Transdiagnostic or Disorder Specific? Indicators of Substance and Behavioral Addictions Nominated by People with Lived Experience
Abstract
1. Introduction
2. Methods
2.1. Participants and Procedure
2.2. Identifying Respondents with Lived Experience
2.3. Eliciting Indicators of Problematic Substance Use and Behavioral Engagement
2.4. Data Analytic Plan
3. Results
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Jacobs, D.F. A general theory of addictions: A new theoretical model. J. Gambl. Behav. 1986, 2, 15–31. [Google Scholar] [CrossRef]
- Orford, J. Addiction as excessive appetite. Addiction 2001, 96, 15–31. [Google Scholar] [CrossRef]
- Shaffer, H.J.; LaPlante, D.A.; LaBrie, R.A.; Kidman, R.C.; Donato, A.N.; Stanton, M.V. Toward a syndrome model of addiction: Multiple expressions, common etiology. Harv. Rev. Psychiatry 2004, 12, 367–374. [Google Scholar] [CrossRef]
- Griffiths, M. A ‘components’ model of addiction within a biopsychosocial framework. J. Subst. Use 2005, 10, 191–197. [Google Scholar] [CrossRef]
- Grant, J.E.; Potenza, M.N.; Weinstein, A.; Gorelick, D.A. Introduction to behavioral addictions. Am. J. Drug Alcohol Abus. 2010, 36, 233–241. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Hodgins, D.C. Component model of addiction treatment: A pragmatic transdiagnostic treatment model of behavioral and substance addictions. Front. Psychiatry 2018, 9, 9. [Google Scholar] [CrossRef] [PubMed]
- Volkow, N.D.; Koob, G.F.; McLellan, A.T. Neurobiologic advances from the brain disease model of addiction. N. Engl. J. Med. 2016, 374, 363–371. [Google Scholar] [CrossRef] [PubMed]
- Konkoly Thege, B.; Horwood, L.; Slater, L.; Tan, M.C.; Hodgins, D.C.; Wild, T.C. Relationship between interpersonal trauma exposure and addictive behaviors: A systematic review. BMC Psychiatry 2017, 17, 164. [Google Scholar] [CrossRef]
- Nutt, D.; King, L.A.; Saulsbury, W.; Blakemore, C. Development of a rational scale to assess the harm of drugs of potential misuse. Lancet 2007, 369, 1047–1053. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®); American Psychiatric Publication: Washington, DC, USA, 2013. [Google Scholar]
- Reilly, C.; Smith, N. The evolving definition of pathological gambling in the DSM-5. Natl. Cent. Responsible Gaming 2013, 1, 1–6. [Google Scholar]
- Saunders, J.B. Substance use and addictive disorders in DSM-5 and ICD 10 and the draft ICD 11. Curr. Opin. Psychiatry 2017, 30, 227–237. [Google Scholar] [CrossRef] [PubMed]
- Yücel, M.; Oldenhof, E.; Ahmed, S.H.; Belin, D.; Billieux, J.; Bowden-Jones, H.; Daglish, M. A transdiagnostic dimensional approach towards a neuropsychological assessment for addiction: An international Delphi consensus study. Addiction 2019, 114, 1095–1109. [Google Scholar] [CrossRef] [PubMed]
- Fusar-Poli, P.; Solmi, M.; Brondino, N.; Davies, C.; Chae, C.; Politi, P.; McGuire, P. Transdiagnostic psychiatry: A systematic review. World Psychiatry 2019, 18, 192–207. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Hodgins, D.C. A review of the evidence for considering gambling disorder (and other behavioral addictions) as a disorder due to addictive behaviors in the ICD-11: A focus on case-control studies. Curr. Addict. Rep. 2019, 6, 273–295. [Google Scholar] [CrossRef]
- Shaffer, H.J.; Tom, M.A.; Wiley, R.C.; Wong, M.F.; Chan, E.M.; Cheng, G.L.; Lo, C.K.M.; Ma, E.K.; Wong, R.H.; Lee, M. Using the Syndrome Model of Addiction: A preliminary consideration of psychological states and traits. Int. J. Ment. Health Addict. 2018, 16, 1373–1393. [Google Scholar] [CrossRef]
- Blanco, C.; Iza, M.; Rodríguez-Fernández, J.M.; Baca-García, E.; Wang, S.; Olfson, M. Probability and predictors of treatment-seeking for substance use disorders in the US. Drug Alcohol Depend. 2015, 149, 136–144. [Google Scholar] [CrossRef]
- Hodgins, D.C.; Stea, J.N.; Grant, J.E. Gambling disorders. Lancet 2011, 378, 1874–1884. [Google Scholar] [CrossRef]
- Billieux, J.; Schimmenti, A.; Khazaal, Y.; Maurage, P.; Heeren, A. Are we overpathologizing everyday life? A tenable blueprint for behavioral addiction research. J. Behav. Addict. 2015, 4, 119–123. [Google Scholar] [CrossRef]
- Kaptsis, D.; King, D.L.; Delfabbro, P.H.; Gradisar, M. Withdrawal symptoms in Internet gaming disorder: A systematic review. Clin. Psychol. Rev. 2016, 43, 58–66. [Google Scholar] [CrossRef]
- Kardefelt-Winther, D.; Heeren, A.; Schimmenti, A.; van Rooij, A.; Maurage, P.; Carras, M.; Edman, J.; Blaszczynski, A.; Khazaal, Y.; Billieux, J. How can we conceptualize behavioural addiction without pathologizing common behaviours? Addiction 2017, 112, 1709–1715. [Google Scholar] [CrossRef]
- Delfabbro, P.; Thomas, A.; Armstrong, A. Gender differences in the presentation of observable risk indicators of problem gambling. J. Gambl. Stud. 2018, 34, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Davison, C.; Smith, G.D.; Frankel, S. Lay epidemiology and the prevention paradox: The implications of coronary candidacy for health education. Sociol. Health Illn. 1991, 13, 1–19. [Google Scholar] [CrossRef]
- Lovatt, M.; Eadie, D.; Meier, P.S.; Li, J.; Bauld, L.; Hastings, G.; Holmes, J. Lay epidemiology and the interpretation of low-risk drinking guidelines by adults in the United Kingdom. Addiction 2015, 110, 1912–1919. [Google Scholar] [CrossRef]
- Schluter, M.G.; Hodgins, D.C.; Wolfe, J.; Wild, T.C. Can one simple questionnaire assess substance-related and behavioural addiction problems? Results of a proposed new screener for community epidemiology. Addiction 2018, 113, 1528–1537. [Google Scholar] [CrossRef] [PubMed]
- Konkoly Thege, B.; Colman, I.; el-Guebaly, N.; Hodgins, D.C.; Patten, S.B.; Schopflocher, D.; Wolfe, J.; Wild, T.C. Social judgments of behavioral versus substance-related addictions: A population-based study. Addict. Behav. 2015, 42, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Konkoly Thege, B.; Colman, I.; el-Guebaly, N.; Hodgins, D.C.; Patten, S.B.; Schopflocher, D.; Wolfe, J.; Wild, T.C. Substance-related and behavioural addiction problems: Two surveys of Canadian adults. Addict. Res. Theory 2015, 23, 34–42. [Google Scholar] [CrossRef]
- Elo, S.; Kyngäs, H. The qualitative content analysis process. J. Adv. Nurs. 2008, 62, 107–115. [Google Scholar] [CrossRef]
- Wozniak, L.; Prakash, M.; Taylor, M.; Wild, T.C. Everybody’s got it, but…: Situational and strategic participation in normalized HCV discourse among injection drug users in Edmonton, Canada. Int. J. Drug Policy 2007, 18, 388–396. [Google Scholar] [CrossRef]
- Gwet, K.L. Computing inter-rater reliability and its variance in the presence of high agreement. Br. J. Math. Stat. Psychol. 2008, 61, 29–48. [Google Scholar] [CrossRef]
- Allsopp, K.; Read, J.; Corcoran, R.; Kinderman, P. Heterogeneity in psychiatric diagnostic classification. Psychiatry Res. 2019, 279, 15–22. [Google Scholar] [CrossRef]
- Maj, M. Why the clinical utility of diagnostic categories in psychiatry is intrinsically limited and how we can use new approaches to complement them. World Psychiatry 2018, 17, 121–122. [Google Scholar] [CrossRef] [PubMed]
- Sussman, S.; Lisha, N.; Griffiths, M. Prevalence of the addictions: A problem of the majority or the minority? Eval. Health Prof. 2011, 34, 3–56. [Google Scholar] [CrossRef] [PubMed]
- Kasza, K.A.; Ambrose, B.K.; Conway, K.P.; Borek, N.; Taylor, K.; Goniewicz, M.L.; Cummings, K.M.; Sharma, E.; Pearson, J.L.; Green, V.R.; et al. Tobacco-product use by adults and youths in the United States in 2013 and 2014. N. Engl. J. Med. 2017, 376, 342–353. [Google Scholar] [CrossRef] [PubMed]
- Petry, N.M.; Zajac, K.; Ginley, M.K. Behavioral addictions as mental disorders: To be or not to be? Annu. Rev. Clin. Psychol. 2018, 14, 399–423. [Google Scholar] [CrossRef]
- Peracchia, S.; Curcio, G. Exposure to video games: Effects on sleep and on post-sleep cognitive abilities. A sistematic review of experimental evidences. Sleep Sci. 2018, 11, 302–314. [Google Scholar] [CrossRef]
- De Mattos, C.N.; Kim, H.S.; Lacroix, E.; Requião, M.; Filomensky, T.Z.; Hodgins, D.C.; Tavares, H. The need to consume: Hoarding as a shared psychological feature of compulsive buying and binge eating. Compr. Psychiatry 2018, 85, 67–71. [Google Scholar] [CrossRef]
- Widyanto, L.; Griffiths, M.D.; Brunsden, V. A psychometric comparison of the Internet Addiction Test, the Internet-Related Problem Scale, and self-diagnosis. Cyberpsychol. Behav. Soc. Netw. 2011, 14, 141–149. [Google Scholar] [CrossRef]
| Main Category | Subcategories |
|---|---|
| Behavioral Signs (4.7%): Behaviors that point to issues or signs of a problem. |
|
| Deception (2.6%): Engaging in efforts to hide addiction from others. | (no subcategories) |
| Dependence (30.1%): Signs and symptoms that reflect DSM-5 conceptualization of addictions and purported hallmark symptoms of addictions. |
|
| Financial Harms (5.2%): Financial difficulties as a result of addiction. |
|
| Health Harms (3.3%): Harms to health and well-being. |
|
| Interferes with Life (3.7%): Addiction starts to affect daily living. | (no subcategories) |
| Interpersonal Harms (3.8%): Hurting relationships with others. |
|
| Narrowing of Repertoire (1.8%): When life becomes all about the addiction. | (no subcategories) |
| Patterns of Use (21.0%): Qualities or descriptions of how someone engages in the addiction. |
|
| Physical Signs (9.8%): Physical signs that point to problems with substance or behavior. |
|
| Psychological Harms (7.9%): Negative psychological consequences. |
|
| Rationalization (1.1%): Lack of awareness that one has an addiction or resistance to the idea that there is an addiction. |
|
| Workplace or School Harms (0.9%): Negative consequences to professional life or wellbeing. | (no subcategories) |
| Don’t Know (2.9%): Participants reporting they do not know or are unsure about the most important symptom of addiction | (no subcategories) |
| Other (1.3%): Responses that are not categorizable into any existing categories, but are not considered to be uncodable | (no subcategories) |
| Uncodable: Vague, unclear, blank, or nonsense, responses | (no subcategories) |
| No Personal Experience with Addiction (n = 900) | Past 12-Month (Current) Personal Experience with Addiction (n = 1562) | Lifetime Personal Experience with Addiction (n = 1041) | Test | p | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristics | N | % | M (SD) | N | % | M (SD) | N | % | M (SD) | ||
| Age | 49.8 (15.0) | 47.7 (13.8) | 52.3 (14.8) | F = 31.39 | <0.001 | ||||||
| Gender | χ2 =4.80 | 0.910 | |||||||||
| Male | 378 | 42.1 | 647 | 41.1 | 475 | 45.6 | |||||
| Female | 520 | 57.9 | 915 | 58.6 | 566 | 54.4 | |||||
| Marital Status | χ2 = 19.45 | <0.001 | |||||||||
| Married/Stable partner | 617 | 68.7 | 944 | 60.4 | 696 | 66.9 | |||||
| Single | 277 | 30.8 | 604 | 38.7 | 340 | 32.7 | |||||
| Employment Status | χ2 = 98.48 | <0.001 | |||||||||
| Full time employment | 452 | 50.3 | 814 | 52.1 | 483 | 46.4 | |||||
| Part time employment | 112 | 12.5 | 164 | 10.5 | 116 | 11.1 | |||||
| Unemployed | 37 | 4.1 | 97 | 6.2 | 38 | 3.7 | |||||
| Student | 23 | 2.6 | 53 | 3.4 | 28 | 2.7 | |||||
| Retired | 198 | 22.0 | 261 | 16.7 | 306 | 29.4 | |||||
| Not working due to disability | 18 | 2.0 | 93 | 6.0 | 26 | 2.5 | |||||
| Other | 52 | 5.8 | 70 | 4.5 | 39 | 3.7 | |||||
| Education | χ2 = 49.09 | <0.001 | |||||||||
| Less than high school | 29 | 3.2 | 86 | 5.5 | 36 | 3.5 | |||||
| High school | 121 | 13.5 | 266 | 17.0 | 160 | 15.4 | |||||
| Some university | 157 | 17.5 | 395 | 25.3 | 240 | 23.1 | |||||
| University undergraduate degree/college technical diploma | 467 | 52.0 | 657 | 42.1 | 471 | 45.2 | |||||
| University graduate or professional degree | 119 | 13.3 | 155 | 9.9 | 133 | 12.8 | |||||
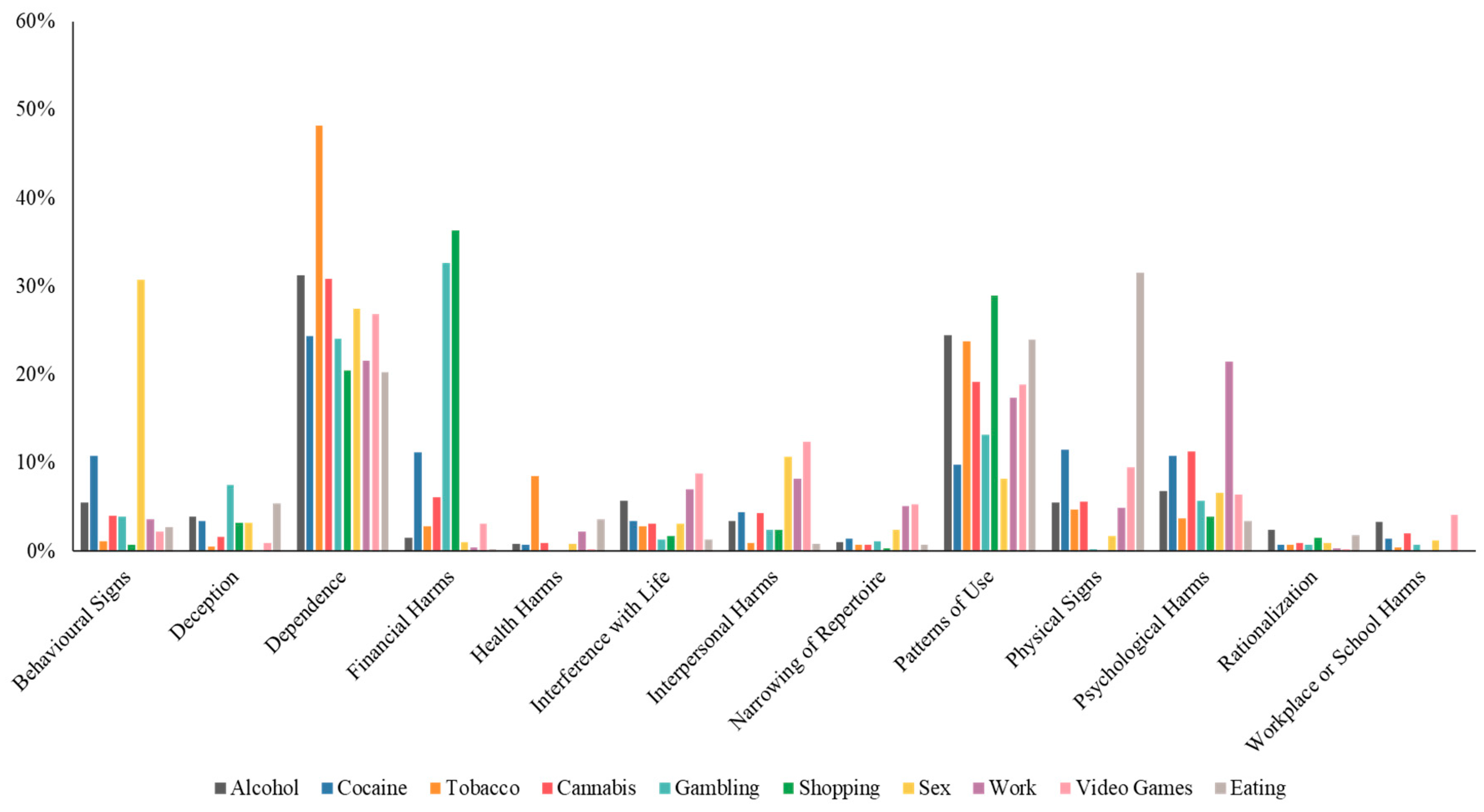
| Alcohol | Cocaine | Tobacco | Cannabis | Gambling | Shopping | Sex | Work | Video Games | Eating | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Dependence | 31.3% | 24.3% | 48.2% | 30.8% | 24.0% | 20.5% | 27.4% | 21.5% | 26.8% | 20.2% | 30.1% |
| Patterns of Use | 24.4% | 9.8% | 23.8% | 19.2% | 13.2% | 29.0% | 8.2% | 17.4% | 18.9% | 24.0% | 21.0% |
| Physical Signs | 5.5% | 11.5% | 4.7% | 5.6% | 0.2% | 0.0% | 1.7% | 4.9% | 9.5% | 31.5% | 9.8% |
| Psychological Harms | 6.8% | 10.8% | 3.7% | 11.3% | 5.7% | 3.9% | 6.6% | 21.4% | 6.4% | 3.4% | 7.9% |
| Financial Harms | 1.5% | 11.2% | 2.8% | 6.1% | 32.7% | 36.3% | 1.0% | 0.4% | 3.1% | 0.2% | 5.2% |
| Behavioral Signs | 5.5% | 10.8% | 1.1% | 3.9% | 3.9% | 0.7% | 30.7% | 3.5% | 2.2% | 2.7% | 4.7% |
| Interpersonal Harms | 3.4% | 4.4% | 0.9% | 4.3% | 2.4% | 1.0% | 10.7% | 8.2% | 12.4% | 0.8% | 3.8% |
| Interferes with Life | 5.7% | 3.4% | 2.8% | 3.1% | 1.3% | 1.7% | 3.1% | 7.0% | 8.8% | 1.3% | 3.7% |
| Health Harms | 0.8% | 0.7% | 8.4% | 0.9% | 0.0% | 0.0% | 0.8% | 2.2% | 0.2% | 3.6% | 3.3% |
| Deception | 3.9% | 3.4% | 0.5% | 1.6% | 7.5% | 3.2% | 3.2% | 0.1% | 0.9% | 5.4% | 2.6% |
| Narrowing of Repertoire | 1.0% | 1.4% | 0.7% | 0.7% | 1.1% | 0.3% | 2.4% | 5.1% | 5.3% | 0.7% | 1.8% |
| Rationalization | 2.4% | 0.7% | 0.7% | 0.9% | 0.7% | 1.5% | 0.9% | 0.3% | 0.2% | 1.8% | 1.1% |
| Workplace or School Harms | 3.3% | 1.4% | 0.4% | 2.0% | 0.7% | 0.1% | 1.2% | 0.0% | 4.1% | 0.1% | 0.9% |
| Substances | Behaviors | χ2 | p | |
|---|---|---|---|---|
| Behavioral Signs | 3.2% | 5.8% | 50.01 | <0.001 |
| Deception | 1.7% | 3.2% | 25.78 | <0.001 |
| Dependence | 40.4% | 22.2% | 490.58 | <0.001 |
| Financial Harms | 3.2% | 6.6% | 74.74 | <0.001 |
| Health Harms | 5.1% | 2.0% | 95.02 | <0.001 |
| Interferes with Life | 3.7% | 3.8% | 0.16 | 0.693 |
| Interpersonal Harms | 2.2% | 5.1% | 74.61 | <0.001 |
| Narrowing of Repertoire | 0.8% | 2.5% | 51.24 | <0.001 |
| Patterns of Use | 22.7% | 19.6% | 18.65 | <0.001 |
| Physical Signs | 5.4% | 13.2% | 216.50 | <0.001 |
| Psychological Harms | 5.7% | 9.5% | 61.19 | <0.001 |
| Rationalization | 1.2% | 1.0% | 0.84 | 0.358 |
| Workplace or School Harms | 1.4% | 0.6% | 25.18 | <0.001 |
| Indicators | Themes | % Responses | |
|---|---|---|---|
| Alcohol | Dependence | Not knowing when to stop | 0.3% |
| Physical signs | Hangovers | 0.4% | |
| Impaired motor coordination | 0.6% | ||
| Passing out | 0.3% | ||
| Speech impairment | 0.6% | ||
| Video Games | Patterns of use | Playing all night | 0.5% |
| Psychological harms | Unreality | 1.9% | |
| Cocaine | Physical signs | Nose issues | 2.7% |
| Eating | Health harms | Diabetes | 0.2% |
| Digestive issues | 0.1% | ||
| High cholesterol | 0.04% | ||
| Patterns of use | Unhealthy eating habits | 2.4% | |
| Eating without hunger | 2.7% | ||
| Psychological harms | Use as a reward | 0.04% | |
| Sex | Behavioral signs | Masturbation | 0.8% |
| Promiscuity and indiscriminate behavior | 11.5% | ||
| Interpersonal harms | Romantic problems and infidelity | 5.0% | |
| Physical signs | Difficulty having sex | 0.6% | |
| Erectile problems | 0.5% | ||
| Psychological harms | Lack of sexual pleasure | 0.5% | |
| Pornography interferes with sex life | 0.4% | ||
| Shopping | Patterns of use | Hoarding and clutter | 6.8% |
| Unnecessary purchases | 14.7% | ||
| Tobacco | Dependence | Smoking despite dislike | 0.2% |
| Smoking in cold weather | 0.9% | ||
| Physical signs | Yellowing of fingers and nails | 2.4% | |
| Gambling | Patterns of use | Chasing losses | 1.5% |
| Re-betting winnings | 0.7% | ||
| Cannabis | Psychological harms | Lack of motivation | 2.2.% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, H.S.; Hodgins, D.C.; Kim, B.; Wild, T.C. Transdiagnostic or Disorder Specific? Indicators of Substance and Behavioral Addictions Nominated by People with Lived Experience. J. Clin. Med. 2020, 9, 334. https://doi.org/10.3390/jcm9020334
Kim HS, Hodgins DC, Kim B, Wild TC. Transdiagnostic or Disorder Specific? Indicators of Substance and Behavioral Addictions Nominated by People with Lived Experience. Journal of Clinical Medicine. 2020; 9(2):334. https://doi.org/10.3390/jcm9020334
Chicago/Turabian StyleKim, Hyoun S., David C. Hodgins, Benjamin Kim, and T. Cameron Wild. 2020. "Transdiagnostic or Disorder Specific? Indicators of Substance and Behavioral Addictions Nominated by People with Lived Experience" Journal of Clinical Medicine 9, no. 2: 334. https://doi.org/10.3390/jcm9020334
APA StyleKim, H. S., Hodgins, D. C., Kim, B., & Wild, T. C. (2020). Transdiagnostic or Disorder Specific? Indicators of Substance and Behavioral Addictions Nominated by People with Lived Experience. Journal of Clinical Medicine, 9(2), 334. https://doi.org/10.3390/jcm9020334





