Effect of Social Support in Pain Sensitivity in Children with Cerebral Palsy and Typically Developing Children
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Procedure and Measures
2.4. Statistical Analysis
3. Results
3.1. Description of the Sample
3.2. Analysis of Outcome Measures
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Mckinnon, C.T.; Morgan, P.E.; Antolovich, G.C.; Clancy, C.H.; Fahey, M.C.; Harvey, A.R. Pain in children with dyskinetic and mixed dyskinet-ic/spastic cerebral palsy. Dev. Med. Child. Neurol. 2020, 62, 1294–1301. [Google Scholar] [CrossRef]
- Ostojic, K.; Paget, S.; Kyriagis, M.; Morrow, A. Acute and Chronic Pain in Children and Adolescents with Cerebral Palsy: Prevalence, Interference, and Management. Arch. Phys. Med. Rehabil. 2020, 101, 213–219. [Google Scholar] [CrossRef] [PubMed]
- Findlay, B.; Switzer, L.; Narayanan, U.G.; Chen, S.; Fehlings, D. Investigating the impact of pain, age, Gross Motor Function Classification System, and sex on health-related quality of life in children with cerebral palsy. Dev. Med. Child Neurol. 2016, 58, 292–297. [Google Scholar] [CrossRef] [PubMed]
- Østergaard, C.S.; Pedersen, N.S.A.; Thomasen, A.; Mechlenburg, I.; Nordbye-Nielsen, K. Pain is frequent in children with cerebral palsy and negatively affects physical activity and participation. Acta Paediatr. 2021, 110, 301–306. [Google Scholar] [CrossRef] [PubMed]
- Blankenburg, M.; Junker, J.; Hirschfeld, G.; Michel, E.; Aksu, F.; Wager, J.; Zernikow, B. Quantitative sensory testing profiles in children, adolescents and young adults (6–20 years) with cerebral palsy: Hints for a neuropathic genesis of pain syndromes. Eur. J. Paediatr. Neurol. 2018, 22, 470–481. [Google Scholar] [CrossRef]
- Chaleat-Valayer, E.; Roumenoff, F.; Bard-Pondarre, R.; Ganne, C.; Verdun, S.; Lucet, A.; Bernard, J.-C. Pain coping strategies in children with cerebral palsy. Dev. Med. Child Neurol. 2019, 61, 1329–1335. [Google Scholar] [CrossRef] [PubMed]
- van Tilburg, M.A.; Claar, R.L.; Romano, J.M.; Langer, S.L.; Walker, L.S.; Whitehead, W.E.; Abdullah, B.; Christie, D.L.; Levy, R.L. Role of Coping With Symptoms in Depression and Disability. J. Pediatr. Gastroenterol. Nutr. 2015, 61, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.P.; Moore, M.R.; Bockow, T.B.; Ehde, D.M.; Engel, J.M. Psychosocial Factors and Adjustment to Chronic Pain in Persons With Physical Disabilities: A Systematic Review. Arch. Phys. Med. Rehabil. 2011, 92, 146–160. [Google Scholar] [CrossRef] [PubMed]
- Colver, A.; Rapp, M.; Eisemann, N.; Ehlinger, V.; Thyen, U.; Dickinson, O.H.; Parkes, J.; Parkinson, K.; Nystrand, M.; Fauconnier, J.; et al. Self-reported quality of life of adolescents with cerebral palsy: A cross-sectional and longitudinal analysis. Lancet 2015, 385, 705–716. [Google Scholar] [CrossRef]
- Simsek, T.T.; Tuc, G. Examination of the relation between body mass index, functional level and health-related quality of life in children with cerebral palsy. Türk Pediatri Arşivi 2014, 49, 130–137. [Google Scholar] [CrossRef] [PubMed]
- Capjon, H.; Bjørk, I.T. Ambulant children with spastic cerebral palsy and their parents’ perceptions and expectations prior to multilevel surgery. Dev. Neurorehabilit. 2010, 13, 80–87. [Google Scholar] [CrossRef] [PubMed]
- Burkitt, C.C.; Breau, L.M.; Zabalia, M. Parental assessment of pain coping in individuals with intellectual and developmental disabilities. Res. Dev. Disabil. 2011, 32, 1564–1571. [Google Scholar] [CrossRef] [PubMed]
- Engel, J.M.; Jensen, M.P.; Schwartz, L. Coping with chronic pain associated with cerebral palsy. Occup. Ther. Int. 2006, 13, 224–233. [Google Scholar] [CrossRef] [PubMed]
- Martin, L.J.; Hathaway, G.; Isbester, K.; Mirali, S.; Acland, E.L.; Niederstrasser, N.; Slepian, P.M.; Trost, Z.; Bartz, J.A.; Sapolsky, R.M.; et al. Reducing Social Stress Elicits Emotional Contagion of Pain in Mouse and Human Strangers. Curr. Biol. 2015, 25, 326–332. [Google Scholar] [CrossRef] [PubMed]
- Hunter, T.; Siess, F.; Colloca, L. Socially induced placebo analgesia: A comparison of a pre-recorded versus live face-to-face observation. Eur. J. Pain 2014, 18, 914–922. [Google Scholar] [CrossRef]
- Lu, Q.; Tsao, J.C.; Myers, C.D.; Kim, S.C.; Zeltzer, L.K. Coping Predictors of Children’s Laboratory-Induced Pain Tolerance, Intensity, and Unpleasantness. J. Pain 2007, 8, 708–717. [Google Scholar] [CrossRef] [PubMed]
- Montoya, P.; Larbig, W.; Braun, C.; Preissl, H.; Birbaumer, N. Influence of social support and emotional context on pain processing and magnetic brain responses in fibromyalgia. Arthritis Rheum. 2004, 50, 4035–4044. [Google Scholar] [CrossRef] [PubMed]
- Gunnar, M.R.; Hostinar, C.E. The social buffering of the hypothalamic–pituitary–adrenocortical axis in humans: Developmental and experiential determinants. Soc. Neurosci. 2015, 10, 479–488. [Google Scholar] [CrossRef]
- Hohmeister, J.; Demirakca, S.; Zohsel, K.; Flor, H.; Hermann, C. Responses to pain in school-aged children with experience in a neonatal intensive care unit: Cognitive aspects and maternal influences. Eur. J. Pain 2009, 13, 94–101. [Google Scholar] [CrossRef]
- Langer, S.L.; Romano, J.; Brown, J.D.; Nielson, H.; Ou, B.; Rauch, C.; Zullo, L.; Levy, R.L. Sequential analysis of child pain behavior and maternal responses: An observational study. Pain 2017, 158, 1678–1686. [Google Scholar] [CrossRef] [PubMed]
- McMurtry, M.C.; Chambers, C.T.; McGrath, P.J.; Asp, E. When “don’t worry” communicates fear: Children’s perceptions of parental reassurance and distraction during a painful medical procedure. Pain 2010, 150, 52–58. [Google Scholar] [CrossRef]
- Levy, R.L.; Langer, S.L.; Walker, L.S.; Romano, J.M.; Christie, D.L.; Youssef, N.; DuPen, M.M.; Feld, A.D.; Ballard, A.S.; Welsh, E.M.; et al. Cognitive-Behavioral Therapy for Children With Functional Abdominal Pain and Their Parents Decreases Pain and Other Symptoms. Am. J. Gastroenterol. 2010, 105, 946–956. [Google Scholar] [CrossRef]
- Cathcart, S.; Pritchard, D. Reliability of pain threshold measurement in young adults. J. Headache Pain 2006, 7, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Riquelme, I.; Montoya, P. Developmental changes in somatosensory processing in cerebral palsy and healthy individuals. Clin. Neurophysiol. 2010, 121, 1314–1320. [Google Scholar] [CrossRef] [PubMed]
- de Araújo Vitor, C.A.; Ortega, A.D.O.L.; Ferreira, A.C.F.M.; Da Silva, C.A.-A.L.; Gallottini, M.H.C.; Santos, M.T.B.R. Pressure pain threshold of masticatory muscles in children and adolescents with and without intellectual disability: A pilot study. Eur. Arch. Paediatr. Dent. 2021, 1–7. [Google Scholar] [CrossRef]
- Palisano, R.; Rosenbaum, P.; Walterm, S.; Russel, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev. Med. Child Neurol. 1997, 39, 214–223. [Google Scholar] [CrossRef]
- Eliasson, A.-C.; Krumlinde-Sundholm, L.; Rösblad, B.; Beckung, E.; Arner, M.; Öhrvall, A.-M.; Rosenbaum, P. The Manual Ability Classification System (MACS) for children with cerebral palsy: Scale development and evidence of validity and reliability. Dev. Med. Child Neurol. 2006, 48, 549–554. [Google Scholar] [CrossRef]
- Roberts, M.H.; Klatzkin, R.R.; Mechlin, B. Social Support Attenuates Physiological Stress Responses and Experimental Pain Sensitivity to Cold Pressor Pain. Ann. Behav. Med. 2015, 49, 557–569. [Google Scholar] [CrossRef] [PubMed]
- Eccleston, C.; Crombez, G.; Scotford, A.; Clinch, J.; Connell, H. Adolescent chronic pain: Patterns and predictors of emotional distress in adolescents with chronic pain and their parents. Pain 2004, 108, 221–229. [Google Scholar] [CrossRef]
- Swiggum, M.; Hamilton, M.L.; Gleeson, P.; Roddey, T. Pain in Children with Cerebral Palsy: Implications for Pediatric Physical Therapy. Pediatr. Phys. Ther. 2010, 22, 86–92. [Google Scholar] [CrossRef]
- Gosset, B.; Dufour, E.; Jonas, M.-V.; Hiriart, B.; Morelle, S.; Keirel, I.; Longue, V.; Lamy, V. The prevention of pain during botulinum toxin injections in children. Soins 2012, 764, 21–24. [Google Scholar] [CrossRef]
- Duschek, S.; Nassauer, L.; Montoro, C.I.; Bair, A.; Montoya, P. Dispositional empathy is associated with experimental pain reduction during provision of social support by romantic partners. Scand. J. Pain 2019, 20, 205–209. [Google Scholar] [CrossRef] [PubMed]

| Clinical Variable | N |
|---|---|
| Gender | |
| Male | 26 |
| Female | 16 |
| Type of cerebral palsy | |
| Bilateral spastic | 28 |
| Diskinetic | 14 |
| Other (unilateral spastic, ataxic, mixed) | 0 |
| Less affected side | |
| Right | 34 |
| Left | 8 |
| Motor impairment (GMFCS) | |
| Level I | 6 |
| Level II | 8 |
| Level III | 8 |
| Level IV | 4 |
| Level V | 16 |
| Manual impairment (MACS) | |
| Level I | 8 |
| Level II | 4 |
| Level III | 12 |
| Level IV | 2 |
| Level V | 16 |
| Cognitive impairment | |
| None | 26 |
| Mild | 2 |
| Moderate | 6 |
| Severe | 8 |
| Type of schooling | |
| Regular school | 24 |
| Special school | 18 |
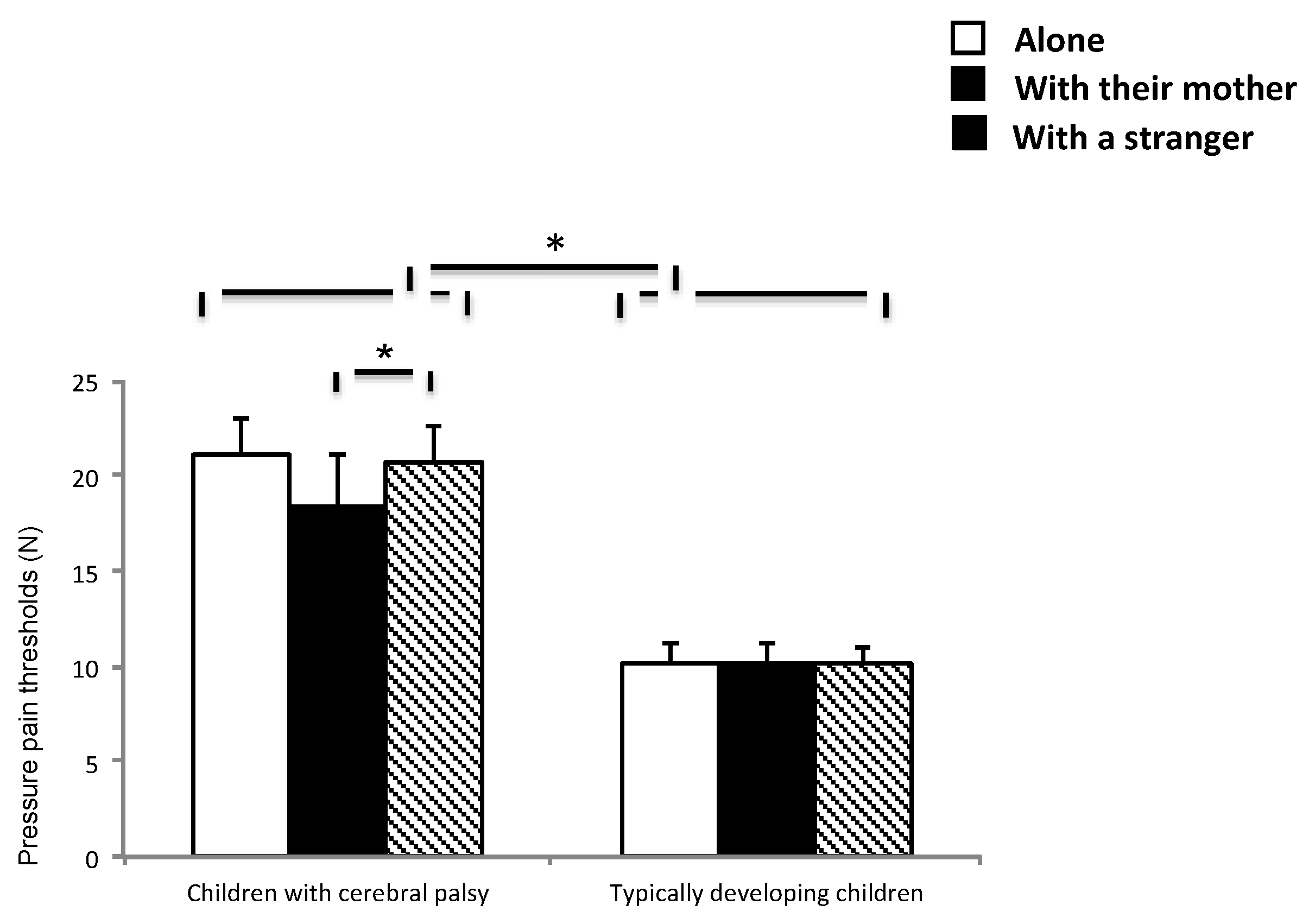
| Mean Difference | Standard Error | Significance Level | 95% Confidence Interval for Difference | |
|---|---|---|---|---|
| Alone | 7.25 | 2.91 | 0.013 | 1.52/12.97 |
| With their mother | 8.37 | 2.96 | 0.005 | 2.54/14.20 |
| With a stranger | 6.97 | 2.85 | 0.015 | 1.35/12.60 |
| Mean Difference | Standard Error | Significance Level | 95% Confidence Interval for Difference | |
|---|---|---|---|---|
| Healthy children | ||||
| Alone vs. with mother | 0.03 | 0.21 | 1.0 | −0.49/0.54 |
| Alone vs. with stranger | −0.01 | 0.15 | 1.0 | −0.37/0.35 |
| Mother vs. stranger | −0.04 | 0.18 | 1.0 | −0.47/0.39 |
| Children with cerebral palsy | ||||
| Alone vs. with mother | −1.09 | 0.64 | 0.27 | −2.63/0.45 |
| Alone vs. with stranger | 0.27 | 0.44 | 1.0 | −0.80/1.33 |
| Mother vs. stranger | 1.36 | 0.54 | 0.036 | 0.063/2.65 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Riquelme, I.; Escobio-Prieto, I.; Oliva-Pascual-Vaca, Á.; Heredia-Rizo, A.M.; Montoya, P. Effect of Social Support in Pain Sensitivity in Children with Cerebral Palsy and Typically Developing Children. Int. J. Environ. Res. Public Health 2021, 18, 4661. https://doi.org/10.3390/ijerph18094661
Riquelme I, Escobio-Prieto I, Oliva-Pascual-Vaca Á, Heredia-Rizo AM, Montoya P. Effect of Social Support in Pain Sensitivity in Children with Cerebral Palsy and Typically Developing Children. International Journal of Environmental Research and Public Health. 2021; 18(9):4661. https://doi.org/10.3390/ijerph18094661
Chicago/Turabian StyleRiquelme, Inmaculada, Isabel Escobio-Prieto, Ángel Oliva-Pascual-Vaca, Alberto Marcos Heredia-Rizo, and Pedro Montoya. 2021. "Effect of Social Support in Pain Sensitivity in Children with Cerebral Palsy and Typically Developing Children" International Journal of Environmental Research and Public Health 18, no. 9: 4661. https://doi.org/10.3390/ijerph18094661
APA StyleRiquelme, I., Escobio-Prieto, I., Oliva-Pascual-Vaca, Á., Heredia-Rizo, A. M., & Montoya, P. (2021). Effect of Social Support in Pain Sensitivity in Children with Cerebral Palsy and Typically Developing Children. International Journal of Environmental Research and Public Health, 18(9), 4661. https://doi.org/10.3390/ijerph18094661









