Improved Accuracy and Safety of Pedicle Screw Placement by Using a Probe with an Electrical Conductivity-Measuring Device during Severe Syndromic and Neuromuscular Scoliosis Spine Surgery
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics Statement
2.2. Patients
2.3. Surgical Procedures, Exposures, and Comparisons
2.4. Radiological Evaluations and Outcome Measures
2.5. Statistical Analysis
3. Results
3.1. Demographic, Clinical, Treatment, and Pedicle Morphological Characteristics of Patients with Syndromic/Neuromuscular Scoliosis
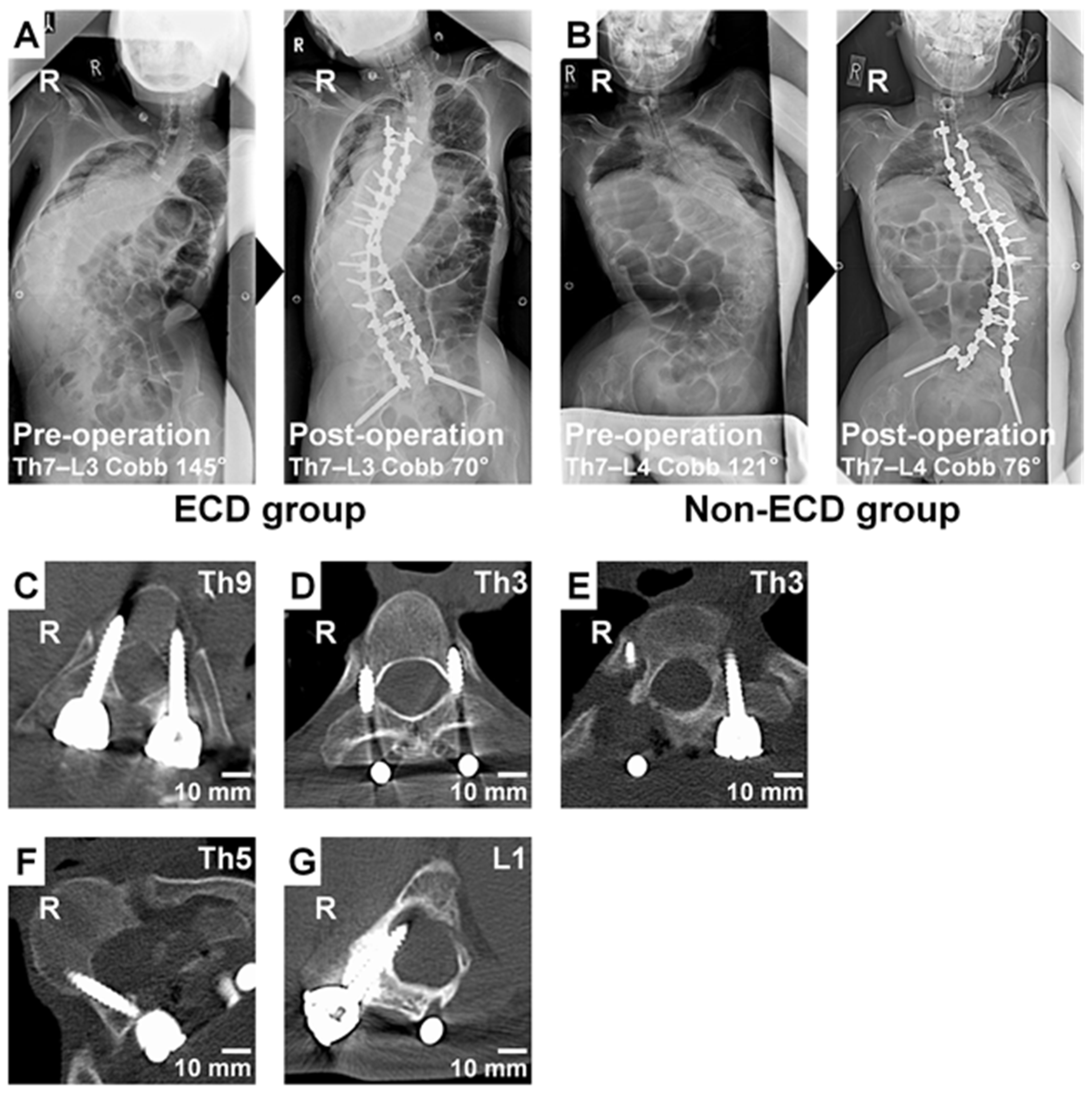
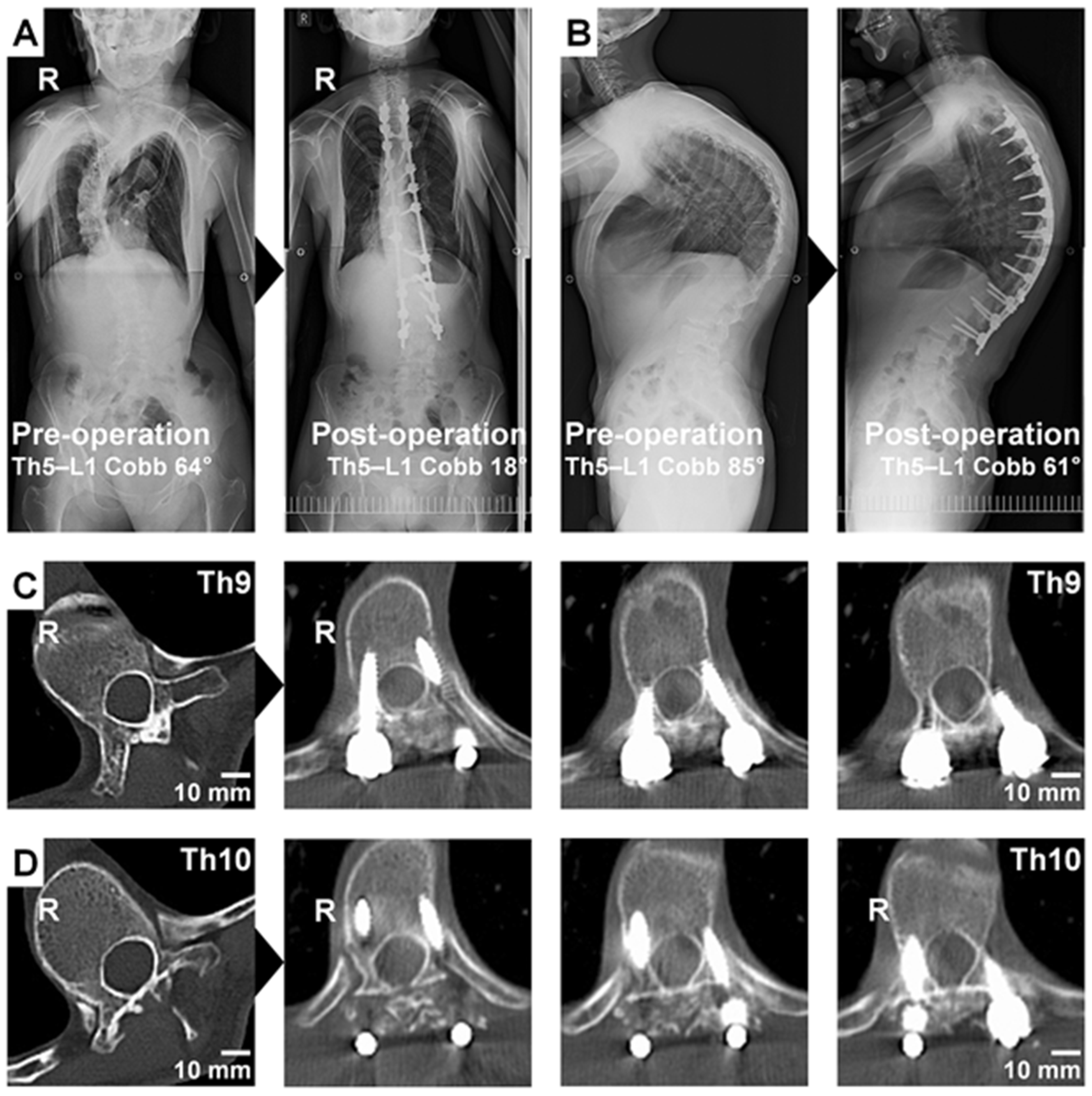
3.2. Pedicle Screw Placement Frequency, Accuracy, and Safety of Patients with Syndromic/Neuromuscular Scoliosis
3.3. Technical Note
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gelalis, I.D.; Paschos, N.K.; Pakos, E.E.; Politis, A.N.; Arnaoutoglou, C.M.; Karageorgos, A.C.; Ploumis, A.; Xenakis, T.A. Accuracy of pedicle screw placement: A systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur. Spine J. 2012, 21, 247–255. [Google Scholar] [CrossRef] [Green Version]
- Samdani, A.F.; Ranade, A.; Sciubba, D.M.; Cahill, P.J.; Antonacci, M.D.; Clements, D.H.; Betz, R.R. Accuracy of free-hand placement of thoracic pedicle screws in adolescent idiopathic scoliosis: How much of a difference does surgeon experience make? Eur. Spine J. 2010, 19, 91–95. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Modi, H.N.; Suh, S.W.; Fernandez, H.; Yang, J.H.; Song, H.R. Accuracy and safety of pedicle screw placement in neuromuscular scoliosis with free-hand technique. Eur. Spine J. 2008, 17, 1686–1696. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- O’Brien, M.F.; Lenke, L.G.; Mardjetko, S.; Lowe, T.G.; Kong, Y.; Eck, K.; Smith, D. Pedicle morphology in thoracic adolescent idiopathic scoliosis: Is pedicle fixation an anatomically viable technique? Spine 2000, 25, 2285–2293. [Google Scholar] [CrossRef]
- Lonstein, J.E. Adolescent idiopathic scoliosis. Lancet 1994, 344, 1407–1412. [Google Scholar] [CrossRef]
- Qiao, J.; Zhu, F.; Xu, L.; Liu, Z.; Sun, X.; Qian, B.; Jiang, Q.; Zhu, Z.; Qiu, Y. Accuracy of pedicle screw placement in patients with Marfan syndrome. BMC Musculoskelet. Disord. 2017, 18, 123. [Google Scholar] [CrossRef] [Green Version]
- Ito, M.; Kakutani, K.; Miyamoto, H.; Suzuki, T.; Yurube, T.; Uno, K. Surgical Outcome of Spinal Fusion for Osteogenesis Imperfecta With Scoliosis: Is the Hybrid System With Pedicle Screws Applicable to Weak, Tiny, and Fragile Vertebrae? J. Pediatr. Orthop. 2021, 41, 368–373. [Google Scholar] [CrossRef]
- Gertzbein, S.D.; Robbins, S.E. Accuracy of pedicular screw placement in vivo. Spine 1990, 15, 11–14. [Google Scholar] [CrossRef]
- Hicks, J.M.; Singla, A.; Shen, F.H.; Arlet, V. Complications of pedicle screw fixation in scoliosis surgery: A systematic review. Spine 2010, 35, E465–E470. [Google Scholar] [CrossRef]
- Suk, S.I.; Kim, W.J.; Lee, S.M.; Kim, J.H.; Chung, E.R. Thoracic pedicle screw fixation in spinal deformities: Are they really safe? Spine 2001, 26, 2049–2057. [Google Scholar] [CrossRef] [PubMed]
- Ryu, K.J.; Suh, S.W.; Kim, H.W.; Lee, D.H.; Yoon, Y.; Hwang, J.H. Quantitative analysis of a spinal surgeon’s learning curve for scoliosis surgery. Bone Jt. J. 2016, 98-B, 679–685. [Google Scholar] [CrossRef]
- Parker, S.L.; McGirt, M.J.; Farber, S.H.; Amin, A.G.; Rick, A.M.; Suk, I.; Bydon, A.; Sciubba, D.M.; Wolinsky, J.P.; Gokaslan, Z.L.; et al. Accuracy of free-hand pedicle screws in the thoracic and lumbar spine: Analysis of 6816 consecutive screws. Neurosurgery 2011, 68, 170–178. [Google Scholar] [CrossRef] [PubMed]
- Rampersaud, Y.R.; Foley, K.T.; Shen, A.C.; Williams, S.; Solomito, M. Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine 2000, 25, 2637–2645. [Google Scholar] [CrossRef]
- Feng, W.; Wang, W.; Chen, S.; Wu, K.; Wang, H. O-arm navigation versus C-arm guidance for pedicle screw placement in spine surgery: A systematic review and meta-analysis. Int. Orthop. 2020, 44, 919–926. [Google Scholar] [CrossRef] [PubMed]
- Verma, R.; Krishan, S.; Haendlmayer, K.; Mohsen, A. Functional outcome of computer-assisted spinal pedicle screw placement: A systematic review and meta-analysis of 23 studies including 5992 pedicle screws. Eur. Spine J. 2010, 19, 370–375. [Google Scholar] [CrossRef] [Green Version]
- Kudo, H.; Wada, K.; Kumagai, G.; Tanaka, S.; Asari, T.; Ishibashi, Y. Accuracy of pedicle screw placement by fluoroscopy, a three-dimensional printed model, local electrical conductivity measurement device, and intraoperative computed tomography navigation in scoliosis patients. Eur. J. Orthop. Surg. Traumatol. 2021, 31, 563–569. [Google Scholar] [CrossRef]
- Uehara, M.; Takahashi, J.; Ikegami, S.; Kuraishi, S.; Shimizu, M.; Futatsugi, T.; Oba, H.; Kato, H. Are pedicle screw perforation rates influenced by distance from the reference frame in multilevel registration using a computed tomography-based navigation system in the setting of scoliosis? Spine J. 2017, 17, 499–504. [Google Scholar] [CrossRef]
- Bolger, C.; Carozzo, C.; Roger, T.; McEvoy, L.; Nagaria, J.; Vanacker, G.; Bourlion, M. A preliminary study of reliability of impedance measurement to detect iatrogenic initial pedicle perforation (in the porcine model). Eur. Spine J. 2006, 15, 316–320. [Google Scholar] [CrossRef]
- Bolger, C.; Kelleher, M.O.; McEvoy, L.; Brayda-Bruno, M.; Kaelin, A.; Lazennec, J.Y.; Le Huec, J.C.; Logroscino, C.; Mata, P.; Moreta, P.; et al. Electrical conductivity measurement: A new technique to detect iatrogenic initial pedicle perforation. Eur. Spine J. 2007, 16, 1919–1924. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allaoui, M.; Zairi, F.; Tetard, M.C.; Gaughan, J.; Chopin, D.; Assaker, R. Contribution of Dynamic Surgical Guidance to the Accurate Placement of Pedicle Screws in Deformity Surgery: A Retrospective Case Series. World Neurosurg. 2018, 120, e466–e471. [Google Scholar] [CrossRef]
- Bai, Y.S.; Niu, Y.F.; Chen, Z.Q.; Zhu, X.D.; Gabriel, L.K.; Wong, H.K.; Li, M. Comparison of the pedicle screws placement between electronic conductivity device and normal pedicle finder in posterior surgery of scoliosis. J. Spinal Disord. Tech. 2013, 26, 316–320. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaput, C.D.; George, K.; Samdani, A.F.; Williams, J.I.; Gaughan, J.; Betz, R.R. Reduction in radiation (fluoroscopy) while maintaining safe placement of pedicle screws during lumbar spine fusion. Spine 2012, 37, E1305–E1309. [Google Scholar] [CrossRef] [Green Version]
- Suess, O.; Schomacher, M. Control of Pedicle Screw Placement with an Electrical Conductivity Measurement Device: Initial Evaluation in the Thoracic and Lumbar Spine. Adv. Med. 2016, 2016, 4296294. [Google Scholar] [CrossRef] [Green Version]
- Ovadia, D.; Korn, A.; Fishkin, M.; Steinberg, D.M.; Wientroub, S.; Ofiram, E. The contribution of an electronic conductivity device to the safety of pedicle screw insertion in scoliosis surgery. Spine 2011, 36, E1314–E1321. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dixon, D.; Darden, B., 2nd; Casamitjana, J.; Weissmann, K.A.; Cristobal, S.; Powell, D.; Baluch, D. Accuracy of a dynamic surgical guidance probe for screw insertion in the cervical spine: A cadaveric study. Eur. Spine J. 2017, 26, 1149–1153. [Google Scholar] [CrossRef]
- Guillen, P.T.; Knopper, R.G.; Kroger, J.; Wycliffe, N.D.; Danisa, O.A.; Cheng, W.K. Independent assessment of a new pedicle probe and its ability to detect pedicle breach: A cadaveric study. J. Neurosurg. Spine 2014, 21, 821–825. [Google Scholar] [CrossRef] [Green Version]
- Sandhu, F.A.; McGowan, J.E.; Felbaum, D.R.; Syed, H.R.; Mueller, K.B. S2-AI screw placement with the aide of electronic conductivity device monitoring: A retrospective analysis. Eur. Spine J. 2017, 26, 2941–2950. [Google Scholar] [CrossRef]
- Zeller, R.; Canavese, F.; Kulkarni, A.V.; Drake, J. Technique for drilling instrument monitoring electrical conductivity in pediatric cervical spine screw insertion: A preliminary report. J. Pediatr. Orthop. 2009, 29, 760–764. [Google Scholar] [CrossRef] [PubMed]
- Aoude, A.A.; Fortin, M.; Figueiredo, R.; Jarzem, P.; Ouellet, J.; Weber, M.H. Methods to determine pedicle screw placement accuracy in spine surgery: A systematic review. Eur. Spine J. 2015, 24, 990–1004. [Google Scholar] [CrossRef]
- Kwan, M.K.; Chiu, C.K.; Gani, S.M.A.; Wei, C.C.Y. Accuracy and Safety of Pedicle Screw Placement in Adolescent Idiopathic Scoliosis Patients: A Review of 2020 Screws Using Computed Tomography Assessment. Spine 2017, 42, 326–335. [Google Scholar] [CrossRef]
- Modi, H.N.; Suh, S.W.; Yang, J.H.; Cho, J.W.; Hong, J.Y.; Singh, S.U.; Jain, S. Surgical complications in neuromuscular scoliosis operated with posterior- only approach using pedicle screw fixation. Scoliosis 2009, 4, 11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| n (%) | |
|---|---|
| Cerebral palsy | 5 (23.8) |
| Marfan syndrome | 4 (19.0) |
| Neurofibromatosis type I/von Recklinghausen | 3 (14.3) |
| Muscle dystrophy | 1 (4.8) |
| Loeys–Dietz syndrome | 1 (4.8) |
| Sotos syndrome | 1 (4.8) |
| Congenital myopathy | 1 (4.8) |
| Escobar syndrome | 1 (4.8) |
| Arthrogryposis multiplex congenita | 1 (4.8) |
| Astrocytoma | 1 (4.8) |
| Osteoblastoma | 1 (4.8) |
| Prune belly syndrome | 1 (4.8) |
| Patients Undergoing Surgery with ECD | Patients Undergoing Surgery with Non-ECD | p | |
|---|---|---|---|
| (n = 11) | (n = 10) | ||
| Age, mean ± SD [years] | 22.4 ± 14.0 | 20.5 ± 7.0 | 0.71 * |
| Male/female sex, n (%) | 6 (54.5)/5 (45.5) | 5 (50.0)/5 (50.0) | 0.84 ** |
| Preoperative Cobb angle, mean ± SD [°] | 83.4 ± 26.0 | 82.3 ± 28.0 | 0.92 * |
| Postoperative Cobb angle, mean ± SD [°] | 41.8 ± 18.4 | 45.7 ± 23.4 | 0.67 * |
| Correction rate of the Cobb angle, mean ± SD [%] | 49.7 ± 18.3 | 46.5 ± 18.6 | 0.70 * |
| Number of the fixed vertebrae, mean ± SD [no.] | 11.9 ± 1.5 | 13.4 ± 1.8 | 0.05 * |
| Operation time, mean ± SD [min] | 478.5 ± 97.5 | 596.8 ± 205.0 | 0.10 * |
| Blood loss, mean ± SD [g] | 2489.7 ± 2020.3 | 2872.2 ± 1294.6 | 0.62 * |
| Pedicles Undergoing Screw Hole Preparation with ECD | Pedicles Undergoing Screw Hole Preparation with Non-ECD | p | |
|---|---|---|---|
| (n = 284) | (n = 288) | ||
| Diameter in the thoracic spine, mean ± SD [mm] | 3.14 ± 1.82 | 3.44 ± 1.98 | 0.13 * |
| Diameter in the lumbar spine, mean ± SD [mm] | 5.52 ± 2.90 | 4.93 ± 2.77 | 0.16 * |
| Pedicles Undergoing Screw Hole Preparation with ECD | Pedicles Undergoing Screw Hole Preparation with Non-ECD | p | |
|---|---|---|---|
| (n = 284) | (n = 288) | ||
| Screw placement, n (%) | 249 (87.7) | 211 (73.3) | <0.01 *,† |
| Pedicles Undergoing Screw Placement with ECD | Pedicles Undergoing Screw Placement with Non-ECD | p | |
|---|---|---|---|
| (n = 249) | (n = 211) | ||
| Acceptable pedicle screw placement | |||
| Intrapedicular position, n (%) | 125 (50.2) | 89 (42.2) | 0.09 * |
| Intrapedicular or <2-mm lateral/cranial position, n (%) | 167 (67.1) | 120 (56.9) | 0.02 *,† |
| Mechanically threatening pedicle screw misplacement | |||
| ≥2-mm lateral/cranial malposition, n (%) | 37 (14.9) | 48 (22.7) | 0.03 *,† |
| ≥5-mm lateral/cranial malposition, n (%) | 4 (1.6) | 11 (5.2) | 0.04 **,† |
| Neurologically threatening pedicle screw misplacement | |||
| Medial/caudal malposition, n (%) | 45 (18.1) | 43 (20.4) | 0.53 * |
| ≥2-mm medial/caudal malposition, n (%) | 8 (3.2) | 11 (5.2) | 0.28 * |
| ≥5-mm medial/caudal malposition, n (%) | 0 (0.0) | 5 (2.4) | 0.02 **,† |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yurube, T.; Kanda, Y.; Ito, M.; Takeoka, Y.; Suzuki, T.; Uno, K.; Kuroda, R.; Kakutani, K. Improved Accuracy and Safety of Pedicle Screw Placement by Using a Probe with an Electrical Conductivity-Measuring Device during Severe Syndromic and Neuromuscular Scoliosis Spine Surgery. J. Clin. Med. 2022, 11, 419. https://doi.org/10.3390/jcm11020419
Yurube T, Kanda Y, Ito M, Takeoka Y, Suzuki T, Uno K, Kuroda R, Kakutani K. Improved Accuracy and Safety of Pedicle Screw Placement by Using a Probe with an Electrical Conductivity-Measuring Device during Severe Syndromic and Neuromuscular Scoliosis Spine Surgery. Journal of Clinical Medicine. 2022; 11(2):419. https://doi.org/10.3390/jcm11020419
Chicago/Turabian StyleYurube, Takashi, Yutaro Kanda, Masaaki Ito, Yoshiki Takeoka, Teppei Suzuki, Koki Uno, Ryosuke Kuroda, and Kenichiro Kakutani. 2022. "Improved Accuracy and Safety of Pedicle Screw Placement by Using a Probe with an Electrical Conductivity-Measuring Device during Severe Syndromic and Neuromuscular Scoliosis Spine Surgery" Journal of Clinical Medicine 11, no. 2: 419. https://doi.org/10.3390/jcm11020419
APA StyleYurube, T., Kanda, Y., Ito, M., Takeoka, Y., Suzuki, T., Uno, K., Kuroda, R., & Kakutani, K. (2022). Improved Accuracy and Safety of Pedicle Screw Placement by Using a Probe with an Electrical Conductivity-Measuring Device during Severe Syndromic and Neuromuscular Scoliosis Spine Surgery. Journal of Clinical Medicine, 11(2), 419. https://doi.org/10.3390/jcm11020419







