Reasons for Utilizing Telemedicine during and after the COVID-19 Pandemic: An Internet-Based International Study
Abstract
1. Introduction
- Prior deployment of telemedicine services by healthcare providers;
- A limited number of socio-demographic variables;
- Specific personal reasons (family influence, previous experience, and location).
2. Materials and Methods
2.1. Participants
2.2. Data Preparation
2.3. Statistical Analysis
3. Results
3.1. Socio-Demographic Characteristics
3.2. Prior Use of Online Medical and Non-Medical Services
3.3. Health Services Consumption
3.3.1. Consumers’ Habits
3.3.2. Non-Queue Requests
- scheduling an appointment with a healthcare practitioner;
- asking for a prescription or prescription renewal;
- requesting a sickness leave/certificate of absence;
- asking for a referral to a specialist;
- getting laboratory or imaging test results;
- purchasing drugs at an online accredited pharmacy.
3.3.3. Teleconsultation and Biometry
3.4. Participants’ Reasons for Using Telemedicine during and after the COVID-19 Pandemic
3.4.1. Family, Friends, and Others
3.4.2. Saving Time
3.5. Technology and Communication as Users’ Satisfaction Triggers
3.5.1. Technological Issues
3.5.2. Communication Issues
3.5.3. User Satisfaction and the Impact of the Pandemic
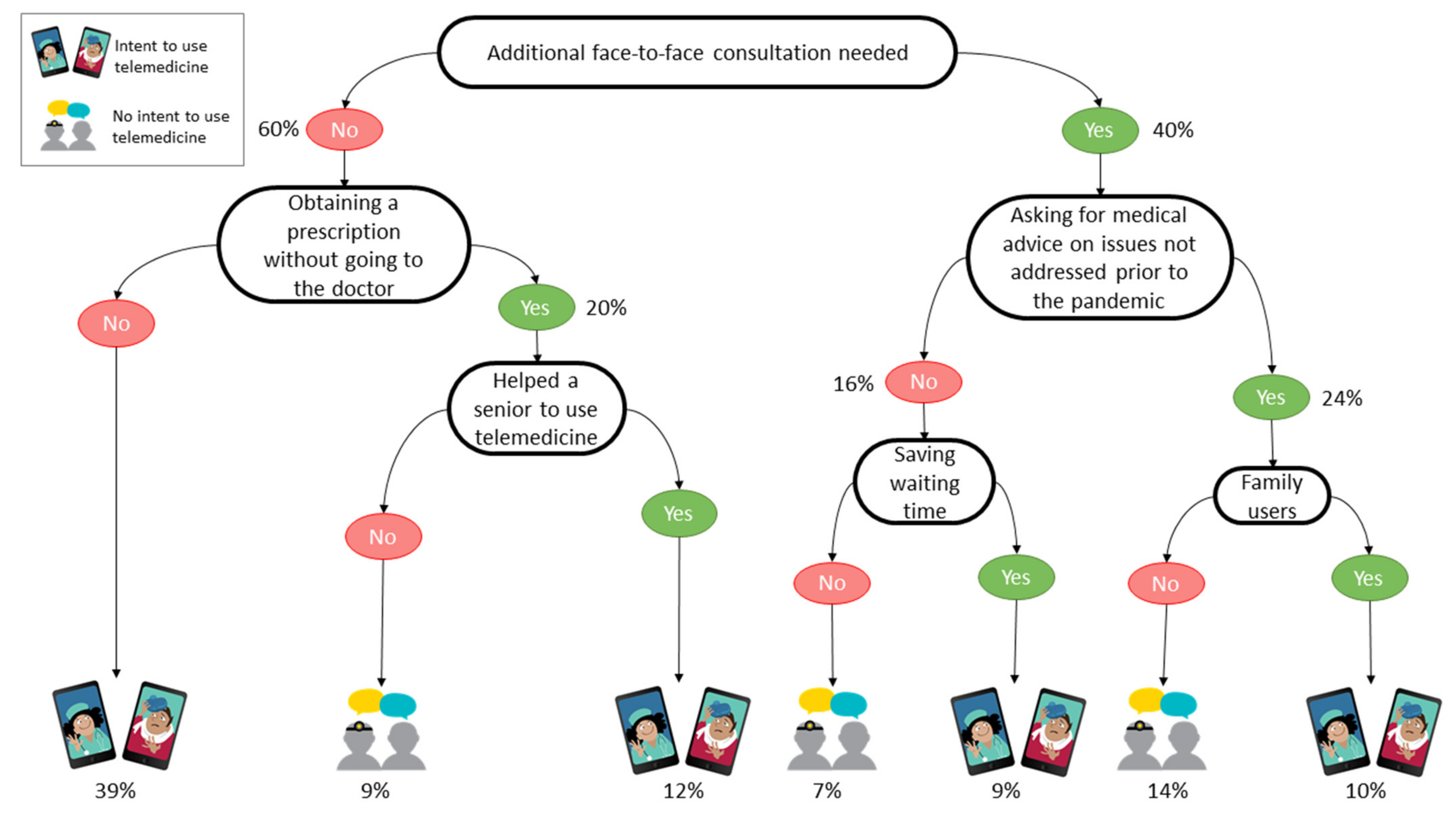
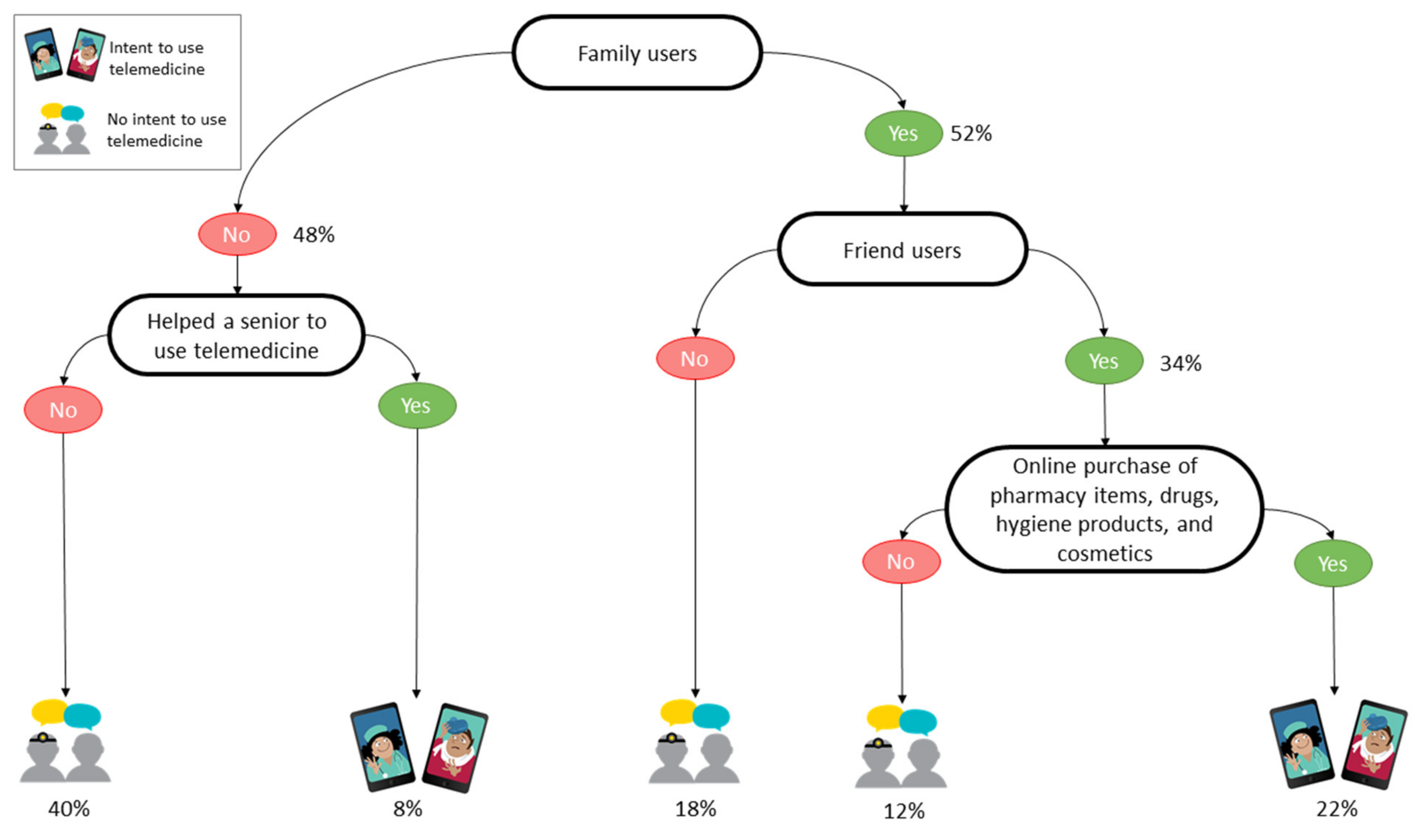
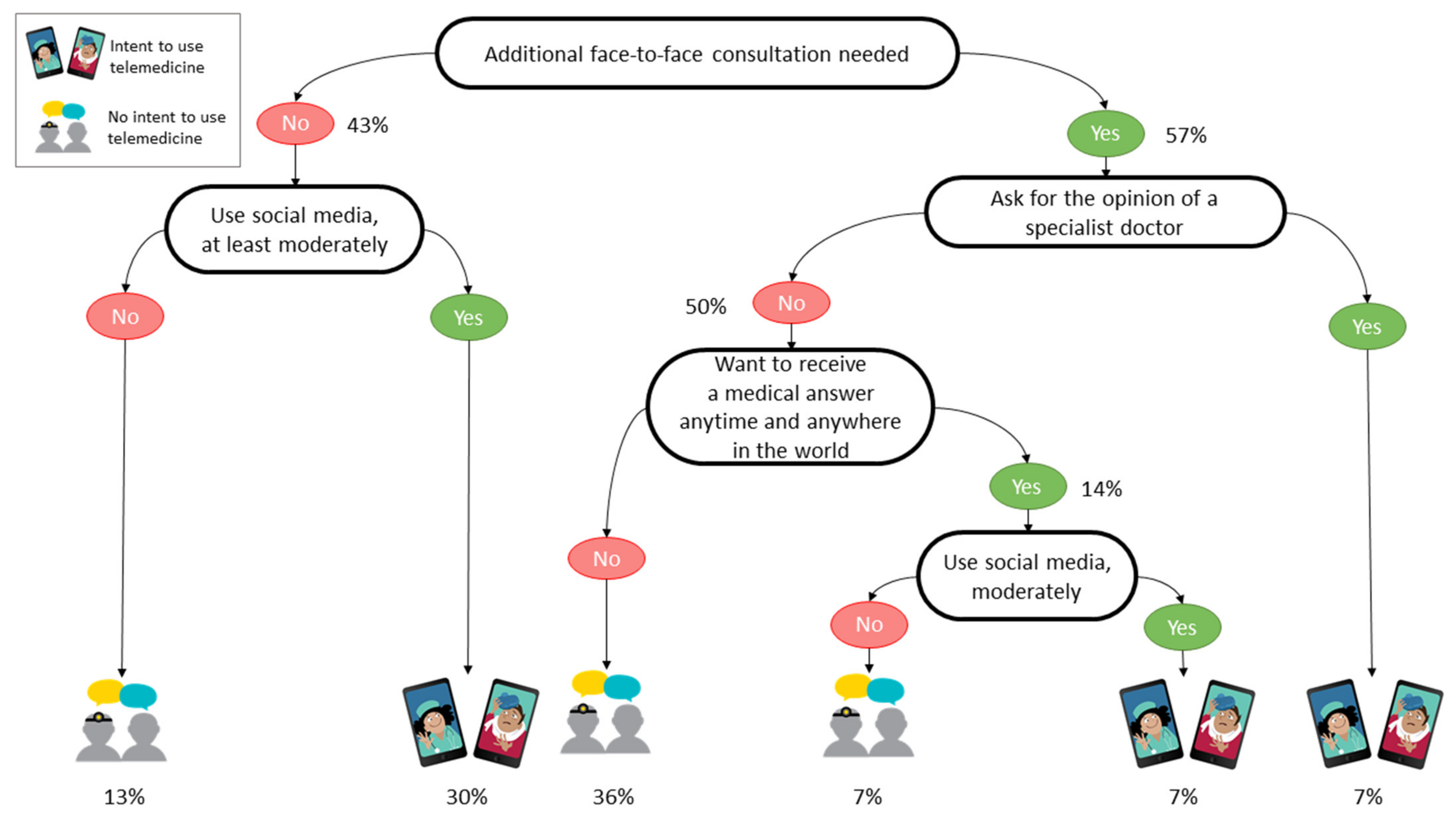
3.6. Multivariate Analysis with Decision Trees
4. Discussion
4.1. Principal Findings
- The overall survey results show that about 40% of the participants intend to continue using telemedicine after the COVID-19 pandemic (188/473, 39.7%). A higher proportion of the Israeli than other participants intend to continue using telemedicine services after the pandemic. It is important to point out that telemedicine have been well-established as a part of the HMOs services in Israel for the last decade [57,58], increasingly used as a standard of care since the beginning of the 2000s [59].
- The major factor influencing the intent to use telemedicine is that a teleconsultation must not require an additional face-to-face consultation in person.
- Moreover, prior use of online services does not always influence the intent to use telemedicine. However, prior use of non-medical online services does help patients to use and to continue to use telemedicine tools. For Israeli participants, frequent use of social media relates to a higher intent to use telemedicine than it does for those in other countries. Additionally, searching for medical information on the Internet increases the intention to be a telemedicine user.
- Non-Queue Requests are appreciated by the survey’s participants, and especially by the Israelis. However, it is critical to bear in mind that delivering medical documents raises ethical and legal issues, such as whether to rely on a patient’s online history and whether to renew a prescription without examining the patient [60,61].
- Triggers for using telemedicine include being close to people who have used it, the need to feel safe by reducing the number of physical contacts, and the perception that it saves time by reducing unnecessary visits to the provider.
- A crisis situation such as the COVID-19 pandemic has an influence on perceptions of telemedicine and so points out the need for the healthcare system to be prepared for drastic changes at any time and to be reactive when it is called for.
4.2. Strengths and Limitations
5. Conclusions
5.1. Implications for Healthcare Practice
5.2. Current and Potential Future Research Directions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Variable | Intention to Use Telemedicine in the Future | ||||
|---|---|---|---|---|---|
| Overall (n = 272) | Intent (n = 139) | Undecided (n = 79) | No Intent (n = 54) | p-Value | |
| What is your age? (n = 271) | <0.001 | ||||
| 18–24 | 9 (3.32%) | 3 (2.16%) | 6 (7.59%) | 0 (0.00%) | |
| 25–34 | 66 (24.4%) | 37 (26.6%) | 16 (20.3%) | 13 (24.5%) | |
| 35–44 | 77 (28.4%) | 42 (30.2%) | 17 (21.5%) | 18 (34.0%) | |
| 45–54 | 68 (25.1%) | 36 (25.9%) | 21 (26.6%) | 11 (20.8%) | |
| 55–64 | 36 (13.3%) | 17 (12.2%) | 12 (15.2%) | 7 (13.2%) | |
| ≥65 | 15 (5.54%) | 4 (2.88%) | 7 (8.86%) | 4 (7.55%) | |
| What is your gender? (n = 271) | 0.515 | ||||
| Female | 188 (69.4%) | 93 (66.9%) | 55 (69.6%) | 40 (75.5%) | |
| Male | 83 (30.6%) | 46 (33.1%) | 24 (30.4%) | 13 (24.5%) | |
| What is your marital status? (n = 272) | 0.087 | ||||
| Single | 36 (13.2%) | 15 (10.8%) | 15 (19.0%) | 6 (11.1%) | |
| Married | 205 (75.4%) | 113 (81.3%) | 54 (68.4%) | 38 (70.4%) | |
| Divorced | 21 (7.72%) | 7 (5.04%) | 9 (11.4%) | 5 (9.26%) | |
| Widower | 6 (2.21%) | 2 (1.44%) | 1 (1.27%) | 3 (5.56%) | |
| No answer | 4 (1.47%) | 2 (1.44%) | 0 (0.00%) | 2 (3.70%) | |
| How many children do you have? (n = 272) | <0.001 | ||||
| 0 | 51 (18.8%) | 22 (15.8%) | 19 (24.1%) | 10 (18.5%) | |
| 1–2 | 158 (58.1%) | 82 (59.0%) | 44 (55.7%) | 32 (59.3%) | |
| 3–4 | 58 (21.3%) | 32 (23.0%) | 15 (19.0%) | 11 (20.4%) | |
| ≥5 | 5 (1.84%) | 3 (2.16%) | 1 (1.27%) | 1 (1.85%) | |
| In what sort of area do you live? (n = 272) | 0.371 | ||||
| City | 249 (91.5%) | 126 (90.6%) | 71 (89.9%) | 52 (96.3%) | |
| Suburb or periphery | 23 (8.46%) | 13 (9.35%) | 8 (10.1%) | 2 (3.70%) | |
| Language used to take the questionnaire (n = 272) | <0.001 | ||||
| Arabic | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | |
| English | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | |
| French | 2 (0.74%) | 1 (0.72%) | 0 (0.00%) | 1 (1.85%) | |
| Hebrew | 141 (51.8%) | 87 (62.6%) | 38 (48.1%) | 16 (29.6%) | |
| Russian | 128 (47.1%) | 51 (36.7%) | 40 (50.6%) | 37 (68.5%) | |
| Spanish | 1 (0.37%) | 0 (0.00%) | 0 (0.00%) | 0 (1.27%) | |
| Variable | Intention to Use Telemedicine in the Future | ||||
|---|---|---|---|---|---|
| Overall (n = 87) | Intent (n = 21) | Undecided (n = 25) | No Intent (n = 41) | p-Value | |
| What is your age? (n = 87) | 0.482 | ||||
| 18–24 | 4 (4.60%) | 1 (4.76%) | 2 (8.00%) | 1 (2.44%) | |
| 25–34 | 3 (3.45%) | 0 (0.00%) | 2 (8.00%) | 1 (2.44%) | |
| 35–44 | 4 (4.60%) | 2 (9.52%) | 0 (0.00%) | 2 (4.88%) | |
| 45–54 | 10 (11.5%) | 2 (9.52%) | 4 (16.0%) | 4 (9.76%) | |
| 55–64 | 60 (69.0%) | 16 (76.2%) | 14 (56.0%) | 30 (73.2%) | |
| ≥65 | 6 (6.90%) | 0 (0.00%) | 3 (12.0%) | 3 (7.32%) | |
| What is your gender? (n = 87) | 0.521 | ||||
| Female | 75 (86.2%) | 17 (81.0%) | 21 (84.0%) | 37 (90.2%) | |
| Male | 12 (13.8%) | 4 (19.0%) | 4 (16.0%) | 4 (9.76% Correct?) | |
| What is your marital status? (n = 87) | 0.864 | ||||
| Single | 13 (14.9%) | 2 (9.52%) | 4 (16.0%) | 7 (17.1%) | |
| Married | 39 (44.8%) | 10 (47.6%) | 13 (52.0%) | 16 (39.0%) | |
| Divorced | 28 (32.2%) | 7 (33.3%) | 7 (28.0%) | 14 (34.1%) | |
| Widower | 4 (4.60%) | 2 (9.52%) | 0 (0.00%) | 2 (4.88%) | |
| No answer | 3 (3.45%) | 0 (0.00%) | 1 (4.00%) | 2 (4.88%) | |
| How many children do you have? (n = 87) | 0.955 | ||||
| 0 | 15 (17.2%) | 4 (19.0%) | 5 (20.0%) | 6 (14.6%) | |
| 1–2 | 54 (62.1%) | 14 (66.7%) | 14 (56.0%) | 26 (63.4%) | |
| 3–4 | 17 (19.5%) | 3 (14.3%) | 6 (24.0%) | 8 (19.5%) | |
| ≥5 | 1 (1.15%) | 0 (0.00%) | 0 (0.00%) | 1 (2.44%) | |
| In what sort of area do you live? (n = 87) | 0.263 | ||||
| City | 83 (95.4%) | 19 (90.5%) | 25 (100%) | 39 (95.1%) | |
| Suburb or periphery | 4 (4.60%) | 2 (9.52%) | 0 (0.00%) | 2 (4.88%) | |
| Language used to take the questionnaire (n = 87) | <0.001 | ||||
| Arabic | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | |
| English | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | |
| French | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | |
| Hebrew | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | |
| Russian | 0 (0.00%) | 0 (0.00%) | 0.00(0%) | 0 (0.00%) | |
| Spanish | 87 (100%) | 21 (100%) | 25 (100%) | 41 (100%) | |
| Variable | Intention to Use Telemedicine in the Future | ||||
|---|---|---|---|---|---|
| Overall (n = 114) | Intent (n = 28) | Undecided (n = 47) | No Intent (n = 39) | p-Value | |
| What is your age? (n = 114) | <0.001 | ||||
| 18–24 | 39 (34.2%) | 5 (17.9%) | 19 (40.4%) | 15 (38.5%) | |
| 25–34 | 28 (24.6%) | 6 (21.4%) | 9 (19.1%) | 13 (33.3%) | |
| 35–44 | 17 (14.9%) | 10 (35.7%) | 5 (10.6%) | 2 (5.13%) | |
| 45–54 | 14 (12.3%) | 3 (10.7%) | 7 (14.9%) | 4 (10.3%) | |
| 55–64 | 12 (10.5%) | 3 (10.7%) | 4 (8.51%) | 5 (12.8%) | |
| ≥65 | 4 (3.51%) | 1 (3.57%) | 3 (6.38%) | 0 (0.00%) | |
| What is your gender? (n = 114) | 0.301 | ||||
| Female | 42 (36.8%) | 13 (46.4%) | 18 (38.3%) | 11 (28.2%) | |
| Male | 72 (63.2%) | 15 (53.6%) | 29 (61.7%) | 28 (71.8%) | |
| What is your marital status? (n = 114) | 0.055 | ||||
| Single | 50 (43.9%) | 7 (25.0%) | 22 (46.8%) | 21 (53.8%) | |
| Married | 58 (50.9%) | 21 (75.0%) | 21 (44.7%) | 16 (41.0%) | |
| Divorced | 1 (0.88%) | 0 (0.00%) | 1 (2.13%) | 0 (0.00%) | |
| Widower | 5 (4.39%) | 0 (0.00%) | 3 (6.38%) | 2 (5.13%) | |
| No answer | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | |
| How many children do you have? (n = 114) | 0.750 | ||||
| 0 | 72 (63.2%) | 15 (53.6%) | 30 (63.8%) | 27 (69.2%) | |
| 1–2 | 38 (33.3%) | 12 (42.9%) | 15 (31.9%) | 11 (28.2%) | |
| 3–4 | 4 (3.51%) | 1 (3.57%) | 2 (4.26%) | 1 (2.56%) | |
| ≥5 | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | |
| In what sort of area do you live? (n = 114) | 0.305 | ||||
| City | 68 (59.6%) | 16 (57.1%) | 25 (53.2%) | 27 (69.2%) | |
| Suburb or periphery | 46 (40.4%) | 12 (42.9%) | 22 (46.8%) | 12 (30.8%) | |
| Language used to take the questionnaire (n = 114) | 0.367 | ||||
| Arabic | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | |
| English | 67 (58.8%) | 17 (60.7%) | 27 (57.4%) | 23 (59.0%) | |
| French | 40 (35.1%) | 9 (32.1%) | 18 (38.3%) | 13 (33.3%) | |
| Hebrew | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | |
| Russian | 5 (4.39%) | 0 (0.00%) | 2 (4.26%) | 3 (7.69%) | |
| Spanish | 2 (1.75%) | 2 (7.14%) | 0 (0.00%) | 0 (0.00%) | |
| Variable | Intention to Use Telemedicine in the Future | ||||
|---|---|---|---|---|---|
| Overall (n = 272) | Intent (n = 139) | Undecided (n = 79) | No Intent (n = 54) | p-Value | |
| Do you use the following online services? Banking services, Food purchases, Clothing purchases, Electrical product purchases, Hotel reservations, Vacation arrangements (planning, purchases), Health consulting, Government services (n = 272) | 0.225 | ||||
| No | 5 (1.84%) | 1 (0.72%) | 2 (2.53%) | 2 (3.70%) | |
| Yes | 267 (98.2%) | 138 (99.3%) | 77 (97.5%) | 52 (96.3%) | |
| Do you use social media (reading, posting) for information and/or advice (not necessarily concerning a medical problem)? (n = 272) | <0.0001 | ||||
| Absolutely not | 11 (4.04%) | 7 (5.04%) | 1 (1.27%) | 3 (5.56%) | |
| A bit | 50 (18.4%) | 19 (13.7%) | 17 (21.5%) | 14 (25.9%) | |
| Moderately | 103 (37.9%) | 48 (34.5%) | 36 (45.6%) | 19 (35.2%) | |
| A lot | 76 (27.9%) | 44 (31.7%) | 18 (22.8%) | 14 (25.9%) | |
| Always | 32 (11.8%) | 21 (15.1%) | 7 (8.86%) | 4 (7.41%) | |
| Do you use online medical services? (n = 272) | <0.0001 | ||||
| No, not interested in using them | 16 (5.88%) | 2 (1.44%) | 4 (5.06%) | 10 (18.5%) | |
| No, but willing to experiment | 41 (15.1%) | 9 (6.47%) | 13 (16.5%) | 19 (35.2%) | |
| Yes, I used them for the first time during the COVID-19 pandemic. | 87 (32.0%) | 45 (32.4%) | 30 (38.0%) | 12 (22.2%) | |
| Yes, I used them before the COVID-19 pandemic. | 128 (47.1%) | 83 (59.7%) | 32 (40.5%) | 13 (24.1%) | |
| Before seeing a doctor, do you use social media to find answers to your question? (n = 272) | <0.0001 | ||||
| Absolutely not | 65 (23.9%) | 33 (23.7%) | 20 (25.3%) | 12 (22.2%) | |
| A bit | 110 (40.4%) | 54 (38.8%) | 29 (36.7%) | 27 (50.0%) | |
| Moderately | 58 (21.3%) | 30 (21.6%) | 20 (25.3%) | 8 (14.8%) | |
| A lot | 24 (8.82%) | 15 (10.8%) | 6 (7.59%) | 3 (5.56%) | |
| Always | 15 (5.51%) | 7 (5.04%) | 4 (5.06%) | 4 (7.41%) | |
| Has your knowledge of using other online services helped you use online medical services? (n = 272) | <0.0001 | ||||
| I have not tried online services. | 28 (10.3%) | 6 (4.32%) | 13 (24.1%) | 9 (11.4%) | |
| Absolutely not | 14 (5.15%) | 4 (2.88%) | 7 (13.0%) | 3 (3.80%) | |
| A bit | 57 (21.0%) | 22 (15.8%) | 10 (18.5%) | 25 (31.6%) | |
| Moderately | 69 (25.4%) | 39 (28.1%) | 14 (25.9%) | 16 (20.3%) | |
| A lot | 80 (29.4%) | 52 (37.4%) | 6 (11.1%) | 22 (27.8%) | |
| Absolutely | 24 (8.82%) | 16 (11.5%) | 4 (7.41%) | 4 (5.06%) | |
| Variable | Intention to Use Telemedicine in the Future | ||||
|---|---|---|---|---|---|
| Overall (n = 87) | Intent (n = 219) | Undecided (n = 259) | No Intent (n = 41) | p-Value | |
| Do you use the following online services? Banking services, Food purchases, Clothing purchases, Electrical product purchases, Hotel reservations, Vacation arrangements (planning, purchases), Health consulting, Government services (n = 87) | 1.000 | ||||
| No | 2 (2.30%) | 0 (0.00%) | 1 (4.00%) | 1 (2.44%) | |
| Yes | 85 (97.7%) | 21 (100%) | 24 (96.0%) | 40 (97.6%) | |
| Do you use social media (reading, posting) for information and/or advice (not necessarily concerning a medical problem)? (n = 87) | 0.770 | ||||
| Absolutely not | 4 (4.60%) | 0 (0.00%) | 1 (4.00%) | 3 (7.32%) | |
| A bit | 19 (21.8%) | 3 (14.3%) | 6 (24.0%) | 10 (24.4%) | |
| Moderately | 38 (43.7%) | 10 (47.6%) | 11 (44.0%) | 17 (41.5%) | |
| A lot | 18 (20.7%) | 7 (33.3%) | 5 (20.0%) | 6 (14.6%) | |
| Always | 8 (9.20%) | 1 (4.76%) | 2 (8.00%) | 5 (12.2%) | |
| Do you use online medical services? (n = 87) | 0.004 | ||||
| No, not interested in using them | 11 (12.6%) | 0 (0.00%) | 0 (0.00%) | 11 (26.8%) | |
| No, but willing to experiment | 13 (14.9%) | 3 (14.3%) | 4 (16.0%) | 6 (14.6%) | |
| Yes, I used them for the first time during the COVID-19 pandemic. | 42 (48.3%) | 9 (42.9%) | 14 (56.0%) | 19 (46.3%) | |
| Yes, I used them before the COVID-19 pandemic. | 21 (24.1%) | 9 (42.9%) | 7 (28.0%) | 5 (12.2%) | |
| Before seeing a doctor, do you use social media to find answers to your question? (n = 87) | 0.446 | ||||
| Absolutely not | 32 (36.8%) | 8 (38.1%) | 6 (24.0%) | 18 (43.9%) | |
| A bit | 24 (27.6%) | 4 (19.0%) | 9 (36.0%) | 11 (26.8%) | |
| Moderately | 19 (21.8%) | 5 (23.8%) | 7 (28.0%) | 7 (17.1%) | |
| A lot | 9 (10.3%) | 2 (9.52%) | 2 (8.00%) | 5 (12.2%) | |
| Always | 3 (3.45%) | 2 (9.52%) | 1 (4.00%) | 0 (0.00%) | |
| Has your knowledge of using other online services helped you use online medical services? (n = 87) | 0.249 | ||||
| I have not tried online services. | 9 (10.3%) | 0 (0.00%) | 7 (17.1%) | 2 (8.00%) | |
| Absolutely not | 14 (16.1%) | 1 (4.76%) | 9 (22.0%) | 4 (16.0%) | |
| A bit | 17 (19.5%) | 4 (19.0%) | 8 (19.5%) | 5 (20.0%) | |
| Moderately | 28 (32.2%) | 9 (42.9%) | 11 (26.8%) | 8 (32.0%) | |
| A lot | 18 (20.7%) | 7 (33.3%) | 6 (14.6%) | 5 (20.0%) | |
| Absolutely | 1 (1.15%) | 0 (0.00%) | 0 (0.00%) | 1 (4.00%) | |
| Variable | Intention to Use Telemedicine in the Future | ||||
|---|---|---|---|---|---|
| Overall (n = 114) | Intent (n = 28) | Undecided (n = 47) | No Intent (n = 39) | p-Value | |
| Do you use the following online services? Banking services, Food purchases, Clothing purchases, Electrical product purchases, Hotel reservations, Vacation arrangements (planning, purchases), Health consulting, Government services (n = 114) | <0.0001 | ||||
| No | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | 0 (0.00%) | |
| Yes | 114 (100%) | 28 (100%) | 47 (100%) | 39 (100%) | |
| Do you use social media (reading, posting) for information and/or advice (not necessarily concerning a medical problem)? (n = 114) | <0.0001 | ||||
| Absolutely not | 18 (15.8%) | 2 (7.14%) | 5 (10.6%) | 11 (28.2%) | |
| A bit | 20 (17.5%) | 3 (10.7%) | 11 (23.4%) | 6 (15.4%) | |
| Moderately | 42 (36.8%) | 9 (32.1%) | 20 (42.6%) | 13 (33.3%) | |
| A lot | 24 (21.1%) | 10 (35.7%) | 8 (17.0%) | 6 (15.4%) | |
| Always | 10 (8.77%) | 4 (14.3%) | 3 (6.38%) | 3 (7.69%) | |
| Do you use online medical services? (n = 114) | 0.003 | ||||
| No, not interested in using them | 29 (25.4%) | 2 (7.14%) | 13 (27.7%) | 14 (35.9%) | |
| No, but willing to experiment | 30 (26.3%) | 4 (14.3%) | 17 (36.2%) | 9 (23.1%) | |
| Yes, I used them for the first time during the COVID-19 pandemic. | 27 (23.7%) | 9 (32.1%) | 7 (14.9%) | 11 (28.2%) | |
| Yes, I used them before the COVID-19 pandemic. | 28 (24.6%) | 13 (46.4%) | 10 (21.3%) | 5 (12.8%) | |
| Before seeing a doctor, do you use social media to find answers to your question? (n = 114) | 0.252 | ||||
| Absolutely not | 33 (28.9%) | 6 (21.4%) | 14 (29.8%) | 13 (33.3%) | |
| A bit | 23 (20.2%) | 4 (14.3%) | 7 (14.9%) | 12 (30.8%) | |
| Moderately | 32 (28.1%) | 11 (39.3%) | 16 (34.0%) | 5 (12.8%) | |
| A lot | 12 (10.5%) | 3 (10.7%) | 4 (8.51%) | 5 (12.8%) | |
| Always | 14 (12.3%) | 4 (14.3%) | 6 (12.8%) | 4 (10.3%) | |
| Has your knowledge of using other online services helped you use online medical services? (n = 114) | <0.0001 | ||||
| I have not tried online services. | 28 (24.6%) | 2 (7.14%) | 11 (28.2%) | 15 (31.9%) | |
| Absolutely not | 8 (7.02%) | 1 (3.57%) | 5 (12.8%) | 2 (4.26%) | |
| A bit | 32 (28.1%) | 9 (32.1%) | 9 (23.1%) | 14 (29.8%) | |
| Moderately | 23 (20.2%) | 6 (21.4%) | 7 (17.9%) | 10 (21.3%) | |
| A lot | 12 (10.5%) | 6 (21.4%) | 4 (10.3%) | 2 (4.26%) | |
| Absolutely | 11 (9.65%) | 4 (14.3%) | 3 (7.69%) | 4 (8.51%) | |
References
- Eysenbach, G. What is e-health? J. Med. Internet Res. 2001, 3, e20. [Google Scholar] [CrossRef]
- Boogerd, E.A.; Arts, T.; Engelen, L.J.; Van De Belt, T.H. “What is eHealth”: Time for An Update? JMIR Res. Protoc. 2015, 4, e29. [Google Scholar] [CrossRef]
- Romanick-Schmiedl, S.; Raghu, G. Telemedicine—Maintaining quality during times of transition. Nat. Rev. Dis. Prim. 2020, 6, 45. [Google Scholar] [CrossRef]
- Monaghesh, E.; Hajizadeh, A. The role of telehealth during COVID-19 outbreak: A systematic review based on current evidence. BMC Public Health 2020, 20, 1193. [Google Scholar] [CrossRef]
- Kichloo, A.; Albosta, M.; Dettloff, K.; Wani, F.; El-Amir, Z.; Singh, J.; Aljadah, M.; Chakinala, R.C.; Kanugula, A.K.; Solanki, S.; et al. Telemedicine, the current COVID-19 pandemic and the future: A narrative review and perspectives moving forward in the USA. Fam. Med. Community Health 2020, 8, e000530. [Google Scholar] [CrossRef] [PubMed]
- Stowe, S.; Harding, S. Telecare, telehealth and telemedicine. Eur. Geriatr. Med. 2010, 1, 193–197. [Google Scholar] [CrossRef]
- Nittari, G.; Khuman, R.; Baldoni, S.; Pallotta, G.; Battineni, G.; Sirignano, A.; Amenta, F.; Ricci, G. Telemedicine Practice: Review of the Current Ethical and Legal Challenges. Telemed. e-Health 2020, 26, 1427–1437. [Google Scholar] [CrossRef] [PubMed]
- Bhaskar, S.; Bradley, S.; Chattu, V.K.; Adisesh, A.; Nurtazina, A.; Kyrykbayeva, S.; Sakhamuri, S.; Yaya, S.; Sunil, T.; Thomas, P.; et al. Telemedicine Across the Globe-Position Paper From the COVID-19 Pandemic Health System Resilience PROGRAM (REPROGRAM) International Consortium (Part 1). Front. Public Health 2020, 8, 556720. [Google Scholar] [CrossRef]
- Napier, A.D.; Ancarno, C.; Butler, B.; Calabrese, J.; Chater, A.; Chatterjee, H.; Guesnet, F.; Horne, R.; Jacyna, S.; Jadhav, S.; et al. Culture and health. Lancet 2014, 384, 1607–1639. [Google Scholar] [CrossRef]
- Plough, A.L. Building a culture of health: A critical role for public health services and systems research. Am. J. Public Health 2015, 105 (Suppl. S2), S150–S152. [Google Scholar] [CrossRef]
- Chandra, A.; Acosta, J.; Carman, K.G.; Dubowitz, T.; Leviton, L.; Martin, L.T.; Miller, C.; Nelson, C.; Orleans, T.; Tait, M.; et al. Building a National Culture of Health: Background, Action Framework, Measures, and Next Steps. Rand Health Q 2017, 6, 3. [Google Scholar]
- Thomas, S.B.; Fine, M.J.; Ibrahim, S.A. Health Disparities: The Importance of Culture and Health Communication. Am. J. Public Health 2004, 94, 2050. [Google Scholar] [CrossRef]
- Innovative Telemedicine Approaches in Different Countries: Opportunity for Adoption, Leveraging, and Scaling-Up. Available online: https://telehealthandmedicinetoday.com/index.php/journal/article/download/160/203?inline=1 (accessed on 20 September 2021).
- Sollazzo, A.; Berterretche, R. The Integrated National Healthcare System in Uruguay and the Challenges for Primary Healthcare. Cien. Saude Colet. 2011, 16, 2829–2840. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rosen, B.; Waitzberg, R.; Merkur, S. Israel: Health System Review. Health Syst. Transit. 2015, 17, 1–212. [Google Scholar]
- Population of Israel on the Eve of 2021. Available online: https://www.cbs.gov.il/en/mediarelease/Pages/2020/Population-of-Israel-on-the-Eve-of-2021.aspx (accessed on 22 September 2021).
- Population, Total—Uruguay. Available online: https://data.worldbank.org/indicator/SP.POP.TOTL?locations=UY (accessed on 22 September 2021).
- Benis, A.; Barkan, R.B.; Sela, T.; Harel, N. Communication Behavior Changes Between Patients with Diabetes and Healthcare Providers Over 9 Years: Retrospective Cohort Study. J. Med. Internet Res. 2020, 22, e17186. [Google Scholar] [CrossRef] [PubMed]
- Beyar, R.; Zeevi, B.; Rechavi, G. Israel: A start-up life science nation. Lancet 2017, 389, 2563–2569. [Google Scholar] [CrossRef]
- Nash, D.B. The Healthcare Start-Up Nation. Am. Health Drug Benefits 2019, 12, 221–222. [Google Scholar]
- Clarfield, A.M.; Manor, O.; Bin Nun, G.; Shvarts, S.; Azzam, Z.S.; Afek, A.; Basis, F.; Israeli, A. Health and health care in Israel: An introduction. Lancet 2017, 389, 2503–2513. [Google Scholar] [CrossRef]
- Behar, J.A.; Liu, C.; Kotzen, K.; Tsutsui, K.; Corino, V.D.A.; Singh, J.; Pimentel, M.A.F.; Warrick, P.; Zaunseder, S.; Andreotti, F.; et al. Remote health diagnosis and monitoring in the time of COVID-19. Physiol. Meas. 2020, 41, 10TR01. [Google Scholar] [CrossRef]
- Liu, N.; Huang, R.; Baldacchino, T.; Sud, A.; Sud, K.; Khadra, M.; Kim, J. Telehealth for Noncritical Patients with Chronic Diseases during the COVID-19 Pandemic. J. Med. Internet Res. 2020, 22, e19493. [Google Scholar] [CrossRef] [PubMed]
- Galiero, R.; Pafundi, P.C.; Nevola, R.; Rinaldi, L.; Acierno, C.; Caturano, A.; Salvatore, T.; Adinolfi, L.E.; Costagliola, C.; Sasso, F.C. The Importance of Telemedicine during COVID-19 Pandemic: A Focus on Diabetic Retinopathy. J. Diabetes Res. 2020, 2020, 9036847. [Google Scholar] [CrossRef]
- Curigliano, G.; Cardoso, M.J.; Poortmans, P.; Gentilini, O.; Pravettoni, G.; Mazzocco, K.; Houssami, N.; Pagani, O.; Senkus, E.; Cardoso, F. Recommendations for triage, prioritization and treatment of breast cancer patients during the COVID-19 pandemic. Breast 2020, 52, 8–16. [Google Scholar] [CrossRef]
- Grossman, Z.; Chodick, G.; Reingold, S.M.; Chapnick, G.; Ashkenazi, S. The future of telemedicine visits after COVID-19: Perceptions of primary care pediatricians. Isr. J. Health Policy Res. 2020, 9, 53. [Google Scholar] [CrossRef] [PubMed]
- Pappot, N.; Taarnhøj, G.A.; Pappot, H. Telemedicine and e-Health Solutions for COVID-19: Patients’ Perspective. Telemed. e-Health 2020, 26, 847–849. [Google Scholar] [CrossRef]
- Philipp, J. Healthcare in Uruguay: Paving the Way in South America. Available online: https://borgenproject.org/healthcare-in-uruguay (accessed on 22 September 2021).
- Ley 19.869. Available online: https://perma.cc/XL9J-CJE8 (accessed on 22 September 2021).
- Telemedicine: Good Practices from Latin America. Available online: https://ww1.issa.int/analysis/telemedicina-buenas-practicas-en-america-latina (accessed on 22 September 2021).
- Kaplan, B. Revisiting health information technology ethical, legial, ans social issues and evaluation: Telehealth/Telemedicine and COVID-19. Int. J. Med. Inform. 2020, 143, 104239. [Google Scholar] [CrossRef]
- Richard, M.-O.; Toffoli, R. Language influence in responses to questionnaires by bilingual respondents: A test of the Whorfian hypothesis. J. Bus. Res. 2009, 62, 987–994. [Google Scholar] [CrossRef]
- Zavala-Rojas, D.; Saris, W.E. Measurement Invariance in Multilingual Survey Research: The Role of the Language of the Questionnaire. Soc. Indic. Res. 2017, 140, 485–510. [Google Scholar] [CrossRef]
- Young, A.; Espinoza, F.; Dodds, C.; Rogers, K.; Giacoppo, R. Adapting an Online Survey Platform to Permit Translanguaging. Field Methods 2021, 33, 388–404. [Google Scholar] [CrossRef]
- Benis, A.; Seidmann, A.; Ashkenazi, S. Reasons for Taking the COVID-19 Vaccine by US Social Media Users. Vaccines 2021, 9, 315. [Google Scholar] [CrossRef] [PubMed]
- Eysenbach, G. Improving the quality of Web surveys: The Checklist for reporting results of internet E-Surveys (CHERRIES). J. Med. Internet Res. 2004, 6, e34. [Google Scholar] [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. J. Clin. Epidemiol. 2008, 61, 344–349. [Google Scholar] [CrossRef]
- Collins, G.S.; Reitsma, J.B.; Altman, D.G.; Moons, K. Transparent Reporting of a Multivariable Prediction Model for Individu-al Prognosis or Diagnosis (TRIPOD): The TRIPOD Statement. BMC Med. 2015, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Matschinske, J.; Alcaraz, N.; Benis, A.; Golebiewski, M.; Grimm, D.G.; Heumos, L.; Kacprowski, T.; Lazareva, O.; List, M.; Louadi, Z.; et al. The AIMe registry for artificial intelligence in biomedical research. Nat. Methods 2021, 18, 1128–1131. [Google Scholar] [CrossRef] [PubMed]
- Maimon, O.Z.; Rokach, L. Data Mining with Decision Trees: Theory and Applications, 2nd ed.; World Scientific: Singapore, 2014; ISBN 9789814590099. [Google Scholar]
- Shmueli, G. Research Dilemmas with Behavioral Big Data. Big Data 2017, 5, 98–119. [Google Scholar] [CrossRef]
- Gmunder, K.N.; Ruiz, J.W.; Franceschi, D.; Suarez, M.M. Demographics associated with US healthcare disparities are exacerbated by the telemedicine surge during the COVID-19 pandemic. J. Telemed. Telecare 2021. [Google Scholar] [CrossRef] [PubMed]
- Personality Project. Available online: http://personality-project.org/r/psych (accessed on 1 July 2021).
- Isaac Subirana, J.V.; Sanz, H. compareGroups 4.0: Descriptives by Groups. Available online: https://cran.r-project.org/web/packages/compareGroups/vignettes/compareGroups_vignette.html (accessed on 1 July 2021).
- Rpart Package—Rdocumentation. Available online: https://www.rdocumentation.org/packages/rpart/versions/4.1-15 (accessed on 1 May 2021).
- Benis, A.; Khodos, A.; Ran, S.; Levner, E.; Ashkenazi, S. Social Media Engagement and Influenza Vaccination During the COVID-19 Pandemic: Cross-sectional Survey Study. J. Med. Internet Res. 2021, 23, e25977. [Google Scholar] [CrossRef]
- Benis, A.; Harel, N.; Barkan, R.B.; Srulovici, E.; Key, C. Patterns of Patients’ Interactions with a Health Care Organization and Their Impacts on Health Quality Measurements: Protocol for a Retrospective Cohort Study. JMIR Res. Protoc. 2018, 7, e10734. [Google Scholar] [CrossRef]
- Krupinski, E.A. History of Telemedicine: Evolution, Context, and Transformation. Telemed. e-Health 2009, 15, 804–805. [Google Scholar] [CrossRef]
- Bashshur, R.; Doarn, C.R.; Frenk, J.M.; Kvedar, J.C.; Woolliscroft, J.O. Telemedicine and the COVID-19 Pandemic, Lessons for the Future. Telemed. e-Health 2020, 26, 571–573. [Google Scholar] [CrossRef]
- Gogia, S. Rationale, history, and basics of telehealth. In Fundamentals of Telemedicine and Telehealth; Elsevier: Amsterdam, The Netherlands, 2020; pp. 11–34. ISBN 9780128143094. [Google Scholar]
- Weiner, J.P. Doctor-patient communication in the e-health era. Isr. J. Health Policy Res. 2012, 1, 33. [Google Scholar] [CrossRef] [PubMed]
- Dreiher, D.; Blagorazumnaya, O.; Balicer, R.; Dreiher, J. National initiatives to promote quality of care and patient safety: Achievements to date and challenges ahead. Isr. J. Health Policy Res. 2020, 9, 62. [Google Scholar] [CrossRef]
- Keshet, Y.; Popper-Giveon, A. Language practice and policy in Israeli hospitals: The case of the Hebrew and Arabic languages. Isr. J. Health Policy Res. 2019, 8, 58. [Google Scholar] [CrossRef] [PubMed]
- Westreich, D.; Lessler, J.; Funk, M.J. Propensity score estimation: Neural networks, support vector machines, decision trees (CART), and meta-classifiers as alternatives to logistic regression. J. Clin. Epidemiol. 2010, 63, 826–833. [Google Scholar] [CrossRef] [PubMed]
- Venkatasubramaniam, A.; Wolfson, J.; Mitchell, N.; Barnes, T.; Jaka, M.; French, S. Decision trees in epidemiological research. Emerg. Themes Epidemiol. 2017, 14, 11. [Google Scholar] [CrossRef]
- Wolfson, J.; Venkatasubramaniam, A. Branching Out: Use of Decision Trees in Epidemiology. Curr. Epidemiol. Rep. 2018, 5, 221–229. [Google Scholar] [CrossRef]
- Irony, A.; Avi, P.; Segal, A.; Iris, M.; Nachman, A. Managing Chronic Care & Tele-Monitoring Model for enhancing integrated care—The MOMA Suggestion. Int. J. Integr. Care 2017, 17, 19. [Google Scholar] [CrossRef][Green Version]
- Hennig, S. The Digital Patient. Available online: https://blog.der-digitale-patient.de/en/telemedicine-israel/ (accessed on 21 August 2021).
- Itzhak, B.; Weinberger, T.; Berkovitch, E.; Reis, S. Telemedicine in Primary Care in Israel. J. Telemed. Telecare 1998, 4, 11–14. [Google Scholar] [CrossRef]
- Jamshed, N.; Ozair, F.F.; Sharma, A.; Aggarwal, P. Ethical issues in electronic health records: A general overview. Perspect. Clin. Res. 2015, 6, 73–76. [Google Scholar] [CrossRef]
- Stoeger, K.; Schmidhuber, M. The use of data from electronic health records in times of a pandemic—A legal and ethical assessment. J. Law Biosci. 2020, 7, lsaa041. [Google Scholar] [CrossRef] [PubMed]
- Roth, A.; Korb, H.; Gadot, R.; Kalter, E. Telecardiology for patients with acute or chronic cardiac complaints: The ‘SHL’ experience in Israel and Germany. Int. J. Med. Inform. 2006, 75, 643–645. [Google Scholar] [CrossRef]
- Hadar, E.; Wolff, L.; Tenenbaum-Gavish, K.; Eisner, M.; Shmueli, A.; Barbash-Hazan, S.; Bergel, R.; Shmuel, E.; Houri, O.; Dollinger, S.; et al. Mobile Self-Operated Home Ultrasound System for Remote Fetal Assessment During Pregnancy. Telemed. e-Health 2021. [Google Scholar] [CrossRef]
- Kemp, S. Digital in Israel: All the Statistics You Need in 2021—DataReportal—Global Digital Insights. Available online: https://datareportal.com/reports/digital-2021-israel (accessed on 29 August 2021).
- Kemp, S. Digital 2021: Global Overview Report. Available online: https://datareportal.com/reports/digital-2021-global-overview-report (accessed on 29 August 2021).
- Punia, V.; Nasr, G.; Zagorski, V.; Lawrence, G.; Fesler, J.; Nair, D.; Najm, I. Evidence of a Rapid Shift in Outpatient Practice During the COVID-19 Pandemic Using Telemedicine. Telemed. e-Health 2020, 26, 1301–1303. [Google Scholar] [CrossRef]
- Ritchie, H.; Roser, M. Age Structure. Our World in Data. Available online: https://ourworldindata.org/age-structure (accessed on 1 July 2021).
- Uruguay—Average Age of the Population 1950–2050. Available online: https://www.statista.com/statistics/439853/average-age-of-the-population-in-uruguay (accessed on 22 September 2021).
- Taboada-Vázquez, A.; Gonzalez-Rodriguez, R.; Gandoy-Crego, M.; Clemente, M. Personality Variables as Predictors of Health Services Consumption. Int. J. Environ. Res. Public Health 2021, 18, 5161. [Google Scholar] [CrossRef]
- Stankova, M.; Mihova, P. Attitudes to telemedicine, and willingness to use in young people. In Intelligent Decision Technologies 2019; Smart Innovation, Systems and Technologies; Springer: Singapore, 2019; pp. 329–336. ISBN 9789811383021. [Google Scholar]
- Rosen, B.; Waitzberg, R.; Israeli, A. Israel’s rapid rollout of vaccinations for COVID-19. Isr. J. Health Policy Res. 2021, 10, 6. [Google Scholar] [CrossRef] [PubMed]
- García-Montero, C.; Fraile-Martínez, O.; Bravo, C.; Torres-Carranza, D.; Sanchez-Trujillo, L.; Gómez-Lahoz, A.M.; Guijarro, L.G.; García-Honduvilla, N.; Asúnsolo, A.; Bujan, J.; et al. An Updated Review of SARS-CoV-2 Vaccines and the Importance of Effective Vaccination Programs in Pandemic Times. Vaccines 2021, 9, 433. [Google Scholar] [CrossRef]
- Gostin, L.O.; Cohen, I.G.; Shaw, J. Digital Health Passes in the Age of COVID-19: Are “Vaccine Passports” Lawful and Ethical? JAMA 2021, 325, 1933–1934. [Google Scholar] [CrossRef] [PubMed]
- Sotis, C.; Allena, M.; Reyes, R.; Romano, A. COVID-19 Vaccine Passport and International Traveling: The Combined Effect of Two Nudges on Americans’ Support for the Pass. Int. J. Environ. Res. Public Health 2021, 18, 8800. [Google Scholar] [CrossRef]
- Schulz, T.; Long, K.; Kanhutu, K.; Bayrak, I.; Johnson, D.; Fazio, T. Telehealth during the coronavirus disease 2019 pandemic: Rapid expansion of telehealth outpatient use during a pandemic is possible if the programme is previously established. J. Telemed. Telecare 2020. [Google Scholar] [CrossRef] [PubMed]
- González, L.; Pidre, S.; Ruggia, R.; Serra, F.; Mendoza, R.; Piñatares, M.; Granja, N. Data Quality Management in e-Health Integration Platforms: The Case of Uruguay. CLEI Electron. J. 2018, 21, 8. [Google Scholar] [CrossRef]
- Lerouge, C.M.; Gupta, M.; Corpart, G.; Arrieta, A. Health System Approaches Are Needed to Expand Telemedicine Use Across Nine Latin American Nations. Health Aff. 2019, 38, 212–221. [Google Scholar] [CrossRef]
- Hassan, A.; Mari, Z.; Gatto, E.M.; Cardozo, A.; Youn, J.; Okubadejo, N.; Bajwa, J.A.; Shalash, A.; Fujioka, S.; Aldaajani, Z.; et al. Global Survey on Telemedicine Utilization for Movement Disorders During the COVID-19 Pandemic. Mov. Disord. 2020, 35, 1701–1711. [Google Scholar] [CrossRef] [PubMed]
- Milano, G.; Vallespir, D.; Viola, A. A technological and innovative approach to COVID-19 in Uruguay. Commun. ACM 2020, 63, 53–55. [Google Scholar] [CrossRef]
- Catan, G.; Espanha, R.; Mendes, R.V.; Toren, O.; Chinitz, D. Health information technology implementation—Impacts and policy considerations: A comparison between Israel and Portugal. Isr. J. Health Policy Res. 2015, 4, 41. [Google Scholar] [CrossRef] [PubMed]
- Miyawaki, A.; Tabuchi, T.; Ong, M.K.; Tsugawa, Y. Age and Social Disparities in the Use of Telemedicine During the COVID-19 Pandemic in Japan: Cross-sectional Study. J. Med. Internet Res. 2021, 23, e27982. [Google Scholar] [CrossRef]
- Ben-Assa, E.; Shacham, Y.; Golovner, M.; Malov, N.; Leshem-Rubinow, E.; Zatelman, A.; Shamir, A.O.; Rogowski, O.; Roth, A. Is Telemedicine an Answer to Reducing 30-Day Readmission Rates Post–Acute Myocardial Infarction? Telemed. e-Health 2014, 20, 816–821. [Google Scholar] [CrossRef]
- mHealthIntelligence Anthem Sees Different Telehealth Adoption Rates Among Populations. Available online: https://mhealthintelligence.com/news/anthem-sees-different-telehealth-adoption-rates-among-populations (accessed on 2 September 2021).
- Almandoz, J.P.; Xie, L.; Schellinger, J.N.; Mathew, M.S.; Edwards, K.; Ofori, A.; Kukreja, S.; Schneider, B.; Messiah, S.E. Telehealth utilization among multi-ethnic patients with obesity during the COVID-19 pandemic. J. Telemed. Telecare 2021. [Google Scholar] [CrossRef]
- De Albornoz, S.C.; Sia, K.-L.; Harris, A. The effectiveness of teleconsultations in primary care: Systematic review. Fam. Pract. 2021, cmab077. [Google Scholar] [CrossRef]
- Reicher, S.; Sela, T.; Toren, O. Using Telemedicine During the COVID-19 Pandemic: Attitudes of Adult Health Care Consumers in Israel. Front. Public Health 2021, 9, 653553. [Google Scholar] [CrossRef]
- Comte, B.; Baumbach, J.; Benis, A.; Basílio, J.; Debeljak, N.; Flobak, Å.; Franken, C.; Harel, N.; He, F.; Kuiper, M.; et al. Network and Systems Medicine: Position Paper of the European Collaboration on Science and Technology Action on Open Multiscale Systems Medicine. Netw. Syst. Med. 2020, 3, 67–90. [Google Scholar] [CrossRef]
- Benis, A.; Tamburis, O.; Chronaki, C.; Moen, A. One Digital Health: A Unified Framework for Future Health Ecosystems. J. Med. Internet Res. 2021, 23, e22189. [Google Scholar] [CrossRef] [PubMed]
- Rajan, B.; Tezcan, T.; Seidmann, A. Service Systems with Heterogeneous Customers: Investigating the Effect of Telemedicine on Chronic Care. Manag. Sci. 2019, 65, 1236–1267. [Google Scholar] [CrossRef]
- Ventola, C.L. Social Media and Health Care Professionals: Benefits, Risks, and Best Practices. Pharm. Ther. 2014, 39, 491–520. [Google Scholar]
- Walsh, L.; Hyett, N.; Howley, J.; Juniper, N.; Li, C.; MacLeod-Smith, B.; Rodier, S.; Hill, S.J. The Risks and Benefits of Using Social Media to Engage Consumers in Service Design and Quality Improvement in Australian Public Hospitals: Findings from an Interview Study of Key Stakeholders. BMC Health Serv. Res. 2021, 21, 876. [Google Scholar] [CrossRef] [PubMed]
- Wannheden, C.; Stenfors, T.; Stenling, A.; Schwarz, U.V.T. Satisfied or Frustrated? A Qualitative Analysis of Need Satisfying and Need Frustrating Experiences of Engaging with Digital Health Technology in Chronic Care. Front. Public Health 2021, 8, 623773. [Google Scholar] [CrossRef]
- Benis, A.; Chatsubi, A.; Levner, E.; Ashkenazi, S. Change in Threads on Twitter Regarding Influenza, Vaccines, and Vaccination During the COVID-19 Pandemic: Artificial Intelligence–Based Infodemiology Study. JMIR Infodemiology 2021, 1, e31983. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benis, A.; Banker, M.; Pinkasovich, D.; Kirin, M.; Yoshai, B.-e.; Benchoam-Ravid, R.; Ashkenazi, S.; Seidmann, A. Reasons for Utilizing Telemedicine during and after the COVID-19 Pandemic: An Internet-Based International Study. J. Clin. Med. 2021, 10, 5519. https://doi.org/10.3390/jcm10235519
Benis A, Banker M, Pinkasovich D, Kirin M, Yoshai B-e, Benchoam-Ravid R, Ashkenazi S, Seidmann A. Reasons for Utilizing Telemedicine during and after the COVID-19 Pandemic: An Internet-Based International Study. Journal of Clinical Medicine. 2021; 10(23):5519. https://doi.org/10.3390/jcm10235519
Chicago/Turabian StyleBenis, Arriel, Maxim Banker, David Pinkasovich, Mark Kirin, Bat-el Yoshai, Raquel Benchoam-Ravid, Shai Ashkenazi, and Abraham Seidmann. 2021. "Reasons for Utilizing Telemedicine during and after the COVID-19 Pandemic: An Internet-Based International Study" Journal of Clinical Medicine 10, no. 23: 5519. https://doi.org/10.3390/jcm10235519
APA StyleBenis, A., Banker, M., Pinkasovich, D., Kirin, M., Yoshai, B.-e., Benchoam-Ravid, R., Ashkenazi, S., & Seidmann, A. (2021). Reasons for Utilizing Telemedicine during and after the COVID-19 Pandemic: An Internet-Based International Study. Journal of Clinical Medicine, 10(23), 5519. https://doi.org/10.3390/jcm10235519







