A Phase Ib Study of Durvalumab (MEDI4736) in Combination with Carbon-Ion Radiotherapy and Weekly Cisplatin for Patients with Locally Advanced Cervical Cancer (DECISION Study): The Early Safety and Efficacy Results
Abstract
:1. Introduction
2. Results
2.1. Patient Population
2.2. Treatment Feasibility and Adverse Events
3. Discussion
4. Materials and Methods
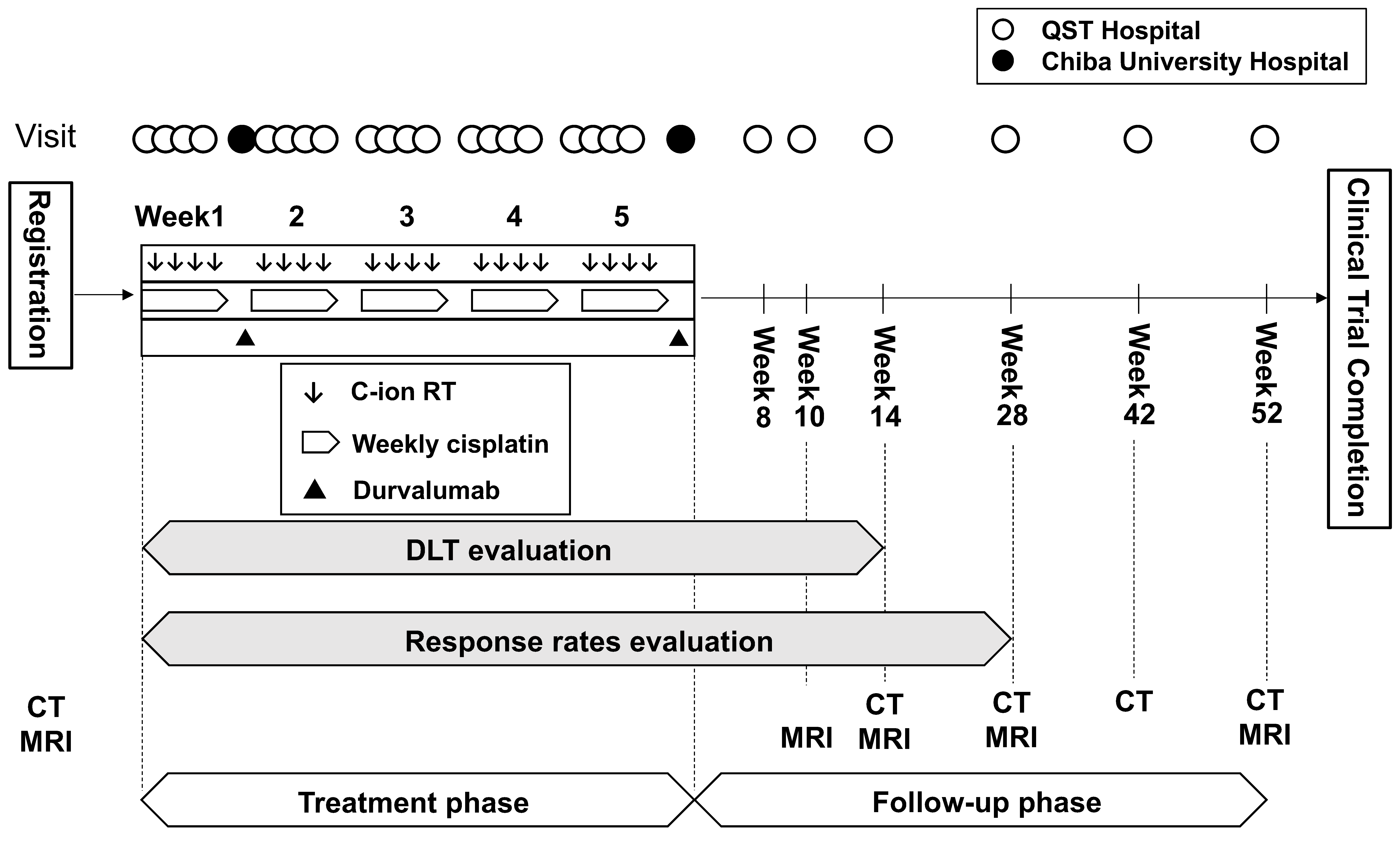
4.1. Overview of Study Design
4.2. Protocol Treatment
4.3. Patient Eligibility
4.4. Endpoints
4.5. Evaluation Methods
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- NCCN Guidelines Ver 1. Cervical Cancer. Available online: https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf (accessed on 21 March 2023).
- Green, J.A.; Kirwan, J.M.; Tierney, J.F.; Symonds, P.; Fresco, L.; Collingwood, M.; Williams, C.J. Survival and recurrence after concomitant chemotherapy and radiotherapy for cancer of the uterine cervix: A systematic review and meta-analysis. Lancet. 2001, 358, 781–786. [Google Scholar] [CrossRef] [PubMed]
- Vale, C.; Tierney, J.; Stewart, L. Concomitant chemoradiotherapy for cervical cancer: A systematic review and meta-analysis of individual patient data. Gynecol. Oncol. 2006, 10, 442–443. [Google Scholar] [CrossRef] [PubMed]
- Chemoradiotherapy for Cervical Cancer Meta-Analysis Collaboration. Reducing uncertainties about the effects of chemoradiotherapy for cervical cancer: A systematic review and meta-analysis of individual patient data from 18 randomized trials. J. Clin. Oncol. 2008, 26, 5802–5812. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haie-Meder, C.; Pötter, R.; Van Limbergen, E.; Briot, E.; De Brabandere, M.; Dimopoulos, J.; Dumas, I.; Hellebust, T.P.; Kirisits, C.; Lang, S.; et al. Recommendations from Gynaecological (GYN) GEC-ESTRO working group (I): Concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother. Oncol. 2005, 74, 235–245. [Google Scholar] [CrossRef] [PubMed]
- Pötter, R.; Haie-Meder, C.; Van Limbergen, E.; Barillot, I.; De Brabandere, M.; Dimopoulos, J.; Dumas, I.; Erickson, B.; Lang, S.; Nulens, A.; et al. Recommendations from gynaecological (GYN) GEC ESTRO working group (II): Concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy-3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother. Oncol. 2006, 78, 67–77. [Google Scholar] [CrossRef]
- Pötter, R.; Tanderup, K.; Schmid, M.P.; Jürgenliemk-Schulz, I.; Haie-Meder, C.; Fokdal, L.U.; Sturdza, A.E.; Hoskin, P.; Mahantshetty, U.; Segedin, B.; et al. MRI-guided adaptive brachytherapy in locally advanced cervical cancer (EMBRACE-I): A multicentre prospective cohort study. Lancet Oncol. 2021, 22, 538–547. [Google Scholar] [CrossRef]
- Minkoff, D.; Gill, B.S.; Kang, J.; Beriwal, S. Cervical cancer outcome prediction to high-dose rate brachytherapy using quantitative magnetic resonance imaging analysis of tumor response to external beam radiotherapy. Radiother. Oncol. 2015, 115, 78–83. [Google Scholar] [CrossRef]
- Kusada, T.; Toita, T.; Ariga, T.; Maemoto, H.; Hashimoto, S.; Shiina, H.; Kakinohana, Y.; Heianna, J.; Nagai, Y.; Kudaka, W.; et al. Computed tomography-based image-guided brachytherapy for cervical cancer: Correlations between dose-volume parameters and clinical outcomes. J. Radiat. Res. 2018, 59, 67–76. [Google Scholar] [CrossRef] [Green Version]
- Yokoi, E.; Mabuchi, S.; Takahashi, R.; Matsumoto, Y.; Kuroda, H.; Kozasa, K.; Kimura, T. Impact of histological subtype on survival in patients with locally advanced cervical cancer that were treated with definitive radiotherapy: Adenocarcinoma/adenosquamous carcinoma versus squamous cell carcinoma. J. Gynecol. Oncol. 2017, 28, e19. [Google Scholar] [CrossRef] [Green Version]
- Kamada, T.; Tsujii, H.; Blakely, E.A.; Debus, J.; De Neve, W.; Durante, M.; Jäkel, O.; Mayer, R.; Orecchia, R.; Pötter, R.; et al. Carbon ion radiotherapy in Japan: An assessment of 20 years of clinical experience. Lancet Oncol. 2015, 16, e93–e100. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okonogi, N.; Wakatsuki, M.; Kato, S.; Shiba, S.; Kobayashi, D.; Kiyohara, H.; Karasawa, K.; Ohno, T.; Nakano, T.; Kamada, T.; et al. Long-term outcomes of carbon-ion radiotherapy for locally advanced squamous cell carcinoma of the uterine cervix. Anticancer Res. 2018, 38, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Wakatsuki, M.; Kato, S.; Ohno, T.; Karasawa, K.; Kiyohara, H.; Tamaki, T.; Ando, K.; Tsujii, H.; Nakano, T.; Kamada, T.; et al. Clinical outcomes of carbon ion radiotherapy for locally advanced adenocarcinoma of the uterine cervix in phase 1/2 clinical trial (protocol 9704). Cancer 2014, 120, 1663–1669. [Google Scholar] [CrossRef]
- Okonogi, N.; Wakatsuki, M.; Kato, S.; Karasawa, K.; Kiyohara, H.; Shiba, S.; Kobayashi, D.; Nakano, T.; Kamada, T.; Shozu, M.; et al. Clinical outcomes of carbon ion radiotherapy with concurrent chemotherapy for locally advanced uterine cervical adenocarcinoma in a phase 1/2 clinical trial (Protocol 1001). Cancer Med. 2018, 7, 351–359. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Okonogi, N.; Wakatsuki, M.; Kato, S.; Murata, H.; Kiyohara, H.; Karasawa, K.; Ohno, T.; Tsuji, H.; Nakano, T.; Shozu, M.; et al. Significance of concurrent use of weekly cisplatin in carbon-ion radiotherapy for locally advanced adenocarcinoma of the uterine cervix: A propensity score-matched analysis. Cancer Med. 2020, 9, 1400–1408. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wang, L.; Wang, X.; Zhang, Q.; Ran, J.; Geng, Y.; Feng, S.; Li, C.; Zhao, X. Is there a role for carbon therapy in the treatment of gynecological carcinomas? A systematic review. Future Oncol. 2019, 15, 3081–3095. [Google Scholar] [CrossRef] [PubMed]
- Keir, M.E.; Butte, M.J.; Freeman, G.J.; Sharpe, A.H. PD-1 and its ligands in tolerance and immunity. Annu. Rev. Immunol. 2008, 26, 677–704. [Google Scholar] [CrossRef] [Green Version]
- Okazaki, T.; Honjo, T. PD-1 and PD-1 ligands: From discovery to clinical application. Int. Immunol. 2007, 19, 813–824. [Google Scholar] [CrossRef] [Green Version]
- Antonia, S.J.; Villegas, A.; Daniel, D.; Vicente, D.; Murakami, S.; Hui, R.; Yokoi, T.; Chiappori, A.; Lee, K.H.; de Wit, M.; et al. Durvalumab after chemoradiotherapy in stage III non-small-cell lung cancer. N. Engl. J. Med. 2017, 377, 1919–1929. [Google Scholar] [CrossRef] [Green Version]
- Antonia, S.J.; Villegas, A.; Daniel, D.; Vicente, D.; Murakami, S.; Hui, R.; Kurata, T.; Chiappori, A.; Lee, K.H.; de Wit, M.; et al. Overall survival with durvalumab after chemoradiotherapy in stage III NSCLC. N. Engl. J. Med. 2018, 379, 2342–2350. [Google Scholar] [CrossRef]
- Schmid, P.; Adams, S.; Rugo, H.S.; Schneeweiss, A.; Barrios, C.H.; Iwata, H.; Diéras, V.; Hegg, R.; Im, S.A.; Shaw Wright, G.; et al. Atezolizumab and Nab-Paclitaxel in Advanced Triple-Negative Breast Cancer. N. Engl. J. Med. 2018, 379, 2108–2121. [Google Scholar] [CrossRef]
- Finn, R.S.; Qin, S.; Ikeda, M.; Galle, P.R.; Ducreux, M.; Kim, T.Y.; Kudo, M.; Breder, V.; Merle, P.; Kaseb, A.O.; et al. Atezolizumab plus Bevacizumab in Unresectable Hepatocellular Carcinoma. N. Engl. J. Med. 2020, 382, 1894–1905. [Google Scholar] [CrossRef] [PubMed]
- Sato, H.; Okonogi, N.; Nakano, T. Rationale of combination of anti-PD-1/PD-L1 antibody therapy and radiotherapy for cancer treatment. Int. J. Clin. Oncol. 2020, 25, 801–809. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Iijima, M.; Okonogi, N.; Nakajima, N.I.; Morokoshi, Y.; Kanda, H.; Yamada, T.; Kobayashi, Y.; Banno, K.; Wakatsuki, M.; Yamada, S.; et al. Significance of PD-L1 expression in carbon-ion radiotherapy for uterine cervical adeno/adenosquamous carcinoma. J. Gynecol. Oncol. 2020, 31, e19. [Google Scholar] [CrossRef]
- Postow, M.A.; Callahan, M.K.; Barker, C.A.; Yamada, Y.; Yuan, J.; Kitano, S.; Mu, Z.; Rasalan, T.; Adamow, M.; Ritter, E.; et al. Immunologic correlates of the abscopal effect in a patient with melanoma. N. Engl. J. Med. 2012, 366, 925–931. [Google Scholar] [CrossRef] [Green Version]
- Kelly, R.J.; Ajani, J.A.; Kuzdzal, J.; Zander, T.; Van Cutsem, E.; Piessen, G.; Mendez, G.; Feliciano, J.; Motoyama, S.; Lièvre, A.; et al. Adjuvant Nivolumab in Resected Esophageal or Gastroesophageal Junction Cancer. N. Engl. J. Med. 2021, 384, 1191–1203. [Google Scholar] [CrossRef] [PubMed]
- Sato, H.; Niimi, A.; Yasuhara, T.; Permata, T.B.M.; Hagiwara, Y.; Isono, M.; Nuryadi, E.; Sekine, R.; Oike, T.; Kakoti, S.; et al. DNA double-strand break repair pathway regulates PD-L1 expression in cancer cells. Nat. Commun. 2017, 8, 1751. [Google Scholar] [CrossRef] [Green Version]
- Bradley, J.D.; Nishio, M.; Okamoto, I.; Newton, M.D.; Trani, L.; Shire, N.J.; Gu, Y.; Dennis, P.A.; Lee, K.H. PACIFIC-2: Phase 3 study of concurrent durvalumab and platinum-based chemoradiotherapy in patients with unresectable, stage III NSCLC. J. Clin. Oncol. 2019, 37 (Suppl. 15), TPS8573. [Google Scholar] [CrossRef]
- Okonogi, N.; Ando, K.; Murata, K.; Wakatsuki, M.; Noda, S.E.; Irie, D.; Tsuji, H.; Shozu, M.; Ohno, T. Multi-Institutional Retrospective Analysis of Carbon-Ion Radiotherapy for Patients with Locally Advanced Adenocarcinoma of the Uterine Cervix. Cancers 2021, 13, 2713. [Google Scholar] [CrossRef] [PubMed]
- Lhuillier, C.; Rudqvist, N.P.; Elemento, O.; Formenti, S.C.; Demaria, S. Radiation therapy and anti-tumor immunity: Exposing immunogenic mutations to the immune system. Genome Med. 2019, 11, 40. [Google Scholar] [CrossRef] [Green Version]
- Oike, T.; Niimi, A.; Okonogi, N.; Murata, K.; Matsumura, A.; Noda, S.E.; Kobayashi, D.; Iwanaga, M.; Tsuchida, K.; Kanai, T.; et al. Visualization of complex DNA double-strand breaks in a tumor treated with carbon ion radiotherapy. Sci. Rep. 2016, 6, 22275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sha, C.M.; Lehrer, E.J.; Hwang, C.; Trifiletti, D.M.; Mackley, H.B.; Drabick, J.J.; Zaorsky, N.G. Toxicity in combination immune checkpoint inhibitor and radiation therapy: A systematic review and meta-analysis. Radiother. Oncol. 2020, 151, 141–148. [Google Scholar] [CrossRef] [PubMed]
- El Sabbagh, R.; Azar, N.S.; Eid, A.A.; Azar, S.T. Thyroid Dysfunctions Due to Immune Checkpoint Inhibitors: A Review. Int. J. Gen. Med. 2020, 13, 1003–1009. [Google Scholar] [CrossRef]
- Okonogi, N.; Usui, H.; Murata, K.; Hori, M.; Kurokawa, T.; Fujiwara, T.; Fujii, Y.; Hanawa, M.; Kawasaki, Y.; Hattori, Y.; et al. Phase Ib study of durvalumab (MEDI4736) in combination with carbon-ion radiotherapy and weekly cisplatin for patients with locally advanced cervical cancer (DECISION study): Study protocol for a prospective open-label single-arm study. BMJ Open 2022, 12, e056424. [Google Scholar] [CrossRef] [PubMed]
- Japanese Society for Radiation Oncology. Authorized Treatment Policy of Carbon-Ion Radiotherapy for Locally Advanced Cervical Cancer. Available online: https://www.jastro.or.jp/medicalpersonnel/particle_beam/2022/07/post-10.html (accessed on 21 March 2023). (in Japanese).
- Inaniwa, T.; Furukawa, T.; Kase, Y.; Matsufuji, N.; Toshito, T.; Matsumoto, Y.; Furusawa, Y.; Noda, K. Treatment planning for a scanned carbon beam with a modified microdosimetric kinetic model. Phys. Med. Biol. 2010, 55, 6721–6737. [Google Scholar] [CrossRef] [PubMed]
- Mayadev, J.; Nunes, A.T.; Li, M.; Marcovitz, M.; Lanasa, M.C.; Monk, B.J. CALLA: Efficacy and safety of concurrent and adjuvant durvalumab with chemoradiotherapy versus chemoradiotherapy alone in women with locally advanced cervical cancer: A phase III, randomized, double-blind, multicenter study. Int. J. Gynecol. Cancer 2020, 30, 1065–1070. [Google Scholar] [CrossRef] [PubMed]
- Integrated Addendum to ICH E6 (R1): Guideline for Good Clinical Practice. Available online: https://database.ich.org/sites/default/files/E6_R2_Addendum.pdf (accessed on 21 March 2023).
- Common Terminology Criteria for Adverse Events (CTCAE) Version 5.0. Available online: https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/ctcae_v5_quick_reference_5x7.pdf (accessed on 21 March 2023).
- Eisenhauer, E.A.; Therasse, P.; Bogaerts, J.; Schwartz, L.H.; Sargent, D.; Ford, R.; Dancey, J.; Arbuck, S.; Gwyther, S.; Mooney, M.; et al. New response evaluation criteria in solid tumours: Revised RECIST guideline (version 1.1). Eur. J. Cancer 2009, 45, 228–247. [Google Scholar] [CrossRef]

| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Age at the enrollment | 7X | 4X | 5X |
| ECOG PS | 0 | 0 | 0 |
| Race and ethnicity | Japanese | Japanese | Japanese |
| Staging, FIGO (2018) | IIIC1r | IIIC1r | IIIC1r |
| Staging, TNM UICC (8th) | cT2bN1M0 | cT2bN1M0 | cT3bN1M0 |
| Tumor histology | Squamous cell carcinoma, NOS | Endocervical adenocarcinoma, usual type | Adenocarcinoma, NOS |
| Maximal tumor diameter, mm | 60 | 46 | 107 |
| Past medical history | Right wrist fracture | Asthma, cerebral aneurysm, and psoriasis | (None) |
| Coexisting disease | Headache | Menopausal disorders | Depression, conjunctival hyperemia, hyperlipidemia, and hay fever |
| Items | Grading, Number of Patients | ||||
|---|---|---|---|---|---|
| Grade 0 | Grade 1 | Grade 2 | Grade 3 | Grade ≥ 4 | |
| Hematologic toxicity | |||||
| Leukopenia | 0 | 0 | 1 | 2 | 0 |
| neutropenia | 0 | 0 | 0 | 3 | 0 |
| Non-hematologic toxicity | |||||
| Hypothyroidism | 2 | 0 | 0 | 1 | 0 |
| Stomatitis | 2 | 1 | 0 | 0 | 0 |
| Colitis/Diarrhea | 3 | 0 | 0 | 0 | 0 |
| Cystitis | 3 | 0 | 0 | 0 | 0 |
| Dry mouth and eyes * | 2 | 1 | 0 | 0 | 0 |
| Eczema | 1 | 1 | 1 | 0 | 0 |
| Creatinine increased | 2 | 0 | 1 | 0 | 0 |
| Serum amylase increased | 2 | 0 | 1 | 0 | 0 |
| GGT increased | 1 | 0 | 1 | 1 | 0 |
| Hematologic Toxicity |
|---|
|
| Non-Hematologic Toxicity |
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Okonogi, N.; Murata, K.; Yamada, S.; Habu, Y.; Hori, M.; Kurokawa, T.; Inaba, Y.; Fujiwara, T.; Fujii, Y.; Hanawa, M.; et al. A Phase Ib Study of Durvalumab (MEDI4736) in Combination with Carbon-Ion Radiotherapy and Weekly Cisplatin for Patients with Locally Advanced Cervical Cancer (DECISION Study): The Early Safety and Efficacy Results. Int. J. Mol. Sci. 2023, 24, 10565. https://doi.org/10.3390/ijms241310565
Okonogi N, Murata K, Yamada S, Habu Y, Hori M, Kurokawa T, Inaba Y, Fujiwara T, Fujii Y, Hanawa M, et al. A Phase Ib Study of Durvalumab (MEDI4736) in Combination with Carbon-Ion Radiotherapy and Weekly Cisplatin for Patients with Locally Advanced Cervical Cancer (DECISION Study): The Early Safety and Efficacy Results. International Journal of Molecular Sciences. 2023; 24(13):10565. https://doi.org/10.3390/ijms241310565
Chicago/Turabian StyleOkonogi, Noriyuki, Kazutoshi Murata, Shigeru Yamada, Yuji Habu, Makoto Hori, Tomoya Kurokawa, Yosuke Inaba, Tadami Fujiwara, Yasuhisa Fujii, Michiko Hanawa, and et al. 2023. "A Phase Ib Study of Durvalumab (MEDI4736) in Combination with Carbon-Ion Radiotherapy and Weekly Cisplatin for Patients with Locally Advanced Cervical Cancer (DECISION Study): The Early Safety and Efficacy Results" International Journal of Molecular Sciences 24, no. 13: 10565. https://doi.org/10.3390/ijms241310565






