Is 0.01% Atropine an Effective and Safe Treatment for Myopic Children? A Systemic Review and Meta-Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Inclusion and Exclusion Criteria
2.4. Data Extraction
2.5. Quality Assessment
2.6. Data Synthesis and Statistical Analyses
3. Results
3.1. Search Results
3.2. Study Characteristics
3.3. Risk of Bias Assessment
3.4. Pooled Effects of the Efficacy Outcome
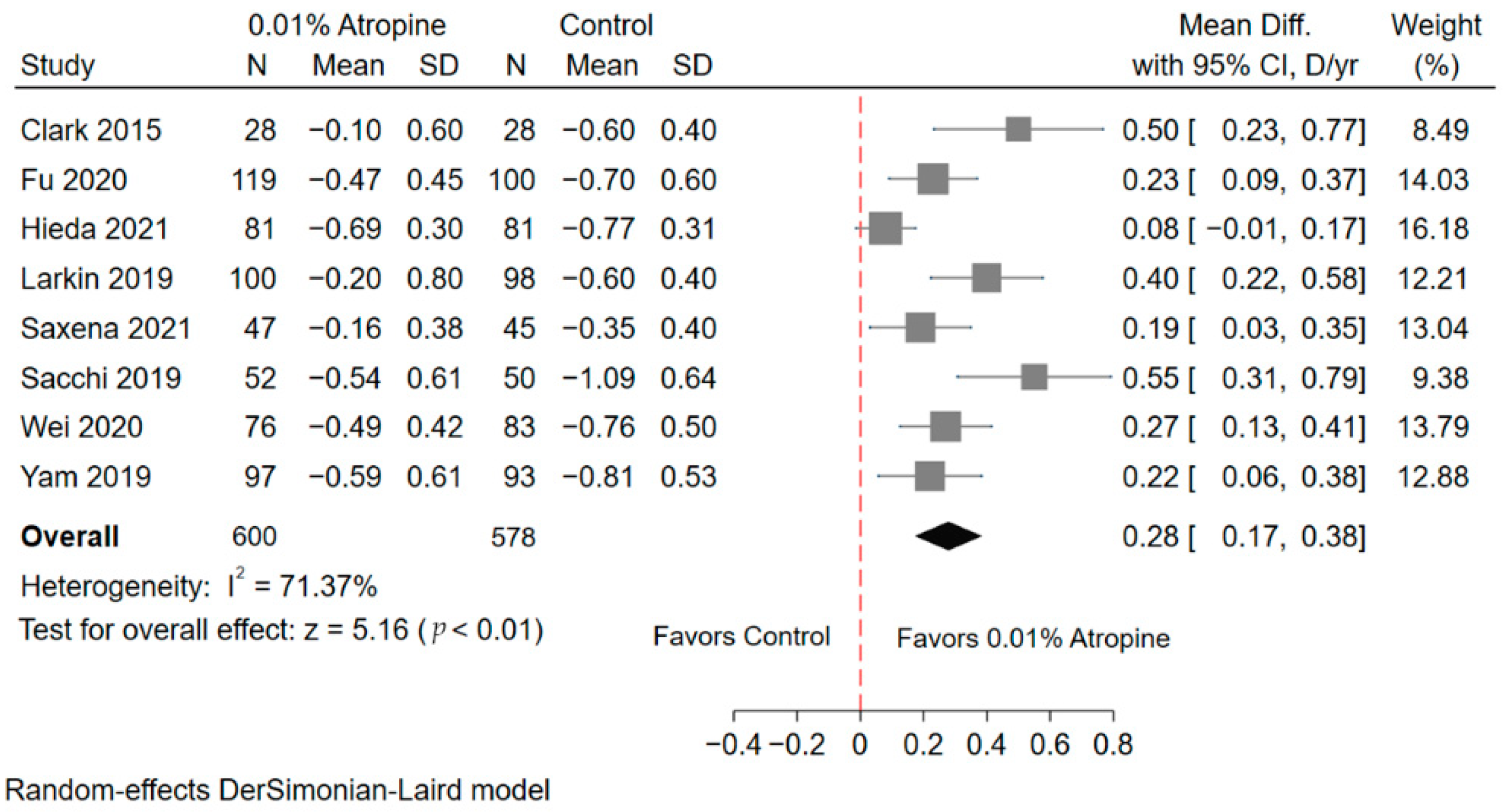
3.4.1. Spherical Equivalent Refractive Error
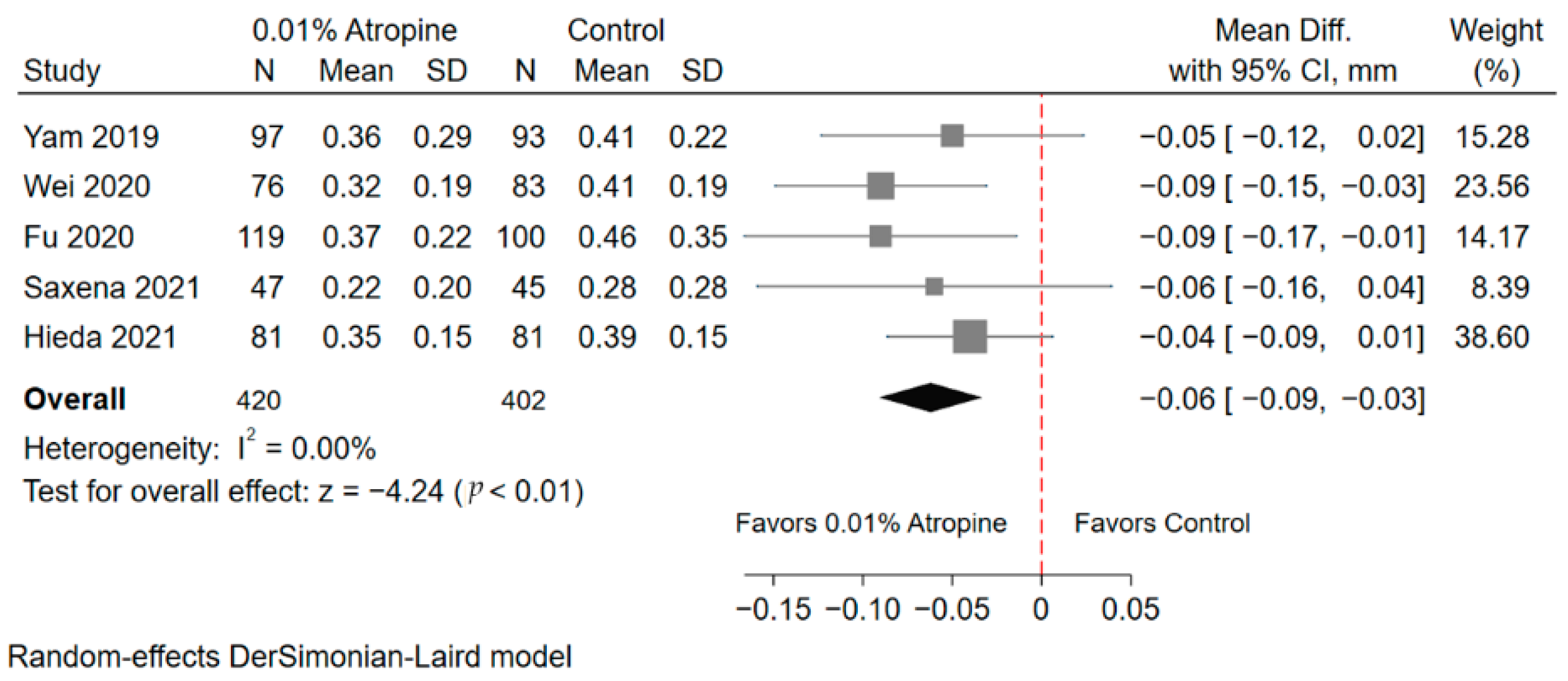
3.4.2. Axial Length
3.5. Pooled Effects of the Safety Outcome
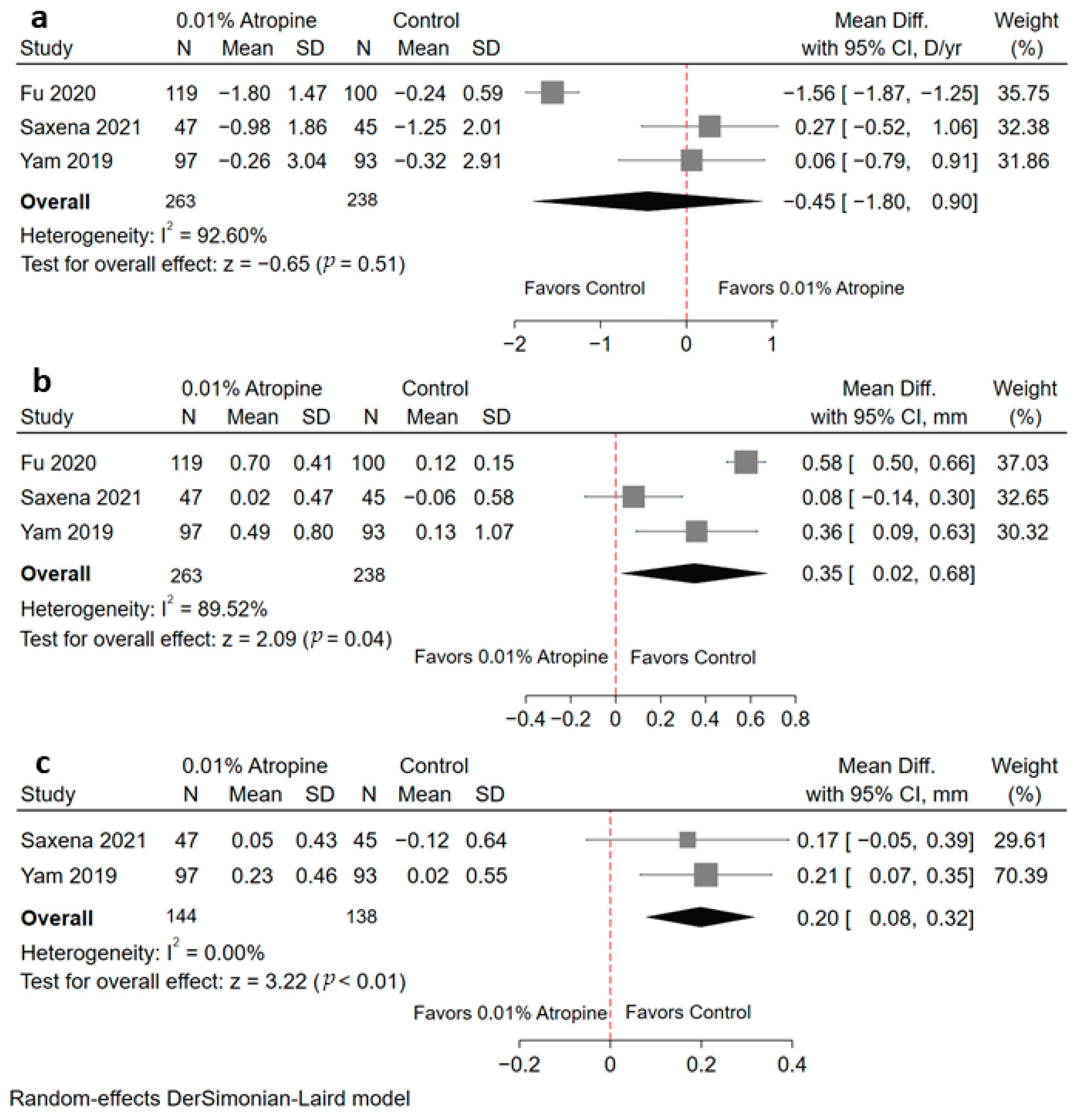
3.5.1. Accommodative Amplitude
3.5.2. Photopic Pupil Diameter
3.5.3. Mesopic Pupil Diameter
3.6. Modified Hartung–Knapp–Sidik–Jonkman (HKSJ) Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jung, S.K.; Lee, J.H.; Kakizaki, H.; Jee, D. Prevalence of myopia and its association with body stature and educational level in 19-year-old male conscripts in seoul, South Korea. Investig. Ophthalmol. Vis. Sci. 2012, 53, 5579–5583. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsumura, H.; Hirai, H. Prevalence of myopia and refractive changes in students from 3 to 17 years of age. Surv. Ophthalmol. 1999, 44 (Suppl. 1), S109–S115. [Google Scholar] [CrossRef]
- Wu, H.-M.; Seet, B.; Yap, E.P.-H.; Saw, S.-M.; Lim, T.-H.; Chia, A.K.-S. Does education explain ethnic differences in myopia prevalence? A population-based study of young adult males in Singapore. Optom. Vis. Sci. 2001, 78, 234–239. [Google Scholar] [CrossRef]
- Wu, J.F.; Bi, H.S.; Wang, S.M.; Hu, Y.Y.; Wu, H.; Sun, W.; Lu, T.L.; Wang, X.R.; Jonas, J.B. Refractive error, visual acuity and causes of vision loss in children in Shandong, China. The Shandong Children Eye Study. PLoS ONE 2013, 8, e82763. [Google Scholar] [CrossRef] [PubMed]
- Wu, L.J.; You, Q.S.; Duan, J.L.; Luo, Y.X.; Liu, L.J.; Li, X.; Gao, Q.; Zhu, H.P.; He, Y.; Xu, L.; et al. Prevalence and associated factors of myopia in high-school students in Beijing. PLoS ONE 2015, 10, e0120764. [Google Scholar] [CrossRef]
- Dolgin, E. The myopia boom. Nature 2015, 519, 276–278. [Google Scholar] [CrossRef] [Green Version]
- Fricke, T.; Holden, B.A.; Wilson, D.A.; Schlenther, G.; Naidoo, K.; Resnikoff, S.; Frick, K.D. Global cost of correcting vision impairment from uncorrected refractive error. Bull. World Health Organ. 2012, 90, 728–738. [Google Scholar] [CrossRef]
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.; Resnikoff, S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef] [Green Version]
- Rada, J.A.S.; Shelton, S.; Norton, T.T. The sclera and myopia. Exp. Eye Res. 2006, 82, 185–200. [Google Scholar] [CrossRef]
- Saw, S.M. How blinding is pathological myopia? Br. J. Ophthalmol. 2006, 90, 525–526. [Google Scholar] [CrossRef] [Green Version]
- Saw, S.-M.; Gazzard, G.; Shih-Yen, E.C.; Chua, W.-H. Myopia and associated pathological complications. Ophthalmic Physiol. Opt. 2005, 25, 381–391. [Google Scholar] [CrossRef] [PubMed]
- Tano, Y. Pathologic myopia: Where are we now? Am. J. Ophthalmol. 2002, 134, 645–660. [Google Scholar] [CrossRef]
- Ang, M.; Flanagan, J.; Wong, C.W.; Müller, A.; Davis, A.; Keys, D.; Resnikoff, S.; Jong, M.; Wong, T.Y.; Sankaridurg, P. Review: Myopia control strategies recommendations from the 2018 WHO/IAPB/BHVI Meeting on Myopia. Br. J. Ophthalmol. 2020, 104, 1482–1487. [Google Scholar] [CrossRef] [PubMed]
- Yam, J.C.; Jiang, Y.; Tang, S.M.; Law, A.K.; Chan, J.J.; Wong, E.; Ko, S.T.; Young, A.L.; Tham, C.C.; Chen, L.J.; et al. Low-Concentration Atropine for Myopia Progression (LAMP) Study: A Randomized, Double-Blinded, Placebo-Controlled Trial of 0.05%, 0.025%, and 0.01% Atropine Eye Drops in Myopia Control. Ophthalmology 2019, 126, 113–124. [Google Scholar] [CrossRef]
- Zhao, C.; Cai, C.; Ding, Q.; Dai, H. Efficacy and safety of atropine to control myopia progression: A systematic review and meta-analysis. BMC Ophthalmol. 2020, 20, 478. [Google Scholar] [CrossRef]
- Chua, W.-H.; Balakrishnan, V.; Chan, Y.-H.; Tong, L.; Ling, Y.; Quah, B.-L.; Tan, D. Atropine for the treatment of childhood myopia. Ophthalmology 2006, 113, 2285–2291. [Google Scholar] [CrossRef] [PubMed]
- Chia, A.; Lu, Q.S.; Tan, D. Five-Year Clinical Trial on Atropine for the Treatment of Myopia 2: Myopia Control with Atropine 0.01% Eyedrops. Ophthalmology 2016, 123, 391–399. [Google Scholar] [CrossRef]
- Chia, A.; Chua, W.-H.; Cheung, Y.-B.; Wong, W.-L.; Lingham, A.; Fong, A.; Tan, D. Atropine for the treatment of childhood myopia: Safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology 2012, 119, 347–354. [Google Scholar] [CrossRef] [PubMed]
- Fu, A.; Stapleton, F.; Wei, L.; Wang, W.; Zhao, B.; Watt, K.; Ji, N.; Lyu, Y. Effect of low-dose atropine on myopia progression, pupil diameter and accommodative amplitude: Low-dose atropine and myopia progression. Br. J. Ophthalmol. 2020, 104, 1535–1541. [Google Scholar] [CrossRef] [PubMed]
- Saxena, R.; Dhiman, R.; Gupta, V.; Kumar, P.; Matalia, J.; Roy, L.; Swaminathan, M.; Phuljhele, S.; Velpandian, T.; Sharma, N. Atropine for treatment of childhood myopia in India (I-ATOM): Multicentric randomized trial. Ophthalmology 2021, 161, 00079-8. [Google Scholar]
- Khanal, S.; Phillips, J.R. Which low-dose atropine for myopia control? Clin. Exp. Optom. 2020, 103, 230–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, F.F.; Kam, K.W.; Zhang, Y.; Tang, S.M.; Young, A.L.; Chen, L.J.; Tham, C.C.; Pang, C.P.; Yam, J.C. Differential Effects on Ocular Biometrics by 0.05%, 0.025%, and 0.01% Atropine: Low-Concentration Atropine for Myopia Progression Study. Ophthalmology 2020, 127, 1603–1611. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Feng, K.; Liu, R.B.; Pan, J.H.; Zhang, L.L.; Xu, Z.P.; Lu, X.J. Atropine 0.01% eye drops slow myopia progression: A systematic review and Meta-analysis. Int. J. Ophthalmol. 2019, 12, 1337–1343. [Google Scholar] [CrossRef]
- Tideman, J.W.L.; Snabel, M.C.C.; Tedja, M.S.; Van Rijn, G.A.; Wong, K.T.; Kuijpers, R.W.A.M.; Vingerling, J.R.; Hofman, A.; Buitendijk, G.H.S.; Keunen, J.E.E.; et al. Association of Axial Length with Risk of Uncorrectable Visual Impairment for Europeans With Myopia. JAMA Ophthalmol. 2016, 134, 1355–1363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moriyama, M.; Ohno-Matsui, K.; Hayashi, K.; Shimada, N.; Yoshida, T.; Tokoro, T.; Morita, I. Topographic analyses of shape of eyes with pathologic myopia by high-resolution three-dimensional magnetic resonance imaging. Ophthalmology 2011, 118, 1626–1637. [Google Scholar] [CrossRef] [PubMed]
- Yi, S.; Huang, Y.; Yu, S.Z.; Chen, X.J.; Yi, H.; Zeng, X.L. Therapeutic effect of atropine 1% in children with low myopia. J. Am. Assoc. Pediatri. Ophthalmol. Strabismus 2015, 19, 426–429. [Google Scholar] [CrossRef]
- Wei, S.; Li, S.M.; An, W.; Du, J.; Liang, X.; Sun, Y.; Zhang, D.; Tian, J.; Wang, N. Safety and Efficacy of Low-Dose Atropine Eyedrops for the Treatment of Myopia Progression in Chinese Children: A Randomized Clinical Trial. JAMA Ophthalmol. 2020, 138, 1178–1184. [Google Scholar] [CrossRef] [PubMed]
- Hieda, O.; Hiraoka, T.; Fujikado, T.; Ishiko, S.; Hasebe, S.; Torii, H.; Takahashi, H.; Nakamura, Y.; Sotozono, C.; Oshika, T.; et al. Efficacy and safety of 0.01% atropine for prevention of childhood myopia in a 2-year randomized placebo-controlled study. Jpn. J. Ophthalmol. 2021, 63, 315–325. [Google Scholar] [CrossRef]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.P.T.; Thomas, T.J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Chichester, UK, 2020. [Google Scholar]
- Guolo, A.; Varin, C. Random-effects meta-analysis: The number of studies matters. Stat. Methods Med. Res. 2017, 26, 1500–1518. [Google Scholar] [CrossRef] [PubMed]
- Veroniki, A.A.; Jackson, D.; Bender, R.; Kuss, O.; Langan, D.; Higgins, J.P.T.; Knapp, G.; Salanti, G. Methods to calculate uncertainty in the estimated overall effect size from a random-effects meta-analysis. Res. Synth. Methods 2019, 10, 23–43. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Higgins, J.P.T.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Larkin, G.L.; Tahir, A.; Epley, K.D.; Beauchamp, C.L.; Tong, J.T.; Clark, R.A. Atropine 0.01% Eye Drops for Myopia Control in American Children: A Multi-ethnic Sample Across Three US Sites. Ophthalmol. Ther. 2019, 8, 589–598. [Google Scholar] [CrossRef] [Green Version]
- Sacchi, M.; Serafino, M.; Villani, E.; Tagliabue, E.; Luccarelli, S.; Bonsignore, F.; Nucci, P. Efficacy of atropine 0.01% for the treatment of childhood myopia in European patients. Acta Ophthalmol. 2019, 97, e1136–e1140. [Google Scholar] [CrossRef] [PubMed]
- Clark, T.Y.; Clark, R.A. Atropine 0.01% Eyedrops Significantly Reduce the Progression of Childhood Myopia. J. Ocul. Pharmacol. Ther. 2015, 31, 541–545. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.; Wen, D.; Wang, Q.; McAlinden, C.; Flitcroft, I.; Chen, H.; Saw, S.M.; Chen, H.; Bao, F.; Zhao, Y.; et al. Efficacy Comparison of 16 Interventions for Myopia Control in Children: A Network Meta-Analysis. Ophthalmology 2016, 123, 697–708. [Google Scholar] [CrossRef] [Green Version]
- Gong, Q.; Janowski, M.; Luo, M.; Wei, H.; Chen, B.; Yang, G.; Liu, L. Efficacy and Adverse Effects of Atropine in Childhood Myopia: A Meta-analysis. JAMA Ophthalmol. 2017, 135, 624–630. [Google Scholar] [CrossRef] [PubMed]
- Myles, W.; Dunlop, C.; McFadden, S.A. The Effect of Long-Term Low-Dose Atropine on Refractive Progression in Myopic Australian School Children. J. Clin. Med. 2021, 10, 1444. [Google Scholar] [CrossRef] [PubMed]
- Cooper, J.; Eisenberg, N.; Schulman, E.; Wang, F.M. Maximum atropine dose without clinical signs or symptoms. Optom. Vis. Sci. 2013, 90, 1467–1472. [Google Scholar] [CrossRef]
- Sankaridurg, P.; Tran, H.D. The Lowdown on Low-Concentration Atropine for Myopia Progression. Ophthalmology 2019, 126, 125–126. [Google Scholar] [CrossRef] [Green Version]
- Yam, J.C.; Li, F.F.; Zhang, X.; Tang, S.M.; Yip, B.H.; Kam, K.W.; Ko, S.T.; Young, A.L.; Tham, C.C.; Chen, L.J.; et al. Two-Year Clinical Trial of the Low-Concentration Atropine for Myopia Progression (LAMP) Study: Phase 2 Report. Ophthalmology 2020, 127, 910–919. [Google Scholar] [CrossRef] [PubMed]
- Joachimsen, L.; Farassat, N.; Bleul, T.; Böhringer, D.; Lagrèze, W.A.; Reich, M. Side effects of topical atropine 0.05% compared to 0.01% for myopia control in German school children: A pilot study. Int. Ophthalmol. 2021, 41, 2001–2008. [Google Scholar] [CrossRef] [PubMed]
- Polling, J.R.; Kok, R.G.; Tideman, J.W.; Meskat, B.; Klaver, C.C. Effectiveness study of atropine for progressive myopia in Europeans. Eye 2016, 30, 998–1004. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Loughman, J.; Flitcroft, D.I. The acceptability and visual impact of 0.01% atropine in a Caucasian population. Br. J. Ophthalmol. 2016, 100, 1525–1529. [Google Scholar] [CrossRef] [Green Version]
- Li, S.M.; Wu, S.S.; Kang, M.T.; Liu, Y.; Jia, S.M.; Li, S.Y.; Zhan, S.Y.; Liu, L.R.; Li, H.; Chen, W.; et al. Atropine slows myopia progression more in Asian than white children by meta-analysis. Optom. Vis. Sci. 2014, 91, 342–350. [Google Scholar] [CrossRef]
| Study (Author, Year) | Country | Study Design | Study Population | Follow- Up, yr | Intervention | Number of Eyes | Mean Age (SD), yr | Mean Baseline Refraction (SD), D | Mean Baseline Axial Length (SD), mm | Drop-Out Rate |
|---|---|---|---|---|---|---|---|---|---|---|
| Clark 2015 | United states | Retrospective Case-control | Multi-ethnicity | 1.1 (0.3) | Placebo 0.01% atropine | 28 28 | 10.2 (2.2) 10.2 (2.2) | −2.0 (1.5) −2.0 (1.6) | NA NA | NA NA |
| Fu 2020 | China | RCT | Asian | 1 | Placebo 0.01% atropine | 100 119 | 9.5 (1.4) 9.3 (1.9) | −2.68 (1.42) −2.70 (1.64) | 24.55 (0.71) 24.58 (0.74) | 20/120 23/142 |
| Heida 2021 | Japan | RCT | Asian | 2 | Placebo 0.01% atropine | 80 * 78 * | 8.98 (1.50) 8.99 (1.44) | R/L: −2.96 (1.24)/ −2.97 (1.22) R//L: −2.92 (1.43)/ −2.90 (1.38) | R:/L: 24.50 (0.69)/ 24.48 (0.70) R:/L: 24.41 (0.86)/ 24.40 (0.87) | 6/86 * 7/85 * |
| Larkin 2019 | United states | Retrospective Case-control | Multi-ethnicity | 2 | Placebo 0.01% atropine | 98 100 | 9.2 (2.11) 9.3 (2.10) | −2.8 (1.6) −3.1 (1.9) | NA NA | NA NA |
| Saxena 2021 | India | RCT | Asian | 1 | Placebo 0.01% atropine | 45 47 | 10.8 (2.2) 10.6 (2.2) | −3.71 (1.37) −3.38 (1.32) | 24.70 (0.80) 24.60 (1.02) | 5/50 3/50 |
| Sacchi 2019 | Italy | Retrospective Cohort | European | 1 | Placebo 0.01% atropine | 50 52 | 12.1 (2.9) 9.7 (2.3) | −2.63 (2.68) −3.00 (2.23) | NA NA | NA NA |
| Wei 2020 | China | RCT | Asian | 1 | Placebo 0.01% atropine | 83 76 | 9.84 (1.53) 9.44 (1.80) | −2.64 (1.46) −2.52 (1.33) | 24.69 (0.97) 24.50 (0.76) | 27/110 34/110 |
| Yam 2019 | Hong Kong | RCT | Asian | 1 | Placebo 0.01% atropine | 93 97 | 8.42 (1.72) 8.23 (1.83) | −3.85 (1.95) −3.77 (1.85) | 24.82 (0.97) 24.70 (0.99) | 18/111 13/110 |
| Standardized Equivalent Refraction (SER) | ||||
|---|---|---|---|---|
| Subgroups | No. of Studies | Pooled MD (95% CI) | p-Value | I2 (%) |
| Overall | 8 | 0.28 (0.17 to 0.38) | <0.01 ** | 71.4 |
| Study design | ||||
| RCTs | 5 | 0.18 (0.11 to 0.26) | <0.01 ** | 38.5 |
| Non-RCTs | 3 | 0.46 (0.34 to 0.59) | <0.01 ** | 0.0 |
| Study population | ||||
| Asian only | 5 | 0.18 (0.11 to 0.26) | <0.01 ** | 38.5 |
| European only | 1 | 0.55 (0.31 to 0.79) | <0.01 ** | - |
| Multi-ethnicity | 2 | 0.43 (0.28 to 0.58) | <0.01 ** | 0.0 |
| Mean age, year | ||||
| Age < 10 | 5 | 0.23 (0.12 to 0.34) | <0.01 ** | 67.5 |
| Age > 10 | 3 | 0.40 (0.15 to 0.65) | <0.01 ** | 73.9 |
| Mean baseline refraction, Diopter | ||||
| >−3.00 | 6 | 0.31 (0.17 to 0.46) | <0.01 ** | 79.4 |
| <−3.00 | 2 | 0.20 (0.09 to 0.32) | <0.01 ** | 0.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsai, H.-R.; Chen, T.-L.; Wang, J.-H.; Huang, H.-K.; Chiu, C.-J. Is 0.01% Atropine an Effective and Safe Treatment for Myopic Children? A Systemic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 3766. https://doi.org/10.3390/jcm10173766
Tsai H-R, Chen T-L, Wang J-H, Huang H-K, Chiu C-J. Is 0.01% Atropine an Effective and Safe Treatment for Myopic Children? A Systemic Review and Meta-Analysis. Journal of Clinical Medicine. 2021; 10(17):3766. https://doi.org/10.3390/jcm10173766
Chicago/Turabian StyleTsai, Hou-Ren, Tai-Li Chen, Jen-Hung Wang, Huei-Kai Huang, and Cheng-Jen Chiu. 2021. "Is 0.01% Atropine an Effective and Safe Treatment for Myopic Children? A Systemic Review and Meta-Analysis" Journal of Clinical Medicine 10, no. 17: 3766. https://doi.org/10.3390/jcm10173766
APA StyleTsai, H.-R., Chen, T.-L., Wang, J.-H., Huang, H.-K., & Chiu, C.-J. (2021). Is 0.01% Atropine an Effective and Safe Treatment for Myopic Children? A Systemic Review and Meta-Analysis. Journal of Clinical Medicine, 10(17), 3766. https://doi.org/10.3390/jcm10173766






