Failures of the Fontan System in Univentricular Hearts and Mortality Risk in Heart Transplantation: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
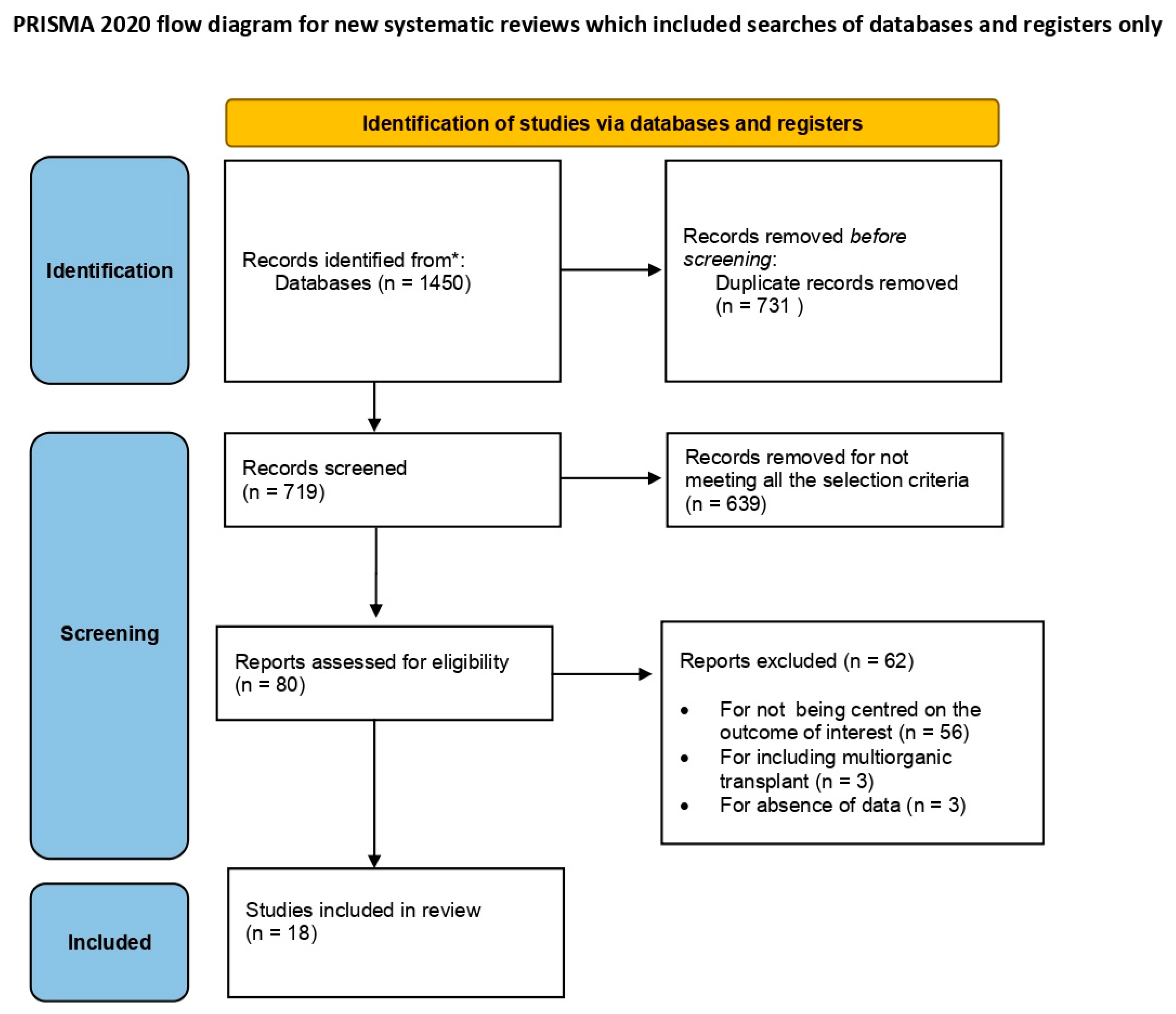
2. Materials and Methods
2.1. Search Strategy and Data Sources
2.2. Eligibility Criteria
2.3. Data Extraction
2.4. Variables
2.5. Bias Control
2.6. Statistical Analysis
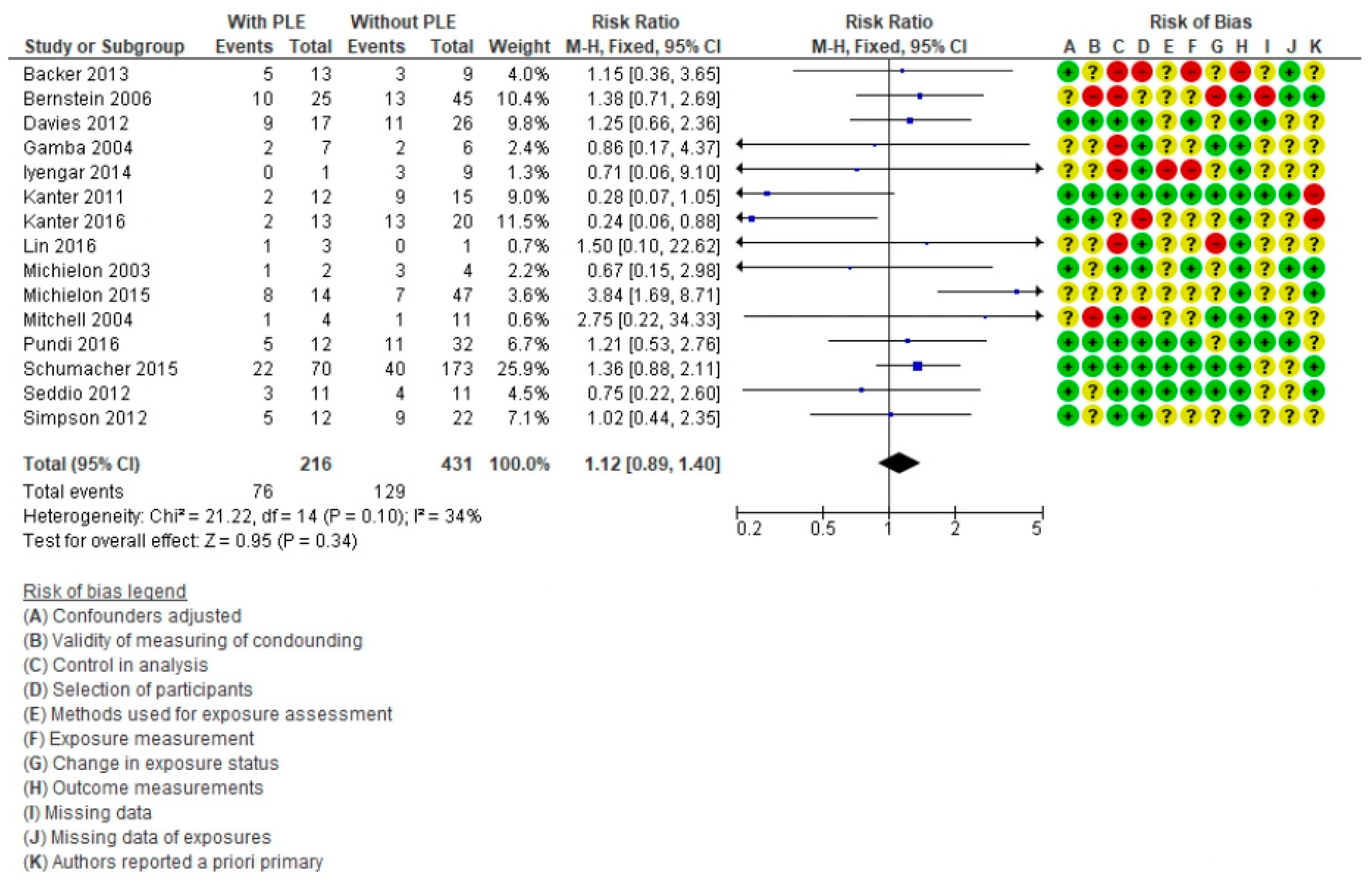
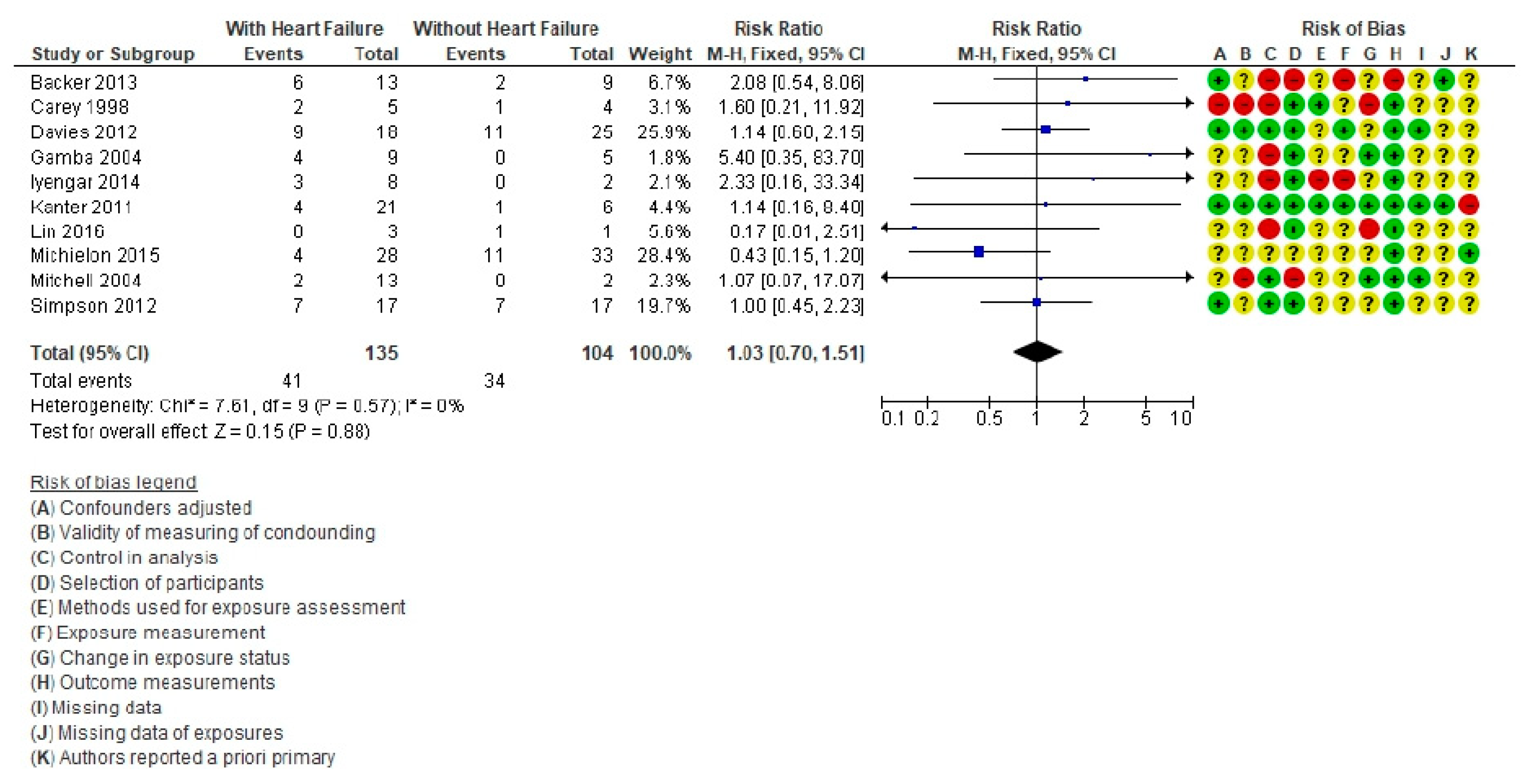
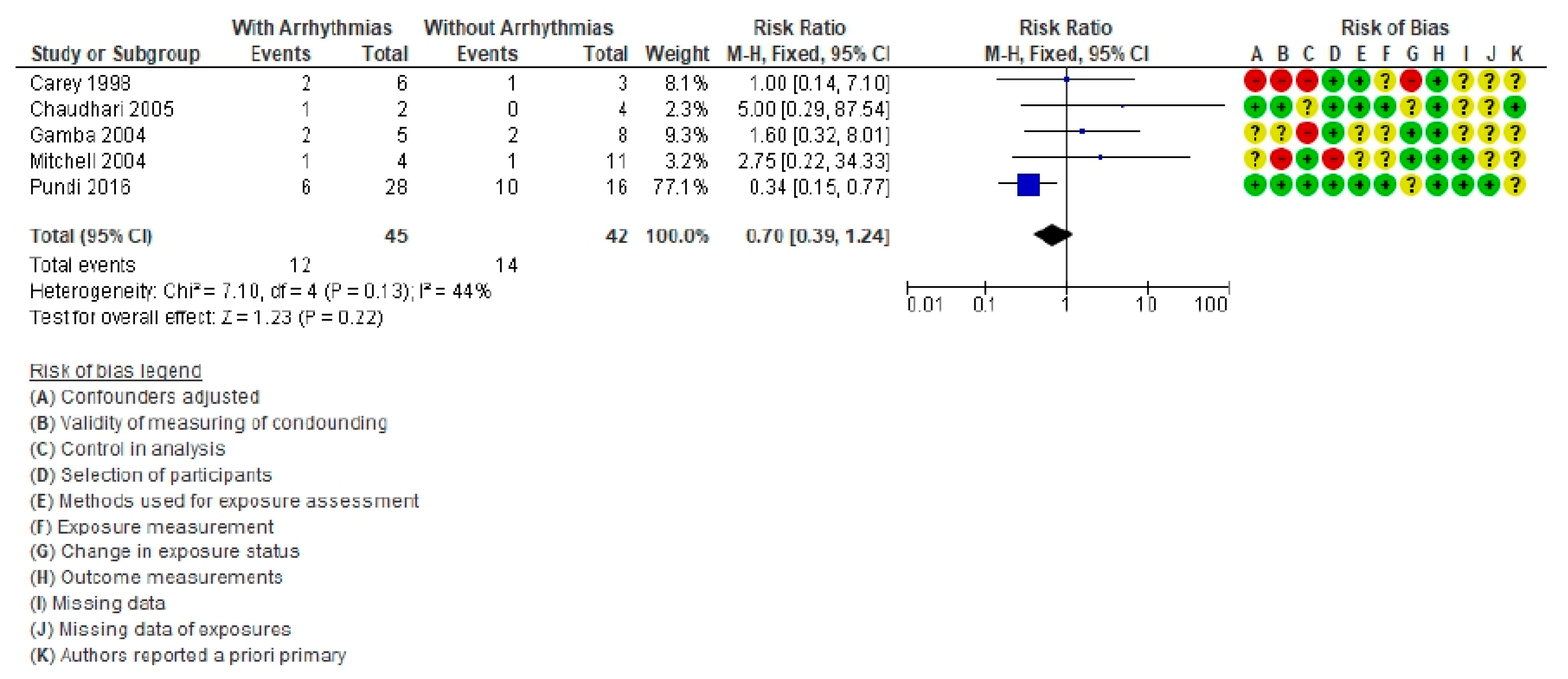
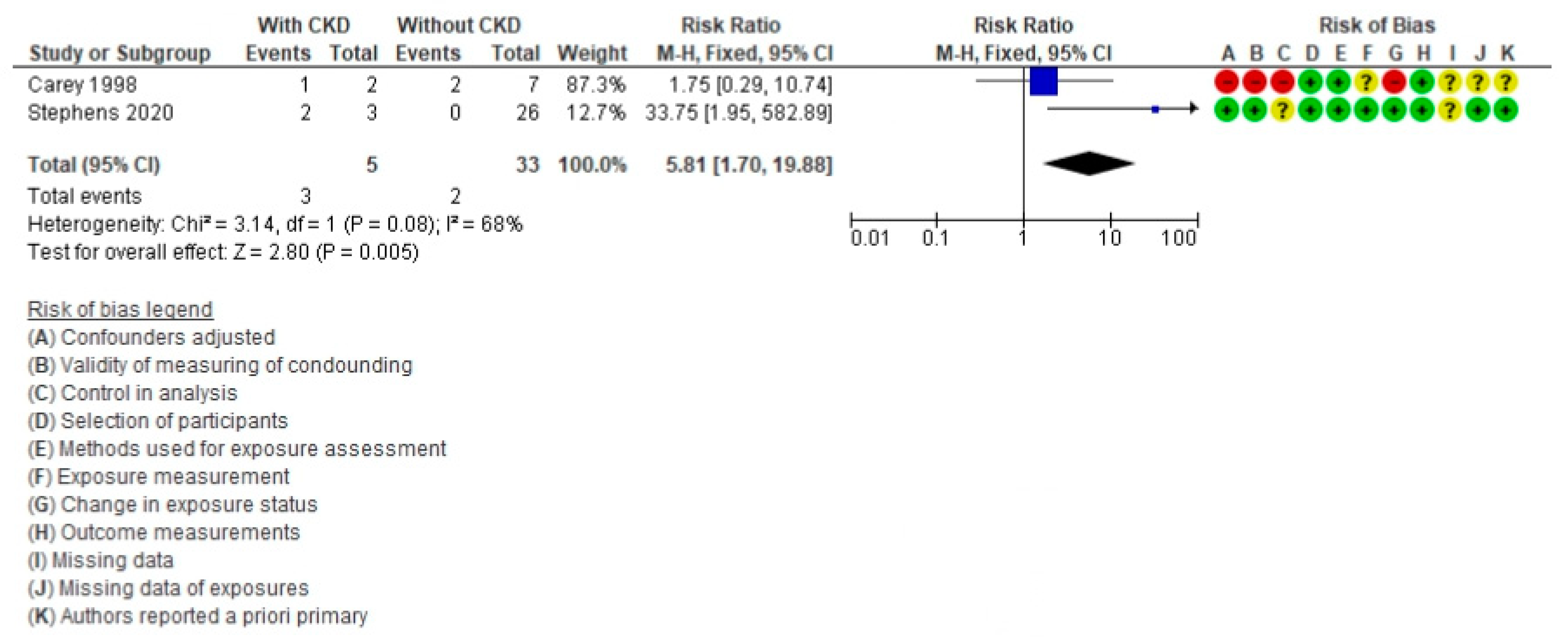
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hoffman, J.I.; Kaplan, S.; Liberthson, R.R. Prevalence of congenital heart disease. Am. Heart J. 2004, 147, 425–439. [Google Scholar] [CrossRef]
- Sairanen, H.I.; Nieminen, H.P.; Jokinen, E.V. Late results and quality of life after pediatric cardiac surgery in Finland: A population-based study of 6,461 patients with follow-up extending up to 45 years. Semin. Thorac. Cardiovasc. Surgery Pediatr. Card. Surg. Annu. 2005, 8, 168–172. [Google Scholar] [CrossRef] [PubMed]
- Jolley, M.; Colan, S.D.; Rhodes, J.; DiNardo, J. Fontan Physiology Revisited. Anesthesia Analg. 2015, 121, 172–182. [Google Scholar] [CrossRef] [PubMed]
- Gewillig, M.; Brown, S.C. The Fontan circulation after 45 years: Update in physiology. Heart 2016, 102, 1081–1086. [Google Scholar] [CrossRef]
- Pekkan, K.; Aka, I.B.; Tutsak, E.; Ermek, E.; Balim, H.; Lazoglu, I.; Turkoz, R. In vitro validation of a self-driving aortic-turbine venous-assist device for Fontan patients. J. Thorac. Cardiovasc. Surg. 2018, 156, 292–301.e7. [Google Scholar] [CrossRef] [Green Version]
- Backer, C.L.; Russell, H.M.; Pahl, E.; Mongé, M.C.; Gambetta, K.; Kindel, S.J.; Gossett, J.G.; Hardy, C.; Costello, J.M.; Deal, B.J. Heart Transplantation for the Failing Fontan. Ann. Thorac. Surg. 2013, 96, 1413–1419. [Google Scholar] [CrossRef]
- Schumacher, K.R.; Gossett, J.; Guleserian, K.; Naftel, D.C.; Pruitt, E.; Dodd, D.; Carboni, M.; Lamour, J.; Pophal, S.; Zamberlan, M.; et al. Fontan-associated protein-losing enteropathy and heart transplant: A Pediatric Heart Transplant Study analysis. J. Heart Lung Transplant. 2015, 34, 1169–1176. [Google Scholar] [CrossRef] [PubMed]
- Al Balushi, A.; Mackie, A.S. Protein-Losing Enteropathy Following Fontan Palliation. Can. J. Cardiol. 2019, 35, 1857–1860. [Google Scholar] [CrossRef] [PubMed]
- Simpson, K.E.; Cibulka, N.; Lee, C.K.; Huddleston, C.H.; Canter, C.E. Failed Fontan heart transplant candidates with preserved vs impaired ventricular ejection: 2 distinct patient populations. J. Heart Lung Transplant. 2012, 31, 545–547. [Google Scholar] [CrossRef]
- Khuong, J.N.; Wilson, T.G.; Grigg, L.E.; Bullock, A.; Celermajer, D.; Disney, P.; Wijesekera, V.A.; Hornung, T.; Zannino, D.; Iyengar, A.J.; et al. Fontan-associated nephropathy: Predictors and outcomes. Int. J. Cardiol. 2020, 306, 73–77. [Google Scholar] [CrossRef]
- Pundi, K.N.; Pundi, K.; Driscoll, D.J.; Dearani, J.A.; Li, Z.; Dahl, S.H.; Mora, B.N.; O’Leary, P.W.; Daly, R.C.; Cetta, F.; et al. Heart transplantation after Fontan: Results from a surgical Fontan cohort. Pediatr. Transplant. 2016, 20, 1087–1092. [Google Scholar] [CrossRef]
- Davies, R.R.; Sorabella, R.A.; Yang, J.; Mosca, R.S.; Chen, J.M.; Quaegebeur, J.M. Outcomes after transplantation for “failed” Fontan: A single-institution experience. J. Thorac. Cardiovasc. Surg. 2012, 143, 1183–1192.e4. [Google Scholar] [CrossRef] [Green Version]
- Hernandez, G.A.; Lemor, A.; Clark, D.; Blumer, V.; Burstein, D.; Byrne, R.; Fowler, R.; Frischhertz, B.; Rn, E.S.; Schlendorf, K.; et al. Heart transplantation and in-hospital outcomes in adult congenital heart disease patients with Fontan: A decade nationwide analysis from 2004 to 2014 . J. Card. Surg. 2019, 35, 603–608. [Google Scholar] [CrossRef]
- Jeon, B.B.; Park, C.S.; Yun, T.-J. Heart Transplantation in Patients with Superior Vena Cava to Pulmonary Artery Anastomosis: A Single-Institution Experience. Korean J. Thorac. Cardiovasc. Surg. 2018, 51, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Michielon, G.; Van Melle, J.P.; Wolff, D.; Di Carlo, D.; Jacobs, J.P.; Mattila, I.P.; Berggren, H.; Lindberg, H.; Padalino, M.; Meyns, B.; et al. Favourable mid-term outcome after heart transplantation for late Fontan failure. Eur. J. Cardio-Thorac. Surg. 2015, 47, 665–671. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tabarsi, N.; Guan, M.; Simmonds, J.; Toma, M.; Kiess, M.; Tsang, V.; Ruygrok, P.; Konstantinov, I.; Shi, W.; Grewal, J. Meta-Analysis of the Effectiveness of Heart Transplantation in Patients with a Failing Fontan. Am. J. Cardiol. 2017, 119, 1269–1274. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, 71. [Google Scholar] [CrossRef] [PubMed]
- Doumouras, B.S.; Alba, A.; Foroutan, F.; Burchill, L.J.; Dipchand, A.I.; Ross, H.J. Outcomes in adult congenital heart disease patients undergoing heart transplantation: A systematic review and meta-analysis. J. Heart Lung Transplant. 2016, 35, 1337–1347. [Google Scholar] [CrossRef] [PubMed]
- Matsuda, H.; Ichikawa, H.; Ueno, T.; Sawa, Y. Heart transplantation for adults with congenital heart disease: Current status and future prospects. Gen. Thorac. Cardiovasc. Surg. 2017, 65, 309–320. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLoS Med. 2007, 4, e296. [Google Scholar] [CrossRef] [Green Version]
- Assenza, G.E.; A Graham, D.; Landzberg, M.J.; Valente, A.M.; Singh, M.N.; Bashir, A.; Fernandes, S.; Mortele, K.J.; Ukomadu, C.; Volpe, M.; et al. MELD-XI score and cardiac mortality or transplantation in patients after Fontan surgery. Heart 2013, 99, 491–496. [Google Scholar] [CrossRef]
- Berg, C.; Bauer, B.S.; Hageman, A.; Aboulhosn, J.A.; Reardon, L.C. Mortality Risk Stratification in Fontan Patients Who Underwent Heart Transplantation. Am. J. Cardiol. 2017, 119, 1675–1679. [Google Scholar] [CrossRef] [PubMed]
- Chrisant, M.; Naftel, D.; Drummond-Webb, J.; Chinnock, R.; Canter, C.; Boucek, M.; Boucek, R.; Hallowell, S.; Kirklin, J.; Morrow, W. Fate of Infants with Hypoplastic Left Heart Syndrome Listed for Cardiac Transplantation: A Multicenter Study. J. Heart Lung Transplant. 2005, 24, 576–582. [Google Scholar] [CrossRef]
- Hofferberth, S.C.; Singh, T.P.; Bastardi, H.; Blume, E.D.; Fynn-Thompson, F. Liver abnormalities and post-transplant survival in pediatric Fontan patients. Pediatr. Transplant. 2017, 21, e13061. [Google Scholar] [CrossRef]
- Jayakumar, K.A.; Addonizio, L.J.; Kichuk-Chrisant, M.R.; Galantowicz, M.E.; Lamour, J.M.; Quaegebeur, J.M.; Hsu, D. Cardiac transplantation after the Fontan or Glenn procedure. J. Am. Coll. Cardiol. 2004, 44, 2065–2072. [Google Scholar] [CrossRef]
- Kaza, A.K.; Kaza, E.; Bullock, E.; Reyna, S.; Yetman, A.; Everitt, M.D. Pulmonary vascular remodelling after heart transplantation in patients with cavopulmonary connection†. Eur. J. Cardio-Thoracic Surg. 2015, 47, 505–510. [Google Scholar] [CrossRef]
- Marrone, C.; Ferrero, P.; Uricchio, N.; Sebastiani, R.; Vittori, C.; Ciuffreda, M.; Terzi, A.; Galletti, L. The unnatural history of failing univentricular hearts: Outcomes up to 25 years after heart transplantation. Interact. Cardiovasc. Thorac. Surg. 2017, 25, 892–897. [Google Scholar] [CrossRef] [Green Version]
- Mavroudis, C.; Deal, B.J.; Backer, C.L.; Stewart, R.D.; Franklin, W.H.; Tsao, S.; Ward, K.M.; DeFreitas, R.A. 111 Fontan Conversions with Arrhythmia Surgery: Surgical Lessons and Outcomes. Ann. Thorac. Surg. 2007, 84, 1457–1466. [Google Scholar] [CrossRef] [PubMed]
- Menachem, J.N.; Golbus, J.R.; Molina, M.; Mazurek, J.A.; Hornsby, N.; Atluri, P.; Fuller, S.; Birati, E.Y.; Kim, Y.Y.; Goldberg, L.R.; et al. Successful cardiac transplantation outcomes in patients with adult congenital heart disease. Heart 2017, 103, 1449–1454. [Google Scholar] [CrossRef] [PubMed]
- Michielon, G.; Parisi, F.; Squitieri, C.; Carotti, A.; Gagliardi, G.; Pasquini, L.; Di Donato, R.M. Orthotopic Heart Transplantation for Congenital Heart Disease: An Alternative for High-Risk Fontan Candidates? Circualtion 2003, 108, II-140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mital, S.; Addonizio, L.J.; Lamour, J.M.; Hsu, D.T. Outcome of children with end-stage congenital heart disease waiting for cardiac transplantation. J. Heart Lung Transplant. 2003, 22, 147–153. [Google Scholar] [CrossRef]
- Murtuza, B.; Dedieu, N.; Vazquez, A.; Fenton, M.; Burch, M.; Hsia, T.-Y.; Tsang, V.T.; Kostolny, M. Results of orthotopic heart transplantation for failed palliation of hypoplastic left heart†. Eur. J. Cardio-Thorac. Surg. 2012, 43, 597–603. [Google Scholar] [CrossRef] [Green Version]
- Murtuza, B.; Hermuzi, A.; Crossland, D.S.; Parry, G.; Lord, S.; Hudson, M.; Chaudhari, M.P.; Haynes, S.; O’Sullivan, J.J.; Hasan, A. Impact of mode of failure and end-organ dysfunction on the survival of adult Fontan patients undergoing cardiac transplantation. Eur. J. Cardio-Thorac. Surg. 2017, 51, 135–141. [Google Scholar] [CrossRef] [PubMed]
- Paniagua Martin, M.J.; Almenar, L.; Brossa, V.; Crespo-Leiro, M.G.; Segovia, J.; Palomo, J.; Delgado, J.; Gonzalez-Vilchez, F.; Manito, N.; Lage, E.; et al. Transplantation for complex congenital heart disease in adults: A subanalysis of the Spanish Heart Transplant Registry. Clin Transplant. 2012, 26, 755–763. [Google Scholar] [CrossRef]
- Petko, M.; Myung, R.J.; Wernovsky, G.; Cohen, M.I.; Rychik, J.; Nicolson, S.C.; Gaynor, J.W.; Spray, T.L. Surgical reinterventions following the Fontan procedure. Eur. J. Cardio-Thorac. Surg. 2003, 24, 255–259. [Google Scholar] [CrossRef] [Green Version]
- Rungan, S.; Finucane, K.; Gentles, T.; Gibbs, H.C.; Hu, R.; Ruygrok, P.N. Heart transplantation in pediatric and congenital heart disease: A single-center experience. World J. Pediatr Congenit Heart Surg. 2014, 5, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Simpson, K.E.; Esmaeeli, A.; Khanna, G.; White, F.; Turnmelle, Y.; Eghtesady, P.; Boston, U.; Canter, C.E. Liver cirrhosis in Fontan patients does not affect 1-year post-heart transplant mortality or markers of liver function. J. Heart Lung Transplant. 2014, 33, 170–177. [Google Scholar] [CrossRef] [Green Version]
- Simpson, K.E.; Pruitt, E.; Kirklin, J.K.; Naftel, D.C.; Singh, R.; Edens, R.E.; Barnes, A.P.; Canter, C.E. Fontan Patient Survival After Pediatric Heart Transplantation Has Improved in the Current Era. Ann. Thorac. Surg. 2017, 103, 1315–1320. [Google Scholar] [CrossRef] [Green Version]
- Shi, W.Y.; Yong, M.; McGiffin, D.C.; Jain, P.; Ruygrok, P.N.; Marasco, S.F.; Finucane, K.; Keogh, A.; D’Udekem, Y.; Weintraub, R.G.; et al. Heart transplantation in Fontan patients across Australia and New Zealand. Heart 2016, 102, 1120–1126. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Melle, J.P.; Wolff, D.; Horer, J.; Belli, E.; Meyns, B.; Padalino, M.; Lindberg, H.; Jacobs, J.P.; Mattila, I.P.; Berggren, H.; et al. Surgical options after Fontan failure. Heart 2016, 102, 1127–1133. [Google Scholar] [CrossRef] [Green Version]
- Griffiths, E.R.; Kaza, A.; von Ballmoos, M.C.W.; Loyola, H.; Valente, A.M.; Blume, E.D.; del Nido, P. Evaluating Failing Fontans for Heart Transplantation: Predictors of Death. Ann. Thorac. Surg. 2009, 88, 558–564. [Google Scholar] [CrossRef] [Green Version]
- Carrillo, S.A.; Texter, K.M.; Phelps, C.; Tan, Y.; McConnell, P.I.; Galantowicz, M. Tricuspid Valve and Right Ventricular Function Throughout the Hybrid Palliation Strategy for Hypoplastic Left Heart Syndrome and Variants. World J. Pediatr. Congenit. Heart Surg. 2021, 12, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Marathe, S.P.; Zannino, D.; Cao, J.Y.; du Plessis, K.; Marathe, S.S.; Ayer, J.; Celermajer, D.S.; Gentles, T.L.; Sholler, G.F.; Justo, R.N.; et al. Heterotaxy Is Not a Risk Factor for Adverse Long-Term Outcomes After Fontan Completion. Ann. Thorac. Surg. 2020, 110, 646–653. [Google Scholar] [CrossRef] [PubMed]
- Schmiegelow, M.D.; Idorn, L.; Gislason, G.; Hlatky, M.; Køber, L.; Torp-Pedersen, C.; Sondergaard, L. Cardiovascular complications in patients with total cavopulmonary connection: A nationwide cohort study. Int. J. Cardiol. 2019, 305, 120–126. [Google Scholar] [CrossRef] [PubMed]
- Kovach, J.R.; Naftel, D.C.; Pearce, F.B.; Tresler, M.A.; Edens, R.E.; Shuhaiber, J.H.; Blume, E.D.; Fynn-Thompson, F.; Kirklin, J.K.; Zangwill, S.D. Comparison of risk factors and outcomes for pediatric patients listed for heart transplantation after bidirectional Glenn and after Fontan: An analysis from the Pediatric Heart Transplant Study. J. Heart Lung Transplant. 2012, 31, 133–139. [Google Scholar] [CrossRef]
- Alsoufi, B.; McCracken, C.; Kanter, K.; Shashidharan, S.; Border, W.; Kogon, B. Outcomes of Multistage Palliation of Infants with Single Ventricle and Atrioventricular Septal Defect. World J. Pediatr. Congenit. Heart Surg. 2020, 11, 39–48. [Google Scholar] [CrossRef]
- Cotter, T.G.; Wang, J.; Peeraphatdit, T.; Sandıkçı, B.; Ayoub, F.; Kim, G.; Te, H.; Jeevanandam, V.; Sabato, D.; Charlton, M. Simultaneous Heart–Liver Transplantation for Congenital Heart Disease in the United States: Rapidly Increasing with Acceptable Outcomes. Hepatology 2021, 73, 1464–1477. [Google Scholar] [CrossRef]
- Daley, M.; Du Plessis, K.; Zannino, D.; Hornung, T.; Disney, P.; Cordina, R.; Grigg, L.; Radford, D.J.; Bullock, A.; D’Udekem, Y. Reintervention and survival in 1428 patients in the Australian and New Zealand Fontan Registry. Heart 2019, 106, 751–757. [Google Scholar] [CrossRef]
- Kim, M.H.; Nguyen, A.; Lo, M.; Kumar, S.R.; Bucuvalas, J.; Glynn, E.F.; Hoffman, M.A.; Fischer, R.; Emamaullee, J. Big Data in Transplantation Practice—the Devil Is in the Detail—Fontan-associated Liver Disease. Transplantation 2021, 105, 18–22. [Google Scholar] [CrossRef]
- Karikari, Y.; Abdulkarim, M.; Li, Y.; Loomba, R.S.; Zimmerman, F.; Husayni, T. The Progress and Significance of QRS Duration by Electrocardiography in Hypoplastic Left Heart Syndrome. Pediatr. Cardiol. 2019, 41, 141–148. [Google Scholar] [CrossRef]
- Moon, J.; Shen, L.; Likosky, D.S.; Sood, V.; Hobbs, R.D.; Sassalos, P.; Romano, J.C.; Ohye, R.G.; Bove, E.L.; Si, M.-S. Relationship of Ventricular Morphology and Atrioventricular Valve Function to Long-Term Outcomes Following Fontan Procedures. J. Am. Coll. Cardiol. 2020, 76, 419–431. [Google Scholar] [CrossRef]
- Stackhouse, K.A.; McCrindle, B.W.; Blackstone, E.H.; Rajeswaran, J.; Kirklin, J.K.; Bailey, L.L.; Jacobs, M.L.; Tchervenkov, C.I.; Jacobs, J.P.; Pettersson, G.B. Surgical palliation or primary transplantation for aortic valve atresia. J. Thorac. Cardiovasc. Surg. 2020, 159, 1451–1461.e7. [Google Scholar] [CrossRef] [Green Version]
- Viegas, M.; Diaz-Castrillon, C.; Castro-Medina, M.; Silva, L.D.F.D.; Morell, V.O. Bidirectional Glenn Procedure in Patients Less Than 3 Months of Age: A 14-Year Experience. Ann. Thorac. Surg. 2020, 110, 622–629. [Google Scholar] [CrossRef] [PubMed]
- Serfas, J.D.; Thibault, D.; Andersen, N.D.; Chiswell, K.; Jacobs, J.P.; Jacobs, M.L.; Krasuski, R.A.; Lodge, A.J.; Turek, J.W.; Hill, K.D. The Evolving Surgical Burden of Fontan Failure: An Analysis of the Society of Thoracic Surgeons Congenital Heart Surgery Database. Ann. Thorac. Surg. 2021, 112, 179–187. [Google Scholar] [CrossRef]
- Schleiger, A.; Ovroutski, S.; Peters, B.; Schubert, S.; Photiadis, J.; Berger, F.; Kramer, P. Treatment strategies for protein-losing enteropathy in Fontan-palliated patients. Cardiol. Young 2020, 30, 698–709. [Google Scholar] [CrossRef] [PubMed]
- Chaudhari, M.; Sturman, J.; O’Sullivan, J.; Smith, J.; Wrightson, N.; Parry, G.; Bolton, D.; Haynes, S.; Hamilton, L.; Hasan, A. Rescue cardiac transplantation for early failure of the Fontan-type circulation in children. J. Thorac. Cardiovasc. Surg. 2005, 129, 416–422. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gamba, A.; Merlo, M.; Fiocchi, R.; Terzi, A.; Mammana, C.; Sebastiani, R.; Ferrazzi, P. Heart transplantation in patients with previous Fontan operations. J. Thorac. Cardiovasc. Surg. 2004, 127, 555–562. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mitchell, M.B.; Campbell, D.N.; Ivy, D.; Boucek, M.M.; Sondheimer, H.M.; Pietra, B.; Das, B.B.; Coll, J.R. Evidence of pulmonary vascular disease after heart transplantation for Fontan circulation failure. J. Thorac. Cardiovasc. Surg. 2004, 128, 693–702. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kanter, K.R. Heart Transplantation in Children after a Fontan Procedure: Better than People Think. Semin. Thorac. Cardiovasc. Surgery: Pediatr. Card. Surg. Annu. 2016, 19, 44–49. [Google Scholar] [CrossRef] [PubMed]
- Lin, S.-N.; Huang, S.-C.; Chen, Y.-S.; Chih, N.-H.; Wang, C.-H.; Chou, N.-K.; Yu, H.-Y.; Wu, I.-H.; Shun, C.-T.; Wang, S.-S. Case Series: Heart Transplantation after Fontan Operation—Single-Center Experience. Transplant. Proc. 2016, 48, 959–964. [Google Scholar] [CrossRef]
- Zhang, Y.; Alonso-Coello, P.; Guyatt, G.H.; Yepes-Nuñez, J.J.; Akl, E.A.; Hazlewood, G.; Pardo-Hernandez, H.; Etxeandia-Ikobaltzeta, I.; Qaseem, A.; Williams, J.W.; et al. GRADE Guidelines: Assessing the certainty of evidence in the importance of outcomes or values and preferences—Risk of bias and indirectness. J. Clin. Epidemiol. 2019, 111, 94–104. [Google Scholar] [CrossRef]
- Review Manager (RevMan), 5.4 ed.; The Cochrane Collaboration; 2020; Available online: revman.cochrane.org (accessed on 2 October 2021).
- Stephens, E.H.; Tannous, P.; Mongé, M.C.; Eltayeb, O.; Devlin, P.J.; Backer, C.L.; Forbess, J.M.; Pahl, E. Normalization of hemodynamics is delayed in patients with a single ventricle after pediatric heart transplantation. J. Thorac. Cardiovasc. Surg. 2020, 159, 1986–1996. [Google Scholar] [CrossRef] [PubMed]
- Alsoufi, B.; Deshpande, S.; McCracken, C.; Kogon, B.; Vincent, R.; Mahle, W.; Kanter, K. Results of heart transplantation following failed staged palliation of hypoplastic left heart syndrome and related single ventricle anomalies. Eur. J. Cardio-Thoracic Surg. 2015, 48, 792–799. [Google Scholar] [CrossRef]
- Alsoufi, B.; Mahle, W.T.; Manlhiot, C.; Deshpande, S.; Kogon, B.; McCrindle, B.W.; Kanter, K. Outcomes of heart transplantation in children with hypoplastic left heart syndrome previously palliated with the Norwood procedure. J. Thorac. Cardiovasc. Surg. 2016, 151, 167–175.e2. [Google Scholar] [CrossRef] [Green Version]
- Alsoufi, B.; Deshpande, S.; McCracken, C.; Kogon, B.; Vincent, R.; Mahle, W.; Kanter, K. Outcomes and risk factors for heart transplantation in children with congenital heart disease. J. Thorac. Cardiovasc. Surg. 2015, 150, 1455–1462.e3. [Google Scholar] [CrossRef]
- Bando, K.; Turrentine, M.W.; Sun, K.; Sharp, T.G.; Caldwell, R.L.; Darragh, R.K.; Ensing, G.J.; Cordes, T.M.; Flaspohler, T.; Brown, J.W. Surgical management of hypoplastic left heart syndrome. Ann. Thorac. Surg. 1996, 62, 70–77. [Google Scholar] [CrossRef]
- Bernstein, D.; Naftel, D.; Chin, C.; Addonizio, L.; Gamberg, P.; Hsu, D.; Blume, E.; Canter, C.; Morrow, R.; Kirklin, J. Outcome of listing for cardiac transplantation (Tx) for failed fontan: A follow-up multi-institutional study. J. Heart Lung Transplant. 2004, 23, S162. [Google Scholar] [CrossRef]
- Carey, J.A.; Hamilton, J.R.; Hilton, C.J.; Dark, J.H.; Forty, J.; Parry, G.; Hasan, A. Orthotopic cardiac transplantation for the failing Fontan circulation. Eur. J. Cardio-Thorac. Surg. 1998, 14, 7–13; discussion 4. [Google Scholar] [CrossRef] [Green Version]
- D’Souza, B.A.; Fuller, S.; Gleason, L.P.; Hornsby, N.; Wald, J.; Krok, K.; Shaked, A.; Goldberg, L.R.; Pochettino, A.; Olthoff, K.M.; et al. Single-center outcomes of combined heart and liver transplantation in the failing Fontan. Clin. Transplant. 2017, 31, e12892. [Google Scholar] [CrossRef]
- Eilers, B.; Albers, E.; Law, Y.; McMullan, D.M.; Shaw, D.; Kemna, M. Posterior reversible encephalopathy syndrome after pediatric heart transplantation: Increased risk for children with preexisting Glenn/Fontan physiology. Pediatr. Transplant. 2016, 20, 552–558. [Google Scholar] [CrossRef] [PubMed]
- Fullerton, D.A.; Campbell, D.N.; Jones, S.D.; Jaggers, J.; Brown, J.M.; Wollmering, M.M.; Grover, F.L.; Mashburn, C.; Luna, M.; Sondheimer, H.M.; et al. Heart transplantation in children and young adults: Early and intermediate-term results. Ann. Thorac. Surg. 1995, 59, 804–812. [Google Scholar] [CrossRef]
- Givertz, M.M. Assessing the liver to predict outcomes in heart transplantation. J. Heart Lung Transplant. 2015, 34, 869–872. [Google Scholar] [CrossRef]
- Iyengar, A.J.; Sharma, V.; Weintraub, R.G.; Shipp, A.; Brizard, C.P.; D’Udekem, Y.; Konstantinov, I.E. Surgical strategies to facilitate heart transplantation in children after failed univentricular palliations: The role of advanced intraoperative surgical preparation. Eur. J. Cardio-Thorac. Surg. 2014, 46, 480–485. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Izquierdo, M.; Almenar, L.; Martínez-Dolz, L.; Moro, J.; Agüero, J.; Sanchez-Lázaro, I.; Cano, O.; Ortiz, V.; Sánchez, R.; Salvador, A. Mortality After Heart Transplantation in Adults with Congenital Heart Disease: A Single-Center Experience. Transplant. Proc. 2007, 39, 2357–2359. [Google Scholar] [CrossRef]
- Jacobs, J.P.; Quintessenza, J.A.; Chai, P.J.; Lindberg, H.L.; Asante-Korang, A.; McCormack, J.; Dadlani, G.; Boucek, R.J. Rescue cardiac transplantation for failing staged palliation in patients with hypoplastic left heart syndrome. Cardiol. Young 2006, 16, 556–562. [Google Scholar] [CrossRef]
- Kanter, K.R.; Mahle, W.T.; Vincent, R.N.; Berg, A.M.; Kogon, B.E.; Kirshbom, P.M. Heart Transplantation in Children with a Fontan Procedure. Ann. Thorac. Surg. 2011, 91, 823–830. [Google Scholar] [CrossRef]
- Kanter, K.R.; Vincent, R.N.; E Miller, B.; McFadden, C. Heart transplantation in children who have undergone previous heart surgery: Is it safe? J. Heart Lung Transplant. 1993, 12, S218–S224. [Google Scholar] [PubMed]
- Lamour, J.M.; Kanter, K.R.; Naftel, D.C.; Chrisant, M.R.; Morrow, W.R.; Clemson, B.S.; Kirklin, J.K. The Effect of Age, Diagnosis, and Previous Surgery in Children and Adults Undergoing Heart Transplantation for Congenital Heart Disease. J. Am. Coll. Cardiol. 2009, 54, 160–165. [Google Scholar] [CrossRef] [Green Version]
- Lewis, M.; Ginns, J.; Schulze, C.; Lippel, M.; Chai, P.; Bacha, E.; Mancini, D.; Rosenbaum, M.; Farr, M. Outcomes of Adult Patients With Congenital Heart Disease After Heart Transplantation: Impact of Disease Type, Previous Thoracic Surgeries, and Bystander Organ Dysfunction. J. Card. Fail. 2016, 22, 578–582. [Google Scholar] [CrossRef]
- Menkis, A.H.; McKenzie, F.; Novick, R.J.; Kostuk, W.J.; Pflugfelder, P.W.; Goldbach, M.; Rosenberg, H. Expanding applicability of transplantation after multiple prior palliative procedures. Ann. Thorac. Surg. 1991, 52, 722–726. [Google Scholar] [CrossRef]
- Michielon, G.; Carotti, A.; Pongiglione, G.; Cogo, P.; Parisi, F. Orthotopic Heart Transplantation in Patients with Univentricular Physiology. Curr. Cardiol. Rev. 2011, 7, 85–91. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Michielon, G.; Parisi, F.; Di Carlo, D.; Squitieri, C.; Carotti, A.; Buratta, M.; Di Donato, R.M. Orthotopic heart transplantation for failing single ventricle physiology. Eur. J. Cardio-Thorac. Surg. 2003, 24, 502–510. [Google Scholar] [CrossRef] [Green Version]
- Miller, J.R.; Simpson, K.E.; Epstein, D.J.; Lancaster, T.S.; Henn, M.C.; Schuessler, R.B.; Balzer, D.T.; Shahanavaz, S.; Murphy, J.J.; Canter, C.E.; et al. Improved survival after heart transplant for failed Fontan patients with preserved ventricular function. J. Heart Lung Transplant. 2016, 35, 877–883. [Google Scholar] [CrossRef]
- Mitchell, M.B.; Campbell, D.N.; Boucek, M.M. Heart transplantation for the failing Fontan circulation. Semin. Thorac. Cardiovasc. Surgery: Pediatr. Card. Surg. Annu. 2004, 7, 56–64. [Google Scholar] [CrossRef] [PubMed]
- Mueller, M.F.; Paul, A.C.; Mann, V.; Koerner, C.M.; Valeske, K.; Thul, J.; Mazhari, N.; Bauer, J.; Schranz, D.; Akintuerk, H. Anesthesia for Pediatric Heart Transplantation: Are Patients with a Failing Hemi-Fontan- or Fontan-Physiology Different? Semin. Cardio-Thorac. Vasc. Anesth. 2019, 23, 393–398. [Google Scholar] [CrossRef] [PubMed]
- Navaratnam, M.; Ng, A.; Williams, G.D.; Maeda, K.; Mendoza, J.M.; Concepcion, W.; Hollander, S.A.; Ramamoorthy, C. Perioperative management of pediatric en-bloc combined heart-liver transplants: A case series review. Pediatr. Anesthesia 2016, 26, 976–986. [Google Scholar] [CrossRef]
- Pawlak, S.; Przybylski, R.; Skalski, J.; Śliwka, J.; Kansy, A.; Grzybowski, A.; Wierzyk, A.; Białkowski, J.; Maruszewski, B.; Zembala, M. First Polish analysis of the treatment of advanced heart failure in children with the use of BerlinHeart EXCOR mechanical circulatory support. Kardiol. Polska 2018, 76, 83–90. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pereira, N.L.; Shirali, G. Cardiac Transplant Following Failed Fontan or Glenn Procedures. J. Am. Coll. Cardiol. 2005, 46, 1374–1375. [Google Scholar] [CrossRef] [Green Version]
- Polyviou, S.; O’Sullivan, J.; Hasan, A.; Coats, L. Mortality Risk Stratification in Small Patient Cohorts: The Post-Fontan Heart Transplantation Paradigm. Am. J. Cardiol. 2018, 122, 182–183. [Google Scholar] [CrossRef]
- Razzouk, A.J.; Bailey, L.L. Heart Transplantation in Children for End-Stage Congenital Heart Disease. Semin. Thorac. Cardiovasc. Surgery: Pediatr. Card. Surg. Annu. 2014, 17, 69–76. [Google Scholar] [CrossRef]
- Reardon, L.C.; DePasquale, E.C.; Tarabay, J.; Cruz, D.; Laks, H.; Biniwale, R.M.; Busuttil, R.W.; Kaldas, F.M.; Saab, S.; Venick, R.S.; et al. Heart and heart-liver transplantation in adults with failing Fontan physiology. Clin. Transplant. 2018, 32, e13329. [Google Scholar] [CrossRef]
- Schumacher, K.R.; Almond, C.; Singh, T.P.; Kirk, R.; Spicer, R.; Hoffman, T.M.; Hsu, D.; Naftel, D.C.; Pruitt, E.; Zamberlan, M.; et al. Predicting graft loss by 1 year in pediatric heart transplantation candidates: An analysis of the Pediatric Heart Transplant Study database. Circulation 2015, 131, 890–898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schumacher, K.R.; Yu, S.; Butts, R.; Castleberry, C.; Chen, S.; Edens, E.; Godown, J.; Johnson, J.; Kemna, M.; Lin, K.; et al. Fontan-associated protein-losing enteropathy and post-heart transplant outcomes: A multicenter study. J. Heart Lung Transplant. 2019, 38, 17–25. [Google Scholar] [CrossRef] [Green Version]
- Schure, A.Y.; Kussman, B.D. Pediatric heart transplantation: Demographics, outcomes, and anesthetic implications*. Pediatr. Anesthesia 2010, 21, 594–603. [Google Scholar] [CrossRef] [PubMed]
- Seddio, F.; Gorislavets, N.; Iacovoni, A.; Cugola, D.; Fontana, A.; Galletti, L.; Terzi, A.; Ferrazzi, P. Is heart transplantation for complex congenital heart disease a good option? A 25-year single centre experience†. Eur. J. Cardio-Thorac. Surg. 2012, 43, 605–611. [Google Scholar] [CrossRef] [Green Version]
- Serfas, J.D.; Patel, P.A.; Krasuski, R.A. Heart Transplantation and Mechanical Circulatory Support in Adults with Congenital Heart Disease. Curr. Cardiol. Rep. 2018, 20, 81. [Google Scholar] [CrossRef] [PubMed]
- Sglimbea, A.; Opriş, M.; Suciu, M.; Ispas, M.; Deac, R.; Suciu, H. Indication for transplantation in a patient with univentricular heart. Chirurgia 2013, 108, 770–773. [Google Scholar]
- Tjan, T.D.; Scheld, H.H.; Schmid, C. Heart transplantation after Fontan’s procedure with bilateral cavopulmonary connections. Thorac. Cardiovasc. Surg. 2006, 54, 210–212. [Google Scholar] [CrossRef] [PubMed]
- Vaikunth, S.S.; Concepcion, W.; Daugherty, T.; Fowler, M.; Lutchman, G.; Maeda, K.; Rosenthal, D.; Teuteberg, J.; Woo, Y.J.; Lui, G.K. Short-term outcomes of en bloc combined heart and liver transplantation in the failing Fontan. Clin. Transplant. 2019, 33, e13540. [Google Scholar] [CrossRef]
- Voeller, R.K.; Epstein, D.J.; Guthrie, T.J.; Gandhi, S.; Canter, C.E.; Huddleston, C.B. Trends in the Indications and Survival in Pediatric Heart Transplants: A 24-year Single-Center Experience in 307 Patients. Ann. Thorac. Surg. 2012, 94, 807–816. [Google Scholar] [CrossRef]
- Kinsella, A.; Rao, V.; Fan, C.; Manlhiot, C.; Stehlik, J.; Ross, H.; Alba, A.C. Post-transplant survival in adult congenital heart disease patients as compared to dilated and ischemic cardiomyopathy patients; an analysis of the thoracic ISHLT registry. Clin. Transplant. 2020, 34. [Google Scholar] [CrossRef] [PubMed]
- Rossano, J.W.; Singh, T.P.; Cherikh, W.S.; Chambers, D.C.; Harhay, M.O.; Hayes, D.; Jr Hsich, E.; Khush, K.K.; Meiser, B.; Potena, L.; et al. The International Thoracic Organ Transplant Registry of the International Society for Heart and Lung Transplantation: Twenty-second pediatric heart transplantation report–2019; Focus theme: Donor and recipient size match. J. Heart Lung Transplant. 2019, 38, 1028–1041. [Google Scholar] [CrossRef]
- Rodriguez de Santiago, E.; Tellez, L.; Garrido-Lestache Rodriguez-Monte, E.; Garrido-Gomez, E.; Aguilera-Castro, L.; Alvarez-Fuente, M.; Del Cerro, M.J.; Albillos, A. Fontan protein-losing enteropathy is associated with advanced liver disease and a proinflammatory intestinal and systemic state. Liver Int. 2020, 40, 638–645. [Google Scholar] [CrossRef] [PubMed]
- Grutter, G.; Di Carlo, D.; Gandolfo, F.; Adorisio, R.; Alfieri, S.; Michielon, G.; Carotti, A.; Pongiglione, G. Plastic Bronchitis After Extracardiac Fontan Operation. Ann. Thorac. Surg. 2012, 94, 860–864. [Google Scholar] [CrossRef]
- Fauziah, M.; Lilyasari, O.; Liastuti, L.D.; Rahmat, B. Systemic ventricle morphology impact on ten-year survival after Fontan surgery. Asian Cardiovasc. Thorac. Ann. 2018, 26, 677–684. [Google Scholar] [CrossRef] [PubMed]
- Julsrud, P.R.; Weigel, T.J.; A Van Son, J.; Edwards, W.D.; Mair, D.D.; Driscoll, D.J.; Danielson, G.K.; Puga, F.J.; Offord, K.P. Influence of ventricular morphology on outcome after the Fontan procedure. Am. J. Cardiol. 2000, 86, 319–323. [Google Scholar] [CrossRef]
- Pundi, K.N.; Pundi, K.; Johnson, J.N.; Dearani, J.A.; Li, Z.; Driscoll, D.J.; Wackel, P.L.; McLeod, C.J.; Cetta, F.; Cannon, B.C. Sudden cardiac death and late arrhythmias after the Fontan operation. Congenit. Heart Dis. 2017, 12, 17–23. [Google Scholar] [CrossRef]
- De Vadder, K.; Van De Bruaene, A.; Gewillig, M.; Meyns, B.; Troost, E.; Budts, W. Predicting outcome after Fontan palliation: A single-centre experience, using simple clinical variables. Acta Cardiol. 2014, 69, 7–14. [Google Scholar] [CrossRef]
- Rösner, A.; Khalapyan, T.; Dalen, H.; McElhinney, D.B.; Friedberg, M.K.; Lui, G.K. Classic-Pattern Dyssynchrony in Adolescents and Adults with a Fontan Circulation. J. Am. Soc. Echocardiogr. 2018, 31, 211–219. [Google Scholar] [CrossRef]
- De Groot, N.M.S.; Bogers, A. Development of Tachyarrhythmias Late After the Fontan Procedure: The Role of Ablative Therapy. Card. Electrophysiol. Clin. 2017, 9, 273–284. [Google Scholar] [CrossRef]
- Mizuno, M.; Ohuchi, H.; Matsuyama, T.-A.; Miyazaki, A.; Ishibashi-Ueda, H.; Yamada, O. Diverse multi-organ histopathologic changes in a failed Fontan patient. Pediatr. Int. 2016, 58, 1061–1065. [Google Scholar] [CrossRef] [PubMed]
- Hollander, S.A.; Cantor, R.S.; Sutherland, S.M.; Koehl, D.A.; Pruitt, E.; McDonald, N.; Kirklin, J.K.; Ravekes, W.J.; Ameduri, R.; Chrisant, M.; et al. Renal injury and recovery in pediatric patients after ventricular assist device implantation and cardiac transplant. Pediatr. Transplant. 2019, 23, e13477. [Google Scholar] [CrossRef]
- Potena, L.; Zuckermann, A.; Barberini, F.; Aliabadi-Zuckermann, A. Complications of Cardiac Transplantation. Curr. Cardiol. Rep. 2018, 20, 9–73. [Google Scholar] [CrossRef] [PubMed]
- Di Nora, C.; Paldino, A.; Miani, D.; Finato, N.; Pizzolitto, S.; De Maglio, G.; Igor, V.; Sandro, S.; Chiara, N.; Gianfranco, S.; et al. Transplantation in Kearns-Sayre Syndrome. Transplantation 2019, 103, e393–e394. [Google Scholar] [CrossRef] [PubMed]
- Di Nora, C.; Livi, U. Heart transplantation in cardiac storage diseases: Data on Fabry disease and cardiac amyloidosis. Curr. Opin. Organ. Transplant. 2020, 25, 211–217. [Google Scholar] [CrossRef]
- de Diego-Sola, A.; Egues Dubuc, C.A.; Goena Vives, C.; Intxausti Irazabal, J.J.; Maiz Alonso, O.; Cobo Belaustegi, M. Heart Transplantation in Systemic Sclerosis: A Therapeutic Option. Presentation of a Case and Literature Review. Reumatol. Clin. (Engl. Ed.) 2021. Online ahead of print; S1699-258X(21)00125-X. [Google Scholar] [CrossRef] [PubMed]
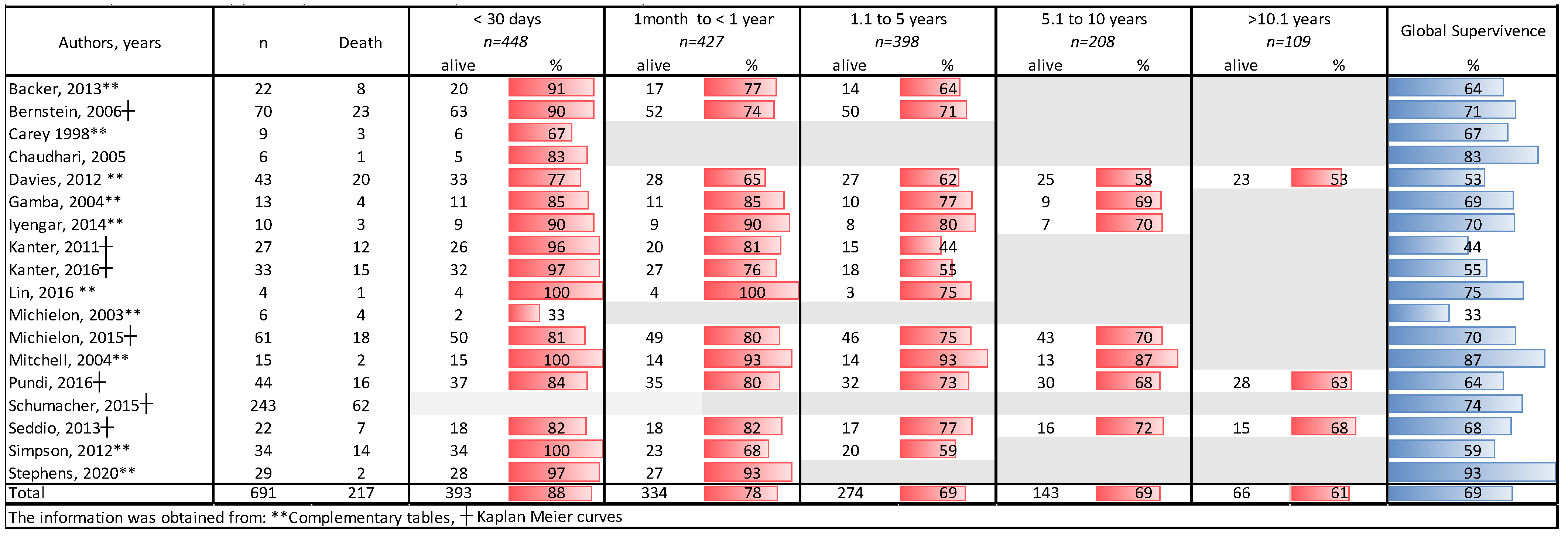


| Author, Year | Country | Design | Overall Results | Outcomes | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Transplantation | Fontan Population | Death | PLE | Arrythmia | HF | PB | CKD | |||
| Backer, 2013 [6] | USA | A retrospective study | 206 | 22 | 8 | 5/13 (18%) | N/A | 6/13 (46%) | 0/2 (0%) | N/A |
| Bernstein, 2006 [68] | USA | A retrospective, multi-institutional study | 1746 | 70 | 23 | 10/25 (40%) | N/A | N/A | N/A | N/A |
| Carey, 1998 [69] | UK | A retrospective review study in a single center, case series | 46 | 9 | 3 | N/A | 2/6 (33%) | 2/5 (40%) | N/A | 1/2 (50%) |
| Chaudhar, 2005 [56] | UK | A retrospective review, a case series. | 110 | 6 | 1 | N/A | 1/2 (50%) | N/A | N/A | N/A |
| Davies, 2012 [12] | USA | A retrospective review study | 172 | 43 | 20 | 9/17 (53%) | N/A | 9/18 (50%) | 0/1 (0%) | N/A |
| Gamba, 2004 [57] | Italy | A retrospective review | 575 | 13 | 4 | 2/7 (29%) | 2/5 (40%) | 4/9 (44%) | N/A | N/A |
| Iyengar, 2014 [74] | Australia | A retrospective study in a single center | 111 | 10 | 3 | 0/1 (0%) | N/A | 3/8 (38%) | NA | NA |
| Kanter, 2011 [77] | USA | A retrospective study in a Single center. | 222 | 27 | 12 | 2/12 (17%) | N/A | 4/21 (19%) | N/A | N/A |
| Kanter, 2016 [59] | USA | A retrospective study in a Single center. | 311 | 33 | 15 | 2/13 (15%) | N/A | N/A | N/A | N/A |
| Lin, 2016 [60] | Taiwan | A retrospective study in a Single center, cases series. | 513 | 4 | 1 | 1/3 (33%) | N/A | 0/3 (0%) | N/A | N/A |
| Michielon, 2003 [83] | Italy | A Cohort study | 25 | 6 | 8 | 1/2 (50%) | N/A | N/A | N/A | N/A |
| Michielon, 2015 [15] | Netherlands | A retrospective multicenter review. | 61 | 61 | 18 | 11/14 (79%) | N/A | 14/28 (50%) | N/A | N/A |
| Mitchell, 2004 [58] | USA | A retrospective study in a single center. | 15 | 15 | 1 | 1/4 (25%) | 1/4 (25%) | 2/13 (15%) | N/A | N/A |
| Pundi, 2016 [11] | USA | A retrospective review, cohort study in a single center. | 44 | 44 | 16 | 5/12 (42%) | 6/28 (21%) | N/A | N/A | N/A |
| Schumacher, 2015 [7] | USA | A retrospective cohort study | 3686 | 356 | 62 | 22/70 (31%) | N/A | N/A | N/A | N/A |
| Seddio, 2013 [96] | Italy | A retrospective cohort study | 839 | 22 | 15 | 6/11 (55%) | N/A | N/A | N/A | N/A |
| Simpson, 2012 [9] | USA | A retrospective review study | 34 | 34 | 11 | 5/12 (42%) | N/A | 7/17 (41%) | N/A | N/A |
| Stephens, 2020 [63] | USA | A retrospective cohort study | 153 | 32 | 5 | N/A | N/A | N/A | N/A | 2/3 (67%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Márquez-González, H.; Hernández-Vásquez, J.G.; Del Valle-Lom, M.; Yáñez-Gutiérrez, L.; Klünder-Klünder, M.; Almeida-Gutiérrez, E.; Koretzky, S.G. Failures of the Fontan System in Univentricular Hearts and Mortality Risk in Heart Transplantation: A Systematic Review and Meta-Analysis. Life 2021, 11, 1363. https://doi.org/10.3390/life11121363
Márquez-González H, Hernández-Vásquez JG, Del Valle-Lom M, Yáñez-Gutiérrez L, Klünder-Klünder M, Almeida-Gutiérrez E, Koretzky SG. Failures of the Fontan System in Univentricular Hearts and Mortality Risk in Heart Transplantation: A Systematic Review and Meta-Analysis. Life. 2021; 11(12):1363. https://doi.org/10.3390/life11121363
Chicago/Turabian StyleMárquez-González, Horacio, Jose Gustavo Hernández-Vásquez, Montserrat Del Valle-Lom, Lucelli Yáñez-Gutiérrez, Miguel Klünder-Klünder, Eduardo Almeida-Gutiérrez, and Solange Gabriela Koretzky. 2021. "Failures of the Fontan System in Univentricular Hearts and Mortality Risk in Heart Transplantation: A Systematic Review and Meta-Analysis" Life 11, no. 12: 1363. https://doi.org/10.3390/life11121363







