Overview of Dual-Acting Drug Methotrexate in Different Neurological Diseases, Autoimmune Pathologies and Cancers
Abstract
:1. Introduction
2. Methotrexate—Mechanisms of Drug Action
3. Methotrexate—Applications in Medicine
3.1. Methotrexate—Anti-Inflammatory and Immunosuppressive Drug
3.1.1. Methotrexate-Based Therapy of Myasthenia Gravis
3.1.2. Methotrexate-Based Therapy of Rheumatoid Arthritis
3.1.3. Methotrexate-Based Therapy of Alzheimer’s Disease
3.1.4. Methotrexate-Based Therapy of Other Diseases
3.2. Methotrexate—the Anti-Tumour Agent
3.2.1. Methotrexate-Based Therapy of Haematologic Malignancies
3.2.2. Central Nervous System—Methotrexate Brain Cancer Therapy and Brain Drug Delivery
3.2.3. Methotrexate-Based Therapy of Head and Neck
3.2.4. Methotrexate-Based Therapy of Breast Cancer
3.2.5. Methotrexate-Based Therapy of Lung Cancer
3.2.6. Methotrexate-Based Therapy of Prostate and Bladder Cancers
3.2.7. Methotrexate-Based Therapy of Osteosarcoma
3.2.8. Methotrexate-Based Therapy of Gestational Trophoblastic Disease
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| 5-FU | 5-fluorouracil |
| A1, A2A, A2B, A3 | Adenosine receptors |
| A549 | Human non-small cell lung carcinoma cell line |
| ACT | Dactinomycin, actinomycin D |
| AD | Alzheimer’s disease |
| ADA | Adenosine deaminase |
| AICART | 5-Aminoimidazole-4-carboxamide ribonucleotide transformylase |
| AICAR | 5-Aminoimidazole-4-carboxamide ribonucleotide |
| ALL | Acute lymphoblastic leukaemia |
| AML | Acute myelogenous leukaemia |
| AMP | Adenosine monophosphate |
| AMPDA | Adenosine monophosphate deaminase |
| Ara-C | Cytarabine, cytosine arabinoside |
| ASA | Acetylsalicylic acid, aspirin |
| ATCV | Anthracyclines-taxanes-capecitabine-vinorelin |
| ATP | Adenosine triphosphate |
| AZT | Azathioprine |
| BBB | Blood-brain barrier |
| BCD | Bleomycin-cyclophosphamide-dactinomycin |
| C225 | Cetuximab |
| cAMP | Cyclic adenosine monophosphate |
| CL1-0 | Human non-small cell lung carcinoma cell line |
| CD73 | ecto-5′-nucleotidase |
| CLL | Chronic lymphocytic leukaemia |
| CMF | Cyclophosphamide-methotrexate-5-fluorouracil |
| CMFEV | Cyclophosphamide-methotrexate-5-fluorouracil-epirubicin or vincristine |
| CML | Chronic myelogenous leukaemia |
| CMV | Cisplatin-methotrexate-vinblastine |
| CNS | Central nervous system |
| COB | Cisplatin-Oncovin(vincristine)-bleomycin |
| CXH | Chering Cross Hospital |
| DFS | Disease-free survival |
| DHFR | Dihydrofolate reductase |
| DIA | Cisplatin-ifosfamide-doxorubicin |
| DMARDs | Disease-modifying anti-rheumatic drugs |
| DNA | Deoxyribonucleic acid |
| dUMP | Deoxyuridine monophosphate |
| EMA | European Medicines Agency |
| EP-EMA | Etoposide-cisplatin + etoposiede-methotrexate-dactinomycin |
| EPR | Epirubicin |
| ER | Oestrogen receptor |
| FA | Folic acid |
| FAC | 5-Fluorouracil-Adriamycin-cyclophosphamide |
| FAICAR | 5-Formamidoimidazole- 4-carboxamide ribotide |
| FIGO | The International Federation of Gynecology and Obstetrics |
| FDA | The US Food and Drug Administration |
| FRs | Folate receptors |
| FPGS | Folylpolyglutamyl synthase |
| G5 | Generation 5 |
| GCS | Glucocorticosteroid |
| Glu | Glutamic acid |
| GMP | Guanosine monophosphate |
| GPI | Glycosyl-phosphatidyl-inositol |
| GTN | Gestational trophoblastic neoplasia |
| hCG | Human chorionic gonadotropin |
| HDMTX | High-dose methotrexate |
| HDMVAC | High-dose methotrexate-vinblastine-Adriamycin-cisplatin |
| HER2 | Human epidermal growth factor receptor-2 |
| HNSCC | Head and neck squamous cell carcinoma |
| HSA | Human serum albumin |
| IDMTX | Intermediate-dose methotrexate |
| IFN-γ | Interferon γ |
| IL | Interleukin |
| IMP | Inosine monophosphate |
| i.v. | Intravenous |
| LDMTX | Low-dose methotrexate |
| LLC | Murine epidermal lung carcinoma cell line |
| LV | Leucovorin, folinic acid |
| MACT | Methotrexate and dactinomycin |
| MAP | Methotrexate-doxorubicin-cisplatin |
| MF | Mycosis fungoides |
| MG | Myasthenia gravis |
| miRNA | microRNA |
| MLCC | Methotrexate-leucovorin-cyclophosphamide-cytosine arabinoside |
| MM | Mitomycin C and methotrexate |
| MNP | Mitomycin C-vinorelbine-cisplatinum |
| M-MNP | Methotrexate-mitomycin C-vinorelbine-cisplatinum |
| M-MVP | Methotrexate-mitomycin C-vinblastin-cisplatin |
| MOAC | Methotrexate-vincristine(Oncovin)-doxorubicin(Adriamycin)-cyclophosphamide |
| MS | Multiple sclerosis |
| MTX | Methotrexate |
| MUL | Methotrexate-tegafur-uracil-leucovorin |
| MVAC | Methotrexate-vinblastine-Adriamycin-cisplatin |
| MVP | Mitomycin C-vinblastin-cisplatin |
| NHL | Non-Hodgkin lymphoma |
| NP | Nanoparticulate |
| NSAIDs | Non-steroidal anti-inflammatory drugs |
| NSCLC | Non-small cell lung cancer |
| OR | Objective response |
| OS | Overall survival |
| PABA | p-Aminobenzoic acid |
| PAMAM | poly(Amidoamine) |
| PCFT | Proton-coupled folate transporter |
| PCNPs | PEGylated chitosan nanoparticles |
| PCNSL | Primary central nervous system lymphoma |
| PDD | Cisplatin, cis-diammindichloridoplatin |
| PEG | poly(Ethylene glycol) |
| PEPE | polyester-co-polyether |
| PFS | Progression-free survival |
| PIS | Prognostic index score |
| PLA | poly(lactic acid) |
| PLGA | poly(d,l-lactide-co-glycolide) |
| PMX | Pemetrexed |
| PR | Progesterone receptor |
| RA | Rheumatoid arthritis |
| R-CHOP | Rituximab-cyclophosphamide-doxorubicin-vincristine-prednisolone |
| RFC1 | Reduced folate carrier 1 |
| R-MAD | Rituximab-methotrexate-cytarabine-dexamethasone |
| R-MPV | Rituximab-methotrexate-procarbazine-vincristine |
| RNA | Ribonucleic acid |
| SCLC | Small cell lung cancer |
| S-SLM | Rat osteosarcoma cell line |
| TCC | Transitional cell carcinoma |
| THF | Tetrahydrofolate |
| TNBC | Triple-negative breast cancer |
| TNF-α | Tumour necrosis factor α |
| TYMS | Thymidylate synthase |
| UAPI | Uterine artery pulsatility index |
| UC | Urothelial cancer |
| WHO | World Health Organization |
References
- Farber, S. Some observations on the effect of folic acid antagonists on acute leukemia and other forms of incurable cancer. Blood 1949, 4, 160–167. [Google Scholar] [CrossRef] [Green Version]
- Gubner, R.; August, S.; Ginsberg, V. Therapeutic suppression of tissue reactivity. II. Effect of aminopterin in rheumatoid arthritis and psoriasis. Am. J. Med. Sci. 1951, 221, 176–182. [Google Scholar] [CrossRef]
- Edmundson, W.F.; Guy, W.B. Treatment of Psoriasis with Folic Acid Antagonists. AMA Arch. Derm. 1958, 78, 200–203. [Google Scholar] [CrossRef] [PubMed]
- Williams, H.J.; Willkens, R.F.; Samuelson, C.O., Jr.; Alarcon, G.S.; Guttadauria, M.; Yarboro, C.; Polisson, R.P.; Weiner, S.R.; Luggen, M.E.; Billingsley, L.M.; et al. Comparison of low-dose oral pulse methotrexate and placebo in the treatment of rheumatoid arthritis. A controlled clinical trial. Arthritis Rheum. 1985, 28, 721–730. [Google Scholar] [CrossRef]
- Weinstein, A.; Marlowe, S.; Korn, J.; Farouhar, F. Low-dose methotrexate treatment of rheumatoid arthritis. Long-term observations. Am. J. Med. 1985, 79, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Methotrexate Injection, USP. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/011719s125lbl.pdf (accessed on 2 January 2020).
- Methotrexate oral solution, FDA Full Prescribing Information. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/208004s002lbl.pdf (accessed on 2 January 2020).
- Frei, E., III; Jaffe, N.; Tattersall, M.H.N.; Pitman, S.; Parker, L. New Approaches to Cancer Chemotherapy with Methotrexate. N. Engl. J. Med. 1975, 292, 846–851. [Google Scholar] [CrossRef] [PubMed]
- Evans, W.E.; Crom, W.R.; Abromowitch, M.; Dodge, R.; Look, A.T.; Bowman, W.P.; George, S.L.; Pui, C.H. Clinical Pharmacodynamics of High-Dose Methotrexate in Acute Lymphocytic Leukemia. N. Engl. J. Med. 1986, 314, 471–477. [Google Scholar] [CrossRef] [PubMed]
- Natale, R.B.; Yagoda, A.; Watson, R.C.; Whitmore, W.F.; Blumenreich, M.; Braun, D.W., Jr. Methotrexate: An Active Drug in Bladder Cancer. Cancer 1981, 47, 1246–1250. [Google Scholar] [CrossRef]
- Huennekens, F.M. The methotrexate story: A paradigm for development of cancer chemotherapeutic agents. Advan. Enzym. Regul. 1994, 34, 397–419. [Google Scholar] [CrossRef]
- Bonadonna, G.; Valagussa, P.; Moliterni, A.; Zambetti, M.; Brambilla, C. Adjuvant Cyclophosphamide, Methotrexate, and Fluorouracil in Node-Positive Breast Cancer—The Results of 20 Years of Follow-up. N. Engl. J. Med. 1995, 332, 901–906. [Google Scholar] [CrossRef]
- Crews, K.R.; Liu, T.; Rodriguez-Galindo, C.; Tan, M.; Meyer, W.H.; Panetta, J.C.; Link, M.P.; Daw, N.C. High-dose methotrexate pharmacokinetics and outcome of children and young adults with osteosarcoma. Cancer 2004, 100, 1724–1733. [Google Scholar] [CrossRef] [PubMed]
- Tugwell, P.; Bennett, K.; Gent, M. Methotrexate in rheumatoid arthritis. Health and Public Policy Committee, American College of Physicians. Ann. Intern. Med. 1987, 107, 418–419. [Google Scholar]
- Cronstein, B.N. Low-Dose Methotrexate: A Mainstay in the Treatment of Rheumatoid Arthritis. Pharmacol. Rev. 2005, 57, 163–172. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roenigk, H.H., Jr.; Auerbach, R.; Maibach, H.I.; Weinstein, G.D. Methotrexate in psoriasis: Revised guidelines. J. Am. Acad. Dermatol. 1988, 19, 145–156. [Google Scholar] [CrossRef]
- Karaahmet, O.Z.; Bal, A.; Dulgeroglu, D.; Bahceci, H.K.; Cakci, A. Methotrexate treatment in myasthenia gravis. J. Clin. Neuromuscul. Dis. 2014, 16, 106–107. [Google Scholar] [CrossRef]
- Lémann, M.; Zenjari, T.; Bouhnik, Y.; Cosnes, J.; Mesnard, B.; Rambaud, J.C.; Modigliani, R.; Cortot, A.; Colombel, J.F. Methotrexate in Crohn’s disease: Long-term efficacy and toxicity. Am. J. Gastroenterol. 2000, 95, 1730–1734. [Google Scholar] [CrossRef]
- Goodkin, D.E.; Rudick, R.A.; VanderBrug Medendorp, S.; Daughtry, M.M.; Schwetz, K.M.; Fischer, J.; Van Dyke, C. Low-dose (7.5 mg) oral methotrexate reduces the rate of progression in chronic progressive multiple sclerosis. Ann. Neurol. 1995, 37, 30–40. [Google Scholar] [CrossRef]
- ACEP Clinical Policies Committee and the Clinical Policies Subcommittee on Early Pregnancy. Clinical policy: Critical issues in the initial evaluation and management of patients presenting to the emergency department in early pregnancy. Ann. Emerg. Med. 2003, 41, 123–133. [Google Scholar] [CrossRef]
- Jacobs, J.W. Optimal use of non-biologic therapy in the treatment of rheumatoid arthritis. Rheumatology (Oxford) 2012, 51 (Suppl. S4), iv3–iv8. [Google Scholar] [CrossRef] [Green Version]
- Singh, J.A.; Furst, D.E.; Bharat, A.; Curtis, J.R.; Kavanaugh, A.F.; Kremer, J.M.; Moreland, L.W.; O’Dell, J.; Winthrop, K.L.; Beukelman, T.; et al. 2012 update of the 2008 American College of Rheumatology recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of rheumatoid arthritis. Arthritis Care Res. (Hoboken) 2012, 64, 625–639. [Google Scholar] [CrossRef] [Green Version]
- Chattopadhyay, S.; Moran, R.G.; Goldman, I.D. Pemetrexed: Biochemical and cellular pharmacology, mechanisms, and clinical applications. Mol. Cancer. Ther. 2007, 6, 404–417. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matera, C.; Gomila, A.M.J.; Camarero, N.; Libergoli, M.; Soler, C.; Gorostiza, P. Photoswitchable Antimetabolite for Targeted Photoactivated Chemotherapy. J. Am. Chem. Soc. 2018, 140, 15764–15773. [Google Scholar] [CrossRef] [Green Version]
- Raimondi, M.V.; Randazzo, O.; La Franca, M.; Barone, G.; Vignoni, E.; Rossi, D.; Collina, S. DHFR Inhibitors: Reading the Past for Discovering Novel Anticancer Agents. Molecules 2019, 24, 1140. [Google Scholar] [CrossRef] [Green Version]
- Huschtascha, L.I.; Bartier, W.A.; Ross, C.E.; Tattersall, M.H.N. Characteristics of cancer cell death after exposure to cytotoxic drugs in vitro. Br. J. Cancer 1996, 73, 54–60. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chan, E.S.L.; Cronstein, B.N. Mechanism of Action of Methotrexate. Bull. Hosp. Jt. Dis. 2013, 71 (Suppl. S1), S5–S8. [Google Scholar]
- Genestier, L.; Paillot, R.; Quemeneur, L.; Izeradjene, K.; Revillard, J.P. Mechanisms of action of methotrexate. Immunopharmacology 2000, 47, 247–257. [Google Scholar] [CrossRef]
- Tian, H.; Cronstein, B.N. Understanding the mechanisms of action of methotrexate: Implications for the treatment of rheumatoid arthritis. Bull. NYU Hosp. Jt. Dis. 2007, 65, 168–173. [Google Scholar] [PubMed]
- Inoue, K.; Yuasa, H. Molecular Basis for Pharmacokinetics and Pharmacodynamics of Methotrexate in Rheumatoid Arthritis Treatment. Drug Metab. Pharmacokinet. 2014, 29, 12–19. [Google Scholar] [CrossRef] [Green Version]
- Matherly, L.H.; Goldman, D.I. Membrane transport of folates. In Vitamins and Hormones; Litwack, G., Ed.; Elsevier: Amsterdam, The Netherlands, 2003; Volume 66, pp. 403–456. [Google Scholar] [CrossRef]
- Sabharanjak, S.; Mayor, S. Folate receptor endocytosis and trafficking. Adv. Drug. Deliv. Rev. 2004, 56, 1099–1109. [Google Scholar] [CrossRef]
- Nogueira, E.; Sarria, M.P.; Azoia, N.G.; Antunes, E.; Loureiro, A.; Guimaraes, D.; Noro, J.; Rollett, A.; Guebitz, G.; Cavaco-Paulo, A. Internalization of Methotrexate Conjugates by Folate Receptor-α. Biochemistry 2018, 57, 6780–6786. [Google Scholar] [CrossRef] [Green Version]
- Baugh, C.M.; Krumdieck, C.L.; Nair, M.G. Polygammaglutamyl metabolites of methotrexate. Biochem. Biophys. Res. Commun. 1973, 52, 27–34. [Google Scholar] [CrossRef]
- Dervieux, T.; Furst, D.; Lein, D.O.; Capps, R.; Smith, K.; Walsh, M.; Kremer, J. Polyglutamation of methotrexate with common polymorphisms in reduced folate carrier, aminoimidazole carboxamide ribonucleotide transformylase, and thymidylate synthase are associated with methotrexate effects in rheumatoid arthritis. Arthritis Rheum. 2004, 50, 2766–2774. [Google Scholar] [CrossRef] [PubMed]
- Chabner, B.A.; Allegra, C.J.; Curt, G.A.; Clendeninn, N.J.; Baram, J.; Koizumi, S.; Drake, J.C.; Jolivet, J. Polyglutamation of methotrexate: Is methotrexate a prodrug? J. Clin. Invest. 1985, 76, 907–912. [Google Scholar] [CrossRef] [PubMed]
- Wu, K.M. A New Classification of Prodrugs: Regulatory Perspectives. Pharmaceuticals 2009, 2, 77–81. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Allegra, C.J.; Chabner, B.A.; Drake, J.C.; Lutz, R.; Rodbard, D.; Jolivet, J. Enhanced inhibition of thymidylate synthase by methotrexate polyglutamates. J. Biol. Chem. 1985, 260, 9720–9726. [Google Scholar]
- Baggott, J.E.; Vaughn, W.H.; Hudson, B.B. Inhibition of 5-aminoimidazole4-carboxamide ribotide transformylase, adenosine deaminase and 5’-adenylate deaminase by polyglutamates of methotrexate and oxidized folates and by 5-aminoimidazole-4-carboxamide riboside and ribotide. Biochem. J. 1986, 236, 193–200. [Google Scholar] [CrossRef] [Green Version]
- Allegra, C.J.; Drake, J.C.; Jolivet, J.; Chabner, B.A. Inhibition of phosphoribosylaminoimidazolecarboxamide transformylase by methotrexate and dihydrofolic acid polyglutamates. Proc. Natl. Acad. Sci. USA 1985, 82, 4881–4885. [Google Scholar] [CrossRef] [Green Version]
- Sant, M.E.; Lyons, S.D.; Phillips, L.; Christopherson, R.I. Antifolates Induce Inhibition of Amido Phosphoribosyltransferase in Leukemia. Cell J. Biol. Chem. 1992, 267, 11038–11045. [Google Scholar]
- Fairbanks, L.D.; Rückermann, K.; Qiu, Y.; Hawrylowicz, C.M.; Richards, D.F.; Swaminathan, R.; Kirschbaum, B.; Simmonds, H.A. Methotrexate Inhibits the First Committed Step of Purine Biosynthesis in Mitogen-Stimulated Human T-lymphocytes: A Metabolic Basis for Efficacy in Rheumatoid Arthritis? Biochem. J. 1999, 341, 143–152. [Google Scholar] [CrossRef]
- Genestier, L.; Paillot, R.; Fournel, S.; Ferraro, C.; Miossec, P.; Revillard, J.P. Immunosuppressive Properties of Methotrexate: Apoptosis and Clonal Deletion of Activated Peripheral T Cells. J. Clin. Invest. 1998, 102, 322–328. [Google Scholar] [CrossRef]
- Morabito, L.; Montesinos, M.C.; Schreibman, D.M.; Balter, L.; Thompson, L.F.; Resta, R.; Carlin, G.; Huie, M.A.; Cronstein, B.N. Methotrexate and Sulfasalazine Promote Adenosine Release by a Mechanism that Requires Ecto-59-nucleotidase–mediated Conversion of Adenine Nucleotides. J. Clin. Invest. 1998, 101, 295–300. [Google Scholar] [CrossRef] [PubMed]
- Montesinos, M.C.; Desai, A.; Delano, D.; Chen, J.F.; Fink, J.S.; Jacobson, M.A.; Cronstein, B.N. Adenosine A2A or A3 receptors are required for inhibition of inflammation by methotrexate and its analog MX-68. Arthritis Rheum. 2003, 48, 240–247. [Google Scholar] [CrossRef] [PubMed]
- Varani, K.; Vincenzi, F.; Tosi, A.; Targa, M.; Masieri, F.F.; Ongaro, A.; De Mattei, M.; Massari, L.; Borea, P.A. Expression and Functional Role of Adenosine Receptors in Regulating Inflammatory Responses in Human Synoviocytes. Br. J. Pharmacol. 2010, 160, 101–115. [Google Scholar] [CrossRef] [Green Version]
- Stamp, L.K.; Hazlett, J.; Roberts, R.L.; Frampton, C.; Highton, J.; Hessian, P.A. Adenosine receptor expression in rheumatoid synovium: A basis for methotrexate action. Arthritis Res. Ther. 2012, 14, R138. [Google Scholar] [CrossRef] [Green Version]
- Vincenzi, F.; Padovan, M.; Targa, M.; Corciulo, C.; Giacuzzo, S.; Merighi, S.; Gessi, S.; Govoni, M.; Borea, P.A.; Varani, K. A2A Adenosine Receptors Are Differentially Modulated by Pharmacological Treatments in Rheumatoid Arthritis Patients and Their Stimulation Ameliorates Adjuvant-Induced Arthritis in Rats. PLoS ONE 2013, 8, e54195. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cronstein, B.N.; Eberle, M.A.; Gruber, H.E.; Levin, R.I. Methotrexate inhibits neutrophil function by stimulating adenosine release from connective tissue cells. Proc. Natl. Acad. Sci. USA 1991, 88, 2441–2445. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cronstein, B.N.; Levin, R.I.; Belanoff, J.; Weissmann, G.; Hirschhorn, R. Adenosine: An endogenous inhibitor of neutrophil-mediated injury to endothelial cells. J. Clin. Invest. 2001, 78, 760–770. [Google Scholar] [CrossRef]
- Leroux, J.L.; Damon, M.; Chavis, C.; Crates de Paulet, A.; Blotman, F. Effects of methotrexate on leukotriene and derivated lipoxygenase synthesis in polynuclear neutrophils in rheumatoid polyarthritis. Rev. Rheum. Mal. Osteoartic. 1992, 59, 587–591. [Google Scholar]
- Brody, M.; Bohm, I.; Bauer, R. Mechanism of action of methotrexate: Experimental evidence that methotrexate blocks the binding of interleukin-1 beta to the interleukin-1 receptor on target cells. Eur. J. Chem. Clin. Biochem. 1993, 31, 667–674. [Google Scholar] [CrossRef] [Green Version]
- Bouma, M.G.; Stad, R.K.; van der Wildenberg, F.A.J.M.; Buurman, W.A. Differential regulatory effects of adenosine on cytokine release by activated human monocytes. J. Immunol. 1994, 153, 4159–4168. [Google Scholar]
- Becker, C.; Barbulescu, K.; Hildner, K.; Meyer zum Buschenfelde, K.H.; Neurath, M.F. Activation and methotrexate-mediated suppression of the TNF alpha promoter in T cells and macrophages. Ann. N. Y. Acad. Sci. 1998, 859, 311–314. [Google Scholar] [CrossRef] [PubMed]
- Constantin, A.; Loubet-Lescoulie, P.; Lambert, N.; Yassine-Diab, B.; Abbal, M.; Mazieres, B.; de Preval, C.; Cantagrel, A. Antiinflammatory and immunoregulatory action of methotrexate in the treatment of rheumatoid arthritis: Evidence of increased interleukin-4 and interleukin-10 gene expression demonstrated in vitro by competitive reverse transcriptase-polymerase chain reaction. Arthritis Rheum. 1998, 41, 48–57. [Google Scholar] [CrossRef] [PubMed]
- Hasko, G.; Cronstein, B.N. Adenosine: An endogenous regulator of innate immunity. Trends Immunol. 2004, 25, 33–39. [Google Scholar] [CrossRef] [PubMed]
- Bouma, M.G.; van der Wildenberg, F.A.; Buurman, W.A. Adenosine inhibits cytokine release and expression of adhesion molecules by activated human endothelial cells. Am. J. Physiol. 1996, 270, C522–C529. [Google Scholar] [CrossRef] [PubMed]
- Nesher, G.; Moore, T.L. The in vitro effects of methotrexate on peripheral blood mononuclear cells. Modulation by methyl donors and spermidine. Arthritis Rheum. 1990, 33, 954–959. [Google Scholar] [CrossRef]
- Yukioka, K.; Wakitani, S.; Yukioka, M.; Furumitsu, Y.; Shichikawa, K.; Ochi, T.; Goto, H.; Matsui-Yuasa, I.; Otani, S.; Nishizawa, Y. Polyamine levels in synovial tissues and synovial fluids of patients with rheumatoid arthritis. J. Rheumatol. 1992, 19, 689–692. [Google Scholar]
- Nesher, G.; Osborn, T.G.; Moore, T.L. In vitro effects of methotrexate on polyamine levels in lymphocytes from rheumatoid arthritis patients. Clin. Exp. Rheumatol. 1996, 14, 395–399. [Google Scholar]
- Nesher, G.; Osborn, T.G.; Moore, T.L. Effect of treatment with methotrexate, hydroxychloroquine, and prednisone on lymphocyte polyamine levels in rheumatoid arthritis: Correlation with the clinical response and rheumatoid factor synthesis. Clin. Exp. Rheumatol. 1997, 15, 343–347. [Google Scholar]
- Wong, P.T.; Choi, S.K. Mechanisms and Implications of Dual-Acting Methotrexate in Folate-Targeted Nanotherapeutic Delivery. Int. J. Mol. Sci. 2015, 16, 1772–1790. [Google Scholar] [CrossRef] [Green Version]
- Theti, D.S.; Jackman, A.L. The Role of α-Folate Receptor-Mediated Transport in the Antitumor Activity of Antifolate Drugs. Clin. Cancer Res. 2004, 10, 1080–1089. [Google Scholar] [CrossRef] [Green Version]
- Kerschbaumer, A.; Sepriano, A.; Smolen, J.S.; van der Heijde, D.; Dougados, M.; van Vollenhoven, R.; McInnes, I.B.; Bijlsma, J.W.J.; Burmester, G.R.; de Wit, M.; et al. Efficacy of pharmacological treatment in rheumatoid arthritis: A systematic literature research informing the 2019 update of the EULAR recommendations for management of rheumatoid arthritis. Ann. Rheum. Dis. 2020, 1–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Smolen, J.S.; Aletaha, D.; Bijlsma, J.W.; Breedveld, F.C.; Boumpas, D.; Burmester, G.; Combe, B.; Cutolo, M.; de Wit, M.; Dougados, M.; et al. Treating rheumatoid arthritis to target: Recommendations of an international task force. Ann. Rheum. Dis. 2010, 69, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Díaz-Manera, J.; García, R.R.; Illa, I. Treatment strategies for myasthenia gravis: An update. Expert Opin. Pharmacother. 2012, 13, 1873–1883. [Google Scholar] [CrossRef] [PubMed]
- Gotterer, L.; Li, Y. Maintenance immunosuppression in myasthenia gravis. J. Neurol. Sci. 2016, 369, 294–302. [Google Scholar] [CrossRef] [PubMed]
- Chantam, W. Rheumatic manifestations of systemic disease: Sarcoidosis. Curr. Opin. Rheumatol. 2010, 22, 85–90. [Google Scholar] [CrossRef]
- Baughman, R.P.; Lower, E.E. A clinical approach to the use of methotrexate for sarcoidosis. Thorax 1999, 54, 742–746. [Google Scholar] [CrossRef] [Green Version]
- Mahr, A.D.; Jover, J.A.; Spiera, R.F.; Hernández-García, C.; Fernández-Gutiérrez, B.; LaValley, M.P.; Merkel, P.A. Adjunctive Methotrexate for Treatment of Giant Cell Arteritis. An Individual Patient Data Meta-Analysis. Arthritis Rheum. 2007, 56, 2789–2797. [Google Scholar] [CrossRef]
- Ferrara, G.; Mastrangelo, G.; Barone, P.; La Torre, F.; Martino, S.; Pappagallo, G.; Ravelli, A.; Taddio, A.; Zulian, F.; Cimaz, R. Methotrexate in juvenile idiopathic arthritis: Advice and recommendations from the MARAJIA expert consensus meeting. Pediatr. Rheumatol. 2018, 16, 46. [Google Scholar] [CrossRef] [Green Version]
- Joshi, P.; Dhaneshwar, S.S. An update on Disease Modifying Antirheumatic drugs. Inflamm. Allergy Drug Target 2014, 13, 249–261. [Google Scholar] [CrossRef]
- Gilhus, N.E. Myasthenia and the neuromuscular junction. Curr. Opin. Neurol. 2012, 25, 523–529. [Google Scholar] [CrossRef]
- Andersen, J.B.; Heldal, A.T.; Engeland, A.; Gilhus, N.E. Myasthenia gravis epidemiology in a national cohort; combining multiple disease registries. Acta Neurol. Scand. 2014, 129, 26–31. [Google Scholar] [CrossRef]
- Gilhus, N.E.; Hong, Y. Maternal myasthenia gravis represents a risk for the child through autoantibody transfer, immunosuppressive therapy and genetic influence. Eur. J. Neurol. 2018, 25, 1402–1409. [Google Scholar] [CrossRef] [PubMed]
- Kupersmith, M.J.; Latkany, R.; Homel, P. Development of generalized disease at 2 years in patients with ocular myasthenia gravis. Arch. Neurol. 2003, 60, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Sathasivam, S. Steroids and immunosuppressant drugs in myasthenia gravis. Nat. Clin. Pract. Neurol. 2008, 4, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Higuchi, O.; Hamuro, J.; Motomura, M.; Yamanashi, Y. Autoantibodies to low density lipoprotein receptor-related protein 4 in myasthenia gravis. Ann. Neurol. 2011, 69, 418–422. [Google Scholar] [CrossRef]
- Grob, D.; Brunner, N.; Namba, T.; Pagala, M. Lifetime course of myasthenia gravis. Muscle Nerve 2008, 37, 141–149. [Google Scholar] [CrossRef] [PubMed]
- Kostera-Pruszczyk, A.; Kamińska, A.; Dutkiewicz, M.; Emeryk-Szajewska, B.; Strugalska-Cynowska, M.H.; Vincent, A.; Kwieciński, H. MuSK-positive myasthenia gravis is rare in the Polish population. Eur. J. Neurol. 2008, 15, 720–724. [Google Scholar] [CrossRef]
- Morren, J.; Li, Y. Maintenance immunosuppression in myasthenia gravis, an update. J. Neurol. Sci. 2020, 410, 116648. [Google Scholar] [CrossRef]
- Gold, R.; Hohlfeld, R.; Toyka, K.V. Progress in the treatment of myasthenia gravis. Ther. Adv. Neurol. Disord. 2008, 1, 99–114. [Google Scholar] [CrossRef] [Green Version]
- Sathasivam, S. Current and emerging treatments for the management of myasthenia gravis. Ther. Clin. Risk Manag. 2011, 7, 313–323. [Google Scholar] [CrossRef] [Green Version]
- Urban, P.P.; Jacobi, C.; Jander, S. Treatment Standards and Individualized Therapy of Myasthenia Gravis. Neurol. Int. Open 2018, 2, E84–E92. [Google Scholar] [CrossRef] [Green Version]
- Sieb, J.P. Myasthenia gravis: An update for the clinician. Clin. Exp. Immunol. 2014, 175, 408–418. [Google Scholar] [CrossRef] [PubMed]
- Hartmann, J.; Rivner, M.H. Methotrexate in myasthenia gravis. Clin. Neurophysiol. 2009, 120, e123–e124. [Google Scholar] [CrossRef]
- Gold, R.; Schneider-Gold, C. Current and future standards in treatment of myasthenia gravis. Neurotherapeutics 2008, 5, 535–541. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdou, A.M. Methotrexate for treatment of myasthenia gravis. Neurology 2007, 62 (Suppl. S1), 300–301. [Google Scholar]
- Heckmann, J.M.; Rawoot, A.; Bateman, K.; Renison, R.; Badri, M. A single-blinded trial of methotrexate versus azathioprine as steroid-sparing agents in generalized myasthenia gravis. BMC Neurol. 2011, 11, 97. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pasnoor, M.; He, J.; Herbelin, L.; Burns, T.M.; Nations, S.; Bril, V.; Wang, A.K.; Elsheikh, B.H.; Kissel, J.T.; Saperstein, D.; et al. Methotrexate in MG Investigators of the Muscle Study Group. A randomized controlled trial of methotrexate for patients with generalized myasthenia gravis. Neurology 2016, 87, 57–64. [Google Scholar] [CrossRef] [Green Version]
- Smolen, J.S.; Aletaha, D.; McInnes, I.B. Rheumatoid arthritis. Lancet 2016, 388, 2023–2038. [Google Scholar] [CrossRef]
- Alamanos, Y.; Drosos, A.A. Epidemiology of adult rheumatoid arthritis. Autoimmun. Rev. 2005, 4, 130–136. [Google Scholar] [CrossRef]
- Kumar, P.; Yao, L.J.; Said, S.; Paleja, B.; van Loosdregt, J.; Chua, C.; Arkachaisri, T.; Consolaro, A.; Gattorno, M.; Martini, A.; et al. Molecular mechanisms of autophagic memory in pathogenic T cells in human arthritis. J. Autoimmun. 2018, 94, 90–98. [Google Scholar] [CrossRef]
- Mellado, M.; Martínez-Muñoz, L.; Cascio, G.; Lucas, P.; Pablos, J.L.; Rodríguez-Frade, J.M. T Cell Migration in Rheumatoid Arthritis. Front. Immunol. 2015, 6, 384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lipsky, P.E.; van der Heijde, D.M.; St Clair, E.W.; Furst, D.E.; Breedveld, F.C.; Kalden, J.R.; Smolen, J.S.; Weisman, M.; Emery, P.; Feldmann, M.; et al. Infliximab and methotrexate in the treatment of rheumatoid arthritis. N. Engl. J. Med. 2000, 343, 1594–1602. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feldmann, M.; Brennan, F.M.; Foxwell, B.M.; Maini, R.N. The role of TNF alpha and IL-1 in rheumatoid arthritis. Curr. Dir. Autoimmun. 2001, 3, 188–199. [Google Scholar] [CrossRef]
- Farrugia, M.; Baron, B. The role of TNF-α in rheumatoid arthritis: A focus on regulatory T cells. J. Clin. Transl. Res. 2016, 2, 84–90. [Google Scholar] [CrossRef] [PubMed]
- Ponchel, F.; Burska, A.N.; Hunt, L.; Gul, H.; Rabin, T.; Parmar, R.; Buch, M.H.; Conaghan, P.G.; Emery, P. T-cell subset abnormalities predict progression along the Inflammatory Arthritis disease continuum: Implications for management. Sci. Rep. 2020, 10, 3669. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Furst, D.E.; Koehnke, R.; Burmeister, L.F.; Kohler, J.; Cargill, I. Increasing methotrexate effect with increasing dose in the treatment of resistant rheumatoid arthritis. J. Rheumatol. 1989, 16, 313–320. [Google Scholar]
- Weinblatt, M.E. Methotrexate in rheumatoid arthritis: A quarter century of development. Trans. Am. Clin. Climatol. Assoc. 2013, 124, 16–25. [Google Scholar]
- Kaneko, Y.; Atsumi, T.; Tanaka, Y.; Inoo, M.; Kobayashi-Haraoka, H.; Amano, K.; Miyata, M.; Murakawa, Y.; Yasuoka, H.; Hirata, S.; et al. Comparison of adding tocilizumab to methotrexate with switching to tocilizumab in patients with rheumatoid arthritis with inadequate response to methotrexate: 52-week results from a prospective, randomised, controlled study (SURPRISE study). Ann. Rheum. Dis. 2016, 75, 1917–1923. [Google Scholar] [CrossRef]
- Hazlewood, G.S.; Barnabe, C.; Tomlinson, G.; Marshall, D.; Devoe, D.; Bombardier, C. Methotrexate monotherapy and methotrexate combination therapy with traditional and biologic disease modifying antirheumatic drugs for rheumatoid arthritis: Abridged Cochrane systematic review and network meta-analysis. BMJ 2016, 353, i1777. [Google Scholar] [CrossRef] [Green Version]
- McGeer, P.L.; Rogers, J.; McGeer, E.G.; Sibley, J. Anti-inflammatory drugs and Alzheimer disease. Lancet 1990, 335, 1037. [Google Scholar] [CrossRef]
- Judge, A.; Garriga, C.; Arden, N.K.; Lovestone, S.; Prieto-Alhambra, D.; Cooper, C.; Edwards, C.J. Protective effect of antirheumatic drugs on dementia in rheumatoid arthritis patients. Alzheimers Dement. 2017, 3, 612–621. [Google Scholar] [CrossRef] [PubMed]
- Zhou, M.; Xu, R.; Kaelber, D.C.; Gurney, M.E. Tumor Necrosis Factor (TNF) blocking agents are associated with lower risk for Alzheimer’s disease in patients with rheumatoid arthritis and psoriasis. PLoS ONE 2020, 15, e0229819. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chou, R.C.; Kane, M.; Ghimire, S.; Gautam, S.; Gui, J. Treatment for Rheumatoid Arthritis and Risk of Alzheimer’s Disease: A Nested Case-Control Analysis. CNS Drugs 2016, 30, 1111–1120. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haustein, U.F.; Rytter, M. Methotrexate in psoriasis: 26 years’ experience with low-dose long-term treatment. J. Eur. Acad. Dermatol. Venereol. 2000, 14, 382–388. [Google Scholar] [CrossRef] [PubMed]
- Shen, S.; O’Brien, T.; Yap, L.M.; Prince, H.M.; McCormack, C.J. The use of methotrexate in dermatology: A review. Australas. J. Dermatol. 2012, 53, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, G.D. Methotrexate. Ann. Intern. Med. 1977, 86, 199–204. [Google Scholar] [CrossRef]
- Busger op Vollenbroek, F.T.M.; Doggen, C.J.M.; Janssens, R.W.A.; Bernelot Moens, H.J. Dermatological guidelines for monitoring methotrexate treatment reduce drug-survival compared to rheumatological guidelines. PLoS ONE 2018, 13, e0194401. [Google Scholar] [CrossRef] [Green Version]
- Berthelot, C.; Rivera, A.; Duvic, M. Skin directed therapy for mycosis fungoides: A review. J. Drugs Dermatol. 2008, 7, 655–666. [Google Scholar]
- Kanwar, A.J.; De, D. Methotrexate for treatment of lichen planus: Old drug, new indication. J. Eur. Acad. Dermatol. Venereol. 2013, 27, e410–e413. [Google Scholar] [CrossRef]
- Puza, C.; Cardones, A.R. Concepts and controversies in the treatment of cutaneous lichen planus. G. Ital. Dermatol. Venereol. 2017, 152, 607–614. [Google Scholar] [CrossRef]
- Schutt, A.C.; Bullington, W.M.; Judson, M.A. Pharmacotherapy for pulmonary sarcoidosis: A Delphi consensus study. Respir. Med. 2010, 104, 717–723. [Google Scholar] [CrossRef] [Green Version]
- Baughman, R.P.; Culver, D.A.; Judson, M.A. A concise review of pulmonary sarcoidosis. Am. J. Respir. Crit. Care Med. 2011, 183, 573–581. [Google Scholar] [CrossRef] [Green Version]
- Goljan-Geremek, A.; Bednarek, M.; Franczuk, M.; Puścińska, E.; Nowiński, A.; Czystowska, M.; Kamiński, D.; Korzybski, D.; Stokłosa, A.; Kowalska, A.; et al. Methotrexate as a single agent for treating pulmonary sarcoidosis: A single centre real-life prospective study. Pneumonol. Alergol. Pol. 2014, 82, 518–533. [Google Scholar] [CrossRef] [PubMed]
- Feagan, B.G.; Rochon, J.; Fedorak, R.N.; Irvine, E.J.; Wild, G.; Sutherland, L.; Steinhart, A.H.; Greenberg, G.R.; Gillies, R.; Hopkins, M.; et al. Methotrexate for the treatment of Crohn’s disease. N. Engl. J. Med. 1995, 332, 292–297. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Feagan, B.G.; Fedorak, R.N.; Irvine, E.J.; Wild, G.; Sutherland, L.; Steinhart, A.H.; Greenberg, G.R.; Koval, J.; Wong, C.J.; Hopkins, M.; et al. A comparison of methotrexate with placebo for the maintenance of remission in Crohn’s disease. N. Engl. J. Med. 2000, 342, 1627–1632. [Google Scholar] [CrossRef] [PubMed]
- Compston, A. The 150th anniversary of the first depiction of the lesions of multiple sclerosis. J. Neurol. Neurosurg. Psychiatry. 1988, 51, 1249–1252. [Google Scholar] [CrossRef] [Green Version]
- Compston, A.; Coles, A. Multiple sclerosis. Lancet 2008, 372, 1502–1517. [Google Scholar] [CrossRef]
- Calabresi, P.A.; Wilterdink, J.L.; Rogg, J.M.; Mills, P.; Webb, A.; Whartenby, K.A. An open-label trial of combination therapy with interferon beta-1a and oral methotrexate in MS. Neurology 2002, 58, 314–317. [Google Scholar] [CrossRef]
- Ashtari, F.; Savoj, M.R. Effects of low dose methotrexate on relapsing-remitting multiple sclerosis in comparison to Interferon β-1α: A randomized controlled trial. J. Res. Med. Sci. 2011, 16, 457–462. [Google Scholar]
- Stark, J.W.; Josephs, L.; Dulak, D.; Clague, M.; Sadiq, S.A. Safety of long-term intrathecal methotrexate in progersive forms of MS. Ther. Adv. Neurol. Disord. 2019, 12, 1–8. [Google Scholar] [CrossRef]
- Swerdlow, S.H. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissue, 4th ed.; International Agency for Research on Cancer: Lyon, France, 2008; (updated in 2016). [Google Scholar]
- Quintanilla-Martinez, L. The 2016 updated WHO classification of lymphoid neoplasias. Hematol. Oncol. 2017, 35 (Suppl. S1), 37–45. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Khan, Z.A.; Tripathi, R.; Mishra, B. Methotrexate: A detailed review on drug delivery and clinical aspects. Expert Opin. Drug Deliv. 2012, 9, 151–169. [Google Scholar] [CrossRef] [PubMed]
- Karami, F.; Ranjbar, S.; Ghasemi, Y.; Negahdaripour, M. Analytical methodologies for determination of methotrexate and its metabolites in pharmaceutical, biological and environmental samples. J. Pharm. 2019, 9, 373–391. [Google Scholar] [CrossRef] [PubMed]
- Mantadakis, E.; Cole, P.D.; Kamen, B.A. High-Dose Methotrexate in Acute Lymphoblastic Leukemia: Where Is the Evidence for Its Continued Use? Pharmacotherapy 2005, 25, 748–755. [Google Scholar] [CrossRef] [PubMed]
- Kamel, O.W. Lymphomas during Long-term Methotrexate Therapy. Arch. Dermatol. 1997, 133, 903–904. [Google Scholar] [CrossRef] [PubMed]
- Paul, C.; Le Tourneau, A.; Cayuela, J.M.; Devidas, A.; Robert, C.; Molinie, V.; Dubertret, L. Epstein-Barr Virus-Associated Lymphoproliferative Disease During Methotrexate Therapy for Psoriasis. Arch. Dermatol. 1997, 133, 867–871. [Google Scholar] [CrossRef]
- Alpdogan, O.; Kartan, S.; Johnson, W.; Sokol, K.; Porcu, P. Systemic therapy of cutaneous T-cell lymphoma (CTCL). Chin. Clin. Oncol. 2019, 8, 10. [Google Scholar] [CrossRef]
- Zackheim, H.S.; Kashani-Sabet, M.; McMillan, A. Low-dose methotrexate to treat mycosis fungoides: A retrospective study in 69 patients. J. Am. Acad. Dermatol. 2003, 49, 873–878. [Google Scholar] [CrossRef]
- Whittaker, S.; Hoppe, R.; Prince, H.M. How I treat mycosis fungoides and Sèzary syndrome. Blood 2016, 127, 3142–3153. [Google Scholar] [CrossRef] [Green Version]
- Olek-Hrab, K.; Maj, J.; Chmielowska, E.; Jankowska-Konsur, A.; Olszewska, B.; Kręcisz, B.; Iwankowski, P.; Mackiewicz-Wysocka, M.; Adamski, Z.; Nowicki, R.; et al. Methotrexate in the treatment of mycosis fungoides-a multicenter observational study in 79 patients. Eur. Rev. Med. Pharmacol. Sci. 2018, 22, 3586–3594. [Google Scholar] [CrossRef]
- Guo, Y.; Ahn, M.J.; Chan, A.; Wang, C.-H.; Kang, J.-H.; Kim, S.-B.; Bello, M.; Arora, R.S.; Zhang, Q.; He, X.; et al. Afatinib versus methotrexate as second-line treatment in Asian patients with recurrent or metastatic squamous cell carcinoma of the head and neck progressing on or after platinum-based therapy (LUX-Head & Neck 3): An open-label, randomised phase III trial. Ann. Oncol. 2019, 30, 1831–1839. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Maiti, R. Metronomic chemotherapy. J. Pharmacol. Pharmacother. 2014, 5, 186–192. [Google Scholar] [CrossRef] [Green Version]
- Wen, J.; Ma, X.; Ruan, D.; Chen, J.; Lin, Q.; Dong, M.; Li, H.; Wu, H. The efficacy of metronomic thalimomide and methotrexate for refractory/relapsed non-Hodgkin lymphoma. J. Clin. Oncol. 2014, 32. [Google Scholar] [CrossRef]
- Bertino, J.B.; Mosher, M.B.; DeConti, R.C. Chemotherapy of cancer of the head and neck. Cancer 1973, 31, 1141–1149. [Google Scholar] [CrossRef]
- Chang, P.M.H.; Teng, H.W.; Chen, P.M.; Chang, S.Y.; Chu, P.Y.; Tsai, T.L.; Tai, S.K.; Wang, Y.F.; Huang, J.L.; Yang, M.H. Methotrexate and Leucovorin Double-Modulated 5-fluorouracil Combined With Cisplatin (MPFL) in Metastatic/Recurrent Head and Neck Cancer. J. Chin. Med. Assoc. 2008, 71, 336–341. [Google Scholar] [CrossRef] [Green Version]
- Kushwaha, V.S.; Gupta, S.; Husain, N.; Khan, H.; Negi, M.P.S.; Jamal, N.; Ghatak, A. Gefitinib, Methotrexate and Methotrexate plus 5-Fluorouracil as palliative treatment in recurrent head and neck squamous cell carcinoma. Cancer Biol. Ther. 2015, 16, 346–351. [Google Scholar] [CrossRef] [Green Version]
- Pai, P.S.; Vaidya, A.D.; Prabhash, K.; Banavali, S.D. Oral metronomic scheduling of anticancer therapy-based treatment compared to existing standard of care in locally advanced oral squamous cell cancers: A matched-pair analysis. Indian J. Cancer 2013, 50, 135–141. [Google Scholar] [CrossRef]
- Kumar, K.S.S.; Arumugam, V. Outcome of Oral Metronomic Therapy with Methotrexate and Celecoxib in Advanced/Recurrent Head and Neck Squamous Cell Carcinoma. Int. J. Sci. Study 2019, 6, 203–208. [Google Scholar]
- Mateen, A.; Adil, A.R.; Maken, R.N.; Khan, S.A.; Arif, M. Metronomic chemotherapy in recurrent head and neck cancer. J. Clin. Oncol. 2015, 33 (Suppl. abstr), e17007. [Google Scholar] [CrossRef]
- Denis, D.; Beneton, N.; Laribi, K.; Maillard, H. Management of mycosis fungoides-type cutaneous T-cell lymphoma (MF-CTCL): Focus on chlormethine gel. Cancer Manag. Res. 2019, 20, 2241–2251. [Google Scholar] [CrossRef] [Green Version]
- Aviles, A.; Neri, N.; Fernandez-Diez, J.; Silva, L.; Nambo, M. Interferon and low doses of methotrexate versus interferon and retinoids in the treatment of refractory/relapsed cutaneous T-cell lymphoma. Hematology 2015, 20, 538–542. [Google Scholar] [CrossRef] [PubMed]
- Wood, G.S.; Wu, J. Methotrexate and Pralatrexate. Dermatol. Clin. 2015, 33, 747–755. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aviles, A.; Nambo, M.J.; Neri, N.; Castañeda, C.; Cleto, S.; Gonzalez, M.; Huerta-Guzmán, J. Interferon and low dose methotrexate improve outcome in refractory mycosis fungoides/Sézary syndrome. Cancer Biother. Radiopharm. 2007, 22, 836–840. [Google Scholar] [CrossRef] [PubMed]
- Kuo, Y.-H.; Chang, C.-H. Erythrodermic mycosis fungoides treated with low-dose methotrexate and 311 nm UV-B: A case report with 3-year follow up and literature review. Dermatol. Sin. 2016, 34, 37–41. [Google Scholar] [CrossRef] [Green Version]
- Raychaudhury, T. Management strategies for mycosis fungoides in India. Indian J. Dermatol. 2017, 62, 137–141. [Google Scholar] [CrossRef]
- Zakem, M.H.; Davis, B.R.; Adelstei, D.J.; Hines, J.D. Treatment of advanced stage mycosis fungoides with bleomycin, doxorubicin, and methotrexate with topical nitrogen mustard (BAM-M). Cancer 1986, 58, 2611–2616. [Google Scholar] [CrossRef]
- Vincent, R.G.; Wilson, H.E.; Lane, W.W.; Chen, T.Y.; Raza, S.; Gutierrez, A.C.; Caracandas, J.E. Progress in the Chemotherapy of Small Cell. Carcinoma of the Lung. Cancer 1981, 47, 229–235. [Google Scholar] [CrossRef]
- Hande, K.R.; Oldham, R.K.; Fer, M.F.; Richardson, R.L.; Greco, F.A. Randomized study of high-dose versus low-dose methotrexate in the treatment of extensive small cell lung cancer. Am. J. Med. 1982, 73, 413–419. [Google Scholar] [CrossRef]
- Neijstrom, E.S.; Capizzi, R.L.; Rudnick, S.A.; Kirsch, M.; Delaney, D.; Kahn, L.; Lipper, S.; Carney, C. High-dose methotrexate in small cell lung cancer. Lack of efficacy in preventing CNS relapse. Cancer 1983, 51, 1056–1061. [Google Scholar] [CrossRef]
- Preiss, R.; Brovtsyn, V.K.; Perevodchikova, N.L.; Bychkov, M.B.; Hüller, H.; Belova, L.A.; Michailov, P. Effect of methotrexate on the pharmacokinetics and renal excretion of cisplatin. Eur. J. Clin. Pharmacol. 1988, 34, 139–144. [Google Scholar] [CrossRef]
- Malzyner, A.; Caponero, R.; Donato, E.M.; Nadalin, W.; Vargas, F.S. Methotrexate (MTX), mitomycin C (MMC), vinorelbine (M) and cisplatinum (P) [M-MNP] in the treatment of advanced non-small cell lung cancer (NSCLC). Lung Cancer 1994, 11, 123. [Google Scholar] [CrossRef]
- Hall, R.R.; Bloom, H.J.G.; Freeman, J.E.; Nawrocki, A.; Wallace, D.M. Methotrexate Treatment for Advanced Bladder Cancer. Br. J. Urol. 1974, 46, 431–438. [Google Scholar] [CrossRef] [PubMed]
- Andrews, M.C.; Wilson, W.L. Phase II study of methotrexate (NSC-740) in solid tumors. Cancer Chemother. Rep. 1976, 51, 471–474. [Google Scholar]
- Turner, A.G.; Hendry, W.F.; Williams, G.B.; Bloom, H.J.G. The Treatment of Advanced Bladder Cancer with Methotrexate. Br. J. Urol. 1977, 49, 673–678. [Google Scholar] [CrossRef]
- Kaye, S.B.; McWhinnie, D.; Hart, A.; Deane, R.F.; Billaert, P.; Welsh, J.; Milsted, R.V.; Stuart, J.F.B.; Kalman, K.C. The treatment of advanced bladder cancer with methotrexate and cisplatinum—A pharmacokinetic study. Eur. J. Cancer Clin. Oncol. 1984, 20, 249–252. [Google Scholar] [CrossRef]
- Newling, D.W.W.; Stoter, G.; Sylvester, R.; de Pauw, M. The chemotherapy of advanced bladder cancer. Cancer Chemother. Pharmacol. 1987, 20, S39–S43. [Google Scholar] [CrossRef]
- Ismaili, N.; Amzerin, M.; Flechon, A. Chemotherapy in advanced bladder cancer: Current status and future. J. Hematol. Oncol. 2011, 4, 35. [Google Scholar] [CrossRef] [Green Version]
- Pavone-Macaluso, M.; Sternberg, C. Second-Line Chemotherapy in Advanced Bladder Cancer. Urol. Int. 2000, 64, 61–69. [Google Scholar] [CrossRef]
- Ahmed, T.; Yagoda, A.; Needles, B.; Scher, H.I.; Watson, R.C.; Geller, N. Vinblastine and methotrexate for advanced bladder cancer. J. Urol. 1985, 133, 602–604. [Google Scholar] [CrossRef]
- Sinha, A.K.; Anand, S.; Ortel, B.J.; Chang, Y.; Mai, Z.; Hasan, T.; Maytin, E.V. Methotrexate used in combination with aminolaevulinic acid for photodynamic killing of prostate cancer cells. Br. J. Cancer 2006, 95, 485–495. [Google Scholar] [CrossRef]
- Dimitriadis, I.; Bamias, A. Systemic Chemotherapy for Urothelial Cancer–How to Select Systemic Therapy in Bladder Cancer. Eur. Oncol. Haematol. 2017, 13, 134–138. [Google Scholar] [CrossRef] [Green Version]
- Sakura, T.; Hayakawa, F.; Sugiura, I.; Murayama, T.; Imai, K.; Usui, N.; Fujisawa, S.; Yamauchi, T.; Yujiri, T.; Kakihana, K.; et al. High-dose methotrexate therapy significantly improved survival of adult acute lymphoblastic leukemia: A phase III study by JALSG. Leukemia 2018, 32, 626–632. [Google Scholar] [CrossRef] [PubMed]
- van der Plas, E.; Nieman, B.J.; Butcher, D.T.; Hitzler, J.K.; Weksberg, R.; Ito, S.; Schachar, R. Neurocognitive late effects of chemotherapy in survivors of acute lymphoblastic leukemia: Focus on methotrexate. J. Can. Acad. Child. Adolesc. Psychiatry 2015, 24, 25–32. [Google Scholar] [PubMed]
- Hryniuk, W.M.; Bertino, J.R. Treatment of leukemia with large doses of methotrexate and folinic acid: Clinical-biochemical correlates. J. Clin. Investig. 1969, 48, 2140–2155. [Google Scholar] [CrossRef] [PubMed]
- Brenner, T.L.; Evans, W.E. Rationale for High-Dose Methotrexate in Childhood Acute Lymphoblastic Leukemia. In Treatment of Acute Leukemias, Antileukemic Drugs; Humana Press: Totowa, NJ, USA, 2003; pp. 339–356. [Google Scholar]
- Camitta, B.M.; Kamen, B.A. Role of Methotrexate in the Treatment of Acute Lymphoblastic Leukemia. In Treatment of Acute Leukemias: Antileukemic Drugs; Humana Press: Totowa, NJ, USA, 2003; pp. 357–362. [Google Scholar]
- Rizzoli, V.; Mangoni, L.; Caramatti, C.; Degliantoni, G.; Costi, D. High-dose methotrexate-leucovorin rescue therapy: Selected application in non-Hodgkin’s lymphoma. Tumori 1985, 71, 155–158. [Google Scholar] [CrossRef]
- Canellos, G.P.; Skarin, A.T.; Rosenthal, D.S.; Moloney, W.C.; Frei, E. Methotrexate as a single agent and in combination chemotherapy for the treatment of non-Hodgkin’s lymphoma of unfavorable histology. Cancer Treat. Rep. 1981, 65, 125–129. [Google Scholar]
- Khan, R.B.; Shi, W.; Thaler, H.T.; DeAngelis, L.M.; Abrey, L.E. Is Intrathecal Methotrexate Necessary in the Treatment of Primary CNS Lymphoma? J. Neurooncol. 2002, 58, 175–178. [Google Scholar] [CrossRef]
- Batchelor, T.T.; Kolak, G.; Ciordia, R.; Foster, C.S.; Henson, J.W. High-Dose Methotrexate for Intraocular Lymphoma. Clin. Cancer Res. 2003, 9, 711–715. [Google Scholar] [CrossRef]
- Fahey, J.B. High-Dose Methotrexate and Primary Central Nervous System Lymphoma. J. Neurosci. Nurs. 2007, 39, 83–88. [Google Scholar] [CrossRef]
- Zhu, J.-J.; Gerstner, E.R.; Engler, D.A.; Mrugala, M.M.; Nugent, W.; Nierenberg, K.; Hochberg, F.H.; Betensky, R.A.; Batchelor, T.T. High-dose methotrexate for elderly patients with primary CNS lymphoma. Neuro-Oncology 2009, 11, 211–215. [Google Scholar] [CrossRef] [Green Version]
- Gong, F.; Meng, Q.; Liu, C.; Zhao, Y. Efficacy and association analysis of high-dose methotrexate in the treatment of children with acute lymphoblastic leukemia. Oncol. Lett. 2019, 17, 4423–4428. [Google Scholar] [CrossRef] [PubMed]
- De Wilde, V.; Dierickx, D.; Schroyens, W.; Van Den Neste, E.; Bonnet, C.; Andre, M.; Janssens, A.; Van Hende, V.; Van Hoof, A. BHS guidelines for primary central nervous system lymphoma. Belg. J. Hematol. 2016, 7, 69–78. [Google Scholar]
- Bergner, N.; Monsef, I.; Illerhaus, G.; Engert, A.; Skoetz, N. Role of chemotherapy additional to high-dose methotrexate for primary central nervous system lymphoma (PCNSL). Cochrane Database Syst. Rev. 2012, 11. [Google Scholar] [CrossRef] [PubMed]
- Bokstein, F.; Lossos, A.; Lossos, I.S.; Siegal, T. Central Nervous System Relapse of Systemic Non-Hodgkin’s Lymphoma: Results of Treatment Based on High-dose Methotrexate Combination Chemotherapy. Leuk. Lymphoma 2002, 43, 587–593. [Google Scholar] [CrossRef] [PubMed]
- Omuro, A.M.; Taillandier, L.; Chinot, O.; Carnin, C.; Barrie, M.; Hoang-Xuan, K. Temozolomide and methotrexate for primary central nervous system lymphoma in the elderly. J. Neurooncol. 2007, 85, 207–211. [Google Scholar] [CrossRef]
- Sun, X.; Liu, J.; Wang, Y.; Bai, X.; Chen, Y.; Qian, J.; Zhu, H.; Liu, F.; Qiu, X.; Sun, S.; et al. Methotrexate-cytarabine-dexamethasone combination chemotherapy with or without rituximab in patients with primary central nervous system lymphoma. Oncotarget 2017, 8, 49156–49164. [Google Scholar] [CrossRef]
- Reinius, M.; Ahmad, S.S.; Crawley, C.; Williams, M.V.; Wimperis, J.; Follows, G.A. High-Dose Methotrexate in the Treatment of Primary Testicular Lymphoma. Blood 2013, 122, 5108. [Google Scholar] [CrossRef]
- Morris, P.G.; Correa, D.D.; Yahalom, J.; Raizer, J.J.; Schiff, D.; Grant, B.; Grimm, S.; Lai, R.K.; Reiner, A.S.; Panageas, K.; et al. Rituximab, Methotrexate, Procarbazine, and Vincristine Followed by Consolidation Reduced-Dose Whole-Brain Radiotherapy and Cytarabine in Newly Diagnosed Primary CNS Lymphoma: Final Results and Long-Term Outcome. J. Clin. Oncol. 2013, 31, 3971–3979. [Google Scholar] [CrossRef]
- Kansara, R.R.; Shenkier, T.; Connors, J.M.; Gerrie, A.S.; Klasa, R.; Savage, K.J.; Sehn, L.H.; Villa, D. Rituximab with High Dose Methotrexate in the Management of Primary Central Nervous System Diffuse Large B-Cell Lymphoma. Blood 2014, 124, 3090. [Google Scholar] [CrossRef]
- Inaly, K.; Crew, L.L.; Graham, C.A.; Mrugala, M.M. Primary central nervous system lymphoma treated with high-dose methotrexate and rituximab: A single-institution experience. Oncol. Lett. 2016, 11, 3471–3476. [Google Scholar] [CrossRef] [Green Version]
- BC Cancer Protocol Summary LYHDMRP. BC Cancer Protocol Summary for Treatment of Primary Intracerebral Lymphoma with High Dose Methotrexate and rituximab. Available online: http://www.bccancer.bc.ca/chemotherapy-protocols-site/Documents/Lymphoma-Myeloma/LYHDMRP_Protocol.pdf (accessed on 2 January 2020).
- Buechler, M.; Mukherji, B.; Chasin, W.; Nathanson, L. High dose methotrexate with and without BCG therapy in advanced head and neck malignancy. Cancer 1979, 43, 1095–1100. [Google Scholar] [CrossRef]
- Schappell, D.L.; Alper, J.C.; McDonald, C.J. Treatment of Advanced Mycosis Fungoides and Sézary Syndrome with Continuous Infusions of Methotrexate Followed by Fluorouracil and Leucovorin Rescue. Arch. Dermatol. 1995, 131, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Singh, V.K.; Subudhi, B.B. Development of reversible glutamine conjugate of methotrexate for enhanced brain delivery. Med. Chem. Res. 2015, 24, 624–635. [Google Scholar] [CrossRef]
- Singh, V.K.; Subudhi, B.B. Development and characterization of lysine-methotrexate conjugate for enhanced brain delivery. Drug Deliv. 2016, 23, 2327–2337. [Google Scholar] [CrossRef]
- Corem-Salkmon, E.; Ram, Z.; Daniels, D.; Perlstein, B.; Last, D.; Salomon, S.; Tamar, G.; Shneor, R.; Guez, D.; Margel, S.; et al. Convection-enhanced delivery of methotrexate-loaded maghemite nanoparticles. Int. J. Nanomed. 2011, 6, 1595–1602. [Google Scholar] [CrossRef] [Green Version]
- Gagliardi, M.; Bardi, G.; Bifone, A. Polymeric nanocarriers for controlled and enhanced delivery of therapeutic agents to the CNS. Ther. Deliv. 2012, 3, 875–887. [Google Scholar] [CrossRef]
- Wosikowski, K.; Biedermann, E.; Rattel, B.; Breiter, N.; Jank, P.; Löser, R.; Jansen, G.; Peters, G.J. Vivo Antitumor Activity of Methotrexate Conjugated to Human Serum Albumin in Human Cancer Cells. Clin. Cancer Res. 2003, 9, 1917–1926. [Google Scholar]
- Burger, A.M.; Hartung, G.; Stehle, G.; Sinn, H.; Fiebig, H.H. Pre-clinical Evaluation of a Methotrexate-Albumin Conjugate (MTX-HSA) in Human Tumor Xenografts in Vivo. Int. J. Cancer 2001, 92, 718–724. [Google Scholar] [CrossRef]
- Kohler, N.; Sun, C.; Wang, J.; Zhang, M. Methotrexate-Modified Superparamagnetic Nanoparticles and Their Intracellular Uptake into Human Cancer Cells. Langmuir 2005, 21, 8858–8864. [Google Scholar] [CrossRef]
- Gao, K.; Jiang, X. Influence of particle size on transport of methotrexate across blood brain barrier by polysorbate 80-coated polybutylcyanoacrylate nanoparticles. Int. J. Pharm. 2006, 310, 213–219. [Google Scholar] [CrossRef]
- Trapani, A.; Denora, N.; Iacobellis, G.; Sitterberg, J.; Bakowsky, U.; Kissel, T. Methotrexate-loaded chitosan- and glycol chitosan-based nanoparticles: A promising strategy for the administration of the anticancer drug to brain tumors. AAPS Pharm. Sci. Tech. 2011, 12, 1302–1311. [Google Scholar] [CrossRef] [Green Version]
- Mc Carthy, D.J.; Malhotra, M.; O’Mahony, A.M.; Cryan, J.F.; O’Driscoll, C.M. Nanoparticles and the Blood-Brain Barrier: Advancing from In-Vitro Models towards Therapeutic Significance. Pharm. Res. 2015, 32, 1161–1185. [Google Scholar] [CrossRef] [PubMed]
- Kosasih, A.; Bowman, B.J.; Wigent, R.J.; Ofner, C.M., III. Characterization and in Vitro Release of Methotrexate From Gelatin/Methotrexate Conjugates Formed Using Different Preparation Variables. Int. J. Pharm. 2000, 204, 81–89. [Google Scholar] [CrossRef]
- Narayani, R.; Rao, K.P. Controlled release of anticancer drug methotrexate from biodegradable gelatin microspheres. J. Microencapsul. 1994, 11, 69–77. [Google Scholar] [CrossRef] [PubMed]
- Narayani, R.; Rao, K.P. Biodegradable microspheres using two different gelatin drug conjugates for the controlled delivery of methotrexate. Int. J. Pharm. 1996, 128, 261–268. [Google Scholar] [CrossRef]
- Pica, K.; Tchao, R.; Ofner, C.M., III. Gelatin–methotrexate conjugate microspheres as a potential drug delivery system. J. Pharm. Sci. 2006, 95, 1896–1908. [Google Scholar] [CrossRef]
- Ofner, C.M., III; Pica, K.; Bowman, B.J.; Chen, C.S. Growth inhibition, drug load, and degradation studies of gelatin/methotrexate conjugates. Int. J. Pharm. 2006, 308, 90–99. [Google Scholar] [CrossRef]
- Nagy, G.; Király, G.; Veres, P.; Lázár, I.; Fábián, I.; Bánfalvi, G.; Juhász, I.; Kalmár, J. Controlled release of methotrexate from functionalized silica-gelatin aerogel microparticles applied against tumor cell growth. Int. J. Pharm. 2019, 558, 396–403. [Google Scholar] [CrossRef]
- Kukowska-Latallo, J.F.; Candido, K.A.; Cao, Z.; Nigavekar, S.S.; Majoros, I.J.; Thomas, T.P.; Balogh, L.P.; Khan, M.K.; Baker, J.R., Jr. Nanoparticle Targeting of Anticancer Drug Improves Therapeutic Response in Animal Model of Human Epithelial Cancer. Cancer Res. 2005, 65, 5317–5324. [Google Scholar] [CrossRef] [Green Version]
- Majoros, I.J.; Myc, A.; Thomas, T.; Mehta, C.B.; Baker, J.R., Jr. PAMAM dendrimer-based multifunctional conjugate for cancer therapy: Synthesis, characterization, and functionality. Biomacromolecules 2006, 7, 572–579. [Google Scholar] [CrossRef]
- Wu, G.; Barth, R.F.; Yang, W.; Kawabata, S.; Zhang, L.; Green-Church, K. Targeted delivery of methotrexate to epidermal growth factor receptor–positive brain tumors by means of cetuximab (IMC-C225) dendrimer bioconjugates. Mol. Cancer Ther. 2006, 5, 52–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bhattacharya, S.; Alkharfy, K.M.; Janardhanan, R.; Mukhopadhyay, D. Nanomedicine: Pharmacological perspectives. Nanotechnol. Rev. 2012, 1, 235–253. [Google Scholar] [CrossRef]
- Dhanikula, R.S.; Hildgen, P. Influence of molecular architecture of polyether-co-polyester dendrimers on the encapsulation and release of methotrexate. Biomaterials 2007, 28, 3140–3152. [Google Scholar] [CrossRef]
- Riebeseel, K.; Biedermann, E.; Löser, R.; Breiter, N.; Hanselmann, R.; Mülhaupt, R.; Unger, C.; Kratz, F. Polyethylene glycol conjugates of methotrexate varying in their molecular weight from MW 750 to MW 40000: Synthesis, characterization, and structure-activity relationships in vitro and in vivo. Bioconjug. Chem. 2002, 13, 773–785. [Google Scholar] [CrossRef] [PubMed]
- Kmiecik, S.; Krzyścik, M.; Filip-Psurska, B.; Wietrzyk, J.; Boratyński, J.; Goszczyński, T.M. Methotrexate and epirubicin conjugates as potential antitumor drugs. Adv. Clin. Exp. Med. 2017, 71, 618–623. [Google Scholar] [CrossRef]
- Martin, M.; Casado, A.; López-Martin, J.A.; Rodriguez-lescure, A.; Nieto, Y.; Ayala, F.; Diaz-rubio, E. Preliminary results. UFT/Methotrexate/Leucovorin for Breast Cancer Patients in Progression after HDCT/PBPC Support. Oncology (Williston Park) 1997, 11, 83–85. [Google Scholar]
- Martin, M.; Casado, A.; Macias, J.A.; Garcia-Carbonero, I.; Garcia-Saenz, J.A.; Oruezabal, M.; Manrique, I.; Diaz-Rubio, E. Methotrexate, uracil and tegafur, and leucovorin chemotherapy for patients with breast cancer in progression after high-dose chemotherapy with peripheral blood progenitor cell transplant: A phase II study. Am. J. Clin. Oncol. 2000, 23, 617–621. [Google Scholar] [CrossRef]
- Moreno, A.; Moreno, A.; Escobedo, A.; Benito, E.; Serra, J.M.; Guma, A.; Riu, F. Pathologic Changes Related to CMF Primary Chemotherapy in Breast Cancer. Breast Cancer Res. Treat. 2002, 75, 119–125. [Google Scholar] [CrossRef]
- Cocconi, G.; Blasio, B.D.; Boni, C.; Bisagni, G.; Rondini, E.; Bella, M.A.; Leonardi, F.; Savoldi, L.; Vallisneri, C.; Camisa, R.; et al. Primary chemotherapy in operable breast carcinoma comparing CMF (cyclophosphamide, methotrexate, 5-fluorouracil) with an anthracycline-containing regimen: Short-term responses translated into long-term outcomes. Ann. Oncol. 2005, 16, 1469–1476. [Google Scholar] [CrossRef]
- Leone, J.P.; Leone, J.; Vallejo, C.T.; Pérez, J.E.; Romero, A.O.; Machiavelli, M.R.; Acuña, L.R.; Domínguez, M.E.; Langui, M.; Fasce, H.M.; et al. Sixteen years follow-up results of a randomized phase II trial of neoadjuvant fluorouracil, doxorubicin, and cyclophosphamide (FAC) compared with cyclophosphamide, methotrexate, and 5-fluorouracil (CMF) in stage III breast cancer: GOCS experience. Breast Cancer Res. Treat. 2014, 143, 313–332. [Google Scholar] [CrossRef]
- Colleoni, M.; Rocca, A.; Sandri, M.T.; Zorzino, L.; Masci, G.; Nolè, F.; Peruzzotti, G.; Robertson, C.; Orlando, L.; Cinieri, S.; et al. Low-dose oral methotrexate and cyclophosphamide in metastatic breast cancer: Antitumor activity and correlation with vascular endothelial growth factor levels. Ann. Oncol. 2002, 13, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, T.; Tanabe, M.; Kobayashi, K.; Fukada, I.; Takahashi, S.; Iwase, T.; Ito, Y. Combination chemotherapy with mitomycin C and methotrexate is active against metastatic HER2-negative breast cancer even after treatment with anthracycline, taxane, capecitabine, and vinorelbine. Springerplus 2015, 4, 376. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cheng, X.I.; Zhou, T.Y.; Li, B.; Li, M.; Li, L.; Li, Z.; Lu, W. Methotrexate and 5-aminoimidazole-4-carboxamide riboside exert synergistic anticancer action against human breast cancer and hepatocellular carcinoma. Acta Pharmacol. Sin. 2013, 34, 951–959. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, C.W.; Liu, H.C.; Yu, Y.L.; Hung, Y.T.; Wei, C.W.; Yiang, G.T. Combined treatment with vitamin C and methotrexate inhibits triple-negative breast cancer cell growth by increasing H2O2 accumulation and activating caspase-3 and p38 pathways. Oncol. Rep. 2017, 37, 2177–2184. [Google Scholar] [CrossRef] [Green Version]
- Bhasin, R.R.; Nogeirie, C.P. Combination Chemotherapy (High-Dose Methotrexate with Citrovorum Factor Rescue, Mechlorethamine, and Procarbazine) in Non-Small Cell Lung Cancer. Cancer Chemother. Pharmacol. 1983, 11, 106–107. [Google Scholar] [CrossRef]
- Chen, J.; Yang, X.; Huang, L.; Lai, H.; Gan, C.; Luo, X. Development of dual-drug-loaded stealth nanocarriers for targeted and synergistic anti-lung cancer efficacy. Drug Deliv. 2018, 25, 1932–1942. [Google Scholar] [CrossRef]
- Kern, S.; Truebenbach, I.; Höhn, M.; Gorges, J.; Kazmaier, U.; Zahler, S.; Vollmar, A.M.; Wagner, E. Combined antitumoral effects of pretubulysin and methotrexate. Pharmacol. Res. Perspect. 2019, 7, e00460. [Google Scholar] [CrossRef]
- Yan, K.; Lee, L.; Hsieh, M.; Yan, M.; Yao, C.; Chang, P.; Chen, T.; Chang, H.; Cheng, A.; Lai, G.; et al. Aspirin antagonizes the cytotoxic effect of methotrexate in lung cancer cells. Oncol. Rep. 2013, 30, 1497–1505. [Google Scholar] [CrossRef]
- Abdelrady, H.; Hathout, R.M.; Osman, R.; Saleem, I.; Mortada, N.D. Exploiting gelatin nanocarriers in the pulmonary delivery of methotrexate for lung cancer therapy. Eur. J. Pharm. Sci. 2019, 133, 115–126. [Google Scholar] [CrossRef]
- Kubota, Y.; Shuin, T.; Miura, T.; Moriyama, M.; Fukushima, S.; Shiozaki, H. Vincristine, bleomycin, cyclophosphamide, mitomycin, and methotrexate. Cancer Treat. Rep. 1984, 68, 1167–1168. [Google Scholar]
- Hall, R.R.; Newling, D.W.W.; Ramsden, P.D.; Richards, B.; Robinson, M.R.G.; Phillips, P.A. Treatment of invasive bladder cancer by local resection and high dose Methotrexate. Br. J. Urol. 1984, 56, 668–672. [Google Scholar] [CrossRef] [PubMed]
- Jaffe, N.; Gorlick, R. High-Dose Methotrexate in Osteosarcoma: Let the Questions Surcease—Time for Final Acceptance. J. Clin. Oncol. 2008, 26, 4365–4366. [Google Scholar] [CrossRef] [PubMed]
- Bielack, S.S.; Smeland, S.; Whelan, J.S.; Marina, N.M.; Jovic, G.; Hook, J.M.; Krailo, M.; Gebhardt, M.C.; Papai, Z.; Mayer, J.; et al. Methotrexate, Doxorubicin, and Cisplatin (MAP) Plus Maintenance Pegylated Interferon Alfa-2b Versus MAP Alone in Patients With Resectable High-Grade Osteosarcoma and Good Histologic Response to Preoperative MAP: First Results of the EURAMOS-1 Good Response Randomized Controlled Trial. J. Clin. Oncol. 2015, 33, 2279–2287. [Google Scholar] [CrossRef] [PubMed]
- Krailo, M.; Ertel, I.; Makley, J.; Fryjer, C.J.; Baum, E.; Weetman, R.; Yunis, E.; Barnes, L.; Bleyer, W.A.; Hammond, G.D. A randomized study comparing high-dose methotrexate with moderate-dose methotrexate as components of adjuvant chemotherapy in childhood nonmetastatic osteosarcoma: A report from the Childrens Cancer Study Group. Med. Pediatr. Oncol. 1987, 15, 69–77. [Google Scholar] [CrossRef]
- Meyers, P.A.; Schwartz, C.L.; Krailo, M.; Kleinerman, E.S.; Betcher, D.; Bernstein, M.L.; Conrad, E.; Ferguson, W.; Gebhardt, M.; Goorin, A.M.; et al. Osteosarcoma: A randomized, prospective trial of the addition of ifosfamide and/or muramyl tripeptide to cisplatin, doxorubicin, and high-dose methotrexate. J. Clin. Oncol. 2005, 23, 2004–2011. [Google Scholar] [CrossRef] [PubMed]
- Winkler, K.; Beron, G.; Delling, G.; Heise, U.; Kabisch, H.; Purfurst, C.; Berger, J.; Ritter, J.; Jurgens, H.; Gerein, V. Neoadjuvant chemotherapy of osteosarcoma: Results of a randomized cooperative trial (COSS-82) with salvage chemotherapy based on histological tumor response. J. Clin. Oncol. 1988, 6, 329–337. [Google Scholar] [CrossRef]
- Bacci, G.; Picci, P.; Ferrari, S.; Ruggieri, P.; Casadei, R.; Tienghi, A.; Brach del Prever, A.; Gherlinzoni, F.; Mercuri, M.; Monti, C. Primary chemotherapy and delayed surgery for nonmetastatic osteosarcoma of the extremities. Results in 164 patients preoperatively treated with high doses of methotrexate followed by cisplatin and doxorubicin. Cancer 1993, 72, 3227–3238. [Google Scholar] [CrossRef]
- Bacci, G.; Ferrari, S.; Bertoni, F.; Ruggieri, P.; Picci, P.; Longhi, A.; Casadei, R.; Fabbri, N.; Forni, C.; Versari, M.; et al. Long-term outcome for patients with nonmetastatic osteosarcoma of the extremity treated at the istituto ortopedico rizzoli according to the istituto ortopedico rizzoli/osteosarcoma-2 protocol: An updated report. J. Clin. Oncol. 2000, 18, 4016–4027. [Google Scholar] [CrossRef]
- Geller, D.S.; Richard Gorlick, R. Osteosarcoma: A Review of Diagnosis, Management, and Treatment Strategies. Clin. Adv. Hematol. Oncol. 2010, 8, 705–718. [Google Scholar]
- Abrão, R.; de Andrade, J.; Tiezzi, D.; Marana, H.; dos Reis, F.C.; Clagnan, W. Treatment for Low-Risk Gestational Trophoblastic Disease: Comparison of Single-Agent Methotrexate, Dactinomycin and Combination Regimens. Gynecol. Oncol. 2008, 108, 149–153. [Google Scholar] [CrossRef]
- Han, S.N.; Amant, F.; Leunen, K.; Devi, U.K.; Neven, P.; Berteloot, P.; Vergote, I. Treatment of high-risk gestational trophoblastic neoplasia with weekly high-dose methotrexate-etoposide. Gynecol. Oncol. 2012, 127, 47–50. [Google Scholar] [CrossRef]
- Nebraska Lymphoma Study Group. Treatment of Non-Hodgkin’s Lymphoma and Hodgkin’s Lymphoma. University of Nebraska Medical Center, Department of Internal Medicine. 2009. Available online: https://www.unmc.edu/media/lymphoma/ne_lymphoma_book.pdf (accessed on 2 January 2020).
- Malcolm, T.I.M.; Hodson, D.J.; Macintyre, E.A.; Turner, S.D. Challenging perspectives on the cellular origins of lymphoma. Open Biol. 2016, 6, 160232. [Google Scholar] [CrossRef] [Green Version]
- Burkhardt, B. Paediatric lymphoblastic T-cell leukaemia and lymphoma: One or two diseases? Br. J. Haematol. 2009, 149, 653–668. [Google Scholar] [CrossRef] [PubMed]
- Davis, T.P.; Enna, S.J.; Lecount, L. Pharmacology of the Blood Brain Barrier: Targeting CNS Disorders, 1st ed.; Elsevier INC: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Cho, K.M.; Kim, Y.J.; Kim, S.H.; Kim, J.W.; Lee, J.O.; Han, J.H.; Lee, K.W.; Kim, J.H.; Kim, C.Y.; Bang, S.M.; et al. Salvage Treatment with Intracerebrospinal Fluid Thiotepa in Patients with Leptomeningeal Metastasis After Failure of Methotrexate-based Treatment. Anticancer Res. 2015, 35, 5631–5638. [Google Scholar] [PubMed]
- Kapke, J.T.; Schneidewend, R.J.; Jawa, Z.A.; Chiang-Ching, H.; Connelly, J.M.; Chitambar, C.R. High-dose intravenous methotrexate in the management of breast cancer with leptomeningeal disease: Case series and review of the literature. Hematol. Oncol. Stem Cell Ther. 2019, 12, 189–193. [Google Scholar] [CrossRef]
- Kasim, A.; Whitehouse, M.; Ramachandran, C.; Sanz, M.B.; Lennernäs, H.; Hussain, A.S.; Junginger, H.E.; Stavchansky, S.; Midha, K.K.; Shah, V.P.; et al. Molecular Properties of WHO Essential Drugs and Provisional Biopharmaceutical Classification. Mol. Pharm. 2004, 1, 85–96. [Google Scholar] [CrossRef] [PubMed]
- Torchilin, V.P. Multifunctional Pharmaceutical Nanocarriers, 1st ed.; Springer: Boston, MA, USA, 2008. [Google Scholar]
- Martin-Banderas, L.; Holgado, M.A.; Venero, J.L.; Alvarez-Fuentes, J.; Fernández-Arévalo, M. Nanostructures for Drug Delivery to the Brain. Curr. Med. Chem. 2011, 18, 5303–5321. [Google Scholar] [CrossRef]
- Ricci, M.; Blasi, P.; Giovagnoli, S.; Rossi, C. Delivering drugs to the central nervous system: A medicinal chemistry or a pharmaceutical technology issue? Curr. Med. Chem. 2006, 13, 1757–1775. [Google Scholar] [CrossRef]
- Jang, J.H.; Jeong, S.H.; Lee, Y.B. Preparation and In Vitro/In Vivo Characterization of Polymeric Nanoparticles Containing Methotrexate to Improve Lymphatic Delivery. Int. J. Mol. Sci. 2019, 20, 3312. [Google Scholar] [CrossRef] [Green Version]
- Leone, L.A.; Albala, M.M.; Rege, V.B. Treatment of carcinoma of head and neck with intravenous methotrexate. Cancer 1968, 21, 828–837. [Google Scholar] [CrossRef]
- Capizzi, R.L.; DeConti, R.C.; Marsh, J.C.; Bertino, J.R. Methotrexate Therapy of Head and Neck Cancer: Improvement in Therapeutic Index by the Use of Leucovorin “Rescue”. Cancer Res. 1970, 30, 1782–1788. [Google Scholar] [PubMed]
- Pant, G.C.; Sanyal, B.; Khanna, N.N.; Rastogi, B.L. Sequential treatment of advanced oral carcinoma by methotrexate and radiotherapy. Indian J. Med. Res. 1973, 61, 848–855. [Google Scholar] [PubMed]
- Frei, E., III; Blum, R.H.; Pitman, S.W.; Kirkwood, J.M.; Henderson, I.C.; Skarin, A.T.; Mayer, R.S.; Bast, R.C.; Garnick, M.B.; Parker, L.M.; et al. High dose methotrexate with leucovorin rescue. Rationale and spectrum of antitumor activity. Am. J. Med. 1980, 68, 370–376. [Google Scholar] [CrossRef]
- Woods, R.L.; Fox, R.M.; Tattersall, M.H. Methotrexate treatment of squamous-cell head and neck cancers: Dose-response evaluation. Br. Med. J. (Clin. Res. Ed). 1981, 282, 600–602. [Google Scholar] [CrossRef] [Green Version]
- DeConti, R.C.; Schoenfeld, D. A randomized prospective comparison of intermittent methotrexate, methotrexate with leucovorin, and a methotrexate combination in head and neck cancer. Cancer 1981, 48, 1061–1072. [Google Scholar] [CrossRef]
- Hong, W.K.; Schaefer, S.; Issell, B.; Cummings, C.; Luedke, D.; Bromer, R.; Fotonoff, S.D.; Aoust, J.; Shapsay, S.; Welch, J.; et al. A prospective randomized trial of methotrexate versus cisplatin in the treatment of recurrent squamous cell carcinoma of the head and neck. Cancer 1983, 52, 206–210. [Google Scholar] [CrossRef]
- Drelichman, A.; Cummings, G.; Al-Sarraf, M. A randomized trial of the combination of cis-platinum, oncovin and bleomycin (COB) versus methotrexate in patients with advanced squamous cell carcinoma of the head and neck. Cancer 1983, 52, 399–403. [Google Scholar] [CrossRef]
- Pradhan, S.; Asthana, A.K.; Jain, R.K.; Pant, G.C.; Sahni, K. Single agent methotrexate chemotherapy for head and neck cancers. Indian J. Otolaryngol 1991, 43, 175. [Google Scholar] [CrossRef]
- Vermorken, J.B.; Specenier, P. Optimal treatment for recurrent/metastatic head and neck cancer. Ann. Oncol. 2010, 21, 252–261. [Google Scholar] [CrossRef]
- Pathak, A.B.; Kulkarni, H. Weekly methotrexate in squamous cell cancers of head and neck. J. Clin. Oncol. 2006, 24, 15539. [Google Scholar] [CrossRef]
- Banipal, R.P.S.; Mahajan, M.K. Methotrexate Revisited—in Recurrent Head and Neck Cancer. Palliat. Care Res. Treat. 2011, 5, 9–13. [Google Scholar] [CrossRef]
- Sharma, M.; Gupta, M.; Fotedar, V.; Sharma, A. Methotrexate, an attractive agent for palliation in head and neck cancers. South Asian J. Cancer 2014, 3, 229. [Google Scholar] [CrossRef] [PubMed]
- Gasparini, G. Metronomic scheduling: The future of chemotherapy? Lancet Oncol. 2001, 2, 733–740. [Google Scholar] [CrossRef]
- De Felice, F.; Musio, D.; Tombolini, V. Head and neck cancer: Metronomic chemotherapy. BMC Cancer 2015, 15, 677. [Google Scholar] [CrossRef] [Green Version]
- Schwartz, M.A. High-dose methotrexate for metastatic breast cancer to the central nervous system: A single-institution review of 46 patients. J. Clin. Oncol. 2014, 32, 1079. [Google Scholar] [CrossRef]
- Colleoni, M.; Cole, B.F.; Viale, G.; Regan, M.M.; Price, K.N.; Maiorano, E.; Mastropasqua, M.G.; Crivellari, D.; Gelber, R.D.; Goldhirsch, A.; et al. Classical cyclophosphamide, methotrexate, and fluorouracil chemotherapy is more effective in triple-negative, node-negative breast cancer: Results from two randomized trials of adjuvant chemoendocrine therapy for nodenegative breast cancer. J. Clin. Oncol. 2010, 28, 2966–2973. [Google Scholar] [CrossRef] [Green Version]
- Wu, C.E.; Chen, S.C.; Lin, Y.C.; Lo, Y.F.; Hsueh, S.; Chang, H.K. Identification of patients with node-negative, triple-negative breast cancer who benefit from adjuvant cyclophosphamide, methotrexate, and 5-fluorouracil chemotherapy. Anticancer. Res. 2014, 34, 1301–1306. [Google Scholar]
- Kumaki, N.; Okamatsu, C.; Tokuda, Y.; Nakamura, N. Breast Cancer in Patients of Rheumatoid Arthritis with Methotrexate Therapy Mimicking Histopathological Changes after Neoadjuvant Chemotherapy. Tokai J. Exp. Clin. Med. 2017, 42, 104–108. [Google Scholar]
- Hoeng, J.; Maeder, S.; Vanscheeuwijck, P.; Peitsch, M.C. Assessing the lung cancer risk reduction potential of candidate modified risk tobacco products. Intern. Emerg. Med. 2019, 14, 821–834. [Google Scholar] [CrossRef] [Green Version]
- Tomoda, R.; Seto, M.; Hioki, Y.; Sonoda, J.; Matsumine, A.; Kusuzaki, K.; Uchida, A. Low-dose Methotrexate Inhibits Lung Metastasis and Lengthens Survival in Rat Osteosarcoma. Clin. Exp. Metastasis 2005, 22, 559–564. [Google Scholar] [CrossRef]
- Sekimura, A.; Iwai, S.; Funasaki, A.; Motono, N.; Usuda, K.; Uramoto, H. Lung cancer combined with methotrexate-associated lymphoproliferative disorder: A case report. Int. J. Surg. Case Rep. 2019, 59, 161–164. [Google Scholar] [CrossRef] [PubMed]
- deKernion, J.B. The Chemotherapy of Advanced Bladder Carcinoma. Cancer Res. 1977, 37, 2771–2774. [Google Scholar] [PubMed]
- Osasan, S.; Zhang, M.; Shen, F.; Paul, P.J.; Persad, S.; Sergi, C. Osteogenic Sarcoma: A 21st Century Review. Anticancer Res. 2016, 36, 4391–4398. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Xu, M.; Xu, S.F.; Yu, X.C. Clinical analysis of osteosarcoma patients treated with high-dose methotrexate-free neoadjuvant chemotherapy. Curr. Oncol. 2014, 21, e678–e684. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wippel, B.; Gundle, K.R.; Dang, T.; Paxton, J.; Bubalo, J.; Stork, L.; Fu, R.; Ryan, C.W.; Davis, L.E. Safety and Efficacy of High-Dose Methotrexate for Osteosarcoma in Adolescents Compared With Young Adults. Cancer Med. 2019, 8, 111–116. [Google Scholar] [CrossRef] [Green Version]
- Guo, W.; Healey, J.H.; Meyers, P.A.; Ladanyi, M.; Huvos, A.G.; Bertino, J.R.; Gorlick, R. Mechanisms of methotrexate resistance in osteosarcoma. Clin. Cancer. Res. 1999, 5, 621–627. [Google Scholar]
- Wang, J.; Li, G. Mechanisms of methotrexate resistance in osteosarcoma cell lines and strategies for overcoming this resistance. Oncol. Lett. 2014, 9, 940–944. [Google Scholar] [CrossRef] [Green Version]
- Xu, W.; Li, Z.; Zhu, X.; Xu, R.; Xu, Y. miR-29 Family Inhibits Resistance to Methotrexate and Promotes Cell Apoptosis by Targeting COL3A1 and MCL1 in Osteosarcoma. Med. Sci. Monit. 2018, 24, 8812–8821. [Google Scholar] [CrossRef]
- Kobayashi, E.; Hornicek, F.J.; Duan, Z. MicroRNA involvement in osteosarcoma. Sarcoma 2012, 2012, 359739. [Google Scholar] [CrossRef]
- Lurain, J.R.; Elfstrand, E.P. Single-agent methotrexate chemotherapy for the treatment of nonmetastatic gestational trophoblastic tumors. Am. J. Obstet. Gynecol. 1995, 172, 574–579. [Google Scholar] [CrossRef]
- Chapman-Davis, E.; Hoekstra, A.V.; Rademaker, A.W.; Schink, J.C.; Lurain, J.R. Treatment of nonmetastatic and metastatic low-risk gestational trophoblastic neoplasia: Factors associated with resistance to single-agent methotrexate chemotherapy. Gynecol. Oncol. 2012, 125, 572–575. [Google Scholar] [CrossRef] [PubMed]
- Couder, F.; Massardier, J.; You, B.; Abbas, F.; Hajri, T.; Lotz, J.-P.; Schott, A.-M.; Golfier, F. Predictive factors of relapse in low-risk gestational trophoblastic neoplasia patients successfully treated with methotrexate alone. Am. J. Obstet. Gynecol. 2016, 215, 80.e1–80.e7. [Google Scholar] [CrossRef] [PubMed]
- Lawrie, T.A.; Alazzam, M.; Tidy, J.; Hancock, B.W.; Osborne, R. First-line chemotherapy in low-risk gestational trophoblastic neoplasia. Cochrane Database Syst. Rev. 2016, 2016, CD007102. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- May, T.; Goldstein, D.P.; Berkowitz, R.S. Current Chemotherapeutic Management of Patients with Gestational Trophoblastic Neoplasia. Chemother. Res. Pract. 2011, 2011, 12. [Google Scholar] [CrossRef] [PubMed]
- Aminimoghaddam, S.; Abolghasem, N.; Ashraf-Ganjooie, T. New Management of Gestational trophoblastic diseases; A Continuum of Moles to Choriocarcinoma: A Review Article. J. Obstet. Gynecol. Cancer Res. 2018, 3, 123–128. [Google Scholar]
- Alazzam, M.; Tidy, J.; Osborne, R.; Coleman, R.; Hancock, B.W.; Lawrie, T.A. Chemotherapy for resistant or recurrent gestational trophoblastic neoplasia. Cochrane Database Syst. Rev. 2016, 1. [Google Scholar] [CrossRef]
- Skubisz, M.M.; Tong, S. The Evolution of Methotrexate as a Treatment for Ectopic Pregnancy and Gestational Trophoblastic Neoplasia: A Review. Obstet. Gynecol. 2012, 2012, 8. [Google Scholar] [CrossRef]
- Agarwal, R.; Harding, V.; Short, D.; Fisher, R.A.; Sebire, N.J.; Harvey, R.; Patel, D.; Savage, P.M.; Lim, A.K.; Seckl, M.J. Uterine artery pulsatility index: A predictor of methotrexate resistance in gestational trophoblastic neoplasia. Br. J. Cancer 2012, 106, 1089–1094. [Google Scholar] [CrossRef] [PubMed]
- Seckl, M.J.; Sebire, N.J.; Fisher, R.A.; Golfier, F.; Massuger, L.; Sessa, C. Gestational trophoblastic disease: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2013, 24, vi39–vi50. [Google Scholar] [CrossRef]
- Hussain, A.; Aziz, S.A.; Bhat, G.M.; Lone, A.R. Management of gestational trophoblastic neoplasia. Clin. Obstet. Gynecol. Reprod. Med. 2015, 1, 5–11. [Google Scholar] [CrossRef] [Green Version]
- Biscaro, A.; Braga, A.; Berkowitz, R.S. Diagnosis, classification and treatment of gestational trophoblastic neoplasia. Rev. Bras. Ginecol. Obstet. 2015, 37, 42–51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Eysbouts, Y.K.; Ottevanger, P.B.; Massuger, L.F.A.G.; IntHout, J.; Short, D.; Harvey, R.; Kaur, B.; Sebire, N.J.; Sarwar, N.; Sweep, F.C.G.J.; et al. Can the FIGO 2000 scoring system for gestational trophoblastic neoplasia be simplified? A new retrospective analysis from a nationwide dataset. Ann. Oncol. 2017, 28, 1856–1861. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.; Malkovska, V.; Krishnan, J.; Lessin, L.; Barth, W.; Krishnan, J.; Lessin, L.; Barth, W. Lymphoma in a patient with rheumatoid arthritis receiving methotrexate treatment: Successful treatment with rituximab. Ann. Rheum. Dis. 2001, 60, 892–893. [Google Scholar] [PubMed]
- Mariette, X.; Cazals-Hatem, D.; Warszawki, J.; Liote, F.; Balandraud, N.; Sibilia, J. Lymphomas in rheumatoid arthritis patients treated with methotrexate: A 3-year prospective study in France. Blood 2002, 99, 3909–3915. [Google Scholar] [CrossRef] [Green Version]
- Gelfand, J.M.; Shin, D.B.; Neimann, A.L.; Wang, X.; Margolis, D.J.; Troxel, A.B. The risk of lymphoma in patients with psoriasis. J. Invest. Dermatol. 2006, 126, 2194–2201. [Google Scholar] [CrossRef] [Green Version]
- Jankowitz, R.C.; Ganon, J.; Blodgett, T.; Garcia, C.; Jacobs, S. A Putative Case of Methotrexate-Related Lymphoma: Clinical Course and PET/CT Findings. Case Rep Med 2009, 2009. [Google Scholar] [CrossRef]
- Anderson, L.A.; Gadalla, S.; Morton, L.M.; Landgren, O.; Pfeiffer, R.; Warren, J.L.; Berndt, S.I.; Ricker, W.; Parsons, R.; Engels, E.A. Population-based study of autoimmune conditions and the risk of specific lymphoid malignancies. Int. J. Cancer 2009, 125, 398–405. [Google Scholar] [CrossRef] [Green Version]
- Hagihara, M.; Mese, T.; Ohara, S.; Hua, J.; Ide, S.; Inoue, M. Methotrexate-associated Intravascular Large B-cell Lymphoma in a Patient with Rheumatoid Arthritis: A Very Rare Case. Intern. Med. 2018, 57, 3001–3005. [Google Scholar] [CrossRef] [Green Version]
- Bolonga, C.; Picot, M.C.; Jorgensen, C.; Viu, P.; Verdier, R.; Sany, J. Study of eight cases of cancer in 426 rheumatoid arthritis patients treated with methotrexate. Ann. Rheum. Dis. 1997, 56, 97–102. [Google Scholar] [CrossRef] [Green Version]
- Ruymann, F.B.; Mosijczuk, A.D.; Sayers, R.J. Hepatoma in a Child with Methotrexate-Induced Hepatic Fibrosis. JAMA 1977, 238, 2631–2633. [Google Scholar] [CrossRef]
- Al-Anazi, K.A.; Eltayeb, K.I.; Bakr, M.; Al-Mohareb, F.I. Methotrexate-induced acute leukemia: Report of three cases and review of the literature. Clin. Med. Case Rep. 2009, 2, 43–49. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jones, L.A.; Robertson, N.P. An update on treatments in myasthenia gravis. J. Neurol. 2017, 264, 205–207. [Google Scholar] [CrossRef] [PubMed] [Green Version]
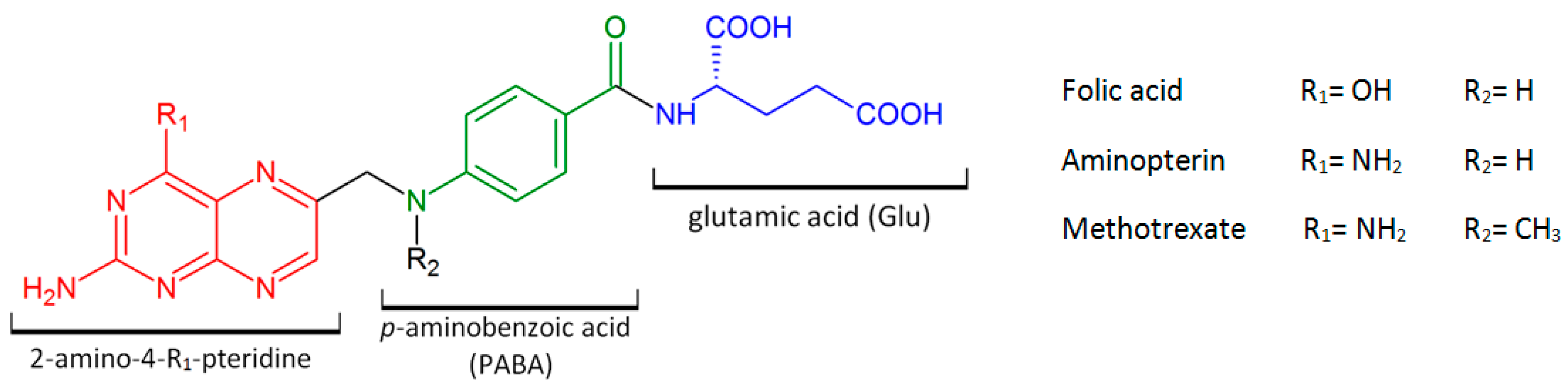
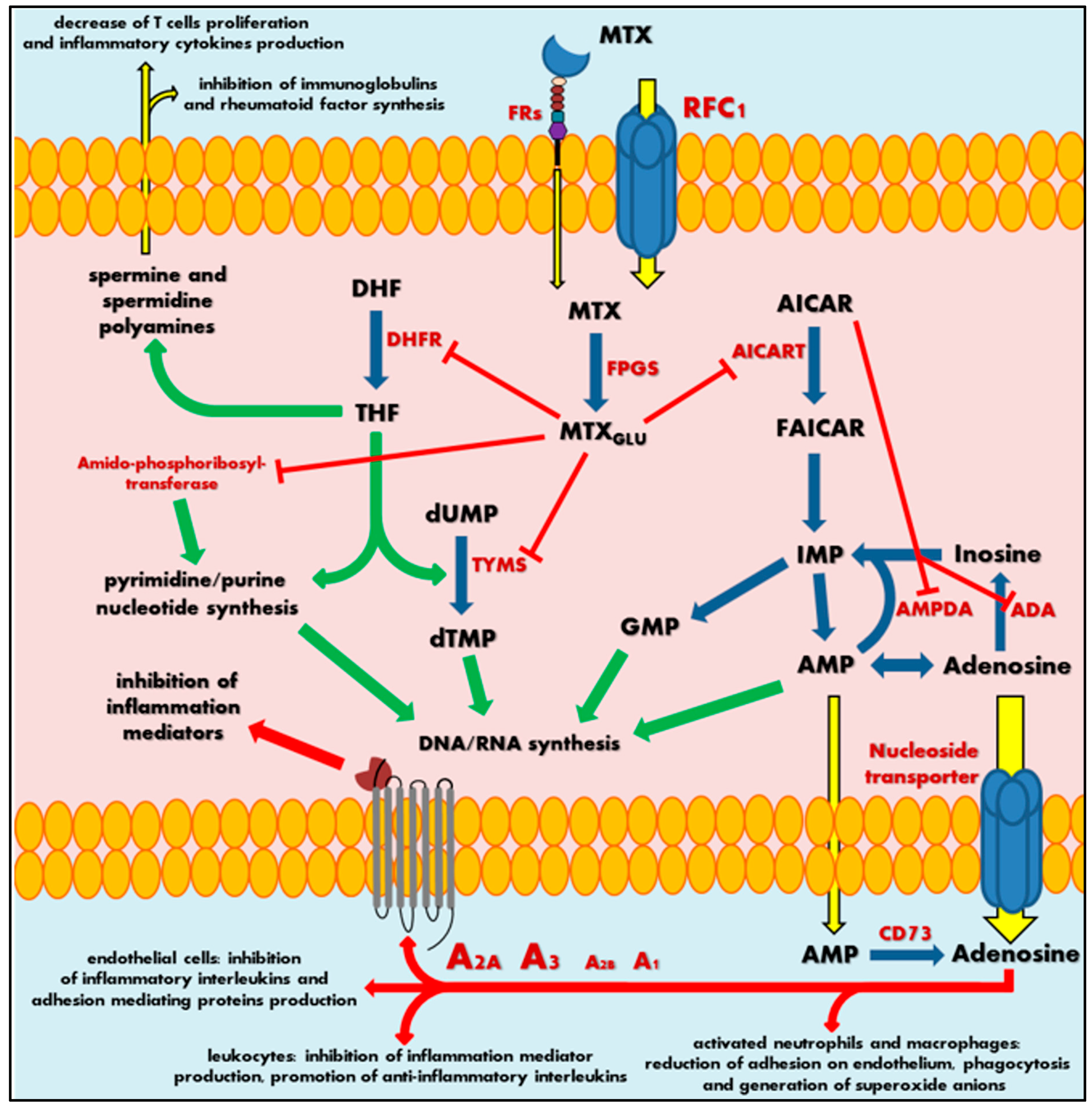
| Disease | FDA/EMA Approval | References |
|---|---|---|
| Myasthenia gravis | −/− | [17,80,81,82,83,84,85,86,87,88,89,90] |
| Rheumatoid arthritis | +/+ | [14,15,95,100,101,102] |
| Psoriasis | +/+ | [16,68,107,114,115,116] |
| Crohn’s disease | −/− | [18,117,118] |
| Sarcoidosis | +/+ | [68,114,115,116] |
| Alzheimer’s disease | −/− | [104,105,106] |
| Multiple sclerosis | −/− | [19,121,122,123] |
| Content of Combination Regimens | Type of Cancer | Reference |
|---|---|---|
| LDMTX | childhood ALL | [128] |
| PCNSL | [129,130] | |
| mycosis fungoides | [131,132,133,134] | |
| HNSCC | [135] | |
| LDMTX + thalidomide | refractory NHL | [136,137] |
| LDMTX + bleomycin | HNSCC | [138] |
| LDMTX-LV + PDD + 5-FU | [139] | |
| LDMTX or LDMTX-5-FU | [140] | |
| LDMTX + celecoxib | [141,142] | |
| LDMTX + capecitabine | [143] | |
| LDMTX + interferons | mycosis fungoides | [131,144,145,146,147] |
| LDMTX + 311 nm UV-B | [148] | |
| LDMTX + radiotherapy | [149] | |
| LDMTX + bleomycin + doxorubicin + topical nitrogen mustard | [150] | |
| LDMTX + CTX + lomustine + etoposide or Adriamycin or vincristine | SCLC | [151] |
| LDMTX-LV/HDMTX-LV + combination + CTX doxorubicin + vincristine or LDMTX-LV/HDMTX-LV + etoposide + vincristine + hexamethylmelamine | [152] | |
| LDMTX-LV/HDMTX-LV + vincristine + doxorubicin + CTX [MOAC] | [153] | |
| LDMTX + PDD | NSCLC | [154] |
| LDMTX + mitomycin C + vinblastin + PDD [M-MVP] | [155] | |
| LDMTX-LV / HDMTX-LV | bladder cancer | [10,156,157,158] |
| LDMTX + PDD | [159] | |
| LDMTX + vinblastine + Adriamycin + cisplatin [MVAC] | [160,161,162,163,164,165] | |
| HDMTX + vinblastine + Adriamycin + PDD [HDMVAC] | ||
| LDMTX + cisplatin + vinblastine [CMV] | ||
| IDMTX | childhood ALL | [166] |
| HDMTX-LV | childhood ALL | [167,168,169,170] |
| PCNSL, widespread NHL | [171,172,173,174,175,176] | |
| HDMTX + citrovorum factor | ALL (B-lineage or T-lineage) | [177] |
| HDMTX + cytarabine | NHL | [178,179,180] |
| HDMTX + temozolomide | PCNSL | [181] |
| HDMTX + rituximab + cytarabine + dexamethasone (R-MAD) | lymphoma | [182] |
| HDMTX+ bleomycin + Adriamycin + Cytoxan + vincristine | [172] | |
| HDMTX + rituximab +CTX+ doxorubicin + vincristine + prednisolone (R-CHOP) | [183] | |
| HDMTX + rituximab + procarbazine + vincristine (R-MPV) | [184] | |
| HDMTX + rituximab | [185,186,187] | |
| HDMTX-BCG vaccine | HNSCC | [188] |
| MTX-LV + 5-FU | mycosis fungoides | [189] |
| MTX-(glutamine)2 | brain tumour delivery system | [190] |
| MTX-(lysine)2 | [191] | |
| MTX- magneticNPs-HSA | [192,193,194,195] | |
| MTX- magnetic(iron oxide)NPs | [196] | |
| MTX-polyacrylateNPs | [197] | |
| MTX-chitosanNPs | [198] | |
| MTX-polymersNPs | [199,200] | |
| MTX-protein microspheres | [199,200,201,202,203,204,205,206] | |
| MTX-dendrimers [G5(MTX)n] | [62] | |
| MTX-dendrimers [C225-G5-MTX] | [206,207,208,209] | |
| MTX-dendrimers [PEPE-MTX] | [210] | |
| MTX-PEG | [211] | |
| MTX-EPR | [212] | |
| CTX + MTX + 5-FU [CMF] 5-FU + Adriamycin + CTX [FAC] MTX-LV + tegafur and/or uracil [MUL] | breast cancer (TNBC) | [213,214,215,216,217] |
| MTX + CTX | [218] | |
| [CMF] + CMFEV + epirubicin or vincristine (rotationally) [CMFEV] | [216] | |
| MTX + mitomycin C [MM] | [219] | |
| MTX + 5-aminoimidazole-4-carboxamide riboside (AICAR) | [220] | |
| MTX + vitamin C | [221] | |
| HDMTX-LV + mechlorethamine + procarbazine | NSCLC | [222] |
| MTX + PTX + PCNPs [MTX-PMX-PCNPs] | [223] | |
| MTX + pretubulysin | NSCLC (in vitro study) | [224] |
| MTX + acetylsalicylic acid (ASA) | [225] | |
| MTX-gelatinNPs | pulmonary lung delivery | [226] |
| HDMTX + 5-FU + vincristine + bleomycin + mitomycin C | blade cancer | [227,228] |
| HDMTX-LV + doxorubicin + cisplatin + ifosfamide and/or CTX | osteosarcoma | [229] |
| HDMTX + doxorubicin + PDD [MAP] HDMTX + doxorubicin + PDD + IFN-α-2b | [230] | |
| HDMTX or moderate MTX + Adriamycin + vincristine | [231] | |
| HDMTX + cisplatin + isofosfamide + doxorubicin + muramyl tripeptide encapsulated in liposomes | [232] | |
| HDMTX + bleomycin + CTX + dactinomycin (BCD) | [233] | |
| HDMTX + cisplatin + doxorubicin | [234,235] | |
| HDMTX + trimetrexate; HDMTX + PDD + doxorubicin + ifosfamide + etoposide + zoledronic acid | [236] | |
| MTX + ACT [MACT] | low risk GTN | [237] |
| HDMTX + etoposide; etoposide + cisplatin /+/ etoposide + MTX + dactinomycin [EP-EMA] | high risk GTN | [238] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Koźmiński, P.; Halik, P.K.; Chesori, R.; Gniazdowska, E. Overview of Dual-Acting Drug Methotrexate in Different Neurological Diseases, Autoimmune Pathologies and Cancers. Int. J. Mol. Sci. 2020, 21, 3483. https://doi.org/10.3390/ijms21103483
Koźmiński P, Halik PK, Chesori R, Gniazdowska E. Overview of Dual-Acting Drug Methotrexate in Different Neurological Diseases, Autoimmune Pathologies and Cancers. International Journal of Molecular Sciences. 2020; 21(10):3483. https://doi.org/10.3390/ijms21103483
Chicago/Turabian StyleKoźmiński, Przemysław, Paweł Krzysztof Halik, Raphael Chesori, and Ewa Gniazdowska. 2020. "Overview of Dual-Acting Drug Methotrexate in Different Neurological Diseases, Autoimmune Pathologies and Cancers" International Journal of Molecular Sciences 21, no. 10: 3483. https://doi.org/10.3390/ijms21103483





