Effectiveness and Quality of Implementing a Best Practice Model of Care for Low Back Pain (BetterBack) Compared with Routine Care in Physiotherapy: A Hybrid Type 2 Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants and Setting
2.3. Participants and Setting
2.3.1. Control Group
2.3.2. Intervention Group
- Why: The main PT target behavior was the adoption of the BetterBack☺ MoC to influence delivery of care coherent with best practice clinical guideline recommendations.
- What: This would require the contents of the BetterBack☺ MoC as outlined in Supplementary File S1 to change barrier behaviors such as PTs having low confidence in skills/capabilities for improving LBP patient management and low awareness of evidence based clinical guidelines or coordinated care pathways.
- How: BetterBack☺ MoC content used to overcome the modifiable barriers were support tools including clinical practice guidelines, patient-centered coordinated care pathway, assessment and clinical reasoning tools, patient education brochures and group education material on LBP and self-care, as well as functional restoration program resources.
- When/How much/Tailoring: Intervention delivery, dosing, frequency and progression was stratified based on the PTs’ clinical reasoning regarding risk of pain persistence towards patient’s goals and was delivered at local PT clinics.
- Procedure: A flow diagram for content delivery was provided in the BetterBack☺ MoC. A sustainable multifaceted implementation strategy for PTs use of the BetterBack☺ MoC was composed of the following 3 main facets: (1) Involving an already existing regional implementation steering group including clinic managers who requested an improvement of LBP care and the clinical implementation researchers responsible for overarching logistics; (2) Forming a regional MoC support team comprised of experienced PTs (clinical champions) as local clinic based MoC ambassadors; (3) PT workshops (13.5 h) conducted by the regional support team and steering group at baseline and 3 months (2 h) and a web-based education module for BetterBack☺ MoC users. The behavior change wheel [28] was applied as a theoretical basis for the PT workshops where functions such as education and persuasion about evidence-based recommendations for LBP care as well as training and modelling of the practical use of the BetterBack☺ MoC were used. Detailed information about development and the multifaceted implementation strategy of the BetterBack☺ MoC can be found in the a-priori published protocol [20].
2.4. Patient Reported Outcome Measures (PROMs)
2.4.1. Primary Outcome Measures
2.4.2. Secondary Outcome Measures
2.5. Data Analysis
3. Results
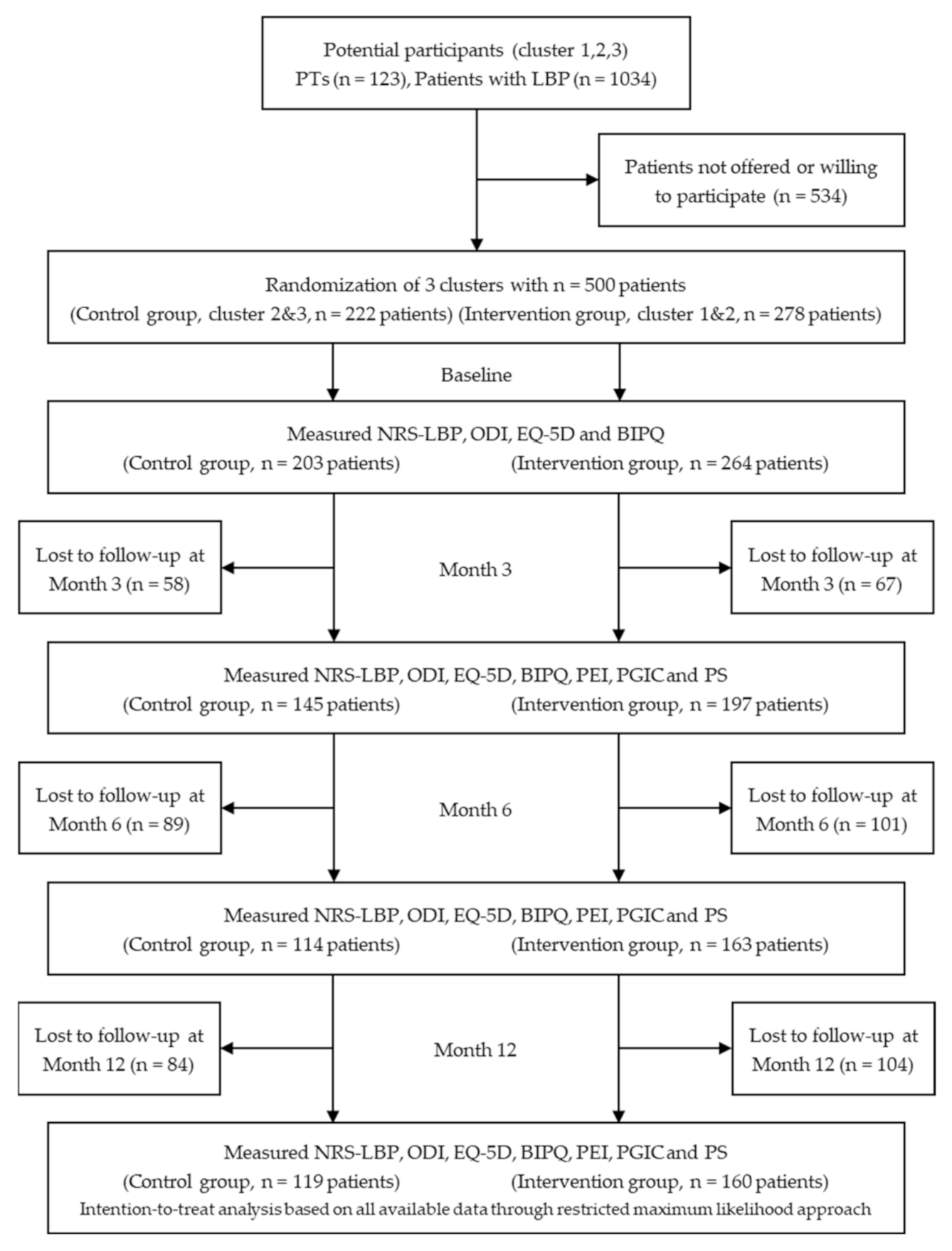
3.1. Participant Flow and Baseline Characteristics
3.2. Minimum Clinically Important Differences in PROMs
3.3. Patient Outcomes Based on Control and Intervention Group within and Between-Group Effects
3.4. Patient Outcomes Based on the Fidelity of CPQI Adherence Regarding PTs’ Care
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jordan, K.P.; Jöud, A.; Bergknut, C.; Croft, P.; Edwards, J.J.; Peat, G.; Petersson, I.F.; Turkiewicz, A.; Wilkie, R.; Englund, M. International comparisons of the consultation prevalence of musculoskeletal conditions using population-based healthcare data from England and Sweden. Ann. Rheum. Dis. 2014, 73, 212–218. [Google Scholar] [CrossRef]
- Ludvigsson, M.L.; Enthoven, P. Evaluation of physiotherapists as primary assessors of patients with musculoskeletal disorders seeking primary health care. Physiotherapy 2012, 98, 131–137. [Google Scholar] [CrossRef]
- Goodwin, R.W.; Hendrick, P.A. Physiotherapy as a first point of contact in general practice: A solution to a growing problem? Prim. Health Care Res. Dev. 2016, 17, 489–502. [Google Scholar] [CrossRef] [PubMed]
- Childs, J.D.; Fritz, J.M.; Wu, S.S.; Flynn, T.W.; Wainner, R.S.; Robertson, E.K.; Kim, F.S.; George, S.Z. Implications of early and guideline adherent physical therapy for low back pain on utilization and costs. BMC Health Serv. Res. 2015, 15, 150. [Google Scholar] [CrossRef]
- Oliveira, C.B.; Maher, C.G.; Pinto, R.Z.; Traeger, A.C.; Lin, C.C.; Chenot, J.F.; van Tulder, M.; Koes, B.W. Clinical practice guidelines for the management of non-specific low back pain in primary care: An updated overview. Eur. Spine J. 2018, 27, 2791–2803. [Google Scholar] [CrossRef] [PubMed]
- O’Connell, N.E.; Cook, C.E.; Wand, B.M.; Ward, S.P. Clinical guidelines for low back pain: A critical review of consensus and inconsistencies across three major guidelines. Best Pract. Res. Clin. Rheumatol. 2016, 30, 968–980. [Google Scholar] [CrossRef] [PubMed]
- Delitto, A.; George, S.Z.; Van Dillen, L.R.; Whitman, J.M.; Sowa, G.; Shekelle, P.; Denninger, T.R.; Godges, J.J. Low back pain. J. Orthopaed. Sports Phys. Ther. 2012, 42, A1–A57. [Google Scholar] [CrossRef]
- Foster, N.E.; Anema, J.R.; Cherkin, D.; Chou, R.; Cohen, S.P.; Gross, D.P.; Ferreira, P.H.; Fritz, J.M.; Koes, B.W.; Peul, W.; et al. Prevention and treatment of low back pain: Evidence, challenges, and promising directions. Lancet 2018, 391, 2368–2383. [Google Scholar] [CrossRef]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What low back pain is and why we need to pay attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef]
- Forsetlund, L.; Bjorndal, A.; Rashidian, A.; Jamtvedt, G.; O’Brien, M.A.; Wolf, F.; Davis, D.; Odgaard-Jensen, J.; Oxman, A.D. Continuing education meetings and workshops: Effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2009. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, M.A.; Rogers, S.; Jamtvedt, G.; Oxman, A.D.; Odgaard-Jensen, J.; Kristoffersen, D.T.; Forsetlund, L.; Bainbridge, D.; Freemantle, N.; Davis, D.A.; et al. Educational outreach visits: Effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2007. [Google Scholar] [CrossRef] [PubMed]
- Mesner, S.A.; Foster, N.E.; French, S.D. Implementation interventions to improve the management of non-specific low back pain: A systematic review. BMC Musculoskelet. Disord. 2016, 17, 258. [Google Scholar] [CrossRef]
- Berube, M.E.; Poitras, S.; Bastien, M.; Laliberte, L.A.; Lacharite, A.; Gross, D.P. Strategies to translate knowledge related to common musculoskeletal conditions into physiotherapy practice: A systematic review. Physiotherapy 2018, 104, 1–8. [Google Scholar] [CrossRef]
- Scott, S.D.; Albrecht, L.; O’Leary, K.; Ball, G.D.; Hartling, L.; Hofmeyer, A.; Jones, C.A.; Klassen, T.P.; Kovacs Burns, K.; Newton, A.S.; et al. Systematic review of knowledge translation strategies in the allied health professions. Implement. Sci. 2012, 7, 70. [Google Scholar] [CrossRef]
- Bekkering, G.E.; van Tulder, M.W.; Hendriks, E.J.; Koopmanschap, M.A.; Knol, D.L.; Bouter, L.M.; Oostendorp, R.A. Implementation of clinical guidelines on physical therapy for patients with low back pain: Randomized trial comparing patient outcomes after a standard and active implementation strategy. Phys. Ther. 2005, 85, 544–555. [Google Scholar] [CrossRef]
- van der Wees, P.J.; Jamtvedt, G.; Rebbeck, T.; de Bie, R.A.; Dekker, J.; Hendriks, E.J. Multifaceted strategies may increase implementation of physiotherapy clinical guidelines: A systematic review. Aust. J. Physiother. 2008, 54, 233–241. [Google Scholar] [CrossRef]
- Stevenson, K.; Lewis, M.; Hay, E. Does physiotherapy management of low back pain change as a result of an evidence-based educational programme? J. Eval. Clin. Pract. 2006, 12, 365–375. [Google Scholar] [CrossRef]
- Suman, A.; Dikkers, M.F.; Schaafsma, F.G.; van Tulder, M.W.; Anema, J.R. Effectiveness of multifaceted implementation strategies for the implementation of back and neck pain guidelines in health care: A systematic review. Implement. Sci. 2016, 11, 126. [Google Scholar] [CrossRef] [PubMed]
- Hanney, W.J.; Masaracchio, M.; Liu, X.; Kolber, M.J. The Influence of Physical Therapy Guideline Adherence on Healthcare Utilization and Costs among Patients with Low Back Pain: A Systematic Review of the Literature. PLoS ONE 2016, 11, e0156799. [Google Scholar] [CrossRef]
- Abbott, A.; Schroder, K.; Enthoven, P.; Nilsen, P.; Oberg, B. Effectiveness of implementing a best practice primary healthcare model for low back pain (BetterBack) compared with current routine care in the Swedish context: An internal pilot study informed protocol for an effectiveness-implementation hybrid type 2 trial. BMJ Open 2018, 8, e019906. [Google Scholar] [CrossRef]
- Schröder, K.; Öberg, B.; Enthoven, P.; Kongsted, A.; Abbott, A. Confidence, attitudes, beliefs and determinants of implementation behaviours among physiotherapists towards clinical management of low back pain before and after implementation of the BetterBack model of care. BMC Health Serv. Res. 2020, 20, 443. [Google Scholar] [CrossRef]
- Hemming, K.; Haines, T.P.; Chilton, P.J.; Girling, A.J.; Lilford, R.J. The stepped wedge cluster randomised trial: Rationale, design, analysis, and reporting. BMJ Clin. Res. 2015, 350, h391. [Google Scholar] [CrossRef]
- Hooper, R.; Bourke, L. The dog-leg: An alternative to a cross-over design for pragmatic clinical trials in relatively stable populations. Int. J. Epidemiol. 2014, 43, 930–936. [Google Scholar] [CrossRef]
- Pinnock, H.; Barwick, M.; Carpenter, C.R.; Eldridge, S.; Grandes, G.; Griffiths, C.J.; Rycroft-Malone, J.; Meissner, P.; Murray, E.; Patel, A.; et al. Standards for Reporting Implementation Studies (StaRI) Statement. BMJ Clin. Res. 2017, 356, i6795. [Google Scholar] [CrossRef]
- National Clinical Guideline Center (NICE). Low Back Pain and Sciatica in over 16s: Assessment and Management. Available online: http://www.nice.org.uk/guidance/gid-cgwave0681/documents (accessed on 24 June 2020).
- Sundhedsstyrelsen. The National Clinical Guideline for Non-Surgical Treatment of Recently Lumbar Nervous System Impact (Lumbar Radiculopathy) Provides Recommendations on Non-Surgical Treatment Options. Available online: http://sundhedsstyrelsen.dk/da/udgivelser/2016/lumbal-nerverodspaavirkning-ikke-kirurgisk-behandling (accessed on 24 June 2020).
- Sundhedsstyrelsen. National Clinical Guidelines for Non-Surgical Treatment of Newly Occurring Lower Back Pain. Available online: http://sundhedsstyrelsen.dk/da/udgivelser/2016/nkr-laenderygsmerer (accessed on 3 May 2016).
- Michie, S.; van Stralen, M.M.; West, R. The behaviour change wheel: A new method for characterising and designing behaviour change interventions. Implement. Sci. 2011, 6, 42. [Google Scholar] [CrossRef]
- Michie, S.; Johnston, M.; Francis, J.; Hardeman, W.; Eccles, M. From theory to intervention: Mapping theoretically derived behavioural determinants to behaviour change techniques. Appl. Psychol. 2008, 57, 660–680. [Google Scholar] [CrossRef]
- Michie, S.; Johnston, M. Changing clinical behaviour by making guidelines specific. BMJ Clin. Res. 2004, 328, 343–345. [Google Scholar] [CrossRef]
- Briggs, A.M.; Jordan, J.E.; Jennings, M.; Speerin, R.; Chua, J.; Bragge, P.; Slater, H. A Framework to Evaluate Musculoskeletal Models of Care. Cornwall: Global Alliance for Musculoskeletal Health of the Bone and Joint Decade. Available online: https://www.aci.health.nsw.gov.au/__data/assets/pdf_file/0020/338141/Framework-to-Evaluate-Musculoskeletal-MoC.pdf (accessed on 24 June 2020).
- Leventhal, H.; Phillips, L.A.; Burns, E. The Common-Sense Model of Self-Regulation (CSM): A dynamic framework for understanding illness self-management. J. Behav. Med. 2016, 39, 935–946. [Google Scholar] [CrossRef]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ Clin. Res. 2014, 348, g1687. [Google Scholar] [CrossRef]
- Jensen, M.P.; Turner, J.A.; Romano, J.M.; Fisher, L.D. Comparative reliability and validity of chronic pain intensity measures. Pain 1999, 83, 157–162. [Google Scholar] [CrossRef]
- Fairbank, J.C.; Pynsent, P.B. The Oswestry Disability Index. Spine 2000, 25, 2940–2952, discussion 2952. [Google Scholar] [CrossRef] [PubMed]
- Goldsmith, E.S.; Taylor, B.C.; Greer, N.; Murdoch, M.; MacDonald, R.; McKenzie, L.; Rosebush, C.E.; Wilt, T.J. Focused Evidence Review: Psychometric Properties of Patient-Reported Outcome Measures for Chronic Musculoskeletal Pain. J. Gen. Intern. Med. 2018, 33, 61–70. [Google Scholar] [CrossRef]
- Chapman, J.R.; Norvell, D.C.; Hermsmeyer, J.T.; Bransford, R.J.; DeVine, J.; McGirt, M.J.; Lee, M.J. Evaluating common outcomes for measuring treatment success for chronic low back pain. Spine 2011, 36, S54–S68. [Google Scholar] [CrossRef]
- The EuroQol Group. EuroQol—A new facility for the measurement of health-related quality of life. Health Policy 1990, 16, 199–208. [Google Scholar] [CrossRef]
- Broadbent, E.; Petrie, K.J.; Main, J.; Weinman, J. The brief illness perception questionnaire. J. Psychosom. Res. 2006, 60, 631–637. [Google Scholar] [CrossRef]
- Roost, M.; Zielinski, A.; Petersson, C.; Strandberg, E.L. Reliability and applicability of the Patient Enablement Instrument (PEI) in a Swedish general practice setting. BMC Fam. Pract. 2015, 16, 31. [Google Scholar] [CrossRef][Green Version]
- Kamper, S.J.; Maher, C.G.; Mackay, G. Global rating of change scales: A review of strengths and weaknesses and considerations for design. J. Man. Manip. Ther. 2009, 17, 163–170. [Google Scholar] [CrossRef]
- Butler, R.J.; Johnson, W.G. Satisfaction with low back pain care. Spine J. Off. J. N. Am. Spine Soc. 2008, 8, 510–521. [Google Scholar] [CrossRef]
- Cieza, A.; Stucki, G.; Weigl, M.; Disler, P.; Jackel, W.; van der Linden, S.; Kostanjsek, N.; de Bie, R. ICF Core Sets for low back pain. J. Rehab. Med. 2004, 69–74. [Google Scholar] [CrossRef]
- Revicki, D.; Hays, R.D.; Cella, D.; Sloan, J. Recommended methods for determining responsiveness and minimally important differences for patient-reported outcomes. J. Clin. Epidemiol. 2008, 61, 102–109. [Google Scholar] [CrossRef]
- van der Roer, N.; Ostelo, R.W.; Bekkering, G.E.; van Tulder, M.W.; de Vet, H.C. Minimal clinically important change for pain intensity, functional status, and general health status in patients with nonspecific low back pain. Spine 2006, 31, 578–582. [Google Scholar] [CrossRef]
- Soer, R.; Reneman, M.F.; Vroomen, P.C.; Stegeman, P.; Coppes, M.H. Responsiveness and minimal clinically important change of the Pain Disability Index in patients with chronic back pain. Spine 2012, 37, 711–715. [Google Scholar] [CrossRef]
- Hosmer, D.W.; Lemeshow, S. Applied Logistic Regression, 2nd ed.; John Wiley and Sons: New York, NY, USA, 2000; pp. 160–164. [Google Scholar]
- Fox-Wasylyshyn, S.M.; El-Masri, M.M. Handling missing data in self-report measures. Res. Nurs. Health 2005, 28, 488–495. [Google Scholar] [CrossRef]
- Enthoven, P.; Eddeborn, F.; Abbott, A.; Schröder, K.; Fors, M.; Öberg, B. Patients’ experiences of the BetterBack model of care for low back pain in primary care—A qualitative interview study. Int. J. Qual. Stud. Health Well Being 2021, 16, 1861719. [Google Scholar] [CrossRef]
- Bamm, E.L.; Rosenbaum, P.; Wilkins, S. Is Health Related Quality of Life of people living with chronic conditions related to patient satisfaction with care? Disab. Rehab. 2013, 35, 766–774. [Google Scholar] [CrossRef]
- Al Zoubi, F.M.; Menon, A.; Mayo, N.E.; Bussières, A.E. The effectiveness of interventions designed to increase the uptake of clinical practice guidelines and best practices among musculoskeletal professionals: A systematic review. BMC Health Serv. Res. 2018, 18, 435. [Google Scholar] [CrossRef]
- Beneciuk, J.M.; George, S.Z. Pragmatic Implementation of a Stratified Primary Care Model for Low Back Pain Management in Outpatient Physical Therapy Settings: Two-Phase, Sequential Preliminary Study. Phys. Ther. 2015, 95, 1120–1134. [Google Scholar] [CrossRef] [PubMed]
- Cherkin, D.; Balderson, B.; Wellman, R.; Hsu, C.; Sherman, K.J.; Evers, S.C.; Hawkes, R.; Cook, A.; Levine, M.D.; Piekara, D.; et al. Effect of Low Back Pain Risk-Stratification Strategy on Patient Outcomes and Care Processes: The MATCH Randomized Trial in Primary Care. J. Gen. Intern. Med. 2018, 33, 1324–1336. [Google Scholar] [CrossRef] [PubMed]
- Masterson-Algar, P.; Burton, C.R.; Rycroft-Malone, J.; Sackley, C.M.; Walker, M.F. Towards a programme theory for fidelity in the evaluation of complex interventions. J. Eval. Clin. Pract. 2014, 20, 445–452. [Google Scholar] [CrossRef]
- Rycroft-Malone, J. It’s more complicated than that Comment on “Translating evidence into healthcare policy and practice: Single versus multi-faceted implementation strategies—Is there a simple answer to a complex question?”. Int. J. Health Policy Manag. 2015, 4, 481–482. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hoeijenbos, M.; Bekkering, T.; Lamers, L.; Hendriks, E.; van Tulder, M.; Koopmanschap, M. Cost-effectiveness of an active implementation strategy for the Dutch physiotherapy guideline for low back pain. Health Policy 2005, 75, 85–98. [Google Scholar] [CrossRef]
- Shenoy, S. Cluster Randomized Controlled Trial to Evaluate the Effectiveness of a Multifaceted Active Strategy to Implement Low Back Pain Practice Guidelines: Effect on Competence, Process of Care and Patient Outcome in Physical Therapy. Ph.D. Thesis, University of Pittsburgh, Pittsburgh, PA, USA, 1 July 2013. [Google Scholar]
- Foster, N.E. Barriers and progress in the treatment of low back pain. BMC Med. 2011, 9, 108. [Google Scholar] [CrossRef]
- Evans, D.W.; Breen, A.C.; Pincus, T.; Sim, J.; Underwood, M.; Vogel, S.; Foster, N.E. The effectiveness of a posted information package on the beliefs and behavior of musculoskeletal practitioners: The UK Chiropractors, Osteopaths, and Musculoskeletal Physiotherapists Low Back Pain ManagemENT (COMPLeMENT) randomized trial. Spine 2010, 35, 858–866. [Google Scholar] [CrossRef]
- Bekkering, G.E.; Hendriks, H.J.; van Tulder, M.W.; Knol, D.L.; Hoeijenbos, M.; Oostendorp, R.A.; Bouter, L.M. Effect on the process of care of an active strategy to implement clinical guidelines on physiotherapy for low back pain: A cluster randomised controlled trial. Qual. Saf. Health Care 2005, 14, 107–112. [Google Scholar] [CrossRef]
- Fritz, J.M.; Cleland, J.A.; Speckman, M.; Brennan, G.P.; Hunter, S.J. Physical therapy for acute low back pain: Associations with subsequent healthcare costs. Spine 2008, 33, 1800–1805. [Google Scholar] [CrossRef]
- Ostelo, R.W.; Deyo, R.A.; Stratford, P.; Waddell, G.; Croft, P.; Von Korff, M.; Bouter, L.M.; de Vet, H.C. Interpreting change scores for pain and functional status in low back pain: Towards international consensus regarding minimal important change. Spine 2008, 33, 90–94. [Google Scholar] [CrossRef]
- Hurwitz, E.L.; Morgenstern, H.; Yu, F. Satisfaction as a predictor of clinical outcomes among chiropractic and medical patients enrolled in the UCLA low back pain study. Spine 2005, 30, 2121–2128. [Google Scholar] [CrossRef] [PubMed]
- Meucci, R.D.; Fassa, A.G.; Faria, N.M. Prevalence of chronic low back pain: Systematic review. Rev. Saude Publica 2015, 49, 1. [Google Scholar] [CrossRef]
- Öberg, B.; Enthoven, P.; Kjellman, G.; Skargren, E. Back pain in primary care: A prospective cohort study of clinical outcome and healthcare consumption. Adv. Physiother. 2003, 5, 98–108. [Google Scholar] [CrossRef]
- Boissoneault, J.; Mundt, J.; Robinson, M.; George, S.Z. Predicting Low Back Pain Outcomes: Suggestions for Future Directions. J. Orthopaed. Sports Phys. Ther. 2017, 47, 588–592. [Google Scholar] [CrossRef]
- Fritz, J.M.; Magel, J.S.; McFadden, M.; Asche, C.; Thackeray, A.; Meier, W.; Brennan, G. Early Physical Therapy vs Usual Care in Patients with Recent-Onset Low Back Pain: A Randomized Clinical Trial. JAMA 2015, 314, 1459–1467. [Google Scholar] [CrossRef]
- Bier, J.D.; Sandee-Geurts, J.J.W.; Ostelo, R.; Koes, B.W.; Verhagen, A.P. Can Primary Care for Back and/or Neck Pain in the Netherlands Benefit from Stratification for Risk Groups According to the STarT Back Tool Classification? Arch. Phys. Med. Rehab. 2018, 99, 65–71. [Google Scholar] [CrossRef]
- Enthoven, P.; Skargren, E.; Oberg, B. Clinical course in patients seeking primary care for back or neck pain: A prospective 5-year follow-up of outcome and health care consumption with subgroup analysis. Spine 2004, 29, 2458–2465. [Google Scholar] [CrossRef] [PubMed]
- Folkhälsomyndigheten. Open Comparisons Public Health. Available online: https://www.folkhalsomyndigheten.se/publicerat-material/publikationsarkiv/oe/oppna-jamforelser-folkhalsa-2019/ (accessed on 24 June 2020).
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D.; et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ Clin. Res. 2015, 350, h1258. [Google Scholar] [CrossRef]
| Clinical Practice Quality Indices Forming the Clinical Practice Quality Index | |
|---|---|
| Assessment quality index | 1. No referral to specialist consultation (pain clinic, orthopedic or neurosurgical care) during the physiotherapy treatment period |
| 2. No imaging during the physiotherapy treatment period | |
| Treatment quality index | 1. Use of patient education interventions |
| 2. Use of exercise interventions | |
| 3. No use of non-evidence-based interventions | |
| Clinical practice quality index | All 5 quality indices fulfilled |
| Control Group (n = 203) | Intervention Group (n = 264) | |
|---|---|---|
| Age, mean ± SD | 46 ± 12 | 45 ± 12 |
| Sex, female, n (%) | 109 (54) | 152 (58) |
| Educational level, n (%) | ||
| Elementary | 24 (12) | 34 (13) |
| High school | 112 (55) | 158 (60) |
| University | 66 (33) | 71 (27) |
| Pain Duration, n (%) | ||
| <12 weeks | 111 (57) | 138 (55) |
| >12 weeks | 83 (43) | 115 (46) |
| Employed, n (%) | 164 (81) | 217 (82) |
| Sick leave due to back pain, n (%) | 34 (18) | 48 (19) |
| STB risk groups, n (%) | ||
| Low risk group | 75 (37) | 97 (37) |
| Medium risk group High risk group | 102 (50) 26 (13) | 132 (50) 35 (13) |
| Number of PT treatment sessions, mean ± SD, n | 3.1 ± 2.7, n = 165 | 4.6 ± 3.8, n = 223 |
| Duration PT intervention period, mean days ± SD, n | 59 ± 84, n = 164 | 63 ± 61, n = 218 |
| PROMs | Correlation with PGIC | Change from Baseline, Mean ± SD | MCID, OCP | Youden Index | (Sensitivity; Specificity) | AUC |
|---|---|---|---|---|---|---|
| 3 months | ||||||
| ODI (n = 337) | 0.45 | 8.7 ± 15.1 | 4.5 | 0.52 | (0.69; 0.83) | 0.81 |
| NRS-LPB (n = 337) | 0.39 | 2.7 ± 2.9 | 2.5 | 0.41 | (0.58; 0.82) | 0.76 |
| EQ-5D (n = 320) | 0.36 | 0.12 ± 0.32 | 0.02 | 0.39 | (0.66; 0.73) | 0.74 |
| BIPQ (n = 339) | 0.52 | 8.6 ± 16.1 | 0.5 † | 0.56 | (0.81; 0.75) | 0.87 |
| PEI * (n = 335) | 0.50 | 4.4 ± 4.0 | 2.5 | 0.59 | (0.76; 0.83) | 0.86 |
| 6 months | ||||||
| ODI (n = 270) | 0.40 | 10.4 ± 16.6 | 4.5 | 0.44 | (0.68; 0.76) | 0.78 |
| NRS-LPB (n = 270) | 0.30 | 2.6 ± 2.9 | 2.5 | 0.35 | (0.59; 0.76) | 0.70 |
| EQ-5D (n = 259) | 0.21 | 0.18 ± 0.31 | 0.03 | 0.27 | (0.71; 0.56) | 0.67 |
| BIPQ (n = 273) | 0.37 | 9.4 ± 16.0 | 8.5 | 0.40 | (0.58; 0.82) | 0.74 |
| PEI * (n = 265) | 0.48 | 4.6 ± 4.2 | 3.5 | 0.55 | (0.67; 0.88) | 0.82 |
| 12 months | ||||||
| ODI (n = 270) | 0.35 | 11.9 ± 15.6 | 8.5 | 0.38 | (0.59; 0.79) | 0.75 |
| NRS-LPB (n = 273) | 0.32 | 2.9 ± 2.8 | 1.5 | 0.35 | (0.77; 0.58) | 0.72 |
| EQ-5D (n = 264) | 0.31 | 0.18 ± 0.32 | 0.18 | 0.30 | (0.49; 0.81) | 0.70 |
| BIPQ (n = 271) | 0.47 | 10.8 ± 16.0 | 12.5 | 0.49 | (0.53; 0.98) | 0.82 |
| PEI * (n = 261) | 0.47 | 4.9 ± 4.2 | 2.5 | 0.53 | (0.76; 0.78) | 0.82 |
| Within-Group Analysis of Change from Baseline | Between-Group Effects (1–2) at Each Endpoint | |||
|---|---|---|---|---|
| 1. Control Group (n = 203) | 2. Intervention Group (n = 264) | |||
| Mean (95% CI) p-Value | Mean (95% CI) p-Value | Mean (95% CI) p-Value | ICC | |
| ODI (0–100) | 31.6 (27.2 to 36.1) * | 30.4 (25.6 to 35.3) * | ||
| 3 months | −10.5 (−13.4 to −7.6) p < 0.001 | −8.7 (−11.2 to −6.2) p < 0.001 | −1.8 (−5.0 to 1.3) p = 0.248 | 0.012 |
| 6 months | −10.9 (−14.1 to −7.7) p < 0.001 | −10.2 (−12.9 to −7.5) p < 0.001 | −0.7 (−4.2 to 2.7) p = 0.674 | |
| 12 months | −14.2 (−17.3 to −11.1) p < 0.001 | −11.3 (−13.9 to −8.6) p < 0.001 | −3.0 (−6.3 to 0.4) p = 0.081 | |
| NRS-LBP (0–10) | 6.1 (5.6 to 6.7) * | 6.4 (5.7 to 7.0) * | ||
| 3 months | −2.6 (−3.1 to −2.1) p < 0.001 | −2.9 (−3.4 to −2.5) p < 0.001 | −0.3 (−0.3 to 0.9) p = 0.263 | 0.008 |
| 6 months | −2.4 (−3.0 to −1.8) p < 0.001 | −2.7 (−3.2 to −2.2) p < 0.001 | −0.3 (−0.3 to 0.9) p = 0.357 | |
| 12 months | −3.1 (−3.7 to −2.5) p < 0.001 | −2.8 (−3.3 to −2.3) p < 0.001 | −0.3 (−0.9 to 0.3) p = 0.297 | |
| EQ-5D index (−0.59–1) | 0.55 (0.50 to 0.60) * | 0.52 (0.46 to 0.58) * | ||
| 3 months | 0.12 (0.06 to 0.18) p < 0.001 | 0.15 (0.10 to 0.21) p < 0.001 | −0.03 (−0.10 to 0.04) p = 0.381 | 0.004 |
| 6 months | 0.13 (0.07 to 0.19) p < 0.001 | 0.20 (0.15 to 0.25) p < 0.001 | −0.07 (−0.14 to −0.01) p = 0.034 | |
| 12 months | 0.19 (0.13 to 0.25) p < 0.001 | 0.20 (0.14 to 0.25) p < 0.001 | −0.01 (−0.07 to 0.06) p = 0.838 | |
| BIPQ total score (0–80) | 44.6 (40.4 to 48.8) * | 45.4 (40.7 to 50.2) * | ||
| 3 months | −8.2 (−11.4 to −5.1) p < 0.001 | −9.0 (−11.6 to −6.3) p < 0.001 | −0.8 (−2.6 to 4.1) p = 0.659 | 0.007 |
| 6 months | −9.1 (−12.5 to −5.8) p < 0.001 | −8.8 (−11.6 to −6.0) p < 0.001 | −0.2 (−3.9 to 3.2) p = 0.853 | |
| 12 months | −11.7 (−15.0 to −8.4)p < 0.001 | −10.4 (−13.2 to −7.5) p < 0.001 | −1.3 (−4.9 to 2.2) p = 0.457 | |
| PEI (0–12) | Transition score, mean ± SE | Transition score, mean ± SE | ||
| 3 months | 4.4 ± 0.3 | 4.5 ± 0.3 | −0.1 (−1.0 to 0.7) p = 0.768 | < 0.001 |
| 6 months | 4.2 ± 0.4 | 4.8 ± 0.3 | −0.6 (−0.4 to 1.6) p = 0.257 | |
| 12 months | 5.1 ± 0.4 | 4.9 ± 0.3 | 0.2 (−1.2 to 0.9) p = 0.742 | |
| 1. Control Group, n/N (%) | 2. Intervention Group, n/N (%) | Between-Group Comparison (2/1), OR (95% CI), p-Value, ICC | |
|---|---|---|---|
| Patient satisfaction | |||
| Satisfied after 3 months | 93/144 (64.6) | 149/197 (75.6) | 1.7 (1.5 to 1.9), p < 0.001, ICC = 0.006 |
| Satisfied after 6 months | 68/111 (61.3) | 109/163 (66.9) | 1.3 (1.0 to 1.6), p = 0.027, ICC = 0.002 |
| Satisfied after 12 months | 73/116 (62.9) | 98/158 (62.0) | 0.9 (0.5 to 1.6), p = 0.748, ICC < 0.001 |
| Patient global rating of change | |||
| Improved after 3 months | 105/144 (72.9) | 149/197 (75.6) | 1.2 (0.7 to 1.9), p = 0.570, ICC < 0.001 |
| Improved in after 6 months | 74/111 (66.7) | 126/163 (77.3) | 1.7 (1.0 to 2.9), p = 0.054, ICC < 0.001 |
| Improvement after 12 months | 86/118 (72.9) | 121/158 (76.6) | 1.6 (0.7 to 3.9), p = 0.290, ICC = 0.035 |
| Within-Group Analysis of Change from Baseline | Between-Group Effects (1–2) at Each Endpoint | |||
|---|---|---|---|---|
| 1. Non CPQI Adherent Care Group (n = 191) | 2. CPQI Adherent Care Group (n = 164) | |||
| Mean (95% CI) p-Value | Mean (95% CI) p-Value | Mean (95% CI) p-Value | ICC | |
| ODI (0–100) | 32.4 (27.5 to 37.3) * | 28.3 (23.5 to 33.2) * | ||
| 3 months | −9.0 (−11.8 to −6.2) p < 0.001 | −11.3 (−14.2 to −8.3) p < 0.001 | 2.3 (−1.1 to 5.6) p = 0.178 | 0.012 |
| 6 months | −8.9 (−12.1 to −6.0) p < 0.001 | −12.7 (−16.1 to −9.4) p < 0.001 | 3.8 (0.3 to 7.6) p = 0.048 | |
| 12 months | −10.7 (−13.9 to −7.6) p < 0.001 | −13.2 (−16.5 to −9.8) p < 0.001 | 2.4 (−1.4 to 6.2) p = 0.207 | |
| NRS-LBP (0–10) | 6.3 (5.5 to 7.1) * | 6.1 (5.4 to 6.9) * | ||
| 3 months | −2.5 (−3.0 to −2.0) p < 0.001 | −3.4 (−4.0 to −2.8) p < 0.001 | 0.9 (0.3 to 1.6) p = 0.004 | 0.008 |
| 6 months | −2.1 (−2.7 to −1.5) p < 0.001 | −3.2 (−3.8 to −2.6) p < 0.001 | 1.1 (0.4 to 1.8) p = 0.002 | |
| 12 months | −2.6 (−3.2 to −2.0) p < 0.001 | −3.1 (−3.7 to −2.5) p < 0.001 | 0.5 (−0.2 to 1.2) p = 0.169 | |
| EQ-5D index (−0.59–1) | 0.51 (0.45 to 0.57) * | 0.59 (0.52 to 0.65) * | ||
| 3 months | 0.12 (0.05 to 0.18) p < 0.001 | 0.15 (0.09 to 0.22) p < 0.001 | −0.03 (−0.11 to 0.03) p = 0.294 | 0.004 |
| 6 months | 0.14 (0.08 to 0.20) p < 0.001 | 0.19 (0.13 to 0.26) p < 0.001 | −0.05 (−0.12 to 0.02) p = 0.161 | |
| 12 months | 0.19 (0.13 to 0.25) p < 0.001 | 0.19 (0.12 to 0.25) p < 0.001 | 0.00 (−0.07 to 0.07) p = 0.985 | |
| BIPQ total score (0–80) | 46.0 (43.2 to 48.8) * | 43.9 (41.0 to 46.9) * | ||
| 3 months | −7.1 (−10.1 to −4.1) p < 0.001 | −12.2 (−15.4 to −9.0) p < 0.001 | 5.1 (1.5 to 8.6) p = 0.006 | 0.007 |
| 6 months | −6.9 (−10.1 to −3.6) p < 0.001 | −12.8 (−16.2 to −9.4) p < 0.001 | 6.0 (2.1 to 9.8) p = 0.002 | |
| 12 months | −9.3 (−12.7 to 5.9) p < 0.001 | −13.2 (−16.7 to −9.6) p < 0.001 | 3.8 (−0.2 to 7.8) p = 0.060 | |
| PEI (0–12) | Transition score, mean ± SE | Transition score, mean ± SE | ||
| 3 months | 4.1 ± 0.3 | 5.4 ± 0.3 | −1.4 (−2.3 to −0.4) p = 0.005 | < 0.001 |
| 6 months | 4.1 ± 0.4 | 5.6 ± 0.4 | −1.6 (−2.7 to −0.4) p = 0.007 | |
| 12 months | 4.3 ± 0.5 | 5.9 ± 0.5 | −1.6 (−2.7 to −0.4) p = 0.008 | |
| 1. Non CPQI Adherent Care Group n/N (%) | 2. CPQI Adherent Care Group n/N (%) | Between-Group Comparison (2/1), OR (95% CI), p-Value, ICC | |
|---|---|---|---|
| Patient satisfaction | |||
| Satisfied after 3 months | 90/138 (65.2) | 101/125 (80.8) | 2.2 (1.3 to 4.0), p = 0.006, ICC = 0.006 |
| Satisfied after 6 months | 62/110 (56.4) | 80/103 (77.7) | 2.7 (1.5 to 6.4), p = 0.001, ICC = 0.002 |
| Satisfied after 12 months | 58/104 (55.8) | 71/102 (69.6) | 1.2 (1.0 to 3.2), p = 0.042, ICC < 0.001 |
| Patient global rating of change | |||
| Improved after 3 months | 98/138 (71.0) | 106/125 (84.8) | 2.3 (1.2 to 4.2), p = 0.009, ICC < 0.001 |
| Improved after 6 months | 74/110 (67.3) | 84/104 (80.8) | 2.0 (1.1 to 3.9), p = 0.027, ICC < 0.001 |
| Improved after 12 months | 75/106 (70.8) | 79/102 (77.5) | 1.5 (0.8 to 2.8), p = 0.206, ICC = 0.035 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schröder, K.; Öberg, B.; Enthoven, P.; Hedevik, H.; Fors, M.; Abbott, A. Effectiveness and Quality of Implementing a Best Practice Model of Care for Low Back Pain (BetterBack) Compared with Routine Care in Physiotherapy: A Hybrid Type 2 Trial. J. Clin. Med. 2021, 10, 1230. https://doi.org/10.3390/jcm10061230
Schröder K, Öberg B, Enthoven P, Hedevik H, Fors M, Abbott A. Effectiveness and Quality of Implementing a Best Practice Model of Care for Low Back Pain (BetterBack) Compared with Routine Care in Physiotherapy: A Hybrid Type 2 Trial. Journal of Clinical Medicine. 2021; 10(6):1230. https://doi.org/10.3390/jcm10061230
Chicago/Turabian StyleSchröder, Karin, Birgitta Öberg, Paul Enthoven, Henrik Hedevik, Maria Fors, and Allan Abbott. 2021. "Effectiveness and Quality of Implementing a Best Practice Model of Care for Low Back Pain (BetterBack) Compared with Routine Care in Physiotherapy: A Hybrid Type 2 Trial" Journal of Clinical Medicine 10, no. 6: 1230. https://doi.org/10.3390/jcm10061230
APA StyleSchröder, K., Öberg, B., Enthoven, P., Hedevik, H., Fors, M., & Abbott, A. (2021). Effectiveness and Quality of Implementing a Best Practice Model of Care for Low Back Pain (BetterBack) Compared with Routine Care in Physiotherapy: A Hybrid Type 2 Trial. Journal of Clinical Medicine, 10(6), 1230. https://doi.org/10.3390/jcm10061230








