Differences in the Prevalence and Clinical Correlates Between Early-Onset and Late-Onset Major Depressive Disorder Patients with Comorbid Abnormal Lipid Metabolism
Abstract
1. Introduction
2. Methods
2.1. Subjects
2.2. Demographic Characteristics, Clinical Interview, and Assessment
2.3. Biomarker Measurements
2.4. Statistical Analysis
3. Results
3.1. Prevalence of ALM in Early-Onset and Late-Onset MDD Patients
3.2. Comparison of Demographic and Clinical Variables and Lipid Levels Between ALM and Non-ALM Subgroups in Early- and Late-Onset MDD Patients
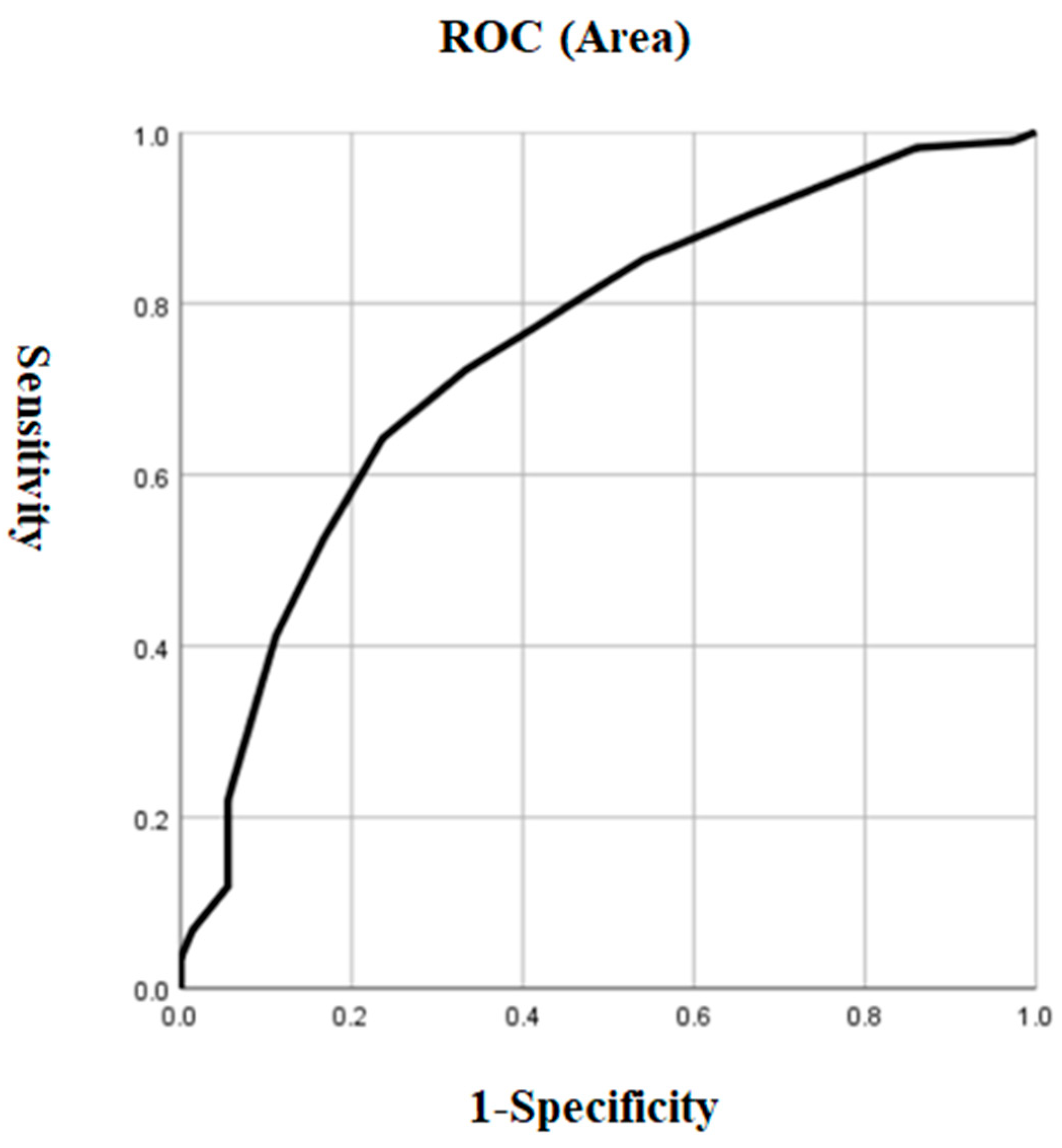
3.3. Risk Factors Associated with ALM in the Early-Onset Group
3.4. Risk Factors Associated with ALM in the Late-Onset Group
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Greenberg, P.E.; Fournier, A.A.; Sisitsky, T.; Simes, M.; Berman, R.; Koenigsberg, S.H.; Kessler, R.C. The Economic Burden of Adults with Major Depressive Disorder in the United States (2010 and 2018). PharmacoEconomics 2021, 39, 653–665. [Google Scholar] [CrossRef]
- Friedrich, M.J. Depression Is the Leading Cause of Disability Around the World. JAMA 2017, 317, 1517. [Google Scholar] [CrossRef] [PubMed]
- Rozing, M.P.; Veerhuis, R.; Westendorp, R.G.J.; Eikelenboom, P.; Stek, M.; Marijnissen, R.M.; Oude Voshaar, R.C.; Comijs, H.C.; van Exel, E. Inflammation in older subjects with early- and late-onset depression in the NESDO study: A cross-sectional and longitudinal case-only design. Psychoneuroendocrinology 2019, 99, 20–27. [Google Scholar] [CrossRef]
- Köhler, C.A.; Freitas, T.H.; Maes, M.; de Andrade, N.Q.; Liu, C.S.; Fernandes, B.S.; Stubbs, B.; Solmi, M.; Veronese, N.; Herrmann, N.; et al. Peripheral cytokine and chemokine alterations in depression: A meta-analysis of 82 studies. Acta Psychiatr. Scand. 2017, 135, 373–387. [Google Scholar] [CrossRef] [PubMed]
- Hirano, S.; Shinotoh, H.; Shimada, H.; Ota, T.; Sato, K.; Tanaka, N.; Zhang, M.R.; Higuchi, M.; Fukushi, K.; Irie, T.; et al. Voxel-Based Acetylcholinesterase PET Study in Early and Late Onset Alzheimer’s Disease. J. Alzheimer’s Dis. JAD 2018, 62, 1539–1548. [Google Scholar] [CrossRef] [PubMed]
- Szücs, A.; Szanto, K.; Wright, A.G.C.; Dombrovski, A.Y. Personality of late- and early-onset elderly suicide attempters. Int. J. Geriatr. Psychiatry 2020, 35, 384–395. [Google Scholar] [CrossRef]
- Tebeka, S.; Le Strat, Y.; Mandelbrot, L.; Benachi, A.; Dommergues, M.; Kayem, G.; Lepercq, J.; Luton, D.; Ville, Y.; Ramoz, N.; et al. Early- and late-onset postpartum depression exhibit distinct associated factors: The IGEDEPP prospective cohort study. BJOG Int. J. Obstet. Gynaecol. 2021, 128, 1683–1693. [Google Scholar] [CrossRef] [PubMed]
- Mai, N.; Wu, Y.; Zhong, X.; Chen, B.; Zhang, M.; Peng, Q.; Ning, Y. Different Modular Organization Between Early Onset and Late Onset Depression: A Study Base on Granger Causality Analysis. Front. Aging Neurosci. 2021, 13, 625175. [Google Scholar] [CrossRef]
- Korten, N.C.; Comijs, H.C.; Lamers, F.; Penninx, B.W. Early and late onset depression in young and middle aged adults: Differential symptomatology, characteristics and risk factors? J. Affect. Disord. 2012, 138, 259–267. [Google Scholar] [CrossRef]
- Grayson, L.; Thomas, A. A systematic review comparing clinical features in early age at onset and late age at onset late-life depression. J. Affect. Disord. 2013, 150, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.H.; Chen, L.; Su, Y.A.; Fang, Y.R.; Srisurapanont, M.; Hong, J.P.; Hatim, A.; Chua, H.C.; Bautista, D.; Si, T.M. Is early-onset in major depression a predictor of specific clinical features with more impaired social function? Chin. Med. J. 2015, 128, 811–815. [Google Scholar] [CrossRef]
- Emslie, G.J.; Mayes, T.L.; Ruberu, M. Continuation and maintenance therapy of early-onset major depressive disorder. Paediatr. Drugs 2005, 7, 203–217. [Google Scholar] [CrossRef] [PubMed]
- Shaker, N.M.; Sultan, M.; Mohamed, M.Y.; Helal, S.A.; Abd El Moneam, M.H.E. Lipid Profile and Impulsivity in Suicidal Patients with Major Depressive Disorder. Arch. Suicide Res. Off. J. Int. Acad. Suicide Res. 2021, 25, 641–656. [Google Scholar] [CrossRef] [PubMed]
- Gohar, S.M.; Dieset, I.; Steen, N.E.; Mørch, R.H.; Iversen, T.S.; Steen, V.M.; Andreassen, O.A.; Melle, I. Association between serum lipid levels, osteoprotegerin and depressive symptomatology in psychotic disorders. Eur. Arch. Psychiatry Clin. Neurosci. 2019, 269, 795–802. [Google Scholar] [CrossRef] [PubMed]
- Korczak, D.J.; Cleverley, K.; Birken, C.S.; Pignatiello, T.; Mahmud, F.H.; McCrindle, B.W. Cardiovascular Disease Risk Factors Among Children and Adolescents With Depression. Front. Psychiatry 2021, 12, 702737. [Google Scholar] [CrossRef]
- Almulla, A.F.; Thipakorn, Y.; Algon, A.A.A.; Tunvirachaisakul, C.; Al-Hakeim, H.K.; Maes, M. Reverse cholesterol transport and lipid peroxidation biomarkers in major depression and bipolar disorder: A systematic review and meta-analysis. Brain Behav. Immun. 2023, 113, 374–388. [Google Scholar] [CrossRef] [PubMed]
- Morelli, N.R.; Maes, M.; Bonifacio, K.L.; Vargas, H.O.; Nunes, S.O.V.; Barbosa, D.S. Increased nitro-oxidative toxicity in association with metabolic syndrome, atherogenicity and insulin resistance in patients with affective disorders. J. Affect. Disord. 2021, 294, 410–419. [Google Scholar] [CrossRef] [PubMed]
- Maes, M.; Delanghe, J.; Meltzer, H.Y.; Scharpé, S.; D’Hondt, P.; Cosyns, P. Lower degree of esterification of serum cholesterol in depression: Relevance for depression and suicide research. Acta Psychiatr. Scand. 1994, 90, 252–258. [Google Scholar] [CrossRef] [PubMed]
- Stuchtey, F.C.; Block, A.; Osei, F.; Wippert, P.M. Lipid Biomarkers in Depression: Does Antidepressant Therapy Have an Impact? Healthcare 2022, 10, 333. [Google Scholar] [CrossRef]
- Pinto, B.; Conde, T.; Domingues, I.; Domingues, M.R. Adaptation of Lipid Profiling in Depression Disease and Treatment: A Critical Review. Int. J. Mol. Sci. 2022, 23, 2032. [Google Scholar] [CrossRef] [PubMed]
- Heron, D.S.; Shinitzky, M.; Hershkowitz, M.; Samuel, D. Lipid fluidity markedly modulates the binding of serotonin to mouse brain membranes. Proc. Natl. Acad. Sci. USA 1980, 77, 7463–7467. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, S.; Nagappa, A.N.; Patil, C.R. Role of oxidative stress in depression. Drug Discov. Today 2020, 25, 1270–1276. [Google Scholar] [CrossRef]
- Zhu, T.; De Luca, V.; Gallaugher, L.A.; Woldeyohannes, H.O.; Soczynska, J.K.; Szymkowicz, S.; Muzina, D.J.; Kennedy, S.H.; McIntyre, R.S. Admixture analysis of age at onset in major depressive disorder. Gen. Hosp. Psychiatry 2012, 34, 686–691. [Google Scholar] [CrossRef]
- Zhao, Y.; Wang, N.; Chen, J.; Guan, Q.; Yuan, X.; Shen, Y.; Zhang, X.; Hao, W.; Zhang, R.; Zhai, D. Association between early-onset affective disorders and hypothyroidism in a larger number of psychiatric drug-free patients. J. Affect. Disord. 2022, 299, 31–36. [Google Scholar] [CrossRef]
- Huang, X.; Sun, Y.; Wu, A.; Zhang, X. Differences in the prevalence and clinical correlates of comorbid suicide attempts in patients with early- and late-onset major depressive disorder. Front. Psychiatry 2023, 14, 1173917. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M. A rating scale for depression. J. Neurol. Neurosurg. Psychiatry 1960, 23, 56–62. [Google Scholar] [CrossRef]
- Zimmerman, M.; Martinez, J.H.; Young, D.; Chelminski, I.; Dalrymple, K. Severity classification on the Hamilton Depression Rating Scale. J. Affect. Disord. 2013, 150, 384–388. [Google Scholar] [CrossRef] [PubMed]
- HAMILTONM The assessment of anxiety states by rating. Br. J. Med. Psychol. 1959, 32, 50–55. [CrossRef] [PubMed]
- Dong, M.X.; Wei, Y.D.; Hu, L. The disturbance of lipid metabolism is correlated with neuropsychiatric symptoms in patients with Parkinson’s disease. Chem. Phys. Lipids 2021, 239, 105112. [Google Scholar] [CrossRef]
- Kay, S.R.; Fiszbein, A.; Opler, L.A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 1987, 13, 261–276. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Li, Z.; Wang, Y.; Huang, H.; Chen, W.; Dong, L.; Wu, J.; Chen, J.; Miao, Y.; Qi, L.; et al. Prevalence and clinical correlates of psychotic depression in first-episode and drug-naïve outpatients with major depressive disorder in a Chinese Han population. J. Affect. Disord. 2020, 263, 500–506. [Google Scholar] [CrossRef]
- Tanir, Y.; Karayagmurlu, A.; Kaya, İ.; Kaynar, T.B.; Türkmen, G.; Dambasan, B.N.; Meral, Y.; Coşkun, M. Exacerbation of obsessive compulsive disorder symptoms in children and adolescents during COVID-19 pandemic. Psychiatry Res. 2020, 293, 113363. [Google Scholar] [CrossRef]
- Liu, Y.; Kong, X.; Wang, W.; Fan, F.; Zhang, Y.; Zhao, M.; Wang, Y.; Wang, Y.; Wang, Y.; Qin, X.; et al. Association of peripheral differential leukocyte counts with dyslipidemia risk in Chinese patients with hypertension: Insight from the China Stroke Primary Prevention Trial. J. Lipid Res. 2017, 58, 256–266. [Google Scholar] [CrossRef]
- Hosmer, D.; Lemeshow, S. Applied Logistic Regression; Wiley-Interscience: Hoboken, NJ, USA, 2000. [Google Scholar]
- Li, Z.; Wang, Z.; Zhang, C.; Chen, J.; Su, Y.; Huang, J.; Yi, Z.; Yuan, C.; Hong, W.; Wang, Y.; et al. Reduced ENA78 levels as novel biomarker for major depressive disorder and venlafaxine efficiency: Result from a prospective longitudinal study. Psychoneuroendocrinology 2017, 81, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Hickie, I.; Scott, E.; Naismith, S.; Ward, P.B.; Turner, K.; Parker, G.; Mitchell, P.; Wilhelm, K. Late-onset depression: Genetic, vascular and clinical contributions. Psychol. Med. 2001, 31, 1403–1412. [Google Scholar] [CrossRef]
- Skoog, I.; Waern, M.; Duberstein, P.; Blennow, K.; Zetterberg, H.; Börjesson-Hanson, A.; Östling, S.; Guo, X.; Kern, J.; Gustafson, D.; et al. A 9-year prospective population-based study on the association between the APOE*E4 allele and late-life depression in Sweden. Biol. Psychiatry 2015, 78, 730–736. [Google Scholar] [CrossRef] [PubMed]
- Smith, P.J.; Blumenthal, J.A.; Babyak, M.A.; Doraiswamy, P.M.; Hinderliter, A.; Hoffman, B.M.; Waugh, R.; Sherwood, A. Intima-media thickness and age of first depressive episode. Biol. Psychol. 2009, 80, 361–364. [Google Scholar] [CrossRef] [PubMed]
- Zhou, P.; Shen, Y.; Wang, L.; Cao, Z.; Feng, W.; Liu, J.; Wang, L.; Meng, P.; Yang, J.; Xu, W.Y.; et al. Association between carotid intima media thickness and small dense low-density lipoprotein cholesterol in acute ischaemic stroke. Lipids Health Dis. 2020, 19, 177. [Google Scholar] [CrossRef] [PubMed]
- Hou, Q.; Li, S.; Gao, Y.; Tian, H. Relations of lipid parameters, other variables with carotid intima-media thickness and plaque in the general Chinese adults: An observational study. Lipids Health Dis. 2018, 17, 107. [Google Scholar] [CrossRef]
- Mulvahill, J.S.; Nicol, G.E.; Dixon, D.; Lenze, E.J.; Karp, J.F.; Reynolds, C.F., 3rd; Blumberger, D.M.; Mulsant, B.H. Effect of Metabolic Syndrome on Late-Life Depression: Associations with Disease Severity and Treatment Resistance. J. Am. Geriatr. Soc. 2017, 65, 2651–2658. [Google Scholar] [CrossRef]
- Bharti, V.; Bhardwaj, A.; Hood, K.; Elias, D.A.; Metcalfe, A.W.S.; Kim, J.S. A systematic review and meta-analysis of lipid metabolomic signatures of Major Depressive Disorder. J. Psychiatr. Res. 2021, 139, 197–205. [Google Scholar] [CrossRef]
- Mehdi, S.M.A.; Costa, A.P.; Svob, C.; Pan, L.; Dartora, W.J.; Talati, A.; Gameroff, M.J.; Wickramaratne, P.J.; Weissman, M.M.; McIntire, L.B.J. Depression and cognition are associated with lipid dysregulation in both a multigenerational study of depression and the National Health and Nutrition Examination Survey. Transl. Psychiatry 2024, 14, 142. [Google Scholar] [CrossRef]
- Wang, J.J.; Zhuang, Z.H.; Shao, C.L.; Yu, C.Q.; Wang, W.Y.; Zhang, K.; Meng, X.B.; Gao, J.; Tian, J.; Zheng, J.L.; et al. Assessment of causal association between thyroid function and lipid metabolism: A Mendelian randomization study. Chin. Med. J. 2021, 134, 1064–1069. [Google Scholar] [CrossRef]
- Delitala, A.P.; Fanciulli, G.; Maioli, M.; Delitala, G. Subclinical hypothyroidism, lipid metabolism and cardiovascular disease. Eur. J. Intern. Med. 2017, 38, 17–24. [Google Scholar] [CrossRef]
- Vogel, A.; Brunner, J.S.; Hajto, A.; Sharif, O.; Schabbauer, G. Lipid scavenging macrophages and inflammation. Biochim. Et Biophys. Acta. Mol. Cell Biol. Lipids 2022, 1867, 159066. [Google Scholar] [CrossRef]
- Yang, C.; He, Z.; Zhang, Q.; Lu, M.; Zhao, J.; Chen, W.; Gao, L. TSH Activates Macrophage Inflammation by G13- and G15-dependent Pathways. Endocrinology 2021, 162, bqab077. [Google Scholar] [CrossRef]

| Early Onset (n = 349) | Late Onset (n = 1369) | |||||||
|---|---|---|---|---|---|---|---|---|
| With ALM (n = 277) | Without ALM (n = 72) | F | p | With ALM (1116) | Without ALM (253) | F | p | |
| Age, year | 19 (18, 20) | 19 (18, 20) | −0.262 | 0.793 | 39 (30, 48) | 37 (29, 46.5) | −2.08 | 0.038 |
| Duration of illness | 3.5 (2.5, 5) | 3.5 (2.5, 6) | −1.096 | 0.273 | 6 (3, 9) | 4.5 (3, 7.5) | −3.949 | <0.001 |
| Age of onset | 19 (18, 20) | 19 (18, 20) | −0.67 | 0.503 | 39 (30, 48) | 37 (29, 46) | −2.03 | 0.042 |
| Sex, n (%) | 0.76 | 0.383 | 0.545 | 0.46 | ||||
| 1 | 115 (41.5) | 34 (47.2) | 353 (31.6) | 86 (34) | ||||
| 2 | 162 (58.5) | 38 (52.8) | 763 (68.4) | 167 (66) | ||||
| BMI, kg/m2 | 24.17 (2.16) | 24.03 (1.97) | 0.244 | 0.622 | 24.5 (1.91) | 24.08 (1.64) | 10.739 | 0.001 |
| Education, n (%) | 3.936 | 0.268 | 1.691 | 0.639 | ||||
| 1 | 9 (3.2) | 1 (1.4) | 333 (29.8) | 70 (27.7) | ||||
| 2 | 187 (67.5) | 49 (68.1) | 428 (38.4) | 96 (37.9) | ||||
| 3 | 76 (27.4) | 18 (25) | 282 (25.3) | 73 (28.9) | ||||
| 4 | 5 (1.8) | 4 (5.6) | 73 (6.5) | 14 (5.5) | ||||
| Married, n (%) | 25 (9) | 7 (9.7) | 0 | 1 | 974 (87.3) | 210 (83) | 2.865 | 0.091 |
| Early Onset (n = 349) | Late Onset (n = 1369) | |||||||
|---|---|---|---|---|---|---|---|---|
| With ALM (n = 277) | Without ALM (n = 72) | F | p | With ALM (1116) | Without ALM (253) | F | p | |
| Suicide attempt, n (%) | 48 (17.3) | 7 (9.7) | 1.95 | 0.163 | 254 (22.8) | 37 (14.6) | 7.676 | 0.006 |
| Severe anxiety, n (%) | 26 (9.4) | 5 (6.9) | 0.173 | 0.677 | 154 (13.8) | 19 (7.5) | 6.831 | 0.009 |
| Exhibiting psychotic symptoms, n (%) | 34 (12.3) | 2 (2.8) | 4.592 | 0.032 | 124 (11.1) | 11 (4.3) | 9.866 | 0.002 |
| TSH, mIU/L | 4.77 (3.2, 6.8) | 3.76 (2.13, 4.51) | −4.793 | <0.001 | 5.82 (2.44) | 3.45 (1.87) | 339.477 | <0.001 |
| FT3, pmol/L | 4.97 (0.72) | 4.88 (0.75) | 0.995 | 0.319 | 4.91 (0.73) | 4.81 (0.7) | 3.676 | 0.055 |
| FT4, pmol/L | 16.65 (3) | 17.05 (3.05) | 0.996 | 0.319 | 16.73 (3.08) | 16.54 (3.26) | 0.741 | 0.389 |
| Fasting plasma glucose, mmol/L | 5.38 (0.7) | 5.21 (0.5) | 3.572 | 0.06 | 5.47 (0.63) | 5.18 (0.61) | 43.556 | <0.001 |
| LDL-C, mmol/L | 3.01 (0.93) | 2.3 (0.51) | 38.969 | <0.001 | 3.12 (0.87) | 2.52 (0.48) | 114.088 | <0.001 |
| HAMD | 31 (28, 32) | 28 (26, 29) | −6.557 | <0.001 | 31 (29, 32) | 28 (27, 30) | −11.271 | <0.001 |
| HAMA | 21 (18, 23) | 19 (17, 22) | −2.917 | 0.004 | 21 (19, 23) | 19 (17, 22) | −5.834 | <0.001 |
| PANSS | 7 (7, 9) | 7 (7, 7) | −3.775 | <0.001 | 7 (7, 9) | 7 (7, 7) | −6.595 | <0.001 |
| CGI | 6 (5, 7) | 5 (5,6) | −4.566 | <0.001 | 6 (5, 7) | 5 (5, 6) | −9.642 | <0.001 |
| A-TG, IU/mL | 19.12 (13.7, 31.29) | 18.92 (13.22, 24.48) | −1.044 | 0.297 | 22.21 (15.02, 59.06) | 19.89 (14.04, 33.65) | −2.248 | 0.025 |
| A-TPO, IU/mL | 17.13 (12.2, 33.06) | 16.01 (11.2, 28.0) | −1.453 | 0.146 | 17.79 (12.32, 36.93) | 17.48 (12.6, 28.81) | −0.867 | 0.386 |
| TC, mmol/L | 5.32 (1.14) | 4.13 (0.63) | −14.012 | <0.001 | 5.51 (1.06) | 4.34 (0.56) | 291.031 | <0.001 |
| HDL-C, mmol/L | 1.25 (0.98, 1.42) | 1.3 (1.18, 1.54) | −3.329 | 0.001 | 1.21 (0.95, 1.38) | 1.27 (1.18, 1.52) | −6.840 | <0.001 |
| TG, mmol/L | 2.34 (1.72, 2.92) | 1.26 (1.09, 1.50 | −10.193 | <0.001 | 2.25 (1.7, 2.87) | 1.26 (1.09, 1.47) | −19.775 | <0.001 |
| SBP, mmHg | 110.9 (9.8) | 106.1 (7.95) | 14.529 | <0.001 | 122.66 (9.73) | 118.67 (9.63) | 34.778 | <0.001 |
| DBP, mmHg | 72.5 (6.14) | 70.36 (5.37) | 7.291 | 0.007 | 77.26 (6.63) | 75.55 (6.02) | 14.222 | <0.001 |
| B | Wald | p | OR | 95% CI Lower | 95% CI Upper | |
|---|---|---|---|---|---|---|
| Suicide attempt | −0.391 | 3.001 | 0.083 | 0.676 | 0.434 | 1.053 |
| HAMD | 0.174 | 24.247 | <0.001 | 1.19 | 1.11 | 1.275 |
| TSH | 0.226 | 31.344 | <0.001 | 1.254 | 1.158 | 1.357 |
| CGI | 0.528 | 16.475 | <0.001 | 1.695 | 1.314 | 2.187 |
| Fasting plasma glucose | 0.265 | 3.648 | 0.056 | 1.303 | 0.993 | 1.711 |
| Severe anxiety | 0.799 | 6.953 | 0.008 | 2.223 | 1.228 | 4.024 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Huang, X.; Wu, A.; Zhang, X. Differences in the Prevalence and Clinical Correlates Between Early-Onset and Late-Onset Major Depressive Disorder Patients with Comorbid Abnormal Lipid Metabolism. Metabolites 2025, 15, 117. https://doi.org/10.3390/metabo15020117
Huang X, Wu A, Zhang X. Differences in the Prevalence and Clinical Correlates Between Early-Onset and Late-Onset Major Depressive Disorder Patients with Comorbid Abnormal Lipid Metabolism. Metabolites. 2025; 15(2):117. https://doi.org/10.3390/metabo15020117
Chicago/Turabian StyleHuang, Xiao, Anshi Wu, and Xiangyang Zhang. 2025. "Differences in the Prevalence and Clinical Correlates Between Early-Onset and Late-Onset Major Depressive Disorder Patients with Comorbid Abnormal Lipid Metabolism" Metabolites 15, no. 2: 117. https://doi.org/10.3390/metabo15020117
APA StyleHuang, X., Wu, A., & Zhang, X. (2025). Differences in the Prevalence and Clinical Correlates Between Early-Onset and Late-Onset Major Depressive Disorder Patients with Comorbid Abnormal Lipid Metabolism. Metabolites, 15(2), 117. https://doi.org/10.3390/metabo15020117







