Determination of the Standard Visual Criterion for Diagnosing and Treating Presbyopia According to Subjective Patient Symptoms
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
2.2. Inclusion and Exclusion Criteria
2.3. Ophthalmic Examinations and Questionnaire
2.4. Statistical Analysis
3. Results
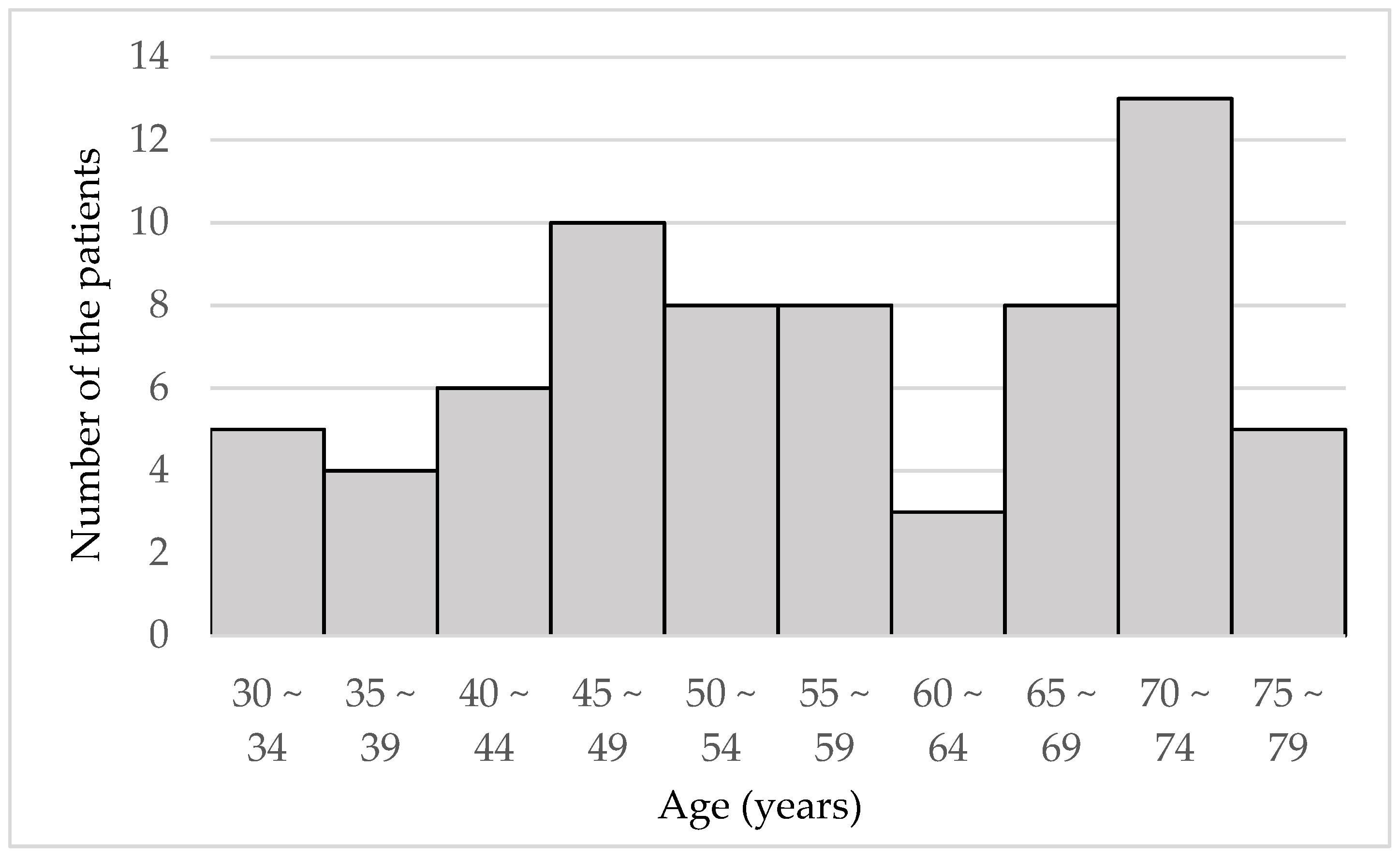
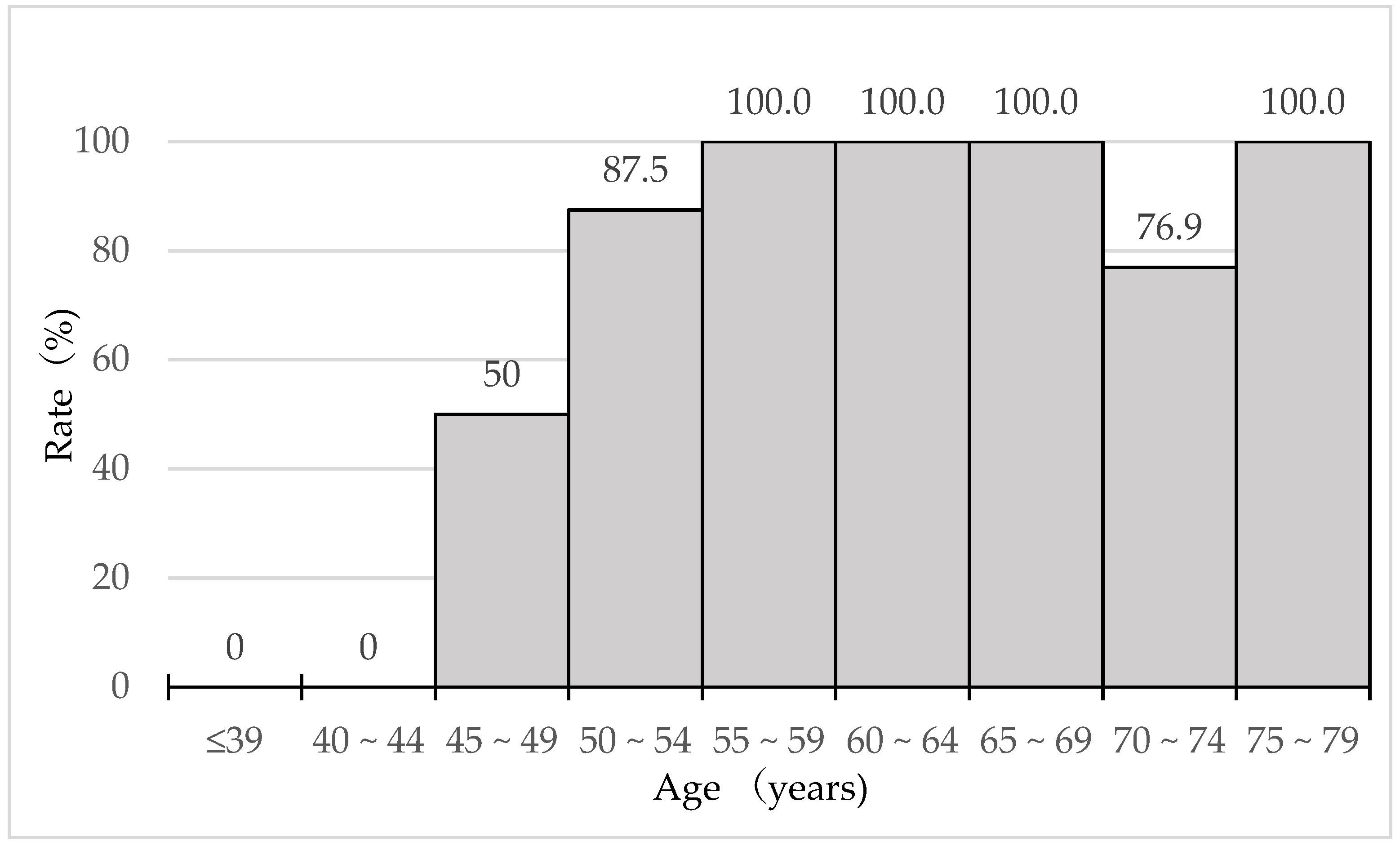
3.1. Patient Profile
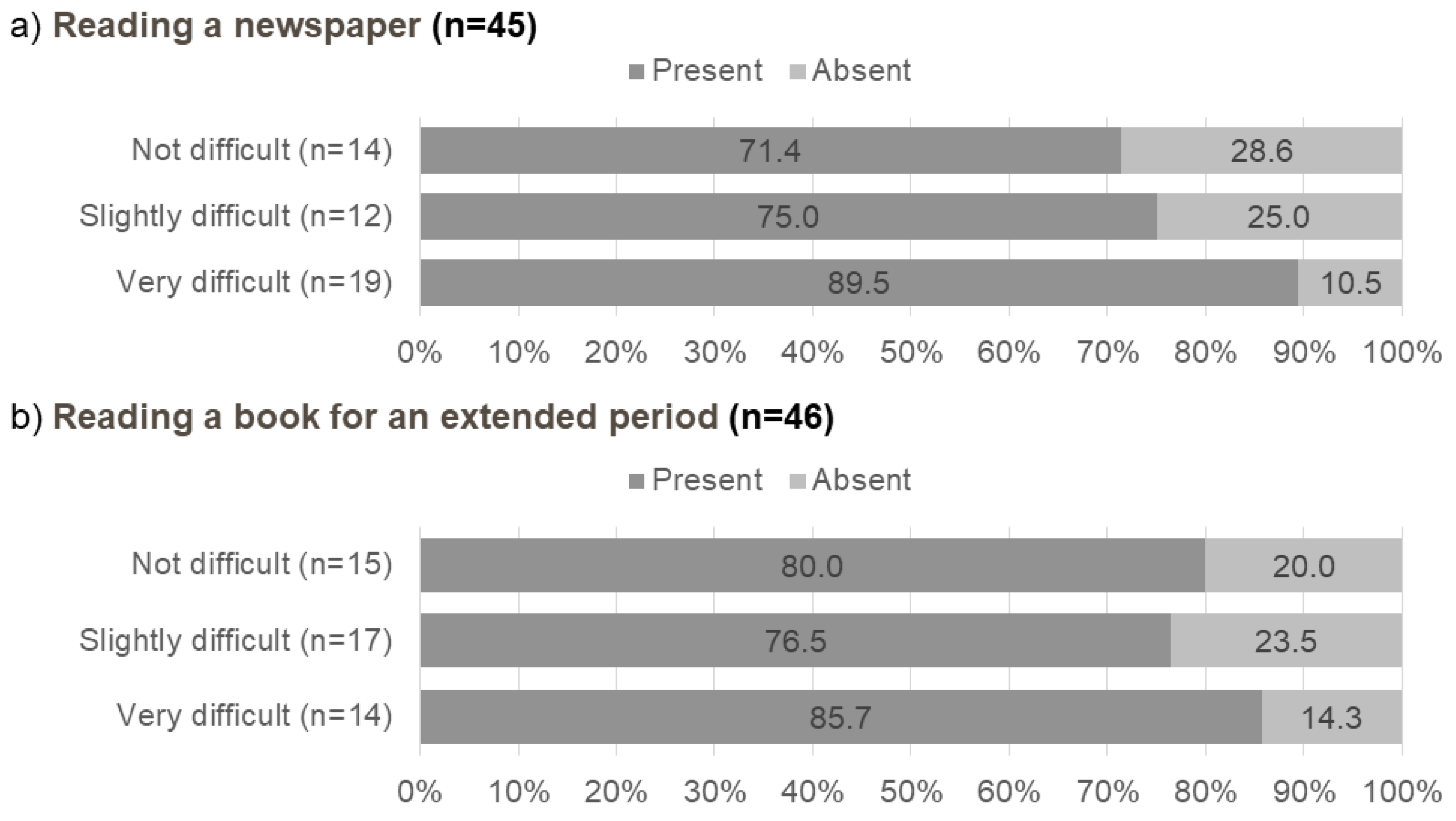
3.2. Questionnaire Results
3.3. Differences in Subjective Refraction and VAs between Patients with/without Awareness of Presbyopia
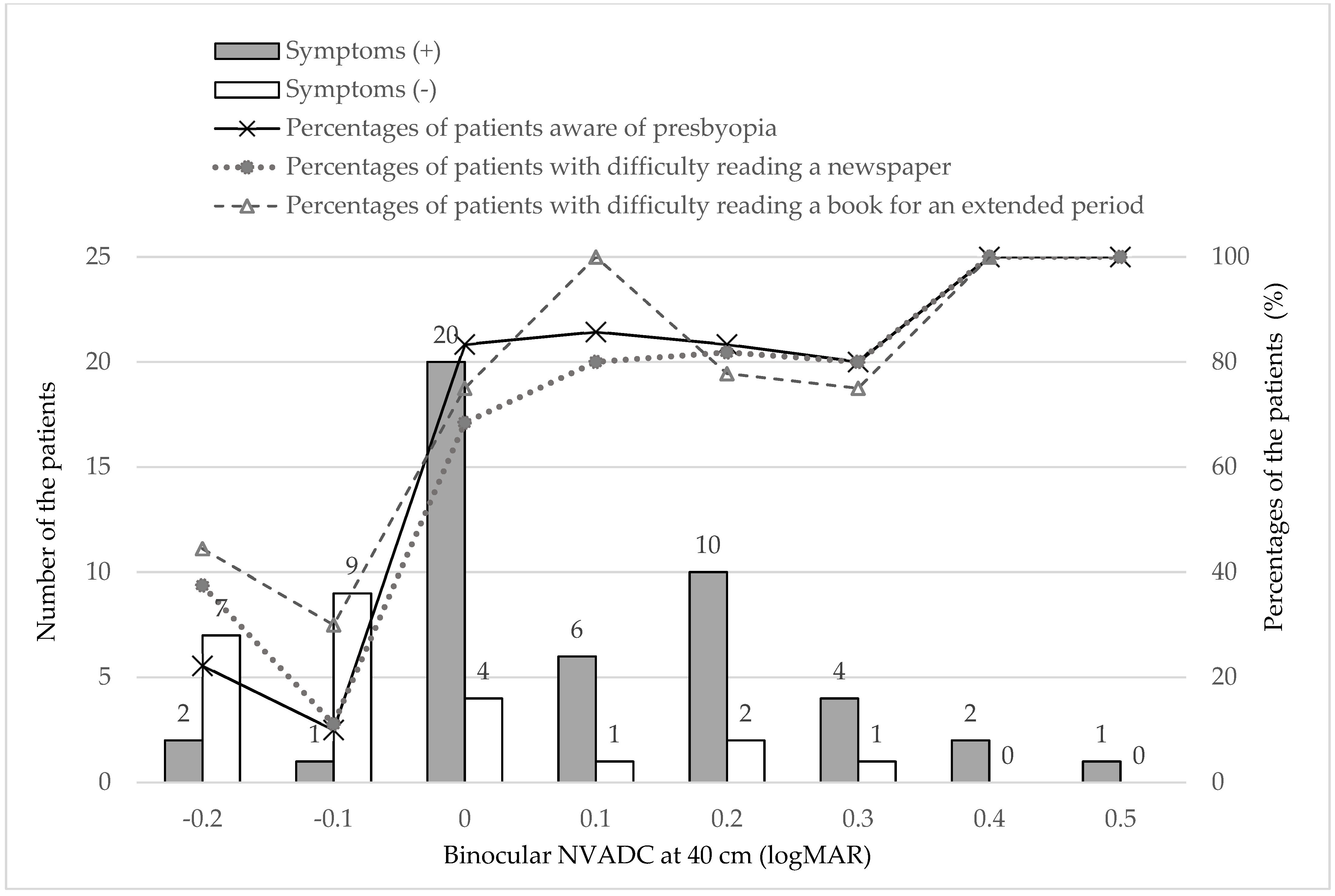
3.4. Relationship between Binocular NVA and Subjective Symptoms
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fricke, T.R.; Tahhan, N.; Resnikoff, S.; Papas, E.; Burnett, A.; Ho, S.M.; Naduvilath, T.; Naidoo, K.S. Global Prevalence of Presbyopia and Vision Impairment from Uncorrected Presbyopia: Systematic Review, Meta-analysis, and Modelling. Ophthalmology 2018, 125, 1492–1499. [Google Scholar] [CrossRef]
- Frick, K.D.; Joy, S.M.; Wilson, D.A.; Naidoo, K.S.; Holden, B.A. The Global Burden of Potential Productivity Loss from Uncorrected Presbyopia. Ophthalmology 2015, 122, 1706–1710. [Google Scholar] [CrossRef] [Green Version]
- Wolffsohn, J.S.; Davies, L.N. Presbyopia: Effectiveness of correction strategies. Prog. Retin. Eye Res. 2019, 68, 124–143. [Google Scholar] [CrossRef] [Green Version]
- Sharma, G.; Chiva-Razavi, S.; Viriato, D.; Naujoks, C.; Patalano, F.; Bentley, S.; Findley, A.; Johnson, C.; Arbuckle, R.; Wolffsohn, J. Patient-reported outcome measures in presbyopia: A literature review. BMJ Open Ophthalmol. 2020, 5, e000453. [Google Scholar] [CrossRef] [PubMed]
- Bennett, E.S. Contact lens correction of presbyopia. Clin. Exp. Optom. 2008, 91, 265–278. [Google Scholar] [CrossRef] [PubMed]
- Grzybowski, A.; Markeviciute, A.; Zemaitiene, R. A Review of Pharmacological Presbyopia Treatment. Asia Pac. J. Ophthalmol. 2020, 9, 226–233. [Google Scholar] [CrossRef]
- Hipsley, A.; Hall, B.; Rocha, K.M. Scleral surgery for the treatment of presbyopia: Where are we today? Eye Vis. 2018, 5, 4. [Google Scholar] [CrossRef] [Green Version]
- Moarefi, M.A.; Bafna, S.; Wiley, W. A Review of Presbyopia Treatment with Corneal Inlays. Ophthalmol. Ther. 2017, 6, 55–65. [Google Scholar] [CrossRef] [Green Version]
- Renna, A.; Alió, J.L.; Vejarano, L.F. Pharmacological treatments of presbyopia: A review of modern perspectives. Eye Vis. 2017, 4, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Holladay, J.T. Visual acuity measurements. J. Cataract. Refract. Surg. 2004, 30, 287–290. [Google Scholar] [CrossRef] [PubMed]
- Holden, B.A. Global Vision Impairment Due to Uncorrected Presbyopia. Arch. Ophthalmol. 2008, 126, 1731. [Google Scholar] [CrossRef] [Green Version]
- Cheng, F.; Shan, L.; Song, W.; Fan, P.; Yuan, H. Distance-and near-visual impairment in rural Chinese adults in Kailu, Inner Mongolia. Acta Ophthalmol. 2016, 94, 407–413. [Google Scholar] [CrossRef] [Green Version]
- Girum, M.; Desalegn Gudeta, A.; Shiferaw Alemu, D. Determinants of high unmet need for presbyopia correction: A community-based study in northwest Ethiopia. Clin. Optom. 2017, 9, 25–31. [Google Scholar] [CrossRef]
- Muhit, M.; Minto, H.; Parvin, A.; Jadoon, M.Z.; Islam, J.; Yasmin, S.; Khandaker, G. Prevalence of refractive error, presbyopia, and unmet need of spectacle coverage in a northern district of Bangladesh: Rapid Assessment of Refractive Error study. Ophthalmic Epidemiol. 2018, 25, 126–132. [Google Scholar] [CrossRef]
- Nsubuga, N.; Ramson, P.; Govender, P.; Chan, V.F.; Wepo, M.; Naidoo, K.S. Uncorrected refractive errors, presbyopia and spectacle coverage in Kamuli District, Uganda. Afr. Vis. Eye Health J. 2016, 75, 1–6. [Google Scholar] [CrossRef]
- Ide, T.; Fujkado, T.; Maeda, N.; Oshika, T.; Bissen-Miyajima, H.; Kurosaka, D.; Toda, I.; Arai, H.; Okamoto, S.; Hieda, O.; et al. Definition and diagnostic criteria of presbyopia 2010. Atarasii Ganka 2011, 28, 985–988. [Google Scholar]
- A Clinical Trial of the VisAbility Micro Insert System for Presbyopic Patients. Available online: https://clinicaltrials.gov/ct2/show/NCT02374671 (accessed on 29 August 2021).
- Korenfeld, M.S.; Robertson, S.M.; Stein, J.M.; Evans, D.G.; Rauchman, S.H.; Sall, K.N.; Venkataraman, S.; Chen, B.-L.; Wuttke, M.; Burns, W. Topical lipoic acid choline ester eye drop for improvement of near visual acuity in subjects with presbyopia: A safety and preliminary efficacy trial. Eye 2021, 1–10. [Google Scholar] [CrossRef]
- Vukich, J.A.; Durrie, D.S.; Pepose, J.S.; Thompson, V.; Van De Pol, C.; Lin, L. Evaluation of the small-aperture intracorneal inlay: Three-year results from the cohort of the U.S. Food and Drug Administration clinical trial. J. Cataract. Refract. Surg. 2018, 44, 541–556. [Google Scholar] [CrossRef]
- Katada, Y.; Negishi, K.; Watanabe, K.; Shigeno, Y.; Saiki, M.; Torii, H.; Kaido, M.; Tsubota, K. Functional Visual Acuity of Early Presbyopia. PLoS ONE 2016, 11, e0151094. [Google Scholar] [CrossRef] [Green Version]
- Rabbetts, R.B. Accommodation and Near Vision. The Inadequate-Stimulus Myopias; Butterworth-Heinemann: Oxford, UK; Woburn, MA, USA, 1998; pp. 114–116. [Google Scholar]
- Berdahl, J.; Bala, C.; Dhariwal, M.; Lemp-Hull, J.; Thakker, D.; Jawla, S. Patient and Economic Burden of Presbyopia: A Systematic Literature Review. Clin. Ophthalmol. 2020, 14, 3439–3450. [Google Scholar] [CrossRef]
- Hookway, L.A.; Frazier, M.; Rivera, N.; Ramson, P.; Carballo, L.; Naidoo, K. Population-based study of presbyopia in Nicaragua. Clin. Exp. Optom. 2016, 99, 559–563. [Google Scholar] [CrossRef] [PubMed]
- Naidoo, K.S.; Jaggernath, J.; Ramson, P.; Chinanayi, F.; Zhuwau, T.; Øverland, L. The prevalence of self-reported vision difficulty in economically disadvantaged regions of South Africa. Afr. J. Disabil. 2015, 4, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schellini, S.; Ferraz, F.; Opromolla, P.; Oliveira, L.; Padovani, C. Main visual symptoms associated to refractive errors and spectacle need in a Brazilian population. Int. J. Ophthalmol. 2016, 9, 1657–1662. [Google Scholar] [PubMed]
- Coles-Brennan, C.; Sulley, A.; Young, G. Management of digital eye strain. Clin. Exp. Optom. 2019, 102, 18–29. [Google Scholar] [CrossRef] [Green Version]
- Reindel, W.; Zhang, L.N.; Chinn, J.; Rah, M. Evaluation of binocular function among pre-and early-presbyopes with asthenopia. Clin. Optom. 2018, 10, 1–8. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Aware (n = 46) | Unaware (n = 24) | p Value | |
|---|---|---|---|
| Age (years) | 62.2 ± 9.7 | 44.2 ± 12.0 | 0.000 |
| Sex (male/female) | 16/30 | 14/10 | 0.059 |
| Monocular examination | |||
| Subjective refraction (SE) of the relatively hyperopic eye (D) | −1.58 ± 3.48 | −4.13 ± 3.37 | 0.005 |
| Subjective refraction (SE) of the relatively myopic eye (D) | −2.21 ± 3.80 | −4.80 ± 3.11 | 0.006 |
| CDVA (logMAR) of the better eye | −0.10 ± 0.08 | −0.12 ± 0.08 | 0.118 |
| CDVA (logMAR) of the worse eye | −0.06 ± 0.09 | −0.11 ± 0.10 | 0.013 |
| DCNVA (logMAR) at 40 cm of the better eye | 0.37 ± 0.22 | −0.03 ± 0.23 | 0.000 |
| DCNVA (logMAR) at 40 cm of the worse eye | 0.49 ± 0.27 | −0.00 ± 0.25 | 0.000 |
| Binocular examination | |||
| DVAHC (logMAR) | −0.28 ± 0.11 | −0.04 ± 0.15 | 0.434 |
| Binocular NVAHC at 40 cm (logMAR) | 0.11 ± 0.15 | −0.05 ± 0.13 | 0.000 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsuneyoshi, Y.; Masui, S.; Arai, H.; Toda, I.; Kubota, M.; Kubota, S.; Tsubota, K.; Ayaki, M.; Negishi, K. Determination of the Standard Visual Criterion for Diagnosing and Treating Presbyopia According to Subjective Patient Symptoms. J. Clin. Med. 2021, 10, 3942. https://doi.org/10.3390/jcm10173942
Tsuneyoshi Y, Masui S, Arai H, Toda I, Kubota M, Kubota S, Tsubota K, Ayaki M, Negishi K. Determination of the Standard Visual Criterion for Diagnosing and Treating Presbyopia According to Subjective Patient Symptoms. Journal of Clinical Medicine. 2021; 10(17):3942. https://doi.org/10.3390/jcm10173942
Chicago/Turabian StyleTsuneyoshi, Yukari, Sachiko Masui, Hiroyuki Arai, Ikuko Toda, Miyuki Kubota, Shunsuke Kubota, Kazuo Tsubota, Masahiko Ayaki, and Kazuno Negishi. 2021. "Determination of the Standard Visual Criterion for Diagnosing and Treating Presbyopia According to Subjective Patient Symptoms" Journal of Clinical Medicine 10, no. 17: 3942. https://doi.org/10.3390/jcm10173942
APA StyleTsuneyoshi, Y., Masui, S., Arai, H., Toda, I., Kubota, M., Kubota, S., Tsubota, K., Ayaki, M., & Negishi, K. (2021). Determination of the Standard Visual Criterion for Diagnosing and Treating Presbyopia According to Subjective Patient Symptoms. Journal of Clinical Medicine, 10(17), 3942. https://doi.org/10.3390/jcm10173942







