Using Out-of-Hospital Cardiac Arrest (OHCA) and Cardiac Arrest Hospital Prognosis (CAHP) Scores with Modified Objective Data to Improve Neurological Prognostic Performance for Out-of-Hospital Cardiac Arrest Survivors
Abstract
:1. Introduction
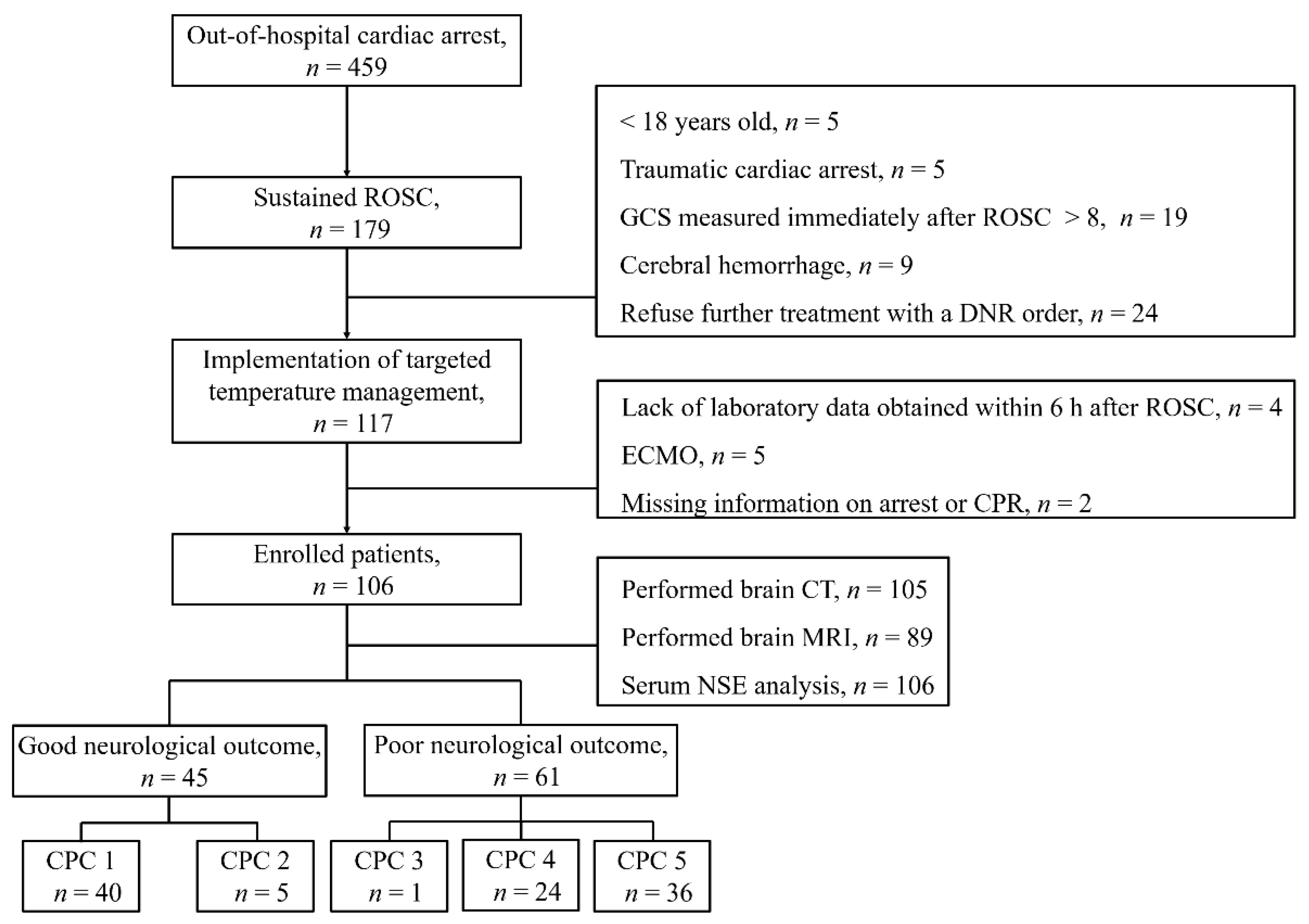
2. Patients and Methods
2.1. Study Design and Patients
2.2. Target Temperature Management Protocol
2.3. Brain Imaging and Biochemical Indicators
2.4. Outcomes and Data Collection
2.5. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Prognostic Performance of Each Method
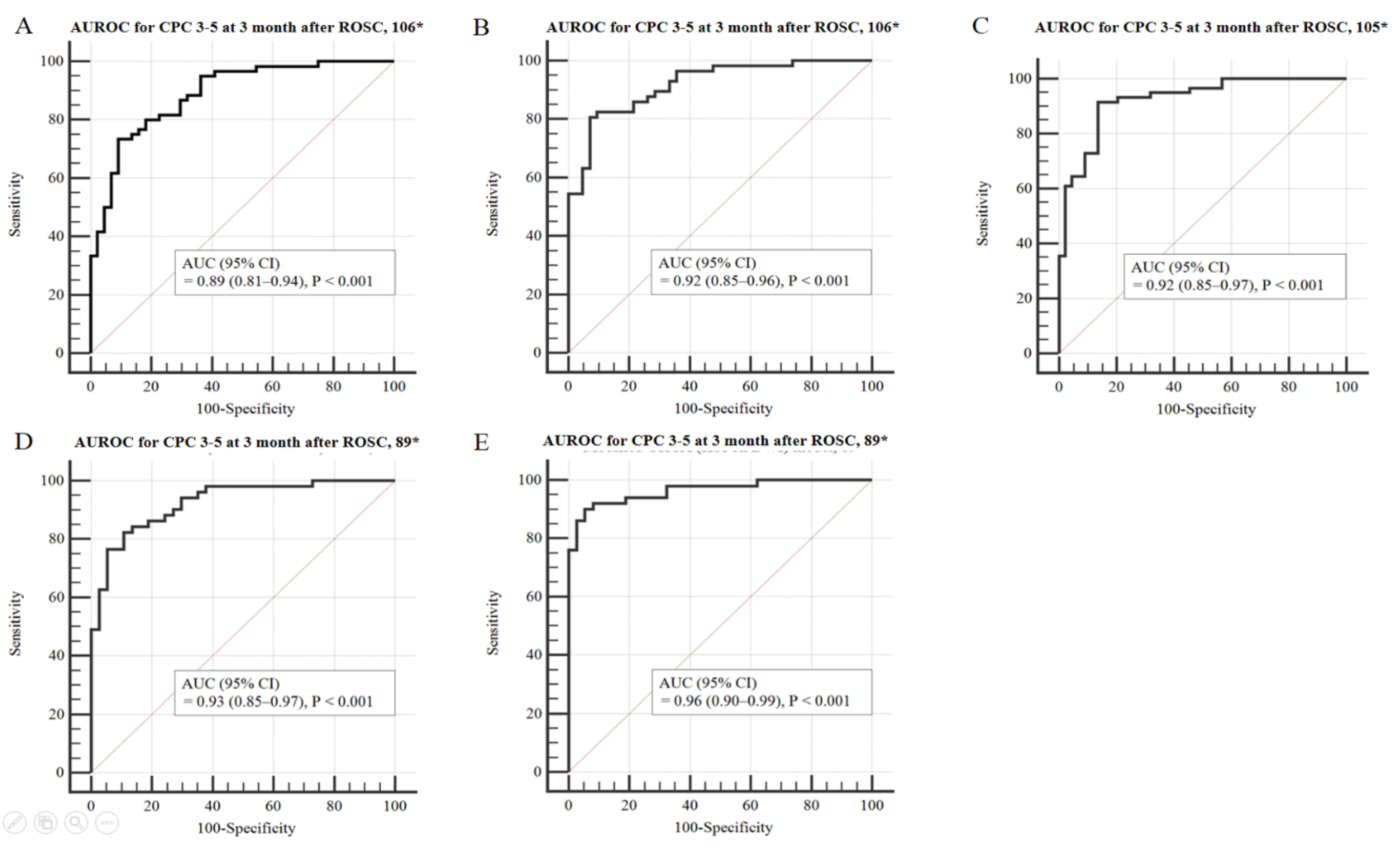
3.3. Prognostic Performance Comparison Using Modified OHCA and CAHP Models
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ADC | apparent diffusion coefficient |
| AUROC | area under the receiver operating characteristic curve |
| CA | cardiac arrest |
| CAHP | cardiac arrest hospital prognosis |
| CI | confidence interval |
| CK-MB | creatinine kinase myocardial band |
| CN | caudate nucleus |
| CPC | cerebral performance category |
| CPR | cardiopulmonary resuscitation |
| CNUH | Chungnam National University Hospital |
| CT | computed tomography |
| DWI | diffusion-weighted imaging |
| ECMO | extracorporeal membrane oxygenation |
| FMRIB | functional magnetic resonance imaging of the brain |
| GWR | grey/white matter ratio |
| HIS | high-signal intensity |
| IQR | interquartile range |
| MRI | magnetic resonance imaging |
| NGAL | neutrophil gelatinase-associated lipocalin |
| NSE OHCA | neuron-specific enolase out-of-hospital cardiac arrest |
| P | putamen |
| PIC | posterior limb of the internal capsule |
| PV | percentage voxels |
| ROC | receiver operating curve |
| ROSC | return of spontaneous circulation |
| T | thalamus |
| TTM | targeted temperature management |
| TWA | time-weighted average |
| WLST | withdrawal of life-sustaining treatment |
References
- Benjamin, E.J.; Muntner, P.; Alonso, A.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Das, S.R.; et al. Heart disease and stroke statistics—2019 update: A report from the American heart association. Circulation 2019, 139, e56–e528. [Google Scholar] [CrossRef]
- Dragancea, I.; Wise, M.P.; Al-Subaie, N.; Cranshaw, J.; Friberg, H.; Glover, G.; Pellis, T.; Rylance, R.; Walden, A.; Nielsen, N.; et al. Protocol-driven neurological prognostication and withdrawal of life-sustaining therapy after cardiac arrest and targeted temperature management. Resuscitation 2017, 117, 50–57. [Google Scholar] [CrossRef]
- Elmer, J.; Torres, C.; Aufderheide, T.P.; Austin, M.A.; Callaway, C.W.; Golan, E.; Herren, H.; Jasti, J.; Kudenchuk, P.J.; Scales, D.C.; et al. Association of early withdrawal of life-sustaining therapy for perceived neurological prognosis with mortality after cardiac arrest. Resuscitation 2016, 102, 127–135. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Adrie, C.; Cariou, A.; Mourvillier, B.; Laurent, I.; Dabbane, H.; Hantala, F.; Rhaoui, A.; Thuong, M.; Monchi, M. Predicting survival with good neurological recovery at hospital admission after successful resuscitation of out-of-hospital cardiac arrest: The OHCA score. Eur. Heart J. 2006, 27, 2840–2845. [Google Scholar] [CrossRef] [Green Version]
- Maupain, C.; Bougouin, W.; Lamhaut, L.; Deye, N.; Diehl, J.-L.; Geri, G.; Perier, M.-C.; Beganton, F.; Marijon, E.; Jouven, X.; et al. The CAHP (Cardiac Arrest Hospital Prognosis) score: A tool for risk stratification after out-of-hospital cardiac arrest. Eur. Heart J. 2016, 37, 3222–3228. [Google Scholar] [CrossRef] [PubMed]
- Kiehl, E.L.; Parker, A.M.; Matar, R.M.; Gottbrecht, M.F.; Johansen, M.C.; Adams, M.P.; Griffiths, L.A.; Dunn, S.P.; Bidwell, K.L.; Menon, V.; et al. C-GRApH: A Validated Scoring System for Early Stratification of Neurologic Outcome After Out-of-Hospital Cardiac Arrest Treated with Targeted Temperature Management. J. Am. Heart Assoc. 2017, 6, e003821. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.S.; Park, K.N.; Kim, S.H.; Lee, B.K.; Oh, S.H.; Jeung, K.W.; Choi, S.P.; Youn, C.S. Prognostic value of OHCA, C-GRApH and CAHP scores with initial neurologic examinations to predict neurologic outcomes in cardiac arrest patients treated with targeted temperature management. PLoS ONE 2020, 15, e0232227. [Google Scholar] [CrossRef] [PubMed]
- Bae, D.H.; Lee, H.Y.; Jung, Y.H.; Jeung, K.W.; Lee, B.K.; Youn, C.S.; Kang, B.S.; Heo, T.; Min, Y.I. PROLOGUE (PROgnostication using LOGistic regression model for Unselected adult cardiac arrest patients in the Early stages): Development and validation of a scoring system for early prognostication in unselected adult cardiac arrest patients. Resuscitation 2021, 159, 60–68. [Google Scholar] [CrossRef] [PubMed]
- Chelly, J.; Mpela, A.-G.; Jochmans, S.; Brunet, J.; Legriel, S.; Guerin, L.; Soummer, A.; Persichini, R.; Sauneuf, B.; Pham, T.; et al. OHCA (Out-of-Hospital Cardiac Arrest) and CAHP (Cardiac Arrest Hospital Prognosis) scores to predict outcome after in-hospital cardiac arrest: Insight from a multicentric registry. Resuscitation 2020, 156, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Nishikimi, M.; Matsuda, N.; Matsui, K.; Takahashi, K.; Ejima, T.; Liu, K.; Ogura, T.; Higashi, M.; Umino, H.; Makishi, G.; et al. A novel scoring system for predicting the neurologic prognosis prior to the initiation of induced hypothermia in cases of post-cardiac arrest syndrome: The CAST score. Scand. J. Trauma Resusc. Emerg. Med. 2017, 25, 49. [Google Scholar] [CrossRef]
- Soar, J.; Callaway, C.W.; Aibiki, M.; Böttiger, B.W.; Brooks, S.C.; Deakin, C.D.; Donnino, M.W.; Drajer, S.; Kloeck, W.; Morley, P.T.; et al. Part 4: Advanced life support. Resuscitation 2015, 95, e71–e120. [Google Scholar] [CrossRef]
- Lee, B.K.; Jeung, K.W.; Song, K.H.; Jung, Y.H.; Choi, W.J.; Kim, S.H.; Youn, C.S.; Cho, I.S.; Lee, D.H. Prognostic values of gray matter to white matter ratios on early brain computed tomography in adult comatose patients after out-of-hospital cardiac arrest of cardiac etiology. Resuscitation 2015, 96, 46–52. [Google Scholar] [CrossRef]
- Jeon, C.H.; Park, J.S.; Lee, J.H.; Kim, H.; Kim, S.C.; Park, K.H.; Yi, K.S.; Kim, S.M.; Youn, C.S.; Kim, Y.-M.; et al. Comparison of brain computed tomography and diffusion-weighted magnetic resonance imaging to predict early neurologic outcome before target temperature management comatose cardiac arrest survivors. Resuscitation 2017, 118, 21–26. [Google Scholar] [CrossRef]
- Park, J.S.; In, Y.N.; You, Y.H.; Min, J.H.; Ahn, H.J.; Yoo, I.S.; Kim, S.W.; Lee, J.W.; Ryu, S.; Jeong, W.J.; et al. Ultra-early neurologic outcome prediction of out-of-hospital cardiac arrest survivors using combined diffusion-weighted imaging findings and quantitative analysis of apparent diffusion coefficient. Resuscitation 2020, 148, 39–48. [Google Scholar] [CrossRef]
- Son, S.H.; Lee, I.H.; Park, J.S.; Yoo, I.S.; Kim, S.W.; Lee, J.W.; Ryu, S.; You, Y.; Min, J.H.; Cho, Y.C.; et al. Does Combining Biomarkers and Brain Images Provide Improved Prognostic Predictive Performance for Out-Of-Hospital Cardiac Arrest Survivors before Target Temperature Management? J. Clin. Med. 2020, 9, 744. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.I.; Lee, I.H.; Park, J.S.; Kim, D.M.; You, Y.; Min, J.H.; Cho, Y.C.; Jeong, W.J.; Ahn, H.J.; Kang, C.; et al. The Usefulness of Quantitative Analysis of Blood-Brain Barrier Disruption Measured Using Contrast-Enhanced Magnetic Resonance Imaging to Predict Neurological Prognosis in Out-of-Hospital Cardiac Arrest Survivors: A Preliminary Study. J. Clin. Med. 2020, 9, 3013. [Google Scholar] [CrossRef]
- You, Y.; Park, J.S.; Min, J.; Yoo, I.; Ahn, H.J.; Cho, Y.; Ryu, S.; Lee, J.; Kim, S.; Cho, S.; et al. The usefulness of neuron-specific enolase in cerebrospinal fluid to predict neurological prognosis in cardiac arrest survivors who underwent target temperature management: A prospective observational study. Resuscitation 2019, 145, 185–191. [Google Scholar] [CrossRef]
- Kang, C.; In, Y.N.; Park, J.S.; You, Y.; Min, J.H.; Yoo, I.; Cho, Y.C.; Jeong, W.; Ahn, H.J.; Ryu, S.; et al. Impact of low and high partial pressure of carbon dioxide on neuron-specific enolase derived from serum and cerebrospinal fluid in patients who underwent targeted temperature management after out-of-hospital cardiac arrest: A retrospective study. Resuscitation 2020, 153, 79–87. [Google Scholar] [CrossRef] [PubMed]
- Hong, J.Y.; Lee, D.H.; Oh, J.H.; Lee, S.H.; Choi, Y.H.; Kim, S.H.; Min, J.H.; Kim, S.J.; Park, Y.S. Grey–white matter ratio measured using early unenhanced brain computed tomography shows no correlation with neurological outcomes in patients undergoing targeted temperature management after cardiac arrest. Resuscitation 2019, 140, 161–169. [Google Scholar] [CrossRef] [PubMed]
- Wijman, C.A.C.; Mlynash, M.; Caulfield, A.F.; Hsia, A.W.; Eyngorn, I.; Bammer, R.; Fischbein, N.; Albers, G.W.; Moseley, M. Prognostic value of brain diffusion-weighted imaging after cardiac arrest. Ann. Neurol. 2009, 65, 394–402. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Panchal, A.R.; Bartos, J.A.; Cabañas, J.G.; Donnino, M.W.; Drennan, I.R.; Hirsch, K.G.; Kudenchuk, P.J.; Kurz, M.C.; Lavonas, E.J.; Morley, P.T.; et al. Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2020, 142, S366–S468. [Google Scholar] [CrossRef]
- Vondrakova, D.; Kruger, A.; Janotka, M.; Malek, F.; Dudkova, V.; Neuzil, P.; Ostadal, P. Association of neuron-specific enolase values with outcomes in cardiac arrest survivors is dependent on the time of sample collection. Crit. Care 2017, 21, 172. [Google Scholar] [CrossRef] [Green Version]
- Perkins, G.D.; Handley, A.J.; Koster, R.W.; Castrén, M.; Smyth, M.A.; Olasveengen, T.; Monsieurs, K.G.; Raffay, V.; Gräsner, J.-T.; Wenzel, V.; et al. European Resuscitation Council Guidelines for Resuscitation 2015. Resuscitation 2015, 95, 81–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nielsen, N.; Wetterslev, J.; Cronberg, T.; Erlinge, D.; Gasche, Y.; Hassager, C.; Horn, J.; Hovdenes, J.; Kjaergaard, J.; Kuiper, M.; et al. Targeted Temperature Management at 33 °C versus 36 °C after Cardiac Arrest. N. Engl. J. Med. 2013, 369, 2197–2206. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lascarrou, J.-B.; Merdji, H.; Le Gouge, A.; Colin, G.; Grillet, G.; Girardie, P.; Coupez, E.; Dequin, P.-F.; Cariou, A.; Boulain, T.; et al. Targeted Temperature Management for Cardiac Arrest with Nonshockable Rhythm. N. Engl. J. Med. 2019, 381, 2327–2337. [Google Scholar] [CrossRef]
- Hirsch, K.G.; Fischbein, N.; Mlynash, M.; Kemp, S.; Bammer, R.; Eyngorn, I.; Tong, J.; Moseley, M.; Venkatasubramanian, C.; Caulfield, A.F.; et al. Prognostic value of diffusion-weighted MRI for post-cardiac arrest coma. Neurology 2020, 94, e1684–e1692. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Cohort (n = 106) | Good Neurological Outcome (n = 45) | Poor Neurological Outcome (n = 61) | p-Value |
|---|---|---|---|---|
| Age, years, median (IQR) | 57.0 (41.0–69.0) | 57.0 (42.0–68.0) | 57.0 (40.5–76.8) | 0.773 |
| Male gender, n (%) | 78 (73.6) | 37 (82.2) | 41 (67.2) | 0.193 |
| Comorbidities, n (%) | 0.544 | |||
| Coronary artery disease | 23 (21.7) | 11 (24.4) | 12 (19.7) | |
| Arrhythmia | 15 (14.2) | 5 (11.1) | 10 (16.4) | |
| Atrial fibrillation | 12 (11.3) | 3 (6.7) | 9 (14.8) | |
| WPW syndrome | 1 (0.9) | 1 (2.2) | 0 (0) | |
| VPC | 1 (0.9) | 0 (0) | 1 (1.6) | |
| 1st degree AV block | 1 (0.9) | 1 (2.2) | 0 (0) | |
| Cardiomyopathy | 2 (1.9) | 1 (2.2) | 1 (1.6) | |
| Hypertrophic cardiomyopathy | 2 (19) | 1 (2.2) | 1 (1.6) | |
| Heart failure | 7 (6.6) | 3 (6.7) | 4 (6.6) | |
| Etiology of cardiac arrest, n (%) | 0.863 | |||
| Acute coronary syndrome | 25 (23.6) | 12 (26.7) | 13 (21.3) | |
| Arrythmia | 16 (15.1) | 6 (13.3) | 10 (16.4) | |
| Hypoxia | 48 (45.3) | 21 (46.7) | 27 (44.3) | |
| Hyperkalemia | 4 (3.8) | 2 (4.4) | 2 (3.3) | |
| Metabolic acidosis | 2 (1.9) | 2 (4.4) | 2 (3.3) | |
| Anaphylaxis | 1 (0.9) | 1 (2.2) | 0 (0) | |
| Pulmonary thromboembolism | 1 (0.9) | 0 (0) | 1 (1.6) | |
| Unknown | 9 (8.5) | 3 (6.7) | 6 (9.8) | |
| Arrest characteristics | ||||
| Witness, n (%), | 69 (63.9) | 36 (80) | 33 (53.2) | 0.004 |
| Location of arrest, public place, n (%) | 29 (26.9) | 13 (28.9) | 15 (24.2) | 0.586 |
| Bystander CPR, n (%) | 77 (71.3) | 39 (86.7) | 38 (61.3) | 0.004 |
| Shockable rhythm, n (%) | 30 (27.8) | 24 (53.3) | 5 (8.1) | <0.001 |
| No flow time, min, median (IQR) | 2.0 (0–13.0) | 0.0 (0.0–5.0) | 5.0 (0.0–22.0) | 0.02 |
| Low flow time, min, median (IQR) | 20.0 (6.4–33.0) | 15.0 (8.0–20.0) | 29.0 (19.0–43.8) | <0.001 |
| Epinephrine dose administered during CPR, mg, median (IQR) | 2 (0–4) | 0 (0–2) | 3 (1.5–5) | <0.001 |
| Laboratory parameters | ||||
| pH, median (IQR) | 7.16 (7.00–7.32) | 7.27 (7.08–7.35) | 7.10 (6.97–7.30) | 0.024 |
| Lactate, mmol L−1, median (IQR) | 7.75 (4.73–11.33) | 7.70 (4.00–11.00) | 7.80 (4.90–12.00) | 0.050 |
| Albumin, g dL−1, median (IQR) | 3.3 (2.9–3.6) | 3.4 (3.2–3.6) | 3.2 (2.9–3.6) | 0.015 |
| Creatinine, mg dL−1, median (IQR) | 1.26 (0.95–2.55) | 1.26 (0.95–1.84) | 1.27 (0.94–2.91) | 0.350 |
| NGAL, ng mL−1, median (IQR) | 231.1 (100.8–677.7) | 155.4 (78.3–451.6) | 265.0 (130.7–683.0) | 0.002 |
| NSE, ng mL−1, median (IQR) | ||||
| Day 0 | 30.8 (23.3–58.0) | 24.0 (18.0–30.1) | 50.4 (29.4–73.3) | <0.001 |
| Day 1 | 39.8 (24.3–116.0), 95 * | 26.9 (20.6–35.8),40 * | 82.6 (33.7–277), 55 * | <0.001 |
| Day 2 | 35.1 (21.4–121.3), 88 * | 22.4 (16.4–24.5), 39 * | 97.2 (42.3–296.5), 49 * | <0.001 |
| Day 3 | 36.6 (17.6–144.0), 83 * | 18.3 (14.0–28.3), 38 * | 113.4 (37.2–276.0), 45 * | <0.001 |
| CK-MB, ng mL−1, median (IQR) | 5.6 (2.6–9.8) | 4.8 (1.9–8.4) | 6.6 (3.4–12.0) | 0.037 |
| Troponin I, ng mL−1, median (IQR) | 0.55 (0.06–52.8) | 0.17 (0.03–34.6) | 1.77 (0.10–273.00) | 0.131 |
| White blood cell, 103 u L−1, median (IQR) | 12.8 (8.8–17.6) | 12.8 (8.7–17.4) | 12.8 (8.8–18.7) | 0.625 |
| C-reactive protein, mg L−1, median (IQR) | 0.6 (0.5–0.7) | 0.5 (0.5–0.6) | 0.6 (0.5–0.9) | 0.249 |
| Procalcitonin, ng mL−1, median (IQR) | 0.22 (0.05–0.56) | 0.05 (0.05–0.22) | 0.30 (0.06–2.05) | 0.003 |
| Interleukin-6, pg mL−1, median (IQR) | 411.8 (017.4–2012.5) | 205.5 (57.8–513.6) | 595.0 (129.8–5000.0) | 0.013 |
| TWA–PaCO2, mmHg, median (IQR) | 38.8 (33.5–45.7) | 41.4 (34.2–47.3) | 37.9 (33.5–45.7) | 0.334 |
| ROSC to induction time at 33 °C, min (IQR) | 357 (0.0-1140.0) | 350.0 (120.0-767.0) | 358.0 (0.0-1140.0) | 0.680 |
| Received intervention prior to TTM, n (%) | ||||
| Coronary angiography | 31 (29.2) | 12 (26.7) | 19 (31.1) | 0.670 |
| Percutaneous coronary intervention | 13 (12.3) | 7 (15.6) | 6 (9.8) | 0.551 |
| Brain image | ||||
| ROSC to CT time, min (IQR) | 76.0 (41.0–117.0), 105 * | 67.0 (35.0–93.0), 45 * | 84.5 (49.8–134.3), 60 * | 0.129 |
| ROSC to MRI time, min (IQR) | 156.0 (111.5–227.5), 89 * | 131.0 (100.0–200.0), 37 * | 165.0 (120.3–240.3), 52 * | 0.294 |
| GWR of CT, median (IQR) | 1.21(1.11–1.29), 105 * | 1.25 (1.20–1.31), 45 * | 1.14 (1.06–1.24), 60 * | <0.001 |
| HSI on DWI, number (%) | 36 (33.3), 89 * | 0 (0), 37 * | 36 (69.2), 52 * | <0.001 |
| PV 400 ** of ADC, median (IQR) | 2.29 (0.32–4.18), 89* | 0.38 (1.18–2.89), 37 * | 3.41 (1.20–16.46), 52 * | <0.001 |
| CA-specific risk score | ||||
| OHCA score | 35.1 (23.4–56.0) | 23.5 (16.9–29.3) | 52.7 (38.0–61.2) | <0.001 |
| CAHP score | 181.0 (130.5–231.5) | 130.5 (103.4–156.6) | 217.5 (191.0–266.5) | <0.001 |
| C-GRApH score | 2.0 (2.0–3.0) | 2.0 (1.0–3.0) | 3.0 (2.0–3.0) | <0.001 |
| AUROC (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | PPV | NPV (95% CI) | p-Value for AUROC Comparison | |
|---|---|---|---|---|---|---|
| Predicting CA-specific risk score | ||||||
| OHCA | 0.86 (0.78–0.92) | 25.0 (14.7–37.9) | 100.0 (92.0–100.0) | 100.0 | 49.4 (45.8–53.1) | Reference |
| CAHP | 0.80 (0.71–0.87) | 5.0 (1.0–13.9) | 100.0 (92.0-100.0) | 100.0 | 43.6 (42.1–45.0) | 0.17 |
| C-GRApH | 0.70 (0.60–0.78) | 0.0 (0.0–6.0) | 100.0 (92.0–100.0) | 42.3 (42.3–42.3) | 0.001 | |
| Brain image and serum NSE | ||||||
| HSI on DWI, 89 * | 0.85 (0.75–0.91) | 69.2 (54.9–81.3) | 100.0 (90.5–100.0) | 100.0 | 69.8 (60.6–77.7) | Reference |
| PV 400 ** of ADC, 89 * | 0.78 (0.68–0.86) | 40.4 (27.0–54.9) | 100.0 (90.5–100.0) | 100.0 | 54.4 (48.8–59.9) | 0.19 |
| GWR of CT, 105 * | 0.75 (0.66–0.83) | 13.3 (5.9–24.6) | 100.0 (92.1–100.0) | 100.0 | 46.4 (43.9–48.9) | 0.09 |
| NSE, 106 * | 0.81 (0.73–0.88) | 47.5 (34.6–60.7) | 100.0 (92.1–100.0) | 100.0 | 58.4 (52.5–64.1) | 0.55 |
| Provability Values | AUROC (95% CI) | Sensitivity (95% CI) | Specificity (95% CI) | PPV | NPV (95% CI) | p-Value for AUROC Comparison |
|---|---|---|---|---|---|---|
| Modified OHCA model, 106 * | 0.89 (0.81–0.94) | 33.3 (21.7–46.7) | 100.0 (92.0–100.0) | 100.0 | 52.4 (47.9–56.8) | Reference |
| Modified OHCA (HSI on DWI), 89 * | 0.96 (0.90–0.99) | 74.5 (60.4–85.7) | 100.0 (90.5–100.0) | 100.0 | 74.0 (64.0–82.0) | 0.01 |
| Modified OHCA (PV 400 of ADC), 89 * | 0.93 (0.85–0.97) | 49.0 (34.8–63.4) | 100.0 (90.5–100.0) | 100.0 | 58.7 (52.1–65.1) | 0.27 |
| Modified OHCA (GWR of CT), 105 * | 0.92 (0.85–0.97) | 35.6 (23.6–49.1) | 100.0 (92.0–100.0) | 100.0 | 53.7 (48.9–58.3) | 0.09 |
| Modified OHCA(NSE), 106 * | 0.92 (0.85–0.96) | 54.4 (40.7–67.6) | 100.0 (91.6–100.0) | 100.0 | 61.8 (54.9–68.2) | 0.05 |
| Modified CAHP model, 106 * | 0.90 (0.82–0.95) | 30.0 (18.8–43.2) | 100.0 (92.0–100.0) | 100.0 | 51.2 (47.0–55.3) | Reference |
| Modified CAHP (HSI on DWI), 89 * | 0.97 (0.91–0.99) | 82.4 (69.1–91.6) | 100.0 (90.5–100.0) | 100.0 | 80.4 (69.4–88.1) | 0.01 |
| Modified CAHP (PV 400 ** of ADC), 89 * | 0.93 (0.86–0.97) | 60.8 (46.1–74.2) | 100.0 (90.5–100.0) | 100.0 | 64.9 (56.8–72.2) | 0.13 |
| Modified CAHP (GWR of CT), 105 * | 0.92 (0.85–0.97) | 18.6 (9.7–30.9) | 100.0 (92.0–100.0) | 100.0 | 47.8 (44.8–50.9) | 0.18 |
| Modified CAHP (NSE), 106 * | 0.91 (0.83–0.96) | 57.9 (44.1–70.9) | 100.0 (91.6–100.0) | 100.0 | 63.6 (56.3–70.4) | 0.64 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Song, H.; Park, J.; You, Y.; Ahn, H.; Yoo, I.; Kim, S.; Lee, J.; Ryu, S.; Jeong, W.; Cho, Y.; et al. Using Out-of-Hospital Cardiac Arrest (OHCA) and Cardiac Arrest Hospital Prognosis (CAHP) Scores with Modified Objective Data to Improve Neurological Prognostic Performance for Out-of-Hospital Cardiac Arrest Survivors. J. Clin. Med. 2021, 10, 1825. https://doi.org/10.3390/jcm10091825
Song H, Park J, You Y, Ahn H, Yoo I, Kim S, Lee J, Ryu S, Jeong W, Cho Y, et al. Using Out-of-Hospital Cardiac Arrest (OHCA) and Cardiac Arrest Hospital Prognosis (CAHP) Scores with Modified Objective Data to Improve Neurological Prognostic Performance for Out-of-Hospital Cardiac Arrest Survivors. Journal of Clinical Medicine. 2021; 10(9):1825. https://doi.org/10.3390/jcm10091825
Chicago/Turabian StyleSong, Hogul, Jungsoo Park, Yeonho You, Hongjoon Ahn, Insool Yoo, Seungwhan Kim, Jinwoong Lee, Seung Ryu, Wonjoon Jeong, Yongchul Cho, and et al. 2021. "Using Out-of-Hospital Cardiac Arrest (OHCA) and Cardiac Arrest Hospital Prognosis (CAHP) Scores with Modified Objective Data to Improve Neurological Prognostic Performance for Out-of-Hospital Cardiac Arrest Survivors" Journal of Clinical Medicine 10, no. 9: 1825. https://doi.org/10.3390/jcm10091825
APA StyleSong, H., Park, J., You, Y., Ahn, H., Yoo, I., Kim, S., Lee, J., Ryu, S., Jeong, W., Cho, Y., & Kang, C. (2021). Using Out-of-Hospital Cardiac Arrest (OHCA) and Cardiac Arrest Hospital Prognosis (CAHP) Scores with Modified Objective Data to Improve Neurological Prognostic Performance for Out-of-Hospital Cardiac Arrest Survivors. Journal of Clinical Medicine, 10(9), 1825. https://doi.org/10.3390/jcm10091825






