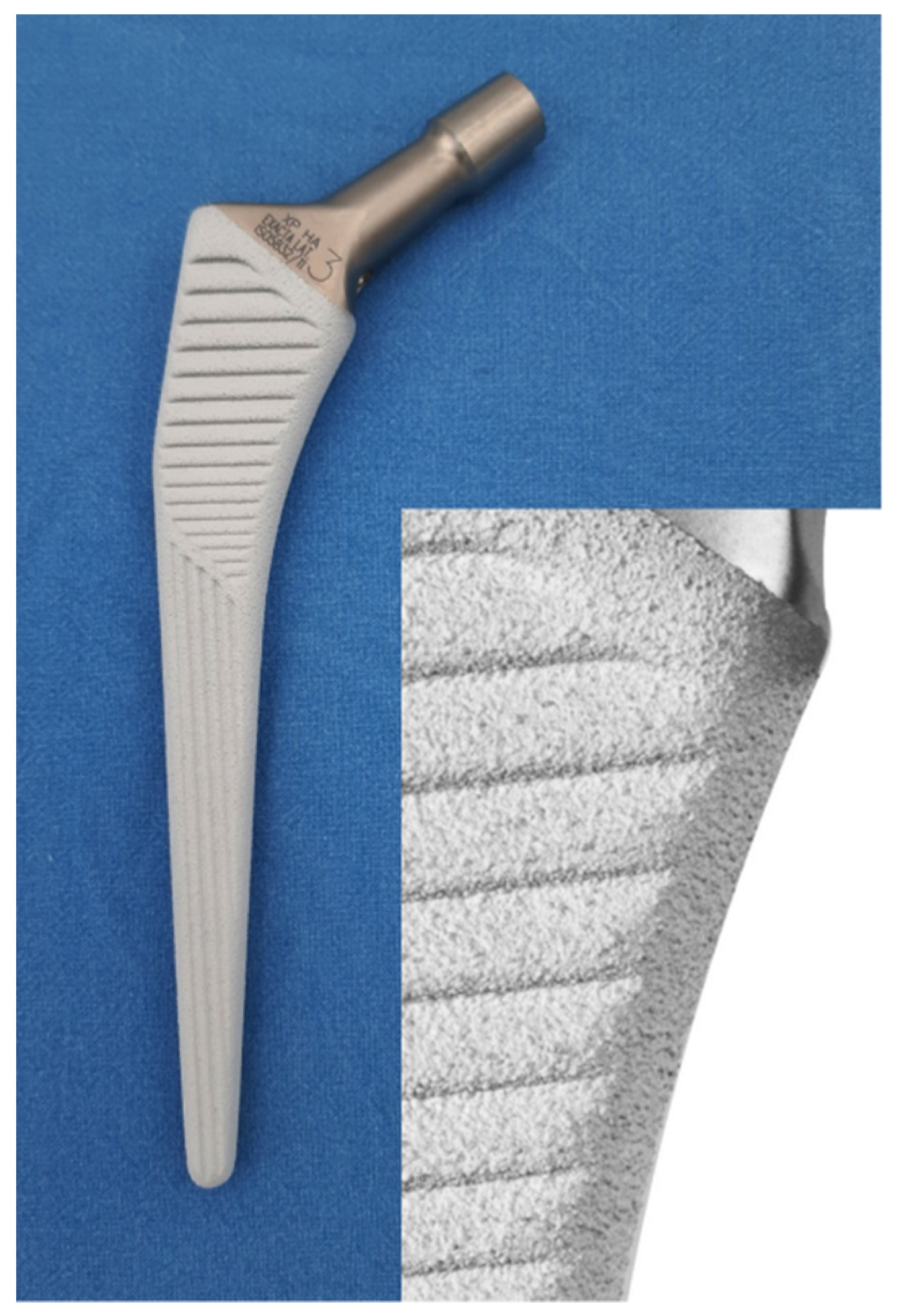
Use of a Plasma-Sprayed Titanium-Hydroxyapatite Femoral Stem in Hip Arthroplasty in Patients Older than 70 Years. Is Cementless Fixation a Reliable Option in the Elderly?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Clinical Evaluation
2.3. Radiographic Analysis
2.4. Statistical Analysis
3. Results
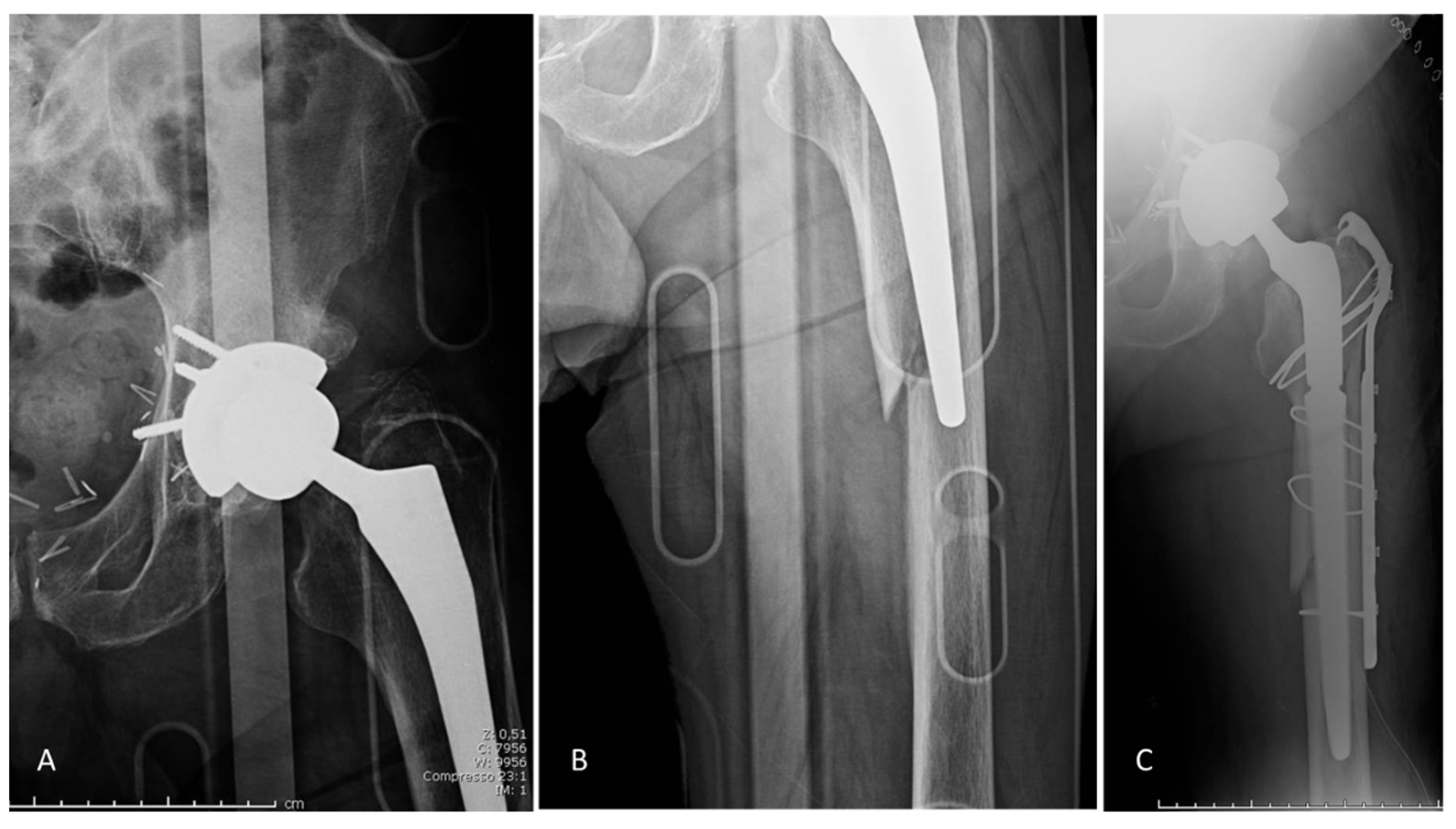
3.1. Complications
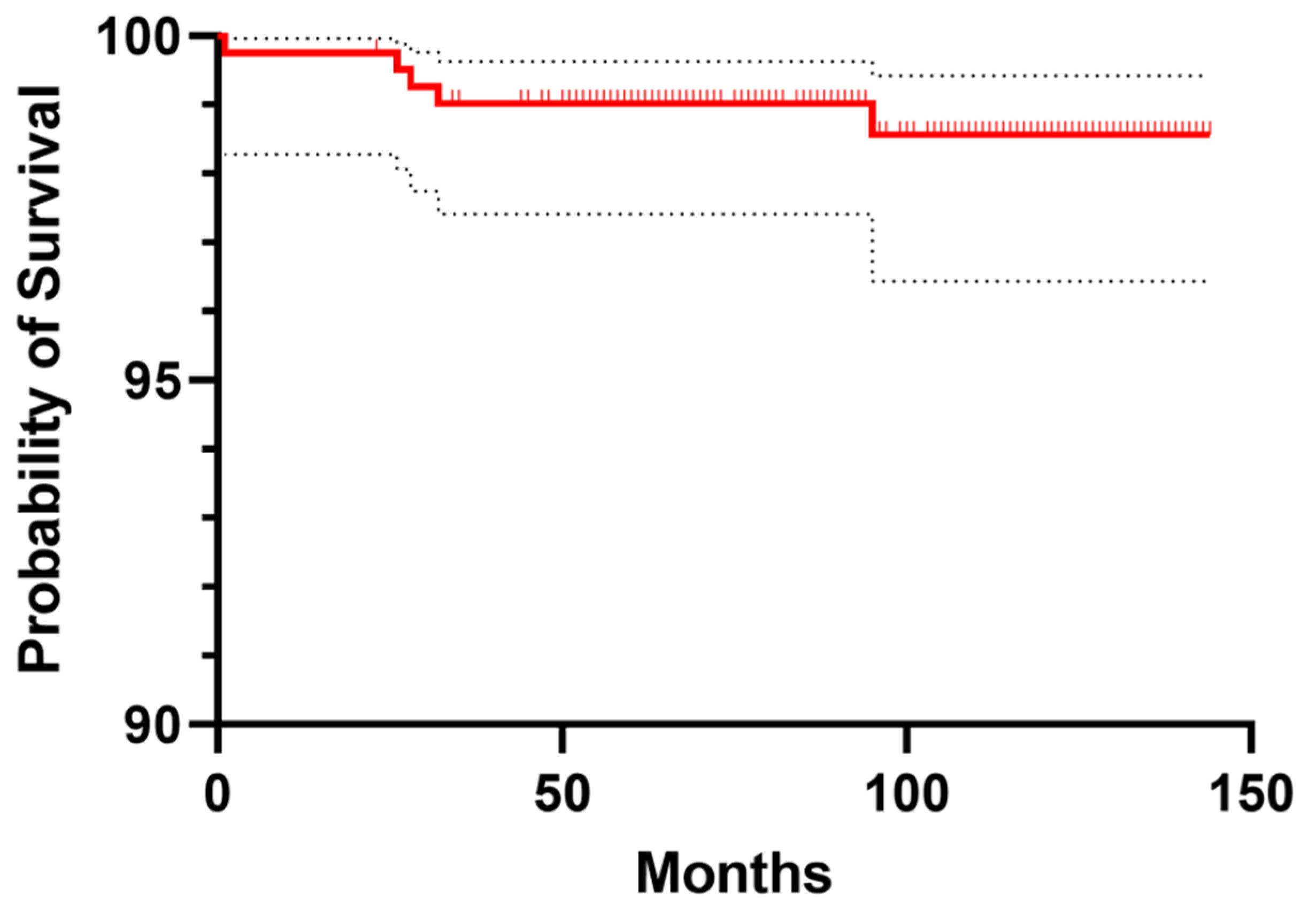
3.2. Implant Survival
3.3. Clinical Analysis
3.4. Radiological Analysis
4. Discussion
Strengths and Weaknesses
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Learmonth, I.D.; Young, C.; Rorabeck, C. The Operation of the Century: Total Hip Replacement. Lancet 2007, 370, 1508–1519. [Google Scholar] [CrossRef]
- Evans, J.T.; Evans, J.P.; Walker, R.W.; Blom, A.W.; Whitehouse, M.R.; Sayers, A. How Long Does a Hip Replacement Last? A Systematic Review and Meta-Analysis of Case Series and National Registry Reports with More than 15 Years of Follow-Up. Lancet 2019, 393, 647–654. [Google Scholar] [CrossRef] [Green Version]
- Emilia-Romagna Region Register of the Orthopaedic Prosthetic Implants. Annual Report 2020. Available online: Https://Ripo.Cineca.It/Authzssl/Pdf/Report_RIPO_2018_ENG.Pdf (accessed on 7 September 2021).
- Kheir, M.M.; Drayer, N.J.; Chen, A.F. An Update on Cementless Femoral Fixation in Total Hip Arthroplasty. J. Bone Jt. Surg. Am. 2020, 102, 1646–1661. [Google Scholar] [CrossRef] [PubMed]
- The German Arthroplasty Registry. Annual Report 2020. Available online: Https://Www.Eprd.de/Fileadmin/User_upload/Dateien/Publikationen/Berichte/AnnualReport2020-Web_2021-05-11_F.Pdf (accessed on 7 September 2021).
- Konan, S.; Abdel, M.P.; Haddad, F.S. Cemented Versus Uncemented Hip Implant Fixation: Should There Be Age Thresholds? Bone Jt. Res. 2019, 8, 604–607. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Zhong, L.; Wang, C.; Xu, M.; Li, W. Cemented Versus Uncemented Hemi-Arthroplasty for Femoral Neck Fractures in Elderly Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Medicine (Baltimore) 2020, 99, e19039. [Google Scholar] [CrossRef] [PubMed]
- Imam, M.; Shehata, M.; Morsi, M.; Shawqi, M.; Elsehili, A.; Trikha, P.; Ernstbrunner, L.; Unnithan, A.; Khaleel, A.; Monga, P.; et al. The Effect of Type of Femoral Component Fixation on Mortality and Morbidity after Hip Hemiarthroplasty: A Systematic Review and Meta-Analysis. HSS J. 2020, 16, 222–232. [Google Scholar] [CrossRef] [PubMed]
- Troelsen, A.; Malchau, E.; Sillesen, N.; Malchau, H. A Review of Current Fixation Use and Registry Outcomes in Total Hip Arthroplasty: The Uncemented Paradox. Clin. Orthop. Relat. Res. 2013, 471, 2052–2059. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Australian Orthopaedic Association National Joint Replacement Registry. Hip, Knee & Shoulder Arthroplasty Annual Report 2020. Available online: Https://Aoanjrr.Sahmri.Com/Annual-Reports-2020 (accessed on 7 September 2021).
- Norwegian National Advisory Unit on Arthroplasty and Hip Fractures. Norwegian Arthroplasty Register Report 2019. Available online: Http://Nrlweb.Ihelse.Net (accessed on 7 September 2021).
- Canadian Joint Replacement Registry. Revision Risk Curves, 2019–2020. Available online: Https://Www.Cihi.ca/Sites/Default/Files/Document/Cjrr-Revision-Risk-Curves-Data-Tables-2009-2019-En.Pdf (accessed on 7 September 2021).
- Springer, B.D.; Etkin, C.D.; Shores, P.B.; Gioe, T.J.; Lewallen, D.G.; Bozic, K.J. Perioperative Periprosthetic Femur Fractures Are Strongly Correlated with Fixation Method: An Analysis from the American Joint Replacement Registry. J. Arthroplast. 2019, 34, S352–S354. [Google Scholar] [CrossRef] [PubMed]
- Wyatt, M.; Hooper, G.; Frampton, C.; Rothwell, A. Survival Outcomes of Cemented Compared to Uncemented Stems in Primary Total Hip Replacement. World J. Orthop. 2014, 5, 591–596. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wechter, J.; Comfort, T.K.; Tatman, P.; Mehle, S.; Gioe, T.J. Improved Survival of Uncemented versus Cemented Femoral Stems in Patients Aged <70 Years in a Community Total Joint Registry. Clin. Orthop. Relat. Res. 2013, 471, 3588–3595. [Google Scholar] [CrossRef] [Green Version]
- Garden, R.S. Low-Angle Fixation in Fractures of the Femoral Neck. J. Bone Jt. Surg. Br. 1961, 43, 647–663. [Google Scholar] [CrossRef]
- Behrend, H.; Giesinger, K.; Giesinger, J.M.; Kuster, M.S. The “Forgotten Joint” as the Ultimate Goal in Joint Arthroplasty: Validation of a New Patient-Reported Outcome Measure. J. Arthroplast. 2012, 27, 430–436.e1. [Google Scholar] [CrossRef]
- Zicat, B.; Engh, C.A.; Gokcen, E. Patterns of Osteolysis around Total Hip Components Inserted with and without Cement. J. Bone Jt. Surg. Am. 1995, 77, 432–439. [Google Scholar] [CrossRef]
- Aldinger, P.R.; Breusch, S.J.; Lukoschek, M.; Mau, H.; Ewerbeck, V.; Thomsen, M. A Ten- to 15-Year Follow-Up of the Cementless Spotorno Stem. J. Bone Jt. Surg. Br. 2003, 85, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Gruen, T.A.; McNeice, G.M.; Amstutz, H.C. “Modes of Failure” of Cemented Stem-Type Femoral Components: A Radiographic Analysis of Loosening. Clin. Orthop. Relat. Res. 1979, 141, 17–27. [Google Scholar] [CrossRef]
- Clauss, M.; Van Der Straeten, C.; Goossens, M. Prospective Five-Year Subsidence Analysis of a Cementless Fully Hydroxyapatite-Coated Femoral Hip Arthroplasty Component. Hip Int. 2014, 24, 91–97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meding, J.B.; Ritter, M.A.; Keating, E.M.; Faris, P.M. Clinical and Radiographic Evaluation of Long-Stem Femoral Components Following Revision Total Hip Arthroplasty. J. Arthroplast. 1994, 9, 399–408. [Google Scholar] [CrossRef]
- Duncan, C.P.; Masri, B.A. Fractures of the Femur after Hip Replacement. Instruct. Course Lect. 1995, 44, 293–304. [Google Scholar] [PubMed]
- Magill, P.; Blaney, J.; Hill, J.C.; Bonnin, M.P.; Beverland, D.E. Impact of a Learning Curve on the Survivorship of 4802 Cementless Total Hip Arthroplasties. Bone Jt. J. 2016, 98-B, 1589–1596. [Google Scholar] [CrossRef] [PubMed]
- Reikerås, O. Total Hip Arthroplasty with a Fully Hydroxyapatite-Coated Stem: A Cohort Study During 23–28 Years. J. Arthroplast. 2017, 32, 1543–1546. [Google Scholar] [CrossRef] [PubMed]
- Wangen, H.; Nordsletten, L.; Boldt, J.G.; Fenstad, A.M.; Beverland, D.E. The Corail Stem as a Reverse Hybrid—Survivorship and x-Ray Analysis at 10 Years. Hip Int. 2017, 27, 354–360. [Google Scholar] [CrossRef]
- Jameson, S.S.; Baker, P.N.; Mason, J.; Rymaszewska, M.; Gregg, P.J.; Deehan, D.J.; Reed, M.R. Independent Predictors of Failure up to 7.5 Years after 35 386 Single-Brand Cementless Total Hip Replacements: A Retrospective Cohort Study Using National Joint Registry Data. Bone Jt. J. 2013, 95-B, 747–757. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zheng, X.; Huang, M.; Ding, C. Bond Strength of Plasma-Sprayed Hydroxyapatite/Ti Composite Coatings. Biomaterials 2000, 21, 841–849. [Google Scholar] [CrossRef]
- Walsh, W.R.; Pelletier, M.H.; Bertollo, N.; Lovric, V.; Wang, T.; Morberg, P.; Parr, W.C.H.; Bergadano, D. Bone Ongrowth and Mechanical Fixation of Implants in Cortical and Cancellous Bone. J. Orthop. Surg. Res. 2020, 15, 177. [Google Scholar] [CrossRef]
- Willburger, R.E.; Heukamp, M.; Lindenlaub, P.; Efe, T.; Peterlein, C.-D.; Schüttler, K.-F. Excellent Midterm Survival and Functional Outcomes of a Fully Hydroxyapatite-Coated Cementless Stem: First Results of a Prospective Multicenter Study. Arthroplast. Today 2020, 6, 201–205. [Google Scholar] [CrossRef] [PubMed]
- Cypres, A.; Fiquet, A.; Girardin, P.; Fitch, D.; Bauchu, P.; Bonnard, O.; Noyer, D.; Roy, C. Long-Term Outcomes of a Dual-Mobility Cup and Cementless Triple-Taper Femoral Stem Combination in Total Hip Replacement: A Multicenter Retrospective Analysis. J. Orthop. Surg. Res. 2019, 14, 376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Assaf, A.; Manara, J.R.; Teoh, K.H.; Evans, A.R. Mid-Term Clinical Results of the Cementless R3 Cup and Polarstem Total Hip Arthroplasty. Eur. J. Orthop. Surg. Traumatol. 2019, 29, 827–833. [Google Scholar] [CrossRef]
- Zimmerer, A.; Navas, L.; Kinkel, S.; Weiss, S.; Hauschild, M.; Streit, M. Midterm Survivorship of an Uncemented Hydroxyapatite-Coated Titanium Femoral Component and Clinically Meaningful Outcomes in Patients Older than 75 Years. J. Clin. Med. 2021, 10, 1019. [Google Scholar] [CrossRef]
- Ahmad, A.; Mirza, Y.; Evans, A.R.; Teoh, K.H. A Comparative Study between Uncemented and Hybrid Total Hip Arthroplasty in Octogenarians. J. Arthroplast. 2018, 33, 3719–3723. [Google Scholar] [CrossRef]
- Castellini, I.; Andreani, L.; Parchi, P.D.; Bonicoli, E.; Piolanti, N.; Risoli, F.; Lisanti, M. Hydroxyapatite in Total Hip Arthroplasty. Our Experience with a Plasma Spray Porous Titanium Alloy/Hydroxyapatite Double-Coated Cementless Stem. Clin. Cases Min. Bone Metab. 2016, 13, 221–227. [Google Scholar] [CrossRef]
- Abdel, M.P.; Watts, C.D.; Houdek, M.T.; Lewallen, D.G.; Berry, D.J. Epidemiology of Periprosthetic Fracture of the Femur in 32 644 Primary Total Hip Arthroplasties: A 40-Year Experience. Bone Jt. J. 2016, 98-B, 461–467. [Google Scholar] [CrossRef]
- Figved, W.; Opland, V.; Frihagen, F.; Jervidalo, T.; Madsen, J.E.; Nordsletten, L. Cemented versus Uncemented Hemiarthroplasty for Displaced Femoral Neck Fractures. Clin. Orthop. Relat. Res. 2009, 467, 2426–2435. [Google Scholar] [CrossRef] [Green Version]
- Grammatopoulos, G.; Wilson, H.A.; Kendrick, B.J.L.; Pulford, E.C.; Lippett, J.; Deakin, M.; Andrade, A.J.; Kambouroglou, G. Hemiarthroplasty Using Cemented or Uncemented Stems of Proven Design: A Comparative Study. Bone Jt. J. 2015, 97-B, 94–99. [Google Scholar] [CrossRef]
- Bell, K.R.; Clement, N.D.; Jenkins, P.J.; Keating, J.F. A Comparison of the Use of Uncemented Hydroxyapatite-Coated Bipolar and Cemented Femoral Stems in the Treatment of Femoral Neck Fractures: A Case-Control Study. Bone Jt. J. 2014, 96-B, 299–305. [Google Scholar] [CrossRef]
- Faisal, M.; Thomas, G.; Young, S.K. Subsidence of the Corail Femoral Component in the Elderly. A Retrospective Radiological Review. Hip Int. 2011, 21, 325–329. [Google Scholar] [CrossRef] [PubMed]
- Critchley, O.; Callary, S.; Mercer, G.; Campbell, D.; Wilson, C. Long-Term Migration Characteristics of the Corail Hydroxyapatite-Coated Femoral Stem: A 14-Year Radiostereometric Analysis Follow-Up Study. Arch. Orthop. Trauma Surg. 2020, 140, 121–127. [Google Scholar] [CrossRef] [PubMed]
- Song, J.-H.; Jo, W.-L.; Lee, K.-H.; Cho, Y.-J.; Park, J.; Oh, S. Subsidence and Perioperative Periprosthetic Fractures Using Collarless Hydroxyapatite-Coated Stem for Displaced Femoral Neck Fractures According to Dorr Type. J. Orthop. Surg. (Hong Kong) 2019, 27, 2309499019877530. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Syed, F.; Hussein, A.; Katam, K.; Saunders, P.; Young, S.K.; Faisal, M. Risk of Subsidence and Peri-Prosthetic Fractures Using Collared Hydroxyapatite-Coated Stem for Hip Arthroplasty in the Elderly. Hip Int. 2018, 28, 663–667. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Piolanti, N.; Neri, E.; Bonicoli, E.; Parchi, P.D.; Marchetti, S.; Manca, M.; Bonini, L.; Banci, L.; Scaglione, M. Use of a Plasma-Sprayed Titanium-Hydroxyapatite Femoral Stem in Hip Arthroplasty in Patients Older than 70 Years. Is Cementless Fixation a Reliable Option in the Elderly? J. Clin. Med. 2021, 10, 4735. https://doi.org/10.3390/jcm10204735
Piolanti N, Neri E, Bonicoli E, Parchi PD, Marchetti S, Manca M, Bonini L, Banci L, Scaglione M. Use of a Plasma-Sprayed Titanium-Hydroxyapatite Femoral Stem in Hip Arthroplasty in Patients Older than 70 Years. Is Cementless Fixation a Reliable Option in the Elderly? Journal of Clinical Medicine. 2021; 10(20):4735. https://doi.org/10.3390/jcm10204735
Chicago/Turabian StylePiolanti, Nicola, Elisabetta Neri, Enrico Bonicoli, Paolo Domenico Parchi, Stefano Marchetti, Mario Manca, Luca Bonini, Lorenzo Banci, and Michelangelo Scaglione. 2021. "Use of a Plasma-Sprayed Titanium-Hydroxyapatite Femoral Stem in Hip Arthroplasty in Patients Older than 70 Years. Is Cementless Fixation a Reliable Option in the Elderly?" Journal of Clinical Medicine 10, no. 20: 4735. https://doi.org/10.3390/jcm10204735
APA StylePiolanti, N., Neri, E., Bonicoli, E., Parchi, P. D., Marchetti, S., Manca, M., Bonini, L., Banci, L., & Scaglione, M. (2021). Use of a Plasma-Sprayed Titanium-Hydroxyapatite Femoral Stem in Hip Arthroplasty in Patients Older than 70 Years. Is Cementless Fixation a Reliable Option in the Elderly? Journal of Clinical Medicine, 10(20), 4735. https://doi.org/10.3390/jcm10204735




