Bosworth Fractures of the Ankle: A Systematic Literature Review
Abstract
:1. Introduction
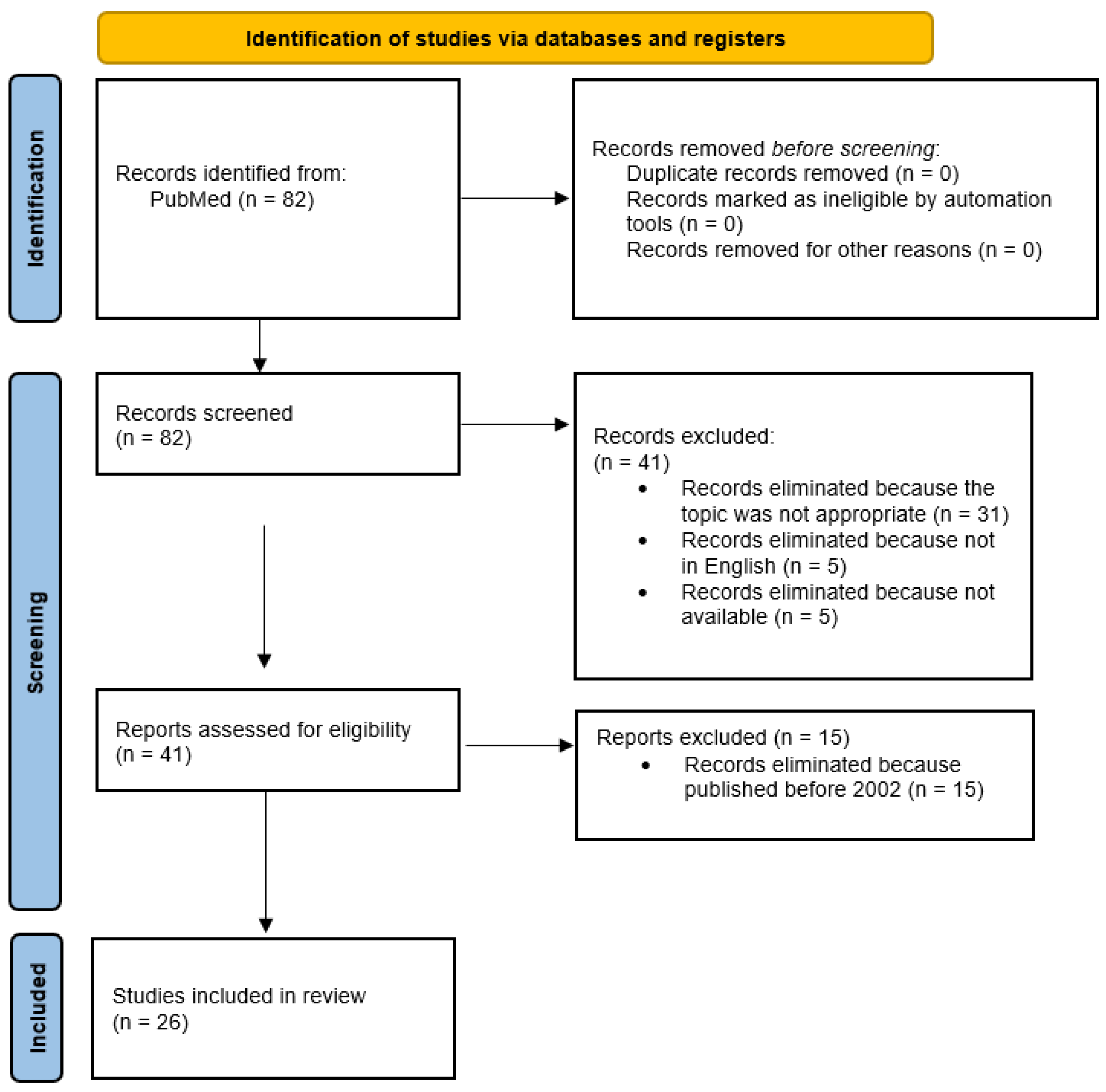
2. Literature Search
2.1. Literature Search Strategy
2.2. Selection Criteria
2.3. Data Extraction and Criteria Appraisal
3. Studies
3.1. Study Selection
3.2. Participants
3.3. Treatment
3.4. Follow-Up, Post-Operative Complications, and Outcomes
4. Discussion
- (1)
- AP view: overlap of the proximal fibular fragment and the distal tibia;
- (2)
- Lateral view: posterior displacement of the fibula and posterior subluxation of the talus;
- (3)
- Mortise view: widened medial joint space.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bosworth, D.M. Fracture-Dislocation of the Ankle with Fixed Displacement of the Fibula behind the Tibia. J. Bone Jt. Surg. Am. 1947, 29, 130–135. [Google Scholar]
- Ren, W.; Hu, Y.-C.; Lu, J.-K. Rare Variants of Bosworth Fracture-Dislocation: Bosworth Fracture-Dislocation with Medial Malleolus Adduction Type Fracture. Chin. J. Traumatol. 2019, 22, 120–124. [Google Scholar] [CrossRef] [PubMed]
- Martin-Somoza, F.J.; Picazo, D.R.; Cabezuelo, J.A.M.; González, A.V. Bosworth Fracture. An Atypical Case of Irreducible Ankle Fracture-Dislocation. Trauma Case Rep. 2020, 28, 100322. [Google Scholar] [CrossRef]
- Yang, K.H.; Won, Y.; Lim, J.-R.; Kang, D.-H. Assessment of Bosworth-Type Fracture by External Oblique Radiographs. Am. J. Emerg. Med. 2014, 32, 1387–1390. [Google Scholar] [CrossRef]
- Cappuccio, M.; Leonetti, D.; Di Matteo, B.; Tigani, D. An Uncommon Case of Irreducible Ankle Fracture-Dislocation: The “Bosworth-like” Tibio-Fibular Fracture. Foot Ankle Surg. 2017, 23, e1–e4. [Google Scholar] [CrossRef] [PubMed]
- Bartoníček, J.; Rammelt, S.; Kostlivý, K. Bosworth Fracture: A Report of Two Atypical Cases and Literature Review of 108 Cases. Fuß Sprunggelenk 2017, 15, 126–137. [Google Scholar] [CrossRef]
- Cho, B.-K.; Choi, S.-M.; Shin, Y.-D. Prognostic Factors for Intermediate-Term Clinical Outcomes Following Bosworth Fractures of the Ankle Joint. Foot Ankle Surg. 2019, 25, 601–607. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Fan, J.; Michelin, R.M.; Jenkins, R.; Hwang, M.; French, M. A Novel Technique for a Successful Closed Reduction of a Bosworth Fracture-Dislocation of the Ankle. Cureus 2020, 12, e6632. [Google Scholar] [CrossRef]
- Won, Y.; Lee, G.-S.; Hwang, J.-M.; Park, I.; Song, J.-H.; Kang, C.; Hwang, D.-S. Improved Functional Outcome after Early Reduction in Bosworth Fracture-Dislocation. Foot Ankle Surg. 2019, 25, 798–803. [Google Scholar] [CrossRef] [PubMed]
- Arora, A.; Saidapur, S.K.; Uppin, R.B.; Bose, S. Ankle Arthrodesis Using Retrograde Nail in Case of Bosworth Fracture with Ankle Dislocation: A Rare Case Report. J. Orthop. Case Rep. 2021, 11, 11–15. [Google Scholar]
- Moerenhout, K.; Gkagkalis, G.; Baalbaki, R.; Crevoisier, X. Association of Bosworth, Pilon, and Open Talus Fractures: A Very Unusual Ankle Trauma. Case Rep. Orthop. 2019, 2019, 6316137. [Google Scholar] [CrossRef] [PubMed]
- Ji, W.-B.; Xu, Y.-F.; Lu, Z. Case Report: Bosworth Fracture-Dislocation Managed by Closed Reduction and Conservative Treatment. Front. Surg. 2022, 8, 788575. [Google Scholar] [CrossRef] [PubMed]
- Peterson, N.D.; Shah, F.; Narayan, B. An Unusual Ankle Injury: The Bosworth-Pilon Fracture. J. Foot Ankle Surg. 2015, 54, 751–753. [Google Scholar] [CrossRef]
- Schepers, T.; Hagenaars, T.; Den Hartog, D. An Irreducible Ankle Fracture Dislocation: The Bosworth Injury. J. Foot Ankle Surg. 2012, 51, 501–503. [Google Scholar] [CrossRef] [PubMed]
- Khan, F.; Borton, D. A Constant Radiological Sign in Bosworth’s Fractures: “The Axilla Sign”. Foot Ankle Int. 2008, 29, 55–57. [Google Scholar] [CrossRef]
- Delasotta, L.A.; Hansen, R.H.; Sands, A.K. Surgical Management of the Posterior Fibula Fracture Dislocation: Case Report. Foot Ankle Int. 2013, 34, 1443–1446. [Google Scholar] [CrossRef]
- Han, S.-J.; Kim, J.-H.; Yang, D.-B.; Kim, B.-S.; Ok, H.-S. Bosworth-Type Fibular Entrapment Fracture of the Ankle without Dislocation: A Rare Case Report and a Review of the Literature. Ann. Transl. Med. 2021, 9, 178. [Google Scholar] [CrossRef]
- Bartoníček, J.; Frič, V.; Svatoš, F.; Luňáček, L. Bosworth-Type Fibular Entrapment Injuries of the Ankle-The Bosworth Lesion: A Report of 6 Cases and Literature Review. J. Orthop. Trauma 2007, 21, 710–717. [Google Scholar] [CrossRef] [PubMed]
- Lui, T.H.; Chan, K.B.; Kong, C.C.; Ngai, W.K. Ankle Stiffness after Bosworth Fracture Dislocation of the Ankle. Arch. Orthop. Trauma Surg. 2008, 128, 49–53. [Google Scholar] [CrossRef]
- He, S.; Zhu, J. Ankle Arthroscopy–Assisted Closed Reduction in Bosworth Fracture Dislocation. SAGE Open Med. Case Rep. 2020, 8, 2050313X2097452. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.D.; Blue, M.; Douthit, C.; Caroom, C. Bosworth Dislocation without Associated Fracture. Case Rep. Orthop. 2018, 2018, 7284643. [Google Scholar] [CrossRef]
- Wenxian, P.; Mehta, K.V. Rare Bosworth Fracture-Dislocation Variant of an Irreducible Distal Fibula Dislocation of the Ankle without Fibula Fracture. Foot Ankle Orthop. 2019, 4, 247301141882090. [Google Scholar] [CrossRef]
- Bartoníček, J.; Rammelt, S.; Kostlivý, K. Bosworth Fracture Complicated by Unrecognized Compartment Syndrome: A Case Report and Review of the Literature. Arch. Orthop. Trauma Surg. 2022, 142, 1435–1441. [Google Scholar] [CrossRef]
- Perry, C.R.; Rice, S.; Rao, A.; Burdge, R. Posterior Fracture-Dislocation of the Distal Part of the Fibula. Mechanism and Staging of Injury. J. Bone Jt. Surg. Am. 1983, 65, 1149–1157. [Google Scholar] [CrossRef]
- Wright, S.E.; Legg, A.; Davies, M.B. A Contemporary Approach to the Management of a Bosworth Injury. Injury 2012, 43, 252–253. [Google Scholar] [CrossRef] [PubMed]
- Fahey, J.J.; Schlenker, L.T.; Stauffer, R.C. Fracture Dislocation of the Ankle with Fixed Displacement of the Fibula behind the Tibia. Am. J. Roentgenol. Radium Ther. Nucl. Med. 1956, 76, 1102–1113. [Google Scholar] [PubMed]
- Beekman, R.; Watson, J.T. Bosworth Fracture-Dislocation and Resultant Compartment Syndrome. A Case Report. J. Bone Jt. Surg. Am. 2003, 85, 2211–2214. [Google Scholar] [CrossRef]
- Szalay, M.D.; Roberts, J.B. Compartment Syndrome after Bosworth Fracture-Dislocation of the Ankle: A Case Report. J. Orthop. Trauma 2001, 15, 301–303. [Google Scholar] [CrossRef]
- Hockenbury, R.T.; Friermood, T.G. Dislocation of the Distal Tibiofibular Joint. J. Orthop. Trauma 1992, 6, 120–124. [Google Scholar] [PubMed]
- Foldager, C.B.; Barckman, J.; Robertsen, K.; Borris, L.C. Bosworth Fracture Dislocation of the Ankle: Two Case Reports with Perioperative Illustration. Trauma Case Rep. 2018, 17, 39–42. [Google Scholar] [CrossRef] [PubMed]
- Pollak, A.N.; Mccarthy, M.L.; Bess, R.S.; Agel, J.; Swiontkowski, M.F. Outcomes after treatment of high-energy tibial plafond fractures. J. Bone Jt. Surg. 2003, 85, 1893–1900. [Google Scholar] [CrossRef] [PubMed]
- Fournier, A.; Barba, N.; Steiger, V.; Lourdais, A.; Frin, J.-M.; Williams, T.; Falaise, V.; Pineau, V.; Salle de Chou, E.; Noailles, T.; et al. Total Talar Fracture—Long-Term Results of Internal Fixation of Talar Fractures. A Multicentric Study of 114 Cases. Orthop. Traumatol. Surg. Res. 2012, 98, S48–S55. [Google Scholar] [CrossRef] [PubMed]


| AUTHOR | N° PATIENTS | ARTICLE | SEX |
|---|---|---|---|
| Arora 2021 | 1 | Ankle Arthrodesis Using Retrograde Nail in Case of Bosworth Fracture with Ankle Dislocation: A Rare Case Report | Female |
| Bartonicek 2007 | 6 | Bosworth-type fibular entrapment injuries of the ankle: the Bosworth lesion. A report of 6 cases and literature review | (I) Female (II) Male (III) Male (IV) Female (V) Female (VI) Male |
| Bartonicek 2022 | 1 | Bosworth fracture complicated by unrecognized compartment syndrome: a case report and review of the literature | Male |
| Cappuccio 2017 | 1 | An uncommon case of irreducible ankle fracture-dislocation: the “Bosworth-like” tibio-fibular fracture | Male |
| Cho 2019 | 15 | Prognostic factors for intermediate-term clinical outcomes following Bosworth fractures of the ankle joint | 11 male; 4 female |
| Delasotta 2013 | 1 | Surgical management of the posterior fibula fracture dislocation: case report | Male |
| Ellanti 2013 | 1 | Acutely irreducible ankle fracture dislocation: a report of a Bosworth fracture and its management | Male |
| Fan 2020 | 1 | A Novel Technique for a Successful Closed Reduction of a Bosworth Fracture-Dislocation of the Ankle | Male |
| Foldager 2018 | 2 | Bosworth fracture dislocation of the ankle: - Two case reports with perioperative illustration | (I) Male (II) Male |
| Han 2021 | 1 | Bosworth-type fibular entrapment fracture of the ankle without dislocation: a rare case report and a review of the literature | Male |
| He 2020 | 1 | Ankle arthroscopy-assisted closed reduction in Bosworth fracture dislocation | Female |
| Ji 2022 | 1 | Case Report: Bosworth Fracture-Dislocation managed by Closed Reduction and Conservative Treatment | Male |
| Khan 2008 | 1 | A constant radiological sign in Bosworth’s fractures: “the Axilla sign” | Female |
| Lu 2016 | 1 | A radiological sign (which we are calling the ‘tongues of flame’ sign) in irreducible trimalleolar fractures of the ankle | Female |
| Lui 2008 | 4 | Ankle stiffness after Bosworth fracture dislocation of the ankle | (I) Male (II)Male (III) Female (IV) Male |
| Maertin-Somoza 2020 | 1 | Bosworth fracture. An atypical case of irreducible ankle fracture-dislocation | Female |
| Moerenhout 2019 | 1 | Association of Bosworth, Pilon, and Open Talus Fractures: A Very Unusual Ankle Trauma | Male |
| Peterson 2015 | 1 | An Unusual Ankle Injury: The Bosworth-Pilon Fracture | Male |
| Ren 2019 | 2 | Rare variants of Bosworth fracture-dislocation: Bosworth fracture-dislocation with medial malleolus adduction type fracture | 2 Male |
| Schepers 2012 | 1 | An irreducible ankle fracture dislocation: the Bosworth injury | Female |
| Wenxian 2019 | 1 | Rare Bosworth Fracture-Dislocation Variant of an Irreducible Distal Fibula Dislocation of the Ankle Without Fibula Fracture | Male |
| Williams 2018 | 1 | Bosworth Dislocation without Associated Fracture | Male |
| Won 2019 | 51 | Improved functional outcome after early reduction in Bosworth fracture-dislocation | 32 male; 19 female |
| Wright 2012 | 1 | A contemporary approach to the management of a Bosworth injury | Male |
| Yang 2014 | 4 | Assessment of Bosworth-type fracture by external oblique radiographs | 4 Male |
| Yeoh 2013 | 1 | Bosworth fracture-dislocation of the ankle: a case report | Male |
| Mechanism of Injury | Percentage | N° of Patients |
|---|---|---|
| Accidental trauma | 58.2% | 60 |
| Sport injury | 18.4% | 19 |
| Traffic accident | 18.4% | 19 |
| Working injury | 0.97% | 1 |
| No data | 3.9% | 4 |
| AUTHOR | INJURY TYPE (WEBER) | Axilla Sign | CT SCAN | CLOSED REDUCTION |
|---|---|---|---|---|
| Arora | Gustilo 2b | No data | No data | Unsuccessful |
| Bartonicek | Weber B | No data | Yes | Successful (2nd attempt) |
| Bartonicek | (I) Weber C (II) Weber C (III) Weber C (IV) Weber B (V) Weber B (VI) Weber B | No data | (I) No data (II) No data (III) No data (IV) Yes (V) no data (VI) No data | (I) Unsuccessful (II) Unsuccessful (III) Unsuccessful (III) Unsuccessful (IV) Unsuccessful (V) Unsuccessful (VI) Unsuccessful |
| Cappuccio | Weber C | No data | Yes | Unsuccessful |
| Cho | 13 Weber B; 2 Weber C | No data | Yes | 14 Unsuccessful; 1 successful |
| Delasotta | Weber B | Yes | Yes | unsuccessful |
| Ellanti | Weber C | No data | no data | unsuccessful |
| Fan | No data | No data | No | Successful (2nd attempt) |
| Foldager | No data | No data | (I) no data (II) no data | (I) Unsuccessful (II) unsuccessful |
| Han | Weber B | No data | Yes | Not attempted |
| He | No data | No data | Yes | Unsuccessful |
| Ji | Weber B | Yes | Yes | Unsuccessful |
| Khan | No data | Yes | No data | unsuccessful |
| Lu | Weber B | No data | Yes | unsuccessful |
| Lui | (I) No data (II)Weber B (III) Weber B (IV) No data | No data | (I) Yes (II) No data (III) No data (IV) no data | (I) Unsuccessful (II) Unsuccessful (III) Unsuccessful |
| Maertin-Somoza | No data | No data | No | Unsuccessful |
| Moerenhout | Gustilo 3B | No data | Yes | unsuccessful |
| Peterson | The initial radiographs showed a bimalleolar ankle fracture dislocation with a comminuted fracture of the tibial plafond | Yes | Yes | unsuccessful |
| Ren | Weber B | No data | Yes | Unsuccessful |
| Schepers | Weber B | Yes | No data | unsuccessful |
| Wenxian | No data | No data | Yes | Unsuccessful |
| Williams | No data | No data | No | Unsuccessful |
| Won | 1 Weber A; 48 Weber B; 2 Weber C | No data | Yes | Unsuccessful |
| Wright | No data | No data | Yes | unsuccessful |
| Yang | 4 Weber B | Yes | Yes | |
| Yeoh | Weber B | No data | No | Unsuccessful |
| AUTHOR | DEFINITIVE TREATMENT | Cast after Surgery | Syndesmotic Screw Removed (weeks/months) | HARDWARE Removed | USE OF EXTERNAL FIXATION | USE OF TRACTION | USE OF CAST |
|---|---|---|---|---|---|---|---|
| Arora | ORIF | 6 weeks | Yes | No | Yes | ||
| Bartonicek | ORIF | 6 weeks | 2 months | Not reported | No | No | Yes |
| Bartonicek | (I) ORIF (II) cast(III) ORIF (IV) ORIF (V) ORIF (VI) ORIF | (I) 5 weeks (II)–(III) 6 weeks (IV)6 weeks (V) 6 weeks (VI) 6 weeks | (I) 8 weeks after surgery (II)–(III) suprasyndesmotic screws were removed after 2 months (IV) suprasyndesmotic screw was removed 4 months after (V) patient declined removal of the suprasyndesmotic screw (VI) - | (I) Yes, after 2 years (IV) Yes, after 11 month | No | No | Yes |
| Cappuccio | ORIF | 4 weeks | No | Yes | Yes | ||
| Cho | 8 weeks | 12–16 weeks after surgery | No | No | Yes | ||
| Delasotta | ORIF | 6 weeks | 4 months after surgery | No | No | Yes | |
| Ellanti | ORIF | 6 weeks | 3 months after surgery | No | No | Yes | |
| Fan | ORIF | 6 weeks | No data | Not reported | No | No | Yes |
| Foldager | ORIF | (I) 6 weeks (II) 6 weeks | (I) no data (II) no data | No | No | Yes | |
| Han | ORIF | 6 weeks | No syndesmotic screw | Not reported | No | No | Yes |
| He | Ankle arthroscopy and ORIF | 4 weeks | 3 months after surgery | No | No | Yes | |
| Ji | cast | 9 weeks | No | No | Yes | ||
| Khan | ORIF | 6 weeks | 6 weeks after surgery | No | No | Yes | |
| Lu | ORIF | 6 weeks | No | No | Yes | ||
| Lui | Arthroscopy and ORIF | (I) 6 weeks (II) no cast (III) no cast (IV) no cast | (I) 12 weeks after surgery (II) 12 weeks after surgery (III)12 weeks after surgery (IV)12 weeks after surgery | No | No | Yes | |
| Maertin-Somoza | ORIF | 10 days | No | Not reported | No | No | Yes |
| Moerenhout | ORIF | 12 weeks | No | No | Yes | ||
| Peterson | ORIF | 6 weeks | No data | Yes | No | Yes | |
| Ren | ORIF | 2 weeks | 8 weeks | Not reported | No | No | Yes |
| Schepers | ORIF | 6 weeks | Syndesmotic screws were not removed in the absence of complaints | yes, after 9 months (because of shoe wear problems caused by the implant) | No | No | Yes |
| Wenxian | ORIF | 6 weeks | 6 weeks after surgery | Yes | Yes | No | Yes |
| Williams | ORIF | No data | 4 months | 4 months | No | No | Yes |
| Won | ORIF | no data | No data | no data | No data | No data | No data |
| Wright | ORIF | 6 weeks | No | No | Yes | ||
| Yang | ORIF | No data | No data | Not reported | No data | No data | No data |
| Yeoh | ORIF | No data | 16 weeks | Not reported | No | No | No data |
| AUTHOR | Complication/Sequelae | Type of Complication | OUTCOME | FOLLOW UP |
|---|---|---|---|---|
| Arora | No data | No data | No data | No data |
| Bartonicek | Compartment syndrome | A fixed fexion contracture of the great toe was observed without the possibility of passive correction, with ulcerations on the plantar and medial aspect of the great toe and below the first metatarsal head | Unsuccessful | 3 years |
| Bartonicek | (I) No (II) Yes (III) No (IV) Yes (V) No (VI) No | (I) The patient had no subjective complaints (II) severe posttraumatic osteoarthritis of the ankle and an arthrodesis was performed (III) the patient had no subjective complaints (IV) pain (V) no (VI) no | (I) Successful (II) unsuccessful (III) successful (IV) successful (V) successful (VI) successful | (I) 8 years (II) 2 years (III) 5 years (IV) 2.5 years (V) 3.5 years (VI) 3 years |
| Cappuccio | No data | No data | Successful | 1 year |
| Cho | 2 patients with joint stiffness in dorsiflexion and plantarflexion | Joint stiffness | Successful | 2 years |
| Delasotta | No | Successful | 6 months; 8 months | |
| Ellanti | No | No complication | Successful | 3 months |
| Fan | No | No | No data | No data |
| Foldager | (I) No (II) No | (I) No complication (II) No complication | (I) Successful (II) successful | (I) Lost follow up (II) 3 months |
| Han | No | No | Successful | 2 years |
| He | No | Successful | 6 months | |
| Ji | No | No complication | Successful | 9 months; 2.5 years |
| Khan | No | Successful | 3 months | |
| Lu | No | Successful | 3 months | |
| Lui | (I) Yes (II) Yes (III) Yes (IV) No | (I) Painful stiffness and using stairs, plantarflexed limitation (open anterior ankle capsular release and extensor tendon adhesiolysis at the level of superior extensor retinaculum was performed. Posterior ankle capsulectomy was also performed through posterior ankle endoscopy) (II) painful stiffness (arthroscopic ankle capsular release was performed) (III) painful stiffness (arthroscopic ankle capsular release was performed) | (I) Unsuccessful (II) unsuccessful (III) unsucessful (IV) successful | (I) 5 months (II) 3 months (III) 3 months (IV) No data |
| Maertin-Somoza | No | No | Successful | 18 months |
| Moerenhout | No acute complication, but after 1 year he had an invalidating partial necrosis of the talus and pilon | No acute complication, but after 1 year he had an invalidating partial necrosis of the talus and pilon | Unsuccessful | 14 months |
| Peterson | At 18 months, the patient was struggling owing to pain in the ankle that developed clinical and radiologic post-traumatic arthritis | At 18 months, the patient was struggling owing to pain in the ankle that developed clinical and radiologic post-traumatic arthritis | Successful | 1.5 years |
| Ren | No | 1 compartment syndrome followed by fasciotomy the day after surgery | Successful | 21 months |
| Schepers | Problems with wearing shoes caused by the implant | Problems eith wearing shoes caused by the implant | Successful | 1 years |
| Wenxian | No | No | Successful | 22 months |
| Williams | No | No | Successful | 6 months |
| Won | Yes | 8 wound complication; 2 compartment syndrome; 9 osteoarthritis; 5 mal-union | Successful | 6 weeks; 3–6–12 months |
| Wright | No | Successful | 3 months; | |
| Yang | No data | No data | No data | 7–9–12–34 months |
| Yeoh | No | No | Successful | 3 months |
| COMPLICATIONS | Percentage | N of Patients |
|---|---|---|
| Post-traumatic arthritis | 10.7% | 11 |
| Wound complications | 7.7% | 8 |
| Painful joint stiffness | 5.8% | 6 |
| Malunion | 4.8% | 5 |
| Compartment syndrome | 3.9% | 4 |
| Fixed flexion contracture of great toe | 0.97% | 1 |
| Necrosis of talus and pilon | 0.97% | 1 |
| Total | 34.9% | 36 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lucenti, L.; Testa, G.; Nocera, C.; Culmone, A.; Dell’Agli, E.; Pavone, V. Bosworth Fractures of the Ankle: A Systematic Literature Review. J. Pers. Med. 2023, 13, 713. https://doi.org/10.3390/jpm13050713
Lucenti L, Testa G, Nocera C, Culmone A, Dell’Agli E, Pavone V. Bosworth Fractures of the Ankle: A Systematic Literature Review. Journal of Personalized Medicine. 2023; 13(5):713. https://doi.org/10.3390/jpm13050713
Chicago/Turabian StyleLucenti, Ludovico, Gianluca Testa, Chiara Nocera, Annalisa Culmone, Eleonora Dell’Agli, and Vito Pavone. 2023. "Bosworth Fractures of the Ankle: A Systematic Literature Review" Journal of Personalized Medicine 13, no. 5: 713. https://doi.org/10.3390/jpm13050713






