Injectable Platelet-Rich Fibrin (I-PRF) Administered to Temporomandibular Joint Cavities: A Scoping Review
Abstract
:1. Introduction
1.1. Rationale
1.2. Objectives
2. Methods
2.1. Eligibility Criteria
2.2. Information Sources and Search Strategy
2.3. Selection Process
2.4. Data Collection Process
2.5. Data Items
2.6. Study Risk of Bias Assessment
2.7. Synthesis Methods
3. Results
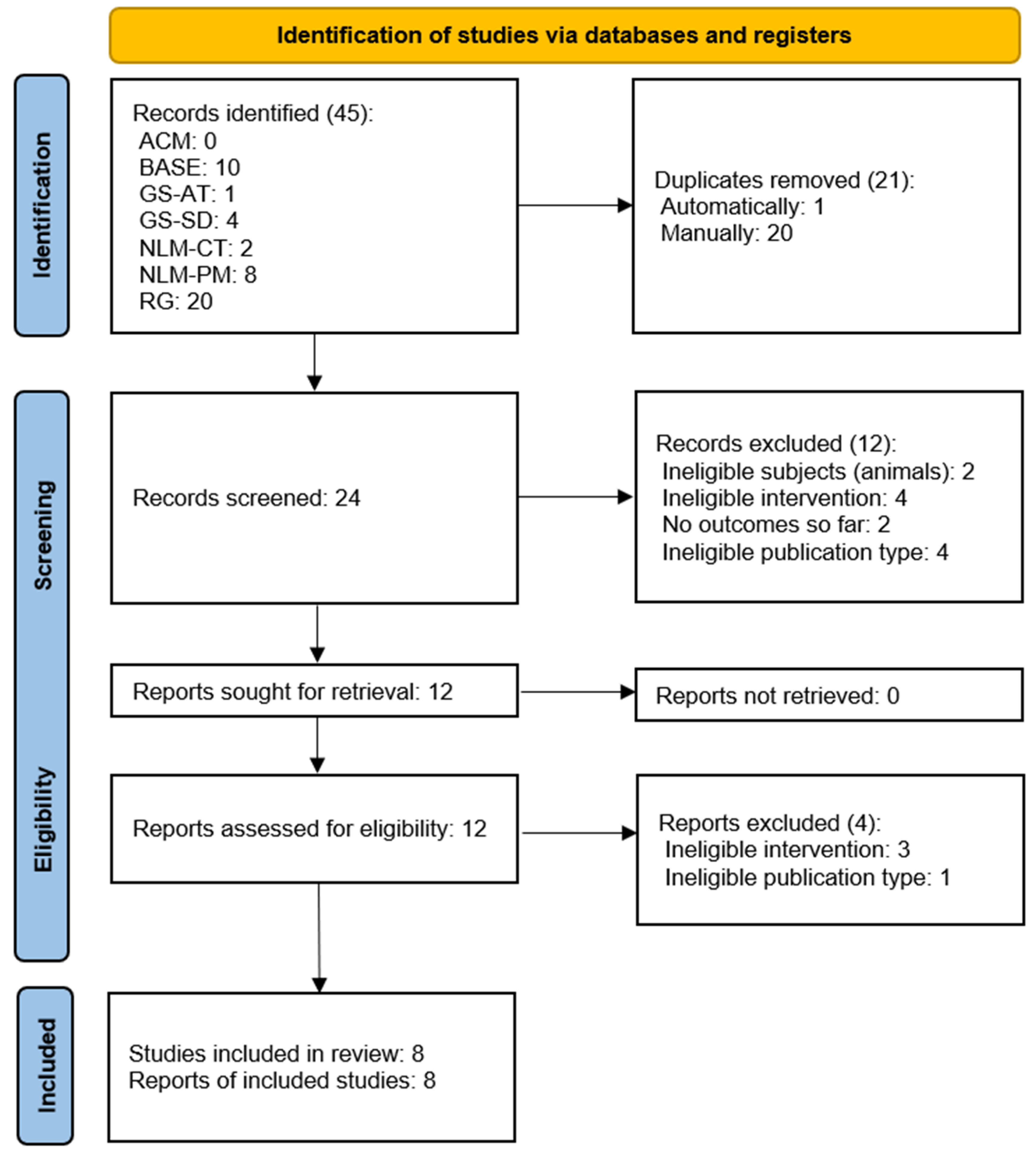
3.1. Study Selection
3.2. Study Characteristics
3.3. Risk of Bias in Studies
3.4. Results of Individual Studies
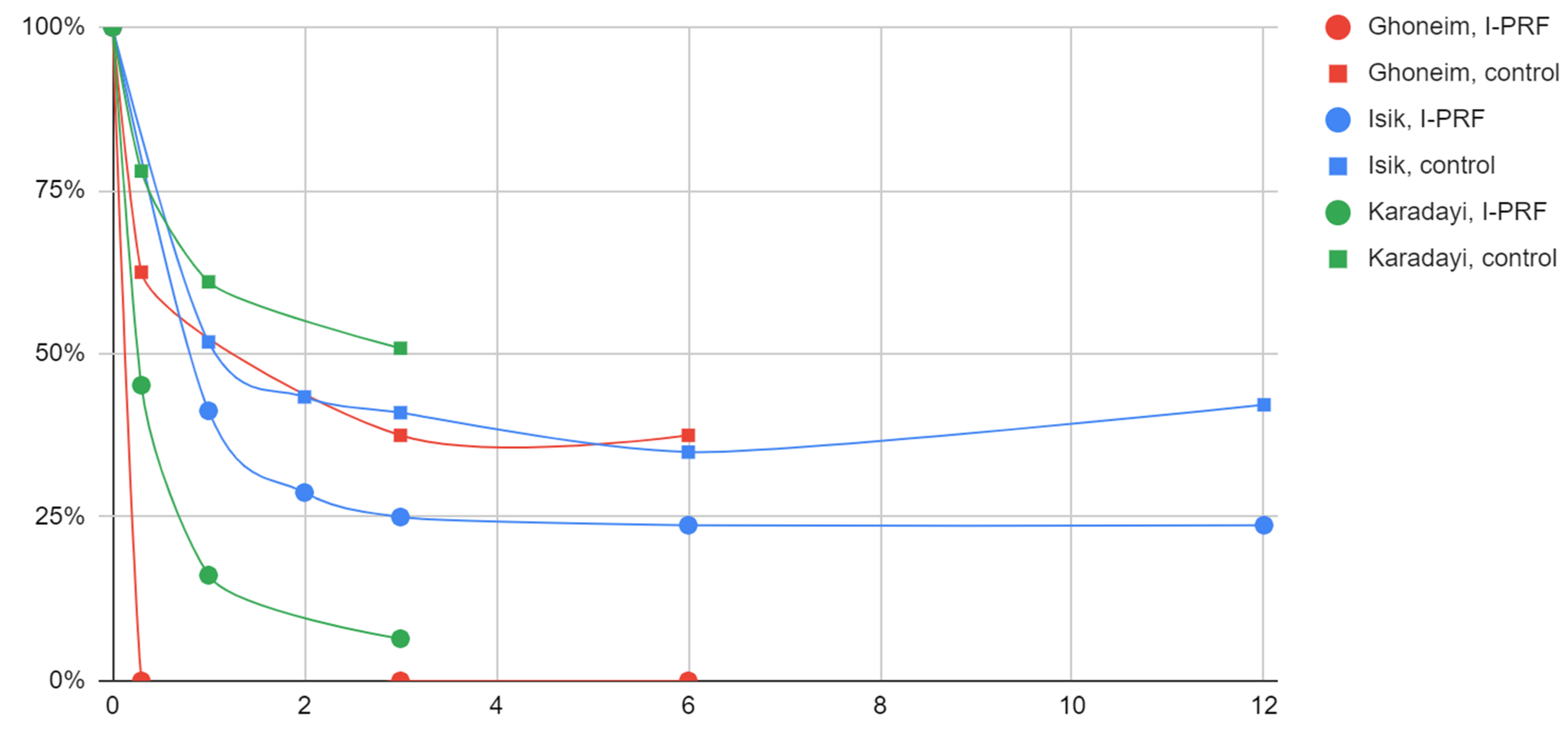
3.4.1. Articular Pain
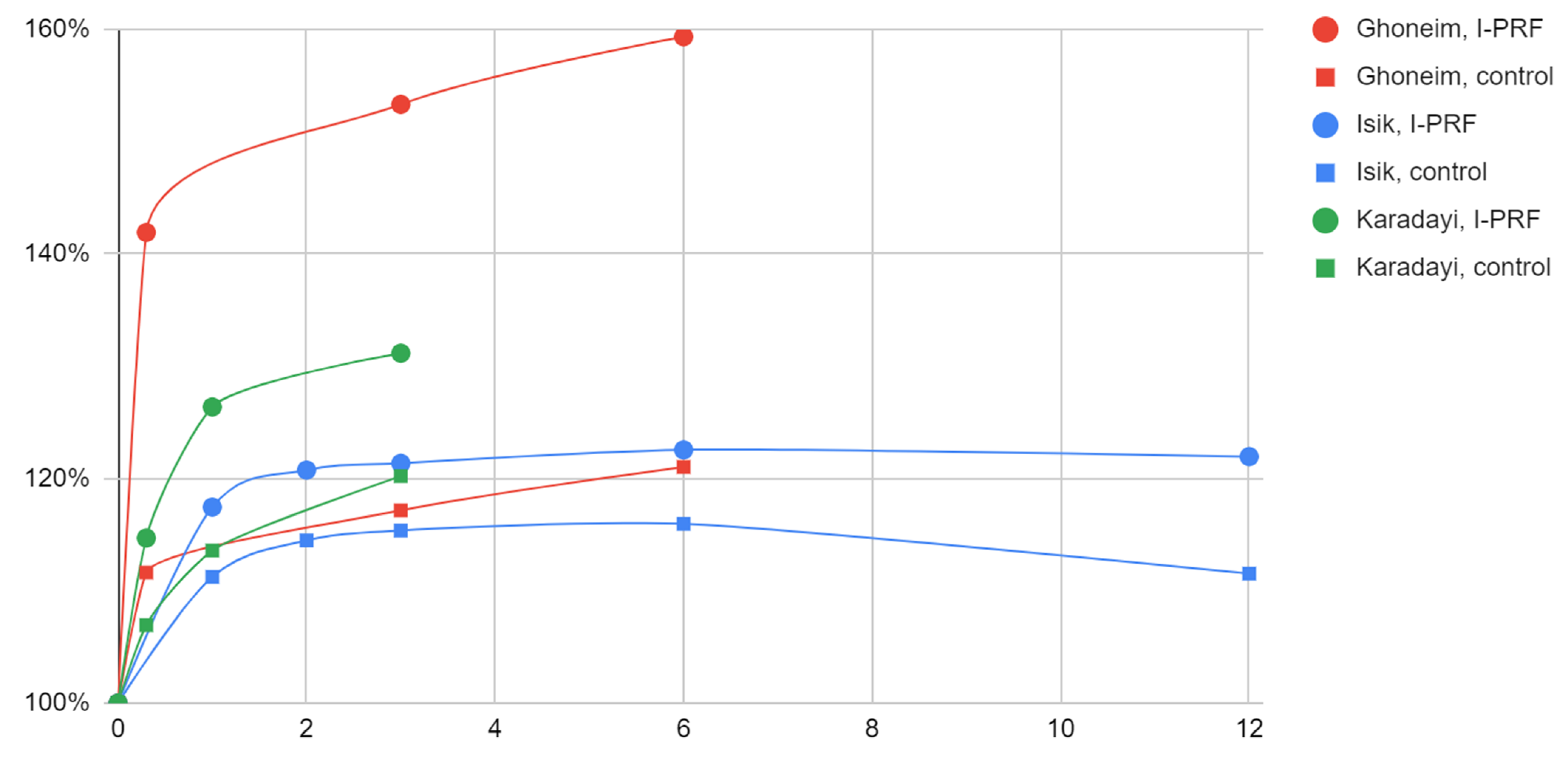
3.4.2. Mandibular Mobility
3.4.3. TMD Indices
3.5. Other Studies
4. Discussion
4.1. General Interpretation of the Results
4.1.1. Arthrocentesis with I-PRF Administration versus Sole Arthrocentesis
4.1.2. Arthrocentesis with I-PRF Administration versus Arthrocentesis with HA Administration
4.2. Limitations of the Evidence
4.3. Limitations of the Review Processes
4.4. Rejected Reports
4.5. Future Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Marcelino, V.; De Rovere, S.; Paço, M.; Gonçalves, M.; Marcelino, S.; Guimarães, A.S.; Pinho, T. Masticatory Function in Individuals with Temporomandibular Disorders: A Systematic Review and Meta-Analysis. Life 2023, 13, 472. [Google Scholar] [CrossRef] [PubMed]
- Vieira, L.S.; Pestana, P.R.M.; Miranda, J.P.; Soares, L.A.; Silva, F.; Alcantara, M.A.; Oliveira, V.C. The Efficacy of Manual Therapy Approaches on Pain, Maximum Mouth Opening and Disability in Temporomandibular Disorders: A Systematic Review of Randomised Controlled Trials. Life 2023, 13, 292. [Google Scholar] [CrossRef] [PubMed]
- Greenbaum, T.; Pitance, L.; Kedem, R.; Emodi-Perlman, A. The Mouth-opening Muscular Performance in Adults with and without Temporomandibular Disorders: A Systematic Review. J. Oral Rehabil. 2022, 49, 476–494. [Google Scholar] [CrossRef]
- Sójka, A.; Huber, J.; Hędzelek, W.; Wiertel-Krawczuk, A.; Szymankiewicz-Szukała, A.; Seraszek-Jaros, A.; Kulczyk, A.; Wincek, A.; Sobieska, M. Relations between the Results of Complex Clinical and Neurophysiological Examinations in Patients with Temporomandibular Disorders Symptoms. CRANIO® 2018, 36, 44–52. [Google Scholar] [CrossRef]
- Chęciński, M.; Sikora, M.; Chęcińska, K.; Nowak, Z.; Chlubek, D. The Administration of Hyaluronic Acid into the Temporomandibular Joints’ Cavities Increases the Mandible’s Mobility: A Systematic Review and Meta-Analysis. J. Clin. Med. 2022, 11, 1901. [Google Scholar] [CrossRef] [PubMed]
- Tournavitis, A.; Sandris, E.; Theocharidou, A.; Slini, T.; Kokoti, M.; Koidis, P.; Tortopidis, D. Effectiveness of Conservative Therapeutic Modalities for Temporomandibular Disorders-Related Pain: A Systematic Review. Acta Odontol. Scand. 2022, 81, 286–297. [Google Scholar] [CrossRef] [PubMed]
- Derwich, M.; Górski, B.; Amm, E.; Pawłowska, E. Oral Glucosamine in the Treatment of Temporomandibular Joint Osteoarthritis: A Systematic Review. Int. J. Mol. Sci. 2023, 24, 4925. [Google Scholar] [CrossRef] [PubMed]
- Turosz, N.; Chęcińska, K.; Chęciński, M.; Kamińska, M.; Nowak, Z.; Sikora, M.; Chlubek, D. A Scoping Review of the Use of Pioglitazone in the Treatment of Temporo-Mandibular Joint Arthritis. Int. J. Environ. Res. Public Health 2022, 19, 16518. [Google Scholar] [CrossRef]
- Müggenborg, F.; de Castro Carletti, E.M.; Dennett, L.; de Oliveira-Souza, A.I.S.; Mohamad, N.; Licht, G.; von Piekartz, H.; Armijo-Olivo, S. Effectiveness of Manual Trigger Point Therapy in Patients with Myofascial Trigger Points in the Orofacial Region—A Systematic Review. Life 2023, 13, 336. [Google Scholar] [CrossRef]
- Brighenti, N.; Battaglino, A.; Sinatti, P.; Abuín-Porras, V.; Sánchez Romero, E.A.; Pedersini, P.; Villafañe, J.H. Effects of an Interdisciplinary Approach in the Management of Temporomandibular Disorders: A Scoping Review. Int. J. Environ. Res. Public Health 2023, 20, 2777. [Google Scholar] [CrossRef]
- Nitecka-Buchta, A.; Walczynska-Dragon, K.; Batko-Kapustecka, J.; Wieckiewicz, M. Comparison between Collagen and Lidocaine Intramuscular Injections in Terms of Their Efficiency in Decreasing Myofascial Pain within Masseter Muscles: A Randomized, Single-Blind Controlled Trial. Pain Res. Manag. 2018, 2018, 8261090. [Google Scholar] [CrossRef] [PubMed]
- Nowak, Z.; Chęciński, M.; Nitecka-Buchta, A.; Bulanda, S.; Ilczuk-Rypuła, D.; Postek-Stefańska, L.; Baron, S. Intramuscular Injections and Dry Needling within Masticatory Muscles in Management of Myofascial Pain. Systematic Review of Clinical Trials. Int. J. Environ. Res. Public Health 2021, 18, 9552. [Google Scholar] [CrossRef]
- Arribas-Pascual, M.; Hernández-Hernández, S.; Jiménez-Arranz, C.; Grande-Alonso, M.; Angulo-Díaz-Parreño, S.; La Touche, R.; Paris-Alemany, A. Effects of Physiotherapy on Pain and Mouth Opening in Temporomandibular Disorders: An Umbrella and Mapping Systematic Review with Meta-Meta-Analysis. J. Clin. Med. 2023, 12, 788. [Google Scholar] [CrossRef] [PubMed]
- Thorpe, A.R.D.S.; Haddad, Y.; Hsu, J. A Systematic Review and Meta-Analysis of Randomized Controlled Trials Comparing Arthrocentesis with Conservative Management for Painful Temporomandibular Joint Disorder. Int. J. Oral Maxillofac. Surg. 2023, in press. [Google Scholar] [CrossRef]
- Chęciński, M.; Chęcińska, K.; Nowak, Z.; Sikora, M.; Chlubek, D. Treatment of Mandibular Hypomobility by Injections into the Temporomandibular Joints: A Systematic Review of the Substances Used. J. Clin. Med. 2022, 11, 2305. [Google Scholar] [CrossRef] [PubMed]
- Bhattacharjee, B.; Bera, R.N.; Verma, A.; Soni, R.; Bhatnagar, A. Efficacy of Arthrocentesis and Stabilization Splints in Treatment of Temporomandibular Joint Disc Displacement Disorder Without Reduction: A Systematic Review and Meta-Analysis. J. Maxillofac. Oral Surg. 2023, 22, 83–93. [Google Scholar] [CrossRef]
- Ozawa, M.; Okaue, M.; Kaneko, K.; Hasegawa, M.; Matsunaga, S.; Matsumoto, M.; Hori, M.; Kudo, I.; Takagi, M. Clinical Assessment of the Pumping Technique in Treating TMJ Arthrosis with Closed Lock. J. Nihon Univ. Sch. Dent. 1996, 38, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Torres-Rosas, R.; Marcela Castro-Gutiérrez, M.; Flores-Mejía, L.; Torres-Rosas, E.; Nieto-García, R.; Argueta-Figueroa, L. Ozone for the Treatment of Temporomandibular Joint Disorders: A Systematic Review and Meta-Analysis. Med. Gas Res. 2023, 13, 149. [Google Scholar] [CrossRef] [PubMed]
- Sit, R.W.-S.; Reeves, K.D.; Zhong, C.C.; Wong, C.H.L.; Wang, B.; Chung, V.C.; Wong, S.Y.; Rabago, D. Efficacy of Hypertonic Dextrose Injection (Prolotherapy) in Temporomandibular Joint Dysfunction: A Systematic Review and Meta-Analysis. Sci. Rep. 2021, 11, 14638. [Google Scholar] [CrossRef]
- Zarate, M.A.; Frusso, R.D.; Reeves, K.D.; Cheng, A.-L.; Rabago, D. Dextrose Prolotherapy Versus Lidocaine Injection for Temporomandibular Dysfunction: A Pragmatic Randomized Controlled Trial. J. Altern. Complement. Med. 2020, 26, 1064–1073. [Google Scholar] [CrossRef] [PubMed]
- Gutiérrez, I.Q.; Sábado-Bundó, H.; Gay-Escoda, C. Intraarticular Injections of Platelet Rich Plasma and Plasma Rich in Growth Factors with Arthrocenthesis or Arthroscopy in the Treatment of Temporomandibular Joint Disorders: A Systematic Review. J. Stomatol. Oral Maxillofac. Surg. 2021, 123, e327–e335. [Google Scholar] [CrossRef]
- Haigler, M.C.; Abdulrehman, E.; Siddappa, S.; Kishore, R.; Padilla, M.; Enciso, R. Use of Platelet-Rich Plasma, Platelet-Rich Growth Factor with Arthrocentesis or Arthroscopy to Treat Temporomandibular Joint Osteoarthritis: Systematic Review with Meta-Analyses. J. Am. Dent. Assoc. 2018, 149, 940–952.e2. [Google Scholar] [CrossRef] [PubMed]
- Chęciński, M.; Chęcińska, K.; Turosz, N.; Kamińska, M.; Nowak, Z.; Sikora, M.; Chlubek, D. Autologous Stem Cells Transplants in the Treatment of Temporomandibular Joints Disorders: A Systematic Review and Meta-Analysis of Clinical Trials. Cells 2022, 11, 2709. [Google Scholar] [CrossRef] [PubMed]
- Sikora, M.; Sielski, M.; Chęciński, M.; Nowak, Z.; Czerwińska-Niezabitowska, B.; Chlubek, D. Repeated Intra-Articular Administration of Platelet-Rich Plasma (PRP) in Temporomandibular Disorders: A Clinical Case Series. J. Clin. Med. 2022, 11, 4281. [Google Scholar] [CrossRef]
- Giacomello, M.; Giacomello, A.; Mortellaro, C.; Gallesio, G.; Mozzati, M. Temporomandibular Joint Disorders Treated with Articular Injection: The Effectiveness of Plasma Rich in Growth Factors-Endoret. J. Craniofac. Surg. 2015, 26, 709–713. [Google Scholar] [CrossRef] [PubMed]
- Albilia, J.; Herrera-Vizcaíno, C.; Weisleder, H.; Choukroun, J.; Ghanaati, S. Liquid Platelet-Rich Fibrin Injections as a Treatment Adjunct for Painful Temporomandibular Joints: Preliminary Results. Cranio J. Craniomandib. Pract. 2020, 38, 292–304. [Google Scholar] [CrossRef]
- Derwich, M.; Mitus-Kenig, M.; Pawlowska, E. Mechanisms of Action and Efficacy of Hyaluronic Acid, Corticosteroids and Platelet-Rich Plasma in the Treatment of Temporomandibular Joint Osteoarthritis—A Systematic Review. Int. J. Mol. Sci. 2021, 22, 7405. [Google Scholar] [CrossRef] [PubMed]
- Kałużyński, K.; Trybek, G.; Smektała, T.; Masiuk, M.; Myśliwiec, L.; Sporniak-Tutak, K. Effect of Methylprednisolone, Hyaluronic Acid and Pioglitazone on Histological Remodeling of Temporomandibular Joint Cartilage in Rabbits Affected by Drug-Induced Osteoarthritis. Postep. Hig. Med. Dosw. Online 2016, 70, 74–79. [Google Scholar] [CrossRef]
- Sikora, M.; Chęciński, M.; Nowak, Z.; Chlubek, D. Variants and Modifications of the Retroauricular Approach Using in Temporomandibular Joint Surgery: A Systematic Review. J. Clin. Med. 2021, 10, 2049. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, E.F.C.; Lemos, C.A.A.; Vasconcellos, R.J.H.; Moraes, S.L.D.; Vasconcelos, B.C.E.; Pellizzer, E.P. Does Arthroscopy Cause More Complications than Arthrocentesis in Patients with Internal Temporomandibular Joint Disorders? Systematic Review and Meta-Analysis. Br. J. Oral Maxillofac. Surg. 2021, 59, 1166–1173. [Google Scholar] [CrossRef]
- Matheus, H.R.; Özdemir, Ş.D.; Guastaldi, F.P.S. Stem Cell-Based Therapies for Temporomandibular Joint Osteoarthritis and Regeneration of Cartilage/Osteochondral Defects: A Systematic Review of Preclinical Experiments. Osteoarthr. Cartil. 2022, 30, 1174–1185. [Google Scholar] [CrossRef] [PubMed]
- Pagotto, L.E.C.; de Santana Santos, T.; Pastore, G.P. The Efficacy of Mesenchymal Stem Cells in Regenerating Structures Associated with the Temporomandibular Joint: A Systematic Review. Arch. Oral Biol. 2021, 125, 105104. [Google Scholar] [CrossRef] [PubMed]
- Minervini, G.; Del Mondo, D.; Russo, D.; Cervino, G.; D’Amico, C.; Fiorillo, L. Stem Cells in Temporomandibular Joint Engineering: State of Art and Future Persectives. J. Craniofac. Surg. 2022, 33, 2181–2187. [Google Scholar] [CrossRef]
- Bhalla, M.; El-Housseini, Z.; Asaria, R. Corrigendum to “Blindness Associated with Platelet-Rich Plasma Temporomandibular Joint Injections” [Br. J. Oral Maxillofac. Surg. 58(9) (2020) 1197–1199]. Br. J. Oral Maxillofac. Surg. 2022, 60, 1004. [Google Scholar] [CrossRef] [PubMed]
- Putthirangsiwong, B.; Vongsilpavattana, V.; Leelawongs, S.; Chanthanaphak, E.; Tunlayadechanont, P.; Chokthaweesak, W. Superior Ophthalmic Vein Embolism Following Forehead Augmentation with Autologous Fat Injection. Aesthetic Plast. Surg. 2022, 46, 450–455. [Google Scholar] [CrossRef] [PubMed]
- Szantyr, A.; Orski, M.; Marchewka, I.; Szuta, M.; Orska, M.; Zapała, J. Ocular Complications Following Autologous Fat Injections into Facial Area: Case Report of a Recovery from Visual Loss After Ophthalmic Artery Occlusion and a Review of the Literature. Aesthetic Plast. Surg. 2017, 41, 580–584. [Google Scholar] [CrossRef] [PubMed]
- Farshidfar, N.; Jafarpour, D.; Firoozi, P.; Sahmeddini, S.; Hamedani, S.; de Souza, R.F.; Tayebi, L. The Application of Injectable Platelet-Rich Fibrin in Regenerative Dentistry: A Systematic Scoping Review of In Vitro and In Vivo Studies. Jpn. Dent. Sci. Rev. 2022, 58, 89–123. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ. 2021, 88, 105906. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Schiavenato, M.; Chu, F. PICO: What It Is and What It Is Not. Nurse Educ. Pract. 2021, 56, 103194. [Google Scholar] [CrossRef]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Więckowska, B.; Kubiak, K.B.; Jóźwiak, P.; Moryson, W.; Stawińska-Witoszyńska, B. Cohen’s Kappa Coefficient as a Measure to Assess Classification Improvement Following the Addition of a New Marker to a Regression Model. Int. J. Environ. Res. Public. Health 2022, 19, 10213. [Google Scholar] [CrossRef] [PubMed]
- Ooi, K.; Aihara, M.; Matsumura, H.; Matsuda, S.; Watanabe, Y.; Yuasa, H.; Matsuka, Y. Therapy Outcome Measures in Temporomandibular Disorder: A Scoping Review. BMJ Open 2022, 12, e061387. [Google Scholar] [CrossRef] [PubMed]
- Idáñez-Robles, A.M.; Obrero-Gaitán, E.; Lomas-Vega, R.; Osuna-Pérez, M.C.; Cortés-Pérez, I.; Zagalaz-Anula, N. Exercise Therapy Improves Pain and Mouth Opening in Temporomandibular Disorders: A Systematic Review with Meta-Analysis. Clin. Rehabil. 2023, 37, 443–461. [Google Scholar] [CrossRef]
- Keller, S.; Bocell, F.D.; Mangrum, R.; McLorg, A.; Logan, D.; Chen, A.L.; Steen, A.I.; Woods, P.; Weinberg, J.; Royce, L.; et al. Patient-Reported Outcome Measures for Individuals with Temporomandibular Joint Disorders: A Systematic Review and Evaluation. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2023, 135, 65–78. [Google Scholar] [CrossRef]
- OCEBM. Levels of Evidence—Centre for Evidence-Based Medicine (CEBM), University of Oxford. Available online: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence (accessed on 29 March 2023).
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Baiomy, A.A.; Edrees, M.; Al-Ashmawy, M. Versatility of Injectable Platelet Rich Fibrin versus Autologous Blood Injection in the Treatment of Chronic Recurrent Temporomandibular Joint Dislocation. Egypt. J. Oral Maxillofac. Surg. 2019, 10, 64–69. [Google Scholar] [CrossRef]
- Vingender, S.; Dőri, F.; Schmidt, P.; Hermann, P.; Vaszilkó, M.T. Evaluation of the Efficiency of Hyaluronic Acid, PRP and I-PRF Intra-Articular Injections in the Treatment of Internal Derangement of the Temporomandibular Joint: A Prospective Study. J. Cranio-Maxillofac. Surg. 2023, 51, 1–6. [Google Scholar] [CrossRef]
- Da Silva Lima, G.L.; de Souza Carvalho, A.A.; de Toledo Lourenço, A.H. Ácido Hialurônico Vs Fibrina Rica em Plaquetas: Qual Utilizar em Tratamentos de Osteoartrite Temporomandibular? In Anais da II Jornada Odontológica Online; Instituto de Saúde: Nova Friburgo, Brazil, 2022; pp. 299–300. [Google Scholar]
- González, L.V.; López, J.P.; Díaz-Báez, D.; Orjuela, M.P.; Chavez, M. Clinical Outcomes of Operative Arthroscopy and Temporomandibular Medical Infiltration with Platelet-Rich Fibrin in Upper and Lower Articular Space. J. Cranio-Maxillofac. Surg. Off. Publ. Eur. Assoc. Cranio-Maxillofac. Surg. 2021, 49, 1162–1168. [Google Scholar] [CrossRef]
- Manafikhi, M.; Ataya, J.; Heshmeh, O. Evaluation of the Efficacy of Platelet Rich Fibrin (I-PRF) Intra-Articular Injections in the Management of Internal Derangements of Temporomandibular Joints—A Controlled Preliminary Prospective Clinical Study. BMC Musculoskelet. Disord. 2022, 23, 454. [Google Scholar] [CrossRef]
- Ghoneim, N.I.; Mansour, N.A.; Elmaghraby, S.A.; Abdelsameaa, S.E. Treatment of Temporomandibular Joint Disc Displacement Using Arthrocentesis Combined with Injectable Platelet Rich Fibrin versus Arthrocentesis Alone. J. Dent. Sci. 2022, 17, 468–475. [Google Scholar] [CrossRef] [PubMed]
- Işık, G.; Kenç, S.; Özveri Koyuncu, B.; Günbay, S.; Günbay, T. Injectable Platelet-Rich Fibrin as Treatment for Temporomandibular Joint Osteoarthritis: A Randomized Controlled Clinical Trial. J. Cranio-Maxillofac. Surg. 2022, 50, 576–582. [Google Scholar] [CrossRef]
- Karadayi, U.; Gursoytrak, B. Randomised Controlled Trial of Arthrocentesis with or without PRF for Internal Derangement of the TMJ. J. Cranio-Maxillofac. Surg. 2021, 49, 362–367. [Google Scholar] [CrossRef]
- Torul, D.; Cezairli, B.; Kahveci, K. The Efficacy of Intra-Articular Injectable Platelet-Rich Fibrin Application in the Management of Wilkes Stage III Temporomandibular Joint Internal Derangement. Int. J. Oral Maxillofac. Surg. 2021, 50, 1485–1490. [Google Scholar] [CrossRef]
- Yuce, E.; Komerik, N. Comparison of the Efficiacy of Intra-Articular Injection of Liquid Platelet-Rich Fibrin and Hyaluronic Acid After in Conjunction with Arthrocentesis for the Treatment of Internal Temporomandibular Joint Derangements. J. Craniofac. Surg. 2020, 31, 1870–1874. [Google Scholar] [CrossRef]
- Muhammad, K.; Khaldoun, A. Evaluation of the Combination Efficacy of Injectable Platelet Rich Fibrin (I-PRF) with Ultrasound as an Adjunctive Therapy in the Management of TMJ Pain (Clinical Study). Damascus Univ. J. Med. Sci. 2022, 38, 273–284. [Google Scholar]
- Chęciński, M.; Chęcińska, K.; Turosz, N.; Sikora, M.; Chlubek, D. Intra-Articular Injections into the Inferior versus Superior Compartment of the Temporomandibular Joint: A Systematic Review and Meta-Analysis. J. Clin. Med. 2023, 12, 1664. [Google Scholar] [CrossRef]
- Gürsoytrak, B. Evaluation of The Clinical Efficacy of Liquid Platelet Rich Fibrin Application in Painful Temporomandibular Joint Disorders. 2020. Available online: https://clinicaltrials.gov/ct2/show/NCT04317560 (accessed on 22 March 2023).
- Smardz, J. Assessment of the Effectiveness of Intra-Articular Injectable Platelet-Rich Fibrin (IPRF) Injections in the Management of Mild and Moderate Degeneration of the Temporomandibular Joints. 2022. Available online: https://clinicaltrials.gov/ct2/show/NCT05214924 (accessed on 22 March 2023).
- Barath, Z.; Rasko, Z. Technique for Achieving a Stable Position of the Condylar Process during Injection into the Temporomandibular Joint. Br. J. Oral Maxillofac. Surg. 2020, 58, 92–95. [Google Scholar] [CrossRef] [PubMed]
- Champs, B.; Corre, P.; Hamel, A.; Laffite, C.D.; Le Goff, B. US-Guided Temporomandibular Joint Injection: Validation of an in-Plane Longitudinal Approach. J. Stomatol. Oral Maxillofac. Surg. 2019, 120, 67–70. [Google Scholar] [CrossRef]
- Matheson, E.M.; Fermo, J.D.; Blackwelder, R.S. Temporomandibular Disorders: Rapid Evidence Review. Am. Fam. Physician 2023, 107, 52–58. [Google Scholar]
- Sikora, M.; Czerwińska-Niezabitowska, B.; Chęciński, M.A.; Sielski, M.; Chlubek, D. Short-Term Effects of Intra-Articular Hyaluronic Acid Administration in Patients with Temporomandibular Joint Disorders. J. Clin. Med. 2020, 9, 1749. [Google Scholar] [CrossRef] [PubMed]
- Torres, D.; Zaror, C.; Iturriaga, V.; Tobias, A. Intra-Articular Corticosteroids for Treatment of Temporomandibular Joint Internal Disorders: Protocol for Systematic Review and Network Meta-Analysis. BMJ Open 2020, 10, e034327. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, N.; Masterson, D.; Lopes de Lima, R.; de Souza Moura, B.; Oliveira, A.T.; Kelly da Silva Fidalgo, T.; Carvalho, A.C.P.; DosSantos, M.F.; Grossmann, E. Efficacy of Viscosupplementation with Hyaluronic Acid in Temporomandibular Disorders: A Systematic Review. J. Cranio-Maxillofac. Surg. Off. Publ. Eur. Assoc. Cranio-Maxillofac. Surg. 2018, 46, 1943–1952. [Google Scholar] [CrossRef] [PubMed]
- Moldez, M.A.; Camones, V.R.; Ramos, G.E.; Padilla, M.; Enciso, R. Effectiveness of Intra-Articular Injections of Sodium Hyaluronate or Corticosteroids for Intracapsular Temporomandibular Disorders: A Systematic Review and Meta-Analysis. J. Oral Facial Pain Headache 2018, 32, 53–66. [Google Scholar] [CrossRef] [PubMed]
| Domain | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Patients | Diagnosis of TMDs in human patients | TMDs as a symptom of generalized joint disease |
| Intervention | I-PRF intra-articular injection alone or preceded by arthrocentesis | Additional interventions |
| Control | One of the following: (1) arthrocentesis; (2) placebo injection; (3) hyaluronic acid administration | Not applicable |
| Outcomes | At least one of the following: (1) TMJ articular pain; (2) mandibular mobility; (3) TMD severity scale | Values of variables expressed qualitatively (present/absent) without using any scale |
| Search Engine | Query |
|---|---|
| ACM | [[All: i-prf] OR [All: “injectable platelet-rich fibrin”]] AND [All: temporomandibular] |
| BASE | (i-prf OR “injectable platelet-rich fibrin”) AND temporomandibular |
| GS-AT | allintitle: (i-prf OR “injectable platelet-rich fibrin”) AND temporomandibular |
| GS-SD | (i-prf OR “injectable platelet-rich fibrin”) AND temporomandibular; “Sort by date” filter |
| NLM-CT | (i-prf OR “injectable platelet-rich fibrin”) AND temporomandibular |
| NLM-PM | (i-prf OR “injectable platelet-rich fibrin”) AND temporomandibular |
| RG | (“i-prf” OR “injectable platelet-rich fibrin”) AND “temporomandibular” |
| Search Engine | Number of Records |
|---|---|
| ACM | 0 |
| BASE | 10 |
| GS-AT | 1 |
| GS-SD | 4 |
| NLM-CT | 2 |
| NLM-PM | 8 |
| RG | 20 |
| Total: | 45 |
| First Author, Publication Year | Title | Reason for Rejection |
|---|---|---|
| Vingender, 2023 [49] | Evaluation of the efficiency of hyaluronic acid, PRP and I-PRF intra-articular injections in the treatment of internal derangement of the temporomandibular joint: A prospective study. | Additional interventions (splint therapy, physiotherapy) |
| da Silva Lima, 2022 [50] | Ácido Hialurônico Vs Fibrina Rica Em Plaquetas: Qualutilizar Em Tratamentos De Osteoartritetemporomandibular? | Review paper |
| Gonzalez, 2021 [51] | Clinical outcomes of operative arthroscopy and temporomandibular medical infiltration with platelet-rich fibrin in upper and lower articular space | Additional interventions (arthroscopy) |
| Baiomy, 2019 [48] | Versatility of Injectable Platelet Rich Fibrin versus autologous blood injection in the Treatment of Chronic Recurrent Temporomandibular Joint Dislocation | Additional interventions (pericapsular injection, immobilization) |
| First Author, Publication Year | Total Number of Patients/Patients in the I-PRF Group | Diagnosis | Dose | Number of Doses/Interval | Comparators | Level of Evidence |
|---|---|---|---|---|---|---|
| Ghoneim, 2022 [53] | 40/20 | Disc displacement with reduction | 1.5 mL intra-articularly | 1/N/A | AC | 2 |
| Isik, 2022 [54] | 36/18 | TMJ osteoarthritis | 1 mL intra-articularly | 4/1 week | AC | 2 |
| Manafikhi,2022 [52] | 20/20 | Unilateral TMJ acoustic symptoms | 1 mL intra-articularly | 2/1 week | None | 4 |
| Muhammad, 2022 [58] | 30/10 | TMDs | 1.5 mL intra-articularly | 1/N/A | Ineligible (ultra-sound therapy) | 3 |
| Karadayi, 2021 [55] | 36/18 | Unilateral TMD | maximum of 2 mL intra-articularly | 1/N/A | AC | 2 |
| Torul, 2021 [56] | 54/18 | TMJ internal derangement(Wilkes stage III) | 1 mL intra-articularly | 1/N/A | AC; AC + HA injection | 3 |
| Albilia, 2020 [26] | 37/37 | TMJ internal derangement(Wilkes stage I–V) | 1.5–2 mL intra-articularly | Various/2 weeks | None | 4 |
| Yuce, 2020 [57] | 47/24 | TMJ internal derangement | 2 mL intra-articularly | 3/1 week | AC; AC + HA injection | 3 |
| First Author, Publication Year | Study Design | Randomization Process | Deviations from the Intended Interventions | Missing Outcome Data | Measurement of the Outcome | Selection of the Reported Result | Overall Risk of Bias |
|---|---|---|---|---|---|---|---|
| Ghoneim, 2022 [53] | Randomized controlled trial | Some concerns | Some concerns | Low | Some concerns | Low | Some concerns |
| Isik, 2022 [54] | Randomized controlled trial | Low | Some concerns | Low | Some concerns | Low | Some concerns |
| Karadayi, 2021 [55] | Randomized controlled trial | Low | Some concerns | Some concerns | Some concerns | Low | Some concerns |
| Torul, 2021 [56] | Retrospective study | N/A | N/A | N/A | N/A | N/A | N/A |
| Yuce, 2020 [57] | Retrospective study | N/A | N/A | N/A | N/A | N/A | N/A |
| First Author, Publication Year | Patient Group (Number of Patients) | Initial Value | After 7–10 Days | After 1 Month | After 2 Months | After 3 Months | After 6 Months | After 12 Months | Effect after 3 Months (the Lower the Better) |
|---|---|---|---|---|---|---|---|---|---|
| Ghoneim, 2022 [53] | AC + I-PRF | 6.0 | 0.0 * | N/A | N/A | 0.0 * | 0.0 * | N/A | 0.0% * |
| AC | 8.0 | 5.0 * | N/A | N/A | 3.0 * | 3.0 * | N/A | 37.5% * | |
| Isik, 2022 [54] | AC + I-PRF | 8.0 | N/A | 3.3 * | 2.3 * | 2.0 * | 1.9 * | 1.9 * | 25.0% * |
| AC | 8.3 | N/A | 4.3 * | 3.6 * | 3.4 * | 2.9 * | 3.5 * | 41.0% * | |
| Karadayi, 2021 [55] | AC + I-PRF | 6.2 | 2.8 * | 1.0 * | N/A | 0.4 * | N/A | N/A | 6.5% * |
| AC | 5.9 | 4.6 | 3.6 * | N/A | 3.0 * | N/A | N/A | 50.1% * |
| First Author, Publication Year | Patient Group | Initial Value | After 7–10 Days | After 1 Month | After 2 Months | After 3 Months | After 6 Months | After 12 Months | Effect after 3 Months (the Higher the Better) |
|---|---|---|---|---|---|---|---|---|---|
| Ghoneim, 2022 [53] | AC + I-PRF | 31.5 | 44.7 * | N/A | N/A | 48.3 * | 50.2 * | N/A | 153.3% |
| AC | 36.2 | 40.4 * | N/A | N/A | 42.4 * | 43.8 * | N/A | 117.1% * | |
| Isik, 2022 [54] | AC + I-PRF | 33.3 | N/A | 39.1 * | 40.2 * | 40.4 * | 40.8 * | 40.6 * | 121.3% * |
| AC | 33.9 | N/A | 37.7 * | 38.8 * | 39.1 * | 39.3 * | 37.8 * | 115.3% * | |
| Karadayi, 2021 [55] | AC + I-PRF | 33.4 | 38.3 | 42.2 * | N/A | 43.8 * | N/A | N/A | 131.1% * |
| AC | 31.7 | 33.9 | 36.0 * | N/A | 38.1 * | N/A | N/A | 120.2% * |
| First Author, Publication Year; TMD Index | Patient Group | Initial Value | After 7–10 Days | After 1 Month | After 3 Months | After 6 Months | Effect after 3 Months (the Lower the Better) |
|---|---|---|---|---|---|---|---|
| Ghoneim, 2022 [53] | AC + I-PRF | 20.0 | 0.0 * | N/A | 0.0 * | 0.0 * | 0.0% * |
| Clicking score | AC | 20.0 | 12.0 * | N/A | 6.0 * | 9.0 * | 30.0% * |
| Karadayi, 2021 [55] | AC + I-PRF | 15.7 | 7.7 | 3.4 * | 2.1 * | N/A | 13.4% * |
| Helkimo index | AC | 15.7 | 11.8 * | 8.4 * | 6.4 * | N/A | 40.8% * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sielski, M.; Chęcińska, K.; Chęciński, M.; Sikora, M. Injectable Platelet-Rich Fibrin (I-PRF) Administered to Temporomandibular Joint Cavities: A Scoping Review. J. Clin. Med. 2023, 12, 3326. https://doi.org/10.3390/jcm12093326
Sielski M, Chęcińska K, Chęciński M, Sikora M. Injectable Platelet-Rich Fibrin (I-PRF) Administered to Temporomandibular Joint Cavities: A Scoping Review. Journal of Clinical Medicine. 2023; 12(9):3326. https://doi.org/10.3390/jcm12093326
Chicago/Turabian StyleSielski, Marcin, Kamila Chęcińska, Maciej Chęciński, and Maciej Sikora. 2023. "Injectable Platelet-Rich Fibrin (I-PRF) Administered to Temporomandibular Joint Cavities: A Scoping Review" Journal of Clinical Medicine 12, no. 9: 3326. https://doi.org/10.3390/jcm12093326
APA StyleSielski, M., Chęcińska, K., Chęciński, M., & Sikora, M. (2023). Injectable Platelet-Rich Fibrin (I-PRF) Administered to Temporomandibular Joint Cavities: A Scoping Review. Journal of Clinical Medicine, 12(9), 3326. https://doi.org/10.3390/jcm12093326








