Nursing Students’ Knowledge, Awareness, and Experiences of Emergency Contraception Pills’ Use
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Measures
2.3. Data Collection
2.4. Ethical Aspects
2.5. Data Analysis
3. Results
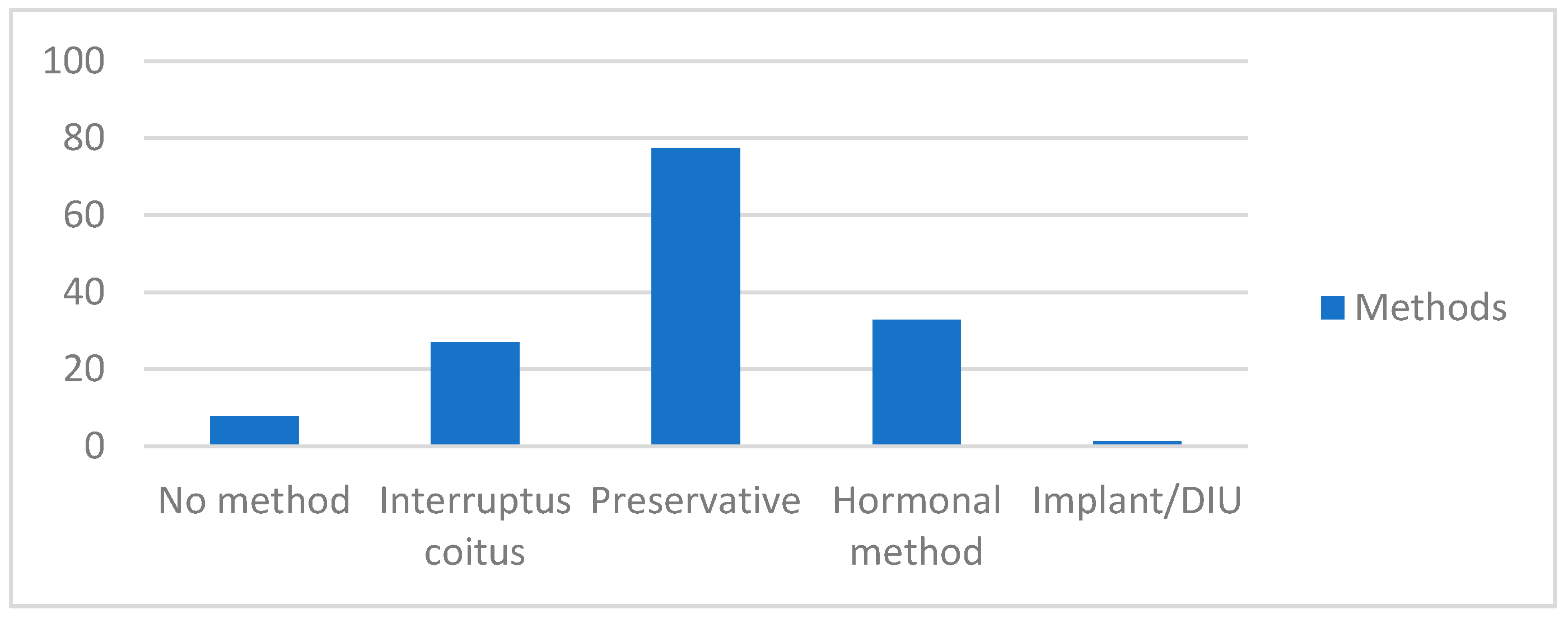
3.1. ECP Use and Attitudes
3.2. Knowledge about ECP
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- FIGO. Mechanism of Action for Emergency Contraception|FIGO. 2021. Available online: https://www.figo.org/mechanism-action-emergency-contraception (accessed on 22 November 2021).
- Leelakanok, N.; Methaneethorn, J. A Systematic Review and Meta-analysis of the Adverse Effects of Levonorgestrel Emergency Oral Contraceptive. Clin. Drug Investig. 2020, 40, 395–420. [Google Scholar] [CrossRef] [PubMed]
- Raine, T.R.; Harper, C.C.; Rocca, C.H.; Fischer, R.; Padian, N.; Klausner, J.D.; Darney, P.D. Direct access to emergency contraception through pharmacies and effect on unintended pregnancy and STIs: A randomized controlled trial. JAMA 2005, 293, 54–62. [Google Scholar] [CrossRef]
- Jambrina, A.M.; Rius, P.; Gascón, P.; Armelles, M.; Camps-Bossacoma, M.; Franch, À.; Rabanal, M. Characterization of the Use of Emergency Contraception from Sentinel Pharmacies in a Region of Southern Europe. J. Clin. Med. 2021, 10, 2793. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, R.M.; Kalckmann, S.; Arilha, M.; Giacomo do Lago, T.D. The emergency contraceptive pill in Brazil: High usage rates but schooling differences persist. Contraception 2021, 104, 401–405. [Google Scholar] [CrossRef] [PubMed]
- Hussain, R.; Kavanaugh, M.L. Changes in use of emergency contraceptive pills in the United States from 2008 to 2015. Contraception 2021, 10, 100065. [Google Scholar] [CrossRef]
- Bauzà, M.L.; Esteva, M.; Molina, J.; Pereiró, I.; Ingla, M.; March, S. Emergency contraception and risk habits in a university population. Eur. J. Contracept. Reprod. Health Care 2018, 23, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Heller, C.; Perreira, K.M.; Shartzer, A.; Johnston, E.M.; Courtot, B. Emergency Contraception Use: The Influence of Awareness, Attitudes, and Beliefs among Non-Hispanic White, Non-Hispanic Black, and Hispanic Women in the United States. Women’s Health Issues 2019, 29, 161–169. [Google Scholar] [CrossRef]
- Chofakian, C.B.; Moreau, C.; Borges, A.L.V.; Dos Santos, O.A. Contraceptive discontinuation: Frequency and associated factors among undergraduate women in Brazil. Reprod. Health 2019, 16, 131. [Google Scholar] [CrossRef] [PubMed]
- Nappi, R.E.; Lobo Abascal, P.; Mansour, D.; Rabe, T.; Shojai, R. Emergency Contraception Study Group. Use of and attitudes towards emergency contraception: A survey of women in five European countries. Eur. J. Contracept. Reprod. Health Care 2014, 19, 93–101. [Google Scholar] [CrossRef]
- Williams, B.N.; Jauk, V.C.; Szychowski, J.M.; Arbuckle, J.L. Adolescent emergency contraception usage, knowledge, and perception. Contraception 2021, 103, 361–366. [Google Scholar] [CrossRef]
- Jiménez-Iglesias, A.; Moreno, C.; García-Moya, I.; Rivera, F. Prevalence of emergency contraceptive pill use among Spanish adolescent girls and their family and psychological profiles. BMC Women’s Health 2018, 18, 67. [Google Scholar] [CrossRef]
- Leon-Larios, F.; Macías-Seda, J. Factors related to healthy sexual and contraceptive behaviors in undergraduate students at university of Seville: A cross-sectional study. Reprod. Health 2017, 14, 179. [Google Scholar] [CrossRef]
- Martínez, J.L.; Vicario-Molina, I.; González, E.; Ilabaca, P. Sex education in Spain: The relevance of teachers’ training and attitudes/Educación sexual en España: Importancia de la formación y las actitudes del profesorado. J. Study Educ. Dev. 2014, 37, 117–148. [Google Scholar] [CrossRef]
- Morales, A.; Espada, J.P.; Orgilés, M. A 1-year follow-up evaluation of a sexual-health education program for Spanish adolescents compared with a well-established program. Eur. J. Public Health 2016, 26, 35–41. [Google Scholar] [CrossRef]
- Morales, A.; Orgilés, M.; Espada, J.P. Sexually Unexperienced Adolescents Benefit the Most From a Sexual Education Program for Adolescents: A Longitudinal Cluster Randomized Controlled Study. AIDS Educ. Prev. 2020, 32, 493–511. [Google Scholar] [CrossRef]
- Amengual, M.L.; Canto, M.E.; Berenguer, I.P.; Pol, M.I. Systematic Review of the profile of emergency contraception users. Rev. Lat. Am. Enfermagem 2016, 24, e2733. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sharon, D.; Gonen, A.; Linetsky, I. Factors influencing nursing students’ intention to practice sexuality education in their professional work. Am. J. Sex. Educ. 2020, 15, 262–278. [Google Scholar] [CrossRef]
- Abera, L.; Sema, A.; Guta, A.; Belay, Y. Emergency contraceptive utilization and associated factors among college students in Dire Dawa City, Eastern Ethiopia: A cross-sectional study. Eur. J. Midwifery 2021, 5, 28. [Google Scholar] [CrossRef] [PubMed]
- Addo, V.N.; Tagoe-Darko, E.D. Knowledge, practices, and attitudes regarding emergency contraception among students at a university in Ghana. Int. J. Gynaecol. Obstet. 2009, 105, 206–209. [Google Scholar] [CrossRef]
- Bauzà-Amengual, M.L.; Esteva, M.; Ingla-Pol, M.; Font-Oliver, M.A.; March, S. Discourses on the postcoital pill in young women. BMC Public Health 2018, 18, 803. [Google Scholar] [CrossRef] [PubMed]
- Asut, O.; Ozenli, O.; Gur, G.; Deliceo, E.; Cagin, B.; Korun, O.; Turk, O.; Vaizoglu, S.; Cali, S. The knowledge and perceptions of the first year medical students of an International University on family planning and emergency contraception in Nicosia (TRNC). BMC Women’s Health 2018, 18, 149. [Google Scholar] [CrossRef]
- Hoque, M.E.; Ghuman, S. Knowledge, practices, and attitudes of emergency contraception among female university students in KwaZulu-Natal, South Africa. PLoS ONE 2012, 7, e46346. [Google Scholar] [CrossRef][Green Version]
- Black, K.I.; Geary, R.; French, R.; Leefe, N.; Mercer, C.H.; Glasier, A.; Macdowall, W.; Gibson, L.; Datta, J.; Palmer, M.; et al. Trends in the use of emergency contraception in Britain: Evidence from the second and third National Surveys of Sexual Attitudes and Lifestyles. BJOG 2016, 123, 1600–1607. [Google Scholar] [CrossRef] [PubMed]
- Chandna, A.; Nath, J.; Dhingra, D. Awareness of emergency contraception among 1st year medical students. Int. J. Contemp. Med. Res. 2016, 3. [Google Scholar] [CrossRef]
- Lehan Mackin, M.; Clark, M.K.; McCarthy, A.M.; Farris, K. Knowledge and use of emergency contraception in college women. West. J. Nurs. Res. 2015, 37, 462–480. [Google Scholar] [CrossRef]
- Shiferaw, B.Z.; Gashaw, B.T.; Tesso, F.Y. Factors associated with utilization of emergency contraception among female students in Mizan-Tepi University, South West Ethiopia. BMC Res. Notes 2015, 8, 817. [Google Scholar] [CrossRef]
- Miller, L.M. College student knowledge and attitudes toward emergency contraception. Contraception 2011, 83, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Kgosiemang, B.; Blitz, J. Emergency contraceptive knowledge, attitudes and practices among female students at the University of Botswana: A descriptive survey. Afr. J. Prim. Health Care Fam. Med. 2018, 10, e1–e6. [Google Scholar] [CrossRef]
- Bastianelli, C.; Rosato, E.; Farris, M.; Benagiano, G. Emergency contraception: A survey of 1773 women. Eur. J. Contracept. Reprod. Health Care 2016, 21, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Fontes, E.; Guerreiro, J.; Costa, T.; Miranda, A. Pattern of use of emergency oral contraception among Portuguese women. Pharm. World Sci. 2010, 32, 496–502. [Google Scholar] [CrossRef] [PubMed]
- Collins, J.C.; Schneider, C.R.; Moles, R.J. Emergency contraception supply in Australian pharmacies after the introduction of ulipristal acetate: A mystery shopping mixed-methods study. Contraception 2018, 98, 243–246. [Google Scholar] [CrossRef] [PubMed]
- Glasier, A.F.; Cameron, S.T.; Fine, P.M.; Logan, S.J.; Casale, W.; Van Horn, J.; Sogor, L.; Blithe, D.L.; Scherrer, B.; Mathe, H.; et al. Ulipristal acetate versus levonorgestrel for emergency contraception: A randomised non-inferiority trial and meta-analysis. Lancet 2010, 375, 555–562. [Google Scholar] [CrossRef]
- Cwiak, C.; Howard, B.; Hsieh, J.; Ricciotti, N.; Sucato, G.S. Sexual and Contraceptive Behaviors among Adolescents Requesting Emergency Contraception. J. Pediatr. Adolesc. Gynecol. 2016, 29, 643–647. [Google Scholar] [CrossRef]
- Bastianelli, C.; Farris, M.; Benagiano, G. Reasons for requesting emergency contraception: A survey of 506 Italian women. Eur. J. Contracept. Reprod. Health Care 2005, 10, 157–163. [Google Scholar] [CrossRef]
- Chofakian, C.B.D.N.; Moreau, C.; Borges, A.L.V.; Santos, O.A.D. Contraceptive patterns after use of emergency contraception among female undergraduate students in Brazil. Eur. J. Contracept. Reprod. Health Care 2018, 23, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Hansen, C.C.; Svare, E.I.; Petersen, R.H.; Bock, J.E. Hvem anvender nødpraevention? [Who are the users of emergency contraception?]. Ugeskr Laeger 2002, 164, 5003–5005. [Google Scholar]
- Frost, J.J.; Lindberg, L.D.; Finer, L.B. Young adults’ contraceptive knowledge, norms and attitudes: Associations with risk of unintended pregnancy. Perspect. Sex. Reprod. Health 2012, 44, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Von Rosen, F.T.; von Rosen, A.J.; Müller-Riemenschneider, F.; Tinnemann, P. Awareness and knowledge regarding emergency contraception in Berlin adolescents. Eur. J. Contracept. Reprod. Health Care 2017, 22, 45–52. [Google Scholar] [CrossRef]
- Veloso, D.L.; Peres, V.C.; Lopes, J.S.; Salge, A.K.; Guimarães, J.V. Anticoncepção de emergência: Conhecimento e atitude de acadêmicos de enfermagem [Emergency contraception: Knowledge and attitudes of nursing students]. Rev. Gaucha Enferm 2014, 35, 33–39. (In Portuguese) [Google Scholar] [CrossRef][Green Version]
- Cleland, K.; Raymond, E.G.; Westley, E.; Trussell, J. Emergency contraception review: Evidence-based recommendations for clinicians. Clin. Obstet. Gynecol. 2014, 57, 741–750. [Google Scholar] [CrossRef]
- Raymond, E.G.; Halpern, V.; Lopez, L.M. Pericoital oral contraception with levonorgestrel: A systematic review. Obstet. Gynecol. 2011, 117, 673–681. [Google Scholar] [CrossRef] [PubMed]
- Downing, A. University students’ knowledge and attitudes toward emergency contraception pills. J. Community Health Nurs. 2014, 31, 75–89. [Google Scholar] [CrossRef]
- Garrett, K.P.; Widman, L.; Francis, D.B.; Noar, S.M. Emergency contraception: Sources of information and perceptions of access among young adults. Women Health 2016, 56, 668–679. [Google Scholar] [CrossRef]
- Davis, P.; Sarasveni, M.; Krishnan, J.; Bhat, L.D.; Kodali, N.K. Knowledge and attitudes about the use of emergency contraception among college students in Tamil Nadu, India. J. Egypt. Public Health Assoc. 2020, 95, 1. [Google Scholar] [CrossRef]
- Richards, M.J.; Peters, M.; Sheeder, J.; Kaul, P. Contraception and Adolescent Males: An Opportunity for Providers. J. Adolesc. Health 2016, 58, 366–368. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Coronado, P.J.; Delgado-Miguel, C.; Rey-Cañas, A.; Herráiz, M.A. Sexual and reproductive health in Spanish University Students. A comparison between medical and law students. Sex. Reprod. Healthc. 2017, 11, 97–101. [Google Scholar] [CrossRef] [PubMed]

| Socio-Demographic Variables | Total % (n) 100 (478) | Men 1 % (n) 18.8 (90) | Women % (n) 81.2 (288) | p-Value |
|---|---|---|---|---|
| Age (years), Mean (SD) | 20.87 (4.52) | 22.13 (6.48) | 20.58 (3.88) | 0.003 |
| Sexual orientation, % (n) | ||||
| Heterosexual | 86.2 (412) | 84.3 (75) | 87.1 (337) | |
| Homosexual | 3.1 (15) | 10.1 (9) | 1.6 (6) | n.a. 2 |
| Bisexual | 10.3 (49) | 5.6 (5) | 11.4 (44) | |
| Have you had any intercourse? Yes, % (n) | 83.9 (401) | 93.3 (84) | 81.7 (317) | 0.006 |
| Age of first sexual intercourse, Median (SD) | 16.53 (1.46) | 16.99 (1.57) | 16.41 (1.41) | 0.001 |
| Received any information on the ECP, Yes, % (n) | 70.5 (337) | 74.4 (67) | 69.6 (270) | 0.442 |
| Item | Men | Women | p-Value |
|---|---|---|---|
| Correct (n)% | Correct (n)% | ||
| 1. ECP are abortive, lead to embryo abortion, False | 58.9 (53) | 75.5 (293) | 0.001 |
| 2. A medical prescription is needed to purchase the postcoital pill, False | 82.2 (74) | 87.9 (341) | 0.167 |
| 3. If the woman is pregnant, the pill may harm the zygote or embryo, False | 48.9 (44) | 46.6 (181) | 0.726 |
| 4. The ECP protect against sexual transmission infections (STI), False | 100 (90) | 98.2 (381) | 0.357 |
| 5. There is one type of oral emergency contraception that can be used within 5 days after risk of pregnancy sex, True | 38.9 (35) | 35.3 (137) | 0.543 |
| 6. Morning-after pill affects women’s reproductive health in the long term, reducing the possibilities to conceive on later life stages, False | 50 (45) | 49.7 (193) | 1.000 |
| 7. Efficacy of postcoital contraception is reduced each hour after risk of pregnancy sex, True | 75.6 (68) | 78.4 (304) | 0.575 |
| 8. A pregnancy test is required prior to take ECP, False | 83.3 (75) | 86.1 (334) | 0.507 |
| 9. Postcoital pills can be used whenever necessary, without affecting its efficacy, True | 5.6 (5) | 6.7 (26) | 0.816 |
| 10. ECP is a contraceptive method, False | 50 (45) | 66.8 (259) | 0.004 |
| Crude OR (95% CI) | p-Value | Adjusted OR (95% CI) | p-Value | |
|---|---|---|---|---|
| Age * (older than 20 years) | 3.08 (1.98; 4.79) | <0.001 | 3.04 (1.92; 4.79) | <0.001 |
| Sex (Woman) | 2.90 (1.53; 5.47) | 0.001 | 2.87 (1.47; 5.61) | 0.002 |
| Had you ever received any information/guidance on postcoital contraception? (Yes) | 1.26 (0.77; 2.06) | 0.35 | ||
| Contraceptive Methods ** (Withdrawal/No method) | 2.02 (1.31; 3.12) | 0.001 | 1.90 (1.20; 3.01) | 0.006 |
| Total score | 1.19 (1.05; 1.37) | 0.008 | 1.16 (1.01; 1.34) | 0.032 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leon-Larios, F.; Ruiz-Ferron, C.; Jalon-Neira, R.-M.; Praena-Fernández, J.-M. Nursing Students’ Knowledge, Awareness, and Experiences of Emergency Contraception Pills’ Use. J. Clin. Med. 2022, 11, 418. https://doi.org/10.3390/jcm11020418
Leon-Larios F, Ruiz-Ferron C, Jalon-Neira R-M, Praena-Fernández J-M. Nursing Students’ Knowledge, Awareness, and Experiences of Emergency Contraception Pills’ Use. Journal of Clinical Medicine. 2022; 11(2):418. https://doi.org/10.3390/jcm11020418
Chicago/Turabian StyleLeon-Larios, Fatima, Cecilia Ruiz-Ferron, Rocio-Marina Jalon-Neira, and Juan-Manuel Praena-Fernández. 2022. "Nursing Students’ Knowledge, Awareness, and Experiences of Emergency Contraception Pills’ Use" Journal of Clinical Medicine 11, no. 2: 418. https://doi.org/10.3390/jcm11020418
APA StyleLeon-Larios, F., Ruiz-Ferron, C., Jalon-Neira, R.-M., & Praena-Fernández, J.-M. (2022). Nursing Students’ Knowledge, Awareness, and Experiences of Emergency Contraception Pills’ Use. Journal of Clinical Medicine, 11(2), 418. https://doi.org/10.3390/jcm11020418







