What Was First, Obesity or Inflammatory Bowel Disease? What Does the Gut Microbiota Have to Do with It?
Abstract
1. Introduction
2. Causes of Weight Gain in IBD
3. Obesity Followed by IBD
4. Influence of Obesity on the Course of IBD
4.1. Molecular Mechanisms of the Influence of Adipose Tissue on IBD
4.2. The Role of Adipose Tissue in the Therapeutic Outcomes of Inflammatory Bowel Disease
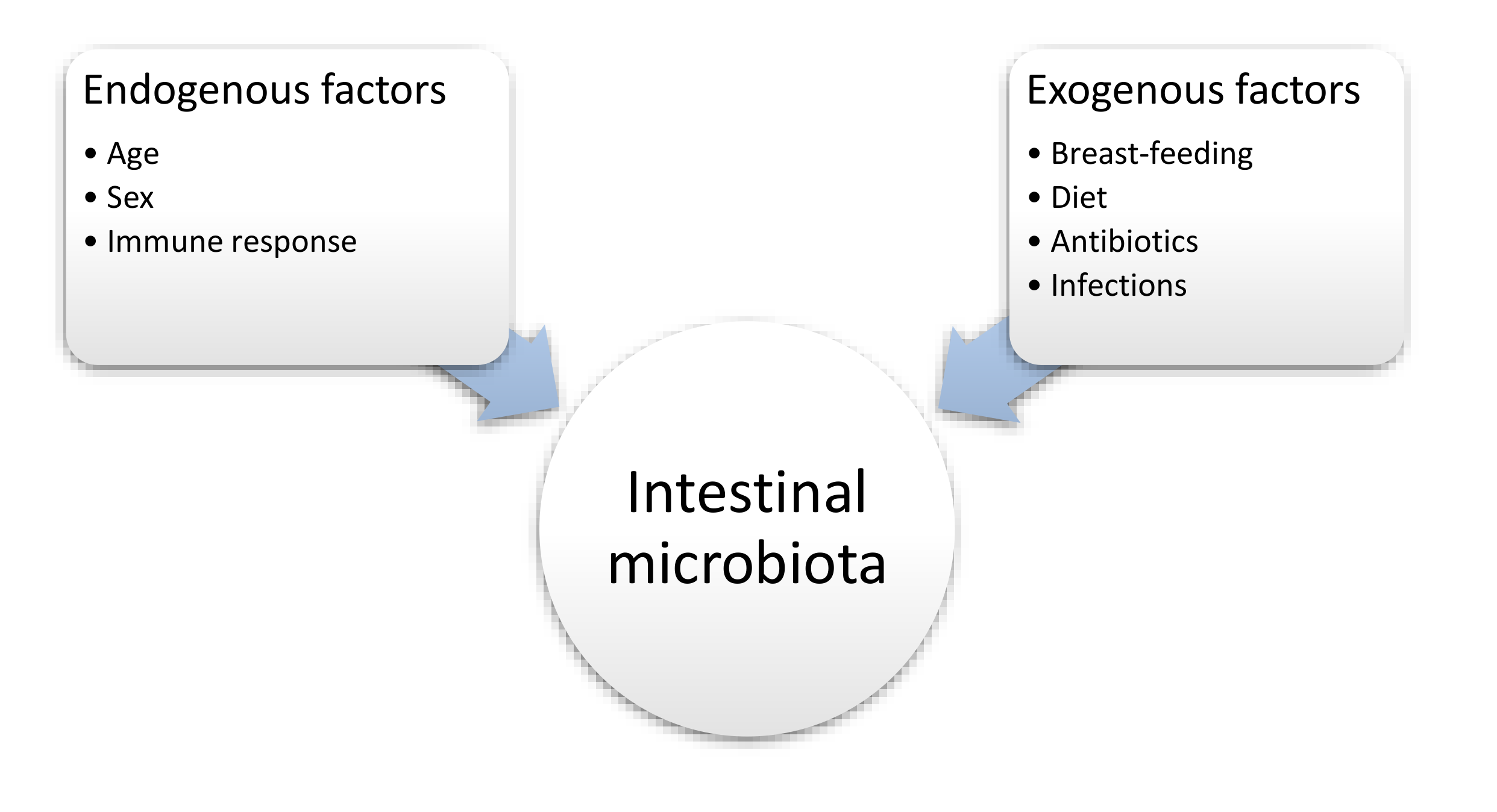
5. Intestinal Microbiota, Excess Body Weight and IBD
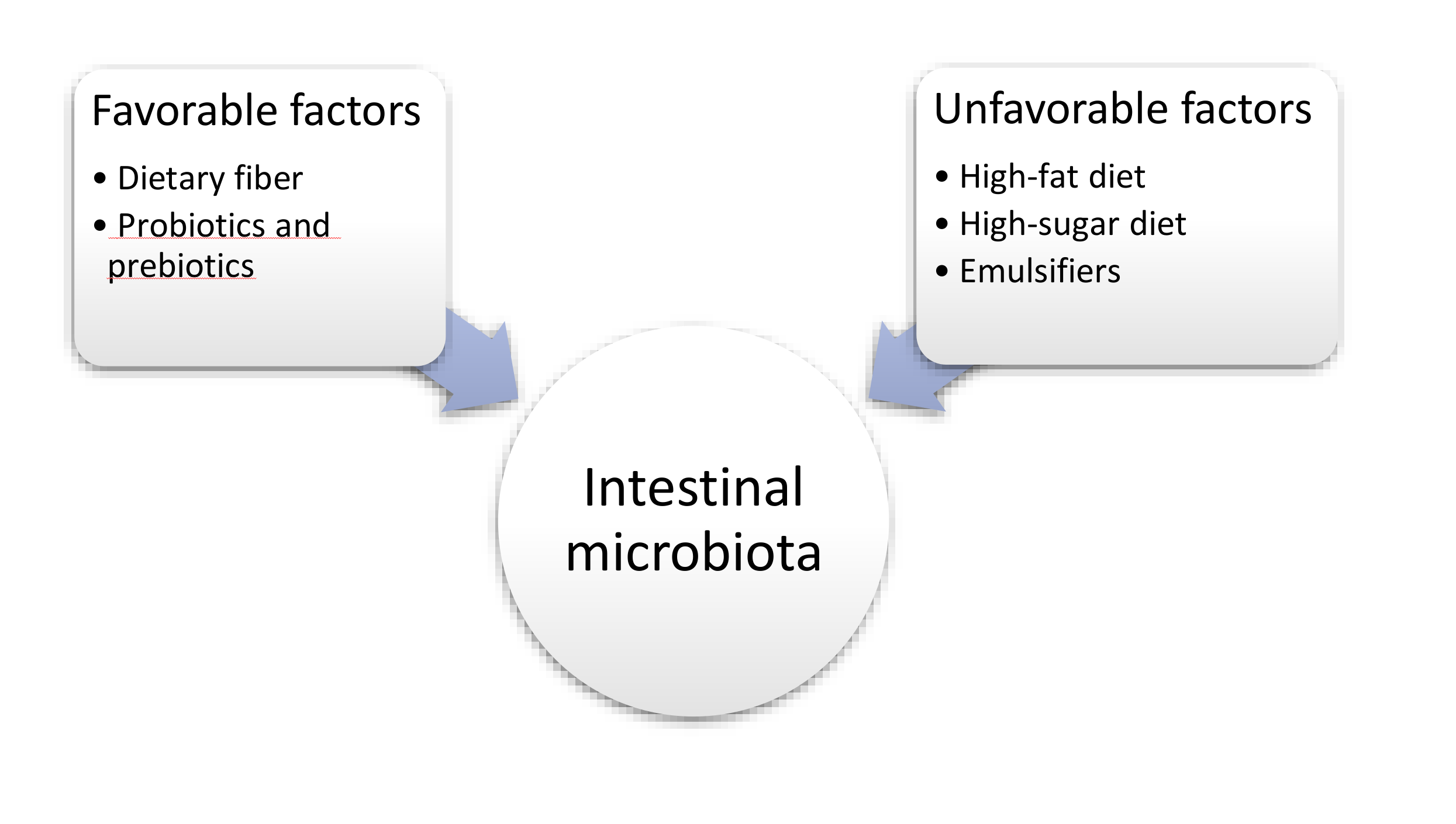
6. The Influence of Selected Nutritional Factors on the Intestinal Microbiota
6.1. Fat
6.2. Carbohydrates
6.3. Protein
6.4. Vitamin D
6.5. Sweeteners
6.6. Emulsifiers, Stabilizers
7. Summary
Author Contributions
Funding
Conflicts of Interest
References
- Sairenji, T.; Collins, K.; Evans, D. An Update on Inflammatory Bowel Disease. Prim. Care. 2017, 44, 673–692. [Google Scholar] [CrossRef] [PubMed]
- Windsor, J.; Kaplan, G. Evolving Epidemiology of IBD. Curr. Gastroenterol. Rep. 2019, 21, 40. [Google Scholar] [CrossRef] [PubMed]
- Malik, T. Inflammatory Bowel Disease: Historical Perspective, Epidemiology, and Risk Factors. Surg. Clin. North Am. 2015, 95, 1105–1122. [Google Scholar] [CrossRef] [PubMed]
- Murawska-Ciałowicz, E. Tkanka tłuszczowa – charakterystyka morfologiczna i biochemiczna różnych depozytów. Postepy Hig. Med. Dosw. (online) 2017, 71, 466–484. [Google Scholar]
- World Health Organization. Body mass index – BMI. Available online: https://www.euro.who.int/en/health-topics/disease-prevention/nutrition/a-healthy-lifestyle/body-mass-index-bmi?fbclid=IwAR0QjGXU9BP-naKzg8p8fSFz6CEE-JKwIUxJi6Kl9e3JLrJI4zATWphx8L0 (accessed on 21 May 2020).
- Harper, J.; Zisman, T. Interaction of obesity and inflammatory bowel disease. World J. Gastroenterol. 2016, 21, 7868–7881. [Google Scholar] [CrossRef]
- Flores, A.; Burstein, E.; Cipher, D.; Feagins, L. Obesity in Inflammatory Bowel Disease: A Marker of Less Severe Disease. Dig. Dis. Sci. 2015, 60, 2436–2445. [Google Scholar] [CrossRef]
- Chan, S.; Luben, R.; Olsen, A.; Tjonneland, A.; Kaaks, R.; Teucher, B.; Lindgren, S.; Grip, O.; Key, T.; Crowe, F.L.; et al. Body mass index and the risk for Crohn’s disease and ulcerative colitis: Data from a European Prospective Cohort Study (The IBD in EPIC Study). Am. J. Gastroenterol. 2013, 108, 575–582. [Google Scholar] [CrossRef]
- Singh, S.; Dulai, P.; Zarrinpar, A.; Ramamoorthy, S.; Sandborn, W. Obesity in IBD: Epidemiology, pathogenesis, disease course and treatment outcomes. Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 110–121. [Google Scholar] [CrossRef]
- Sharma, P.; McCarty, T.; Njei, B. Impact of Bariatric Surgery on Outcomes of Patients with Inflammatory Bowel Disease: A Nationwide Inpatient Sample Analysis, 2004-2014. Obes. Surg. 2018, 28, 1015–1024. [Google Scholar] [CrossRef]
- Ungar, B.; Kopylov, U.; Goitein, D.; Lahat, A.; Bardan, E.; Avidan, B.; Lang, A.; Maor, Y.; Eliakim, R.; Ben-Horin, S. Severe and morbid obesity in Crohn’s disease patients: Prevalence and disease associations. Digestion 2013, 88, 26–32. [Google Scholar] [CrossRef]
- Causey, M.; Johnson, E.; Miller, S.; Martin, M.; Maykel, J.; Steele, S. The impact of obesity on outcomes following major surgery for Crohn’s disease: An American College of Surgeons National Surgical Quality Improvement Program assessment. Dis. Colon. Rectum 2011, 54, 1488–1495. [Google Scholar] [CrossRef] [PubMed]
- Hossne, R.S.; Sassaki, L.Y.; Baima, J.P.; Meira Júnior, J.D.; Campos, L.M. Analysis of risk factors and postoperative complications in patients with crohn’disease. Arq. Gastroenterol. 2018, 55, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Keidar, A.; Hazan, D.; Sadot, E.; Kashtan, H.; Wasserberg, N. The role of bariatric surgery in morbidly obese patients with inflammatory bowel disease. Surg. Obes. Relat. Dis. 2015, 11, 132–136. [Google Scholar] [CrossRef] [PubMed]
- Shoar, S.; Shahabuddin Hoseini, S.; Naderan, M.; Mahmoodzadeh, H.; Ying Man, F.; Shoar, N.; Hosseini, M.; Bagheri-Hariri, S. Bariatric surgery in morbidly obese patients with inflammatory bowel disease: A systematic review. Surg. Obes. Relat. Dis. 2017, 13, 652–659. [Google Scholar] [CrossRef]
- Wright, S.; Aronne, L. Causes of obesity. Abdom. Imaging 2012, 37, 730–732. [Google Scholar] [CrossRef]
- Han, J.; Lawlor, D.; Kimm, S. Childhood obesity. Lancet 2010, 15, 1737–1748. [Google Scholar] [CrossRef]
- Williams, E.; Mesidor, M.; Winters, K.; Dubbert, P.M.; Wyatt, S.B. Overweight and Obesity: Prevalence, Consequences, and Causes of a Growing Public Health Problem. Curr. Obes. Rep. 2015, 4, 363–370. [Google Scholar] [CrossRef]
- Cawley, J. An economy of scales: A selective review of obesity’s economic causes, consequences, and solutions. J. Health Econ. 2015, 43, 244–268. [Google Scholar] [CrossRef]
- Barroso, T.; Conway, F.; Emel, S.; McMillan, D.; Young, D.; Karteszi, H.; Gaya, D.R.; Gerasimidis, K. Patients with inflammatory bowel disease have higher abdominal adiposity and less skeletal mass than healthy controls. Ann. Gastroenterol. 2018, 31, 566–571. [Google Scholar] [CrossRef]
- Choi, K. Sarcopenia and sarcopenic obesity. Korean J. Intern. Med. 2016, 31, 1054–1060. [Google Scholar] [CrossRef]
- Scaldaferri, F.; Pizzoferrato, M.; Lopetuso, L.; Musca, T.; Ingravalle, F.; Sicignano, L.L.; Mentella, M.; Miggiano, G.; Mele, M.C.; Gaetani, E.; et al. Nutrition and IBD: Malnutrition and/or Sarcopenia? A Practical Guide. Gastroenterol. Res. Pract. 2017, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Sakuma, K.; Aoi, W.; Yamaguchi, A. Molecular mechanism of sarcopenia and cachexia: Recent research advances. Pflugers Arch. 2017, 469, 573–591. [Google Scholar] [CrossRef] [PubMed]
- Ryan, E.; McNicholas, D.; Creavin, B.; Kelly, M.; Walsh, T.; Beddy, D. Sarcopenia and Inflammatory Bowel Disease: A Systematic Review. Inflamm. Bowel Dis. 2019, 25, 67–73. [Google Scholar] [CrossRef] [PubMed]
- Cozier, Y.C.; Govender, P.; Berman, J.S. Obesity and sarcoidosis: Consequence or contributor? Curr. Opin. Pulm. Med. 2018, 24, 487–494. [Google Scholar] [CrossRef]
- Parmentier-Decrucq, E.; Duhamel, A.; Ernst, O.; Fermont, C.; Louvet, A.; Vernier-Massouille, G.; Cortot, A.; Colombel, J.F.; Desreumaux, P.; Peyrin-Biroulet, L. Effects of infliximab therapy on abdominal fat and metabolic profile in patients with Crohn’s disease. Inflamm. Bowel Dis. 2009, 15, 1476–1484. [Google Scholar] [CrossRef]
- Ding, Z.; Wu, X.R.; Remer, E.M.; Lian, L.; Stocchi, L.; Li, Y.; McCullough, A.; Remzi, F.H.; Shen, B. Association between high visceral fat area and postoperative complications in patients with Crohn’s disease following primary surgery. Colorectal Dis. 2016, 18, 163–172. [Google Scholar] [CrossRef]
- Li, Y.; Zhu, W.; Gong, J.; Zhang, W.; Gu, L.; Guo, Z.; Cao, L.; Shen, B.; Li, N.; Li, J. Visceral fat area is associated with a high risk for early postoperative recurrence in Crohn’s disease. Colorectal Dis. 2015, 17, 225–234. [Google Scholar] [CrossRef]
- Stidham, R.W.; Waljee, A.K.; Day, N.M.; Bergmans, C.L.; Zahn, K.M.; Higgins, P.D.; Wang, S.C.; Su, G.L. Body fat composition assessment using analytic morphomics predicts infectious complications after bowel resection in Crohn’s disease. Inflamm. Bowel Dis. 2015, 21, 1306–1313. [Google Scholar] [CrossRef]
- Conklin, A.I.; Hong, J. Obesity prevention in corticosteroid-treated patients: Use and effectiveness of strategies for weight management. Clin. Obes. 2019, 9, 1–9. [Google Scholar] [CrossRef]
- Khalili, H.; Ananthakrishnan, A.; Konijeti, G.; Higuchi, L.; Fuchs, C.; Richter, J.; Chan, A.T. Measures of obesity and risk of Crohn’s disease and ulcerative colitis. Inflamm. Bowel Dis. 2015, 21, 361–368. [Google Scholar] [CrossRef]
- Versini, M.; Jeandel, P.; Rosenthal, E.; Shoenfeld, Y. Obesity in autoimmune diseases: Not a passive bystander. Autoimmun. Rev. 2014, 13, 981–1000. [Google Scholar] [CrossRef] [PubMed]
- Emerenziani, E.; Guarino, M.; Trillo Asensio, L.; Altomare, A.; Ribolsi, M.; Balestrieri, P. Role of Overweight and Obesity in Gastrointestinal Disease. Nutrients 2019, 12, 111. [Google Scholar] [CrossRef] [PubMed]
- Bilski, J.; Mazur-Bialy, A.; Wojcik, D.; Surmiak, M.; Magierowski, M.; Sliwowski, Z.; Pajdo, R.; Kwiecien, S.; Danielak, A.; Ptak-Belowska, A.; et al. Role of Obesity, Mesenteric Adipose Tissue, and Adipokines in Inflammatory Bowel Diseases. Biomolecules 2019, 9, 780. [Google Scholar] [CrossRef] [PubMed]
- Chandrakumar, A.; Wang, A.; Grover, K.; El-Matary, W. Obesity Is More Common in Children Newly Diagnosed with Ulcerative Colitis as Compared to those with Crohn Disease. J. Pediatr. Gastroenterol. Nutr. 2020, 70, 593–597. [Google Scholar] [CrossRef]
- Ocón Bretón, M.J.; Ilundain Gonzalez, A.I.; Altemir Trallero, J.; Agudo Tabuenca, A.; Gimeno Orna, J.A. Predictive factors of hypertriglyceridemia in inhospital patients during total parenteral nutrition. Nutr. Hosp. 2017, 34, 505–511. [Google Scholar]
- García Martínez, T.; Montañes Pauls, B.; Vicedo Cabrera, A.M.; Liñana Granell, C.; Ferrando Piqueres, R. Predictive factors of hyperglycemia in hospitalized adults receiving total parenteral nutrition. Farm. Hosp. 2017, 41, 667–673. [Google Scholar]
- Mitra, A.; Ahn, J. Liver Disease in Patients on Total Parenteral Nutrition. Clin. Liver Dis. 2017, 21, 687–695. [Google Scholar] [CrossRef]
- Blüher, M. Obesity: Global epidemiology and pathogenesis. Nat. Rev. Endocrinol. 2019, 15, 288–298. [Google Scholar]
- Hruby, A.; Manson, J.; Qi, L.; Malik, V.S.; Rimm, E.B.; Sun, Q.; Willett, W.C.; Hu, F.B. Determinants and Consequences of Obesity. Am. J. Public Health 2016, 106, 1656–1662. [Google Scholar] [CrossRef]
- Burisch, J.; Munkholm, P. The epidemiology of inflammatory bowel disease. Scand. J. Gastroenterol. 2015, 50, 942–951. [Google Scholar] [CrossRef]
- Iyengar, N.M.; Gucalp, A.; Dannenberg, A.J.; Hudis, C.A. Obesity and Cancer Mechanisms: Tumor Microenvironment and Inflammation. J. Clin. Oncol. 2016, 34, 4270–4276. [Google Scholar] [CrossRef] [PubMed]
- Statovci, D.; Aguilera, M.; MacSharry, J.; Melgar, S. The Impact of Western Diet and Nutrients on the Microbiota and Immune Response at Mucosal Interfaces. Front. Immunol. 2017, 8, 1–21. [Google Scholar] [CrossRef] [PubMed]
- Eder, P.; Adler, M.; Dobrowolska, A.; Kamhieh-Milz, J.; Witowski, J. The Role of Adipose Tissue in the Pathogenesis and Therapeutic Outcomes of Inflammatory Bowel Disease. Cells 2019, 8, 628. [Google Scholar] [CrossRef]
- Barbier, M.; Vidal, H.; Desreumaux, P.; Dubuquoy, L.; Bourreille, A.; Colombel, J.F.; Cherbut, C.; Galmiche, J.P. Overexpression of leptin mRNA in mesenteric adipose tissue in inflammatory bowel diseases. Gastroenterol. Clin. Biol. 2003, 27, 987–991. [Google Scholar] [CrossRef]
- Coope, A.; Pascoal, L.B.; da Silva, F.A.R.; Botezelli, J.D.; Ayrizono, M.L.S.; Milanski, M.; Camargo, M.G.; Planell, N.; Portovedo, M.; Dias, C.B.; et al. Transcriptional and Molecular Pathways Activated in Mesenteric Adipose Tissue and Intestinal Mucosa of Crohn’s Disease Patients. Int. J. Inflam. 2017, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Cañete, F.; Mañosa, M.; Clos, A.; Cabré, E.; Domènech, E. Review article: The relationship between obesity, bariatric surgery, and inflammatory bowel disease. Aliment Pharmacol. Ther. 2018, 48, 807–816. [Google Scholar]
- Karmiris, K.; Koutroubakis, I.; Kouroumalis, E. Leptin, adiponectin, resistin, and ghrelin--implications for inflammatory bowel disease. Mol. Nutr. Food Res. 2008, 52, 855–866. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Q.; Liu, Y.; Tan, L.; Yan, L.; Zuo, X. Adiponectin administration alleviates DSS-induced colonic inflammation in Caco-2 cells and mice. Inflamm. Res. 2018, 67, 663–670. [Google Scholar] [CrossRef]
- Morshedzadeh, N.; Rahimlou, M.; Asadzadeh Aghdaei, H.; Shahrokh, S.; Reza Zali, M.; Mirmiran, P. Association Between Adipokines Levels with Inflammatory Bowel Disease (IBD): Systematic Reviews. Dig. Dis. Sci. 2017, 62, 3280–3286. [Google Scholar] [CrossRef]
- Sideri, A.; Stavrakis, D.; Bowe, C.; Shih, D.Q.; Fleshner, P.; Arsenescu, V.; Turner, J.R.; Pothoulakis, C.; Karagiannides, I. Effects of Obesity on Severity of Colitis and Cytokine Expression in Mouse Mesenteric Fat. Potential Role of Adiponectin Receptor 1. Am. J. Physiol. Gastrointest. Liver Physiol. 2015, 308, 591–604. [Google Scholar] [CrossRef]
- Pavelock, N.; Masood, U.; Minchenberg, S.; Heisih, D. Effects of obesity on the course of inflammatory bowel disease. Proc. (Bayl. Univ. Med. Cent.) 2019, 32, 14–17. [Google Scholar] [CrossRef]
- Yerushalmy-Feler, A.; Ben-Tov, A.; Weintraub, Y.; Amir, A.; Galai, T.; Moran-Lev, H.; Cohen, S. High and low body mass index may predict severe disease course in children with inflammatory bowel disease. Scand. J. Gastroenterol. 2018, 53, 708–713. [Google Scholar] [CrossRef]
- Yilmaz, B.; Juillerat, P.; Øyås, O.; Ramon, C.; Bravo, F.D.; Franc, Y.; Fournier, N.; Michetti, P.; Mueller, C.; Geuking, M.; et al. Microbial network disturbances in relapsing refractory Crohn’s disease. Nature Medicine 2019, 25, 323–336. [Google Scholar] [CrossRef] [PubMed]
- Swanson, S.; Harper, J.; Zisman, T. Obesity and inflammatory bowel disease: Diagnostic and therapeutic implications. Curr. Opin. Gastroenterol. 2018, 34, 112–119. [Google Scholar] [CrossRef] [PubMed]
- Szilagyi, A. Relationship(s) between obesity and inflammatory bowel diseases: Possible intertwined pathogenic mechanisms. Clin. J. Gastroenterol. 2019, 13, 139–152. [Google Scholar] [CrossRef] [PubMed]
- Guerbau, L.; Gerard, R.; Duveau, N.; Staumont-Sallé, D.; Branche, J.; Maunoury, V.; Cattan, S.; Wils, P.; Boualit, M.; Libier, L.; et al. Patients with Crohn’s Disease with High Body Mass Index Present More Frequent and Rapid Loss of Response to Infliximab. Inflamm. Bowel Dis. 2017, 23, 1853–1859. [Google Scholar] [CrossRef] [PubMed]
- Wieser, V.; Gerner, R.; Moschen, A.; Tilg, H. Liver complications in inflammatory bowel diseases. Dig. Dis. 2013, 31, 233–238. [Google Scholar] [CrossRef]
- Liverani, E.; Leonardi, F.; Castellani, L.; Cardamone, C.; Belluzzi, A. Asymptomatic and Persistent Elevation of Pancreatic Enzymes in an Ulcerative Colitis Patient. Case Rep. Gastrointest. Med. 2013, 1–4. [Google Scholar] [CrossRef]
- Teich, N.; Mohl, W.; Bokemeyer, B.; Bündgens, B.; Büning, J.; Miehlke, S.; Hüppe, D.; Maaser, C.; Klugmann, T.; Kruis, W.; et al. Azathioprine-induced Acute Pancreatitis in Patients with Inflammatory Bowel Diseases: A Prospective Study on Incidence and Severity. J. Crohns Colitis 2016, 10, 61–68. [Google Scholar] [CrossRef]
- Bermejo, F.; Lopez-Sanroman, A.; Taxonera, C.; Gisbert, J.P.; Calle-Perez, J.L.; Vera, I.; Menchen, L.; Martin-Arranz, M.D. Opio, V.; Carneros, J.A.; et al. Acute pancreatitis in inflammatory bowel disease, with special reference to azathioprine-induced pancreatitis. Aliment Pharmacol. Ther. 2008, 28, 623–628. [Google Scholar] [CrossRef]
- Tigl, H.; Kaser, A. Gut microbiome, obesity, and metabolic dysfunction. J. Clin. Invest. 2011, 121, 2126–2132. [Google Scholar]
- Qin, J.; Li, R.; Raes, J.; Arumugam, M.; Burgdorf, K.; Manichanh, C.; Nielsen, T.; Pons, N.; Levenez, F.; Yamada, T.; et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature. 2010, 464, 59–65. [Google Scholar] [CrossRef] [PubMed]
- Lynch, S.; Pedersen, O. The Human Intestinal Microbiome in Health and Disease. N. Engl. J. Med. 2016, 15, 2369–2379. [Google Scholar] [CrossRef]
- Meldrum, D.; Morris, M.; Gambone, J. Obesity pandemic: Causes, consequences, and solutions-but do we have the will? Fertil. Steril. 2017, 107, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Lloyd-Price, J.; Abu-Ali, G.; Huttenhower, C. The healthy human microbiome. Genome Med. 2016, 8, 51. [Google Scholar] [CrossRef]
- Blum, H. The human microbiome. Adv. Med. Sci. 2017, 62, 414–420. [Google Scholar] [CrossRef]
- Dominguez-Bello, M.; Godoy-Vitorino, F.; Knight, R.; Blaser, M.J. Role of the microbiome in human development. Gut 2019, 68, 1108–1114. [Google Scholar] [CrossRef]
- Zhang, C.; Yin, A.; Li, H.; Wang, R.; Wu, G.; Shen, J.; Zhang, M.; Wang, L.; Hou, Y.; Ouyang, H.; et al. Dietary Modulation of gut microbiota contributes to alleviation of both genetic and simple obesity in children. EBioMedicine 2015, 2, 968–984. [Google Scholar] [CrossRef]
- Bouter, K.; van Raalte, D.; Groen, A.; Nieuwdorp, M. Role of the Gut Microbiome in the Pathogenesis of Obesity and Obesity-Related Metabolic Dysfunction. Gastroenterology 2017, 152, 1671–1678. [Google Scholar] [CrossRef]
- Qin, J.; Li, Y.; Cai, Z.; Li, S.; Zhu, J.; Zhang, F.; Liang, S.; Zhang, W.; Guan, Y.; Shen, D.; et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 2012, 490, 55–60. [Google Scholar] [CrossRef]
- Dao, M.; Clement, K. Gut microbiota and obesity: Concepts relevant to clinical care. Eur. J. Intern. Med. 2018, 48, 18–24. [Google Scholar] [CrossRef] [PubMed]
- Turnbaugh, P.; Ley, R.; Mahowald, M.; Magrini, V.; Mardis, E.; Gordon, J. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 2006, 21, 1027–1031. [Google Scholar] [CrossRef] [PubMed]
- Chassaing, B.; Koren, O.; Goodrich, J.; Poole, A.; Srinivasan, S.; Ley, R.; Gewirts, T. Dietary emulsifiers impact the mouse gut microbiota promoting colitis and metabolic syndrome. Nature 2015, 519, 92–96. [Google Scholar] [CrossRef] [PubMed]
- John, G.; Mullin, G. The Gut Microbiome and Obesity. Curr. Oncol. Rep. 2016, 18, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Leung, J.; Burke, B.; Ford, D.; Garvin, G.; Korn, C.; Sulis, C.; Bhadelia, N. Possible association between obesity and Clostridium difficile infection. Emerg. Infect. Dis. 2013, 19, 1791–1798. [Google Scholar] [CrossRef] [PubMed]
- Marchesi, J.; Adams, D.; Fava, F.; Hermes, G.; Hirschfield, G.; Hold, G.; Hirschfield, G.M.; Hold, G.; Quraishi, M.N.; Kinross, J.; et al. The gut microbiota and host health: A new clinical frontier. Gut 2016, 65, 330–339. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Fan, X.; Ying, J.; Chen, S. Emerging trends and research foci in gastrointestinal microbiome. J. Transl. Med. 2019, 17, 1–11. [Google Scholar] [CrossRef]
- Vandeputte, D.; Kathagen, G.; D’hoe, K.; Vieira-Silva, S.; Valles-Colomer, M.; Sabino, J.; Wang, J.; Tito, R.Y.; De Commer, L.; Darzi, Y. Quantitative microbiome profiling links gut community variation to microbial load. Nature 2017, 551, 507–511. [Google Scholar] [CrossRef]
- Morrison, D.; Preston, T. Formation of short chain fatty acids by the gut microbiota and their impact on human metabolism. Gut Microbes. 2016, 7, 189–200. [Google Scholar] [CrossRef]
- Sun, M.; Wu, W.; Liu, Z.; Cong, Y. Microbiota metabolite short chain fatty acids, GPCR, and inflammatory bowel diseases. J. Gastroenterol. 2017, 52, 1–8. [Google Scholar] [CrossRef]
- Laster, J.; Bonnes, S.; Rocha, J. Increased Use of Emulsifiers in Processed Foods and the Links to Obesity. Curr. Gastroenterol. Rep. 2019, 21, 61. [Google Scholar] [CrossRef] [PubMed]
- Belizário, J.; Faintuch, J.; Garay-Malpartida, M. Gut Microbiome Dysbiosis and Immunometabolism: New Frontiers for Treatment of Metabolic Diseases. Mediators Inflamm. 2018. [Google Scholar]
- Maruvada, P.; Leone, V.; Kaplan, L.M.; Chang, E.B. The Human Microbiome and Obesity: Moving beyond Associations. Cell Host Microbe 2017, 22, 559–599. [Google Scholar] [CrossRef] [PubMed]
- Ni, J.; Wu, G.D.; Albenberg, L.; Tomov, V.T. Gut microbiota and IBD: Causation or correlation? Nat. Rev. Gastroenterol. Hepatol. 2017, 14, 573–584. [Google Scholar] [CrossRef] [PubMed]
- Bellavia, M.; Damiano, G.; Gioviale, M.C.; Palumbo, V.D.; Cacciabaudo, F.; Buscemi, G.; Lo Monte, A.I. Abnormal expansion of segmented filamentous bacteria in the gut: A role in pathogenesis of chronic inflammatory intestinal diseases? Rev. Med. Microbiol. 2011, 22, 45–47. [Google Scholar] [CrossRef]
- David, L.; Maurice, C.; Carmody, R.; Gootenberg, D.B.; Button, J.E.; Ling, A.V.; Devlin, S.; Varma, Y.; Fishbach, M.A. Diet rapidly and reproducibly alters the human gut microbiome. Nature 2014, 505, 559–563. [Google Scholar] [CrossRef]
- Zhang, M.; Yang, X. Effects of a high fat diet on intestinal microbiota and gastrointestinal diseases. World J. Gastroenterol. 2016, 22, 8905–8909. [Google Scholar] [CrossRef]
- Tremaroli, V.; Bäckhed, F. Functional interactions between the gut microbiota and host metabolism. Nature 2012, 489, 242–249. [Google Scholar] [CrossRef]
- Bibbò, S.; Ianiro, G.; Giorgio, V.; Scaldaferri, F.; Masucci, L.; Gasbarrini, A.; Cammarota, G. The role of diet on gut microbiota composition. Eur. Rev. Med. Pharmacol. Sci. 2016, 20, 4742–4749. [Google Scholar]
- Wan, Y.; Tong, W.; Zhou, R.; Li, J.; Yuan, J.; Wang, F.; Li, D. Habitual animal fat consumption in shaping gut microbiota and microbial metabolites. Food Funct. 2019, 10, 7973–7982. [Google Scholar] [CrossRef]
- Losacco, M.; de Almeida, C.; Hijo, A.H.T.; Bargi-Souza, P.; Gama, P.; Nunes, M.T. Goulart-Silva, F; High-fat diet affects gut nutrients transporters in hypo and hyperthyroid mice by PPAR-a independent mechanism. Life Sci. 2018, 202, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Stenman, L.; Holma, R.; Eggert, A.; Korpela, R. A novel mechanism for gut barrier dysfunction by dietary fat: Epithelial disruption by hydrophobic bile acids. Am. J. Physiol. Gastrointest. Liver Physiol. 2013, 304, G227–G234. [Google Scholar] [CrossRef] [PubMed]
- Fava, F.; Gitau, R.; Griffin, B.; Gibson, G.R.; Tuohy, K.M.; Lovegrove, J.A. Tuohy, K.M. Lovegrove, J.A. The type and quantity of dietary fat and carbohydrate alter faecal microbiome and short-chain fatty acid excretion in a metabolic syndrome ‘at-risk’ population. Int. J. Obes. 2013, 216–223. [Google Scholar] [CrossRef]
- Martinez, K.; Leone, V.; Chang, E. Western diets, gut dysbiosis, and metabolic diseases: Are they linked? Gut Microbes 2017, 8, 130–142. [Google Scholar] [CrossRef]
- Caesar, R.; Tremaroli, V.; Kovatcheva-Datchary, P.; Cani, P.; Bäckhed, F. Crosstalk between Gut Microbiota and Dietary Lipids Aggravates WAT Inflammation through TLR Signaling. Cell Metab. 2015, 22, 658–668. [Google Scholar] [CrossRef]
- Guo, X.; Li, J.; Tang, R.; Guodong, Z.; Zeng., H.; Wood, R.J.; Liu., Z. High Fat Diet Alters Gut Microbiota and the Expression of Paneth Cell-Antimicrobial Peptides Preceding Changes of Circulating Inflammatory Cytokines. Mediators Inflamm. 2017, 2–9. [Google Scholar] [CrossRef]
- Cani, P.D.; Neyrinck, A.M.; Fava, F.; Knauf, C.; Burcelin, R.G.; Tuohy, K.M.; Gibson, G.R.; Delzenne, N.M. Selective increases of bifidobacteria in gut microflora improve high-fat-diet-induced diabetes in mice through a mechanism associated with endotoxaemia. Diabetologia 2007, 2374–2383. [Google Scholar] [CrossRef]
- Holscher, H. Dietary fiber and prebiotics and the gastrointestinal microbiota. Gut Microbes 2017, 8, 172–184. [Google Scholar] [CrossRef]
- Duncan, S.; Louis, P.; Thomson, T.; Flint, H. The role of pH in determining the species composition of the human colonic microbiota. Environ. Microbiol. 2009, 11, 2112–2122. [Google Scholar] [CrossRef]
- Scott, K.; Duncan, S.; Flint, H. Dietary fibre and the gut microbiota. Nutrition Bulletin 2008, 201–211. [Google Scholar] [CrossRef]
- Czajkowska, A.; Szponar, B. Short chain fatty acids (SCFA), the products of gut bacteria. Postepy Hig. Med. Dosw. 2018, 72, 131–142. [Google Scholar] [CrossRef]
- Hallert, C.; Björck, I.; Nyman, M.; Pousette, A.; Grännö, C.; Svensson, H. Increasing fecal butyrate in ulcerative colitis patients by diet: Controlled pilot study. Inflamm. Bowel Dis. 2003, 9, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Chen, L.; Hu, M.; Kim, J.J.; Lin, R.; Xu, J.; Fan, L.; Qi, Y.; Wy, L.; Liu, W.; et al. Dietary type 2 resistant starch improves systemic inflammation and intestinal permeability by modulating microbiota and metabolites in aged mice on high-fat diet. Aging (Albany NY) 2020, 12, 9173–9187. [Google Scholar] [CrossRef] [PubMed]
- Makki, K.; Deehan, E.; Walter, J.; Bäckhed, F. The Impact of Dietary Fiber on Gut Microbiota in Host Health and Disease. Cell Host Microbe 2018, 23, 705–715. [Google Scholar] [CrossRef] [PubMed]
- Simpson, H.; Campbell, B. Review article: Dietary fibre-microbiota interactions. Aliment Pharmacol. Ther. 2015, 42, 158–179. [Google Scholar] [CrossRef] [PubMed]
- Sinagra, E.; Tomasello, G.; Raimondo, D.; Rossi, F.; Facella, T.; Damiani, P.; Abruzzo, A.; Bruno, A.; Palumbo, V.D.; Cosentino, L.; et al. Nutrition, malnutrition and dietary interventions in inflammatory bowel disease. Progr. Nutr. 2014, 16, 79–89. [Google Scholar]
- Zhao, J.; Zhang, X.; Liu, H.; Brown, M.; Qiao, S. Dietary Protein and Gut Microbiota Composition and Function. Curr. Protein Pept. Sci. 2019, 20, 145–154. [Google Scholar] [CrossRef]
- Mills, S.; Stanton, C.; Lane, J.; Smith, G.; Ross, R. Precision Nutrition and the Microbiome, Part I: Current State of the Science. Nutrients 2019, 11, 923. [Google Scholar] [CrossRef]
- Dodd, D.; Spitzer, M.; Van Treuren, W.; Merrill, B.D.; Hryckowian, A.J.; Higginbottom, S.K.; Le, A.; Cowan, T.M.; Nolan, G.P.; Fischbach, M.A.; et al. A gut bacterial pathway metabolizes aromatic amino acids into nine circulating metabolites. Nature 2017, 551, 648–652. [Google Scholar] [CrossRef]
- Zhou, H.; Yu, B.; Gao, J.; Htoo, J.; Chen, D. Regulation of intestinal health by branched-chain amino acids. Anim. Sci. J. 2018, 89, 3–11. [Google Scholar] [CrossRef]
- Lin, R.; Liu, W.; Piao, M.; Zhu, H. A review of the relationship between the gut microbiota and amino acid metabolism. Amino Acids 2017, 49, 2083–2090. [Google Scholar] [CrossRef] [PubMed]
- Schäffler, H.; Herlemann, D.; Klinitzke, P.; Berlin, P.; Kreikemeyer, B.; Jaster, R.; Lamprecht, G. Vitamin D administration leads to a shift of the intestinal bacterial composition in Crohn’s disease patients, but not in healthy controls. J. Dig. Dis. 2018, 19, 225–234. [Google Scholar]
- Sun, J. Dietary vitamin D, vitamin D receptor, and microbiome. Curr. Opin. Clin. Nutr. Metab. Care. 2018, 21, 471–474. [Google Scholar] [CrossRef]
- Tabatabaeizadeh, S.; Tafazoli, N.; Ferns, G.; Avan, A.; Ghayour-Mobarhan, M. Vitamin D, the gut microbiome and inflammatory bowel disease. J. Res. Med. Sci. 2018, 23, 1–6. [Google Scholar]
- Wang, T.; Dabbas, B.; Laperriere, D.; Bitton, A.J.; Soualhine, H.; Tavera-Mendoza, L.E.; Dionne, S.; Servant, M.J.; Bitton, A.; Seidman, E.G. Direct and indirect induction by 1,25-dihydroxyvitamin D3 of the NOD2/CARD15-defensin beta2 innate immune pathway defective in Crohn disease. J. Biol. Chem. 2010, 285, 2227–2231. [Google Scholar] [CrossRef] [PubMed]
- Waterhouse, M.; Hope, B.; Krause, L.; Morrison, M.; Protani, M.M.; Zakrzewski, M.; Neale, R.E. Vitamin D and the gut microbiome: A systematic review of in vivo studies. Eur. J. Nutr. 2019, 58, 2895–2910. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, E.; Jørgensen, T. Relationships Between Vitamin D, Gut Microbiome, and Systemic Autoimmunity. Front. Immunol. 2020, 10, 1–13. [Google Scholar] [CrossRef]
- Dimitrov, V.; White, J. Vitamin D signaling in intestinal innate immunity and homeostasis. Mol. Cell Endocrinol. 2017, 453, 68–78. [Google Scholar] [CrossRef]
- Naderpoor, N.; Mousa, A.; Fernanda Gomez Arango, L.; Barrett, H.; Dekker Nitert, M.; de Courten, B. Effect of Vitamin D Supplementation on Faecal Microbiota: A Randomised Clinical Trial. Nutrients 2019, 11, 2888. [Google Scholar] [CrossRef]
- Lespessailles, E.; Toumi, H. Vitamin D alteration associated with obesity and bariatric surgery. Exp. Biol. Med. (Maywood) 2017, 242, 1086–1094. [Google Scholar] [CrossRef]
- Gominak, S. Vitamin D deficiency changes the intestinal microbiome reducing B vitamin production in the gut. The resulting lack of pantothenic acid adversely affects the immune system, producing a "pro-inflammatory" state associated with atherosclerosis and autoimmunity. Med. Hypotheses 2016, 94, 103–107. [Google Scholar] [PubMed]
- Gubatan, J.; Moss, A. Vitamin D in inflammatory bowel disease: More than just a supplement. Curr. Opin. Gastroenterol. 2018, 34, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Suez, J.; Korem, T.; Zeevi, D.; Schapira-Zilberman, G.; Thaiss, C.A.; Maza, O.; Israeli, D.; Zmora, N.; Gilad, S.; Weinberger, A.; et al. Artificial sweeteners induce glucose intolerance by altering the gut microbiota. Nature 2014, 514, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Suez, J.; Korem, T.; Zilberman-Schapira, G.; Segal, E.; Elinav, E. Non-caloric artificial sweeteners and the microbiome: Findings and challenges. Gut Microbes. 2015, 6, 149–155. [Google Scholar] [CrossRef] [PubMed]
- Bian, X.; Chi, L.; Gao, B.; Tu, P.; Ru, H.; Lu., K. The artificial sweetener acesulfame potassium affects the gut microbiome and body weight gain in CD-1 mice. PLoS ONE 2017, 12, e0178426. [Google Scholar] [CrossRef]
- Uebanso, T.; Kano, S.; Yoshimoto, A.; Natio, C.; Takaaki, S.; Mawatari, K.; Takahashi, A. Effects of Consuming Xylitol on Gut Microbiota and Lipid Metabolism in Mice. Nutrients 2017, 9, 1–12. [Google Scholar]
- Daly, K.; Darby, A.; Shirazi-Beechey, S. Low calorie sweeteners and gut microbiota. Physiol. Behav. 2016, 164, 494–500. [Google Scholar] [CrossRef]
- Wang, Q.; Browman, D.; Herzog, H.; Neely, G. Non-nutritive sweeteners possess a bacteriostatic effect and alter gut microbiota in mice. PLoS ONE 2018, 13, e0199080. [Google Scholar] [CrossRef]
- Deniņa, I.; Semjonovs, P.; Fomina, A.; Treimane, R.; Linde, R. The influence of stevia glycosides on the growth of Lactobacillus reuteri strains. Lett. Appl. Microbiol. 2014, 58, 278–284. [Google Scholar]
- Magnuson, B.; Roberts, A.; Nestmann, E. Critical review of the current literature on the safety of sucralose. Food Chem. Toxicol. 2017, 106, 324–355. [Google Scholar] [CrossRef]
- Abou-Donia, M.; El-Masry, E.; Abdel-Rahman, A.; McLendon, R.; Schiffman, S. Splenda alters gut microflora and increases intestinal p-glycoprotein and cytochrome p-450 in male rats. J. Toxicol. Environ. Health A. 2008, 71, 1415–1429. [Google Scholar] [CrossRef] [PubMed]
- Nettleton, J.; Reimer, R.; Shearer, J. Reshaping the gut microbiota: Impact of low calorie sweeteners and the link to insulin resistance? Physiol. Behav. 2016, 164, 488–493. [Google Scholar] [CrossRef] [PubMed]
- Burke, M.; Small, D. Physiological mechanisms by which non-nutritive sweeteners may impact body weight and metabolism. Physiol. Behav. 2015, 152, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Chassaing, B.; Van de Wiele, T.; De Bodt, J.; Marzorati, M.; Gewirtz, A. Dietary emulsifiers directly alter human microbiota composition and gene expression ex vivo potentiating intestinal inflammation. Gut 2017, 66, 1414–1427. [Google Scholar] [CrossRef] [PubMed]
- Glade, M.; Meguid, M. A glance at dietary emulsifiers, the human intestinal mucus and microbiome, and dietary fiber. Nutrition 2016, 32, 609–614. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.; Zhao, M.; Zhang, H.; Li, Y.; Liu, M.; Feng, F. Antimicrobial Emulsifier-Glycerol Monolaurate Induces Metabolic Syndrome, Gut Microbiota Dysbiosis, and Systemic Low-Grade Inflammation in Low-Fat Diet Fed Mice. Mol. Nutr. Food Res. 2018, 62, 1002. [Google Scholar] [CrossRef]
- Rinninella, E.; Cintoni, M.; Raoul, P.; Lopetuso, L.R.; Scaldaferri, F.; Pulcini, G.; Miggiatno, G.A.D.M.; Gasbarrini, A.; Mele, M.C. Food Components and Dietary Habits: Keys for a Healthy Gut Microbiota Composition. Nutrients 2019, 11, 2393. [Google Scholar] [CrossRef]
- Viennois, E.; Merlin, D.; Gewirtz, A.; Chassaing, B. Dietary Emulsifier-Induced Low-Grade Inflammation Promotes Colon Carcinogenesis. Cancer Res. 2017, 77, 27–40. [Google Scholar] [CrossRef]
- Laudisi, F.; Stolfi, C.; Monteleone, G. Impact of Food Additives on Gut Homeostasis. Nutrients 2019, 11, 2334. [Google Scholar] [CrossRef]
- Geiker, N.; Astrup, A.; Hjorth, M.; Sjödin, A.; Pijls, L.; Markus, C. Does stress influence sleep patterns, food intake, weight gain, abdominal obesity and weight loss interventions and vice versa? Obes. Rev. 2018, 19, 81–97. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jarmakiewicz-Czaja, S.; Sokal, A.; Filip, R. What Was First, Obesity or Inflammatory Bowel Disease? What Does the Gut Microbiota Have to Do with It? Nutrients 2020, 12, 3073. https://doi.org/10.3390/nu12103073
Jarmakiewicz-Czaja S, Sokal A, Filip R. What Was First, Obesity or Inflammatory Bowel Disease? What Does the Gut Microbiota Have to Do with It? Nutrients. 2020; 12(10):3073. https://doi.org/10.3390/nu12103073
Chicago/Turabian StyleJarmakiewicz-Czaja, Sara, Aneta Sokal, and Rafał Filip. 2020. "What Was First, Obesity or Inflammatory Bowel Disease? What Does the Gut Microbiota Have to Do with It?" Nutrients 12, no. 10: 3073. https://doi.org/10.3390/nu12103073
APA StyleJarmakiewicz-Czaja, S., Sokal, A., & Filip, R. (2020). What Was First, Obesity or Inflammatory Bowel Disease? What Does the Gut Microbiota Have to Do with It? Nutrients, 12(10), 3073. https://doi.org/10.3390/nu12103073




