Supplementation with Low Doses of a Cod Protein Hydrolysate on Glucose Regulation and Lipid Metabolism in Adults with Metabolic Syndrome: A Randomized, Double-Blind Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Study Setting
2.3. Definition of Metabolic Syndrome
2.4. Study Visits
2.5. Test Material
2.6. Estimation of Energy and Macronutrient Intake
2.7. Analyses of Blood Samples
2.8. Randomization
2.9. Statistical Analyses
3. Results
3.1. Participants
3.2. Estimated Intake of Energy and Macronutrient
3.3. Anthropometric Measurements
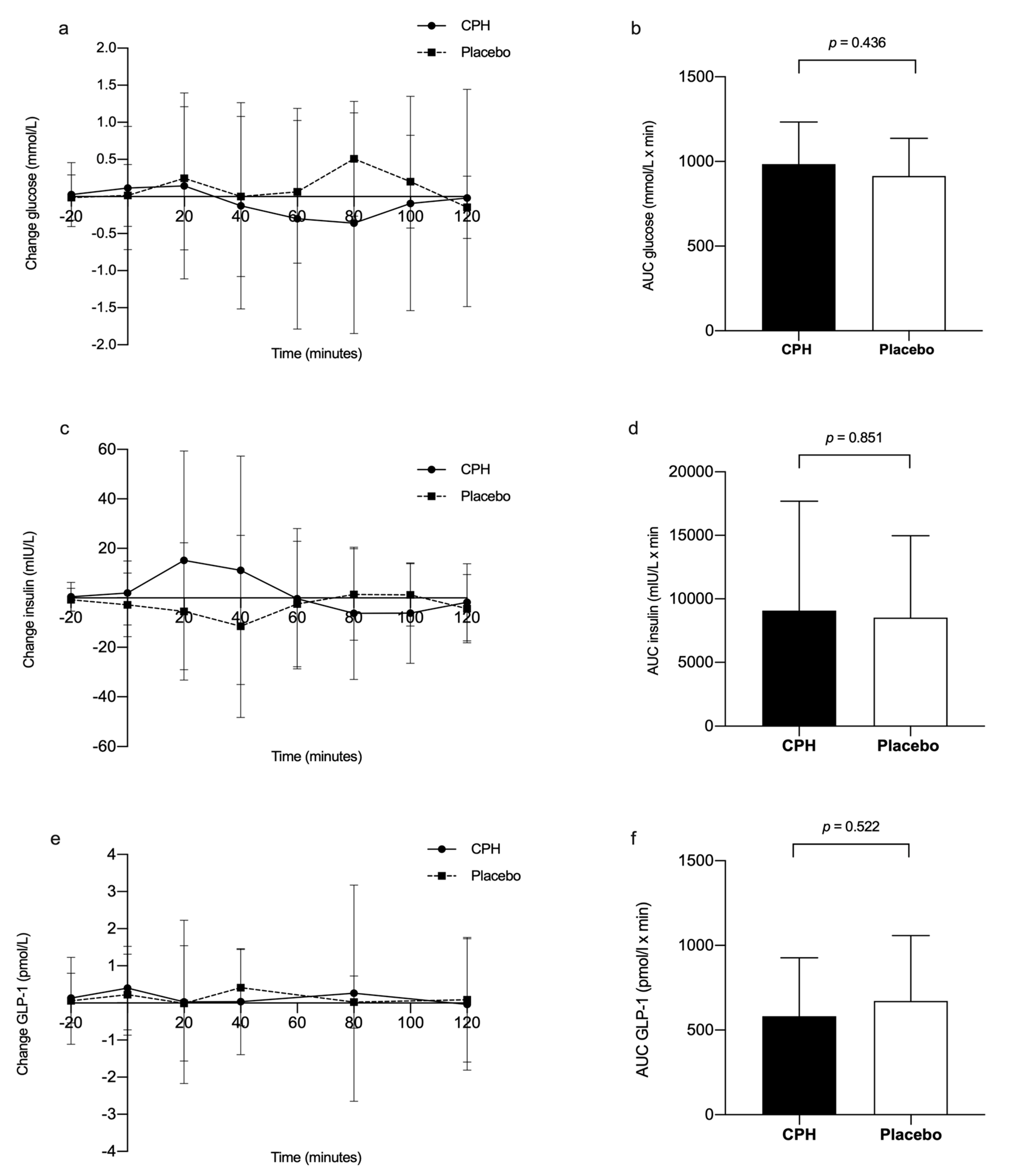
3.4. Glucose Homeostasis
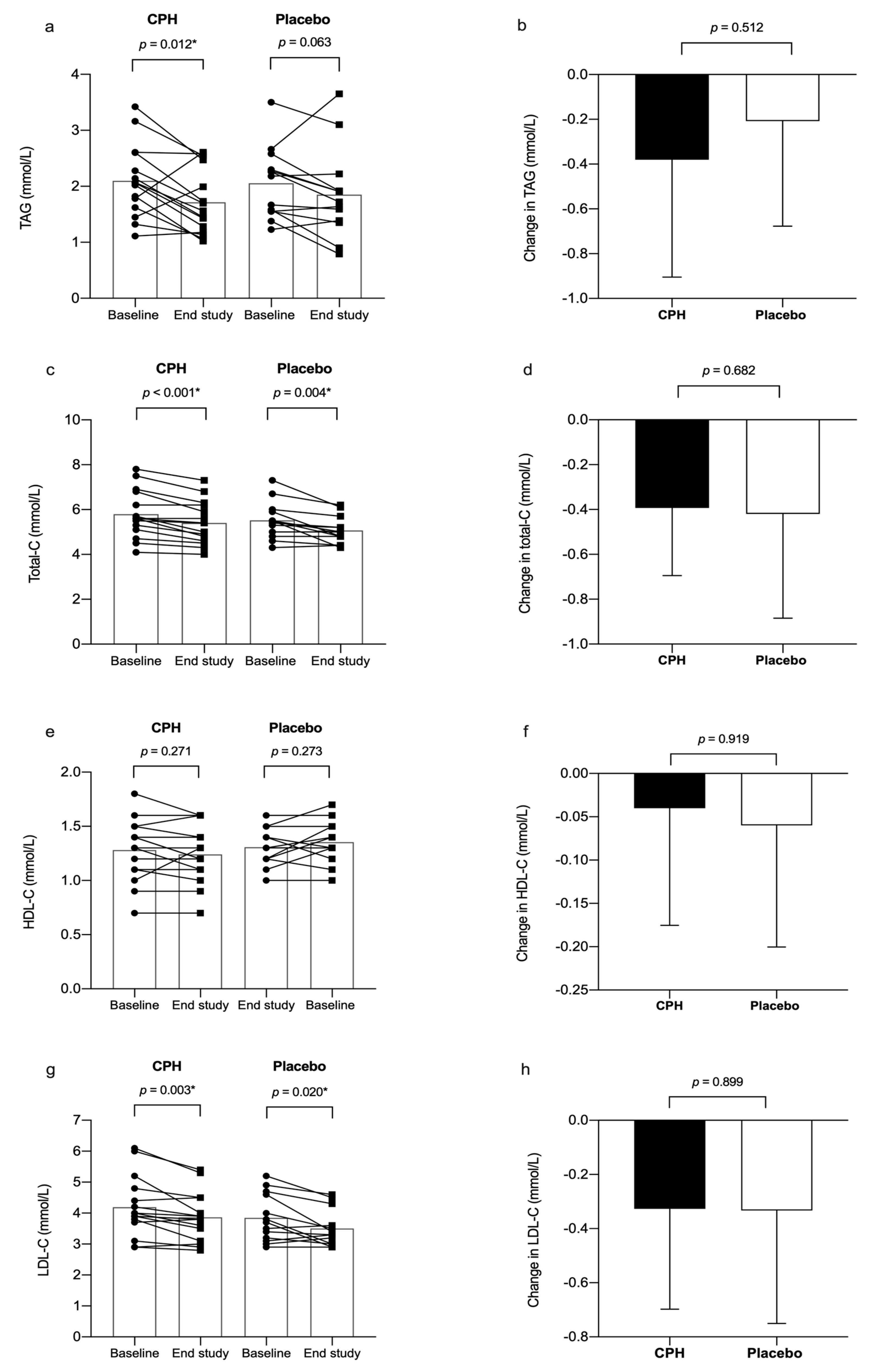
3.5. Lipid Parameters
3.6. Adverse Effects
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef] [PubMed]
- Eckel, R.H.; Alberti, K.G.; Grundy, S.M.; Zimmet, P.Z. The metabolic syndrome. Lancet 2010, 375, 181–183. [Google Scholar] [CrossRef]
- Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z. The metabolic syndrome. Lancet 2005, 365, 1415–1428. [Google Scholar] [CrossRef]
- Grundy, S.M. Metabolic syndrome pandemic. Arterioscler. Thromb. Vasc. Biol. 2008, 28, 629–636. [Google Scholar] [CrossRef]
- Karlsson, T.; Rosendahl-Riise, H.; Dierkes, J.; Drevon, C.A.; Tell, G.S.; Nygard, O. Associations between fish intake and the metabolic syndrome and its components among middle-aged men and women: The Hordaland Health Study. Food Nutr. Res. 2017, 61, 1347479. [Google Scholar] [CrossRef] [PubMed]
- Torris, C.; Molin, M.; Cvancarova, M.S. Lean fish consumption is associated with lower risk of metabolic syndrome: A Norwegian cross sectional study. BMC Public Health 2016, 16, 347. [Google Scholar] [CrossRef]
- Torris, C.; Molin, M.; Cvancarova Smastuen, M. Fish consumption and its possible preventive role on the development and prevalence of metabolic syndrome—A systematic review. Diabetol. Metab. Syndr. 2014, 6, 112. [Google Scholar] [CrossRef]
- Torris, C.; Molin, M.; Smastuen, M.C. Lean Fish Consumption Is Associated with Beneficial Changes in the Metabolic Syndrome Components: A 13-Year Follow-Up Study from the Norwegian Tromso Study. Nutrients 2017, 9, 247. [Google Scholar] [CrossRef]
- Skåre, J.U.; Brantsæter, A.L.; Frøyland, L.; Hemre, G.; Knutsen, H.K.; Lillegaard, I.T.L.; Torstensen, B. Benefit-Risk Assessment of Fish and Fish Products in the Norwegian Diet—An Update; Norwegian Scientific Committee for Food Safety (VKM): Oslo, Norway, 2014. [Google Scholar]
- Le Gouic, A.V.; Harnedy, P.A.; FitzGerald, R.J. Bioactive peptides from fish protein by-products. In Bioactive Molecules in Food; Springer International Publishing: Cham, Switzerland, 2018; pp. 355–388. [Google Scholar] [CrossRef]
- Moller, N.P.; Scholz-Ahrens, K.E.; Roos, N.; Schrezenmeir, J. Bioactive peptides and proteins from foods: Indication for health effects. Eur. J. Nutr. 2008, 47, 171–182. [Google Scholar] [CrossRef]
- Dale, H.F.; Madsen, L.; Lied, G.A. Fish-derived proteins and their potential to improve human health. Nutr. Rev. 2019. [Google Scholar] [CrossRef]
- Bjorndal, B.; Berge, C.; Ramsvik, M.S.; Svardal, A.; Bohov, P.; Skorve, J.; Berge, R.K. A fish protein hydrolysate alters fatty acid composition in liver and adipose tissue and increases plasma carnitine levels in a mouse model of chronic inflammation. Lipids Health Dis. 2013, 12, 143. [Google Scholar] [CrossRef] [PubMed]
- Drotningsvik, A.; Mjos, S.A.; Pampanin, D.M.; Slizyte, R.; Carvajal, A.; Remman, T.; Hogoy, I.; Gudbrandsen, O.A. Dietary fish protein hydrolysates containing bioactive motifs affect serum and adipose tissue fatty acid compositions, serum lipids, postprandial glucose regulation and growth in obese Zucker fa/fa rats. Br. J. Nutr. 2016, 116, 1336–1345. [Google Scholar] [CrossRef] [PubMed]
- Wergedahl, H.; Liaset, B.; Gudbrandsen, O.A.; Lied, E.; Espe, M.; Muna, Z.; Mork, S.; Berge, R.K. Fish protein hydrolysate reduces plasma total cholesterol, increases the proportion of HDL cholesterol, and lowers acyl-CoA:cholesterol acyltransferase activity in liver of Zucker rats. J. Nutr. 2004, 134, 1320–1327. [Google Scholar] [CrossRef] [PubMed]
- Dale, H.F.; Jensen, C.; Hausken, T.; Lied, E.; Hatlebakk, J.G.; Bronstad, I.; Lihaug Hoff, D.A.; Lied, G.A. Effect of a cod protein hydrolysate on postprandial glucose metabolism in healthy subjects: A double-blind cross-over trial. J. Nutr. Sci. 2018, 7, e33. [Google Scholar] [CrossRef]
- Nobile, V.; Duclos, E.; Michelotti, A.; Bizzaro, G.; Negro, M.; Soisson, F. Supplementation with a fish protein hydrolysate (Micromesistius poutassou): Effects on body weight, body composition, and CCK/GLP-1 secretion. Food Nutr. Res. 2016, 60, 29857. [Google Scholar] [CrossRef]
- Zaïr, Y.D.E.; Housez, B.; Vergara, C.; Cazaubiel, M.; Soisson, F. Evaluation of the satiating properties of a fish protein hydrolysate among overweight women: A pilot study. Nutr. Food Sci. 2014, 44, 389–399. [Google Scholar] [CrossRef]
- Hovland, I.H.; Leikanger, I.S.; Stokkeland, O.; Waage, K.H.; Mjos, S.A.; Brokstad, K.A.; McCann, A.; Ueland, P.M.; Slizyte, R.; Carvajal, A.; et al. Effects of low doses of fish and milk proteins on glucose regulation and markers of insulin sensitivity in overweight adults: A randomised, double blind study. Eur. J. Nutr. 2019. [Google Scholar] [CrossRef]
- Vikoren, L.A.; Nygard, O.K.; Lied, E.; Rostrup, E.; Gudbrandsen, O.A. A randomised study on the effects of fish protein supplement on glucose tolerance, lipids and body composition in overweight adults. Br. J. Nutr. 2013, 109, 648–657. [Google Scholar] [CrossRef]
- Vildmyren, I.; Cao, H.J.V.; Haug, L.B.; Valand, I.U.; Eng, O.; Oterhals, A.; Austgulen, M.H.; Halstensen, A.; Mellgren, G.; Gudbrandsen, O.A. Daily Intake of Protein from Cod Residual Material Lowers Serum Concentrations of Nonesterified Fatty Acids in Overweight Healthy Adults: A Randomized Double-Blind Pilot Study. Mar. Drugs 2018, 16, 197. [Google Scholar] [CrossRef]
- Dale, H.F.; Jensen, C.; Hausken, T.; Lied, E.; Hatlebakk, J.G.; Bronstad, I.; Hoff, D.A.L.; Lied, G.A. Acute effect of a cod protein hydrolysate on postprandial acylated ghrelin concentration and sensations associated with appetite in healthy subjects: A double-blind crossover trial. Food Nutr. Res. 2019, 63. [Google Scholar] [CrossRef]
- Dale, H.F.; Jensen, C.; Hausken, T.; Valeur, J.; Hoff, D.A.L.; Lied, G.A. Effects of a Cod Protein Hydrolysate Supplement on Symptoms, Gut Integrity Markers and Fecal Fermentation in Patients with Irritable Bowel Syndrome. Nutrients 2019, 11, 1635. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Foundation (IDF). The IDF Consensus Worldwide Definition of the Metabolic Syndrome. Available online: https://idf.org/our-activities/advocacy-awareness/resources-and-tools/60:idfconsensus-worldwide-definitionof-the-metabolic-syndrome.html (accessed on 1 February 2019).
- World Health Organization (WHO). The WHO STEPwise Approach to Noncommunicable Disease Risk Factor Surveillance. Available online: https://www.who.int/ncds/surveillance/steps/manual/en/ (accessed on 1 February 2019).
- World Health Organization (WHO). Waist circumference and waist–hip ratio. In Report of a WHO Expert Consultation; World Health Organization: Geneva, Swizerland, 2008; p. 39. [Google Scholar]
- Norwegian Food Safety Authority and The Norwegian Directorate of Health. Kostholdsplanleggeren. Available online: https://www.kostholdsplanleggeren.no (accessed on 4 November 2019).
- Ouellet, V.; Marois, J.; Weisnagel, S.J.; Jacques, H. Dietary cod protein improves insulin sensitivity in insulin-resistant men and women: A randomized controlled trial. Diabetes Care 2007, 30, 2816–2821. [Google Scholar] [CrossRef] [PubMed]
- Chevrier, G.; Mitchell, P.L.; Rioux, L.E.; Hasan, F.; Jin, T.; Roblet, C.R.; Doyen, A.; Pilon, G.; St-Pierre, P.; Lavigne, C.; et al. Low-Molecular-Weight Peptides from Salmon Protein Prevent Obesity-Linked Glucose Intolerance, Inflammation, and Dyslipidemia in LDLR-/-/ApoB100/100 Mice. J. Nutr. 2015, 145, 1415–1422. [Google Scholar] [CrossRef] [PubMed]
- Lavigne, C.; Marette, A.; Jacques, H. Cod and soy proteins compared with casein improve glucose tolerance and insulin sensitivity in rats. Am. J. Physiol. Endocrinol. Metab. 2000, 278, E491–E500. [Google Scholar] [CrossRef]
- Jensen, C.; Dale, H.F.; Hausken, T.; Lied, E.; Hatlebakk, J.G.; Bronstad, I.; Lied, G.A.; Hoff, D.A.L. Supplementation with cod protein hydrolysate in older adults: A dose range cross-over study. J. Nutr. Sci. 2019, 8, e40. [Google Scholar] [CrossRef]
- Helland, A.; Bratlie, M.; Hagen, I.V.; Mjos, S.A.; Sornes, S.; Ingvar Halstensen, A.; Brokstad, K.A.; Sveier, H.; Rosenlund, G.; Mellgren, G.; et al. High intake of fatty fish, but not of lean fish, improved postprandial glucose regulation and increased the n-3 PUFA content in the leucocyte membrane in healthy overweight adults: A randomised trial. Br. J. Nutr. 2017, 117, 1368–1378. [Google Scholar] [CrossRef]
- Vildmyren, I.; Halstensen, A.; Oterhals, A.; Gudbrandsen, O.A. Cod protein powder lowered serum nonesterified fatty acids and increased total bile acid concentrations in healthy, lean, physically active adults: A randomized double-blind study. Food Nutr. Res. 2019, 63. [Google Scholar] [CrossRef]
- Zamora-Sillero, J.; Gharsallaoui, A.; Prentice, C. Peptides from Fish By-product Protein Hydrolysates and Its Functional Properties: An Overview. Mar. Biotechnol. 2018, 20, 118–130. [Google Scholar] [CrossRef]
- El Khoury, D.; Anderson, G.H. Recent advances in dietary proteins and lipid metabolism. Curr. Opin. Lipidol. 2013, 24, 207–213. [Google Scholar] [CrossRef]
- Aadland, E.K.; Lavigne, C.; Graff, I.E.; Eng, O.; Paquette, M.; Holthe, A.; Mellgren, G.; Jacques, H.; Liaset, B. Lean-seafood intake reduces cardiovascular lipid risk factors in healthy subjects: Results from a randomized controlled trial with a crossover design. Am. J. Clin. Nutr. 2015, 102, 582–592. [Google Scholar] [CrossRef]
- Shukla, A.; Bettzieche, A.; Hirche, F.; Brandsch, C.; Stangl, G.I.; Eder, K. Dietary fish protein alters blood lipid concentrations and hepatic genes involved in cholesterol homeostasis in the rat model. Br. J. Nutr. 2006, 96, 674–682. [Google Scholar] [PubMed]
- Zhang, X.; Beynen, A.C. Influence of dietary fish proteins on plasma and liver cholesterol concentrations in rats. Br. J. Nutr. 1993, 69, 767–777. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.; Stone, N.J.; Ballantyne, C.; Bittner, V.; Criqui, M.H.; Ginsberg, H.N.; Goldberg, A.C.; Howard, W.J.; Jacobson, M.S.; Kris-Etherton, P.M.; et al. Triglycerides and cardiovascular disease: A scientific statement from the American Heart Association. Circulation 2011, 123, 2292–2333. [Google Scholar] [CrossRef] [PubMed]
- Westerterp-Plantenga, M.S. The significance of protein in food intake and body weight regulation. Curr. Opin. Clin. Nutr. Metab. Care 2003, 6, 635–638. [Google Scholar] [CrossRef] [PubMed]
- Uhe, A.M.; Collier, G.R.; O’Dea, K. A comparison of the effects of beef, chicken and fish protein on satiety and amino acid profiles in lean male subjects. J. Nutr. 1992, 122, 467–472. [Google Scholar] [CrossRef]
- Dailey, M.J.; Moran, T.H. Glucagon-like peptide 1 and appetite. Trends Endocrinol. Metab. 2013, 24, 85–91. [Google Scholar] [CrossRef]
- Holst, J.J. The physiology of glucagon-like peptide 1. Physiol. Rev. 2007, 87, 1409–1439. [Google Scholar] [CrossRef]
- Shah, M.; Vella, A. Effects of GLP-1 on appetite and weight. Rev. Endocr. Metab. Disord. 2014, 15, 181–187. [Google Scholar] [CrossRef]
- Kyle, U.G.; Bosaeus, I.; De Lorenzo, A.D.; Deurenberg, P.; Elia, M.; Manuel Gomez, J.; Lilienthal Heitmann, B.; Kent-Smith, L.; Melchior, J.C.; Pirlich, M.; et al. Bioelectrical impedance analysis-part II: Utilization in clinical practice. Clin. Nutr. 2004, 23, 1430–1453. [Google Scholar] [CrossRef]
- Johnson Stoklossa, C.A.; Forhan, M.; Padwal, R.S.; Gonzalez, M.C.; Prado, C.M. Practical Considerations for Body Composition Assessment of Adults with Class II/III Obesity Using Bioelectrical Impedance Analysis or Dual-Energy X-Ray Absorptiometry. Curr. Obes. Rep. 2016, 5, 389–396. [Google Scholar] [CrossRef]

| Variables | CPH | Placebo | p-Value | ||
|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||
| Gender (female/male) | 11/4 | 13/2 | 0.651 | ||
| Age, years | 52.8 | 6.26 | 53.4 | 6.83 | 0.804 |
| Anthropometric measurements | |||||
| Body weight, kg | 96.5 | 12.8 | 93.4 | 12.2 | 0.509 |
| WC, cm | 107.6 | 9.72 | 105.7 | 10.7 | 0.630 |
| BMI, kg/m2 | 32.7 | 2.24 | 32.4 | 3.25 | 0.751 |
| Blood pressure (BP) | |||||
| Systolic BP, mmHg | 136.9 | 15.9 | 138.5 | 15.1 | 0.756 |
| Diastolic BP, mmHg | 88.2 | 10.1 | 86.7 | 6.44 | 0.702 |
| Glucose metabolism | |||||
| Glucose, mmol/L | 5.73 | 0.75 | 5.63 | 0.79 | 0.704 |
| HbA1c, mmol/mol | 37.5 | 4.47 | 35.7 | 3.40 | 0.208 |
| Lipid metabolism | |||||
| Total cholesterol, mmol/L | 5.8 | 1.1 | 5.5 | 0.8 | 0.466 |
| HDL cholesterol, mmol/L | 1.3 | 0.3 | 1.4 | 0.2 | 0.493 |
| LDL cholesterol, mmol/L | 4.2 | 0.1 | 3.9 | 0.8 | 0.334 |
| Triacylglycerol, mmol/L | 2.10 | 0.7 | 2.05 | 0.6 | 0.870 |
| Numbers using BP medications | 5 | 9 | - | ||
| Tobacco users | 1 | 2 | - | ||
| Variable | Baseline | 8 Weeks | p-Value 2 | p-Value 3 | p-Value 4 | ||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | ||||
| Energy intake, kcal/day | 0.668 | 0.726 | |||||
| CPH | 1882 | 485 | 1777 | 466 | 0.177 | ||
| Placebo | 1812 | 386 | 1746 | 410 | 0.406 | ||
| Protein, g/kg BW/day | 0.922 | 0.815 | |||||
| CPH | 0.91 | 0.22 | 0.85 | 0.24 | 0.357 | ||
| Placebo | 0.91 | 0.29 | 0.87 | 0.23 | 0.569 | ||
| Fat, g/day | 0.122 | 0.396 | |||||
| CPH | 84.9 | 24.4 | 77.8 | 24.2 | 0.128 | ||
| Placebo | 71.9 | 20.2 | 70.2 | 24.99 | 0.723 | ||
| Carbohydrate, g/day | 0.323 | 0.488 | |||||
| CPH | 193.2 | 46.0 | 191.7 | 51.3 | 0.848 | ||
| Placebo | 211.1 | 51.5 | 198.4 | 49.3 | 0.207 | ||
| Basal metabolic rate1, kcal | 0.579 | 0.743 | |||||
| CPH | 1760 | 334 | 1774 | 350 | 0.211 | ||
| Placebo | 1696 | 296 | 1700 | 264 | 0.399 | ||
| Variable | Baseline | End of Study | p-Value2 | p-Value3 | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Body weight, kg | 0.557 | |||||
| CPH | 96.02 | 13.6 | 96.14 | 13.8 | 0.715 | |
| Placebo | 93.15 | 12.7 | 92.93 | 12.2 | 0.694 | |
| BMI, kg/m2 | 0.603 | |||||
| CPH | 32.55 | 2.43 | 32.59 | 2.51 | 0.741 | |
| Placebo | 32.27 | 3.45 | 32.21 | 3.49 | 0.692 | |
| Waist circumference1 | 0.512 | |||||
| CPH | 105.5 | 9.72 | 108.8 | 7.25 | 0.014 | |
| Placebo | 105.9 | 10.7 | 108.2 | 9.49 | 0.040 | |
| Fat mass, % | 0.897 | |||||
| CPH | 39.91 | 6.79 | 39.50 | 7.12 | 0.211 | |
| Placebo | 40.21 | 5.37 | 39.75 | 5.47 | 0.105 | |
| Fat mass, kg | 0.834 | |||||
| CPH | 38.16 | 7.81 | 37.82 | 8.12 | 0.319 | |
| Placebo | 37.46 | 7.05 | 37.03 | 7.46 | 0.163 | |
| Fat-free mass, kg | 0.816 | |||||
| CPH | 57.81 | 11.54 | 58.33 | 12.01 | 0.221 | |
| Placebo | 55.71 | 10.08 | 55.92 | 9.02 | 0.301 | |
| Total body water, kg | 0.325 | |||||
| CPH | 42.39 | 8.47 | 42.45 | 8.89 | 0.974 | |
| Placebo | 41.29 | 7.34 | 40.64 | 6.77 | 0.322 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jensen, C.; Fjeldheim Dale, H.; Hausken, T.; Hatlebakk, J.G.; Brønstad, I.; Lied, G.A.; Hoff, D.A.L. Supplementation with Low Doses of a Cod Protein Hydrolysate on Glucose Regulation and Lipid Metabolism in Adults with Metabolic Syndrome: A Randomized, Double-Blind Study. Nutrients 2020, 12, 1991. https://doi.org/10.3390/nu12071991
Jensen C, Fjeldheim Dale H, Hausken T, Hatlebakk JG, Brønstad I, Lied GA, Hoff DAL. Supplementation with Low Doses of a Cod Protein Hydrolysate on Glucose Regulation and Lipid Metabolism in Adults with Metabolic Syndrome: A Randomized, Double-Blind Study. Nutrients. 2020; 12(7):1991. https://doi.org/10.3390/nu12071991
Chicago/Turabian StyleJensen, Caroline, Hanna Fjeldheim Dale, Trygve Hausken, Jan Gunnar Hatlebakk, Ingeborg Brønstad, Gülen Arslan Lied, and Dag Arne Lihaug Hoff. 2020. "Supplementation with Low Doses of a Cod Protein Hydrolysate on Glucose Regulation and Lipid Metabolism in Adults with Metabolic Syndrome: A Randomized, Double-Blind Study" Nutrients 12, no. 7: 1991. https://doi.org/10.3390/nu12071991
APA StyleJensen, C., Fjeldheim Dale, H., Hausken, T., Hatlebakk, J. G., Brønstad, I., Lied, G. A., & Hoff, D. A. L. (2020). Supplementation with Low Doses of a Cod Protein Hydrolysate on Glucose Regulation and Lipid Metabolism in Adults with Metabolic Syndrome: A Randomized, Double-Blind Study. Nutrients, 12(7), 1991. https://doi.org/10.3390/nu12071991





