1. Introduction
Coronaviruses (CoVs) are large, enveloped, single-stranded positive-sense RNA viruses that cause severe disease in both humans and animals. Until 2019, six α- and β-CoVs were known to cause respiratory diseases of varying severities in humans, including viruses that cause symptoms of the common cold (229E, NL63, OC43, and HKU1) and two highly pathogenic CoVs (SARS-CoV and MERS-CoV). In December 2019, a new highly pathogenic and transmissible CoV was isolated from patients with respiratory disease [
1]. Since then, the severe acute respiratory syndrome (SARS) coronavirus 2 (CoV-2), the causative agent of the CoV disease 19 (COVID-19), was responsible for over 200,000,000 cases and more than 4,000,000 deaths worldwide [
2]. Although potent vaccines are now available, specific antiviral drugs for the prevention and treatment of COVID-19 are urgently needed.
Reverse genetic approaches to generate recombinant viruses are a powerful tool to uncover the biology of viral infections. Infectious molecular clones are highly valuable research tools to better understand the mechanisms of viral infections and to answer important questions regarding virus transmission and pathogenesis. Moreover, recombinant viruses expressing reporter genes facilitate cell culture-based screening assays or small animal models to identify prophylactic or therapeutic compounds. Finally, precise and uncomplicated approaches to manipulate viral genomes are prerequisites to generate live-attenuated vaccine candidates and to identify viral and host factors that are involved in virus biology and immunity.
Several different methods were already used to generate recombinant SARS-CoV-2 viruses, including in vitro ligation [
3], homologous recombination in yeast [
4], and circular polymerase extension reaction [
5,
6], as well as plasmid- and bacterial artificial chromosome (BAC)-based approaches [
7,
8,
9].
In this study, we describe the assembly of a passage-free SARS-CoV-2 B.1 genome into a single BAC and its manipulation by Lambda Red-based recombination, which was originally established for the manipulation of herpesvirus genomes [
10,
11]. We demonstrate that our reverse genetics system can be easily used to recover wild-type and mutant viruses from transfected cells. Red recombination alone or in combination with Gibson assembly were successfully applied to generate different fluorescence and luciferase reporter viruses. Recovered viruses display growth kinetics comparable to the recombinant wild-type (WT) and the clinical isolate. The results obtained within this study demonstrate that our recombinant reporter-expressing SARS-CoV-2 variants represent a reliable tool for the identification of new therapeutics for the prevention and treatment of COVID-19, as shown for the two reference drugs remdesivir (RDV) and GC376. Notably, we designed a marker virus that enables the visualization of incoming viral particles on a single-cell level. Collectively, our methodological platform represents an ideal tool for the fast and easy cloning of modified viruses to promote drug development, live-attenuated vaccine candidates, and a better understanding of the transmission and pathology of constantly emerging variants of concern.
3. Discussion
Reverse genetics approaches to generate recombinant viruses are a powerful tool to characterize newly emerged viruses. Although several reverse genetics systems for CoVs, and especially SARS-CoV-2, have been described, those existing systems have several labor- and cost-intensive, error-prone, and time-consuming drawbacks, including the chemical synthesis of large DNA fragments [
9], in vitro ligation [
3], and in vitro transcription [
3,
4]. Here, we established a BAC-based reverse genetics system by applying Red recombination commonly used in the context of large DNA viruses, particularly herpesviruses. Of note, the technique can avoid the necessity of a previous viral isolate or allow to obtain clones from diagnostic samples in virus-inactivating chaotropic buffers. The advantage of this approach is the fast and easy manipulation of viral sequences by homologous recombination. By using this method, we successfully generated SARS-CoV-2-encoding BACs and reconstituted an infectious virus upon the transfection of HEK293T cells. Those cells allow the application of conventional, cost-efficient, well-established standard transfection methods with high transfection rates, an approach that has also been used by others [
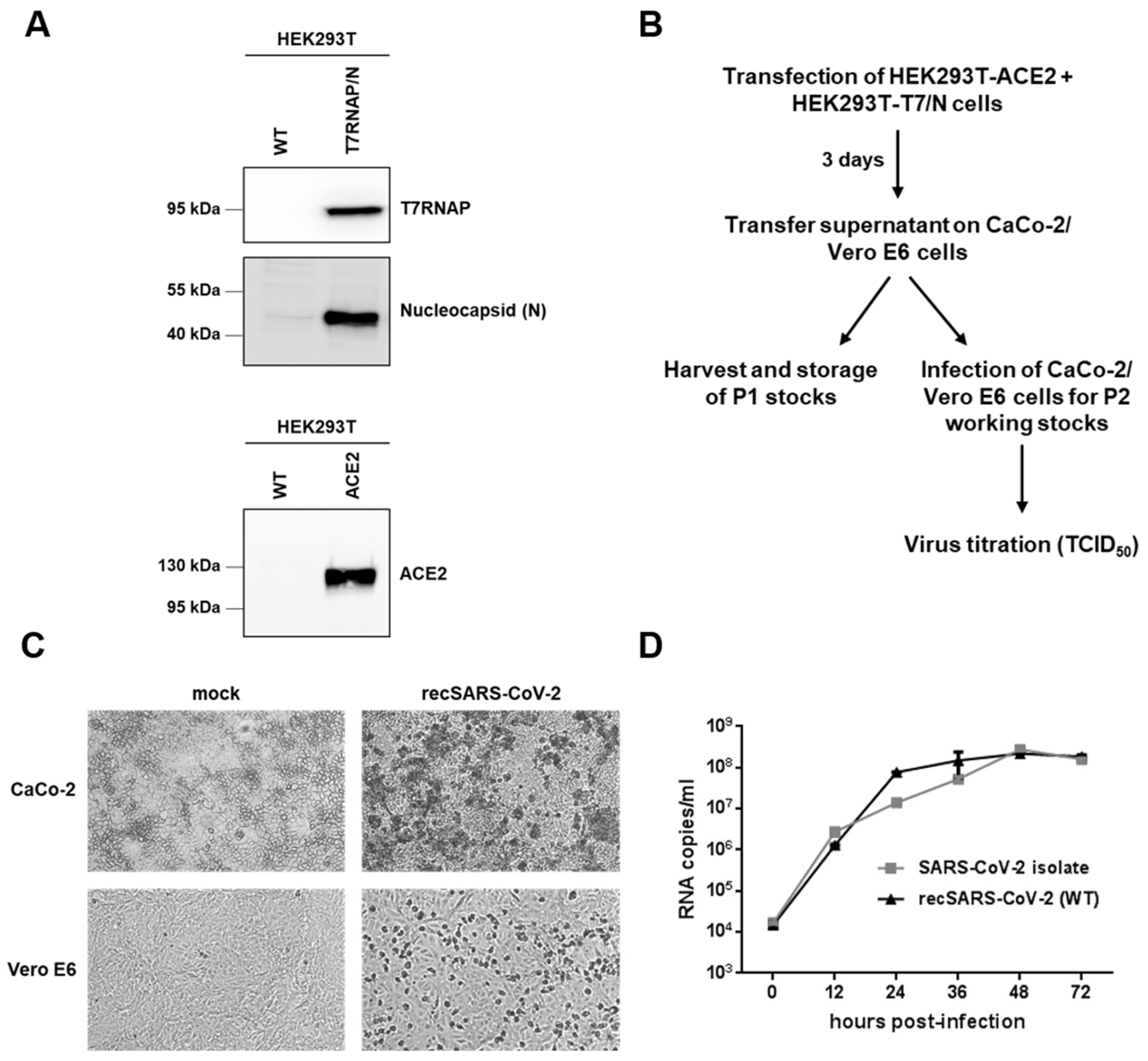
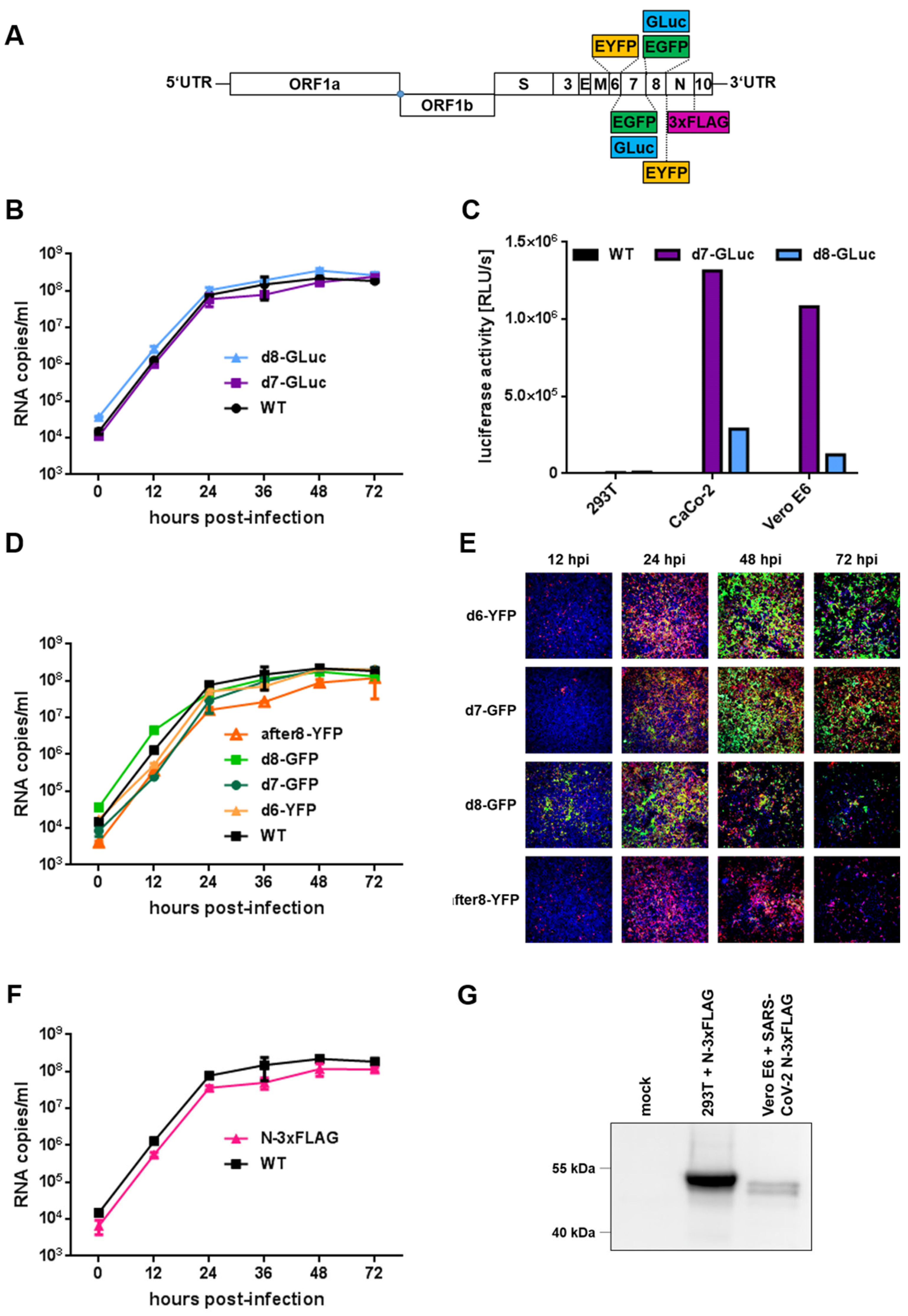
6]. After passaging the supernatant onto susceptible cells, we obtained a recombinant virus with comparable replication characteristics and similar peak virus titers compared to a clinical isolate. Moreover, we successfully applied our recombination technique to generate a set of different reporter viruses. The replacement of viral ORF7a or ORF8 with either EGFP or gaussia luciferase (GLuc) and ORF6 with EYFP led to reporter viruses that display WT-like replication kinetics and peak viral titers. This demonstrates that the deletion of either ORF by GLuc or EGFP/EYFP does not affect the viral fitness and that those ORFs are dispensable for SARS-CoV-2 replication in cell cultures. In contrast to ORF7a-deficient mutants reported by other groups, which showed impaired replication fitness compared to the WT strain [
3,
4,
6], our newly generated d7-GFP and d7-GLuc reporter viruses displayed WT-like growth kinetics in Caco-2 cells, indicating that ORF7a is dispensable in vitro.
When we visually compared cells infected with the distinct reporter viruses, we observed differences in the fluorescence reporter expression profiles and kinetics, depending on the subgenomic localization of the reporter gene. This discrepancy might be explained by variations in the expression kinetics of individual viral proteins. Thus, it might be necessary to choose different time points for fluorescent readouts, depending on the viral strain that is used. Moreover, our results point towards a decreased genomic stability of viruses that express reporter genes instead of ORF8 compared to ORF6 or ORF7 over longer passaging in cell cultures. The reduced stability of d8 constructs indicating a lower genomic stability might be due to the replacement of a fast-evolving area of the SARS-CoV-2 genome [
15]. Deletions or frameshift mutations in SARS-CoV-2 ORF8 have been observed at the beginning of the pandemic [
16], in the recent B.1.1.7 (Alpha) variant, and, correspondingly, in the SARS-CoV ORF8 in the late SARS-CoV epidemic [
17,
18,
19]. Furthermore, it might be possible that the introduction of an additional artificial ORF, like is the case in our full-length after8-YFP reporter virus, is also not stable over time. If this observation is also related to the apparent instability of the ORF8 region requires further investigation. However, since all reporter viruses are stable over time periods that are usually used for standard molecular approaches, all reporter viruses generated within this study are well-suited for the assays applied herein.
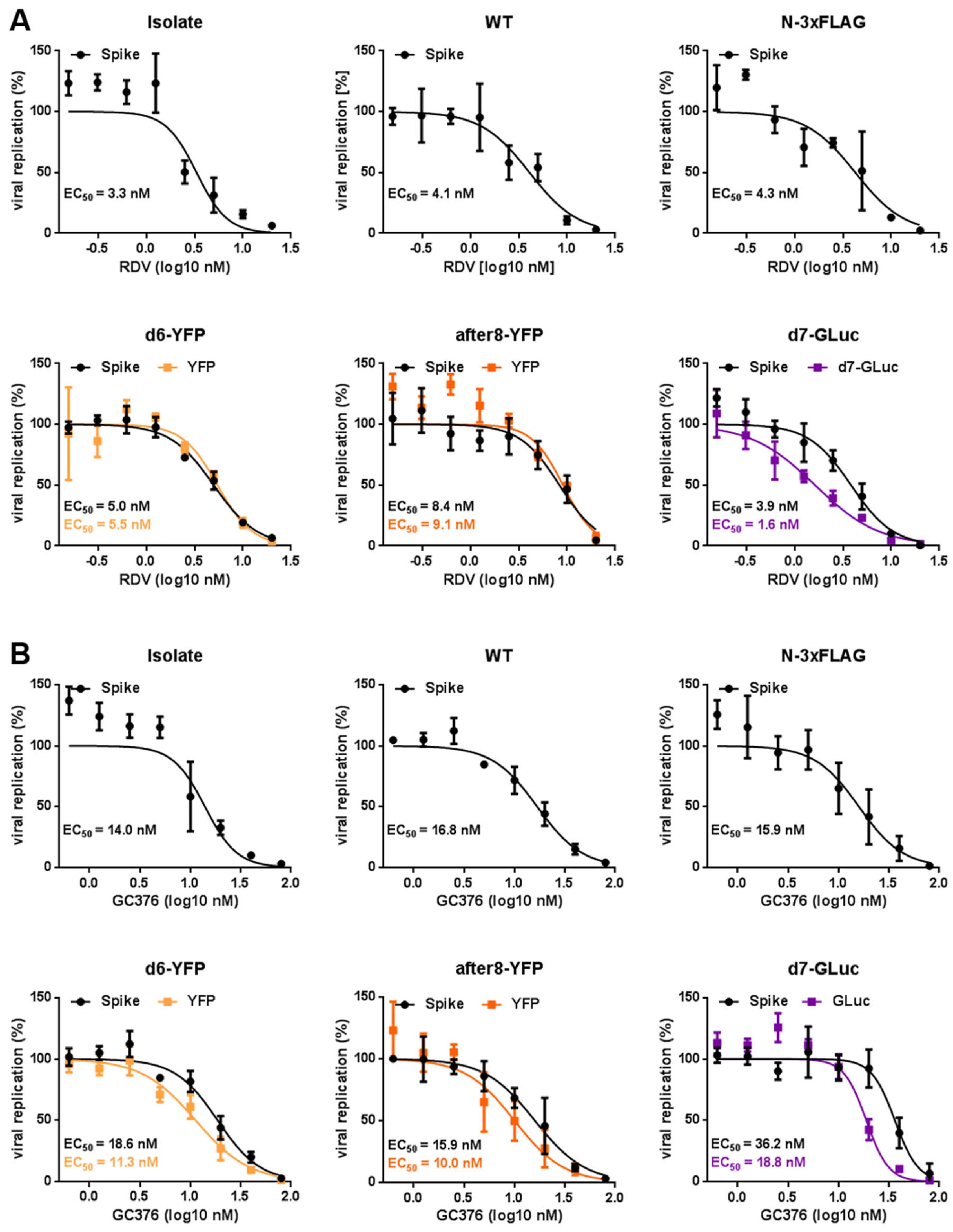
Virus-encoded fluorescent reporters allow the direct and highly quantitative detection of viral replication, as well as imaging approaches, which ease the testing of antiviral drug candidates. Here, we showed that our reporter readouts yielded similar EC50 values for the reference compounds RDV and GC376 compared to the immunostaining of the spike protein. Thus, without the requirement of additional detection reagents like antibodies or nucleic acid extraction followed by RT-qPCR, they provide a time-saving and cost-efficient means of analyses. Based on the available instrumentation present in the individual BSL-3 facilities, different types of reporters like the GLuc-expressing variants described herein can be designed to meet those requirements, thus further accelerating antiviral screenings. In particular, the use of secreted GLuc enables the analysis of different time points from the same sample without the need for cell lysis, thus leaving infected cells intact for additional confirmation or assays.
Moreover, we generated the full-length reporter virus after8-YFP with an additionally introduced artificial ORF encoding EYFP between ORF8 and N. Since this virus shows WT-like replication, this indicates that the plasticity of the SARS-CoV-2 genome tolerates the insertion of an additional ORF. The reduced level of reporter expression compared to the reporter introduced by gene replacement may reflect the TRS usage and may, in future experiments, be optimized by altering this element to increase the generation of reporter-specific sgRNAs. Possibly, the insertion of a second artificial ORF might be feasible, opening the potential of generating dual-reporter viruses encoding both fluorescence and luminescence reporters without the need to replace any viral protein. Thus, such recombinant viruses are prerequisite tools to study SARS-CoV-2 biology in vivo.
Furthermore, this methodological approach is not restricted to the examples presented herein but provides countless possibilities for generating functional knockouts of the versatile SARS-CoV-2 enzymes, the analysis of different spike alleles from circulating variants of concern (VoC), their contribution to immune and vaccine escape [
20,
21], and their relevance for virus transmission and pathogenicity, as well as the characterization of potential drug-resistance mutations [
22,
23] in an otherwise isogenic background. Moreover, our approach enables the rapid deletion of viral proteins to gain more insights into their contributions to replication, pathogenesis, transmission, and disease outcome in an infectious background. Moreover, the introduction of single restriction sites by Red recombination allows the directed integration and replacement of any desired region within the viral genome by techniques such as Gibson assembly [
24].
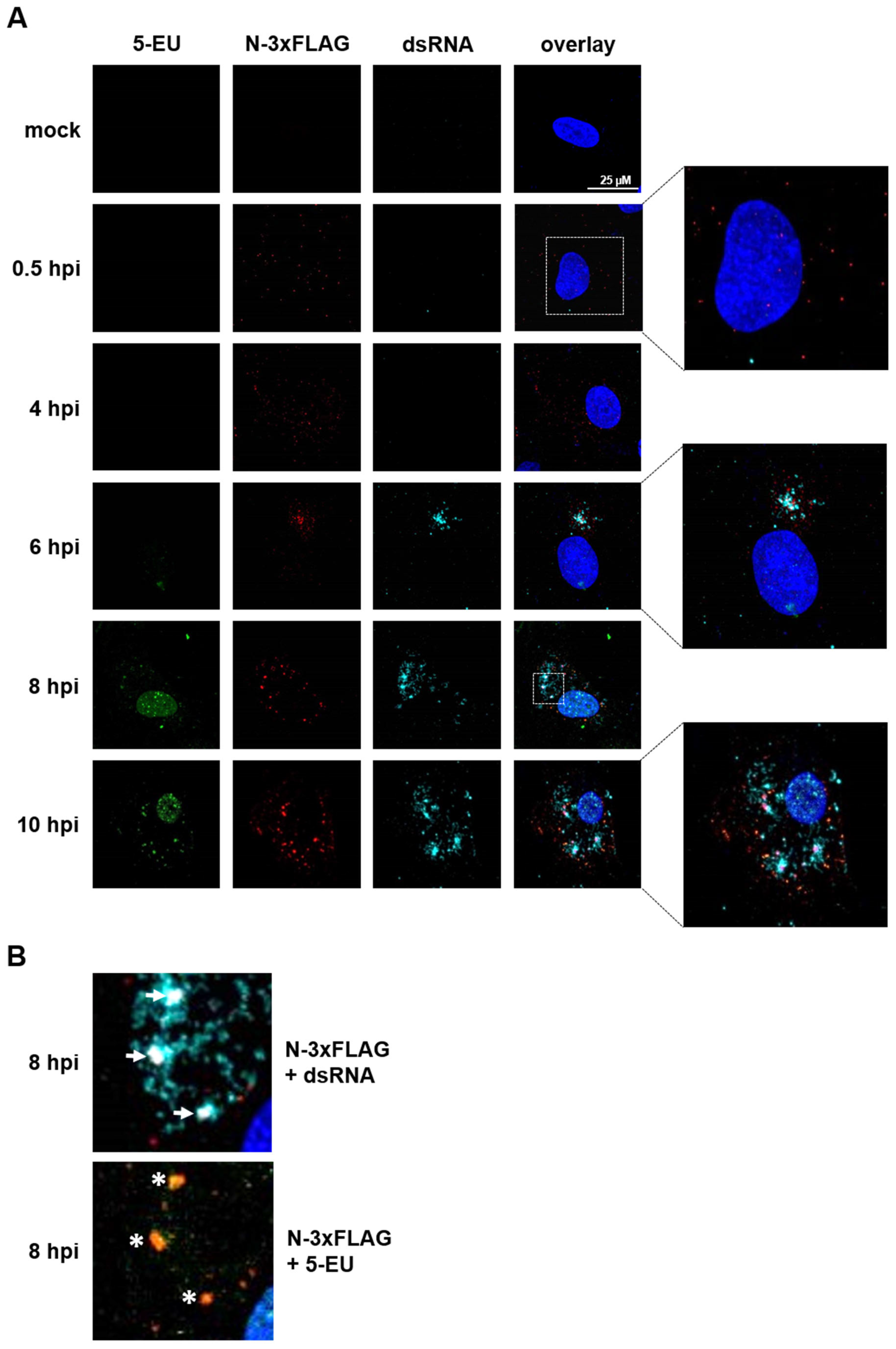
Last, but not least, we cloned a full-length marker virus that expresses 3xFLAG-tagged nucleocapsid, which allows the detection of viral nucleocapsids on the single-cell level. Thus, to our knowledge, we were the first that applied the tagged SARS-CoV-2 N protein for visualization by immunofluorescence approaches, which provides the advantage of specificity and background minimization. In combination with biorthogonal click chemistry to label viral RNAs and/or the detection of dsRNA, these methods facilitate a spatiotemporal analysis of the viral replication processes, as well as the influence of host and/or viral immune regulators.
In summary, by introducing BAC-based Red recombination into SARS-CoV-2 research, we developed a powerful, reliable, and convenient platform to facilitate studies answering numerous questions concerning the biology of SARS-CoV-2. Since CoVs are prone to transmission to new host species, gaining more insights into SARS-CoV-2 replication, pathogenicity, transmission, and interaction with host cell factors leads to a better preparedness for future pandemic CoVs.
4. Materials and Methods
4.1. Biosafety
All infection experiments were performed under biosafety level (BSL)-3 conditions. Modifications and preparations of pBSCoV2 BACs containing the full-length SARS-CoV-2 genome were conducted under BSL-2 conditions.
4.2. Cell Culture
In general, all the cell lines were cultivated at 37 °C, 5% CO2, and 80% humidity. All the cell lines were tested frequently for mycoplasma contaminations using the MycoAlert™ Mycoplasma Detection Kit (LT07-703, Lonza, Basel, Switzerland) according to the supplier’s manual. Human embryonic kidney (HEK) 293T (ATCC® CRL-3216™, ATCC, Manassas, VA, USA) and Vero E6 cells (85020206, Sigma-Aldrich, St. Louis, MO, USA) were maintained in Dulbecco’s Modified Eagle’s Medium (DMEM; 11500516, Thermo Fisher Scientific, Waltham, MA, USA) supplemented with 10% heat-inactivated fetal calf serum (FBS-12A; Capricorn Scientific, Ebsdorfergrund, Germany), 2-mM GlutaMAX™ (35050061, Thermo Fisher Scientific), 25-mM HEPES (15630080, Thermo Fisher Scientific), and 50-µg/mL gentamycin (1405-41-0, Serva Electrophoresis, Heidelberg, Germany). The CaCo-2 cells (kindly provided by Konstantin Sparrer, University Hospital Ulm, Germany) were cultivated in DMEM additionally containing 1x MEM Non-Essential Amino Acids Solution (11140050, Thermo Fisher Scientific). The HEK293T-ACE2 and HEK293T-T7RNAP/N cells were maintained in DMEM additionally supplemented with 5-µg/mL blasticidin (asnt-bl-1, InvivoGen, San Diego, CA, USA) or 5-µg/mL blasticidin and 2-µg/mL puromycin (SC-1080713, Santa Cruz Biotechnology, Dallas, TX, USA), respectively. Stable HEK293T-ACE2 cells were generated by lentiviral transduction with pLV-EF1a-IRES-Blast (#85133, Addgene, Watertown, MA, USA) encoding the human ACE2 gene. HEK293T-T7RNAP/N cells were established using the lentiviral vectors pLV-EF1a-IRES-Blast and pLV-EF1a-IRES-Puro (#85132, Addgene, Watertown, MA, USA) encoding the T7 RNA polymerase or the SARS-CoV-2 nucleoprotein (N), respectively.
4.3. Plasmids
For the cloning of pLV-EIB-N and pLV-EIB-ACE2, the pLV-EF1a-IRES-Blast vector (#85133, Addgene, Watertown, MA, USA) was used. For the cloning of pLV-EIP-T7RNAP, we used the pLV-EF1a-IRES-Puro vector (#85132, Addgene). The viral nucleoprotein (N) was amplified from the patient material, T7 RNA polymerase (T7RNAP) was amplified from pCAGT7 (kindly provided by Marco Thomas, Institute for Clinical and Molecular Virology, Erlangen, Germany), and pCG1-hACE2 [
25] served as the template for the amplification of hACE2. All the vectors were generated by Gibson assembly [
24] and confirmed by Sanger sequencing and a Western blot analysis. For cloning pLV-EF1a-IRES-Blast-N-3xFLAG, the pBSCoV2-N-3xFLAG bacmid generated within this study was used as the template. All the primers used for plasmid generation are listed in
Table S1 and were purchased from Integrated DNA Technologies (IDT, Coralville, IA, USA).
4.4. Western Blot Analysis
For the Western blot analysis, pelleted cells were lysed in RIPA buffer (1% Triton X-100, 0.5% sodium deoxycholate, 0.1% SDS, 150-mM NaCl, 1-mM EDTA, and 50-mM Tris (pH 8.0)) with freshly added aprotinin (A2132, AppliChem, Darmstadt, Germany) and leupeptin (A2183, AppliChem). The protein content of the soluble fraction was assayed with a Pierce™ BCA Protein Assay Kit (23225, Thermo Fisher Scientific). The samples were diluted in a Laemmli SDS sample buffer, separated by SDS-PAGE, and the proteins were transferred on PVDF membranes (Immobilon®-P (IPVH00010) for the HRP-labeled secondary antibodies and Immobilon®-FL (IPFL00010) for the fluorescence-labeled secondary antibodies, both from Merck Millipore, Burlington, MA, USA). The membranes were blocked with 5% dry milk powder prior to antibody incubation. For the detection of T7-RNA polymerase, a mouse monoclonal antibody (70566, Novagen®/Sigma-Aldrich, St. Louis, MO, USA) at a dilution of 1:5000 was used with the HRP-coupled anti-mouse secondary antibody. The viral nucleoprotein was stained with a rabbit polyclonal nucleocapsid (N) antibody (ARC2372, Thermo Fisher Scientific) at a dilution of 1:2000 and an anti-rabbit-Alexa555 secondary antibody. Human ACE2 was probed with a mouse monoclonal antibody (ACE2 E-11, Santa Cruz Biotechnology) at 1:500 and an Alexa647-labled anti-mouse secondary antibody. The 3x-FLAG-tagged nucleoprotein was detected with a rabbit polyclonal anti-DYKDDDDK tag antibody (PA1-984B, 1:1000; Thermo Fisher Scientific).
4.5. Cloning of Full-Length SARS-CoV-2 Genome
For the cloning of a passage-free SARS-CoV-2 genome, an anonymized residual sample from a patient with SARS-CoV-2 infection was used as a template. The total nucleic acids of a respiratory swab sample were extracted on an automated Qiagen EZ1 analyzer (Qiagen, Hilden, Germany) using the Qiagen EZ1 virus mini kit v2.0 (Qiagen, 955134) according to the manufacturer’s instructions. The extracted nucleic acids were eluted in 90-µL ultrapure water. For cDNA synthesis, the extracted nucleic acids were reverse-transcribed with the LunaScript
® RT SuperMix Kit (E3010, New England Biolabs (NEB), Frankfurt am Main, Germany) according to the supplier’s manual. Afterwards, 5 U of RNaseH (M0297, NEB) were added to the mix, followed by incubation for 30 min at 37 °C and further dilution by the addition of 80 µL 0.1× TE buffer. The obtained cDNA was used for the amplification of four fragments covering the entire viral genome using Q5-DNA-Polymerase (NEB). The resulting fragments were assembled with the modified and
PacI-linearized pBeloBAC11 (Gene Bank Accession U51113, NEB) backbone pBeloCoV. For the construction of pBeloCoV, the CMV and T7 promoters, as well as the bGH polyA tail, were amplified from a pcDNA4 vector (V86320, Thermo Fisher Scientific). Gene blocks encoding for the hepatitis virus D ribozyme, the 5′ and the 3′ end of the SARS-CoV-2 genome with a flanking
PacI site, and a linker for the polyA tail were ordered from Integrated DNA Technologies (IDT, Coralville, IA, USA). The assembly of these modules using the NEBuilder HiFi DNA Assembly Cloning Kit (E5520, NEB) resulted in the modified pBeloCoV bacmid. The four fragments covering the SARS-CoV-2 genome were then assembled with the
PacI-digested pBeloCoV vector according to the NEBuilder HiFi DNA Assembly Cloning Kit protocol (E5520, NEB) to obtain pBelo-SARS-CoV-2 (pBSCoV2). After electroporation into
E. coli NEB
® 10-beta (C3019, NEB), the clones were screened by restriction digestion and further analyzed by next-generation sequencing. To receive the clones with a full-length SARS-CoV-2 genome, one clone that was found to lack fragment 2 was transformed into the
E. coli strain GS1783, and Red recombination was performed to insert the missing fragment, as previously described [
10,
11] (
Figure S1). First, a kanamycin resistance cassette with short-sequence duplications to the SARS-CoV-2 genome at the site of recombination and flanking
AscI sites was PCR-amplified (7107-fwd-recAsc and 13997-rev-recAsc) using pEPkan-S as a template [
11] and digested with
DpnI. The purified PCR product was electroporated into
E. coli GS1783 containing the incomplete clone, and recombination was initiated. The positive clones that grew on kanamycin-containing plates were screened by colony PCR and restriction digestion. Purified DNA of two clones was digested with
AscI to remove the kanamycin resistance cassette, and afterwards, an assembly with the lacking fragment 2 was performed according to the NEBuilder HiFi DNA Assembly Cloning Kit protocols (E5520, NEB). The DNA was transformed into
E. coli GS1783, and the resulting colonies were screened by restriction digestion. Clones with restriction patterns matching the pBSCoV2 bacmid with a full-length SARS-CoV-2 genome were confirmed by next-generation sequencing.
4.6. Generation of SARS-CoV-2 Reporter Viruses by Red-Mediated Recombination
To generate different SARS-CoV-2 marker and reporter viruses, the two-step markerless Red recombination system was used [
10,
11]. Within this study, pBSCoV2-N-3xFLAG (N-3xFLAG), deltaORF7a-GLuc (d7-GLuc), deltaORF7a-EGFP (d7-GFP), deltaORF8-GLuc (d8-GLuc), deltaORF8-EGFP (d8-GFP), deltaORF6-EYFP (d6-YFP), and after8-EYFP (after8-YFP) were cloned. All ultramer primers used for their assembly are listed in
Table S1 and were purchased from IDT. As a starting point, the
E. coli strain GS1783 containing the pBSCoV2 bacmid encoding the full-length SARS-CoV-2 genome was used. First, the kanamycin resistance cassettes for the first Red recombination were generated, with either one I-
SceI (for N-3xFLAG, d6-YFP, and after8-YFP) or two flanking
SacII restriction sites (for d7-Luc, d7-GFP, d8-Luc, and d8-GFP), as well as flanking sequences with homology to the corresponding site of insertion within the SARS-CoV-2 genome. For d6-YFP and after8-YFP, the pEP-EYFP-in vector [
10] was used as a template, whereas pEPkan-S served as the template for N-3xFLAG and d7 or d8. Upon electroporation of the purified kanamycin cassettes into
E. coli GS1783 containing pBSCoV2, kanamycin-resistant clones were screened by colony PCR and restriction digestion. In the case of N-3xFLAG, d6-YFP, and after8-YFP, the kanamycin resistance cassette was removed by in vivo cleavage upon the induction of I-
SceI with 1% arabinose, followed by a second Red recombination. For the d7 and d8 reporter viruses, the kanamycin resistance cassette was removed by digestion with
SacII. Assembly with the NEBuilder HiFi DNA Assembly Cloning Kit (E5520, NEB), according to the supplier’s protocols, inserted DNA fragments encoding for either gaussia luciferase (GLuc) or EGFP. Reporter cassettes were PCR-amplified with primers with homology to the site of insertion. Assembled bacmids were transformed again into
E. coli GS1783. Colonies that lost the ability to grow on kanamycin-containing plates were analyzed by restriction digestion and Sanger sequencing of the recombination sites and inserts, as well as next-generation sequencing of the confirmed positive clones.
4.7. Next-Generation Sequencing and Computational Analysis
For library preparation, 50-ng purified bacmid DNA and the Nextera DNA Library Preparation Kit (FC-131.1024, Illumina, San Diego, CA, USA) were used. Tagmented DNA was amplified with specific dual index primers (Integrated DNA Technologies) using the NEBNext® HiFi 2× PCR Master Mix (M0541, NEB) according to the manufacturer’s protocols. The libraries were cleaned up with AMPure XP beads (A63881, Beckman Coulter, Brea, CA, USA) and quantified using the Qubit dsDNA HS Assay Kit (Q32851, Thermo Fisher Scientific). Normalized, pooled libraries were analyzed by paired-end next-generation sequencing using a MiSeq reagent kit v2, with 300 or 500 cycles on a MiSeq™ Instrument (Illumina). The sequences were analyzed with CLC Genomics Workbench 21 (Qiagen Aarhus A/S, Aarhus, Denmark).
4.8. Virus Recovery
For virus reconstitution, a coculture of HEK293T cells stably expressing either ACE2 or the viral N protein and T7-RNA polymerase was transfected with 8 µg of purified pBelo-S-CoV-2 and 2 µg of pLV-EF1a-IRES-Blast-N using 20-µL GenJet™ Reagent (II) (SL100489, SignaGen® Laboratories, Frederick, MD, USA) according to the manufacturer’s protocols in T25 tissue culture flasks. Three days post-transfection, the supernatant (P0) was transferred on CaCo-2 or Vero E6 cells for passage 1 (P1) virus stocks. Passage 2 (P2) virus stocks were obtained after the infection of CaCo-2 cells with 1:50 volume of the P1 virus. The viral titers were calculated by endpoint titration (TCID50). Positive wells were determined by in-cell immunostaining of the viral spike protein.
4.9. In-Cell Immunostaining
For the visualization of intracellular viral antigens, paraformaldehyde-fixed cells were permeabilized and blocked with 1% BSA and 0.2% Triton X-100 in PBS overnight at 4 °C or 1 h at RT. Afterwards, the cells were stained with a mouse monoclonal antibody against the viral spike protein (mAB-S TRES-VI6.18 [
26], 1:2000 diluted in 1% BSA and 0.2% Triton X-100 in PBS) and Alexa488- or Alexa647-conjugated secondary antibodies (A11029/A31571, 1:2000 diluted in 1% BSA and 0.2% Triton X-100 in PBS, Thermo Fisher Scientific), respectively. In parallel, Hoechst 33342 (14533, Sigma-Aldrich) 1:5000 diluted in PBS served as the internal control for estimating the cell counts. To quantitatively evaluate the stained plates, a Victor X4 multilabel reader (Perkin Elmer, Waltham, MA, USA) was used. An ImmunoSpot
® S6 ULTIMATE UV Image Analyzer (Cellular Technology Limited/CTL, Shaker Heights, OH, USA) was used for visualization of the total cell numbers and infected cells.
4.10. RT-qPCR
CaCo-2 cells were seeded in 96-well plates. The next day, the cells were infected with the corresponding virus at an MOI of 0.005. The supernatants were harvested at 0, 12, 24, 36, 48, and 72 h post-infection. To quantify the viral genome copies, the supernatants were diluted 1:10 with H
2O and heat-inactivated for 15 min at 95 °C. Prior to RT-qPCR, the viral supernatants were digested with proteinase K (final concentration of 0.136 mg/mL; PCR-grade, 3115828001, Sigma-Aldrich) for 1 h at 56 °C, followed by heat inactivation for 5 min at 95 °C. For the subsequent analysis, volumes of 5 µL of the digested supernatants were used, and the RT-qPCR was performed according to the Luna
® Universal Probe One-Step RT-qPCR Kit protocol (E3006, NEB) in an Applied Biosystems 7500 Real-Time PCR system (Applied Biosystems, Waltham, MA, USA). The primer and probe sequences targeting the viral polymerase (RdRp) were adapted and modified from Reference [
27]. The probe was 5′-labeled with VIC (2′-chloro-7′phenyl-1,4-dichloro-6-carboxy-fluorescein) and 3′-labeled with BMN535 quencher modification (Biomers, Ulm, Germany).
4.11. Luciferase Assay
To measure the gaussia luciferase (GLuc) activity, the supernatants were heat-inactivated for 15 min at 95 °C and cooled down at RT prior to the luciferase assay. Subsequently, 50 µL of a 1:40 dilution were transferred into a white 96-well plate. Per well, 100-µL Renilla assay buffer (1.1-M NaCl, 2.2-mM Na2EDTA, and 0.22-M KPO4) and 0.2 µL of 0.7-mM Coelenterazine (102171, PJK Biotech, Kleinblittersdorf, Germany) were used. The luciferase activity was determined in an Orion II Microplate Luminometer (Berthold Detection Systems, Bad Wildbad, Germany) with a 4 s delay time and 5 s measurement time.
4.12. Antiviral Compounds and EC50 Calculation
RDV (Gilead, Foster City, CA, USA) and GC376 (T5188, TargetMol, Boston, MA, USA) were used as the reference compounds to determine the anti-SARS-CoV-2 activity for recSARS-CoV-2. The CaCo-2 cells were treated with 2-fold serial dilutions of either RDV (20 nM–0.16 nM) or GC376 (80 nM–0.63 nM) and infected with different SARS-CoV-2 strains at an MOI of 0.005. At 30 hpi, the cells were fixed and analyzed. The infection rates were assessed by immunostaining of the viral spike and reporter expression, respectively. The percentage of viral replication was determined relative to the solvent-treated cells. The 50% effective concentration (EC50) was assessed by nonlinear four-parameter curve fitting using GraphPad Prism 6 (GraphPad Software, San Diego, CA, USA).
4.13. Neutral Red Assay
The cytotoxicity of RDV and GC376 was determined by the neutral red uptake assay (N-2889, Sigma-Aldrich). The CaCo-2 cells were seeded in 96-well plates and incubated with the antiviral compounds for 3 days. Staurosporine (AG-CN2-0022-M005, Biomol, Hamburg, Germany) at a concentration of 10 µM was used as the toxicity control. The assay was performed as previously described [
28] using a final concentration of 40-µg/mL neutral red. The amount of incorporated neutral red was quantitated in a Victor X4 multilabel reader (Perkin Elmer LAS GmbH, Rodgau, Germany) by fluorescence measurements at 560/630 nm.
4.14. Click Chemistry and Immunofluorescence Staining
Vero E6 cells were seeded in 24-well plates on round coverslips. The day after, the cells were infected with pBSCoV2-N-3xFLAG. One hour post-infection (hpi), the virus inoculum was removed, and the cells were incubated in a medium containing 20-µg/mL actinomycin D (CAS 50-76-0, Santa Cruz Biotechnology). After one additional hour, a 100-µL medium containing 20-µg/mL actinomycin D and a final concentration of 1-mM 5-ethynyl uridine (5-EU) (CLK-N002-10, Jena Bioscience, Jena, Germany) were added to the 2, 4, 6, 8, and 10 hpi time points. The cells were harvested at 0.5, 1, 2, 4, 6, 8, and 10 hpi, respectively; washed with PBS; and fixed with 4% paraformaldehyde in PBS for 20 min at RT. After washing with PBS, the cells were blocked and permeabilized with 1% BSA and 0.2% Triton X-100 in PBS overnight at 4 °C. To detect the incorporated 5-EU, a copper(I)-catalyzed alkyne-azide cycloaddition (CuAAC) reaction (also known as click chemistry) was performed. Therefore, the cells were incubated for 30 min with 1-mM CuSO4, 1-mM THPTA (CLK-1010, Jena Bioscience), 1-µM AF488-Picolyl-Azide (CLK-1276, Jena Bioscience), 10-mM sodium ascorbate, and 10% DMSO at RT in PBS in the dark. The cells were incubated with primary and secondary antibodies diluted in 1% BSA and 0.2% Triton X-100, with three washing steps with 0.1% Tween-20 in PBS after each antibody incubation. The viral nucleoprotein (N-3xFLAG) was stained with a rabbit polyclonal anti-DYKDDDDK tag antibody (PA1-984B, 1:1000; Thermo Fisher Scientific) and an anti-rabbit-Alexa555 antibody (A31572, 1:1000, Thermo Fisher Scientific). Double-stranded viral RNA (dsRNA) replication intermediates were stained with a monoclonal anti-dsRNA J2 antibody (IgG2a, RNT-SCI-10010200, 1:000; Jena Bioscience) and an anti-mouse IgG2a-Alexa647 antibody (A21242, 1:1000, Thermo Fisher Scientific). Hoechst 33342 (14533, 1:1000, Sigma-Aldrich) was used for the detection of cellular DNA. The coverslips were mounted on microscope slides in ProLong™ Glass Antifade Mountant (P36982, Thermo Fisher Scientific). The cells were visualized by confocal laser scanning microscopy (Leica TCS SP5 equipped with a 63x1.4 HCX PL APO CS oil immersion objective; Leica Microsystems, Wetzlar, Germany) and Leica Application Suite Advanced Fluorescence (Leica Microsystems); the obtained pictures were minimally processed with Adobe® Photoshop Elements 15 (Adobe, San Jose, CA, USA).
4.15. Reporter Stability Assay
CaCo-2 cells were seeded in a 12-well format and infected with P2 SARS-CoV-2 variants d6-YFP, d7-GFP, d7-Luc, d8-GFP, or after8-YFP at 1:2000 dilution. The viruses were passaged every two days on freshly seeded CaCo-2 cells, and the subgenomic RNA was isolated using TRI Reagent (R2050-1-50, Zymo Research, Freiburg, Germany) according to the manufacturer’s protocols. Five microliters of isolated RNA were utilized for the RT-qPCR. Therefore, the Universal Probe One-Step RT-qPCR kit (NEB) was used according to manufacturer’s instructions. For detection, RdRp-VIC, Luc-FAM, and YFP/GFP-FAM probes were used (
Table S1).