) | 100 (94–107) | 104 (98–112) | <0.001 |
| Conicity index | 1.33 (1.29–1.37) | 1.34 (1.31–1.39) | <0.001 |
| WHR | 0.59 (0.55–0.63) | 0.60 (0.58–0.66) | <0.001 |
| Bonora (cm2) | 183 (145–228) | 209 (171–260) | <0.001 |
| A body shape index | 0.08 (0.08–0.09) | 0.08 (0.08–0.09) | 0.242 |
| Body roundness index | 5.04 (4.27–6.00) | 5.63 (4.82–6.72) | <0.001 |
| Neck circumference (cm) | 40.5 (39.0–42.0) | 41.5 (39.5–43.5) | <0.001 |
| Female Subjects | (n = 2616) | (n = 1551) | |
| Total adiposity | |||
| BMI (Kg/m2) | 27.3 (24.3–30.9) | 29.5 (26.2–33.3) | <0.001 |
| CUN-BAE (%) | 41.0 (37.1–44.9) | 43.6 (39.8–47.3) | <0.001 |
| Deurenberg (%) | 41.2 (37.0–45.7) | 44.1 (40.1–48.7) | <0.001 |
| Visceral adipose tissue | |||
| WC (cm) | 97 (90–105) | 102 (94–110) | <0.001 |
| Conicity index | 1.36 (1.30–1.41) | 1.37 (1.32–1.42) | <0.001 |
| WHR | 0.62 (0.57–0.67) | 0.65 (0.60–0.70) | <0.001 |
| Bonora (cm2) | 177.7 (144.8–213.5) | 199.4 (165.7–234.2) | <0.001 |
| A body shape index | 0.09 (0.08–0.09) | 0.09 (0.08–0.09) | 0.179 |
| Body roundness index | 5.80 (4.65–7.03) | 6.47 (5.37–7.87) | <0.001 |
| Neck circumference (cm) | 34.5 (33.0–36.0) | 35.5 (34.0–37.5) | <0.001 |
| Male Subjects | Female Subjects | |||
|---|---|---|---|---|
| r | p | r | p | |
| BMI (Kg/m2) | 0.152 | <0.001 | 0.156 | <0.001 |
| CUN-BAE (%) | 0.161 | <0.001 | 0.161 | <0.001 |
| Deurenberg (%) | 0.171 | <0.001 | 0.164 | <0.001 |
| Waist circumference (cm) | 0.138 | <0.001 | 0.147 | <0.001 |
| Conicity index | 0.095 | 0.001 | 0.083 | 0.001 |
| WHR | 0.149 | <0.001 | 0.156 | <0.001 |
| Bonora (cm2) | 0.136 | <0.001 | 0.158 | <0.001 |
| A body shape index | 0.018 | 0.542 | 0.007 | 0.777 |
| Body roundness index | 0.149 | <0.001 | 0.156 | <0.001 |
| Neck circumference (cm) | 0.178 | <0.001 | 0.182 | <0.001 |
| Male Subjects | Cutoff | Sensitivity | Specificity | AUROC | 95% CI | p |
|---|---|---|---|---|---|---|
| BMI (Kg/m2) | 28.2 | 0.68 | 0.51 | 0.62 | 0.60 to 0.64 | <0.001 |
| CUN-BAE (%) | 29.9 | 0.66 | 0.53 | 0.63 | 0.61 to 0.65 | <0.001 |
| Deurenberg (%) | 31.5 | 0.59 | 0.60 | 0.63 | 0.61 to 0.65 | <0.001 |
| WC (cm) | 100 | 0.65 | 0.53 | 0.62 | 0.60 to 0.64 | <0.001 |
| Conicity index | 1.33 | 0.62 | 0.49 | 0.58 | 0.56 to 0.60 | <0.001 |
| WHR | 0.59 | 0.65 | 0.54 | 0.63 | 0.61 to 0.65 | <0.001 |
| Bonora (cm2) | 186.5 | 0.65 | 0.53 | 0.62 | 0.60 to 0.64 | <0.001 |
| Body roundness index | 5.29 | 0.62 | 0.57 | 0.63 | 0.61 to 0.65 | <0.001 |
| A body shape index | 0.08 | 0.50 | 0.54 | 0.51 | 0.49 to 0.53 | 0.228 |
| Neck circumference (cm) | 40.8 | 0.63 | 0.55 | 0.61 | 0.59 to 0.63 | <0.001 |
| Female Subjects | ||||||
| BMI (Kg/m2) | 28.6 | 0.58 | 0.60 | 0.62 | 0.60 to 0.64 | <0.001 |
| CUN-BAE (%) | 43.5 | 0.51 | 0.67 | 0.63 | 0.61 to 0.64 | <0.001 |
| Deurenberg (%) | 40.8 | 0.71 | 0.47 | 0.63 | 0.61 to 0.65 | <0.001 |
| WC (cm) | 101.5 | 0.51 | 0.64 | 0.60 | 0.59 to 0.62 | <0.001 |
| Conicity index | 1.35 | 0.59 | 0.48 | 0.55 | 0.53 to 0.57 | <0.001 |
| WHR | 0.62 | 0.62 | 0.54 | 0.62 | 0.60 to 0.63 | <0.001 |
| Bonora (cm2) | 179.0 | 0.67 | 0.51 | 0.62 | 0.60 to 0.63 | <0.001 |
| Body roundness index | 6.10 | 0.59 | 0.57 | 0.62 | 0.60 to 0.63 | <0.001 |
| A body shape index | 0.08 | 0.58 | 0.39 | 0.49 | 0.47 to 0.51 | 0.179 |
| Neck circumference (cm) | 35.3 | 0.55 | 0.63 | 0.62 | 0.60 to 0.64 | <0.001 |
| Male Subjects | Cutoff Point | Prevalence of Prediabetes Below the Cutoff | Prevalence of Prediabetes Above the Cutoff | Odds Ratio (95% CI) | p-Value |
|---|---|---|---|---|---|
| BMI (Kg/m2) | 28.2 | 20.4 | 36.2 | 2.2 (1.9 to 2.5) | <0.001 |
| CUN-BAE (%) | 29.9 | 20.9 | 37.1 | 2.2 (1.9 to 2.6) | <0.001 |
| Deurenberg (%) | 31.5 | 22.8 | 38.2 | 2.2 (1.9 to 2.5) | <0.001 |
| WC (cm) | 100 | 20.8 | 35.4 | 2.1 (1.8 to 2.4) | <0.001 |
| Conicity index | 1.33 | 24.3 | 33.6 | 1.6 (1.4 to 1.8) | <0.001 |
| WHR | 0.59 | 21.0 | 36.8 | 2.2 (1.9 to 2.5) | <0.001 |
| Bonora (cm2) | 186.5 | 21.7 | 36.2 | 2.0 (1.8 to 2.4) | <0.001 |
| Body roundness index | 5.29 | 21.5 | 37.8 | 2.2 (1.9 to 2.6) | <0.001 |
| A body shape index | 0.08 | 27.3 | 29.8 | 1.1 (0.9 to 1.4) | 0.204 |
| Neck circumference (cm) | 40.8 | 22.0 | 36.6 | 2.0 (1.8 to 2.4) | <0.001 |
| Female Subjects | |||||
| BMI (Kg/m2) | 28.6 | 29.3 | 44.8 | 2.0 (1.7 to 2.2) | <0.001 |
| CUN-BAE (%) | 43.5 | 30.4 | 47.8 | 2.1 (1.8 to 2.4) | <0.001 |
| Deurenberg (%) | 40.8 | 26.8 | 44.4 | 2.2 (1.9 to 2.5) | <0.001 |
| WC (cm) | 101.5 | 31.3 | 45.5 | 1.8 (1.6 to 2.1) | <0.001 |
| Conicity index | 1.35 | 33.2 | 40.0 | 1.3 (1.2 to 1.5) | <0.001 |
| WHR | 0.62 | 29.2 | 43.6 | 1.8 (1.6 to 2.1) | <0.001 |
| Bonora (cm2) | 179.0 | 28.2 | 44.4 | 2.0 (1.8 to 2.3) | <0.001 |
| Body roundness index | 6.10 | 29.9 | 45.0 | 1.9 (1.7 to 2.2) | <0.001 |
| A body shape index | 0.08 | 37.8 | 37.1 | 0.9 (0.8 to 1.2) | 0.749 |
| Neck circumference (cm) | 35.3 | 30.1 | 46.3 | 2.2 (1.7 to 2.3) | <0.001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sánchez, M.; Sánchez, E.; Bermúdez-López, M.; Torres, G.; Farràs-Sallés, C.; Pamplona, R.; Castro-Boqué, E.; Valdivielso, J.M.; Purroy, F.; Martínez-Alonso, M.; et al. Clinical Usefulness of Anthropometric Indices to Predict the Presence of Prediabetes. Data from the ILERVAS Cohort. Nutrients 2021, 13, 1002. https://doi.org/10.3390/nu13031002
Sánchez M, Sánchez E, Bermúdez-López M, Torres G, Farràs-Sallés C, Pamplona R, Castro-Boqué E, Valdivielso JM, Purroy F, Martínez-Alonso M, et al. Clinical Usefulness of Anthropometric Indices to Predict the Presence of Prediabetes. Data from the ILERVAS Cohort. Nutrients. 2021; 13(3):1002. https://doi.org/10.3390/nu13031002
Chicago/Turabian StyleSánchez, Marta, Enric Sánchez, Marcelino Bermúdez-López, Gerard Torres, Cristina Farràs-Sallés, Reinald Pamplona, Eva Castro-Boqué, José Manuel Valdivielso, Francisco Purroy, Montserrat Martínez-Alonso, and et al. 2021. "Clinical Usefulness of Anthropometric Indices to Predict the Presence of Prediabetes. Data from the ILERVAS Cohort" Nutrients 13, no. 3: 1002. https://doi.org/10.3390/nu13031002






