Research Progress on 18F-Labeled Agents for Imaging of Myocardial Perfusion with Positron Emission Tomography
Abstract
:1. Introduction
2. Lipophilic Cations
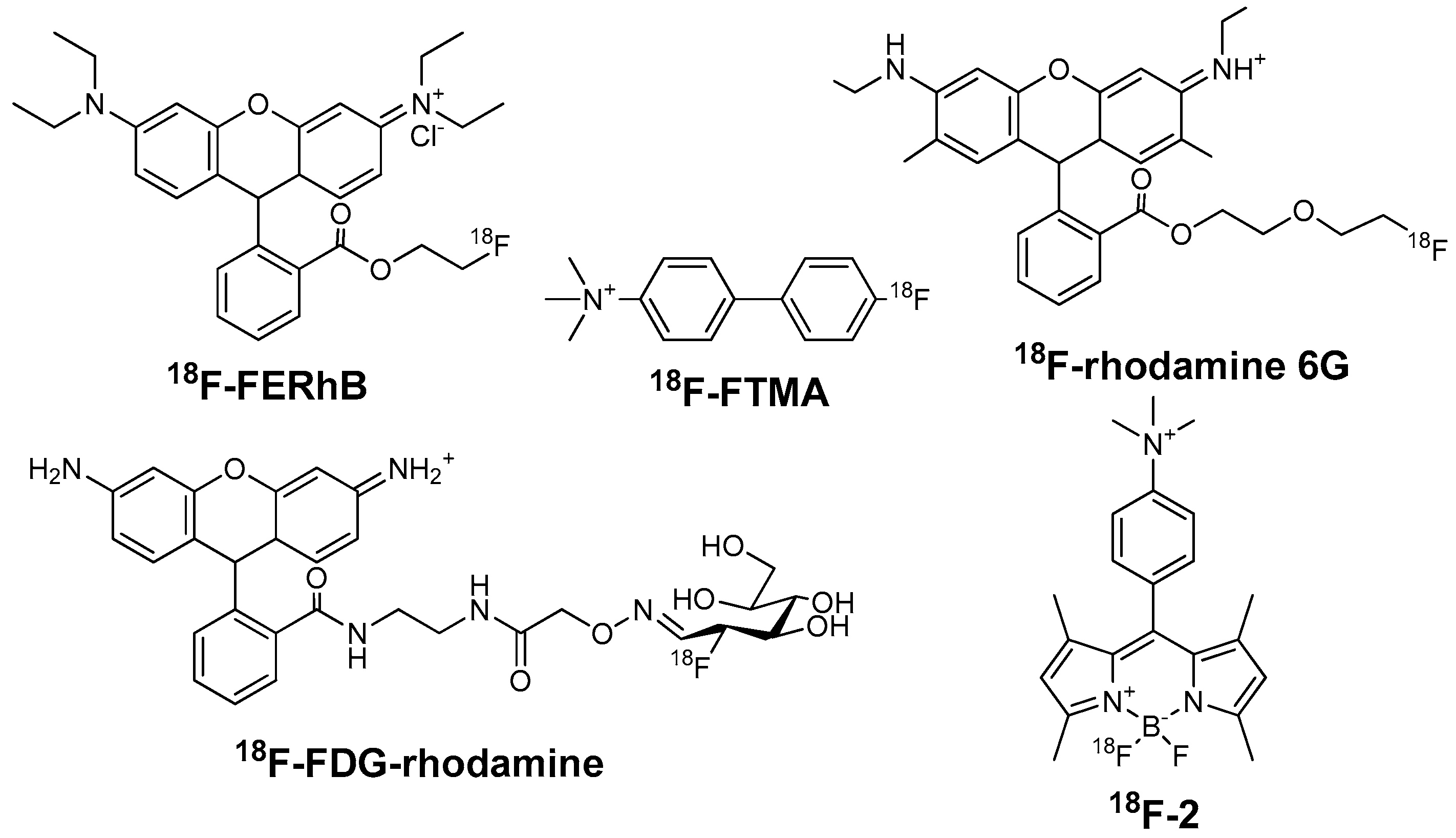
2.1. Ammonium Cations
2.1.1. 4-18F-Fluorotri-N-Methylanilinium Iodide (18F-FTMA)
2.1.2. 18F-Labeled Rhodamines
2.1.3. 18F-Labeled BODIPY Derivatives
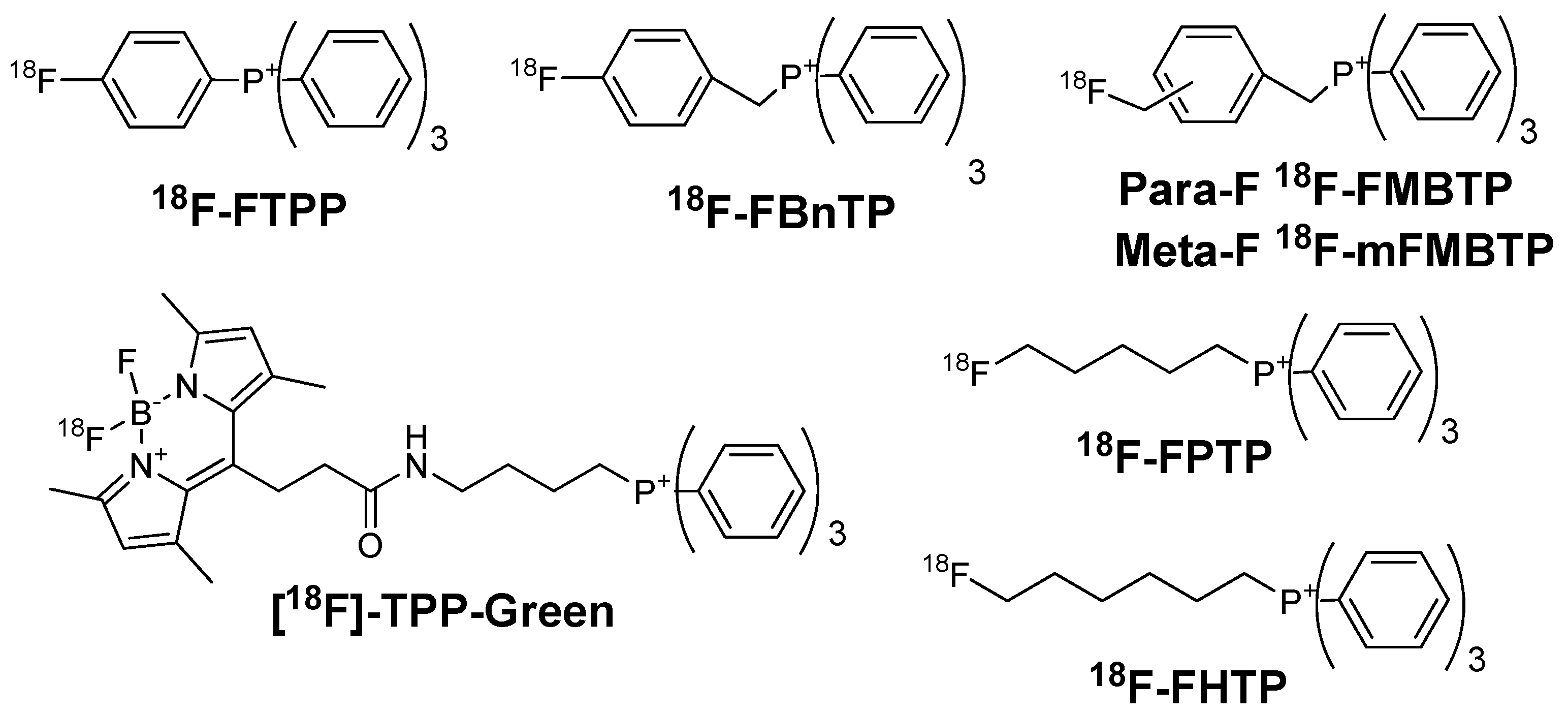
2.2. Phosphonium Cations
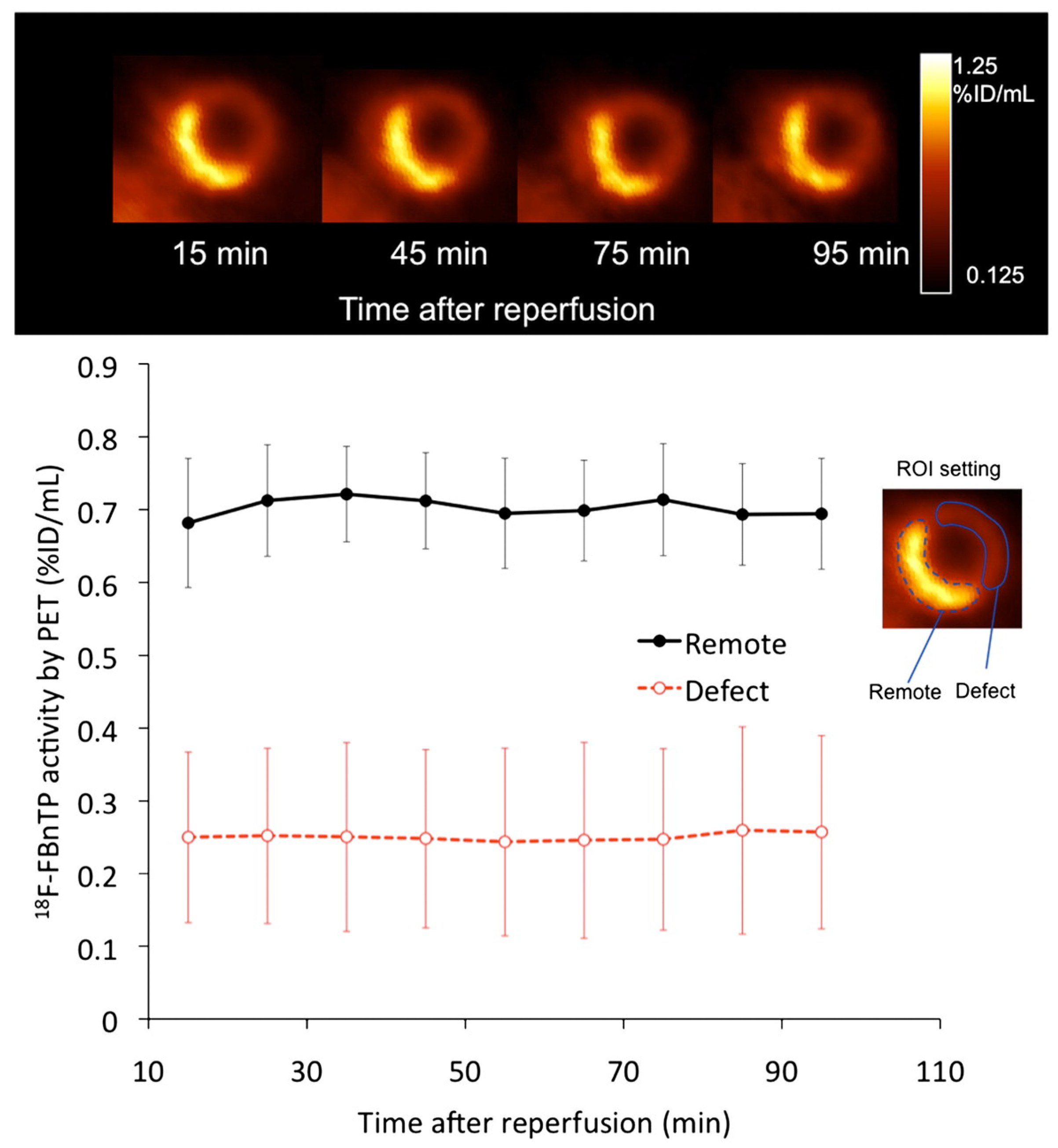
2.2.1. 18F-Fluorobenzyl Triphenyl Phosphonium (18F-FBnTP) Cation
2.2.2. (4-18F-Fluorophenyl)triphenylphosphonium (18F-FTPP) Cation
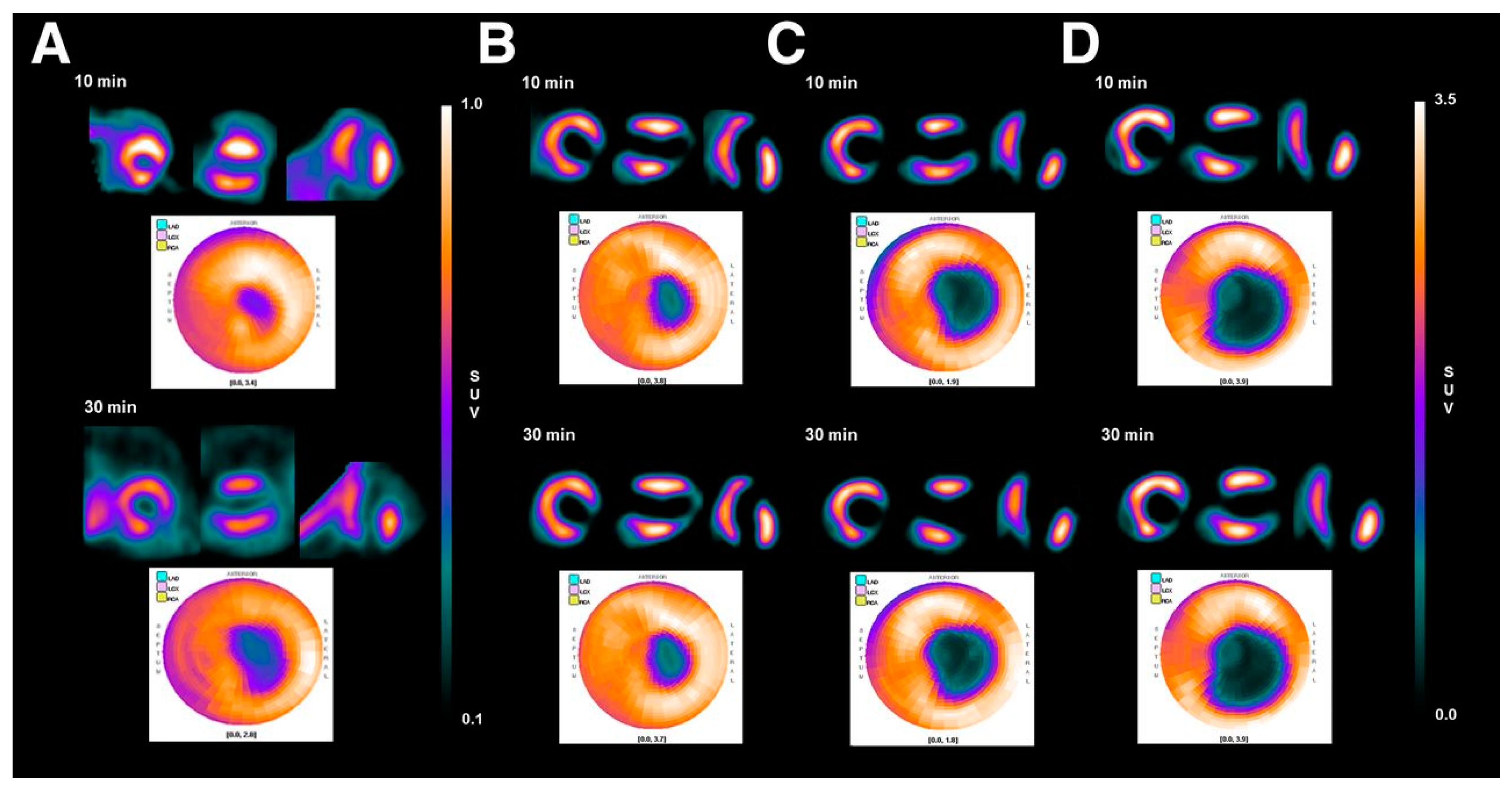
2.2.3. 18F-Labeled Fluoroalkylphosphonium Derivatives
2.2.4. 4-(18F-Fluoromethyl)benzyltriphenyl Phosphonium (18F-FMBTP) Cation and (3-(18F-Fluoro-methyl)benzyl)trisphenylphosphonium (18F-mFMBTP) Cation
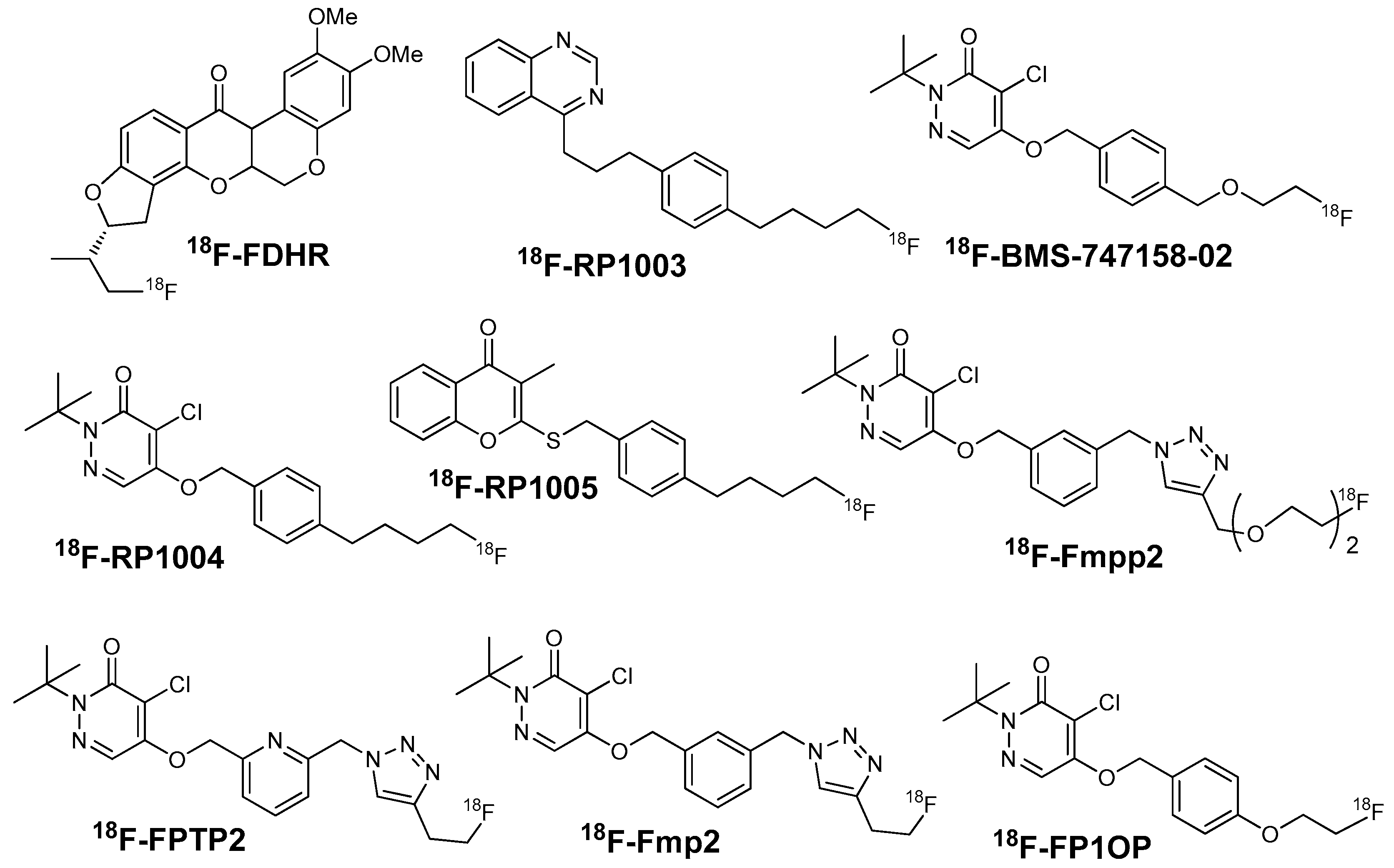
3. Analogues of MC-1 Inhibitors
3.1. 18F-Fluorodihydrorotenone (18F-FDHR)
3.2. (2-Tert-butyl-4-chloro-5-[4-(2-18F-fluoroethoxymethyl)-benzyloxy]-2H-pyridazin-3-one (18F-Flurpiridaz)
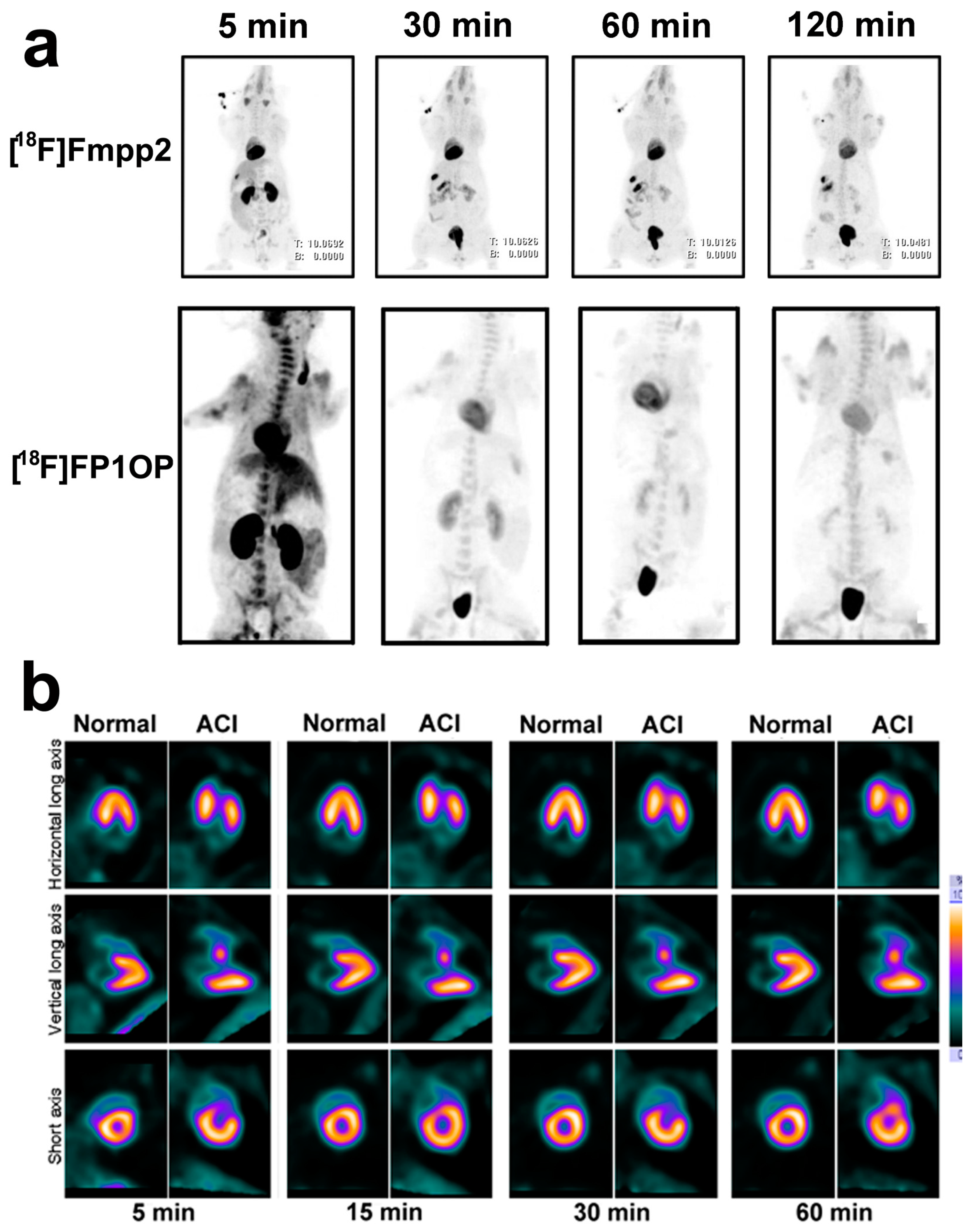
3.3. 2-Tert-butyl-4-chloro-5-(4-(2-18F-fluoroethoxy))benzyloxy-2H-pyridazin-3-one (18F-FP1OP) and 4-Chloro-2-tert-butyl-5-[2-[[1-[2-[2-[18F]fluroethoxy]ethoxymethyl]-1H-1,2,3-triazol-4-yl]methyl]phenyl-methoxy]-3(2H)-pyridazinone ([18F]Fmpp2)
4. Conclusions and Perspectives
Acknowledgments
Author Contributions
Conflicts of Interest
Abbreviations
| CAD | coronary artery disease |
| SPECT | single-photon emission computed tomography |
| MPI | myocardial perfusion imaging |
| PET | positron emission tomography |
| MC-1 | mitochondrial complex-1 |
| SUV | standardized uptake value |
| AcChE | acetylcholinesterase |
| p.i. | post injection |
| PEG | polyethylene glycol |
| NDC | non-decay-corrected |
| DC | decay-corrected |
| 18F-FTMA | 4-18F-fluorotri-N-methylanilinium |
| 18F-FERhB | 2-18F-fluoroethylrhodamine B |
| 18F-FDG-rhodamine | 18F-fluoro-2-deoxy-d-glucose-rhodamine |
| BODIPY | Boron-dipyrromethene |
| 18F-2 | 10-(4-(trimethylammonio)phenyl)-5-fluoro-5-18F-fluoro-1,3,7,9-tetramethyl-5H-dipyrrolo-[1,2-c:2′,1′f][1,3,2] diazaborinin-4-ium-5-ide |
| 18F-FBnTP | 18F-fluorobenzyltriphenylphosphonium |
| 18F-FTPP | (4-18F-fluorophenyl)triphenylphosphonium cation |
| 18F-FPTP | (18F-fluoropentyl)triphenylphosphonium cation |
| 18F-FHTP | (6-18F-Fluorohexyl) triphenylphosphonium cation |
| 18F-FETMP | (2-(2-18F-fluoroethoxy)ethyl) tris(4-methoxyphenyl)phosphonium cation |
| 18F-FMBTP | 4-(18F-fluoromethyl)benzyltriphenylphosphonium |
| 18F-mFMBTP | (3-(18F-fluoromethyl) benzyl)trisphenylphosphonium |
| 18F-FDHR | 18F-fluorodihydrorotenone |
| 18F-flurpiridaz (BMS-747158-02) | 2-tert-butyl-4-chloro-5-[4-(2-18F-fluoroethoxymethyl)benzyloxy]-2H-pyridazin-3-one |
| 18F-FP1OP | 2-tert-butyl-4-chloro-5-(4-(2-18F-fluoroethoxy))benzyloxy-2H-pyridazin-3-one |
| 18F-FPTP2 | 2-tert-butyl-4-chloro-5-((6-((4-(2-18F-fluoroethyl)-1H-1,2,3-triazol-1-yl)methyl)-2-pyridinyl)methoxy)-3(2H)-pyridazinone |
| 18F-Fmp2 | 4-chloro-2-tert-butyl-5-[2-[[1-[2-[18F]fluoroethyl]-1H-1,2,3-triazol-4-yl]methyl]phenyl-methoxy]-3(2H)-pyridazinone |
| [18F]Fmpp2 | 4-chloro-2-tert-butyl-5-[2-[[1-[2-[2-[18F]fluroethoxy]ethoxymethyl]-1H-1,2,3-triazol-4-yl]-methyl]phenylmethoxy]-3(2H)-pyridazinone |
References
- Klocke, F.J.; Baird, M.G.; Lorell, B.H.; Bateman, T.M.; Messer, J.V.; Berman, D.S.; O’Gara, P.T.; Carabello, B.A.; Russell, R.O.J.; Cerqueira, M.D.; et al. ACC/AHA/ASNC Guidelines for the Clinical Use of Cardiac Radionuclide Imaging-Executive Summary: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC Committee to Revise the 1995 Guidelines for the Clinical Use of Cardiac Radionuclide Imaging). Circulation 2003, 108, 1404–1418. [Google Scholar] [PubMed]
- Guludec, D.; Lautamäki, R.; Knuuti, J.; Bax, J.J.; Bengel, F.M. Present and future of clinical cardiovascular PET imaging in Europe—A position statement by the European Council of Nuclear Cardiology (ECNC). Eur. J. Nucl. Med. Mol. Imaging 2008, 35, 1709–1724. [Google Scholar] [CrossRef] [PubMed]
- Dilsizian, V.; Bacharach, S.L.; Beanlands, R.S.; Bergmann, S.R.; Delbeke, D.; Dorbala, S.; Gropler, R.J.; Knuuti, J.; Schelbert, H.R.; Travin, M.I. ASNC imaging guidelines/SNMMI procedure standard for positron emission tomography (PET) nuclear cardiology procedures. J. Nucl. Cardiol. 2016, 23, 1187–1226. [Google Scholar] [CrossRef] [PubMed]
- Dilsizian, V. Transition from SPECT to PET myocardial perfusion imaging: A desirable change in nuclear cardiology to approach perfection. J. Nucl. Cardiol. 2016, 23, 337–338. [Google Scholar] [CrossRef] [PubMed]
- Sciagrà, R.; Passeri, A.; Bucerius, J.; Verberne, H.J.; Slart, R.H.J.A.; Lindner, O.; Gimelli, A.; Hyafil, F.; Agostini, D.; Übleis, C.; et al. Clinical use of quantitative cardiac perfusion PET: Rationale, modalities and possible indications. Position paper of the Cardiovascular Committee of the European Association of Nuclear Medicine (EANM). Eur. J. Nucl. Med. Mol. Imaging 2016, 43, 1530–1545. [Google Scholar] [CrossRef] [PubMed]
- Maddahi, J.; Czernin, J.; Lazewatsky, J.; Huang, S.; Dahlbom, M.; Schelbert, H.; Sparks, R.; Ehlgen, A.; Crane, P.; Zhu, Q.; et al. Phase I, First-in-Human Study of BMS747158, a Novel 18F-Labeled Tracer for Myocardial Perfusion PET: Dosimetry, Biodistribution, Safety, and Imaging Characteristics After a Single Injection at Rest. J. Nucl. Med. 2011, 52, 1490–1498. [Google Scholar] [CrossRef] [PubMed]
- Senthamizhchelvan, S.; Bravo, P.E.; Esaias, C.; Lodge, M.A.; Merrill, J.; Hobbs, R.F.; Sgouros, G.; Bengel, F.M. Human Biodistribution and Radiation Dosimetry of 82Rb. J. Nucl. Med. 2010, 51, 1592–1599. [Google Scholar] [CrossRef] [PubMed]
- Bober, R.M.; Thompson, C.D.; Morin, D.P. The effect of coronary revascularization on regional myocardial blood flow as assessed by stress positron emission tomography. J. Nucl. Cardiol. 2016, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Srivastava, A.V.; Ananthasubramaniam, K. Guiding coronary revascularization using PET stress myocardial perfusion imaging: The proof is in the pudding. J. Nucl. Cardiol. 2016, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Taqueti, V.R.; Dorbala, S. The role of positron emission tomography in the evaluation of myocardial ischemia in women. J. Nucl. Cardiol. 2016, 23, 1008–1015. [Google Scholar] [CrossRef] [PubMed]
- Bateman, T.M.; Dilsizian, V.; Beanlands, R.S.; DePuey, E.G.; Heller, G.V.; Wolinsky, D.A. American Society of Nuclear Cardiology and Society of Nuclear Medicine and Molecular Imaging Joint Position Statement on the Clinical Indications for Myocardial Perfusion PET. J. Nucl. Med. 2016, 57, 1654–1656. [Google Scholar] [CrossRef] [PubMed]
- Dilsizian, V. Highlights from the Updated Joint ASNC/SNMMI PET Myocardial Perfusion and Metabolism Clinical Imaging Guidelines. J. Nucl. Med. 2016, 57, 1327–1328. [Google Scholar] [CrossRef] [PubMed]
- Heller, G.V.; Calnon, D.; Dorbala, S. Recent advances in cardiac PET and PET/CT myocardial perfusion imaging. J. Nucl. Cardiol. 2009, 16, 962–969. [Google Scholar] [CrossRef] [PubMed]
- Sarikaya, I. Cardiac applications of PET. Nucl. Med. Commun. 2015, 36, 971–985. [Google Scholar] [CrossRef] [PubMed]
- Hung, G.; Wang, Y.; Su, H.; Hsieh, T.; Ko, C.; Yen, R. New Trends in Radionuclide Myocardial Perfusion Imaging. Acta Cardiol. Sin. 2016, 32, 156–166. [Google Scholar] [PubMed]
- Maddahi, J.; Packard, R.R.S. Cardiac PET Perfusion Tracers: Current Status and Future Directions. Semin. Nucl. Med. 2014, 44, 333–343. [Google Scholar] [CrossRef] [PubMed]
- Schindler, T.H. Positron-Emitting Myocardial Blood Flow Tracers and Clinical Potential. Prog. Cardiovasc. Dis. 2015, 57, 588–606. [Google Scholar] [CrossRef] [PubMed]
- Lin, X.; Zhang, J.; Wang, X.; Tang, Z.; Zhang, X.; Lu, J. Development of radiolabeled compounds for myocardial perfusion imaging. Curr. Pharm. Des. 2012, 18, 1041–1057. [Google Scholar] [CrossRef] [PubMed]
- Rischpler, C.; Park, M.J.; Fung, G.S.K.; Javadi, M.; Tsui, B.M.W.; Higuchi, T. Advances in PET myocardial perfusion imaging: F-18 labeled tracers. Ann. Nucl. Med. 2012, 26, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.P.; Smith, R.A.J. Targeting Antioxidants to Mitochondria by Conjugation to Lipophilic Cations. Annu. Rev. Pharmacol. Toxicol. 2007, 47, 629–656. [Google Scholar] [CrossRef] [PubMed]
- Madar, I.; Ravert, H.T.; Du, Y.; Hilton, J.; Volokh, L.; Dannals, R.F.; Frost, J.J.; Hare, J.M. Characterization of Uptake of the New PET Imaging Compound 18F-Fluorobenzyl Triphenyl Phosphonium in Dog Myocardium. J. Nucl. Med. 2006, 47, 1359–1366. [Google Scholar] [PubMed]
- Kroemer, G. Mitochondrial control of apoptosis: An introduction. Biochem. Biophys. Res. Commun. 2003, 304, 433–435. [Google Scholar] [CrossRef]
- Studenov, A.R.; Berridge, M.S. Synthesis and properties of 18F-labeled potential myocardial blood flow tracers. Nucl. Med. Biol. 2001, 28, 683–693. [Google Scholar] [CrossRef]
- Vora, M.M.; Dhalla, M. In vivo studies of unlabeled and radioiodinated rhodamine-123. Nucl. Med. Biol. 1992, 19, 405–410. [Google Scholar] [CrossRef]
- Gottumukkala, V.; Heinrich, T.K.; Baker, A.; Dunning, P.; Fahey, F.H.; Treves, S.T.; Packard, A.B. Biodistribution and stability studies of [18F]Fluoroethylrhodamine B, a potential PET myocardial perfusion agent. Nucl. Med. Biol. 2010, 37, 365–370. [Google Scholar] [CrossRef] [PubMed]
- AlJammaz, I.; Al-Otaibi, B.; AlHindas, H.; Okarvi, S.M. Novel synthesis and initial preclinical evaluation of 18F-[FDG] labeled rhodamine: A potential PET myocardial perfusion imaging agent. Nucl. Med. Biol. 2015, 42, 804–808. [Google Scholar] [CrossRef] [PubMed]
- Bartholomä, M.D.; Zhang, S.; Akurathi, V.; Pacak, C.A.; Dunning, P.; Fahey, F.H.; Cowan, D.B.; Ted Treves, S.; Packard, A.B. 18F-labeled rhodamines as potential myocardial perfusion agents: Comparison of pharmacokinetic properties of several rhodamines. Nucl. Med. Biol. 2015, 42, 796–803. [Google Scholar] [CrossRef] [PubMed]
- Nigam, S.; Burke, B.P.; Davies, L.H.; Domarkas, J.; Wallis, J.F.; Waddell, P.G.; Waby, J.S.; Benoit, D.M.; Seymour, A.M.; Cawthorne, C.; et al. Structurally optimised BODIPY derivatives for imaging of mitochondrial dysfunction in cancer and heart cells. Chem. Commun. 2016, 52, 7114–7117. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Lin, T.; Liu, S.; Huang, C.; Hudnall, T.W.; Gabbaï, F.P.; Conti, P.S. Rapid aqueous [18F]-labeling of a bodipy dye for positron emission tomography/fluorescence dual modality imaging. Chem. Commun. 2011, 47, 9324–9326. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Li, D.; Shan, H.; Gabbaï, F.P.; Li, Z.; Conti, P.S. Evaluation of 18F-labeled BODIPY dye as potential PET agents for myocardial perfusion imaging. Nucl. Med. Biol. 2014, 41, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Chansaenpak, K.; Wang, H.; Wang, M.; Giglio, B.; Ma, X.; Yuan, H.; Hu, S.; Wu, Z.; Li, Z. Synthesis and Evaluation of [18F]-Ammonium BODIPY Dyes as Potential Positron Emission Tomography Agents for Myocardial Perfusion Imaging. Chemistry 2016, 22, 12122–12129. [Google Scholar] [CrossRef] [PubMed]
- Ravert, H.T.; Madar, I.; Dannals, R.F. Radiosynthesis of 3-[18F]fluoropropyl and 4-[18F]fluorobenzyl triarylphosphonium ions. J. Label. Compd. Radiopharm. 2004, 47, 469–476. [Google Scholar] [CrossRef]
- Madar, I.; Ravert, H.; DiPaula, A.; Du, Y.; Dannals, R.F.; Becker, L. Assessment of Severity of Coronary Artery Stenosis in a Canine Model Using the PET Agent 18F-Fluorobenzyl Triphenyl Phosphonium: Comparison with 99mTc-Tetrofosmin. J. Nucl. Med. 2007, 48, 1021–1030. [Google Scholar] [CrossRef] [PubMed]
- Higuchi, T.; Fukushima, K.; Rischpler, C.; Isoda, T.; Javadi, M.S.; Ravert, H.; Holt, D.P.; Dannals, R.F.; Madar, I.; Bengel, F.M. Stable Delineation of the Ischemic Area by the PET Perfusion Tracer 18F-Fluorobenzyl Triphenyl Phosphonium After Transient Coronary Occlusion. J. Nucl. Med. 2011, 52, 965–969. [Google Scholar] [CrossRef] [PubMed]
- Ravert, H.T.; Holt, D.P.; Dannals, R.F. A microwave radiosynthesis of the 4-[18F]-fluorobenzyltriphenylphosphonium ion. J. Label. Compd. Radiopharm. 2015, 57, 695–698. [Google Scholar] [CrossRef] [PubMed]
- Tominaga, T.; Ito, H.; Ishikawa, Y.; Ren, I.; Ishiwata, K.; Furumoto, S. Radiosynthesis and preliminary biological evaluation of a new 18F-labeled triethylene glycol derivative of triphenylphosphonium. J. Label. Compd. Radiopharm. 2016, 59, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.; Zhang, C.; Lau, J.; Colpo, N.; Bénard, F.; Lin, K.S. One-step synthesis of 4-[18F]fluorobenzyltriphenylphosphonium cation for imaging with positron emission tomography. J. Label. Compd. Radiopharm. 2016, 59, 467–471. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Z.; Subbarayan, M.; Chen, X.; Gambhir, S.S. Synthesis of (4-[18F]fluorophenyl)triphenylphosphonium as a potential imaging agent for mitochondrial dysfunction. J. Label. Compd. Radiopharm. 2005, 48, 131–137. [Google Scholar] [CrossRef]
- Shoup, T.M.; Elmaleh, D.R.; Brownell, A.; Zhu, A.; Guerrero, J.L.; Fischman, A.J. Evaluation of (4-[18F]Fluorophenyl)triphenylphosphonium Ion. A Potential Myocardial Blood Flow Agent for PET. Mol. Imaging Biol. 2010, 13, 511–517. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Kim, H.; Yu, K.; Min, J. Synthesis of [18F]-labeled (2-(2-fluoroethoxy)ethyl)tris(4-methoxyphenyl)phosphonium cation as a potential agent for positron emission tomography myocardial imaging. Nucl. Med. Biol. 2012, 39, 1093–1098. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Yu, K.; Bom, H.; Min, J. Synthesis of (4-[18F]Fluorophenyl)triphenylphosphonium as a mitochondrial voltage sensor for PET. Nucl. Med. Mol. Imaging 2007, 41, 561–565. [Google Scholar]
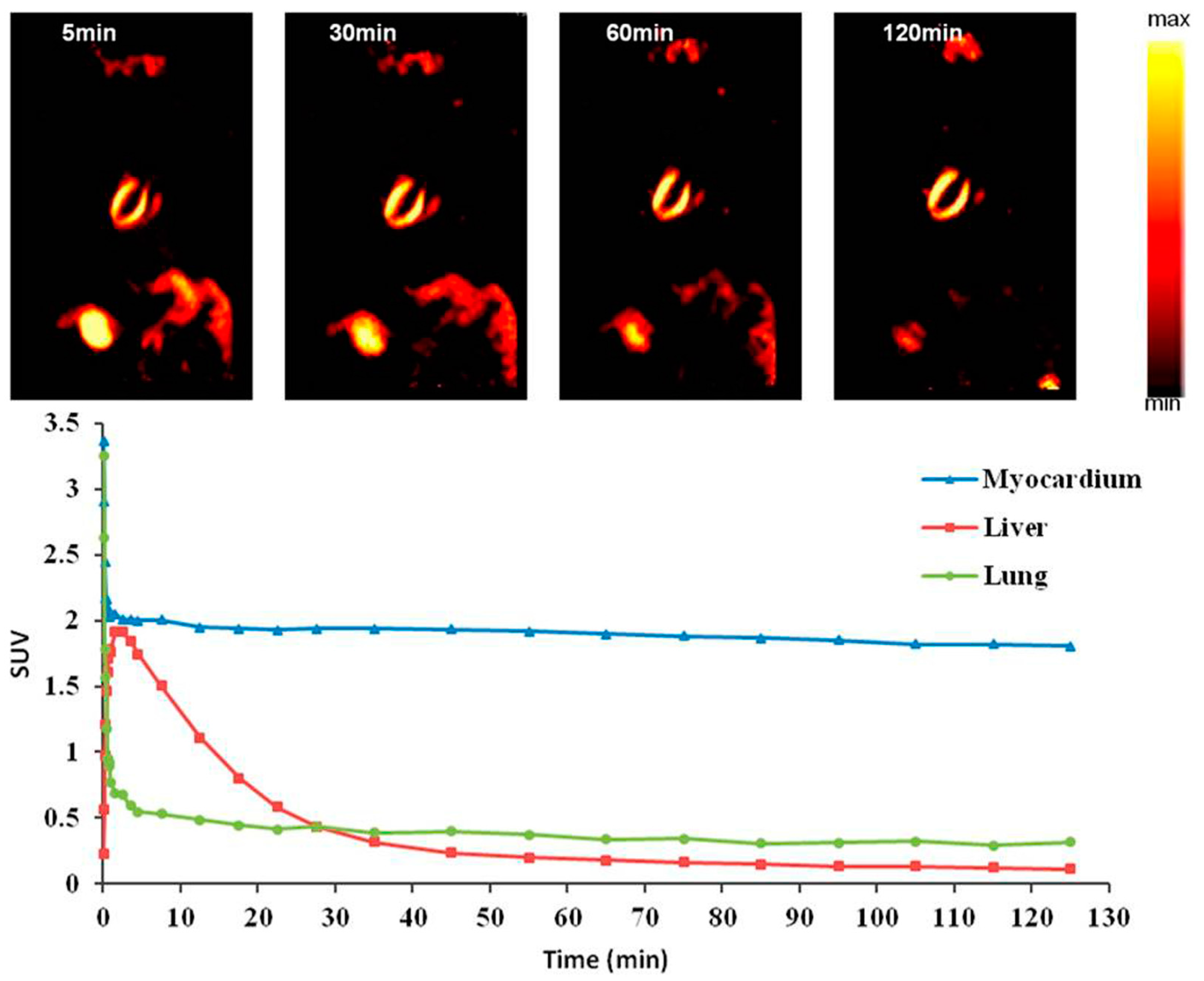
- Kim, D.; Kim, H.S.; Reder, S.; Zheng, J.H.; Herz, M.; Higuchi, T.; Pyo, A.; Bom, H.; Schwaiger, M.; Min, J. Comparison of 18F-Labeled Fluoroalkylphosphonium Cations with 13N-NH3 for PET Myocardial Perfusion Imaging. J. Nucl. Med. 2015, 56, 1581–1586. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.; Min, J. Radiolabeled Phosphonium Salts as Mitochondrial Voltage Sensors for Positron Emission Tomography Myocardial Imaging Agents. Nucl. Med. Mol. Imaging 2016, 50, 185–195. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Z.; Yu, Q.; Mou, T.; Liu, C.; Yang, W.; Fang, W.; Peng, C.; Lu, J.; Liu, Y.; Zhang, X. Highly efficient one-pot labeling of new phosphonium cations with fluorine-18 as potential PET agents for myocardial perfusion imaging. Mol. Pharm. 2014, 11, 3823–3831. [Google Scholar] [CrossRef] [PubMed]
- Degli Esposti, M. Inhibitors of NADH-ubiquinone reductase: An overview. Biochim. Biophys. Acta-Bioenerg. 1998, 1364, 222–235. [Google Scholar] [CrossRef]
- Yuan, H.; Cho, H.; Chen, H.H.; Panagia, M.; Sosnovik, D.E.; Josephson, L. Fluorescent and radiolabeled triphenylphosphonium probes for imaging mitochondria. Chem. Commun. 2013, 49, 10361–10363. [Google Scholar] [CrossRef] [PubMed]
- Hunte, C.; Zickermann, V.; Brandt, U. Functional Modules and Structural Basis of Conformational Coupling in Mitochondrial Complex I. Science 2010, 329, 448–451. [Google Scholar] [CrossRef] [PubMed]
- Marshall, R.C.; Powers-Risius, P.; Reutter, B.W.; Taylor, S.E.; VanBrocklin, H.F.; Huesman, R.H.; Budinger, T.F. Kinetic Analysis of 125I-Iodorotenone as a Deposited Myocardial Flow Tracer: Comparison with 99mTc-Sestamibi. J. Nucl. Med. 2001, 42, 272–281. [Google Scholar] [PubMed]
- Marshall, R.C.; Powers-Risius, P.; Reutter, B.W.; O’Neil, J.P.; La Belle, M.; Huesman, R.H.; VanBrocklin, H.F. Kinetic Analysis of 18F-Fluorodihydrorotenone as a Deposited Myocardial Flow Tracer: Comparison to 201Tl. J. Nucl. Med. 2004, 45, 1950–1959. [Google Scholar] [PubMed]
- Yu, M.; Guaraldi, M.; Kagan, M.; Mistry, M.; McDonald, J.; Bozek, J.; Yalamanchili, P.; Hayes, M.; Azure, M.; Purohit, A.; et al. Assessment of 18F-labeled mitochondrial complex I inhibitors as PET myocardial perfusion imaging agents in rats, rabbits, and primates. Eur. J. Nucl. Med. Mol. Imaging 2008, 36, 63–72. [Google Scholar] [CrossRef] [PubMed]
- Nekolla, S.G.; Reder, S.; Saraste, A.; Higuchi, T.; Dzewas, G.; Preissel, A.; Huisman, M.; Poethko, T.; Schuster, T.; Yu, M.; et al. Evaluation of the Novel Myocardial Perfusion Positron-Emission Tomography Tracer 18F-BMS-747158-02: Comparison to 13N-Ammonia and Validation With Microspheres in a Pig Model. Circulation 2009, 119, 2333–2342. [Google Scholar] [CrossRef] [PubMed]
- Bateman, T.M.; Maddahi, J.; Udelson, J.; Beanlands, R.; Knuuti, J.; Heller, G.; Berman, D.; Lazewatsky, J.; Orlandi, C. Improved assessment of CAD in obese subjects with flurpiridaz F18 PET myocardial perfusion imaging: A subset analysis of the flurpiridaz F18 301 phase 3 study. J. Am. Coll. Cardiol. 2016, 67, 1578. [Google Scholar] [CrossRef]
- Brunken, R.C. Promising New 18F-Labeled Tracers for PET Myocardial Perfusion Imaging. J. Nucl. Med. 2015, 56, 1478–1479. [Google Scholar] [CrossRef] [PubMed]
- Yalamanchili, P.; Wexler, E.; Hayes, M.; Yu, M.; Bozek, J.; Kagan, M.; Radeke, H.S.; Azure, M.; Purohit, A.; Casebier, D.S.; et al. Mechanism of uptake and retention of F-18 BMS-747158-02 in cardiomyocytes: A novel PET myocardial imaging agent. J. Nucl. Cardiol. 2007, 14, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Higuchi, T.; Nekolla, S.G.; Huisman, M.M.; Reder, S.; Poethko, T.; Yu, M.; Wester, H.; Casebier, D.S.; Robinson, S.P.; Botnar, R.M.; et al. A New 18F-Labeled Myocardial PET Tracer: Myocardial Uptake After Permanent and Transient Coronary Occlusion in Rats. J. Nucl. Med. 2008, 49, 1715–1722. [Google Scholar] [CrossRef] [PubMed]
- Huisman, M.C.; Higuchi, T.; Reder, S.; Nekolla, S.G.; Poethko, T.; Wester, H.; Ziegler, S.I.; Casebier, D.S.; Robinson, S.P.; Schwaiger, M. Initial Characterization of an 18F-Labeled Myocardial Perfusion Tracer. J. Nucl. Med. 2008, 49, 630–636. [Google Scholar] [CrossRef] [PubMed]
- Sherif, H.M.; Saraste, A.; Weidl, E.; Weber, A.W.; Higuchi, T.; Reder, S.; Poethko, T.; Henriksen, G.; Casebier, D.; Robinson, S.; et al. Evaluation of a Novel 18F-Labeled Positron-Emission Tomography Perfusion Tracer for the Assessment of Myocardial Infarct Size in Rats. Circ. Cardiovasc. Imaging 2009, 2, 77–84. [Google Scholar] [CrossRef] [PubMed]
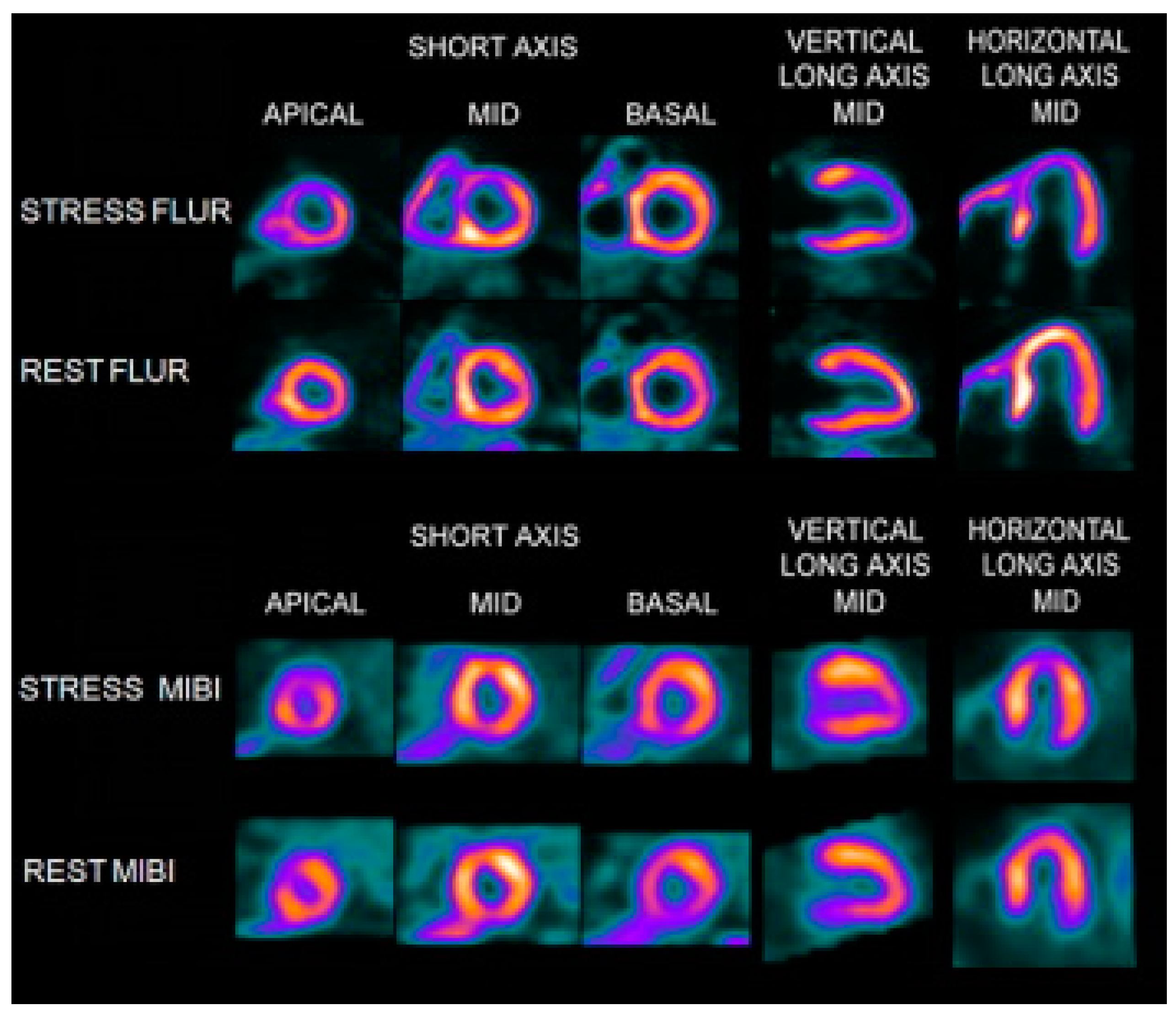
- Berman, D.S.; Maddahi, J.; Tamarappoo, B.K.; Czernin, J.; Taillefer, R.; Udelson, J.E.; Gibson, C.M.; Devine, M.; Lazewatsky, J.; Bhat, G. Phase II Safety and Clinical Comparison With Single-Photon Emission Computed Tomography Myocardial Perfusion Imaging for Detection of Coronary Artery Disease. J. Am. Coll. Cardiol. 2013, 61, 469–477. [Google Scholar] [CrossRef] [PubMed]
- Mou, T.; Jing, H.; Yang, W.; Fang, W.; Peng, C.; Guo, F.; Zhang, X.; Pang, Y.; Ma, Y. Preparation and biodistribution of [18F]FP2OP as myocardial perfusion imaging agent for positron emission tomography. Bioorg. Med. Chem. 2010, 18, 1312–1320. [Google Scholar] [CrossRef] [PubMed]
- Mou, T.; Zhao, Z.; Fang, W.; Peng, C.; Guo, F.; Liu, B.; Ma, Y.; Zhang, X. Synthesis and Preliminary Evaluation of 18F-Labeled Pyridaben Analogues for Myocardial Perfusion Imaging with PET. J. Nucl. Med. 2012, 53, 472–479. [Google Scholar] [CrossRef] [PubMed]
- Mou, T.; Zhao, Z.; Zhang, P.; Fang, W.; Peng, C.; Lu, J.; Wang, Q.; Ma, Y.; Zhang, X. Synthesis and bio-evaluation of New 18F-Labeled Pyridaben Analogs with Improved Stability for Myocardial Perfusion Imaging in Mice. Chem. Biol. Drug Des. 2015, 86, 351–361. [Google Scholar] [CrossRef] [PubMed]
- Mou, T.; Zhao, Z.; You, L.; Li, Y.; Qian, W.; Wei, F.; Jie, L.; Cheng, P.; Zhang, X. Synthesis and Evaluation of 18F-labeled Pyridaben Analogues for Myocardial Perfusion Imaging in Mice, Rats and Chinese mini-swine. Sci. Rep. 2016, 6, 33450. [Google Scholar] [CrossRef] [PubMed]
- Chinese Society of Nuclear Medicine. A brief report on the results of the national survey of nuclear medicine in 2012. Chin. J. Nucl. Med. Mol. Imaging 2012, 32, 357. [Google Scholar]
- Chinese Society of Nuclear Medicine. A brief report on the results of the national survey of nuclear medicine in 2016. Chin. J. Nucl. Med. Mol. Imaging 2016, 36, 479–480. [Google Scholar]
Sample Availability: Not available. |
| Probes | 18F-FDG-Rhodamine | 18F-FBnTP | 18F-FTTP | 18F-mFMBTP | 18F-Flurpiridaz | 18F-Fmpp2 |
|---|---|---|---|---|---|---|
| Class | ammonium cation | phosphonium cation | phosphonium cation | phosphonium cation | MC-1 inhibitors | MC-1 inhibitors |
| Charge | cationic | cationic | cationic | cationic | neutral | neutral |
| Log P | −1.64 ± 0.03 | -- | 1.78 ± 0.05 | 1.05 ± 0.01 | -- | 1.73 ± 0.05 |
| RCY (%) | 97.0 ± 1.9 (based on 18F-FDG) | 62 ± 1.4 (NDC) | 10–15 (EOS) | 50 (DC) | 25 (DC) | 58 ± 7.1 (DC) |
| Heart Uptake (%ID/g) | 11.24 ± 1.97 (rat) | -- | 1.51 ± 0.04 (rat) | 27.39 ± 1.46 (mice) | 9.5 ± 0.5 (mice) | 27.15 ± 3.58 (mice) |
| Heart/Liver Ratio | 21.2 (rat) | 1.2 (dog) | 8 (rat) | 4.84 (mice) | 8.3 (mice) | 3.96 (mice) |
| Heart/Blood Ratio | 28.10 (rat) | 16.6 (dog) | 75.5 (rat) | 23.82 (mice) | -- | 10.29 (mice) |
| Time point (min) * | -- | 60 | 30 | 30 | 60 | 30 |
| Current status | rats | dogs | rabbits | dogs | Clinic trial (Phase III) | pigs |
| References | 26 | 21, 32, 37 | 39 | 44 | 53 | 62 |
© 2017 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mou, T.; Zhang, X. Research Progress on 18F-Labeled Agents for Imaging of Myocardial Perfusion with Positron Emission Tomography. Molecules 2017, 22, 562. https://doi.org/10.3390/molecules22040562
Mou T, Zhang X. Research Progress on 18F-Labeled Agents for Imaging of Myocardial Perfusion with Positron Emission Tomography. Molecules. 2017; 22(4):562. https://doi.org/10.3390/molecules22040562
Chicago/Turabian StyleMou, Tiantian, and Xianzhong Zhang. 2017. "Research Progress on 18F-Labeled Agents for Imaging of Myocardial Perfusion with Positron Emission Tomography" Molecules 22, no. 4: 562. https://doi.org/10.3390/molecules22040562






