Current Experience in Testing Mitochondrial Nutrients in Disorders Featuring Oxidative Stress and Mitochondrial Dysfunction: Rational Design of Chemoprevention Trials
Abstract
:1. Introduction
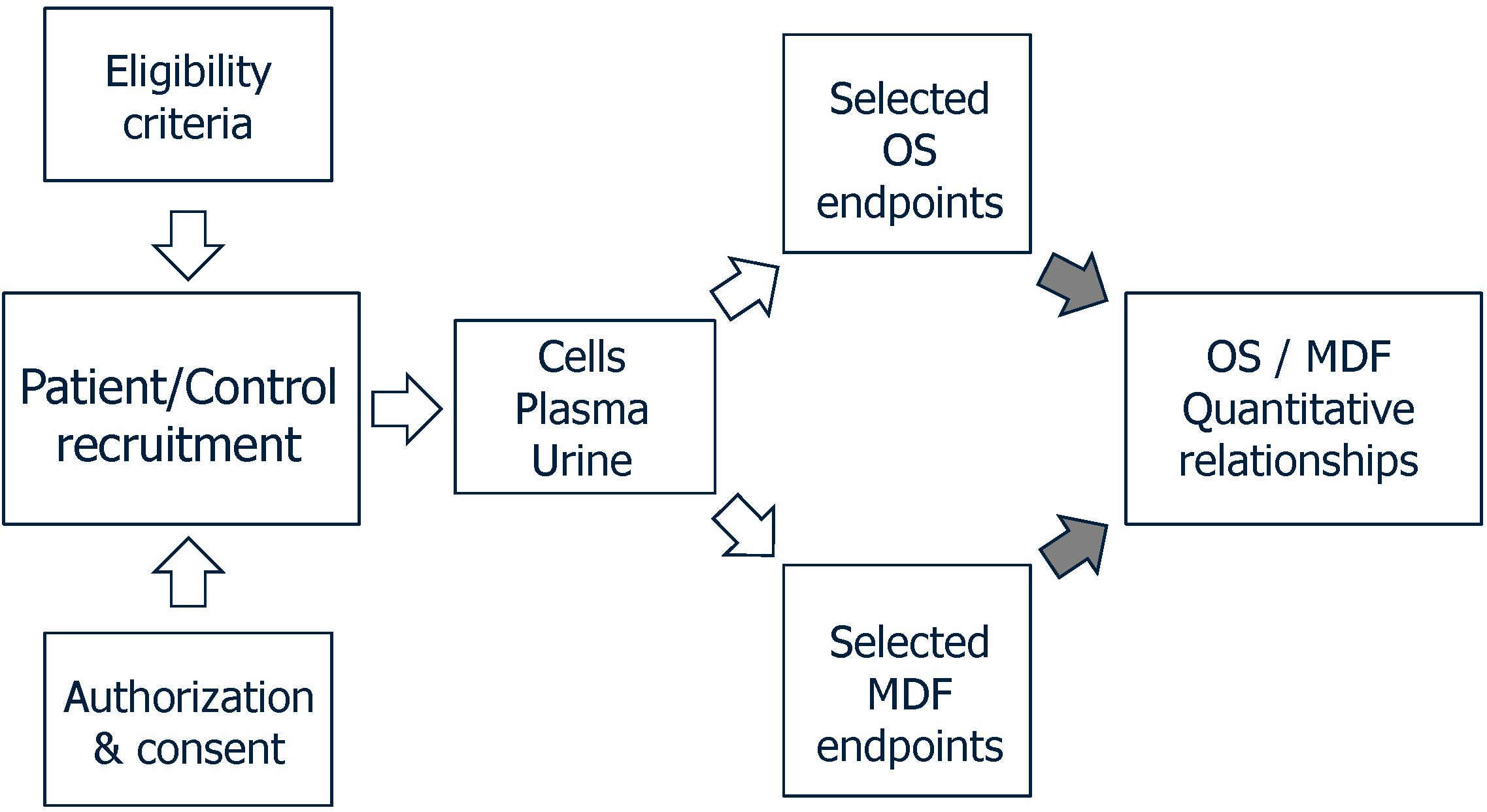
2. Methods
3. α-Lipoic Acid
| Diseases/Conditions | No. Studies (Controlled Studies) | No. Treated Patients | Success Ratio | References |
|---|---|---|---|---|
| Type 1 and Type 2 diabetes | 42 (30) | 2980 | 0.93 | [20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61] |
| Neurological diseases | 9 (5) | 509 | 0.89 | [62,63,64,65,66,67,68,69,70] |
| Liver and metabolic diseases | 8 (5) | 417 | 0.86 | [10,71,72,73,74,75,76,77] |
| Heart and vessel diseases | 4 (4) | 137 | 1.00 | [78,79,80,81] |
| Kidney diseases | 4 (3) | 288 | 0.25 | [82,83,84,85] |
| Genetic and mitochondrial diseases | 3 (2) | 129 | 0.33 | [86,87,88] |
| Burning mouth syndrome | 5 (5) | 293 | 0.60 | [89,90,91,92,93] |
| Other diseases § | 6 (4) | 525 | 1.00 | [94,95,96,97,98,99] |
| Total | 81 | 5278 |
4. Coenzyme Q10
| Diseases/Conditions | No. Studies (Controlled Studies) | No. Treated Patients | Success Ratio | References |
|---|---|---|---|---|
| Heart and vessel diseases | 39 (32) | 3386 | 0.89 | [11,12,81,101,102,103,104,105,106,107,108,109,110,111,112,113,114,115,116,117,118,119,120,121,122,123,124,125,126,127,128,129,130,131,132,133,134,135,136] |
| Genetic and mitochondrial diseases | 18 (8) | 680 | 0.75 | [13,14,88,137,138,139,140,141,142,143,144,145,146,147,148,149,150,151] |
| Neurological diseases | 16 (10) | 1185 | 0.87 | [65,152,153,154,155,156,157,158,159,160,161,162,163,164,165,166] |
| Type 1 and Type 2 Diabetes | 9 (7) | 370 | 0.89 | [41,166,167,168,169,170,171,172,173,174] |
| Malignancies | 6 (2) | 301 | 0.67 | [175,176,177,178,179,180] |
| Kidney diseases | 4 (2) | 171 | 0.50 | [181,182,183,184] |
| Other diseases § | 15 (13) | 555 | 0.59 | [76,185,186,187,188,189,190,191,192,193,194,195,196,197,198] |
| Total | 107 | 6648 |
5. l-Carnitine and Acetyl- or Propionyl-Carnitine
| Diseases/Conditions | No. Studies (Controlled Studies) | No. Treated Patients | Success Ratio | References |
|---|---|---|---|---|
| Kidney diseases | 18 (16) | 427 | 0.58 | [184,204,205,206,207,208,209,210,211,212,213,214,215,216,217,218,219,220] |
| Type 1 and Type 2 Diabetes | 13 (9) | 1894 | 1.00 | [221,222,223,224,225,226,227,228,229,230,231,232,233] |
| Heart and vessel diseases | 9 (6) | 359 | 1.00 | [78,114,234,235,236,237,238,239,240] |
| Liver diseases | 6 (2) | 275 | 1.00 | [241,242,243,244,245,246] |
| Neurological diseases | 9 (9) | 384 | 1.00 | [68,247,248,249,250,251,252,253,254] |
| Malignancies | 7 (6) | 699 | 0.70 | [255,256,257,258,259,260,261] |
| Genetic diseases | 6 (4) | 202 | 1.00 | [262,263,264,265,266,267] |
| HIV | 4 (1) | 93 | 1.00 | [97,268,269,270] |
| Other diseases § | 2 (2) | 99 | 1.00 | [271,272] |
| Total | 74 | 4432 |
6. Treatments with Mitochondrial Nutrient Combinations
| Diseases/Conditions | α-Lipoic Acid | Coenzyme Q10 (Daily Dose, mg/d) | l-Carnitine | References |
|---|---|---|---|---|
| Heart and vessel diseases | 100 | 100 | – | [81] |
| 400 | – | 1000 | [78] | |
| Mitochondrial diseases | 600 | 240 | – | [88] |
| Type 2 diabetes | 100 | 60 | – | [41] |
| Psoriasis | 150 | 50 | – | [76] |
| Sciatalgia | 600 | – | 1180 | [68] |
| Kidney diseases | – | 100 | 500 | [184] |
| Diseases/Conditions | α-Lipoic Acid + Other Agent(s) (Daily Dose) | References |
|---|---|---|
| Type 1 and Type 2 diabetes | ALA 100 mg, CoQ10 60 mg, Vit E 200 mg | [41] |
| ALA 600 mg, Vit E 800 mg | [44] | |
| ALA 800 mg, pyridoxine 80 mg | [56] | |
| ALA 600 mg, transdermal testosterone 50 mg | [59] | |
| ALA 2 × 600 mg, allopurinol 300 mg, nicotinamide 2 × 750 mg | [60] | |
| Heart surgery | ALA 100 mg, CoQ10 100 mg, Mg orotate 400 mg, ω-3 PUFA 300 mg, Se 200 µg | [81] |
| Metabolic syndrome | ALA 600 mg, Vit E 100 IU | [77] |
| Cancer-related anorexia/cachexia | ALA 300 mg, polyphenols 400 mg, carbocysteine 2.7 g, Vit E 400 mg, Vit A 30,000 IU, Vit C 500 mg, (n-3)-PUFA 2 cans | [94] |
| Alzheimer disease | ALA 900 mg, CoQ10 400 mg, Vit C 500 mg, Vit E 800 IU | [65] |
| Parkinson’s disease | ALA 1200 mg, folate 5 mg, Vit B12 1500 µg | [277] |
| Carpal tunnel syndrome | ALA 600 mg, γ-linolenic acid 360 mg, Vit B6 150 mg, Vit B1 100 mg, Vit B12 500 µg | [67] |
| Down syndrome | ALA 600 mg, Vit E 900 IU, Vit C 200 mg | [86] |
| HCV infection | ALA 300 mg, glycyrrhizin 1 g, Schisandra 1.5 g, silymarin 750 mg, Vit C 6 g, l-glutathione 300 mg, Vit E 800 IU | [72] |
| Psoriasis | ALA 600 mg, CoQ10 50 mg, resveratrol 20 mg, Vit E 36 mg, Krill oil 300 mg, Vitis vinifera seed oil 30 mg, Se 27 mg | [76] |
| Osteoporosis | ALA 2 × 300 mg, Vit C 30 mg, Vit E 5 mg, Se 2.75 mg | [99] |
| Vitiligo | ALA 100 mg, Vit C 100 mg, Vit E 40 mg, PUFA 12% | [98] |
| Diseases/Conditions | Coenzyme Q10 + Other Agent(s) (Daily Dose) | References |
|---|---|---|
| Heart surgery | CoQ10 100 mg, ALA 100 mg, Mg orotate 400 mg, ω-3 PUFA 300 mg, Se 200 µg | [81] |
| Chronic heart failure | CoQ10 150 mg, Ca 250 mg, Mg 150 mg, Zn 15 mg, Cu 1.2 mg, Se 50 µg, Vit A 800 µg, thiamine 200 mg, riboflavin 2 mg, Vit B6 200 mg, folate 5 mg, Vit B12 200 µg, Vit C 500 mg, Vit E 400 mg, Vit D 10 µg | [112,124] |
| Cardiovascular diseases | CoQ10 120 mg, Vit C 1 g, Vit E 400 IU, Se 200 µg | [128] |
| Cardiovascular mortality | CoQ10 200 mg, organic Se 200 μg | [136] |
| Breast cancer | CoQ10 100 mg, riboflavin 10 mg, niacin 50 mg | [175] |
| CoQ10 90 mg, Vit C 2850 mg, Vit E 2500 IU, β-carotene 32.5 IU, Se 387 mg, γ-linolenic acid 1.2 g, n-3 fatty acids 3.5 g | [176] | |
| CoQ10 300 mg, Vit E 300 IU | [177] | |
| Prostate cancer | CoQ10 200 mg, Vit C 750 mg, Vit E 350 mg, Se 200 µg | [179] |
| Friedreich ataxia | CoQ10 400 mg, Vit E 2100 IU | [140] |
| CoQ10 600 mg, Vit E 2100 IU | [141] | |
| Fibromyalgia | CoQ10 200 mg, Gingko biloba extract 200 mg | [160] |
7. State-of-Art: Critical Remarks
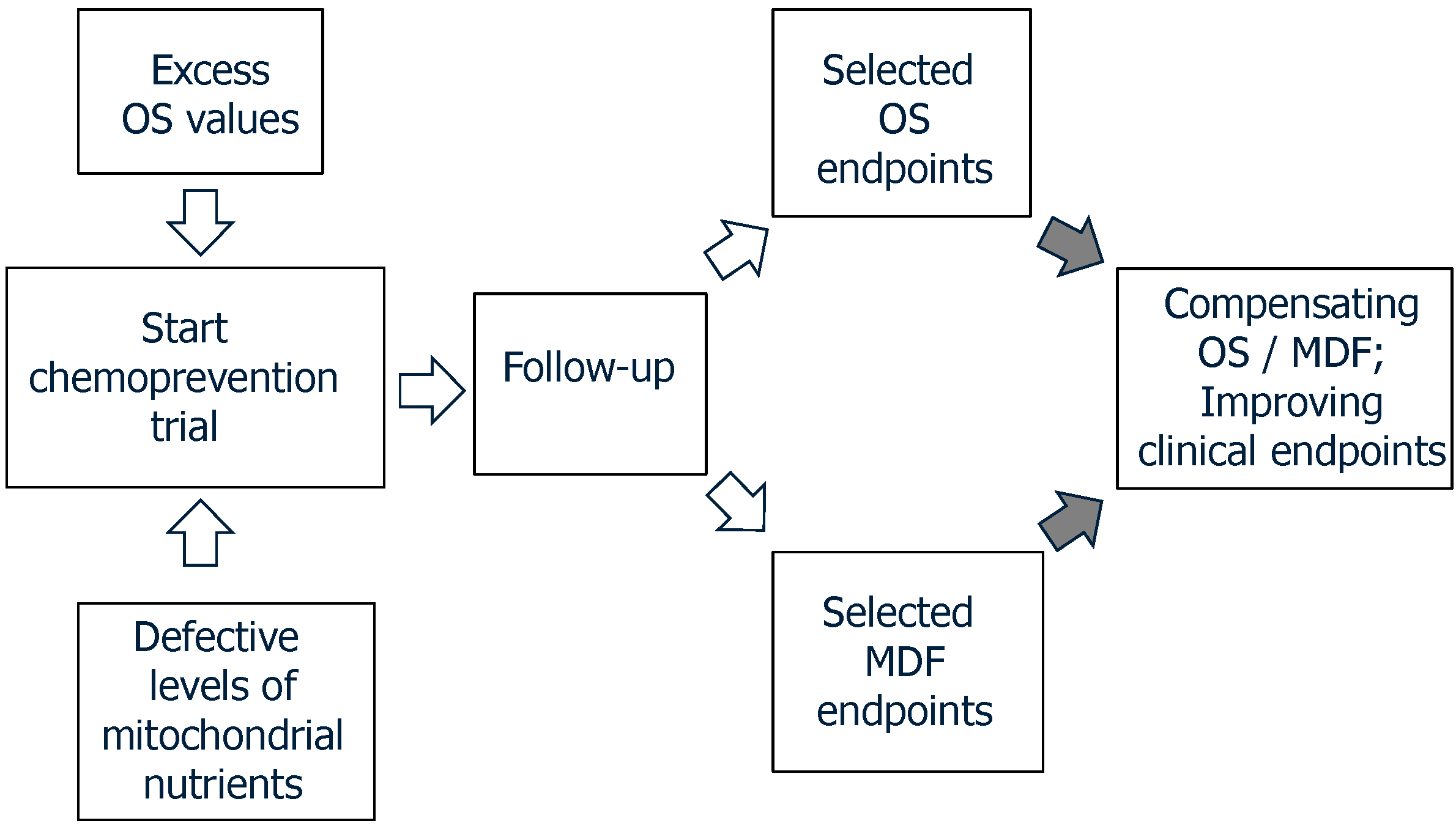
8. Prospects of Clinical Trials in OS/MDF-Related Disorders
Acknowledgments
Conflicts of Interest
References
- Richter, C.C.; Kass, G.E. Oxidative stress in mitochondria: its relationship to cellular Ca2+ homeostasis, cell death, proliferation, and differentiation. Chem. Biol. Interact. 1991, 77, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Sohal, R.S.; Brunk, U.T. Mitochondrial production of pro-oxidants and cellular senescence. Mutat. Res./DNAging 1992, 275, 295–304. [Google Scholar] [CrossRef]
- Di Monte, D.A.; Chan, P.; Sandy, M.S. Glutathione in Parkinson’s disease: A link between oxidative stress and mitochondrial damage? Ann. Neurol. 1992, 32, S111–S115. [Google Scholar]
- Beal, M.F. Therapeutic approaches to mitochondrial dysfunction in Parkinson’s disease. Parkinsonism Relat. Disord. 2009, 15, S189–S194. [Google Scholar] [CrossRef] [PubMed]
- Mischley, L.K.; Allen, J.; Bradley, R. Coenzyme Q10 deficiency in patients with Parkinson’s disease. J. Neurol. Sci. 2012, 318, 72–75. [Google Scholar] [CrossRef] [PubMed]
- Parikh, S.; Goldstein, A.; Koenig, M.K.; Scaglia, F.; Enns, G.M.; Saneto, R.; Mitochondrial Medicine Society Clinical Directors Working Group; Clinical Director’s Work Group. Practice patterns of mitochondrial disease physicians in North America. Part 2: Treatment, care and management. Mitochondrion 2013, 13, 681–687. [Google Scholar] [CrossRef] [PubMed]
- Tarnopolsky, M.A. The mitochondrial cocktail: Rationale for combined nutraceutical therapy in mitochondrial cytopathies. Adv. Drug Deliv. Rev. 2008, 60, 1561–1567. [Google Scholar] [CrossRef] [PubMed]
- Pallardó, F.V.; Lloret, A.; Lebel, M.; d’Ischia, M.; Cogger, V.C.; le Couteur, D.G.; Gadaleta, M.N.; Castello, G.; Pagano, G. Mitochondrial dysfunction in some oxidative stress-related genetic diseases: Ataxia-Telangiectasia, Down Syndrome, Fanconi Anaemia and Werner Syndrome. Biogerontology 2010, 11, 401–419. [Google Scholar] [CrossRef] [PubMed]
- Pagano, G.; Aiello Talamanca, A.; Castello, G.; Cordero, M.D.; d’Ischia, M.; Gadaleta, M.N.; Pallardó, F.V.; Petrović, S.; Tiano, L.; Zatterale, A. Oxidative stress and mitochondrial dysfunction across broad-ranging pathologies: Toward a rational design of chemoprevention strategies by means of mitochondrial nutrients. Oxid. Med. Cell. Longev. 2014, 2014, 541230. [Google Scholar] [CrossRef] [PubMed]
- Marshall, A.W.; Graul, R.S.; Morgan, M.Y.; Sherlock, S. Treatment of alcohol-related liver disease with thioctic acid: A six month randomised double-blind trial. Gut 1982, 23, 1088–1093. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, J.; Tominaga, R.; Yoshitoshi, M.; Matsui, K.; Komori, M.; Sese, A.; Yasui, H.; Tokunaga, K. Coenzyme Q10: The prophylactic effect on low cardiac output following cardiac valve replacement. Ann. Thorac. Surg. 1982, 33, 145–151. [Google Scholar] [CrossRef] [PubMed]
- Langsjoen, P.H.; Vadhanavikit, S.; Folkers, K. Response of patients in classes III and IV of cardiomyopathy to therapy in a blind and crossover trial with coenzyme Q10. Proc. Natl. Acad. Sci. USA 1985, 82, 4240–4244. [Google Scholar] [CrossRef] [PubMed]
- Ogasahara, S.; Nishikawa, Y.; Yorifuji, S.; Soga, F.; Nakamura, Y.; Takahashi, M.; Hashimoto, S.; Kono, N.; Tarui, S. Treatment of Kearns–Sayre syndrome with coenzyme Q10. Neurology 1986, 36, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Scarlato, G.N.; Bresolin, N.I.; Moroni, I.; Doriguzzi, C.; Castelli, E.; Comi, G.; Angelini, C.; Carenzi, A. Multicenter trial with ubidecarenone: Treatment of 44 patients with mitochondrial myopathies. Rev. Neurol. 1991, 147, 542–548. [Google Scholar] [PubMed]
- Mayr, J.A.; Zimmermann, F.A.; Fauth, C.; Bergheim, C.; Meierhofer, D.; Radmayr, D.; Zschocke, J.; Koch, J.; Sperl, W. Lipoic acid synthetase deficiency causes neonatal-onset epilepsy, defective mitochondrial energy metabolism, and glycine elevation. Am. J. Hum. Genet. 2011, 89, 792–797. [Google Scholar] [CrossRef] [PubMed]
- Liu, J. The effects and mechanisms of mitochondrial nutrient alpha-lipoic acid on improving age-associated mitochondrial and cognitive dysfunction: An overview. Neurochem. Res. 2008, 33, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Maes, M.; Mihaylova, I.; Kubera, M.; Uytterhoeven, M.; Vrydags, N.; Bosmans, E. Coenzyme Q10 deficiency in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is related to fatigue, autonomic and neurocognitive symptoms and is another risk factor explaining the early mortality in ME/CFS due to cardiovascular disorder. Neuro Endocrinol. Lett. 2009, 30, 470–476. [Google Scholar] [PubMed]
- Tiano, L.; Busciglio, J. Mitochondrial dysfunction and Down’s syndrome: Is there a role for coenzyme Q10? Biofactors 2011, 37, 386–392. [Google Scholar] [CrossRef]
- Hardas, S.S.; Sultana, R.; Clark, A.M.; Beckett, T.L.; Szweda, L.I.; Murphy, M.P.; Butterfield, D.A. Oxidative modification of lipoic acid by HNE in Alzheimer disease brain. Redox Biol. 2013, 1, 80–85. [Google Scholar] [CrossRef] [PubMed]
- Kähler, W.; Kuklinski, B.; Rühlmann, C.; Plötz, C. Diabetes mellitus—A free radical-associated disease. Results of adjuvant antioxidant supplementation. Z. Gesamte Inn. Med. 1993, 48, 223–232. [Google Scholar] [PubMed]
- Jacob, S.; Henriksen, E.J.; Schiemann, A.L.; Simon, I.; Clancy, D.E.; Tritschler, H.J.; Jung, W.I.; Augustin, H.J.; Dietze, G.J. Enhancement of glucose disposal in patients with type 2 diabetes by alpha-lipoic acid. Arzneimittelforschung 1995, 45, 872–874. [Google Scholar] [PubMed]
- Ziegler, D.; Hanefeld, M.; Ruhnau, K.J.; Meissner, H.P.; Lobisch, M.; Schütte, K.; Gries, F.A. Treatment of symptomatic diabetic peripheral neuropathy with the anti-oxidant alpha-lipoic acid. A 3-week multicentre randomized controlled trial (ALADIN Study). Diabetologia 1995, 38, 1425–1433. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, D.; Schatz, H.; Conrad, F.; Gries, F.A.; Ulrich, H.; Reichel, G. Effects of treatment with the antioxidant alpha-lipoic acid on cardiac autonomic neuropathy in NIDDM patients. A 4-month randomized controlled multicenter trial (DEKAN Study). Deutsche Kardiale Autonome Neuropathie. Diabetes Care 1997, 20, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Strokov, I.A.; Kozlova, N.A.; Mozolevskiĭ, IuV; Miasoedov, S.P.; Iakhno, N.N. The efficacy of the intravenous administration of the trometamol salt of thioctic (alpha-lipoic) acid in diabetic neuropathy. Zh. Nevrol. Psikhiatr. Im. S. S. Korsakova 1999, 99, 18–22. [Google Scholar]
- Jacob, S.P.; Ruus, P.R.; Hermann, R.; Tritschler, H.J.; Maerker, E.; Renn, W.; Augustin, H.J.; Dietze, G.J.; Rett, K. Oral administration of RAC-alpha-lipoic acid modulates insulin sensitivity in patients with type-2 diabetes mellitus: A placebo-controlled pilot trial. Free Radic. Biol. Med. 1999, 27, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, D.; Hanefeld, M.; Ruhnau, K.J.; Hasche, H.; Lobisch, M.; Schütte, K.; Kerum, G.; Malessa, R. Treatment of symptomatic diabetic polyneuropathy with the antioxidant alpha-lipoic acid: A 7-month multicenter randomized controlled trial (ALADIN III study). ALADIN III Study Group. Alpha-lipoic acid in diabetic neuropathy. Diabetes Care 1999, 22, 1296–1301. [Google Scholar] [CrossRef] [PubMed]
- Reljanovic, M.G.; Reichel, G.K.; Rett, K.; Lobisch, M.; Schuette, K.; Möller, W.; Tritschler, H.J.; Mehnert, H. Treatment of diabetic polyneuropathy with the antioxidant thioctic acid (alpha-lipoic acid): A two year multicenter randomized double-blind placebo-controlled trial (ALADIN II). Alpha lipoic acid in diabetic neuropathy. Free Radic. Res. 1999, 31, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Ruhnau, K.J.; Meissner, H.P.; Finn, J.R.; Reljanovic, M.; Lobisch, M.; Schütte, K.; Nehrdich, D.; Tritschler, H.J.; Mehnert, H.; Ziegler, D. Effects of 3-week oral treatment with the antioxidant thioctic acid (alpha-lipoic acid) in symptomatic diabetic polyneuropathy. Diabet. Med. 1999, 16, 1040–1043. [Google Scholar] [CrossRef] [PubMed]
- Negrişanu, G.; Roşu, M.; Bolte, B.; Lefter, D.; Dabelea, D. Effects of 3-month treatment with the antioxidant alpha-lipoic acid in diabetic peripheral neuropathy. Rom. J. Intern. Med. 1999, 37, 297–306. [Google Scholar] [PubMed]
- Androne, L.; Gavan, N.A.; Veresiu, I.A.; Orasan, R. In vivo effect of lipoic acid on lipid peroxidation in patients with diabetic neuropathy. In Vivo 2000, 14, 327–330. [Google Scholar] [PubMed]
- Haak, E.; Usadel, K.H.; Kusterer, K.; Amini, P.; Frommeyer, R.; Tritschler, H.J.; Haak, T. Effects of alpha-lipoic acid on microcirculation in patients with peripheral diabetic neuropathy. Exp. Clin. Endocrinol. Diabetes 2000, 108, 168–174. [Google Scholar] [CrossRef]
- Evans, J.L.; Heymann, C.J.; Goldfine, I.D.; Gavin, L.A. Pharmacokinetics, tolerability, and fructosamine-lowering effect of a novel, controlled-release formulation of alpha-lipoic acid. Endocr. Pract. 2002, 8, 29–35. [Google Scholar] [CrossRef] [PubMed]
- Ametov, A.S.; Barinov, A.; Dyck, P.J.; Hermann, R.; Kozlova, N.; Litchy, W.J.; Low, P.A.; Nehrdich, D.; Novosadova, M.; O’Brien, P.C.; et al. The sensory symptoms of diabetic polyneuropathy are improved with alpha-lipoic acid: The SYDNEY trial. Diabetes Care 2003, 26, 770–776. [Google Scholar] [CrossRef] [PubMed]
- Hahm, J.R.; Kim, B.J.; Kim, K.W. Clinical experience with thioctacid (thioctic acid) in the treatment of distal symmetric polyneuropathy in Korean diabetic patients. J. Diabetes Complicat. 2004, 18, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Ziegler, D.; Ametov, A.; Barinov, A.; Dyck, P.J.; Gurieva, I.; Low, P.A.; Munzel, U.; Yakhno, N.; Raz, I.; Novosadova, M.; et al. Oral treatment with alpha-lipoic acid improves symptomatic diabetic polyneuropathy: The SYDNEY 2 trial. Diabetes Care 2006, 29, 2365–2370. [Google Scholar] [CrossRef] [PubMed]
- Kamenova, P. Improvement of insulin sensitivity in patients with type 2 diabetes mellitus after oral administration of alpha-lipoic acid. Hormones 2006, 5, 251–258. [Google Scholar]
- Liu, F.; Zhang, Y.; Yang, M.; Liu, B.; Shen, Y.D.; Jia, W.P.; Xiang, K.S. Curative effect of alpha-lipoic acid on peripheral neuropathy in type 2 diabetes: A clinical study. Zhonghua Yi Xue Za Zhi 2007, 87, 2706–2709. [Google Scholar] [PubMed]
- Xiang, G.D.; Sun, H.L.; Zhao, L.S.; Hou, J.; Yue, L.; Xu, L. The antioxidant alpha-lipoic acid improves endothelial dysfunction induced by acute hyperglycaemia during OGTT in impaired glucose tolerance. Clin. Endocrinol. 2008, 68, 716–723. [Google Scholar] [CrossRef]
- Bureković, A.; Terzić, M.; Alajbegović, S.; Vukojević, Z.; Hadzić, N. The role of alpha-lipoic acid in diabetic polyneuropathy treatment. Bosn. J. Basic Med. Sci. 2008, 8, 341–245. [Google Scholar] [PubMed]
- Heinisch, B.B.; Francesconi, M.; Mittermayer, F.; Schaller, G.; Gouya, G.; Wolzt, M.; Pleiner, J. Alpha-lipoic acid improves vascular endothelial function in patients with type 2 diabetes: A placebo-controlled randomized trial. Eur. J. Clin. Investig. 2010, 40, 148–154. [Google Scholar] [CrossRef]
- Palacka, P.; Kucharska, J.; Murin, J.; Dostalova, K.; Okkelova, A.; Cizova, M.; Waczulikova, I.; Moricova, S.; Gvozdjakova, A. Complementary therapy in diabetic patients with chronic complications: A pilot study. Bratisl. Lek. Listy 2010, 111, 205–211. [Google Scholar] [PubMed]
- Gu, X.M.; Zhang, S.S.; Wu, J.C.; Tang, Z.Y.; Lu, Z.Q.; Li, H.; Liu, C.; Chen, L.; Ning, G. Efficacy and safety of high-dose α-lipoic acid in the treatment of diabetic polyneuropathy. Zhonghua Yi Xue Za Zhi 2010, 90, 2473–2476. [Google Scholar] [PubMed]
- Xiang, G.; Pu, J.; Yue, L.; Hou, J.; Sun, H. α-Lipoic acid can improve endothelial dysfunction in subjects with impaired fasting glucose. Metabolism 2011, 60, 480–485. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira, A.M.; Rondó, P.H.; Luzia, L.A.; D'Abronzo, F.H.; Illison, V.K. The effects of lipoic acid and α-tocopherol supplementation on the lipid profile and insulin sensitivity of patients with type 2 diabetes mellitus: A randomized, double-blind, placebo-controlled trial. Diabetes Res. Clin. Pract. 2011, 92, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Ansar, H.; Mazloom, Z.; Kazemi, F.; Hejazi, N. Effect of alpha-lipoic acid on blood glucose, insulin resistance and glutathione peroxidase of type 2 diabetic patients. Saudi Med. J. 2011, 32, 584–588. [Google Scholar] [PubMed]
- Ziegler, D.; Low, P.A.; Litchy, W.J.; Boulton, A.J.; Vinik, A.I.; Freeman, R.; Samigull, R.; Tritschler, H.; Munzel, U.; Maus, J.; et al. Efficacy and safety of antioxidant treatment with α-lipoic acid over 4 years in diabetic polyneuropathy: The NATHAN 1 trial. Diabetes Care 2011, 34, 2054–2060. [Google Scholar] [CrossRef] [PubMed]
- Haritoglou, C.; Gerss, J.; Hammes, H.P.; Kampik, A.; Ulbig, M.W.; RETIPON Study Group. Alpha-lipoic acid for the prevention of diabetic macular edema. Ophthalmologica 2011, 226, 127–137. [Google Scholar] [CrossRef] [PubMed]
- Rahman, S.T.; Merchant, N.; Haque, T.; Wahi, J.; Bhaheetharan, S.; Ferdinand, K.C.; Khan, B.V. The impact of lipoic acid on endothelial function and proteinuria in quinapril-treated diabetic patients with stage I hypertension: Results from the QUALITY study. J. Cardiovasc. Pharmacol. Ther. 2012, 17, 139–145. [Google Scholar] [CrossRef] [PubMed]
- Bertolotto, F.; Massone, A. Combination of alpha lipoic acid and superoxide dismutase leads to physiological and symptomatic improvements in diabetic neuropathy. Drugs R&D 2012, 12, 29–34. [Google Scholar] [CrossRef]
- Porasuphatana, S.; Suddee, S.; Nartnampong, A.; Konsil, J.; Harnwong, B.; Santaweesuk, A. Glycemic and oxidative status of patients with type 2 diabetes mellitus following oral administration of alpha-lipoic acid: A randomized double-blinded placebo-controlled study. Asia Pac. J. Clin. Nutr. 2012, 21, 12–21. [Google Scholar] [PubMed]
- Ibrahimpasic, K. Alpha lipoic acid and glycaemic control in diabetic neuropathies at type 2 diabetes treatment. Med. Arch. 2013, 67, 7–9. [Google Scholar] [CrossRef] [PubMed]
- Tankova, T.; Koev, D.; Dakovska, L. Alpha-lipoic acid in the treatment of autonomic diabetic neuropathy (controlled, randomized, open-label study). Rom. J. Intern. Med. 2004, 42, 457–464. [Google Scholar] [PubMed]
- Huang, E.A.; Gitelman, S.E. The effect of oral alpha-lipoic acid on oxidative stress in adolescents with type 1 diabetes mellitus. Pediat. Diabetes 2008, 9, 69–73. [Google Scholar] [CrossRef]
- Mollo, R.; Zaccardi, F.; Scalone, G.; Scavone, G.; Rizzo, P.; Navarese, E.P.; Manto, A.; Pitocco, D.; Lanza, G.A.; Ghirlanda, G.; et al. Effect of α-lipoic acid on platelet reactivity in type 1 diabetic patients. Diabetes Care 2012, 35, 196–197. [Google Scholar] [CrossRef] [PubMed]
- Morcos, M.; Borcea, V.; Isermann, B.; Gehrke, S.; Ehret, T.; Henkels, M.; Schiekofer, S.; Hofmann, M.; Amiral, J.; Tritschler, H.; et al. Effect of alpha-lipoic acid on the progression of endothelial cell damage and albuminuria in patients with diabetes mellitus: An exploratory study. Diabetes Res. Clin. Pract. 2001, 5, 175–183. [Google Scholar] [CrossRef]
- Noori, N.; Tabibi, H.; Hosseinpanah, F.; Hedayati, M.; Nafar, M. Effects of combined lipoic acid and pyridoxine on albuminuria, advanced glycation end-products, and blood pressure in diabetic nephropathy. Int. J. Vitam. Nutr. Res. 2013, 83, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Hegazy, S.K.; Tolba, O.A.; Mostafa, T.M.; Eid, M.A.; el-Afify, D.R. Alpha-lipoic acid improves subclinical left ventricular dysfunction in asymptomatic patients with type 1 diabetes. Rev. Diabet. Stud. 2013, 10, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Huang, Z.; Wan, X.; Liu, J.; Deng, W.; Chen, A.; Liu, L.; Liu, J.; Wei, G.; Li, H.; Fang, D.; et al. Short-term continuous subcutaneous insulin infusion combined with insulin sensitizers rosiglitazone, metformin, or antioxidant α-lipoic acid in patients with newly diagnosed type 2 diabetes mellitus. Diabetes Technol. Ther. 2013, 15, 859–869. [Google Scholar] [CrossRef] [PubMed]
- Mitkov, M.D.; Aleksandrova, I.Y.; Orbetzova, M.M. Effect of transdermal testosterone or alpha-lipoic acid on erectile dysfunction and quality of life in patients with type 2 diabetes mellitus. Folia Med. 2013, 55, 55–63. [Google Scholar]
- Pop-Busui, R.; Stevens, M.J.; Raffel, D.M.; White, E.A.; Mehta, M.; Plunkett, C.D.; Brown, M.B.; Feldman, E.L. Effects of triple antioxidant therapy on measures of cardiovascular autonomic neuropathy and on myocardial blood flow in type 1 diabetes: A randomized controlled trial. Diabetologia 2013, 56, 1835–1844. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhang, Y.; Gao, X.; Wu, J.; Jiao, X.; Zhao, J.; Lv, X. Investigating the role of backward walking therapy in alleviating plantar pressure of patients with diabetic peripheral neuropathy. Arch. Phys. Med. Rehabil. 2014, 95, 832–839. [Google Scholar] [CrossRef] [PubMed]
- Yadav, V.; Marracci, G.; Lovera, J.; Woodward, W.; Bogardus, K.; Marquardt, W.; Shinto, L.; Morris, C.; Bourdette, D. Lipoic acid in multiple sclerosis: A pilot study. Mult. Sclerosis 2005, 11, 159–165. [Google Scholar] [CrossRef]
- Khalili, M.; Azimi, A.; Izadi, V.; Eghtesadi, S.; Mirshafiey, A.; Sahraian, M.A.; Motevalian, A.; Norouzi, A.; Sanoobar, M.; Eskandari, G.; et al. Does lipoic acid consumption affect the cytokine profile in multiple sclerosis patients: A double-blind, placebo-controlled, randomized clinical trial. Neuroimmunomodulation 2014, 21, 291–296. [Google Scholar] [CrossRef] [PubMed]
- Bae, S.C.; Jung, W.J.; Lee, E.J.; Yu, R.; Sung, M.K. Effects of antioxidant supplements intervention on the level of plasma inflammatory molecules and disease severity of rheumatoid arthritis patients. J. Am. Coll. Nutr. 2009, 28, 56–62. [Google Scholar] [CrossRef] [PubMed]
- Galasko, D.R.; Peskind, E.; Clark, C.M.; Quinn, J.F.; Ringman, J.M.; Jicha, G.A.; Cotman, C.; Cottrell, B.; Montine, T.J.; Thomas, R.G.; et al. Alzheimer’s disease cooperative study. Antioxidants for Alzheimer disease: A randomized clinical trial with cerebrospinal fluid biomarker measures. Arch. Neurol. 2012, 69, 836–841. [Google Scholar] [PubMed]
- Magis, D.; Ambrosini, A.; Sándor, P.; Jacquy, J.; Laloux, P.; Schoenen, J. A randomized double-blind placebo-controlled trial of thioctic acid in migraine prophylaxis. Headache 2007, 47, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Di Geronimo, G.; Caccese, A.F.; Caruso, L.; Soldati, A.; Passaretti, U. Treatment of carpal tunnel syndrome with alpha-lipoic acid. Eur. Rev. Med. Pharmacol. Sci. 2009, 13, 133–139. [Google Scholar] [PubMed]
- Memeo, A.; Loiero, M. Thioctic acid and acetyl-l-carnitine in the treatment of sciatic pain caused by a herniated disc: A randomized, double-blind, comparative study. Clin. Drug Investig. 2008, 28, 495–500. [Google Scholar] [CrossRef] [PubMed]
- Ranieri, M.; Sciuscio, M.; Cortese, A.M.; Santamato, A.; di Teo, L.; Ianieri, G.; Bellomo, R.G.; Stasi, M.; Megna, M. The use of alpha-lipoic acid (ALA), gamma linolenic acid (GLA) and rehabilitation in the treatment of back pain: Effect on health-related quality of life. Int. J. Immunopathol. Pharmacol. 2009, 22, 45–50. [Google Scholar] [PubMed]
- Shinto, L.; Quinn, J.; Montine, T.; Dodge, H.H.; Woodward, W.; Baldauf-Wagner, S.; Waichunas, D.; Bumgarner, L.; Bourdette, D.; Silbert, L.; et al. A randomized placebo-controlled pilot trial of omega-3 fatty acids and alpha lipoic acid in Alzheimer’s disease. J. Alzheimers Dis. 2014, 38, 111–120. [Google Scholar] [PubMed]
- Dünschede, F.; Erbes, K.; Kircher, A.; Westermann, S.; Seifert, J.; Schad, A.; Oliver, K.; Kiemer, A.K.; Theodor, J. Reduction of ischemia reperfusion injury after liver resection and hepatic inflow occlusion by alpha-lipoic acid in humans. World J. Gastroenterol. 2006, 12, 6812–6817. [Google Scholar] [PubMed]
- Melhem, A.; Stern, M.; Shibolet, O.; Israeli, E.; Ackerman, Z.; Pappo, O.; Hemed, N.; Rowe, M.; Ohana, H.; Zabrecky, G.; et al. Treatment of chronic hepatitis C virus infection via antioxidants: Results of a phase I clinical trial. J. Clin. Gastroenterol. 2005, 39, 737–742. [Google Scholar] [CrossRef] [PubMed]
- Koh, E.H.; Lee, W.J.; Lee, S.A.; Kim, E.H.; Cho, E.H.; Jeong, E.; Kim, D.W.; Kim, M.S.; Park, J.Y.; Park, K.G.; et al. Effects of alpha-lipoic acid on body weight in obese subjects. Am. J. Med. 2011, 124, 85.e1-8. [Google Scholar] [CrossRef] [PubMed]
- McNeilly, A.M.; Davison, G.W.; Murphy, M.H.; Nadeem, N.; Trinick, T.; Duly, E.; Novials, A.; McEneny, J. Effect of α-lipoic acid and exercise training on cardiovascular disease risk in obesity with impaired glucose tolerance. Lipids Health Dis. 2011, 10, 217. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Han, P.; Wu, N.; He, B.; Lu, Y.; Li, S.; Liu, Y.; Zhao, S.; Liu, L.; Li, Y. Amelioration of lipid abnormalities by α-lipoic acid through antioxidative and anti-inflammatory effects. Obesity 2011, 19, 1647–1653. [Google Scholar] [CrossRef] [PubMed]
- Skroza, N.; Proietti, I.; Bernardini, N.; la Viola, G.; Nicolucci, F.; Pampena, R.; Tolino, E.; Zuber, S.; Mancini, M.T.; Soccodato, V.; et al. Efficacy of food supplement to improve metabolic syndrome parameters in patients affected by moderate to severe psoriasis during anti-TNFα treatment. G. Ital. Dermatol. Venereol. 2013, 148, 661–665. [Google Scholar] [PubMed]
- Manning, P.J.; Sutherland, W.H.; Williams, S.M.; Walker, R.J.; Berry, E.A.; de Jong, S.A.; Ryalls, A.R. The effect of lipoic acid and vitamin E therapies in individuals with the metabolic syndrome. Nutr. Metab. Cardiovasc. Dis. 2013, 23, 543–549. [Google Scholar] [CrossRef] [PubMed]
- McMackin, C.J.; Widlansky, M.E.; Hamburg, N.M. Effect of combined treatment with alpha-lipoic acid and acetyl-l-carnitine on vascular function and blood pressure in patients with coronary artery disease. J. Clin. Hypertens. 2007, 9, 249–255. [Google Scholar] [CrossRef]
- Li, R.J.; Ji, W.Q.; Pang, J.J.; Wang, J.L.; Chen, Y.G.; Zhang, Y. Alpha-lipoic acid ameliorates oxidative stress by increasing aldehyde dehydrogenase-2 activity in patients with acute coronary syndrome. Tohoku J. Exp. Med. 2013, 229, 45–51. [Google Scholar] [CrossRef] [PubMed]
- Vincent, H.K.; Bourguignon, C.M.; Vincent, K.R.; Taylor, A.G. Effects of alpha-lipoic acid supplementation in peripheral arterial disease: A pilot study. J. Altern. Complement. Med. 2007, 13, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Leong, J.Y.; van der Merwe, J.; Pepe, S.; Bailey, M.; Perkins, A.; Lymbury, R.; Esmore, D.; Marasco, S.; Rosenfeldt, F. Perioperative metabolic therapy improves redox status and outcomes in cardiac surgery patients: A randomised trial. Heart Lung Circ. 2010, 19, 584–591. [Google Scholar] [CrossRef] [PubMed]
- Chang, J.W.; Lee, E.K.; Kim, T.H.; Min, W.K.; Chun, S.; Lee, K.U.; Kim, S.B.; Park, J.S. Effects of alpha-lipoic acid on the plasma levels of asymmetric dimethylarginine in diabetic end-stage renal disease patients on hemodialysis: A pilot study. Am. J. Nephrol. 2007, 27, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Ramos, L.F.; Kane, J.; McMonagle, E.; Le, P.; Wu, P.; Shintani, A.; Ikizler, T.A.; Himmelfarb, J. Effects of combination tocopherols and alpha lipoic acid therapy on oxidative stress and inflammatory biomarkers in chronic kidney disease. J. Ren. Nutr. 2011, 21, 211–218. [Google Scholar] [CrossRef] [PubMed]
- Khabbazi, T.; Mahdavi, R.; Safa, J.; Pour-Abdollahi, P. Effects of alpha-lipoic acid supplementation on inflammation, oxidative stress, and serum lipid profile levels in patients with end-stage renal disease on hemodialysis. J. Ren. Nutr. 2012, 22, 244–250. [Google Scholar] [CrossRef] [PubMed]
- Himmelfarb, J.; Ikizler, T.A.; Ellis, C.; Wu, P.; Shintani, A.; Dalal, S.; Kaplan, M.; Chonchol, M.; Hakim, R.M. Provision of antioxidant therapy in hemodialysis (PATH): A randomized clinical trial. J. Am. Soc. Nephrol. 2014, 25, 623–633. [Google Scholar] [CrossRef] [PubMed]
- Lott, I.T.; Doran, E.; Nguyen, V.Q.; Tournay, A.; Head, E.; Gillen, D.L. Down syndrome and dementia: A randomized, controlled trial of antioxidant supplementation. Am. J. Med. Genet. A 2011, 155A, 1939–1948. [Google Scholar] [CrossRef]
- Martins, V.D.; Manfredini, V.; Peralba, M.C.; Benfato, M.S. Alpha-lipoic acid modifies oxidative stress parameters in sickle cell trait subjects and sickle cell patients. Clin. Nutr. 2009, 28, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, M.C.; MacDonald, J.R.; Mahoney, D.J.; Parise, G.; Beal, M.F.; Tarnopolsky, M.A. Beneficial effects of creatine, CoQ10, and lipoic acid in mitochondrial disorders. Muscle Nerve 2007, 35, 235–242. [Google Scholar] [CrossRef] [PubMed]
- Femiano, F.; Gombos, F.; Scully, C.; Busciolano, M.; de Luca, P. Burning mouth syndrome (BMS): Controlled open trial of the efficacy of alpha-lipoic acid (thioctic acid) on symptomatology. Oral Dis. 2000, 6, 274–277. [Google Scholar] [CrossRef] [PubMed]
- Carbone, M.; Pentenero, M.; Carrozzo, M.; Ippolito, A.; Gandolfo, S. Lack of efficacy of alpha-lipoic acid in burning mouth syndrome: A double-blind, randomized, placebo-controlled study. Eur. J. Pain 2009, 13, 492–496. [Google Scholar] [CrossRef] [PubMed]
- López-Jornet, P.; Camacho-Alonso, F.; Leon-Espinosa, S. Efficacy of alpha lipoic acid in burning mouth syndrome: A randomized, placebo-treatment study. J. Oral. Rehabil. 2009, 36, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Marino, R.; Torretta, S.; Capaccio, P.; Pignataro, L.; Spadari, F. Different therapeutic strategies for burning mouth syndrome: Preliminary data. J. Oral Pathol. Med. 2010, 39, 611–616. [Google Scholar] [CrossRef] [PubMed]
- López-D’Alessandro, E.; Escovich, L. Combination of alpha lipoic acid and gabapentin, its efficacy in the treatment of Burning Mouth Syndrome: A randomized, double-blind, placebo controlled trial. Med. Oral Patol. Oral Cir. Bucal. 2011, 16, e635–e640. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, G.; Macciò, A.; Madeddu, C.; Gramignano, G.; Lusso, M.R.; Serpe, R.; Massa, E.; Astara, G.; Deiana, L. A phase II study with antioxidants, both in the diet and supplemented, pharmaconutritional support, progestagen, and anti-cyclooxygenase-2 showing efficacy and safety in patients with cancer-related anorexia/cachexia and oxidative stress. Cancer Epidemiol. Biomark. Prev. 2006, 15, 1030–1034. [Google Scholar] [CrossRef]
- Mantovani, G.; Macciò, A.; Madeddu, C.; Gramignano, G.; Serpe, R.; Massa, E.; Dessì, M.; Tanca, F.M.; Sanna, E.; Deiana, L.; et al. Randomized phase III clinical trial of five different arms of treatment for patients with cancer cachexia: Interim results. Nutrition 2008, 24, 305–313. [Google Scholar] [CrossRef] [PubMed]
- Jariwalla, R.J.; Lalezari, J.; Cenko, D.; Mansour, S.E.; Kumar, A.; Gangapurkar, B.; Nakamura, D. Restoration of blood total glutathione status and lymphocyte function following alpha-lipoic acid supplementation in patients with HIV infection. J. Altern. Complement. Med. 2008, 14, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Milazzo, L.; Menzaghi, B.; Caramma, I.; Nasi, M.; Sangaletti, O.; Cesari, M.; Zanone Poma, B.; Cossarizza, A.; Antinori, S.; Galli, M. Effect of antioxidants on mitochondrial function in HIV-1-related lipoatrophy: A pilot study. AIDS Res. Hum. Retroviruses 2010, 26, 1207–1214. [Google Scholar] [CrossRef] [PubMed]
- Dell’Anna, M.L.; Mastrofrancesco, A.; Sala, R.; Venturini, M.; Ottaviani, M.; Vidolin, A.P.; Leone, G.; Calzavara, P.G.; Westerhof, W.; Picardo, M. Antioxidants and narrow band-UVB in the treatment of vitiligo: A double-blind placebo controlled trial. Clin. Exp. Dermatol. 2007, 32, 631–636. [Google Scholar] [CrossRef] [PubMed]
- Mainini, G.; Rotondi, M.; di Nola, K.; Pezzella, M.T.; Iervolino, S.A.; Seguino, E.; D’Eufemia, D.; Iannicelli, I.; Torella, M. Oral supplementation with antioxidant agents containing alpha lipoic acid: Effects on postmenopausal bone mass. Clin. Exp. Obstet. Gynecol. 2012, 39, 489–493. [Google Scholar] [PubMed]
- Garrido-Maraver, J.; Cordero, M.D.; Oropesa-Avila, M.; Oropesa-Avila, M.; Vega, A.F.; de la Mata, M.; Pavon, A.D.; Alcocer-Gomez, E.; Calero, C.P.; Paz, M.V.; et al. Clinical applications of coenzyme Q10. Front. Biosci. 2014, 19, 619–633. [Google Scholar] [CrossRef]
- Singh, R.B.; Niaz, M.A. Serum concentration of lipoprotein(a) decreases on treatment with hydrosoluble coenzyme Q10 in patients with coronary artery disease: Discovery of a new role. Int. J. Cardiol. 1999, 68, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.B.; Niaz, M.A.; Rastogi, S.S.; Shukla, P.K.; Thakur, A.S. Effect of hydrosoluble coenzyme Q10 on blood pressures and insulin resistance in hypertensive patients with coronary artery disease. J. Hum. Hypertens. 1999, 13, 203–208. [Google Scholar] [CrossRef] [PubMed]
- Tiano, L.; Belardinelli, R.; Carnevali, P.; Principi, F.; Seddaiu, G.; Littarru, G.P. Effect of coenzyme Q10 administration on endothelial function and extracellular superoxide dismutase in patients with ischaemic heart disease: A double-blind, randomized controlled study. Eur. Heart J. 2007, 28, 2249–2255. [Google Scholar] [CrossRef] [PubMed]
- Belardinelli, R.; Muçaj, A.; Lacalaprice, F.; Solenghi, M.; Principi, F.; Tiano, L.; Littarru, G.P. Coenzyme Q10 improves contractility of dysfunctional myocardium in chronic heart failure. Biofactors 2005, 25, 137–145. [Google Scholar] [CrossRef] [PubMed]
- Dai, Y.L.; Luk, T.H.; Yiu, K.H.; Wang, M.; Yip, P.M.; Lee, S.W.; Li, S.W.; Tam, S.; Fong, B.; Lau, C.P.; et al. Reversal of mitochondrial dysfunction by coenzyme Q10 supplement improves endothelial function in patients with ischaemic left ventricular systolic dysfunction: A randomized controlled trial. Atherosclerosis 2011, 216, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Lee, B.J.; Huang, Y.C.; Chen, S.J.; Lin, P.T. Coenzyme Q10 supplementation reduces oxidative stress and increases antioxidant enzyme activity in patients with coronary artery disease. Nutrition 2012, 28, 250–255. [Google Scholar] [CrossRef] [PubMed]
- Hofman-Bang, C.; Rehnqvist, N.; Swedberg, K.; Wiklund, I.; Aström, H. Coenzyme Q10 as an adjunctive in the treatment of chronic congestive heart failure. The Q10 Study Group. J. Card. Fail. 1995, 1, 101–107. [Google Scholar] [CrossRef] [PubMed]
- Munkholm, H.; Hansen, H.H.; Rasmussen, K. Coenzyme Q10 treatment in serious heart failure. Biofactors 1999, 9, 285–289. [Google Scholar] [CrossRef]
- Khatta, M.; Alexander, B.S.; Krichten, C.M.; Fisher, M.L.; Freudenberger, R.; Robinson, S.W.; Gottlieb, S.S. The effect of coenzyme Q10 in patients with congestive heart failure. Ann. Intern. Med. 2000, 132, 636–640. [Google Scholar] [CrossRef] [PubMed]
- Berman, M.; Erman, A.; Ben-Gal, T.; Dvir, D.; Georghiou, G.P.; Stamler, A.; Vered, Y.; Vidne, B.A.; Aravot, D. Coenzyme Q10 in patients with end-stage heart failure awaiting cardiac transplantation: A randomized, placebo-controlled study. Clin. Cardiol. 2004, 27, 295–299. [Google Scholar] [CrossRef] [PubMed]
- Damian, M.S.; Ellenberg, D.; Gildemeister, R.; Lauermann, J.; Simonis, G.; Sauter, W.; Georgi, C. Coenzyme Q10 combined with mild hypothermia after cardiac arrest: A preliminary study. Circulation 2004, 110, 3011–3016. [Google Scholar] [CrossRef] [PubMed]
- Witte, K.K.; Nikitin, N.P.; Parker, A.C.; von Haehling, S.; Volk, H.D.; Anker, S.D.; Clark, A.L.; Cleland, J.G. The effect of micronutrient supplementation on quality-of-life and left ventricular function in elderly patients with chronic heart failure. Eur. Heart J. 2005, 26, 2238–2244. [Google Scholar] [CrossRef] [PubMed]
- Langsjoen, P.H.; Langsjoen, A.M. Supplemental ubiquinol in patients with advanced congestive heart failure. Biofactors 2008, 32, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Singh, R.B.; Saxena, M.; Niaz, M.A.; Josh, S.R.; Chattopadhyay, P.; Mechirova, V.; Pella, D.; Fedacko, J. Effect of carni Q-gel (ubiquinol and carnitine) on cytokines in patients with heart failure in the Tishcon study. Acta Cardiol. 2007, 62, 349–354. [Google Scholar] [CrossRef] [PubMed]
- Belcaro, G.; Cesarone, M.R.; Dugall, M.; Hosoi, M.; Ippolito, E.; Bavera, P.; Grossi, M.G. Investigation of pycnogenol in combination with coenzyme Q10 in heart failure patients (NYHA II/III). Panminerva Med. 2010, 52, 21–25. [Google Scholar] [PubMed]
- Fumagalli, S.; Fattirolli, F.; Guarducci, L.; Cellai, T.; Baldasseroni, S.; Tarantini, F.; di Bari, M.; Masotti, G.; Marchionni, N. Coenzyme Q10 terclatrate and creatine in chronic heart failure: A randomized, placebo-controlled, double-blind study. Clin. Cardiol. 2011, 34, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Kuklinski, B.; Weissenbacher, E.; Fähnrich, A. Coenzyme Q10 and antioxidants in acute myocardial infarction. Mol. Aspects Med. 1994, 15, s143–s147. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.B.; Wander, G.S.; Rastogi, A.; Shukla, P.K.; Mittal, A.; Sharma, J.P.; Mehrotra, S.K.; Kapoor, R.; Chopra, R.K. Randomized, double-blind placebo-controlled trial of coenzyme Q10 in patients with acute myocardial infarction. Cardiovasc. Drugs Ther. 1998, 12, 347–353. [Google Scholar] [CrossRef] [PubMed]
- Singh, R.B.; Neki, N.S.; Kartikey, K.; Pella, D.; Kumar, A.; Niaz, M.A.; Thakur, A.S. Effect of coenzyme Q10 on risk of atherosclerosis in patients with recent myocardial infarction. Mol. Cell. Biochem. 2003, 246, 75–82. [Google Scholar] [CrossRef] [PubMed]
- Permanetter, B.; Rössy, W.; Klein, G.; Weingartner, F.; Seidl, K.F.; Blömer, H. Ubiquinone (coenzyme Q10) in the long-term treatment of idiopathic dilated cardiomyopathy. Eur. Heart J. 1992, 13, 1528–1533. [Google Scholar] [PubMed]
- Langsjoen, P.H.; Folkers, K.; Lyson, K.; Muratsu, K.; Lyson, T.; Langsjoen, P. Pronounced increase of survival of patients with cardiomyopathy when treated with coenzyme Q10 and conventional therapy. Int. J. Tissue React. 1990, 12, 163–168. [Google Scholar] [PubMed]
- Morisco, C.; Trimarco, B.; Condorelli, M. Effect of coenzyme Q10 therapy in patients with congestive heart failure: A long-term multicenter randomized study. Clin. Investig. 1993, 71, S134–S136. [Google Scholar] [CrossRef] [PubMed]
- Ma, A.W.; Zhang, W.; Liu, Z. Effect of protection and repair of injury of mitochondrial membrane-phospholipid on prognosis in patients with dilated cardiomyopathy. Blood Press. Suppl. 1 1996, 3, 53–55. [Google Scholar]
- Sacher, H.L.; Sacher, M.L.; Landau, S.W.; Kersten, R.; Dooley, F.; Sacher, A.; Sacher, M.; Dietrick, K.; Ichkhan, K. The clinical and hemodynamic effects of coenzyme Q10 in congestive cardiomyopathy. Am. J. Ther. 1997, 4, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Soongswang, J.; Sangtawesin, C.; Durongpisitkul, K.; Laohaprasitiporn, D.; Nana, A.; Punlee, K.; Kangkagate, C. The effect of coenzyme Q10 on idiopathic chronic dilated cardiomyopathy in children. Pediatr. Cardiol. 2005, 26, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Caso, G.; Kelly, P.; McNurlan, M.A.; Lawson, W.E. Effect of coenzyme Q10 on myopathic symptoms in patients treated with statins. Am. J. Cardiol. 2007, 99, 1409–1412. [Google Scholar] [CrossRef] [PubMed]
- Kocharian, A.; Shabanian, R.; Rafiei-Khorgami, M.; Kiani, A.; Heidari-Bateni, G. Coenzyme Q10 improves diastolic function in children with idiopathic dilated cardiomyopathy. Cardiol. Young 2009, 19, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Shargorodsky, M.; Debby, O.; Matas, Z.; Zimlichman, R. Effect of long-term treatment with antioxidants (vitamin C, vitamin E, coenzyme Q10 and selenium) on arterial compliance, humoral factors and inflammatory markers in patients with multiple cardiovascular risk factors. Nutr. Metab. 2010, 7, 55. [Google Scholar] [CrossRef]
- Judy, W.V.; Stogsdill, W.W.; Folkers, K. Myocardial preservation by therapy with coenzyme Q10 during heart surgery. Clin. Investig. 1993, 71, S155–S161. [Google Scholar] [CrossRef] [PubMed]
- Taggart, D.P.; Jenkins, M.; Hooper, J.; Hadjinikolas, L.; Kemp, M.; Hue, D.; Bennett, G. Effects of short-term supplementation with coenzyme Q10 on myocardial protection during cardiac operations. Ann. Thorac. Surg. 1996, 61, 829–833. [Google Scholar] [CrossRef] [PubMed]
- Chello, M.; Mastroroberto, P.; Romano, R.; Castaldo, P.; Bevacqua, E.; Marchese, A.R. Protection by coenzyme Q10 of tissue reperfusion injury during abdominal aortic cross-clamping. J. Cardiovasc. Surg. 1996, 37, 229–235. [Google Scholar]
- Zhou, M.; Zhi, Q.; Tang, Y.; Yu, D.; Han, J. Effects of coenzyme Q10 on myocardial protection during cardiac valve replacement and scavenging free radical activity in vitro. J. Cardiovasc. Surg. 1999, 40, 355–361. [Google Scholar]
- Rosenfeldt, F.; Marasco, S.; Lyon, W.; Wowk, M.; Sheeran, F.; Bailey, M.; Esmore, D.; Davis, B.; Pick, A.; Rabinov, M.; et al. Coenzyme Q10 therapy before cardiac surgery improves mitochondrial function and in vitro contractility of myocardial tissue. J. Thorac. Cardiovasc. Surg. 2005, 129, 25–32. [Google Scholar] [CrossRef] [PubMed]
- Keith, M.; Mazer, C.D.; Mikhail, P.; Jeejeebhoy, F.; Briet, F.; Errett, L. Coenzyme Q10 in patients undergoing (coronary artery bypass graft) CABG: Effect of statins and nutritional supplementation. Nutr. Metab. Cardiovasc. Dis. 2008, 18, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Makhija, N.; Sendasgupta, C.; Kiran, U.; Lakshmy, R.; Hote, M.P.; Choudhary, S.K.; Airan, B.; Abraham, R. The role of oral coenzyme Q10 in patients undergoing coronary artery bypass graft surgery. J. Cardiothorac. Vasc. Anesth. 2008, 22, 832–839. [Google Scholar] [CrossRef] [PubMed]
- Alehagen, U.; Johansson, P.; Björnstedt, M.; Rosén, A.; Dahlström, U. Cardiovascular mortality and N-terminal-proBNP reduced after combined selenium and coenzyme Q10 supplementation: A 5-year prospective randomized double-blind placebo-controlled trial among elderly Swedish citizens. Int. J. Cardiol. 2013, 167, 1860–1866. [Google Scholar] [CrossRef] [PubMed]
- Miles, M.V.; Patterson, B.J.; Chalfonte-Evans, M.L.; Horn, P.S.; Hickey, F.J.; Schapiro, M.B.; Steele, P.E.; Tang, P.H.; Hotze, S.L. Coenzyme Q10 (ubiquinol-10) supplementation improves oxidative imbalance in children with trisomy 21. Pediatr. Neurol. 2007, 37, 398–403. [Google Scholar] [CrossRef] [PubMed]
- Tiano, L.; Padella, L.; Santoro, L.; Carnevali, P.; Principi, F.; Brugè, F.; Gabrielli, O.; Littarru, G.P. Prolonged coenzyme Q10 treatment in Down syndrome patients: Effect on DNA oxidation. Neurobiol. Aging 2012, 33, 626.e1-8. [Google Scholar] [CrossRef] [PubMed]
- Sparaco, M.; Gaeta, L.M.; Santorelli, F.M.; Passarelli, C.; Tozzi, G.; Bertini, E.; Simonati, A.; Scaravilli, F.; Taroni, F.; Duyckaerts, C.; et al. Friedreich’s ataxia: Oxidative stress and cytoskeletal abnormalities. J. Neurol. Sci. 2009, 287, 111–118. [Google Scholar] [CrossRef] [PubMed]
- Cooper, J.M.; Korlipara, L.V.; Hart, P.E.; Bradley, J.L.; Schapira, A.H. Coenzyme Q10 and vitamin E deficiency in Friedreich’s ataxia: Predictor of efficacy of vitamin E and coenzyme Q10 therapy. Eur. J. Neurol. 2008, 15, 1371–1379. [Google Scholar] [CrossRef] [PubMed]
- Hart, P.E.; Lodi, R.; Rajagopalan, B.; Bradley, J.L.; Crilley, J.G.; Turner, C.; Blamire, A.M.; Manners, D.; Styles, P.; Schapira, A.H.; et al. Antioxidant treatment of patients with Friedreich ataxia: Four-year follow-up. Arch. Neurol. 2005, 62, 621–626. [Google Scholar] [CrossRef] [PubMed]
- Barbiroli, B.; Frassineti, C.; Martinelli, P.; Iotti, S.; Lodi, R.; Cortelli, P.; Montagna, P. Coenzyme Q10 improves mitochondrial respiration in patients with mitochondrial cytopathies. An in vivo study on brain and skeletal muscle by phosphorous magnetic resonance spectroscopy. Cell. Mol. Biol. 1997, 43, 741–749. [Google Scholar] [PubMed]
- Abe, K.; Matsuo, Y.; Kadekawa, J.; Inoue, S.; Yanagihara, T. Effect of coenzyme Q10 in patients with mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes (MELAS): Evaluation by noninvasive tissue oximetry. J. Neurol. Sci. 1999, 162, 65–68. [Google Scholar] [CrossRef] [PubMed]
- Hanisch, F.; Zierz, S. Only transient increase of serum CoQ subset 10 during long-term CoQ10 therapy in mitochondrial ophthalmoplegia. Eur. J. Med. Res. 2003, 8, 485–491. [Google Scholar] [PubMed]
- Glover, E.I.; Martin, J.; Maher, A.; Thornhill, R.E.; Moran, G.R.; Tarnopolsky, M.A. A randomized trial of coenzyme Q10 in mitochondrial disorders. Muscle Nerve 2010, 42, 739–748. [Google Scholar] [CrossRef] [PubMed]
- Huntington Study Group. A randomized, placebo-controlled trial of coenzyme Q10 and remacemide in Huntington’s disease. Neurology 2001, 57, 397–404. [Google Scholar]
- Huntington Study Group Pre2CARE Investigators; Hyson, H.C.; Kieburtz, K.; Shoulson, I.; McDermott, M.; Ravina, B.; de Blieck, E.A.; Cudkowicz, M.E.; Ferrante, R.J.; Como, P.; et al. Safety and tolerability of high-dosage coenzyme Q10 in Huntington’s disease and healthy subjects. Mov. Disord. 2010, 25, 1924–1928. [Google Scholar] [CrossRef] [PubMed]
- Spurney, C.F.; Rocha, C.T.; Henricson, E.; Florence, J.; Mayhew, J.; Gorni, K.; Pasquali, L.; Pestronk, A.; Martin, G.R.; Hu, F.; et al. CINRG pilot trial of coenzyme Q10 in steroid-treated Duchenne muscular dystrophy. Muscle Nerve 2011, 44, 174–178. [Google Scholar] [CrossRef] [PubMed]
- Folkers, K.; Wolaniuk, J.; Simonsen, R.; Morishita, M.; Vadhanavikit, S. Biochemical rationale and the cardiac response of patients with muscle disease to therapy with coenzyme Q10. Proc. Natl. Acad. Sci. USA 1985, 82, 4513–4516. [Google Scholar] [CrossRef] [PubMed]
- Folkers, K.; Simonsen, R. Two successful double-blind trials with coenzyme Q10 (vitamin Q10) on muscular dystrophies and neurogenic atrophies. Biochim. Biophys. Acta 1995, 1271, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Linnane, A.W.; Kopsidas, G.; Zhang, C.; Yarovaya, N.; Kovalenko, S.; Papakostopoulos, P.; Eastwood, H.; Graves, S.; Richardson, M. Cellular redox activity of coenzyme Q10: Effect of CoQ10 supplementation on human skeletal muscle. Free Radic. Res. 2002, 36, 445–453. [Google Scholar] [CrossRef] [PubMed]
- Shults, C.W.; Oakes, D.; Kieburtz, K.; Beal, M.F.; Haas, R.; Plumb, S.; Juncos, J.L.; Nutt, J.; Shoulson, I.; Carter, J.; et al. Effects of coenzyme Q10 in early Parkinson disease: Evidence of slowing of the functional decline. Arch. Neurol. 2002, 59, 1541–1550. [Google Scholar] [CrossRef] [PubMed]
- Müller, T.; Büttner, T.; Gholipour, A.F.; Kuhn, W. Coenzyme Q10 supplementation provides mild symptomatic benefit in patients with Parkinson’s disease. Neurosci. Lett. 2003, 341, 201–204. [Google Scholar] [CrossRef] [PubMed]
- Storch, A.; Jost, W.H.; Vieregge, P.; Spiegel, J.; Greulich, W.; Durner, J.; Müller, T.; Kupsch, A.; Henningsen, H.; Oertel, W.H.; et al. Randomized, double-blind, placebo-controlled trial on symptomatic effects of coenzyme Q10 in Parkinson disease. Arch. Neurol. 2007, 64, 938–944. [Google Scholar] [CrossRef] [PubMed]
- Sanoobar, M.; Eghtesadi, S.; Azimi, A.; Khalili, M.; Jazayeri, S.; Reza Gohari, M. Coenzyme Q10 supplementation reduces oxidative stress and increases antioxidant enzyme activity in patients with relapsing-remitting multiple sclerosis. Int. J. Neurosci. 2013, 123, 776–782. [Google Scholar] [CrossRef] [PubMed]
- Sanoobar, M.; Eghtesadi, S.; Azimi, A.; Khalili, M.; Khodadadi, B.; Jazayeri, S.; Gohari, M.R.; Aryaeian, N. Coenzyme Q10 supplementation ameliorates inflammatory markers in patients with multiple sclerosis: A double blind, placebo, controlled randomized clinical trial. Nutr. Neurosci. 2014. [Google Scholar] [CrossRef]
- Cordero, M.D.; Cano-García, F.J.; Alcocer-Gómez, E.; de Miguel, M.; Sánchez-Alcázar, J.A. Oxidative stress correlates with headache symptoms in fibromyalgia: Coenzyme Q10 effect on clinical improvement. PLoS One 2012, 7, e35677. [Google Scholar] [CrossRef] [PubMed]
- Cordero, M.D.; Alcocer-Gómez, E.; de Miguel, M.; Culic, O.; Carrión, A.M.; Alvarez-Suarez, J.M.; Bullón, P.; Battino, M.; Fernández-Rodríguez, A.; Sánchez-Alcazar, J.A. Can coenzyme q10 improve clinical and molecular parameters in fibromyalgia? Antioxid. Redox Signal. 2013, 19, 1356–1361. [Google Scholar] [CrossRef]
- Miyamae, T.; Seki, M.; Naga, T.; Uchino, S.; Asazuma, H.; Yoshida, T.; Iizuka, Y.; Kikuchi, M.; Imagawa, T.; Natsumeda, Y.; et al. Increased oxidative stress and coenzyme Q10 deficiency in juvenile fibromyalgia: Amelioration of hypercholesterolemia and fatigue by ubiquinol-10 supplementation. Redox Rep. 2013, 18, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Lister, R.E. An open, pilot study to evaluate the potential benefits of coenzyme Q10 combined with Ginkgo biloba extract in fibromyalgia syndrome. J. Int. Med. Res. 2002, 30, 195–199. [Google Scholar] [CrossRef] [PubMed]
- Kaufmann, P.; Thompson, J.L.; Levy, G.; Buchsbaum, R.; Shefner, J.; Krivickas, L.S.; Katz, J.; Rollins, Y.; Barohn, R.J.; Jackson, C.E.; et al. Phase II trial of CoQ10 for ALS finds insufficient evidence to justify phase III. Ann. Neurol. 2009, 66, 235–244. [Google Scholar] [CrossRef] [PubMed]
- Rozen, T.D.; Oshinsky, M.L.; Gebeline, C.A.; Bradley, K.C.; Young, W.B.; Shechter, A.L.; Silberstein, S.D. Open label trial of coenzyme Q10 as a migraine preventive. Cephalalgia 2002, 22, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Hershey, A.D.; Powers, S.W.; Vockell, A.L.; Lecates, S.L.; Ellinor, P.L.; Segers, A.; Burdine, D.; Manning, P.; Kabbouche, M.A. Coenzyme Q10 deficiency and response to supplementation in pediatric and adolescent migraine. Headache 2007, 47, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Slater, S.K.; Nelson, T.D.; Kabbouche, M.A.; LeCates, S.L.; Horn, P.; Segers, A.; Manning, P.; Powers, S.W.; Hershey, A.D. A randomized, double-blinded, placebo-controlled, crossover, add-on study of CoEnzyme Q10 in the prevention of pediatric and adolescent migraine. Cephalalgia 2011, 31, 897–905. [Google Scholar] [CrossRef] [PubMed]
- Forester, B.P.; Zuo, C.S.; Ravichandran, C.; Harper, D.G.; Du, F.; Kim, S.; Cohen, B.M.; Renshaw, P.F. Coenzyme Q10 effects on creatine kinase activity and mood in geriatric bipolar depression. J. Geriatr. Psychiatry Neurol. 2012, 25, 43–50. [Google Scholar] [CrossRef] [PubMed]
- Stamelou, M.; Reuss, A.; Pilatus, U.; Magerkurth, J.; Niklowitz, P.; Eggert, K.M.; Krisp, A.; Menke, T.; Schade-Brittinger, C.; Oertel, W.H.; et al. Short-term effects of coenzyme Q10 in progressive supranuclear palsy: A randomized, placebo-controlled trial. Mov. Disord. 2008, 23, 942–949. [Google Scholar] [CrossRef] [PubMed]
- Watts, G.F.; Playford, D.A.; Croft, K.D.; Ward, N.C.; Mori, T.A.; Burke, V. Coenzyme Q10 improves endothelial dysfunction of the brachial artery in type II diabetes mellitus. Diabetologia 2002, 45, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, J.M.; Watts, G.F.; Playford, D.A.; Burke, V.; Croft, K.D. Coenzyme Q10 improves blood pressure and glycaemic control: A controlled trial in subjects with type 2 diabetes. Eur. J. Clin. Nutr. 2002, 56, 1137–1142. [Google Scholar] [CrossRef] [PubMed]
- Playford, D.A.; Watts, G.F.; Croft, K.D.; Burke, V. Combined effect of coenzyme Q10 and fenofibrate on forearm microcirculatory function in type 2 diabetes. Atherosclerosis 2003, 168, 169–179. [Google Scholar] [CrossRef] [PubMed]
- Chew, G.T.; Watts, G.F.; Davis, T.M.; Stuckey, B.G.; Beilin, L.J.; Thompson, P.L.; Burke, V.; Currie, P.J. Hemodynamic effects of fenofibrate and coenzyme Q10 in type 2 diabetic subjects with left ventricular diastolic dysfunction. Diabetes Care 2008, 31, 1502–1509. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, S.J.; Chew, G.T.; Watts, G.F. Coenzyme Q10 improves endothelial dysfunction in statin-treated type 2 diabetic patients. Diabetes Care 2009, 32, 810–812. [Google Scholar] [CrossRef] [PubMed]
- Kolahdouz Mohammadi, R.; Hosseinzadeh-Attar, M.J.; Eshraghian, M.R.; Nakhjavani, M.; Khorami, E.; Esteghamati, A. The effect of coenzyme Q10 supplementation on metabolic status of type 2 diabetic patients. Minerva Gastroenterol. Dietol. 2013, 59, 231–236. [Google Scholar] [PubMed]
- Suzuki, S.; Hinokio, Y.; Ohtomo, M.; Hirai, M.; Hirai, A.; Chiba, M.; Kasuga, S.; Satoh, Y.; Akai, H.; Toyota, T. The effects of coenzyme Q10 treatment on maternally inherited diabetes mellitus and deafness, and mitochondrial DNA 3243 (A to G) mutation. Diabetologia 1998, 41, 584–588. [Google Scholar] [CrossRef] [PubMed]
- Henriksen, J.E.; Andersen, C.B.; Hother-Nielsen, O.; Vaag, A.; Mortensen, S.A.; Beck-Nielsen, H. Impact of ubiquinone (coenzyme Q10) treatment on glycaemic control, insulin requirement and well-being in patients with type 1 diabetes mellitus. Diabet. Med. 1999, 16, 312–318. [Google Scholar] [CrossRef] [PubMed]
- Hertz, N.; Lister, R.E. Improved survival in patients with end-stage cancer treated with coenzyme Q10 and other antioxidants: A pilot study. J. Int. Med. Res. 2009, 37, 1961–1971. [Google Scholar] [CrossRef] [PubMed]
- Lockwood, K.; Moesgaard, S.; Folkers, K. Partial and complete regression of breast cancer in patients in relation to dosage of coenzyme Q10. Biochem. Biophys. Res. Commun. 1994, 199, 1504–1508. [Google Scholar] [CrossRef] [PubMed]
- Premkumar, V.G.; Yuvaraj, S.; Sathish, S.; Shanthi, P.; Sachdanandam, P. Anti-angiogenic potential of Coenzyme Q10, riboflavin and niacin in breast cancer patients undergoing tamoxifen therapy. Vascul. Pharmacol. 2008, 48, 191–201. [Google Scholar] [CrossRef] [PubMed]
- Lesser, G.J.; Case, D.; Stark, N.; Williford, S.; Giguere, J.; Garino, L.A.; Naughton, M.J.; Vitolins, M.Z.; Lively, M.O.; Shaw, E.G.; et al. A randomized, double-blind, placebo-controlled study of oral coenzyme Q10 to relieve self-reported treatment-related fatigue in newly diagnosed patients with breast cancer. J. Support Oncol. 2013, 11, 31–42. [Google Scholar] [PubMed]
- Hoenjet, K.M.; Dagnelie, P.C.; Delaere, K.P.; Wijckmans, N.E.; Zambon, J.V.; Oosterhof, G.O. Effect of a nutritional supplement containing vitamin E, selenium, vitamin c and coenzyme Q10 on serum PSA in patients with hormonally untreated carcinoma of the prostate: A randomised placebo-controlled study. Eur. Urol. 2005, 47, 433–439. [Google Scholar] [CrossRef] [PubMed]
- Rusciani, L.; Proietti, I.; Paradisi, A.; Rusciani, A.; Guerriero, G.; Mammone, A.; de Gaetano, A.; Lippa, S. Recombinant interferon alpha-2b and coenzyme Q10 as a postsurgical adjuvant therapy for melanoma: A 3-year trial with recombinant interferon-alpha and 5-year follow-up. Melanoma Res. 2007, 17, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Gazdíková, K.; Gvozdjáková, A.; Kucharská, J.; Spustová, V.; Braunová, Z.; Dzúrik, R. Effect of coenzyme Q10 in patients with kidney diseases. Cas. Lek. Cesk. 2001, 140, 307–310. [Google Scholar] [PubMed]
- Sakata, T.; Furuya, R.; Shimazu, T.; Odamaki, M.; Ohkawa, S.; Kumagai, H. Coenzyme Q10 administration suppresses both oxidative and antioxidative markers in hemodialysis patients. Blood Purif. 2008, 26, 371–378. [Google Scholar] [CrossRef] [PubMed]
- Mori, T.A.; Burke, V.; Puddey, I.; Irish, A.; Cowpland, C.A.; Beilin, L.; Dogra, G.; Watts, G.F. The effects of omega-3 fatty acids and coenzyme Q10 on blood pressure and heart rate in chronic kidney disease: A randomized controlled trial. J. Hypertens. 2009, 27, 1863–1872. [Google Scholar] [CrossRef] [PubMed]
- Shojaei, M.; Djalali, M.; Khatami, M.; Siassi, F.; Eshraghian, M. Effects of carnitine and coenzyme Q10 on lipid profile and serum levels of lipoprotein(a) in maintenance hemodialysis patients on statin therapy. Iran J. Kidney Dis. 2011, 5, 114–118. [Google Scholar] [PubMed]
- Kaikkonen, J.; Nyyssönen, K.; Tomasi, A.; Iannone, A.; Tuomainen, T.P.; Porkkala-Sarataho, E.; Salonen, J.T. Antioxidative efficacy of parallel and combined supplementation with coenzyme Q10 and d-alpha-tocopherol in mildly hypercholesterolemic subjects: A randomized placebo-controlled clinical study. Free Radic. Res. 2000, 33, 329–340. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.J.; Cho, W.J.; Kim, J.K.; Lee, D.C. Effects of coenzyme Q10 on arterial stiffness, metabolic parameters, and fatigue in obese subjects: A double-blind randomized controlled study. J. Med. Food 2011, 14, 386–390. [Google Scholar] [CrossRef] [PubMed]
- Young, J.M.; Florkowski, C.M.; Molyneux, S.L.; McEwan, R.G.; Frampton, C.M.; Nicholls, M.G.; Scott, R.S.; George, P.M. A randomized, double-blind, placebo-controlled crossover study of coenzyme Q10 therapy in hypertensive patients with the metabolic syndrome. Am. J. Hypertens. 2012, 25, 261–270. [Google Scholar] [CrossRef]
- Mabuchi, H.; Nohara, A.; Kobayashi, J.; Kawashiri, M.A.; Katsuda, S.; Inazu, A.; Koizumi, J.; Hokuriku Lipid Research Group. Effects of CoQ10 supplementation on plasma lipoprotein lipid, CoQ10 and liver and muscle enzyme levels in hypercholesterolemic patients treated with atorvastatin: A randomized double-blind study. Atherosclerosis 2007, 195, e182–e189. [Google Scholar] [CrossRef] [PubMed]
- Young, J.M.; Florkowski, C.M.; Molyneux, S.L.; McEwan, R.G.; Frampton, C.M.; George, P.M.; Scott, R.S. Effect of coenzyme Q10 supplementation on simvastatin-induced myalgia. Am. J. Cardiol. 2007, 100, 1400–1403. [Google Scholar] [CrossRef] [PubMed]
- Bookstaver, D.A.; Burkhalter, N.A.; Hatzigeorgiou, C. Effect of coenzyme Q10 supplementation on statin-induced myalgias. Am. J. Cardiol. 2012, 110, 526–529. [Google Scholar] [CrossRef] [PubMed]
- Zlatohlavek, L.; Vrablik, M.; Grauova, B.; Motykova, E.; Ceska, R. The effect of coenzyme Q10 in statin myopathy. Neuro Endocrinol. Lett. 2012, 33, 98–101. [Google Scholar] [PubMed]
- Fedacko, J.; Pella, D.; Fedackova, P.; Hänninen, O.; Tuomainen, P.; Jarcuska, P.; Lopuchovsky, T.; Jedlickova, L.; Merkovska, L.; Littarru, G.P. Coenzyme Q10 and selenium in statin-associated myopathy treatment. Can. J. Physiol. Pharmacol. 2013, 91, 165–170. [Google Scholar] [CrossRef] [PubMed]
- Gvozdjáková, A.; Kucharská, J.; Bartkovjaková, M.; Gazdíková, K.; Gazdík, F.E. Coenzyme Q10 supplementation reduces corticosteroids dosage in patients with bronchial asthma. Biofactors 2005, 25, 235–240. [Google Scholar] [CrossRef] [PubMed]
- Teran, E.; Hernandez, I.; Nieto, B.; Tavara, R.; Ocampo, J.E.; Calle, A. Coenzyme Q10 supplementation during pregnancy reduces the risk of pre-eclampsia. Int. J. Gynaecol. Obstet. 2009, 105, 43–45. [Google Scholar] [CrossRef] [PubMed]
- De Luca, C.; Kharaeva, Z.; Raskovic, D.; Pastore, P.; Luci, A.; Korkina, L. Coenzyme Q10, vitamin E, selenium, and methionine in the treatment of chronic recurrent viral mucocutaneous infections. Nutrition 2012, 28, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Kharaeva, Z.; Gostova, E.; de Luca, C.; Raskovic, D.; Korkina, L. Clinical and biochemical effects of coenzyme Q10, vitamin E, and selenium supplementation to psoriasis patients. Nutrition 2009, 25, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Fogagnolo, P.; Sacchi, M.; Ceresara, G.; Paderni, R.; Lapadula, P.; Orzalesi, N.; Rossetti, L. The effects of topical coenzyme Q10 and vitamin E d-α-tocopheryl polyethylene glycol 1000 succinate after cataract surgery: A clinical and in vivo confocal study. Ophthalmologica 2013, 229, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Safarinejad, M.R.; Safarinejad, S.; Shafiei, N.; Safarinejad, S. Effects of the reduced form of coenzyme Q10 (ubiquinol) on semen parameters in men with idiopathic infertility: A double-blind, placebo controlled, randomized study. J. Urol. 2012, 188, 526–531. [Google Scholar] [CrossRef] [PubMed]
- Gilbert, E.F. Carnitine deficiency. Pathology 1985, 17, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Siliprandi, N.; Siliprandi, D.; Ciman, M. Stimulation of oxidation of mitochondrial fatty acids and of acetate by acetylcarnitine. Biochem. J. 1965, 96, 777–780. [Google Scholar] [PubMed]
- Liu, J.; Head, E.; Kuratsune, H.; Cotman, C.W.; Ames, B.N. Comparison of the effects of l-carnitine and acetyl-l-carnitine on carnitine levels, ambulatory activity, and oxidative stress biomarkers in the brain of old rats. Ann. N. Y. Acad. Sci. 2004, 1033, 117–131. [Google Scholar] [CrossRef] [PubMed]
- Musicco, C.; Capelli, V.; Pesce, V.; Timperio, A.M.; Calvani, M.; Mosconi, L.; Cantatore, P.; Gadaleta, M.N. Rat liver mitochondrial proteome: Changes associated with aging and acetyl-l-carnitine treatment. J. Proteomics 2011, 74, 2536–2547. [Google Scholar] [CrossRef] [PubMed]
- Pesce, V.; Nicassio, L.; Fracasso, F.; Musicco, C.; Cantatore, P.; Gadaleta, M.N. Acetyl-l-carnitine activates the peroxisome proliferator-activated receptor-γ coactivators PGC-1α/PGC-1β-dependent signaling cascade of mitochondrial biogenesis and decreases the oxidized peroxiredoxins content in old rat liver. Rejuvenation Res. 2012, 15, 136–139. [Google Scholar] [CrossRef] [PubMed]
- Bertoli, M.; Battistella, P.A.; Vergani, L.; Naso, A.; Gasparotto, M.L.; Romagnoli, G.F.; Angelini, C. Carnitine deficiency induced during hemodialysis and hyperlipidemia: Effect of replacement therapy. Am. J. Clin. Nutr. 1981, 34, 1496–1500. [Google Scholar] [PubMed]
- Kletzmayr, J.; Mayer, G.; Legenstein, E.; Heinz-Peer, G.; Leitha, T.; Hörl, W.H.; Kovarik, J. Anemia and carnitine supplementation in hemodialyzed patients. Kidney Int. Suppl. 1999, 69, S93–S106. [Google Scholar] [CrossRef] [PubMed]
- Thomas, S.; Fischer, F.P.; Mettang, T.; Pauli-Magnus, C.; Weber, J.; Kuhlmann, U. Effects of l-carnitine on leukocyte function and viability in hemodialysis patients: A double-blind randomized trial. Am. J. Kidney Dis. 1999, 34, 678–687. [Google Scholar] [CrossRef] [PubMed]
- Chazot, C.; Blanc, C.; Hurot, J.M.; Charra, B.; Jean, G.; Laurent, G. Nutritional effects of carnitine supplementation in hemodialysis patients. Clin. Nephrol. 2003, 59, 24–30. [Google Scholar] [CrossRef] [PubMed]
- Vaux, E.C.; Taylor, D.J.; Altmann, P.; Rajagopalan, B.; Graham, K.; Cooper, R.; Bonomo, Y.; Styles, P. Effects of carnitine supplementation on muscle metabolism by the use of magnetic resonance spectroscopy and near-infrared spectroscopy in end-stage renal disease. Nephron Clin. Pract. 2004, 97, c41–c48. [Google Scholar] [CrossRef] [PubMed]
- Steiber, A.L.; Davis, A.T.; Spry, L.; Strong, J.; Buss, M.L.; Ratkiewicz, M.M.; Weatherspoon, L.J. Carnitine treatment improved quality-of-life measure in a sample of Midwestern hemodialysis patients. J. Parenter. Enteral. Nutr. 2006, 30, 10–15. [Google Scholar] [CrossRef]
- Signorelli, S.S.; Fatuzzo, P.; Rapisarda, F.; Neri, S.; Ferrante, M.; Oliveri Conti, G.; Fallico, R.; di Pino, L.; Pennisi, G.; Celotta, G.; et al. A randomised, controlled clinical trial evaluating changes in therapeutic efficacy and oxidative parameters after treatment with propionyl l-carnitine in patients with peripheral arterial disease requiring haemodialysis. Drugs Aging 2006, 23, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Rathod, R.; Baig, M.S.; Khandelwal, P.N.; Kulkarni, S.G.; Gade, P.R.; Siddiqui, S. Results of a single blind, randomized, placebo-controlled clinical trial to study the effect of intravenous l-carnitine supplementation on health-related quality of life in Indian patients on maintenance hemodialysis. Indian J. Med. Sci. 2006, 60, 143–153. [Google Scholar] [CrossRef] [PubMed]
- Duranay, M.; Akay, H.; Yilmaz, F.M.; Senes, M.; Tekeli, N.; Yücel, D. Effects of l-carnitine infusions on inflammatory and nutritional markers in haemodialysis patients. Nephrol. Dial. Transplant. 2006, 21, 3211–3214. [Google Scholar] [CrossRef] [PubMed]
- Verrina, E.; Caruso, U.; Calevo, M.G.; Emma, F.; Sorino, P.; de Palo, T.; Lavoratti, G.; Turrini Dertenois, L.; Cassanello, M.; Cerone, R.; et al. Effect of carnitine supplementation on lipid profile and anemia in children on chronic dialysis. Pediatr. Nephrol. 2007, 22, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Fatouros, I.G.; Douroudos, I.; Panagoutsos, S.; Pasadakis, P.; Nikolaidis, M.G.; Chatzinikolaou, A.; Sovatzidis, A.; Michailidis, Y.; Jamurtas, A.Z.; Mandalidis, D.; et al. Effects of l-carnitine on oxidative stress responses in patients with renal disease. Med. Sci. Sports Exerc. 2010, 42, 1809–1818. [Google Scholar] [CrossRef] [PubMed]
- Hakeshzadeh, F.; Tabibi, H.; Ahmadinejad, M.; Malakoutian, T.; Hedayati, M. Effects of l-carnitine supplement on plasma coagulation and anticoagulation factors in hemodialysis patients. Renal Failure 2010, 32, 1109–1114. [Google Scholar] [CrossRef] [PubMed]
- Tabibi, H.; Hakeshzadeh, F.; Hedayati, M.; Malakoutian, T. Effects of l-carnitine supplement on serum amyloid A and vascular inflammation markers in hemodialysis patients: A randomized controlled trial. J. Ren. Nutr. 2011, 21, 485–491. [Google Scholar] [CrossRef] [PubMed]
- Suchitra, M.M.; Ashalatha, V.L.; Sailaja, E.; Rao, A.M.; Reddy, V.S.; Bitla, A.R.; Sivakumar, V.; Rao, P.V. The effect of l-carnitine supplementation on lipid parameters, inflammatory and nutritional markers in maintenance hemodialysis patients. Saudi J. Kidney Dis. Transpl. 2011, 22, 1155–1159. [Google Scholar] [PubMed]
- Naini, A.E.; Sadeghi, M.; Mortazavi, M.; Moghadasi, M.; Harandi, A.A. Oral carnitine supplementation for dyslipidemia in chronic hemodialysis patients. Saudi J. Kidney Dis. Transpl. 2012, 23, 484–488. [Google Scholar] [PubMed]
- Sgambat, K.; Frank, L.; Ellini, A.; Sable, C.; Moudgil, A. Carnitine supplementation improves cardiac strain rate in children on chronic hemodialysis. Pediatr. Nephrol. 2012, 27, 1381–1387. [Google Scholar] [CrossRef] [PubMed]
- Mercadal, L.; Coudert, M.; Vassault, A.; Pieroni, L.; Debure, A.; Ouziala, M.; Depreneuf, H.; Fumeron, C.; Servais, A.; Bassilios, N.; et al. l-Carnitine treatment in incident hemodialysis patients: The multicenter, randomized, double-blinded, placebo-controlled CARNIDIAL trial. Clin. J. Am. Soc. Nephrol. 2012, 7, 1836–1842. [Google Scholar] [CrossRef] [PubMed]
- Mingrone, G.; Greco, A.V.; Capristo, E.; Benedetti, G.; Giancaterini, A.; de Gaetano, A.; Gasbarrini, G. l-Carnitine improves glucose disposal in type 2 diabetic patients. J. Am. Coll. Nutr. 1999, 18, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Giancaterini, A.; de Gaetano, A.; Mingrone, G.; Gniuli, D.; Liverani, E.; Capristo, E.; Greco, A.V. Acetyl-l-carnitine infusion increases glucose disposal in type 2 diabetic patients. Metabolism 2000, 49, 704–708. [Google Scholar] [CrossRef] [PubMed]
- De Grandis, D.; Minardi, C. Acetyl-l-carnitine (levacecarnine) in the treatment of diabetic neuropathy. A long-term, randomised, double-blind, placebo-controlled study. Drugs R&D 2002, 3, 223–231. [Google Scholar] [CrossRef]
- Derosa, G.; Cicero, A.F.; Gaddi, A.; Mugellini, A.; Ciccarelli, L.; Fogari, R. The effect of l-carnitine on plasma lipoprotein(a) levels in hypercholesterolemic patients with type 2 diabetes mellitus. Clin. Ther. 2003, 25, 1429–1439. [Google Scholar] [CrossRef] [PubMed]
- Ragozzino, G.; Mattera, E.; Madrid, E.; Salomone, P.; Fasano, C.; Gioia, F.; Acerra, G.; del Guercio, R.; Federico, P. Effects of propionyl-carnitine in patients with type 2 diabetes and peripheral vascular disease: Results of a pilot trial. Drugs R&D 2004, 5, 185–190. [Google Scholar] [CrossRef]
- Sima, A.A.; Calvani, M.; Mehra, M.; Amato, A. Acetyl-l-Carnitine Study Group. Acetyl-l-carnitine improves pain, nerve regeneration, and vibratory perception in patients with chronic diabetic neuropathy: An analysis of two randomized placebo-controlled trials. Diabetes Care 2005, 28, 89–94. [Google Scholar] [CrossRef] [PubMed]
- Rahbar, A.R.; Shakerhosseini, R.; Saadat, N.; Taleban, F.; Pordal, A.; Gollestan, B. Effect of l-carnitine on plasma glycemic and lipidemic profile in patients with type II diabetes mellitus. Eur. J. Clin. Nutr. 2005, 59, 592–596. [Google Scholar] [CrossRef] [PubMed]
- Solfrizzi, V.; Capurso, C.; Colacicco, A.M.; D’Introno, A.; Fontana, C.; Capurso, S.A.; Torres, F.; Gadaleta, A.M.; Koverech, A.; Capurso, A.; et al. Efficacy and tolerability of combined treatment with l-carnitine and simvastatin in lowering lipoprotein(a) serum levels in patients with type 2 diabetes mellitus. Atherosclerosis 2006, 188, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Signorelli, S.S.; Neri, S.; di Pino, L.; Marchese, G.; Ferrante, M.; Oliveri Conti, G.; Fallico, R.; Celotta, G.; Pennisi, G.; Anzaldi, M. Effect of PLC on functional parameters and oxidative profile in type 2 diabetes-associated PAD. Diabetes Res. Clin. Pract. 2006, 72, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Malaguarnera, M.; Vacante, M.; Avitabile, T.; Malaguarnera, M.; Cammalleri, L.; Motta, M. l-Carnitine supplementation reduces oxidized LDL cholesterol in patients with diabetes. Am. J. Clin. Nutr. 2009, 89, 71–76. [Google Scholar] [CrossRef] [PubMed]
- Ruggenenti, P.; Cattaneo, D.; Loriga, G.; Ledda, F.; Motterlini, N.; Gherardi, G.; Orisio, S.; Remuzzi, G. Ameliorating hypertension and insulin resistance in subjects at increased cardiovascular risk: Effects of acetyl-l-carnitine therapy. Hypertension 2009, 54, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Molfino, A.; Cascino, A.; Conte, C.; Ramaccini, C.; Rossi Fanelli, F.; Laviano, A. Caloric restriction and l-carnitine administration improves insulin sensitivity in patients with impaired glucose metabolism. J. Parenter. Enteral. Nutr. 2010, 34, 295–299. [Google Scholar] [CrossRef]
- Uzun, N.; Sarikaya, S.; Uluduz, D.; Aydin, A. Peripheric and automatic neuropathy in children with type 1 diabetes mellitus: The effect of l-carnitine treatment on the peripheral and autonomic nervous system. Electromyogr. Clin. Neurophysiol. 2005, 45, 343–351. [Google Scholar] [PubMed]
- Loffredo, L.; Pignatelli, P.; Cangemi, R.; Andreozzi, P.; Panico, M.A.; Meloni, V.; Violi, F. Imbalance between nitric oxide generation and oxidative stress in patients with peripheral arterial disease: Effect of an antioxidant treatment. J. Vasc. Surg. 2006, 44, 525–530. [Google Scholar] [CrossRef] [PubMed]
- De Marchi, S.; Zecchetto, S.; Rigoni, A.; Prior, M.; Fondrieschi, L.; Scuro, A.; Rulfo, F.; Arosio, E. Propionyl-l-carnitine improves endothelial function, microcirculation and pain management in critical limb ischemia. Cardiovasc. Drugs Ther. 2012, 26, 401–408. [Google Scholar] [CrossRef] [PubMed]
- Goldenberg, N.A.; Krantz, M.J.; Hiatt, W.R. l-Carnitine plus cilostazol versus cilostazol alone for the treatment of claudication in patients with peripheral artery disease: A multicenter, randomized, double-blind, placebo-controlled trial. Vasc. Med. 2012, 17, 145–154. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.Q.; Jing, Z.C.; Jiang, X.; Zhao, Q.H.; He, J.; Dai, L.Z.; Wu, W.H.; Li, Y.; Yao, J. Clinical efficacy of intravenous l-carnitine in patients with right-sided heart failure induced by pulmonary arterial hypertension. Zhonghua Xin Xue Guan Bing Za Zhi 2010, 38, 152–155. [Google Scholar] [PubMed]
- Serati, A.R.; Motamedi, M.R.; Emami, S.; Varedi, P.; Movahed, M.R. l-Carnitine treatment in patients with mild diastolic heart failure is associated with improvement in diastolic function and symptoms. Cardiology 2010, 116, 178–182. [Google Scholar] [CrossRef] [PubMed]
- Lango, R.; Smoleński, R.T.; Rogowski, J.; Siebert, J.; Wujtewicz, M.; Słomińska, E.M.; Lysiak-Szydłowska, W.; Yacoub, M.H. Propionyl-l-carnitine improves hemodynamics and metabolic markers of cardiac perfusion during coronary surgery in diabetic patients. Cardiovasc. Drugs Ther. 2005, 19, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Xiang, D.; Sun, Z.; Xia, J.; Dong, N.; Du, X.; Chen, X. Effect of l-carnitine on cardiomyocyte apoptosis and cardiac function in patients undergoing heart valve replacement operation. J. Huazhong Univ. Sci. Technol. Med. Sci. 2005, 25, 501–504. [Google Scholar] [CrossRef] [PubMed]
- Łapiński, T.W.; Grzeszczuk, A. The impact of carnitine on serum ammonia concentration and lipid metabolism in patients with alcoholic liver cirrhosis. Pol. Merkur. Lekarski 2003, 15, 38–41. [Google Scholar] [PubMed]
- Lim, C.Y.; Jun, D.W.; Jang, S.S.; Cho, W.K.; Chae, J.D.; Jun, J.H. Effects of carnitine on peripheral blood mitochondrial DNA copy number and liver function in non-alcoholic fatty liver disease. Korean J. Gastroenterol. 2010, 55, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Malaguarnera, M.; Pistone, G.; Astuto, M.; dell’Arte, S.; Finocchiaro, G.; lo Giudice, E.; Pennisi, G. l-Carnitine in the treatment of mild or moderate hepatic encephalopathy. Dig. Dis. 2003, 21, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Malaguarnera, M.; Vacante, M.; Giordano, M.; Motta, M.; Bertino, G.; Pennisi, M.; Neri, S.; Malaguarnera, M.; Li Volti, G.; Galvano, F. l-Carnitine supplementation improves hematological pattern in patients affected by HCV treated with Peg interferon-α 2b plus ribavirin. World J. Gastroenterol. 2011, 17, 4414–4420. [Google Scholar] [CrossRef] [PubMed]
- Neri, S.; Pistone, G.; Saraceno, B.; Pennisi, G.; Luca, S.; Malaguarnera, M. l-Carnitine decreases severity and type of fatigue induced by interferon-alpha in the treatment of patients with hepatitis C. Neuropsychobiology 2003, 47, 94–97. [Google Scholar] [CrossRef] [PubMed]
- Malaguarnera, M.; Vacante, M.; Giordano, M.; Pennisi, G.; Bella, R.; Rampello, L.; Malaguarnera, M.; Li Volti, G.; Galvano, F. Oral acetyl-l-carnitine therapy reduces fatigue in overt hepatic encephalopathy: A randomized, double-blind, placebo-controlled study. Am. J. Clin. Nutr. 2011, 93, 799–808. [Google Scholar] [CrossRef] [PubMed]
- Tomassini, V.; Pozzilli, C.; Onesti, E.; Pasqualetti, P.; Marinelli, F.; Pisani, A.; Fieschi, C. Comparison of the effects of acetyl l-carnitine and amantadine for the treatment of fatigue in multiple sclerosis: Results of a pilot, randomised, double-blind, crossover trial. J. Neurol. Sci. 2004, 218, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Gavrilova, S.I.; Kalyn, IaB.; Kolykhalov, I.V.; Roshchina, I.F.; Selezneva, N.D. Acetyl-l-carnitine (carnicetine) in the treatment of early stages of Alzheimer's disease and vascular dementia. Zh. Nevrol. Psikhiatr. Im. S. S. Korsakova 2011, 111, 16–22. [Google Scholar] [PubMed]
- Tarighat Esfanjani, A.; Mahdavi, R.; Ebrahimi Mameghani, M.; Talebi, M.; Nikniaz, Z.; Safaiyan, A. The effects of magnesium, l-carnitine, and concurrent magnesium-l-carnitine supplementation in migraine prophylaxis. Biol. Trace Elem. Res. 2012, 150, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Pistone, G.; Marino, A.; Leotta, C.; dell’Arte, S.; Finocchiaro, G.; Malaguarnera, M. Levocarnitine administration in elderly subjects with rapid muscle fatigue: Effect on body composition, lipid profile and fatigue. Drugs Aging 2003, 20, 761–767. [Google Scholar] [CrossRef] [PubMed]
- Miyagawa, T.; Kawamura, H.; Obuchi, M.; Ikesaki, A.; Ozaki, A.; Tokunaga, K.; Inoue, Y.; Honda, M. Effects of oral l-carnitine administration in narcolepsy patients: A randomized, double-blind, cross-over and placebo-controlled trial. PLoS One 2013, 8, e53707. [Google Scholar] [CrossRef] [PubMed]
- Rossini, M.; di Munno, O.; Valentini, G.; Bianchi, G.; Biasi, G.; Cacace, E.; Malesci, D.; la Montagna, G.; Viapiana, O.; Adami, S. Double-blind, multicenter trial comparing acetyl l-carnitine with placebo in the treatment of fibromyalgia patients. Clin. Exp. Rheumatol. 2007, 25, 182–188. [Google Scholar] [PubMed]
- Vermeulen, R.C.; Scholte, H.R. Exploratory open label, randomized study of acetyl- and propionyl-carnitine in chronic fatigue syndrome. Psychosom. Med. 2004, 66, 276–282. [Google Scholar] [CrossRef] [PubMed]
- Beghi, E.; Pupillo, E.; Bonito, V.; Buzzi, P.; Caponnetto, C.; Chiò, A.; Corbo, M.; Giannini, F.; Inghilleri, M.; Bella, V.L.; et al. Randomized double-blind placebo-controlled trial of acetyl-l-carnitine for ALS. Amyotroph. Lateral Scler. Frontotemporal Degener. 2013, 14, 397–405. [Google Scholar] [CrossRef] [PubMed]
- Cruciani, R.A.; Dvorkin, E.; Homel, P.; Malamud, S.; Culliney, B.; Lapin, J.; Portenoy, R.K.; Esteban-Cruciani, N. Safety, tolerability and symptom outcomes associated with l-carnitine supplementation in patients with cancer, fatigue, and carnitine deficiency: A phase I/II study. J. Pain Symptom Manag. 2006, 32, 551–559. [Google Scholar] [CrossRef]
- Cruciani, R.A.; Dvorkin, E.; Homel, P.; Culliney, B.; Malamud, S.; Lapin, J.; Portenoy, R.K.; Esteban-Cruciani, N. l-Carnitine supplementation in patients with advanced cancer and carnitine deficiency: A double-blind, placebo-controlled study. J. Pain Symptom Manag. 2009, 37, 622–631. [Google Scholar] [CrossRef]
- Cruciani, R.A.; Zhang, J.J.; Manola, J.; Cella, D.; Ansari, B.; Fisch, M.J. l-Carnitine supplementation for the management of fatigue in patients with cancer: An eastern cooperative oncology group phase III, randomized, double-blind, placebo-controlled trial. J. Clin. Oncol. 2012, 30, 3864–3869. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, G. Randomised phase III clinical trial of 5 different arms of treatment on 332 patients with cancer cachexia. Eur. Rev. Med. Pharmacol. Sci. 2010, 14, 292–301. [Google Scholar] [PubMed]
- Madeddu, C.; Dessì, M.; Panzone, F.; Serpe, R.; Antoni, G.; Cau, M.C.; Montaldo, L.; Mela, Q.; Mura, M.; Astara, G.; et al. Randomized phase III clinical trial of a combined treatment with carnitine + celecoxib ± megestrol acetate for patients with cancer-related anorexia/cachexia syndrome. Clin. Nutr. 2012, 31, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Kraft, M.; Kraft, K.; Gärtner, S.; Mayerle, J.; Simon, P.; Weber, E.; Schütte, K.; Stieler, J.; Koula-Jenik, H.; Holzhauer, P.; et al. l-Carnitine-supplementation in advanced pancreatic cancer (CARPAN) a randomized multicentre trial. Nutr. J. 2012, 11, 52. [Google Scholar] [CrossRef] [PubMed]
- Hershman, D.L.; Unger, J.M.; Crew, K.D.; Minasian, L.M.; Awad, D.; Moinpour, C.M.; Hansen, L.; Lew, D.L.; Greenlee, H.; Fehrenbacher, L.; et al. Randomized double-blind placebo-controlled trial of acetyl-l-carnitine for the prevention of taxane-induced neuropathy in women undergoing adjuvant breast cancer therapy. J. Clin. Oncol. 2013, 31, 2627–2633. [Google Scholar] [CrossRef] [PubMed]
- Schöls, L.; Zange, J.; Abele, M.; Schillings, M.; Skipka, G.; Kuntz-Hehner, S.; van Beekvelt, M.C.; Colier, W.N.; Müller, K.; Klockgether, T.; et al. l-Carnitine and creatine in Friedreich’s ataxia. A randomized, placebo-controlled crossover trial. J. Neural Transm. 2005, 112, 789–796. [Google Scholar] [CrossRef] [PubMed]
- El-Beshlawy, A.; Ragab, L.; Fattah, A.A.; Ibrahim, I.Y.; Hamdy, M.; Makhlouf, A.; Aoun, E.; Hoffbrand, V.; Taher, A. Improvement of cardiac function in thalassemia major treated with l-carnitine. Acta Haematol. 2004, 111, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Karimi, M.; Mohammadi, F.; Behmanesh, F.; Samani, S.M.; Borzouee, M.; Amoozgar, H.; Haghpanah, S. Effect of combination therapy of hydroxyurea with l-carnitine and magnesium chloride on hematologic parameters and cardiac function of patients with beta-thalassemia intermedia. Eur. J. Haematol. 2010, 84, 52–58. [Google Scholar] [CrossRef] [PubMed]
- Ellaway, C.J.; Peat, J.; Williams, K.; Leonard, H.; Christodoulou, J. Medium-term open label trial of l-carnitine in Rett syndrome. Brain Dev. 2001, 23, S85–S89. [Google Scholar] [CrossRef]
- Torrioli, M.G.; Vernacotola, S.; Peruzzi, L.; Tabolacci, E.; Mila, M.; Militerni, R.; Musumeci, S.; Ramos, F.J.; Frontera, M.; Sorge, G.; et al. A double-blind, parallel, multicenter comparison of l-acetylcarnitine with placebo on the attention deficit hyperactivity disorder in fragile X syndrome boys. Am. J. Med. Genet. A 2008, 146, 803–812. [Google Scholar] [CrossRef]
- Geier, D.A.; Kern, J.K.; Davis, G.; King, P.G.; Adams, J.B.; Young, J.L.; Geier, M.R. A prospective double-blind, randomized clinical trial of levocarnitine to treat autism spectrum disorders. Med. Sci. Monit. 2011, 17, PI15–PI23. [Google Scholar] [CrossRef] [PubMed]
- Osio, M.; Muscia, F.; Zampini, L.; Nascimbene, C.; Mailland, E.; Cargnel, A.; Mariani, C. Acetyl-l-carnitine in the treatment of painful antiretroviral toxic neuropathy in human immunodeficiency virus patients: An open label study. J. Peripher. Nerv. Syst. 2006, 11, 72–76. [Google Scholar] [CrossRef] [PubMed]
- Youle, M.; Osio, M.; ALCAR Study Group. A double-blind, parallel-group, placebo-controlled, multicentre study of acetyl l-carnitine in the symptomatic treatment of antiretroviral toxic neuropathy in patients with HIV-1 infection. HIV Med. 2007, 8, 241–250. [Google Scholar] [CrossRef] [PubMed]
- Benedini, S.; Perseghin, G.; Terruzzi, I.; Scifo, P.; Invernizzi, P.L.; del Maschio, A.; Lazzarin, A.; Luzi, L. Effect of l-acetylcarnitine on body composition in HIV-related lipodystrophy. Horm. Metab. Res. 2009, 41, 840–845. [Google Scholar] [CrossRef] [PubMed]
- Pignatelli, P.; Tellan, G.; Marandola, M.; Carnevale, R.; Loffredo, L.; Schillizzi, M.; Proietti, M.; Violi, F.; Chirletti, P.; Delogu, G. Effect of l-carnitine on oxidative stress and platelet activation after major surgery. Acta Anaesthesiol. Scand. 2011, 55, 1022–1028. [Google Scholar] [PubMed]
- Mikhailova, T.L.; Sishkova, E.; Poniewierka, E.; Zhidkov, K.P.; Bakulin, I.G.; Kupcinskas, L.; Lesniakowski, K.; Grinevich, V.B.; Malecka-Panas, E.; Ardizzone, S.; et al. Randomised clinical trial: The efficacy and safety of propionyl-l-carnitine therapy in patients with ulcerative colitis receiving stable oral treatment. Aliment. Pharmacol. Ther. 2011, 34, 1088–1097. [Google Scholar] [CrossRef] [PubMed]
- Mattiazzi, M.; Vijayvergiya, C.; Gajewski, C.D.; deVivo, D.C.; Lenaz, G.; Wiedmann, M.; Manfredi, G. The mtDNA T8993G (NARP) mutation results in an impairment of oxidative phosphorylation that can be improved by antioxidants. Hum. Mol. Genet. 2004, 13, 869–879. [Google Scholar] [CrossRef] [PubMed]
- Chinnery, P.F. Mitochondrial Disorders Overview. Synonyms: Mitochondrial Encephalomyopathies, Mitochondrial Myopathies, Oxidative Phosphorylation Disorders, Respiratory Chain Disorders. Available online: http://www.ncbi.nlm.nih.gov/books/NBK1224 (accessed on 3 November 2014).
- Di Mauro, S.; Mancuso, M. Mitochondrial diseases: Therapeutic approaches. Biosci. Rep. 2007, 27, 125–137. [Google Scholar] [CrossRef] [PubMed]
- Smith, R.A.; Murphey, M.P. Mitochondria-targeted antioxidants as therapies. Discov. Med. 2011, 11, 106–114. [Google Scholar] [PubMed]
- Lee, S.H.; Kim, M.J.; Kim, B.J.; Kim, S.R.; Chun, S.; Ryu, J.S.; Kim, G.S.; Lee, M.C.; Koh, J.M.; Chung, S.J. Homocysteine-lowering therapy or antioxidant therapy for bone loss in Parkinson’s disease. Mov. Disord. 2010, 25, 332–340. [Google Scholar] [CrossRef] [PubMed]
- Pagano, G.; Aiello Talamanca, A.; Castello, G.; d’Ischia, M.; Pallardó, F.V.; Petrović, S.; Porto, B.; Tiano, L.; Zatterale, A. From clinical description to in vitro and animal studies, and backwards to patients: Oxidative stress and mitochondrial dysfunction in Fanconi anaemia. Free Radic. Biol. Med. 2013, 58, 118–125. [Google Scholar] [CrossRef] [PubMed]
- Seco-Cervera, M.; Spis, M.; García-Giménez, J.L. Oxidative stress and antioxidant response in fibroblasts from Werner and Atypical Werner Syndromes. Aging 2014, 6, 231–245. [Google Scholar] [PubMed]
- Bhagavan, H.N.; Chopra, R.K. Plasma coenzyme Q10 response to oral ingestion of coenzyme Q10 formulations. Mitochondrion 2007, 7, S78–S88. [Google Scholar] [CrossRef] [PubMed]
- Roginsky, V.A.; Tashlitsky, V.N.; Skulachev, V.P. Chain-breaking antioxidant activity of reduced forms of mitochondria-targeted quinones, a novel type of geroprotectors. Aging 2009, 1, 481–489. [Google Scholar] [PubMed]
- Teichert, J.; Hermann, R.; Ruus, P.; Preiss, R. Plasma kinetics, metabolism, and urinary excretion of alpha-lipoic acid following oral administration in healthy volunteers. J. Clin. Pharmacol. 2003, 43, 1257–1267. [Google Scholar] [CrossRef] [PubMed]
- Pettegrew, J.W.; Levine, J.; McClure, R.J. Acetyl-l-carnitine physical-chemical, metabolic and therapeutic properties: Relevance for its mode of action in Alzheimer’disease and geriatric depression. Mol. Psychiatry 2000, 5, 616–632. [Google Scholar] [CrossRef] [PubMed]
- Madiraju, P.; Pande, S.V.; Prentki, M.; Murthy Madiraju, S.R. Mitochondrial acetylcarnitine provides acetyl groups for nuclear histone acetylation. Epigenetics 2009, 4, 4–6. [Google Scholar] [CrossRef]
- Rosca, M.G.; Lemieux, H.; Hoppel, C.L. Mitochondria in the ederly: Is acetylcarnitine a rejuvinator? Adv. Drug Deliv. Rev. 2009, 61, 1332–1342. [Google Scholar]
- Breithaupt-Grögler, K.; Niebch, G.; Schneider, E.; Erb, K.; Hermann, R.; Blume, H.H.; Schug, B.S.; Belz, G.G. Dose-proportionality of oral thioctic acid—Coincidence of assessments via pooled plasma and individual data. Eur. J. Pharm. Sci. 1999, 8, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Rebouche, C.J. Kinetics, pharmacokinetics, and regulation of l-carnitine and acetyl-l-carnitine metabolism. Ann. N. Y. Acad. Sci. 2004, 1033, 30–41. [Google Scholar] [CrossRef] [PubMed]
- Camp, K.M.; Lloyd-Puryear, M.A.; Yao, L.; Groft, S.C.; Parisi, M.A.; Mulberg, A.; Gopal-Srivastava, R.; Cederbaum, S.; Enns, G.M.; Ershow, A.G.; et al. Expanding research to provide an evidence base for nutritional interventions for the management of inborn errors of metabolism. Mol. Genet. Metab. 2013, 109, 319–328. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pagano, G.; Aiello Talamanca, A.; Castello, G.; Cordero, M.D.; D'Ischia, M.; Gadaleta, M.N.; Pallardó, F.V.; Petrović, S.; Tiano, L.; Zatterale, A. Current Experience in Testing Mitochondrial Nutrients in Disorders Featuring Oxidative Stress and Mitochondrial Dysfunction: Rational Design of Chemoprevention Trials. Int. J. Mol. Sci. 2014, 15, 20169-20208. https://doi.org/10.3390/ijms151120169
Pagano G, Aiello Talamanca A, Castello G, Cordero MD, D'Ischia M, Gadaleta MN, Pallardó FV, Petrović S, Tiano L, Zatterale A. Current Experience in Testing Mitochondrial Nutrients in Disorders Featuring Oxidative Stress and Mitochondrial Dysfunction: Rational Design of Chemoprevention Trials. International Journal of Molecular Sciences. 2014; 15(11):20169-20208. https://doi.org/10.3390/ijms151120169
Chicago/Turabian StylePagano, Giovanni, Annarita Aiello Talamanca, Giuseppe Castello, Mario D. Cordero, Marco D'Ischia, Maria Nicola Gadaleta, Federico V. Pallardó, Sandra Petrović, Luca Tiano, and Adriana Zatterale. 2014. "Current Experience in Testing Mitochondrial Nutrients in Disorders Featuring Oxidative Stress and Mitochondrial Dysfunction: Rational Design of Chemoprevention Trials" International Journal of Molecular Sciences 15, no. 11: 20169-20208. https://doi.org/10.3390/ijms151120169
APA StylePagano, G., Aiello Talamanca, A., Castello, G., Cordero, M. D., D'Ischia, M., Gadaleta, M. N., Pallardó, F. V., Petrović, S., Tiano, L., & Zatterale, A. (2014). Current Experience in Testing Mitochondrial Nutrients in Disorders Featuring Oxidative Stress and Mitochondrial Dysfunction: Rational Design of Chemoprevention Trials. International Journal of Molecular Sciences, 15(11), 20169-20208. https://doi.org/10.3390/ijms151120169








