Prediction of Prognosis in Patients with Trauma by Using Machine Learning
Abstract
1. Introduction
2. Methods
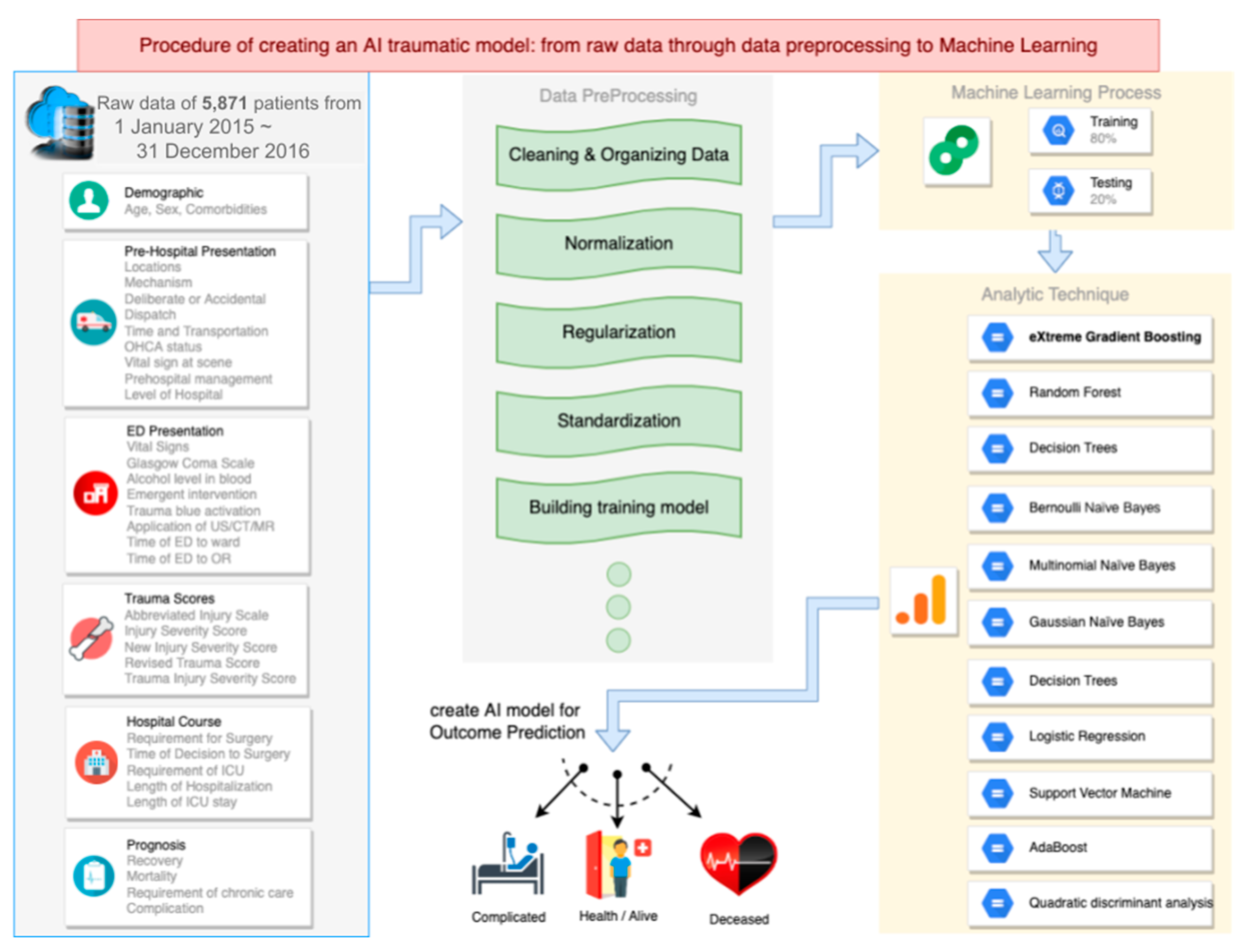
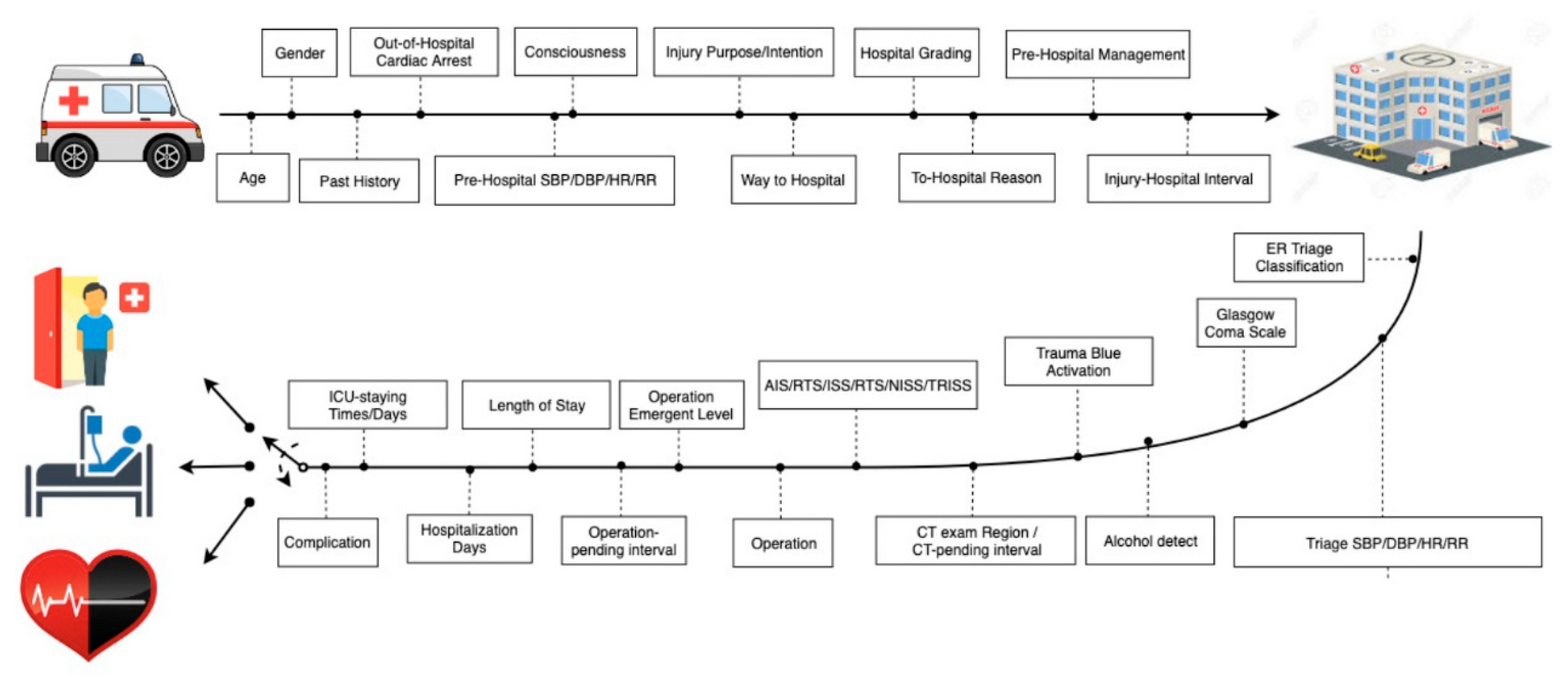
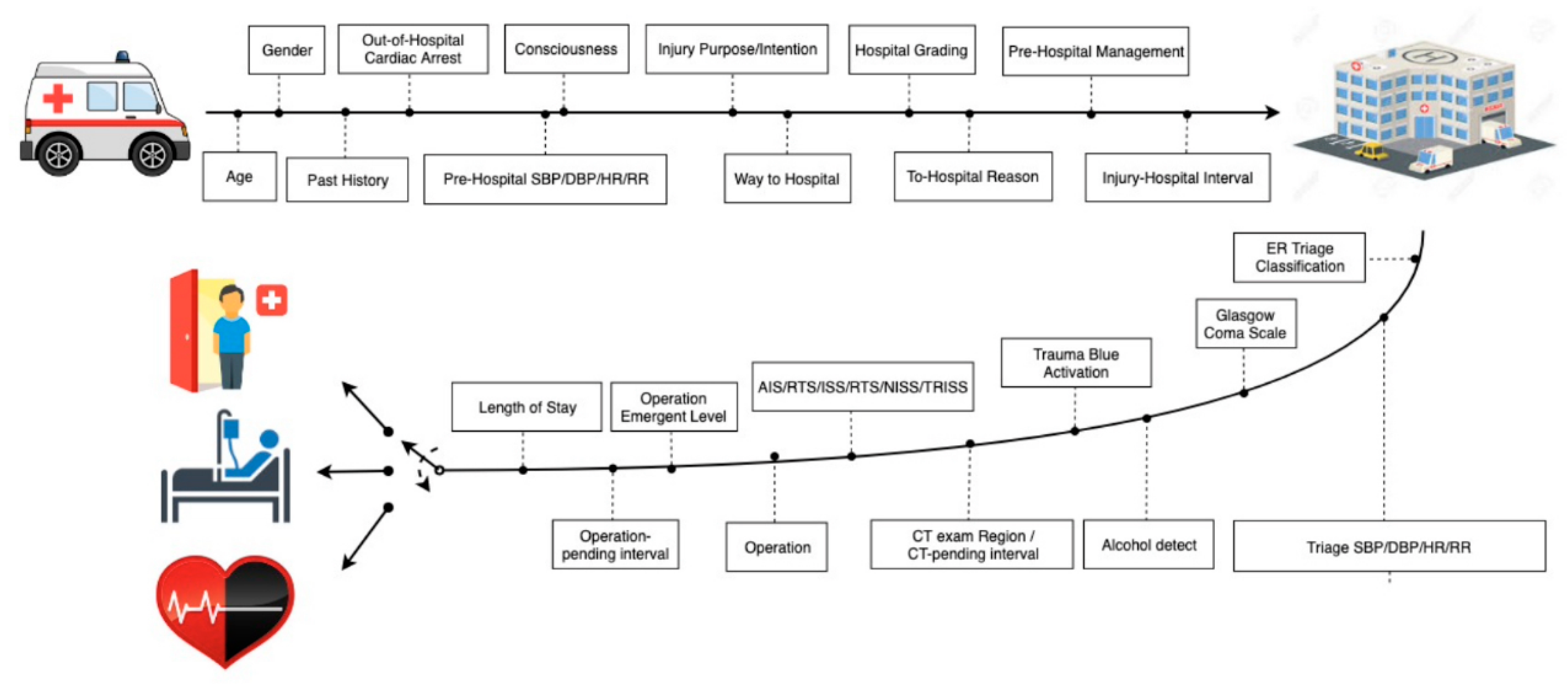
2.1. Dataset Management and ML Technique
2.2. ML Model Prototype
3. Results
3.1. Description of Dataset
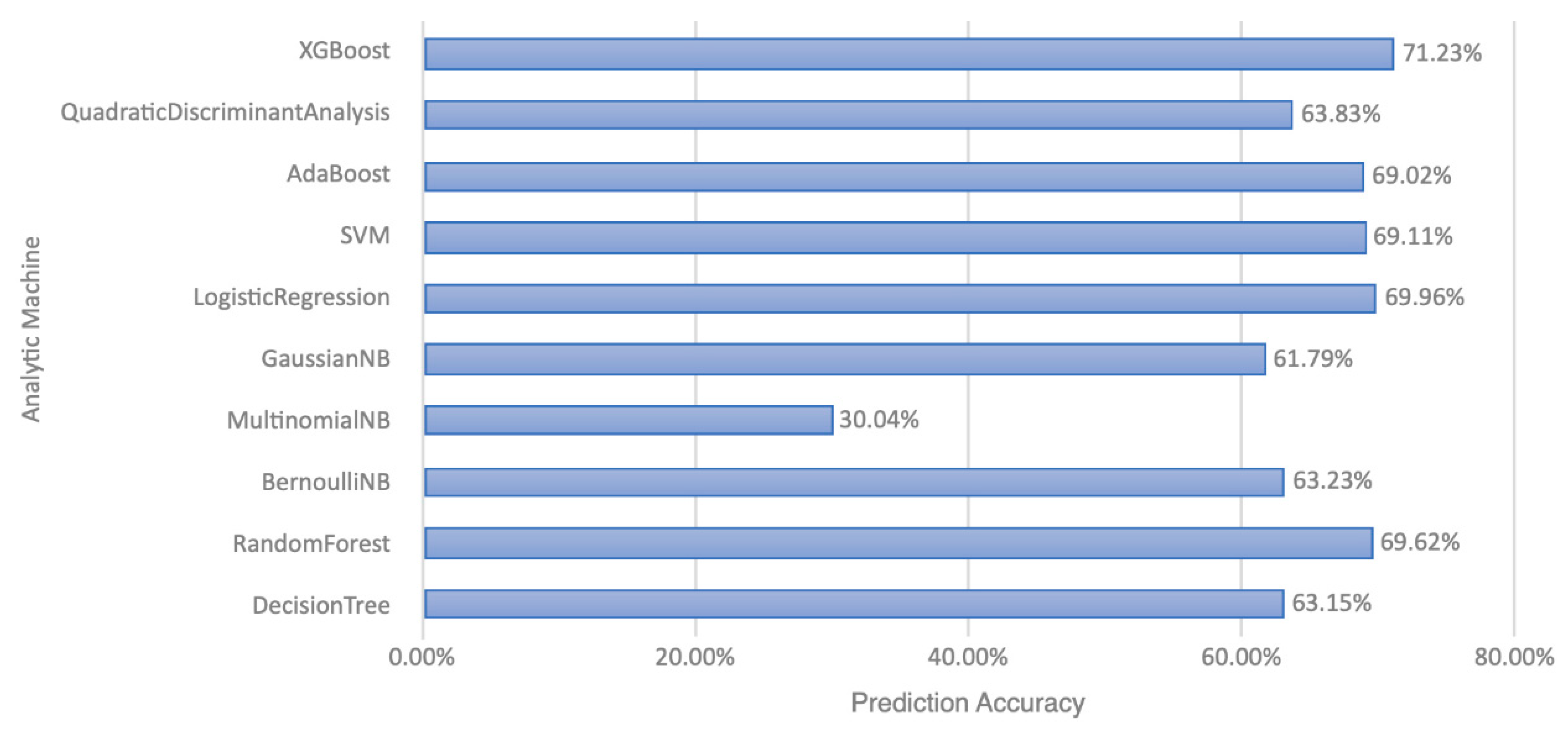
3.2. Models
3.3. Complete Model and High-Ranking Features
3.4. Short-Term Model and High-Ranking Features
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. XGBoost
References
- Ministry of Health and Welfare: Statistics and Publications: Statistics: Cause of Death Statistics 2019. Available online: https://www.mohw.gov.tw/lp-4964-2.html (accessed on 1 May 2020).
- Centers for Disease Control and Prevention: Minority Health and Health Equity: Leading Causes of Death. 2017. Available online: https://www.cdc.gov/healthequity/lcod/index.htm (accessed on 1 May 2020).
- World Health Organization. Global Health Observatory Data: 2016 Update; World Health Organization Press: Geneva, Switzerland, 2020; Available online: https://www.who.int/gho/mortality_burden_disease/causes_death/top_10/en/ (accessed on 1 May 2020).
- Kim, D.; You, S.; So, S.; Lee, J.; Yook, S.; Jang, D.P.; Kim, I.Y.; Park, E.; Cho, K.; Cha, W.C.; et al. A data-driven artificial intelligence model for remote triage in the prehospital environment. PLoS ONE 2018, 13, e0206006. [Google Scholar] [CrossRef] [PubMed]
- Muisyo, T.; Bernardo, E.O.; Camazine, M.; Colvin, R.; Thomas, K.A.; Borgman, M.A.; Spinella, P.C. Mortality prediction in pediatric trauma. J. Pediatric Surg. 2019, 54, 1613–1616. [Google Scholar] [CrossRef] [PubMed]
- Kuo, P.J.; Wu, S.C.; Chien, P.C.; Rau, C.S.; Chen, Y.C.; Hsieh, H.Y.; Hsieh, C.H. Derivation and validation of different machine-learning models in mortality prediction of trauma in motorcycle riders: A cross-sectional retrospective study in southern Taiwan. BMJ Open 2018, 8, e018252. [Google Scholar] [CrossRef] [PubMed]
- Harvin, J.A.; Green, C.E.; Pedroza, C.; Tyson, J.E.; Moore, L.J.; Wade, C.E.; Holcomb, J.B.; Kao, L.S. Using Machine Learning to Identify Change in Surgical Decision Making in Current Use of Damage Control Laparotomy. J. Am. Coll. Surg. 2019, 228, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Rau, C.S.; Kuo, P.J.; Chien, P.C.; Huang, C.Y.; Hsieh, H.Y.; Hsieh, C.H. Mortality prediction in patients with isolated moderate and severe traumatic brain injury using machine learning models. PLoS ONE. 2018, 13, e0207192. [Google Scholar] [CrossRef] [PubMed]
- Wahab, L.; Jiang, H.A. Comparative study on machine learning based algorithms for prediction of motorcycle crash severity. PLoS ONE 2019, 14, e0214966. [Google Scholar]
- Christie, S.A.; Conroy, A.S.; Callcut, R.A.; Hubbard, A.E.; Cohen, M.J. Dynamic multi-outcome prediction after injury: Applying adaptive machine learning for precision medicine in trauma. PLoS ONE 2019, 14, e0213836. [Google Scholar] [CrossRef] [PubMed]
- Cobb, A.N.; Daungjaiboon, W.; Brownlee, S.A.; Baldea, A.J.; Sanford, A.P.; Mosier, M.M.; Kuo, P.C. Seeing the forest beyond the trees: Predicting survival in burn patients with machine learning. Am. J. Surg. 2018, 215, 411–416. [Google Scholar] [CrossRef]
- Pedregosa, F.; Varoquaux, G.; Gramfort, A.; Michel, V.; Thirion, B.; Grisel, O.; Blondel, M.; Müller, A.; Nothman, J.; Louppe, G.; et al. Scikit-learn algorithm cheat-sheet: Machine learning in Python. JMLR 2011, 12, 2825–2830. [Google Scholar]
- Hasan, K.; Alam, A.; Das, D.; Hossain, E.; Hasan, M. Diabetes prediction using ensembling of different machine learning classifiers. IEEE Access 2020, 8, 76516–76531. [Google Scholar] [CrossRef]
- Parreco, J.; Hidalgo, A.; Parks, J.J.; Kozol, R.; Rattan, R. Using artificial intelligence to predict prolonged mechanical ventilation and tracheostomy placement. J. Surg. Res. 2018, 228, 179–187. [Google Scholar] [CrossRef] [PubMed]
- Sefrioui, I.; Amadini, R.; Mauro, J.; El Fallahi, A.; Gabbrielli, M. Survival prediction of trauma patients: A study on US National Trauma Data Bank. Eur. J Trauma Emerg. Surg. 2017, 43, 805–822. [Google Scholar] [CrossRef] [PubMed]
- Ng, C.J.; Yen, Z.S.; Tsai, J.C.H.; Chen, L.C.; Lin, S.J.; Sang, Y.Y.; Chen, J.C.; TTAS National Working Group. Validation of the Taiwan triage and acuity scale: A new computerised five-level triage system. Emerg Med J. 2011, 28, 1026–1031. [Google Scholar] [CrossRef] [PubMed]
- Fortuny, E.J.; Martens, D.; Provost, F. Predictive Modeling with Big Data: Is Bigger Really Better? Big Data 2014, 1, 215–226. [Google Scholar] [CrossRef] [PubMed]
- Hale, A.T.; Stonko, D.P.; Lim, J.; Guillamondegui, O.D.; Shannon, C.N.; Patel, M.B. Using an artificial neural network to predict traumatic brain injury. J. Neurosurg. Pediatrics 2018, 23, 219–226. [Google Scholar] [CrossRef] [PubMed]
- Liang, C.-C.; Liu, H.-T.; Rau, C.-S.; Hsu, S.-Y.; Hsieh, H.-Y.; Hsieh, C.-H. Motorcycle-related hospitalization of adolescents in a Level I trauma center in southern Taiwan: A cross-sectional study. BMC Pediatrics 2015, 15, 105. [Google Scholar] [CrossRef] [PubMed]
- Moore, S.E.; Decker, A.; Hubbard, A.; Callcut, R.A.; Fox, E.E.; Del Junco, D.J.; Holcomb, J.B.; Rahbar, M.H.; Wade, C.E.; Schreiber, M.A.; et al. Statistical Machines for Trauma Hospital Outcomes Research: Application to the PRospective, Observational, Multi-Center Major Trauma Transfusion (PROMMTT) Study. PLoS ONE 2015, 10, e0136438. [Google Scholar] [CrossRef] [PubMed]
- Christie, S.A.; Hubbard, A.E.; Callcut, R.A.; Hameed, M.; Dissak-Delon, F.N.; Mekolo, D.; Saidou, A.; Mefire, A.C.; Nsongoo, P.; Dicker, R.A. Machine learning without borders? An adaptable tool to optimize mortality prediction in diverse clinical settings. J Trauma Acute Care Surg. 2018, 85, 921–927. [Google Scholar] [CrossRef] [PubMed]
- Liu, N.T.; Salinas, J. Machine learning for predicting outcomes in trauma. Shock 2017, 48, 504–510. [Google Scholar] [CrossRef] [PubMed]
| Age | |
| Geriatric patients (>55 years) | 43.8% |
| Non-geriatric adults | 50.1% |
| Pediatric patients (<15 years) | 6.1% |
| Sex | |
| Male | 57.9% |
| Female | 42.1% |
| Transport type | |
| By Emergency Medical Services | 51% |
| By patient’s family or friends | 29.1% |
| Transfer from other hospitals | 19.9% |
| Triage | 2.4 ± 0.6 (mean ± SD) |
| I | 7.9% |
| II | 44.8% |
| III | 47.3% |
| Hospital stays | |
| <7 days | 66.7% |
| 7–30 days | 28.9% |
| >30 days | 4.4% |
| Requirement for intensive care | 17.3% |
| Requirement for surgery | 69.6% |
| Abbreviated Injury Scale ≥ 3 | |
| extremities | 24.4% |
| head | 21.4% |
| chest | 8.5% |
| abdomen | 3.2% |
| face | 0.6% |
| external | 0.6% |
| Major trauma (ISS >15) | 20.7% |
| Trauma scores | (mean ± SD) |
| Injury severity score (ISS) | 9.7 ± 8.8 |
| New injury severity score | 11.7 ± 10.5 |
| Revised trauma score | 7.6560 ± 0.7414 |
| Trauma injury severity score | 0.9543 ± 0.1267 |
| Complete Model | Short-Term Model | |
|---|---|---|
| Recovery | 86% | 89% |
| Chronic Care | 30% | 25% |
| Mortality | 67% | 41% |
| Complication | 80% | |
| High-ranking features | ||
| 1 | Trauma injury severity score | Trauma injury severity score |
| 2 | Abbreviated injury scale of head | Abbreviated injury scale of head |
| 3 | Dispatch of emergency medical service | Dispatch of emergency medical service |
| 4 | Triage | time from injury sites to the hospital |
| 5 | New injury severity score | New injury severity score |
| 6 | Time from injury sites to the hospital | Glasgow Coma Scale in ED |
| 7 | Requirement for intensive care | Triage |
| 8 | Length of hospital stay | transportation from injury sites to the hospital |
| 9 | Glasgow Coma Scale in ED | Gender |
| 10 | Prehospital managements by emergency medical technicians | Prehospital managements by emergency medical technicians |
| 11 | Revised trauma score | Level of transferred hospital |
| 12 | Prehospital consciousness | Time from surgical decision to surgery |
| 13 | Transportation from injury sites to the hospital | Deliberate or accidental injury |
| 14 | Comorbidity | Comorbidity |
| 15 | Deliberate or accidental injury | Age |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, K.-C.; Hsu, C.-C.; Lin, T.-C.; Chiang, H.-F.; Horng, G.-J.; Chen, K.-T. Prediction of Prognosis in Patients with Trauma by Using Machine Learning. Medicina 2022, 58, 1379. https://doi.org/10.3390/medicina58101379
Lee K-C, Hsu C-C, Lin T-C, Chiang H-F, Horng G-J, Chen K-T. Prediction of Prognosis in Patients with Trauma by Using Machine Learning. Medicina. 2022; 58(10):1379. https://doi.org/10.3390/medicina58101379
Chicago/Turabian StyleLee, Kuo-Chang, Chien-Chin Hsu, Tzu-Chieh Lin, Hsiu-Fen Chiang, Gwo-Jiun Horng, and Kuo-Tai Chen. 2022. "Prediction of Prognosis in Patients with Trauma by Using Machine Learning" Medicina 58, no. 10: 1379. https://doi.org/10.3390/medicina58101379
APA StyleLee, K.-C., Hsu, C.-C., Lin, T.-C., Chiang, H.-F., Horng, G.-J., & Chen, K.-T. (2022). Prediction of Prognosis in Patients with Trauma by Using Machine Learning. Medicina, 58(10), 1379. https://doi.org/10.3390/medicina58101379






