Inclination Changes in Incisors During Orthodontic Treatment with Passive Self-Ligating Brackets
Abstract
:1. Introduction
2. Materials and Methods
2.1. Cephalometric Measurements
2.2. Statistics
2.3. Characteristics of the Study Group
3. Results
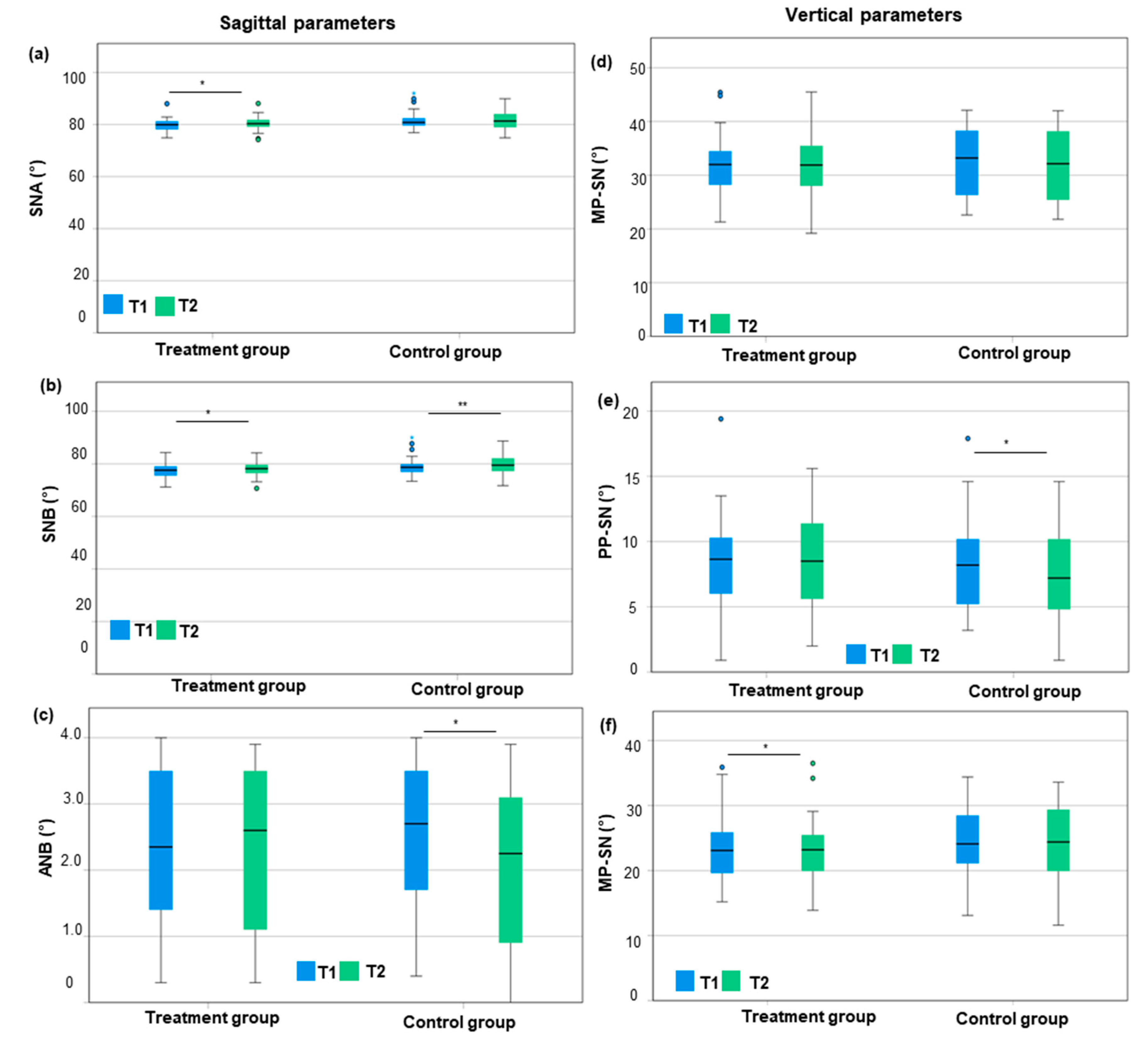
3.1. Sagittal and Vertical Parameters
3.2. Inclination of the Upper and Lower Incisors
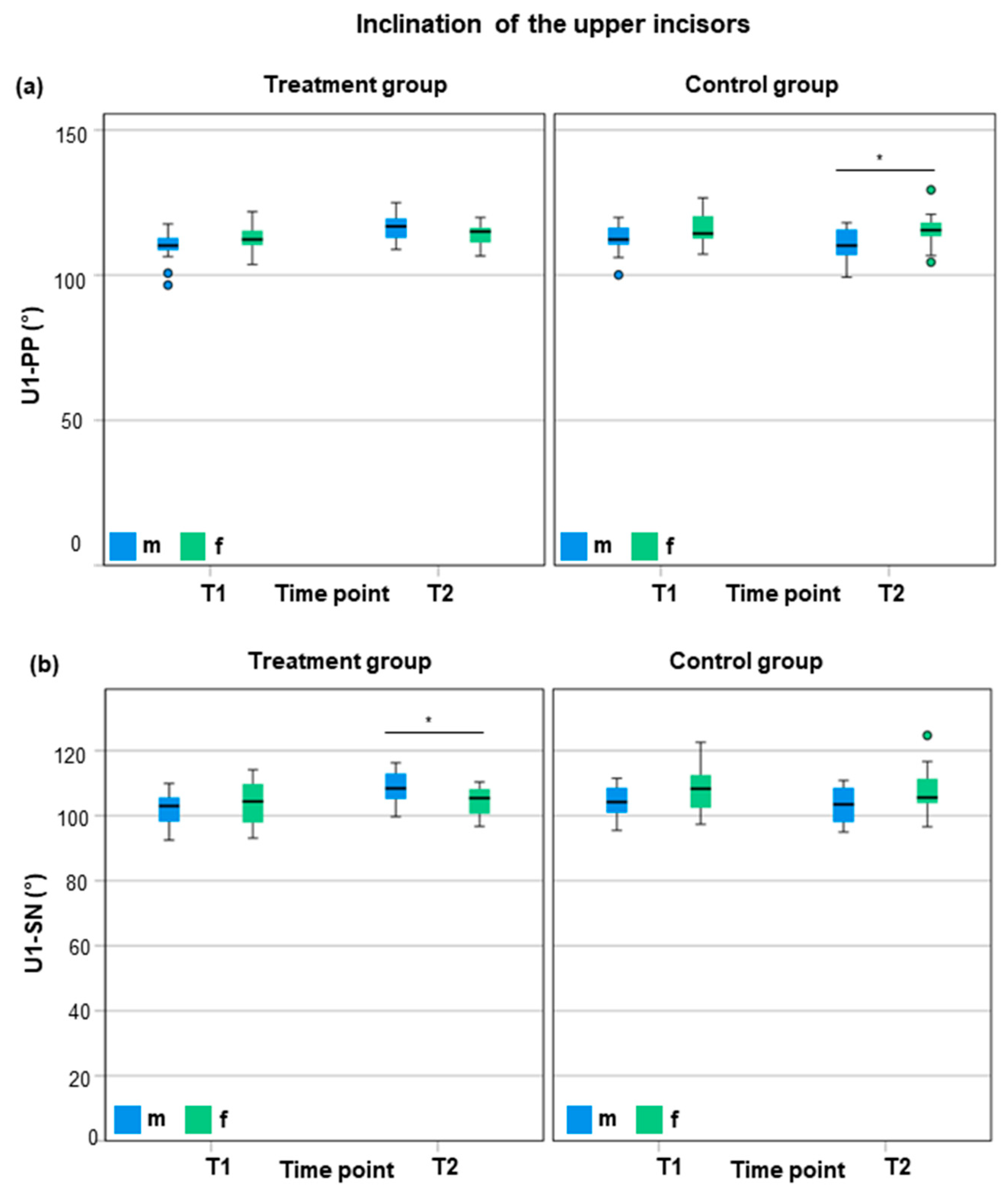
3.3. Sex-Specific Characteristics
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Andrews, L.F. The six keys to normal occlusion. Am. J. Orthod. 1972, 62, 296–309. [Google Scholar] [CrossRef] [PubMed]
- Capelozza Filho, L.; Silva Filho, O.; Ozawaka, T.; Cavassan, A. Brackets individualization in straight-wire technique: Concepts review and suggestions for prescribed use. Rev. Dent. Press Ortod. Ortop. Facial 1999, 4, 78–106. [Google Scholar]
- Burke, S.P.; Silveira, A.M.; Goldsmith, L.J.; Yancey, J.M.; Van Stewart, A.; Scarfe, W.C. A meta-analysis of mandibular intercanine width in treatment and postretention. Angle Orthod. 1998, 68, 53–60. [Google Scholar] [CrossRef] [PubMed]
- Glenn, G.; Sinclair, P.M.; Alexander, R.G. Nonextraction orthodontic therapy: Posttreatment dental and skeletal stability. Am. J. Orthod. Dentofac. Orthop. 1987, 92, 321–328. [Google Scholar] [CrossRef]
- Little, R.M. Stability and relapse of mandibular anterior alignment: University of Washington studies. Semin. Orthod. 1999, 5, 191–204. [Google Scholar] [CrossRef]
- Mills, J.R. The long-term results of the proclination of lower incisors. Br. Dent. J. 1966, 120, 355–363. [Google Scholar] [PubMed]
- Brin, I.; Ben-Bassat, Y.; Heling, I.; Brezniak, N. Profile of an orthodontic patient at risk of dental trauma. Endod. Dent. Traumatol. 2000, 16, 111–115. [Google Scholar] [CrossRef]
- Petti, S.; Tarsitani, G. Traumatic injuries to anterior teeth in Italian schoolchildren: Prevalence and risk factors. Endod. Dent. Traumatol. 1996, 12, 294–297. [Google Scholar] [CrossRef]
- Batista, K.B.; Thiruvenkatachari, B.; Harrison, J.E.; O’Brien, K.D. Orthodontic treatment for prominent upper front teeth (Class II malocclusion) in children and adolescents. Cochrane Database Syst. Rev. 2018, 3, CD003452. [Google Scholar] [CrossRef]
- Seidel, C.L.; Lipp, J.; Dotzer, B.; Janjic Rankovic, M.; Mertmann, M.; Wichelhaus, A.; Sabbagh, H. Investigation of Forces and Moments during Orthodontic Tooth Intrusion Using Robot Orthodontic Measurement and Simulation System (ROSS). Bioengineering 2023, 10, 1356. [Google Scholar] [CrossRef]
- Dotzer, B.; Stocker, T.; Wichelhaus, A.; Janjic Rankovic, M.; Sabbagh, H. Biomechanical simulation of forces and moments of initial orthodontic tooth movement in dependence on the used archwire system by ROSS (Robot Orthodontic Measurement & Simulation System). J. Mech. Behav. Biomed. Mater. 2023, 144, 105960. [Google Scholar] [CrossRef]
- Maizeray, R.; Wagner, D.; Lefebvre, F.; Levy-Benichou, H.; Bolender, Y. Is there any difference between conventional, passive and active self-ligating brackets? A systematic review and network meta-analysis. Int. Orthod. 2021, 19, 523–538. [Google Scholar] [CrossRef]
- Stolzenberg, J. The Russell attachment and its improved advantages. Int. J. Orthod. Dent. Child. 1935, 21, 837–840. [Google Scholar] [CrossRef]
- Gottlieb, E.L.; Wildman, A.J.; Hice, T.L.; Lang, H.M.; Lee, I.F.; Strauch, E.C., Jr. The Edgelok bracket. J. Clin. Orthod. 1972, 6, 613–623 passim. [Google Scholar] [PubMed]
- Hanson, G.H. The SPEED system: A report on the development of a new edgewise appliance. Am. J. Orthod. 1980, 78, 243–265. [Google Scholar] [CrossRef]
- Damon, D.H. The Damon low-friction bracket: A biologically compatible straight-wire system. J. Clin. Orthod. 1998, 32, 670–680. [Google Scholar] [PubMed]
- Damon, D.H. The rationale, evolution and clinical application of the self-ligating bracket. Clin. Orthod. Res. 1998, 1, 52–61. [Google Scholar] [CrossRef]
- Harradine, N.W. Self-ligating brackets: Where are we now? J. Orthod. 2003, 30, 262–273. [Google Scholar] [CrossRef]
- Brauchli, L.M.; Steineck, M.; Wichelhaus, A. Active and passive self-ligation: A myth? Part 1: Torque control. Angle Orthod. 2012, 82, 663–669. [Google Scholar] [CrossRef]
- Berger, J.L. The SPEED System: An Overview of the Appliance and Clinical Performance. Semin. Orthod. 2008, 14, 54–63. [Google Scholar] [CrossRef]
- Pizzoni, L.; Ravnholt, G.; Melsen, B. Frictional forces related to self-ligating brackets. Eur. J. Orthod. 1998, 20, 283–291. [Google Scholar] [CrossRef] [PubMed]
- Wichelhaus, A.; Guggenbühl, S.; Hotzel, L.; Seidel, C.L.; Sabbagh, H.; Hoffmann, L. Comparing Torque Transmission of Different Bracket Systems in Combination with Various Archwires Considering Play in the Bracket Slot: An In Vitro Study. Materials 2024, 17, 684. [Google Scholar] [CrossRef] [PubMed]
- Wichelhaus, A.; Geserick, M.; Hibst, R.; Sander, F.G. The effect of surface treatment and clinical use on friction in NiTi orthodontic wires. Dent. Mater. 2005, 21, 938–945. [Google Scholar] [CrossRef] [PubMed]
- Wichelhaus, A.; Eichenberg, T.; Gruber, P.; Bamidis, E.P.; Stocker, T. Friction Force Adjustment by an Innovative Covering System Applied with Superelastic NiTi Brackets and Wires-An In-Vitro Study. Materials 2022, 15, 4248. [Google Scholar] [CrossRef]
- Stocker, T.; Li, H.; Bamidis, E.P.; Baumert, U.; Hoffmann, L.; Wichelhaus, A.; Sabbagh, H. Influence of normal forces on the frictional behavior in tribological systems made of different bracket types and wire dimensions. Dent. Mater. J. 2022, 41, 402–413. [Google Scholar] [CrossRef]
- Dragomirescu, A.O.; Bencze, M.A.; Vasilache, A.; Teodorescu, E.; Albu, C.C.; Popoviciu, N.O.; Ionescu, E. Reducing Friction in Orthodontic Brackets: A Matter of Material or Type of Ligation Selection? In-Vitro Comparative Study. Materials 2022, 15, 2640. [Google Scholar] [CrossRef]
- Gomez, S.L.; Montoya, Y.; Garcia, N.L.; Virgen, A.L.; Botero, J.E. Comparison of frictional resistance among conventional, active and passive selfligating brackets with different combinations of arch wires: A finite elements study. Acta Odontol. Latinoam. 2016, 29, 130–136. [Google Scholar]
- Faizee, K.S.H.; Thomas, S.; Krishnaswamy, N.R. Frictional characteristics of active and passive self-ligation bracket systems: An in vitro study. J. Indian Orthod. Soc. 2011, 45, 154–159. [Google Scholar] [CrossRef]
- Vartolomei, A.C.; Serbanoiu, D.C.; Ghiga, D.V.; Moldovan, M.; Cuc, S.; Pollmann, M.C.F.; Pacurar, M. Comparative Evaluation of Two Bracket Systems’ Kinetic Friction: Conventional and Self-Ligating. Materials 2022, 15, 4304. [Google Scholar] [CrossRef]
- Szczupakowski, A.; Reimann, S.; Dirk, C.; Keilig, L.; Weber, A.; Jager, A.; Bourauel, C. Friction behavior of self-ligating and conventional brackets with different ligature systems. J. Orofac. Orthop. 2016, 77, 287–295. [Google Scholar] [CrossRef]
- Yang, X.; He, Y.; Chen, T.; Zhao, M.; Yan, Y.; Wang, H.; Bai, D. Differences between active and passive self-ligating brackets for orthodontic treatment: Systematic review and meta-analysis based on randomized clinical trials. J. Orofac. Orthop. 2017, 78, 121–128. [Google Scholar] [CrossRef] [PubMed]
- Jacobs, C.; Gebhardt, P.F.; Jacobs, V.; Hechtner, M.; Meila, D.; Wehrbein, H. Root resorption, treatment time and extraction rate during orthodontic treatment with self-ligating and conventional brackets. Head Face Med. 2014, 10, 2. [Google Scholar] [CrossRef]
- Cattaneo, P.M.; Salih, R.A.; Melsen, B. Labio-lingual root control of lower anterior teeth and canines obtained by active and passive self-ligating brackets. Angle Orthod. 2013, 83, 691–697. [Google Scholar] [CrossRef]
- Pandis, N.; Polychronopoulou, A.; Makou, M.; Eliades, T. Mandibular dental arch changes associated with treatment of crowding using self-ligating and conventional brackets. Eur. J. Orthod. 2010, 32, 248–253. [Google Scholar] [CrossRef]
- Fleming, P.S.; DiBiase, A.T.; Sarri, G.; Lee, R.T. Comparison of mandibular arch changes during alignment and leveling with 2 preadjusted edgewise appliances. Am. J. Orthod. Dentofac. Orthop. 2009, 136, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Hegele, J.; Seitz, L.; Claussen, C.; Baumert, U.; Sabbagh, H.; Wichelhaus, A. Clinical effects with customized brackets and CAD/CAM technology: A prospective controlled study. Prog. Orthod. 2021, 22, 40. [Google Scholar] [CrossRef]
- Atik, E.; Akarsu-Guven, B.; Kocadereli, I.; Ciger, S. Evaluation of maxillary arch dimensional and inclination changes with self-ligating and conventional brackets using broad archwires. Am. J. Orthod. Dentofac. Orthop. 2016, 149, 830–837. [Google Scholar] [CrossRef]
- Little, R.M. The irregularity index: A quantitative score of mandibular anterior alignment. Am. J. Orthod. 1975, 68, 554–563. [Google Scholar] [CrossRef] [PubMed]
- Segner, D.; Hasund, A. Individualisierte Kephalometrie. Segner, D., Ed.; Segner: Monheim am Rhein, Germany, 1998. [Google Scholar]
- American Association of Orthodontics Foundation (AAOF). Craniofacial Growth Legacy Collections Project. Available online: https://www.aaoflegacycollection.org/aaof_home.html (accessed on 16 June 2024).
- Perini, T.A.; Oliveira, G.L.d.; Ornellas, J.d.S.; Oliveira, F.P.d. Technical error of measurement in anthropometry (english version). Rev. Bras. Med. Esporte 2005, 11, 86–90. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef]
- Ciavarella, D.; Tepedino, M.; Gallo, C.; Montaruli, G.; Zhurakivska, K.; Coppola, L.; Troiano, G.; Chimenti, C.; Laurenziello, M.; Lo Russo, L. Post-orthodontic position of lower incisors and gingival recession: A retrospective study. J. Clin. Exp. Dent. 2017, 9, e1425–e1430. [Google Scholar] [CrossRef] [PubMed]
- Lo Russo, L.; Zhurakivska, K.; Montaruli, G.; Salamini, A.; Gallo, C.; Troiano, G.; Ciavarella, D. Effects of crown movement on periodontal biotype: A digital analysis. Odontology 2018, 106, 414–421. [Google Scholar] [CrossRef]
- Bartz, D.; Chitnis, T.; Kaiser, U.B.; Rich-Edwards, J.W.; Rexrode, K.M.; Pennell, P.B.; Goldstein, J.M.; O’Neal, M.A.; LeBoff, M.; Behn, M.; et al. Clinical Advances in Sex- and Gender-Informed Medicine to Improve the Health of All: A Review. JAMA Intern. Med. 2020, 180, 574–583. [Google Scholar] [CrossRef]
- Regitz-Zagrosek, V.; Gebhard, C. Gender medicine: Effects of sex and gender on cardiovascular disease manifestation and outcomes. Nat. Rev. Cardiol. 2023, 20, 236–247. [Google Scholar] [CrossRef] [PubMed]
- Pancherz, H.; Hägg, U. Dentofacial orthopedics in relation to somatic maturation. An analysis of 70 consecutive cases treated with the Herbst appliance. Am. J. Orthod. 1985, 88, 273–287. [Google Scholar] [CrossRef]
- Malmgren, O.; Omblus, J.; Hägg, U.; Pancherz, H. Treatment with an orthopedic appliance system in relation to treatment intensity and growth periods. A study of initial effects. Am. J. Orthod. Dentofac. Orthop. 1987, 91, 143–151. [Google Scholar] [CrossRef]
- McKinney, J.R.; Harris, E.F. Influence of patient age and sex on orthodontic treatment: Evaluations of Begg lightwire, standard edgewise, and straightwire techniques. Am. J. Orthod. Dentofac. Orthop. 2001, 120, 530–541. [Google Scholar] [CrossRef] [PubMed]
- Wichelhaus, A.; Sander, F.G. The dental and skeletal effects of the jumping-the-bite plate and high-pull headgear combination. A clinical study of treated patients. Fortschr. Kieferorthop. 1995, 56, 202–215. [Google Scholar] [CrossRef]
- Martina, R.; Cioffi, I.; Galeotti, A.; Tagliaferri, R.; Cimino, R.; Michelotti, A.; Valletta, R.; Farella, M.; Paduano, S. Efficacy of the Sander bite-jumping appliance in growing patients with mandibular retrusion: A randomized controlled trial. Orthod. Craniofac. Res. 2013, 16, 116–126. [Google Scholar] [CrossRef]
- Albarakati, S.F.; Kula, K.S.; Ghoneima, A.A. The reliability and reproducibility of cephalometric measurements: A comparison of conventional and digital methods. Dentomaxillofac. Radiol. 2012, 41, 11–17. [Google Scholar] [CrossRef]
- Goracci, C.; Ferrari, M. Reproducibility of measurements in tablet-assisted, PC-aided, and manual cephalometric analysis. Angle Orthod. 2014, 84, 437–442. [Google Scholar] [CrossRef]
- Navarro Rde, L.; Oltramari-Navarro, P.V.; Fernandes, T.M.; Oliveira, G.F.; Conti, A.C.; Almeida, M.R.; Almeida, R.R. Comparison of manual, digital and lateral CBCT cephalometric analyses. J. Appl. Oral Sci. 2013, 21, 167–176. [Google Scholar] [CrossRef]
- Polat-Ozsoy, O.; Gokcelik, A.; Toygar Memikoglu, T.U. Differences in cephalometric measurements: A comparison of digital versus hand-tracing methods. Eur. J. Orthod. 2009, 31, 254–259. [Google Scholar] [CrossRef]
- Yu, S.H.; Nahm, D.S.; Baek, S.H. Reliability of landmark identification on monitor-displayed lateral cephalometric images. Am. J. Orthod. Dentofac. Orthop. 2008, 133, 790.e791–796; discussion e791. [Google Scholar] [CrossRef] [PubMed]
- Sommer, T.; Ciesielski, R.; Erbersdobler, J.; Orthuber, W.; Fischer-Brandies, H. Precision of cephalometric analysis via fully and semiautomatic evaluation of digital lateral cephalographs. Dentomaxillofac. Radiol. 2009, 38, 401–406. [Google Scholar] [CrossRef]
- Houston, W.J.; Maher, R.E.; McElroy, D.; Sherriff, M. Sources of error in measurements from cephalometric radiographs. Eur. J. Orthod. 1986, 8, 149–151. [Google Scholar] [CrossRef] [PubMed]
- Kamoen, A.; Dermaut, L.; Verbeeck, R. The clinical significance of error measurement in the interpretation of treatment results. Eur. J. Orthod. 2001, 23, 569–578. [Google Scholar] [CrossRef] [PubMed]
- Cooke, M.S.; Wei, S.H. Cephalometric errors: A comparison between repeat measurements and retaken radiographs. Aust. Dent. J. 1991, 36, 38–43. [Google Scholar] [CrossRef]
- Talari, K.; Goyal, M. Retrospective studies—Utility and caveats. J. R. Coll. Phys. Edinb. 2020, 50, 398–402. [Google Scholar] [CrossRef]
- Gribel, B.F.; Gribel, M.N.; Frazäo, D.C.; McNamara, J.A., Jr.; Manzi, F.R. Accuracy and reliability of craniometric measurements on lateral cephalometry and 3D measurements on CBCT scans. Angle Orthod. 2011, 81, 26–35. [Google Scholar] [CrossRef]
- Haskell, B.S.; Segal, E.S. Ethnic and ethical challenges in treatment planning: Dealing with diversity in the 21st century. Angle Orthod. 2014, 84, 380–382. [Google Scholar] [CrossRef] [PubMed]
- Hung, M.; Zakeri, G.; Su, S.; Mohajeri, A. Profile of Orthodontic Use across Demographics. Dent. J. 2023, 11, 291. [Google Scholar] [CrossRef] [PubMed]
- Tanne, K. Current status of clinical orthodontics in European and American countries. APOS Trends Orthod. 2020, 10, 204–223. [Google Scholar] [CrossRef]


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Seidel, C.L.; Baumert, U.; Ost, F.; Sabbagh, H.; Wichelhaus, A. Inclination Changes in Incisors During Orthodontic Treatment with Passive Self-Ligating Brackets. J. Clin. Med. 2025, 14, 3370. https://doi.org/10.3390/jcm14103370
Seidel CL, Baumert U, Ost F, Sabbagh H, Wichelhaus A. Inclination Changes in Incisors During Orthodontic Treatment with Passive Self-Ligating Brackets. Journal of Clinical Medicine. 2025; 14(10):3370. https://doi.org/10.3390/jcm14103370
Chicago/Turabian StyleSeidel, Corinna L., Uwe Baumert, Franziska Ost, Hisham Sabbagh, and Andrea Wichelhaus. 2025. "Inclination Changes in Incisors During Orthodontic Treatment with Passive Self-Ligating Brackets" Journal of Clinical Medicine 14, no. 10: 3370. https://doi.org/10.3390/jcm14103370
APA StyleSeidel, C. L., Baumert, U., Ost, F., Sabbagh, H., & Wichelhaus, A. (2025). Inclination Changes in Incisors During Orthodontic Treatment with Passive Self-Ligating Brackets. Journal of Clinical Medicine, 14(10), 3370. https://doi.org/10.3390/jcm14103370






