Does a Skills Intervention for Parents Have a Positive Impact on Adolescents’ Anorexia Nervosa Outcome? Answers from a Quasi-Randomised Feasibility Trial of SUCCEAT
Abstract
1. Introduction
2. Materials and Methods
2.1. Trial Design
2.2. Participants
2.2.1. Eligibility Criteria for Participants
2.2.2. How Participants Were Identified and Consented
2.3. Interventions
2.3.1. Workshop (WS) Group
2.3.2. Online (ONL) Group
2.4. Outcome Measurements
- The BMI percentiles were obtained from clinical measures of height and weight; additionally, sex- and age-specific percentiles were analysed [39].
- The Eating Disorder Examination (EDE; [40,41]) is a semi-structured interview conducted by clinicians to diagnose EDs and to obtain a picture as accurate as possible of the participant’s eating behaviour and attitudes. It is rated through a global score and four subscales: “restraint” (e.g., avoidance of eating; dietary rules), “eating concerns” (e.g., fear of losing control of eating; guilt about eating), “weight concerns” (e.g., preoccupation with weight; desire to lose weight), and “shape concerns” (e.g., importance of shape; discomfort seeing one’s own body). Internal consistency is good (Cronbach’ s alpha for the subscales: 0.73 to 0.86; for the total score: 0.93). In our sample, reliability was high for both, for children below the age of 14 (Cronbach’s alpha: 0.90) and for adolescents aged 14 and above (Cronbach’s alpha: 0.92). The higher the score the higher is the ED psychopathology.
- The Eating Disorder Inventory-2 (EDI-2; [42]) is a self-report measure to assess ED specific and ED associated psychopathology, including a total scale and 11 subscales (“drive for thinness”, “bulimia”, “body dissatisfaction”, “ineffectiveness”, “perfectionism”, “interpersonal distrust”, “interoceptive awareness”, “maturity fears”, “asceticism”, “impulse regulation”, and “social insecurity”). The EDI-2 was validated for children and adolescents aged 10 and above. Excellent data concerning reliability are available (total score: Cronbach’ s alpha: 0.97). For the purpose of this study, only the total score was used. The higher the score the more subjective ED attitudes and behaviours are reported.
- The Anorexia Nervosa Stages of Change Questionnaire (ANSOCQ; [43,44]) is a self-report questionnaire assessing motivation to change related to their ED symptomatology. The children and adolescents select a statement for each item, which represents their current stage of change (precontemplation, contemplation, preparation, action, maintenance). Internal consistency is excellent (Cronbach’s alpha: 0.90). One study [45] shows good reliability for adolescents older than 12 years. Cronbach’s alpha in our sample was 0.91 for children under the age of 14 and 0.94 for adolescents aged 14 and above. The calculated mean score ranges from 1 to 5 with higher scores indicating a higher motivation to change, or an advanced stage of change, respectively.
- The Youth Self-Report (YSR; [46]) is a self-report measure assessing various behavioural and emotional problems (e.g., “anxious/depressed”, “social problems”, “aggressive behaviour”). The YSR was validated for children and adolescents from age 11. Reliability is high (Cronbach’s alpha ≥ 0.91). We used the total score in this study only, with a higher score indicating a higher level of general psychopathology.
- The Health-Related Quality of Life Questionnaire for Children and Adolescents (KINDL; [47,48]) is a self-report measure assessing the quality of life. The total score comprises the subscales: “physical well-being”, “psychological well-being”, “self-worth”, “family”, “friends”, and “school”. The KINDL was validated for children and adolescents aged 7 years and above. Internal consistency is rather high (Cronbach’s alpha: 0.80). The total score ranges from 0 to 100; a higher score indicating a higher quality of life.
2.5. Randomisation
2.6. Blinding
2.7. Statistical Analysis
3. Results
3.1. Participant Flow
3.2. Baseline Data
3.3. Main Outcomes
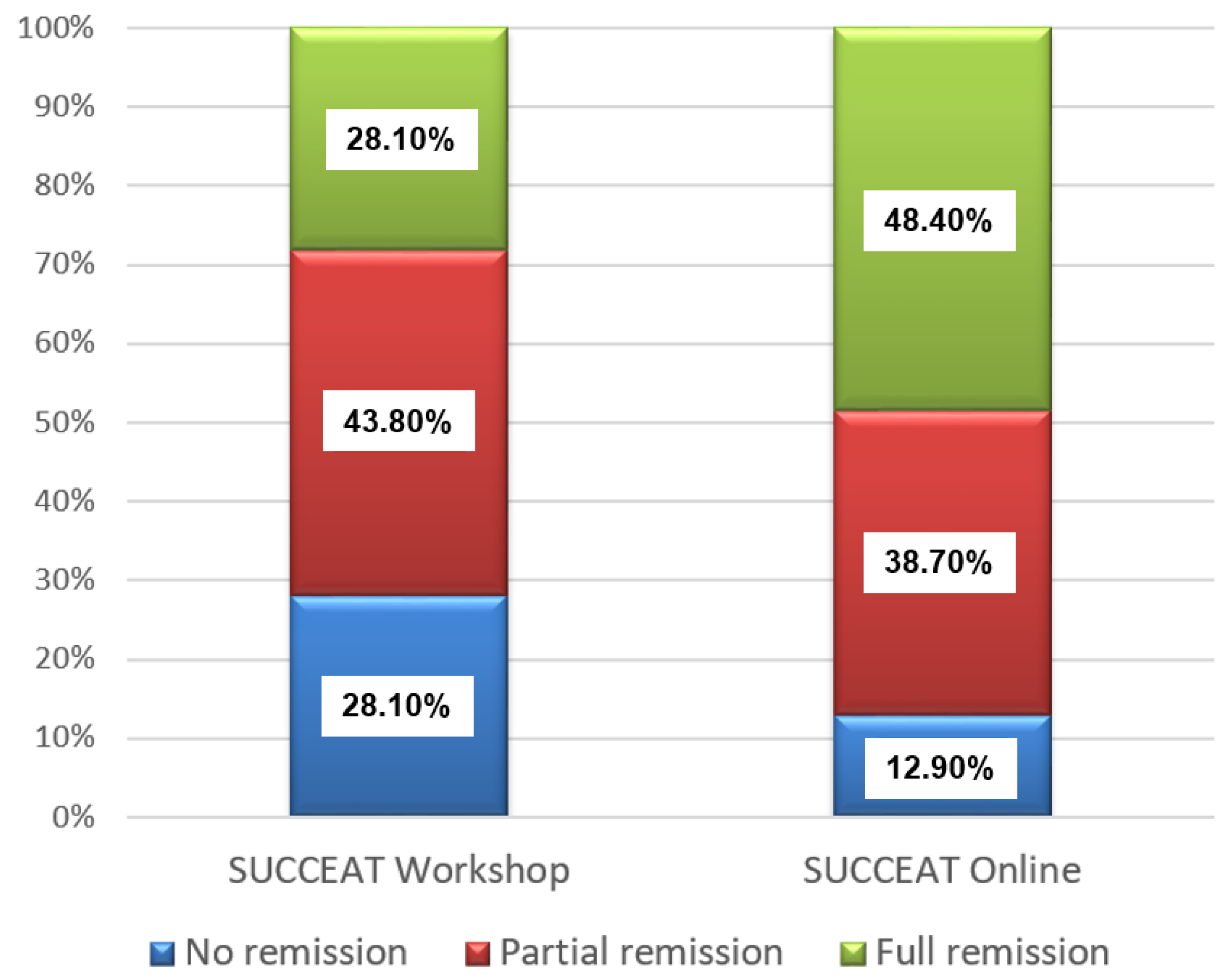
3.4. Remission Rates
3.5. Harms
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Registration
Protocol
References
- Zipfel, S.; Giel, K.E.; Bulik, C.M.; Hay, P.; Schmidt, U. Anorexia Nervosa: Aetiology, Assessment and Treatment. Lancet Psychiatry 2015, 2, 1099–1111. [Google Scholar] [CrossRef]
- Wagner, G.; Zeiler, M.; Waldherr, K.; Philipp, J.; Truttmann, S.; Dür, W.; Treasure, J.L.; Karwautz, A.F.K. Mental Health Problems in Austrian Adolescents: A Nationwide, Two-Stage Epidemiological Study Applying DSM-5 Criteria. Eur Child Adolesc. Psychiatry 2017, 26, 1483–1499. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5, 5th ed.; American Psychiatric Association, Ed.; American Psychiatric Association: Washington, DC, USA, 2013; ISBN 978-0-89042-554-1. [Google Scholar]
- Treasure, J.; Duarte, T.A.; Schmidt, U. Eating Disorders. Lancet 2020, 395, 899–911. [Google Scholar] [CrossRef]
- Karwautz, A.F.K.; Wagner, G.; Waldherr, K.; Nader, I.W.; Fernandez-Aranda, F.; Estivill, X.; Holliday, J.; Collier, D.A.; Treasure, J.L. Gene-Environment Interaction in Anorexia Nervosa: Relevance of Non-Shared Environment and the Serotonin Transporter Gene. Mol. Psychiatry 2011, 16, 590–592. [Google Scholar] [CrossRef] [PubMed]
- Zabala, M.J.; Macdonald, P.; Treasure, J. Appraisal of Caregiving Burden, Expressed Emotion and Psychological Distress in Families of People with Eating Disorders: A Systematic Review. Eur. Eat. Disord. Rev. 2009, 17, 338–349. [Google Scholar] [CrossRef] [PubMed]
- Rhind, C.; Salerno, L.; Hibbs, R.; Micali, N.; Schmidt, U.; Gowers, S.; Macdonald, P.; Goddard, E.; Todd, G.; Tchanturia, K.; et al. The Objective and Subjective Caregiving Burden and Caregiving Behaviours of Parents of Adolescents with Anorexia Nervosa. Eur. Eat. Disord. Rev. 2016, 24, 310–319. [Google Scholar] [CrossRef]
- Kyriacou, O.; Treasure, J.; Schmidt, U. Understanding How Parents Cope with Living with Someone with Anorexia Nervosa: Modelling the Factors That Are Associated with Carer Distress. Int. J. Eat. Disord. 2008, 41, 233–242. [Google Scholar] [CrossRef]
- Anastasiadou, D.; Medina-Pradas, C.; Sepulveda, A.R.; Treasure, J. A Systematic Review of Family Caregiving in Eating Disorders. Eat. Behav. 2014, 15, 464–477. [Google Scholar] [CrossRef]
- Schmidt, U.; Treasure, J. Anorexia Nervosa: Valued and Visible. A Cognitive-Interpersonal Maintenance Model and Its Implications for Research and Practice. Br. J. Clin. Psychol. 2006, 45, 343–366. [Google Scholar] [CrossRef]
- Treasure, J.; Schmidt, U. The Cognitive-Interpersonal Maintenance Model of Anorexia Nervosa Revisited: A Summary of the Evidence for Cognitive, Socio-Emotional and Interpersonal Predisposing and Perpetuating Factors. J. Eat. Disord. 2013, 1, 13. [Google Scholar] [CrossRef]
- Treasure, J.; Willmott, D.; Ambwani, S.; Cardi, V.; Bryan, D.C.; Rowlands, K.; Schmidt, U. Cognitive Interpersonal Model for Anorexia Nervosa Revisited: The Perpetuating Factors That Contribute to the Development of the Severe and Enduring Illness. J. Clin. Med. 2020, 9, 630. [Google Scholar] [CrossRef]
- Hibbs, R.; Rhind, C.; Leppanen, J.; Treasure, J. Interventions for Caregivers of Someone with an Eating Disorder: A Meta-Analysis. Int. J. Eat. Disord. 2015, 48, 349–361. [Google Scholar] [CrossRef]
- Truttmann, S.; Philipp, J.; Zeiler, M.; Franta, C.; Wittek, T.; Merl, E.; Schöfbeck, G.; Koubek, D.; Laczkovics, C.; Imgart, H.; et al. Long-Term Efficacy of the Workshop Vs. Online SUCCEAT (Supporting Carers of Children and Adolescents with Eating Disorders) Intervention for Parents: A Quasi-Randomised Feasibility Trial. J. Clin. Med. 2020, 9, 1912. [Google Scholar] [CrossRef]
- Philipp, J.; Truttmann, S.; Zeiler, M.; Franta, C.; Wittek, T.; Schöfbeck, G.; Mitterer, M.; Mairhofer, D.; Zanko, A.; Imgart, H.; et al. Reduction of High Expressed Emotion and Treatment Outcomes in Anorexia Nervosa—Caregivers’ and Adolescents’ Perspective. J. Clin. Med. 2020, 9, 2021. [Google Scholar] [CrossRef]
- Zeiler, M.; Philipp, J.; Truttmann, S.; Wittek, T.; Franta, C.; Imgart, H.; Zanko, A.; Auer-Welsbach, E.; Kahlenberg, L.; Wagner, G.; et al. A German Version of the Caregiver Skills Scale for Caregivers of Patients with Anorexia Nervosa. Eur. Eat. Disord. Rev. 2021, 29, 257–268. [Google Scholar] [CrossRef]
- Spencer, L.; Potterton, R.; Allen, K.; Musiat, P.; Schmidt, U. Internet-Based Interventions for Carers of Individuals with Psychiatric Disorders, Neurological Disorders, or Brain Injuries: Systematic Review. J. Med. Internet Res. 2019, 21, e10876. [Google Scholar] [CrossRef]
- Dimitropoulos, G.; Landers, A.; Freeman, V.; Novick, J.; Schmidt, U.; Olmsted, M. A Feasibility Study Comparing a Web-Based Intervention to a Workshop Intervention for Caregivers of Adults with Eating Disorders. Eur. Eat. Disord. Rev. 2019, 27, 641–654. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Aranda, F.; Casas, M.; Claes, L.; Bryan, D.C.; Favaro, A.; Granero, R.; Gudiol, C.; Jiménez-Murcia, S.; Karwautz, A.; Grange, D.L.; et al. COVID-19 and Implications for Eating Disorders. Eur. Eat. Disord. Rev. 2020, 28, 239–245. [Google Scholar] [CrossRef]
- Magill, N.; Rhind, C.; Hibbs, R.; Goddard, E.; Macdonald, P.; Arcelus, J.; Morgan, J.; Beecham, J.; Schmidt, U.; Landau, S.; et al. Two-Year Follow-up of a Pragmatic Randomised Controlled Trial Examining the Effect of Adding a Carer’s Skill Training Intervention in Inpatients with Anorexia Nervosa. Eur. Eat. Disord. Rev. 2016, 24, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Whitney, J.; Murphy, T.; Landau, S.; Gavan, K.; Todd, G.; Whitaker, W.; Treasure, J. A Practical Comparison of Two Types of Family Intervention: An Exploratory RCT of Family Day Workshops and Individual Family Work as a Supplement to Inpatient Care for Adults with Anorexia Nervosa. Eur. Eat. Disord. Rev. 2012, 20, 142–150. [Google Scholar] [CrossRef] [PubMed]
- Sepulveda, A.R.; Anastasiadou, D.; Parks, M.; Gutiérrez, E. A Controlled Study of the Collaborative Care Skills Workshops versus Psycho-Educational Workshops among Spanish Caregivers of Relatives with an Eating Disorder. Eur. Eat. Disord. Rev. 2019, 27, 247–262. [Google Scholar] [CrossRef]
- Marcos, Y.Q.; Sebastián, M.J.Q.; Herrera, M.E.; Sanmartín, R.; Treasure, J. Testing Carer Skill Training Programs in Spanish Carers of Patients with Eating Disorders. Psicothema 2018, 30, 295–303. [Google Scholar] [CrossRef]
- Hibbs, R.; Magill, N.; Goddard, E.; Rhind, C.; Raenker, S.; Macdonald, P.; Todd, G.; Arcelus, J.; Morgan, J.; Beecham, J.; et al. Clinical Effectiveness of a Skills Training Intervention for Caregivers in Improving Patient and Caregiver Health Following In-Patient Treatment for Severe Anorexia Nervosa: Pragmatic Randomised Controlled Trial. BJPsych Open 2015, 1, 56–66. [Google Scholar] [CrossRef]
- Hodsoll, J.; Rhind, C.; Micali, N.; Hibbs, R.; Goddard, E.; Nazar, B.P.; Schmidt, U.; Gowers, S.; Macdonald, P.; Todd, G.; et al. A Pilot, Multicentre Pragmatic Randomised Trial to Explore the Impact of Carer Skills Training on Carer and Patient Behaviours: Testing the Cognitive Interpersonal Model in Adolescent Anorexia Nervosa. Eur. Eat. Disord. Rev. 2017, 25, 551–561. [Google Scholar] [CrossRef] [PubMed]
- Franta, C.; Philipp, J.; Waldherr, K.; Truttmann, S.; Merl, E.; Schöfbeck, G.; Koubek, D.; Laczkovics, C.; Imgart, H.; Zanko, A.; et al. Supporting Carers of Children and Adolescents with Eating Disorders in Austria (SUCCEAT): Study Protocol for a Randomised Controlled Trial. Eur. Eat. Disord. Rev. 2018, 26, 447–461. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. International Statistical Classification of Diseases and Related Health Problems, 10th ed.; World Health Organization: Geneva, Switzerland, 2009; ISBN 978-92-4-154766-6. [Google Scholar]
- National Guideline Alliance (UK). Eating Disorders: Recognition and Treatment; National Institute for Health and Care Excellence: Clinical Guidelines. Natl. Inst. Health Care Excell. 2017. Available online: https://www.nice.org.uk/guidance/ng69/resources/eating-disorders-recognition-and-treatment-pdf-1837582159813 (accessed on 26 April 2021).
- Treasure, J.; Schmidt, U.; Macdonald, P. The Clinician’s Guide to Collaborative Caring in Eating Disorders: The New Maudsley Method; Routledge: London, UK, 2010; ISBN 978-0-203-86468-5. [Google Scholar]
- Treasure, J.; Smith, G.; Crane, A. Skills-Based Caring for a Loved One with an Eating Disorder: The New Maudsley Method, 2nd ed.; Routledge: London, UK, 2017; ISBN 978-1-138-82663-2. [Google Scholar]
- Treasure, J.; Smith, G.; Crane, A. Skills-Based Learning for Caring for a Loved One with an Eating Disorder: The New Maudsley Method; Routledge: London, UK, 2007; ISBN 978-0-415-43158-3. [Google Scholar]
- Treasure, J.; Smith, G.; Crane, A.; Karwautz, A.; Wagner, G.; Philipp, J.; Wittek, T. Unterstützung für Angehörige von Menschen mit Essstörungen ein Leitfaden für Eltern, Geschwister, Partner und Fachpersonal; Facultas, Routledge: Vienna, Austria, 2020; ISBN 978-3-7089-1760-3. [Google Scholar]
- Langley, J.; Todd, G.; Treasure, J. Caring for a Loved One with an Eating Disorder: The New Maudsley Skills-Based Training Manual; Routledge: London, UK, 2019; ISBN 978-0-8153-7832-7. [Google Scholar]
- Treasure, J.; Whitaker, W.; Todd, G.; Whitney, J. A Description of Multiple Family Workshops for Carers of People with Anorexia Nervosa. Eur. Eat. Disord. Rev. 2012, 20, e17–e22. [Google Scholar] [CrossRef] [PubMed]
- Miller, W.R.; Rollnick, S. Motivational Interviewing: Preparing People for Change, 2nd ed.; Guilford Press: New York, NY, USA, 2002; ISBN 978-1-57230-563-2. [Google Scholar]
- Prochaska, J.O.; DiClemente, C.C. The Transtheoretical Approach: Crossing Traditional Boundaries of Therapy; Dow Jones-Irwin: Homewood, IL, USA, 1984; ISBN 978-0-87094-438-3. [Google Scholar]
- Ellis, A. Humanistic Psychotherapy: The Rational-Emotive Approach; McGraw-Hill: New York, NY, USA, 1975; ISBN 978-0-07-019237-9. [Google Scholar]
- The Succeed Foundation. How to Care for Someone with an Eating Disorder. Learn. The Techniques Designed by One of the World’s Top. Eating Disorder Researchers. 2011. Available online: https://thenewmaudsleyapproach.co.uk (accessed on 26 April 2021).
- Kromeyer-Hauschild, K.; Wabitsch, M.; Kunze, D.; Geller, F.; Geiß, H.C.; Hesse, V.; von Hippel, A.; Jaeger, U.; Johnsen, D.; Korte, W.; et al. Perzentile für den Body-mass-Index für das Kindes- und Jugendalter unter Heranziehung verschiedener deutscher Stichproben. Mon. Kinderheilkd 2001, 149, 807–818. [Google Scholar] [CrossRef]
- Hilbert, A.; Tuschen-Caffier, B. Eating Disorder Examination: Deutschsprachige Übersetzung; Verlag für Psychotherapie: Münster, Germany, 2006. [Google Scholar]
- Hilbert, A.; Tuschen-Caffier, B. Eating Disorder Examination, 2nd ed.; dgvt-Verlag: Tübingen, Germany, 2016; ISBN 978-3-87159-411-3. [Google Scholar]
- Paul, T.; Thiel, A. EDI-2. Eating Disorder Inventory-2; Hogrefe: Göttingen, Germany, 2005. [Google Scholar]
- Rieger, E.; Touyz, S.W.; Beumont, P.J.V. The Anorexia Nervosa Stages of Change Questionnaire (ANSOCQ): Information Regarding Its Psychometric Properties. Int. J. Eat. Disord. 2002, 32, 24–38. [Google Scholar] [CrossRef]
- Rieger, E.; Touyz, S.; Schotte, D.; Beumont, P.; Russell, J.; Clarke, S.; Kohn, M.; Griffiths, R. Development of an Instrument to Assess Readiness to Recover in Anorexia Nervosa. Int. J. Eat. Disord. 2000, 28, 387–396. [Google Scholar] [CrossRef]
- Pauli, D.; Aebi, M.; Winkler Metzke, C.; Steinhausen, H.-C. Motivation to Change, Coping, and Self-Esteem in Adolescent Anorexia Nervosa: A Validation Study of the Anorexia Nervosa Stages of Change Questionnaire (ANSOCQ). J. Eat. Disord. 2017, 5, 11. [Google Scholar] [CrossRef] [PubMed]
- Arbeitsgruppe Deutsche Child Behavior Checklist. Fragebogen Für Jugendliche; Deutsche Bearbeitung Der Youth Self-Report Form Der Child Behavior Checklist (YSR). Einführung Und Anleitung Zur Handauswertung Mit Deutschen Normen, Bearbeitet von M.; Döpfner, J. Plück, S. Bölte, K. Lenz, P. Melchers & K. Heim (2. Aufl.); Arbeitsgruppe Kinder-, Jugend- und Familiendiagnostik (KJFD): Köln, Germany, 1991. [Google Scholar]
- Ravens-Sieberer, U.; Bullinger, M. News from the KINDL-QuestionnaireA New Version for Adolescents. Qual. Life Res. 1998, 7, 653. [Google Scholar]
- Ravens-Sieberer, U.; Bullinger, M. Assessing Health Related Quality of Life in Chronically Ill Children with the German KINDL: First Psychometric and Content-Analytical Results. Qual. Life Res. 1998, 7, 399–407. [Google Scholar] [CrossRef]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions. Available online: https://handbook-5-1.cochrane.org/ (accessed on 29 April 2020).
- de Zwaan, M. Should we use new media in the treatment of eating disorders? Psychother. Psychosom. Med. Psychol. 2015, 65, 30–32. [Google Scholar] [CrossRef]
- Wagner, G.; Penelo, E.; Wanner, C.; Gwinner, P.; Trofaier, M.-L.; Imgart, H.; Waldherr, K.; Wöber-Bingöl, C.; Karwautz, A.F.K. Internet-Delivered Cognitive-Behavioural Therapy v. Conventional Guided Self-Help for Bulimia Nervosa: Long-Term Evaluation of a Randomised Controlled Trial. Br. J. Psychiatry 2013, 202, 135–141. [Google Scholar] [CrossRef]
- Titov, N.; Hadjistavropoulos, H.D.; Nielssen, O.; Mohr, D.C.; Andersson, G.; Dear, B.F. From Research to Practice: Ten Lessons in Delivering Digital Mental Health Services. J. Clin. Med. 2019, 8, 1239. [Google Scholar] [CrossRef]
- Taylor, C.B.; Fitzsimmons-Craft, E.E.; Graham, A.K. Digital Technology Can Revolutionize Mental Health Services Delivery: The COVID-19 Crisis as a Catalyst for Change. Int. J. Eat. Disord. 2020, 53, 1155–1157. [Google Scholar] [CrossRef]
- Loucas, C.E.; Fairburn, C.G.; Whittington, C.; Pennant, M.E.; Stockton, S.; Kendall, T. E-Therapy in the Treatment and Prevention of Eating Disorders: A Systematic Review and Meta-Analysis. Behav. Res. Ther. 2014, 63, 122–131. [Google Scholar] [CrossRef]
- Fairburn, C.G.; Murphy, R. Treating Eating Disorders Using the Internet. Curr. Opin. Psychiatry 2015, 28, 461–467. [Google Scholar] [CrossRef]
- Eysenbach, G. The Law of Attrition. J. Med. Internet Res. 2005, 7, e11. [Google Scholar] [CrossRef]
- Zeiler, M.; Kuso, S.; Nacke, B.; Klesges, L.M.; Waldherr, K. Evaluating Reach, Adoption, Implementation and Maintenance of Internet-Based Interventions to Prevent Eating Disorders in Adolescents: A Systematic Review. Eur. J. Public Health 2020, 30, 179–188. [Google Scholar] [CrossRef]
- Isserlin, L.; Spettigue, W.; Norris, M.; Couturier, J. Outcomes of Inpatient Psychological Treatments for Children and Adolescents with Eating Disorders at Time of Discharge: A Systematic Review. J. Eat. Disord. 2020, 8, 32. [Google Scholar] [CrossRef] [PubMed]
- Zeeck, A.; Herpertz-Dahlmann, B.; Friederich, H.-C.; Brockmeyer, T.; Resmark, G.; Hagenah, U.; Ehrlich, S.; Cuntz, U.; Zipfel, S.; Hartmann, A. Psychotherapeutic Treatment for Anorexia Nervosa: A Systematic Review and Network Meta-Analysis. Front. Psychiatry 2018, 9, 158. [Google Scholar] [CrossRef] [PubMed]
- Schlegl, S.; Bürger, C.; Schmidt, L.; Herbst, N.; Voderholzer, U. The Potential of Technology-Based Psychological Interventions for Anorexia and Bulimia Nervosa: A Systematic Review and Recommendations for Future Research. J. Med. Internet Res. 2015, 17, e85. [Google Scholar] [CrossRef]
- Berg, E.; Houtzager, L.; Vos, J.; Daemen, I.; Katsaragaki, G.; Karyotaki, E.; Cuijpers, P.; Dekker, J. Meta-analysis on the Efficacy of Psychological Treatments for Anorexia Nervosa. Eur. Eat. Disord. Rev. 2019, 27, 331–351. [Google Scholar] [CrossRef] [PubMed]
| SUCCEAT– WS (N = 48) | SUCCEAT– ONL (N = 50) | p | |
|---|---|---|---|
| Females (%) | 89.6% | 96.0% | 0.218 1 |
| Age (Mean, SD) | 14.65 (1.94) | 15.12 (1.80) | 0.213 2 |
| ED diagnosis (%) | |||
| AN restrictive | 91.7% | 90.0% | 0.945 1 |
| AN binge/purging | 6.3% | 8.0% | |
| Atypical AN | 2.1% | 2.0% | |
| ED duration in months (Mean, SD) | 10.41 (7.10) | 16.03 (16.05) | 0.041 2 |
| BMI (Mean, SD) | 15.54 (2.12) | 16.36 (2.54) | 0.087 2 |
| BMI percentile (Mean, SD) | 8.67 (13.58) | 12.63 (19.77) | 0.252 2 |
| Inpatient treatment (%) | 47.9% | 48.0% | 0.993 1 |
| EDE total score (Mean, SD) | 3.27 (1.62) | 3.32 (1.39) | 0.874 2 |
| EDI-2 total score (Mean, SD) | 67.32 (39.55) | 69.62 (38.79) | 0.776 2 |
| ANSOCQ total score (Mean, SD) | 3.04 (0.98) | 2.81 (1.01) | 0.279 2 |
| YSR total score (Mean, SD) | 42.39 (22.76) | 44.98 (20.65) | 0.561 2 |
| KINDL total score (Mean, SD) | 56.57 (14.78) | 60.16 (13.86) | 0.223 2 |
| Mean ± SD | Time | Time x Group | |||
|---|---|---|---|---|---|
| Baseline | Post-Intervention | 12-Month Follow-Up | F(df), p | F(df), p | |
| BMI | |||||
| Workshop | 15.26 ± 2.12 | 17.04 ± 1.53 | 18.56 ± 2.61 | 70.788 (2,122), <0.001 | 0.321 (2,122), 0.726 |
| Online | 16.13 ± 2.31 | 17.60 ± 2.06 | 19.04 ± 2.16 | ||
| BMI Percentile | |||||
| Workshop | 7.59 ± 12.39 | 16.98 ± 16.44 | 29.41 ± 28.34 | 37.068 (2,122), | 0.073 (2,122), 0.930 |
| Online | 10.2 ± 18.23 | 19.52 ± 20.81 | 30.64 ± 25.02 | <0.001 | |
| EDE total score | |||||
| Workshop | 3.27 ± 1.46 | 2.19 ± 1.50 | 1.68 ± 1.48 | 54.954 (2,118), <0.001 | 0.765 (2,118), 0.468 |
| Online | 3.53 ± 1.21 | 2.35 ± 1.52 | 1.53 ± 1.61 | ||
| EDE restraint | |||||
| Workshop | 3.06 ± 1.89 | 1.50 ± 1.53 | 1.12 ± 138 | 49.061 (2,114), <0.001 | 0.026 (2,114), 0.974 |
| Online | 3.16 ± 1.39 | 1.59 ± 1.50 | 1.14 ± 1.53 | ||
| EDE eating concerns | |||||
| Workshop | 2.39 ± 1.60 | 1.16 ± 1.12 | 1.21 ± 1.26 | 33.877 (2,112), <0.001 | 1.237 (2,112), 0.294 |
| Online | 2.59 ± 1.40 | 1.54 ± 1.43 | 1.04 ± 1.20 | ||
| EDE weight concerns | |||||
| Workshop | 3.58 ± 1.57 | 2.41 ± 1.68 | 1.86 ± 1.78 | 40.513 (2,118), <0.001 | 1.096 (2,118), 0.338 |
| Online | 3.99 ± 1.49 | 2.86 ± 1.79 | 1.72 ± 1.93 | ||
| EDE shape concerns | |||||
| Workshop | 3.71 ± 1.65 | 3.03 ± 1.99 | 2.12 ± 1.91 | 37.742 (2,118), <0.001 | 0.949 (2,118), 0.390 |
| Online | 4.09 ± 1.39 | 3.01 ± 1.68 | 1.93 ± 1.79 | ||
| EDI-2 total score | |||||
| Workshop | 64.77 ± 35.14 | 54.19 ± 36.48 | 50.49 ± 31.85 | 6.867 (2,112), 0.002 | 0.239 (2,112), 0.788 |
| Online | 85.25 ± 35.75 | 69.93 ± 42.65 | 64.38 ± 51.86 | ||
| ANSOCQ total score | |||||
| Workshop | 3.21 ± 0.78 | 3.42 ± 1.06 | 3.65 ± 1.06 | 9.028 (2,116), <0.001 | 0.418 (2,116), 0.660 |
| Online | 2.79 ± 1.02 | 3.22 ± 1.18 | 3.40 ± 1.19 | ||
| YSR total score | |||||
| Workshop | 42.81 ± 23.58 | 35.28 ± 23.16 | 38.95 ± 23.93 | 3.717 (2,118), 0.027 | 0.211 (2,118), 0.810 |
| Online | 51.14 ± 19.11 | 44.93 ± 20.87 | 45.25 ± 23.09 | ||
| KINDL total score | |||||
| Workshop | 57.00 ± 15.90 | 61.84 ± 16.53 | 67.81 ± 16.09 | 10.084 (2,118), <0.001 | 0.912 (2,118), 0.405 |
| Online | 56.83 ± 13.90 | 57.87 ± 14.26 | 62.79 ± 14.75 | ||
| Cohen’s d [95% Confidence Interval] | ||
|---|---|---|
| Workshop Group | Online Group | |
| BMI | 1.17 [0.72; 1.60] | 1.52 [1.01; 2.02] |
| BMI percentile | 0.79 [0.40; 1.17] | 1.06 [0.63; 1.49] |
| EDE total score | 1.06 [0.63; 1.49] | 1.56 [1.02; 2.08] |
| EDE restraint | 1.11 [0.66; 1.55] | 1.22 [0.74; 1.69] |
| EDE eating concerns | 0.76 [0.35; 1.16] | 1.37 [0.86; 1.86] |
| EDE weight concerns | 0.92 [0.51; 1.33] | 1.29 [0.80; 1.76] |
| EDE shape concerns | 0.88 [0.48; 1.28] | 1.40 [0.90; 1.89] |
| EDI-2 total score | 0.26 [−0.11; 0.63] | 0.55 [0.17; 0.93] |
| ANSOCQ total score | 0.32 [−0.05; 0.67] | 0.63 [0.25; 1.00] |
| YSR total score | 0.12 [−0.23; 0.47] | 0.35 [−0.01; 0.72] |
| KINDL total score | 0.54 [0.28; 0.54] | 0.36 [−0.01; 1.20] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Philipp, J.; Franta, C.; Zeiler, M.; Truttmann, S.; Wittek, T.; Imgart, H.; Zanko, A.; Auer-Welsbach, E.; Mairhofer, D.; Mitterer, M.; et al. Does a Skills Intervention for Parents Have a Positive Impact on Adolescents’ Anorexia Nervosa Outcome? Answers from a Quasi-Randomised Feasibility Trial of SUCCEAT. Int. J. Environ. Res. Public Health 2021, 18, 4656. https://doi.org/10.3390/ijerph18094656
Philipp J, Franta C, Zeiler M, Truttmann S, Wittek T, Imgart H, Zanko A, Auer-Welsbach E, Mairhofer D, Mitterer M, et al. Does a Skills Intervention for Parents Have a Positive Impact on Adolescents’ Anorexia Nervosa Outcome? Answers from a Quasi-Randomised Feasibility Trial of SUCCEAT. International Journal of Environmental Research and Public Health. 2021; 18(9):4656. https://doi.org/10.3390/ijerph18094656
Chicago/Turabian StylePhilipp, Julia, Claudia Franta, Michael Zeiler, Stefanie Truttmann, Tanja Wittek, Hartmut Imgart, Annika Zanko, Ellen Auer-Welsbach, Dunja Mairhofer, Michaela Mitterer, and et al. 2021. "Does a Skills Intervention for Parents Have a Positive Impact on Adolescents’ Anorexia Nervosa Outcome? Answers from a Quasi-Randomised Feasibility Trial of SUCCEAT" International Journal of Environmental Research and Public Health 18, no. 9: 4656. https://doi.org/10.3390/ijerph18094656
APA StylePhilipp, J., Franta, C., Zeiler, M., Truttmann, S., Wittek, T., Imgart, H., Zanko, A., Auer-Welsbach, E., Mairhofer, D., Mitterer, M., Laczkovics, C., Schöfbeck, G., Jilka, E., Egermann, W. B., Treasure, J., Karwautz, A. F. K., & Wagner, G. (2021). Does a Skills Intervention for Parents Have a Positive Impact on Adolescents’ Anorexia Nervosa Outcome? Answers from a Quasi-Randomised Feasibility Trial of SUCCEAT. International Journal of Environmental Research and Public Health, 18(9), 4656. https://doi.org/10.3390/ijerph18094656








