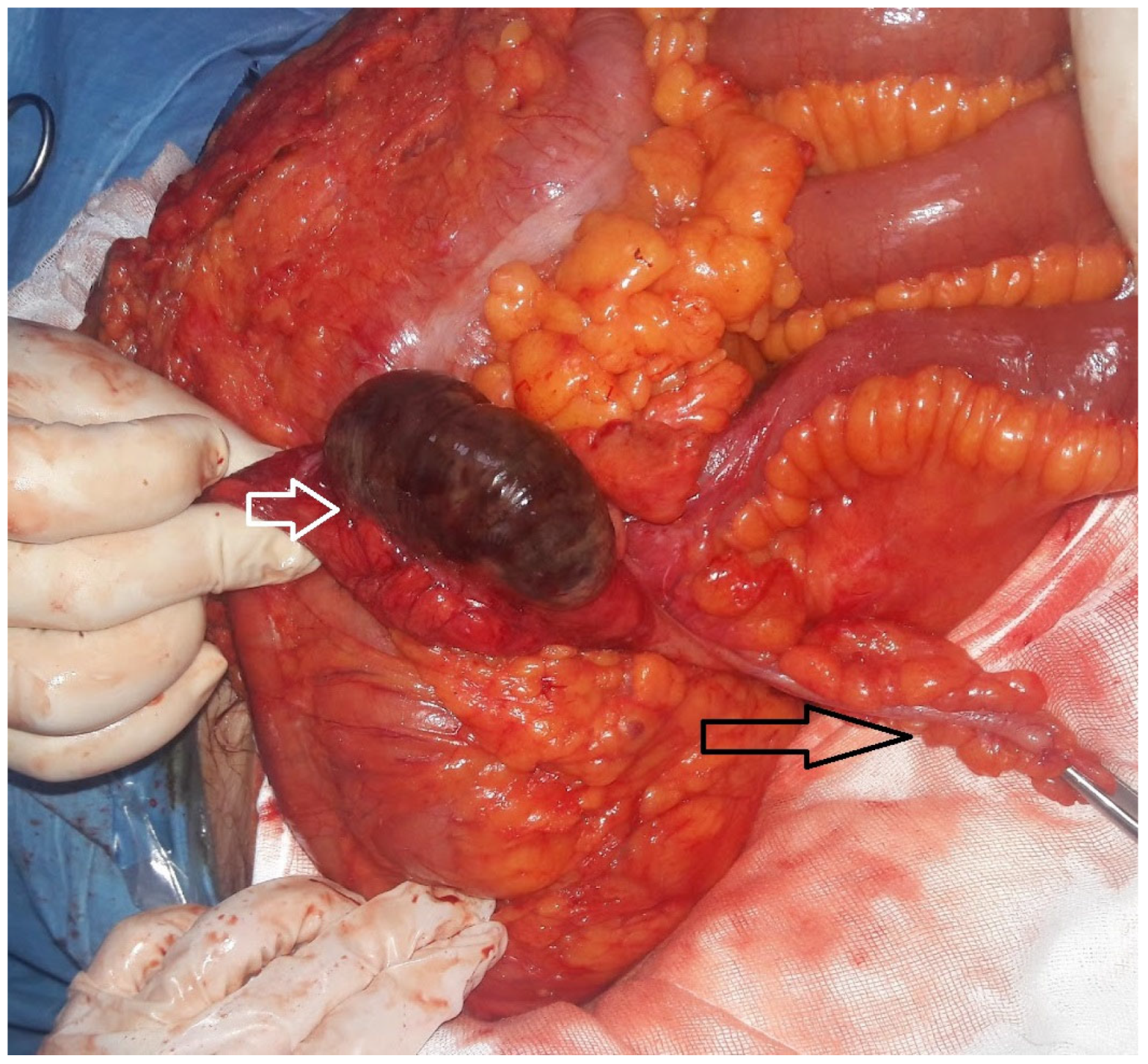
Isolated Cecal Necrosis as a Cause of Acute Abdomen
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ICN | Isolated cecum necrosis |
| ADPKD | Autosomal Polycystic Kidney Disease |
| AVF | Arteriovenous fistula |
| CAD | Coronary artery disease |
| CRF | Chronic renal failure |
| DM | Diabetes mellitus |
| CVA | Cerebrovascular accident |
| CT | Computed tomography |
| F | Female |
| g/dL | Gram per deciliter |
| Hb | Hemoglobin |
| HCT | Hematocrit |
| HT | Hypertension |
| L | Liter |
| M | Male |
| mcL | Microliter |
| PLT | Platelet |
| RLQ | Right lower quadrant pain |
| TAH | The Artificial Heart |
| USG | Ultrasonography |
| WBC | White blood |
References
- Kohga, A.; Yajima, K.; Okumura, T.; Yamashita, K.; Isogaki, J.; Suzuki, K.; Komiyama, A.; Kawabe, A. A Case of Isolated Cecal Necrosis Preoperatively Diagnosed with Perforation of Cecum. Medicina 2019, 55, 9. [Google Scholar] [CrossRef] [PubMed]
- Dirican, A.; Unal, B.; Bassulu, N.; Tatlı, F.; Aydin, C.; Kayaalp, C. Isolated Cecal Necrosis Mimicking Acute Appendicitis: A Case Series. J. Med. Case Rep. 2009, 3, 7443. [Google Scholar] [CrossRef] [PubMed]
- Çakar, E.; Ersöz, F.; Bag, M.; Bayrak, S.; Çolak, Ş.; Bektaş, H.; Güneş, M.E.; Çakar, E. Isolated cecal Necrosis: Our Surgical Experience and a Review of the Literature. Turk. J. Surg. 2014, 30, 214–218. [Google Scholar] [CrossRef] [PubMed]
- Schuler, J.G.; Hudlin, M.M. Cecal Necrosis: Infrequent variant of ischemic colitis. Report of five cases. Dis. Colon Rectum 2000, 43, 708–712. [Google Scholar] [CrossRef] [PubMed]
- Shahverdi, E.; Morshedi, M.; Oraei-Abbasian, F.; Allahverdi Khani, M.; Khodayarnejad, R. A Rare Case of Vasculitis Patched Necrosis of Cecum due to Behçet’s Disease. Case Rep. Surg. 2017, 2017, 1693737. [Google Scholar] [CrossRef] [PubMed]
- Suleimanov, V.; Shahzad, F. Partial Infarction of Cecal Wall Presenting as Acute Appendicitis. Cureus 2022, 14, e31408. [Google Scholar] [CrossRef] [PubMed]
- Janike, K.; Pan, A.; Kheirkhah, P.; Shuja, A. Isolated Cecal Necrosis Mimicking a Colonic Mass. ACG Case Rep. J. 2023, 10, e01030. [Google Scholar] [CrossRef] [PubMed]
- Liao, X.; Rex, D.K.; Zhang, D. Mass-forming isolated ischemic necrosis of the cecum mimicking malignancy: Clinicopathologic features of 11 cases. Ann. Diagn. Pathol. 2024, 75, 152428. [Google Scholar] [CrossRef] [PubMed]
- Karabay, O.; Erdem, M.; Hasbahceci, M. Partial Cecum Necrosis as a Rare Cause of Acute Abdominal Pain in an Elderly Patient. J. Coll. Physicians Surg. Pak. 2018, 28, 81–83. [Google Scholar] [CrossRef] [PubMed]
- Chan, N.H.H.L.; Rafiee, H.; Beales, I.L.P.; Karthigan, R.; Ciorra, A.; Kim, T. Isolated caecal necrosis—A case study. BJR Case Rep. 2018, 5, 20180089. [Google Scholar] [CrossRef] [PubMed]
- Eyvaz, K.; Sıkar, H.E.; Gökçeimam, M.; Küçük, H.F.; Kurt, N. A rare cause of acute abdomen: A rare cause of acute abdomen: Isolated necrosis of the cecum. Turk. J. Surg. 2020, 36, 317–320. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Tovar, J.; Gamallo, C. Ischaemic caecal necrosis. Acta Chir. Belg. 2008, 108, 341–342. [Google Scholar] [CrossRef] [PubMed]
- Rist, C.B.; Watts, J.C.; Lucas, R.J. Isolated ischemic necrosis of the cecum in patients with chronic heart disease. Dis. Colon Rectum 1984, 27, 548–551. [Google Scholar] [CrossRef] [PubMed]
- Hunter, J.P.; Saratzis, A.; Zayyan, K. Spontaneous, Isolated Caecal Necrosis: Report of a Case, Review of the Literature, and Updated Classification. Acta Chir. Belg. 2013, 113, 60–63. [Google Scholar] [CrossRef] [PubMed]
- Kardoun, N.; Hadrich, Z.; Rahma, D.; Harbi, H.; Boujelben, S.; Mzali, R. Isolated cecal necrosis: Report of two cases. Clin. Case Rep. 2021, 9, 04552. [Google Scholar] [CrossRef] [PubMed]
- Gundes, E.; Kucukkartallar, T.; Çolak, M.; Cakir, M.; Aksoy, F. Ischemic Necrosis of the Cecum: A Single Center Experience. Korean J. Gastroenterol. 2013, 61, 265–269. [Google Scholar] [CrossRef] [PubMed]
- Atıcı, S.D.; Ustun, M.; Kuzey, A.E.; Kaya, T.; Çalık, B. A rare cause of right lower quadrant abdominal pain: Isolated Cecal necrosis. Turk. J. Color. Dis. 2022, 32, 31–35. [Google Scholar]
- Sunamak, O.; Corbaci, K.; Akyuz, C.; Gul, M.O.; Besler, E.; Donmez, T.; Ekiz, F. Isolated cecum necrosis: Single center experience in the light of literature. In Proceedings of the 23th National Surgery Congress, Antalya, Turkey, 24–28 April 2024. [Google Scholar]

| The number of patients | 7 |
| Age (median and range) | 61 (36–67) |
| M/F ratio | 5/2 |
| Symptoms | |
| Pain | 7/7 |
| Nausea and vomiting | 3/7 |
| Symptom duration (days) (median and range) | 1 (1–4) |
| Prediagnosis | |
| Acute abdomen | 5/7 |
| Acute appendicitis | 2/7 |
| Chronic Disease | 6/7 |
| CRF | 4/7 |
| DM | 2/7 |
| CAD | 2/7 |
| HT | 2/7 |
| ADPKD | 1/7 |
| CVA | 1/7 |
| TAH | 1/7 |
| None | 1/7 |
| Ejection fraction (%) (6/7) | 60 |
| Dialysis treatment | 4/7 |
| AVF | 4/7 |
| USG | 2/7 |
| USG findings | Intra-abdominal free fluid |
| Findings consistent with acute appendicitis | |
| CT | 4/7 |
| CT findings | |
| Non-specific | 2/7 |
| Air in the bowel wall | 1/7 |
| Increase in thickness of the cecum wall | 2/7 |
| Perforation | 3/7 |
| The interval between the beginning of the symptoms and surgery (Day) (median and range) | 1 (1–4) |
| Incision | |
| Midline laparotomy | 5/7 |
| McBurney | 2/7 |
| Surgical procedure | |
| Right hemi-colectomy + anastomosis | 4/7 |
| Right hemi-colectomy + end ileostomy | 5/7 |
| Hematoma drainage | 1/7 |
| Conversion to end ileostomy | 2/7 |
| Mortality | 1/7 |
| Hospital stay (day) (median and range) | 12 (4–16) |
| 30-day mortality | 1/7 |
| Perforation | Non-Perforation | ||
|---|---|---|---|
| Gender | M | 1 | 4 |
| F | 2 | 0 | |
| Age (median) | 61 | 61.5 | |
| Abdominal Pain | 3 | 4 | |
| Nausea–Vomiting | 1 | 2 | |
| CRF | 2 | 2 | |
| CAD | 1 | 1 | |
| DM | 1 | 1 | |
| HT | 0 | 2 | |
| CVA | 1 | 0 | |
| TAH | 1 | 0 | |
| ADPKD | 0 | 1 | |
| Surgery | Ileostomy | 2 | 1 |
| Anastomosis | 1 | 3 | |
| 2nd Operation | Ileostomy | - | 1 |
| 3rd Operation | Ileostomy | - | 1 |
| Mortality | 0 | 1 | |
| WBC (×109/L) | 16.783 | 12.8525 | |
| NEUT (mcL) | 14.61 | 11.4975 | |
| WBC/NEUT | 1.187 | 1.077 | |
| Hb (g/dL) | 11.53 | 12.9 | |
| HCT (%) | 37.2 | 39.875 | |
| PLT (/mcL) | 324,000 | 212,000 |
| Study/ (Peri-Operative Mortality) | Number (M/F) | Age (Years) | Symptom | Symptom Duration (Day) | WBC Count (/mm3) | US | CT Imaging | Colonoscopy | Comorbidity | Preliminary Diagnosis | Incision | Procedure |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Rist 1984 (0) | 3 (M) | 79 (59–84) | 3xPain, 2xNausea, Vomiting | - | 16.000 (12.600–18.100) | - | - | - | 3xCHF, 2xCVD (Digoxin) 1xCVA | 2xAcute abdomen 2xAcute appendicitis | - | 2xRight hemicolectomy 1 Cecectomy |
| Schuler 2000 (1/5) | 5 (1/4) | 84 (57–91) | 5xPain, 1xNausea/ Vomiting, 1x Diarrhea | 1 (0.3–3) | 17.000 (12.000–20.600) | - | - | - | 2xHT 1xDM 1XCABG 1xCAD 1xCHF | Acute appendicitis Acute abdomen Cecum cancer | - | 4xRight hemicolectomy +anastomosis 1xRight hemicolectomy +end ileostomy |
| Ruiz-Tovar 2008 (0) | 1F | 82 | Pain | 4 | 8.100 | - | Asymmetric thickening of the caecal wall, suggesting a caecal neoplasm | Cecum tumor | Midline laparotomy | Right hemicolectomy +anastomosis | ||
| Dirican 2009 (0) | 4 (2/2) | 59 (46–68) | 4xPain 4xNausea/ Vomiting | 20.200 (16.400–23.700) | 3xFree intra abdominal fluid | 1xNon-specific | - | 2xCRF 1xCRF+DM+HT 1xCOPD | Acute appendicitis | 1xDiagnostic laparoscopy 3xLaparotomy | 3xRight hemicolectomy +anastomosis 1xCecum resection +ileostomy | |
| Gundes 2013 (5/13) | 13 (8/5) | 68 (51–84) | 13xPain 8xDistention, 8xVomiting | 3 (1–7) | 15.200 (8.700–29.000) | 5xFluid in the right lower quadrant and contamination in the fatty planes 3x Normal | 2xThickening and inflammation in the cecal wall | - | 5xCRF 3xHT 2xAF 2xDM 1xCOPD 1xFMF 1xCAD 1xCVA | Acute appendicitis | - | 10xRight hemicolectomy 2xRight hemicolectomy +end ileostomy 1xCecal resection |
| Hunter 2013 (0) | 1F | 74 | Pain Nausea | 0.25 | 12.030 | - | - | HT Diverticulosis | - | Diagnostic laparoscopy +Midline laparotomy | Partial cecum resection | |
| Çakar 2014 (5/6) | 6 (3/3) | 60.3 (38–85) | Pain Vomiting | - | - | 1xAir-fluid level (out of 4) | - | 4xCRF 4xDM 4xHT 1xAF+CAB 1xAortabifemo- ral graft | Acute appendicitis | 1xDiagnostic laparoscopy Laparatomy | 2xRight hemicolectomy +end ileostomy + mucous fistula 2xRight hemicolectomy +anastomosis 1xCecal resection +anastomosis+ 1xCecal resection +end ileostomy + mucous fistula 3xReoperation 2xEnd ileostomy+mucous fistula 1xRight hemicolectomy +end ileostomy +mucous fistula | |
| Shahverdi 2017 (0) | 1 (F) | 62 | Pain Nausea Vomiting | - | 9.700 | Dilated bowels with abundant gas | A minor fluid collection in right lower quadrant | - | DM, HT, CAD, CVA, CABG Behçet’s disease | Acute abdomen | Midline | Right hemicolectomy + anastomosis |
| Karabay 2018 (0) | 1 (F) | 68 | Pain | 7 | 15.390 | Non specific | Linear density at the back of the cecum and a tubular structure extending to the liver | - | DM, HT | Acute appendicits | Laparoscopy +open surgery | Partial cecum resection +anastomosis |
| Kohga 2018 (0) | 1 (M) | 59 | Pain | 0.2 | 8.700 | - | A dilated cecum surrounded by free air | - | AF, digoxin | Cecum perforation | Diagnostic laparosocpy | 1xLaparoscopic assisted ileocecal resection +anastomosis 1xIleostomy |
| Chan 2018 (0) | 1 (F) | Pain Nausea Vomiting/ and Diarrhea. | 10.000 | - | Focal cecum ischemia and chronic SMA stenosis | Cecal ulcer and ischemic mucosa | AF, HT, CRF | Cecum ischemia | - | Medical treatment | ||
| Eyvaz 2020 (0) | 1 (F) | 76 | Pain, Nausea | 0.5 | 16.200 | - | Thickening on the cecum wall | - | TBC Thyroidectomy HT | Acute abdomen, Acute appendicitis | Midline | Ileocecal resection +anastomosis |
| Kardoun 2021 (0) | 2 (F) | 72 (66–78) | 2xPain 1xNausea/ Vomiting | - | 12.850 (11.600–14.100) | - | 1xDilated cecum with mural thickening, edema, and intramural gas (pneumatosis), portal venous gas and mesenteric gas while (appendix normal) 1xCecum surrounded by free air, (appendix normal) | 2xCRF 2xHT 1xCAD 1xDyslipidemia 2xDM 1xAF (Digoxin) | Cecum ischemia | Midline laparotomy | 1xCecum resection +anastomosis 1xIleocecal resection + a double-barrel ileocolostomy | |
| Atıcı 2022 (6) | 17 (9/8) | 56 (22–85) | 17xPain 17xNausea | 1 | 17xPericecal inflammation and cecal wall thickening | 4xCRF 5xCAD 8xHT 3xCHF 5xArrhytmia 4xDM 3xCOPD 1xChronic pancreatitis 1xLung cancer 1xIliac artery stent 1x Aplastic anemia | 2xDiagnostic laparoscopy 17xMidline | 14xRight hemicolectomy +anastomosis 2xRight hemicolectomy +Mikulicz ileocolostomy 1xPartial cecum resection +Mikulicz ileocolostomy | ||||
| Suleimanov 2022 (0) | 1 (M) | 42 | Pain Nausea/ Vomiting | 3 | 16.000 | Unremarkable | - | - | Acute appendicitis | McBurney +extension | Ileocecal resection +anastomosis | |
| Janike 2023 (0) | 1F | 77 | Pain Nausea Vomiting Melena Wigth loss | Several days | 13.000 | - | Colonic mass | Cecal ischemic mass | HT Hyperlipidemia Obesity | ICN | Laparotomy | Right hemicolectomy + anastomosis |
| Liao 2025 (0) | 11 (4/7) | 72 (43–87) | 6xPain 5xGI bleeding 3xDiarrhea 4xNausea/ Vomiting 2xAsymptomatic (screening colonoscopy) | - | - | - | 8xColonic mass (out of 9)m (pathology ischemia) | 9x Colonic mass (out of 9) | 7xHT 5xCVD 4xHyper-lipidemia 2xCOPD 2xDM 1xCRF | ICN | 5x Laparotomy | 6xMedical Treatment 5xRight hemicolectomy |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sunamak, O.; Corbaci, K.; Akyuz, C.; Gul, M.O.; Besler, E.; Donmez, T.; Ekiz, F. Isolated Cecal Necrosis as a Cause of Acute Abdomen. J. Clin. Med. 2025, 14, 1019. https://doi.org/10.3390/jcm14031019
Sunamak O, Corbaci K, Akyuz C, Gul MO, Besler E, Donmez T, Ekiz F. Isolated Cecal Necrosis as a Cause of Acute Abdomen. Journal of Clinical Medicine. 2025; 14(3):1019. https://doi.org/10.3390/jcm14031019
Chicago/Turabian StyleSunamak, Oguzhan, Kadir Corbaci, Cebrail Akyuz, Mehmet Onur Gul, Evren Besler, Turgut Donmez, and Feza Ekiz. 2025. "Isolated Cecal Necrosis as a Cause of Acute Abdomen" Journal of Clinical Medicine 14, no. 3: 1019. https://doi.org/10.3390/jcm14031019
APA StyleSunamak, O., Corbaci, K., Akyuz, C., Gul, M. O., Besler, E., Donmez, T., & Ekiz, F. (2025). Isolated Cecal Necrosis as a Cause of Acute Abdomen. Journal of Clinical Medicine, 14(3), 1019. https://doi.org/10.3390/jcm14031019







